Chapter 4 – Kidney & Urinary tract disease
64
Persistent or recurrent UTI
The kidney and hypertension
Arthur Guyton (1919-2003): There is no hypertension without malfunction of the kidney
(pressure natriuresis relationship)
Hypertension & kidney disease is a marriage that should be prevented.
Pathophysiology
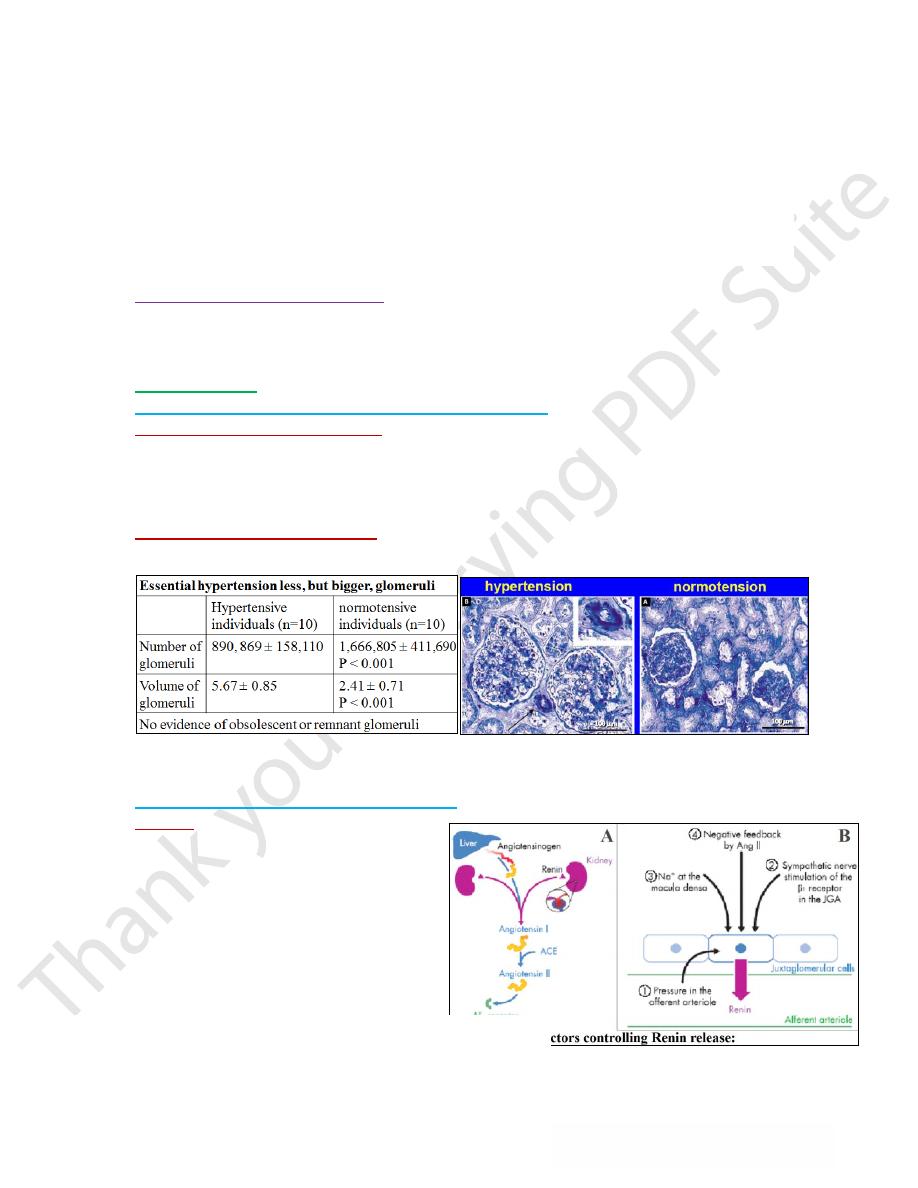
Much of adult pathology has been determined before birth
o
Concept of “prenatal programming”
→developmental plasticity: same genes, different phenotypes
In early life humans are “plastic”, modified by their environment. The critical periods
mostly coincide with periods of rapid cell division. For final nephron number the critical
period is 34-36 weeks- later nephrons are no longer formed
o
Hypothesis-“prenatal programming”
(nephron underdosing) → - Hypertension -
Progression of renal disease
.
The kidney as the cause of hypertension The kidney as the victim of hypertension. Role
of hypertension in CKD patients (progression & CV risk)
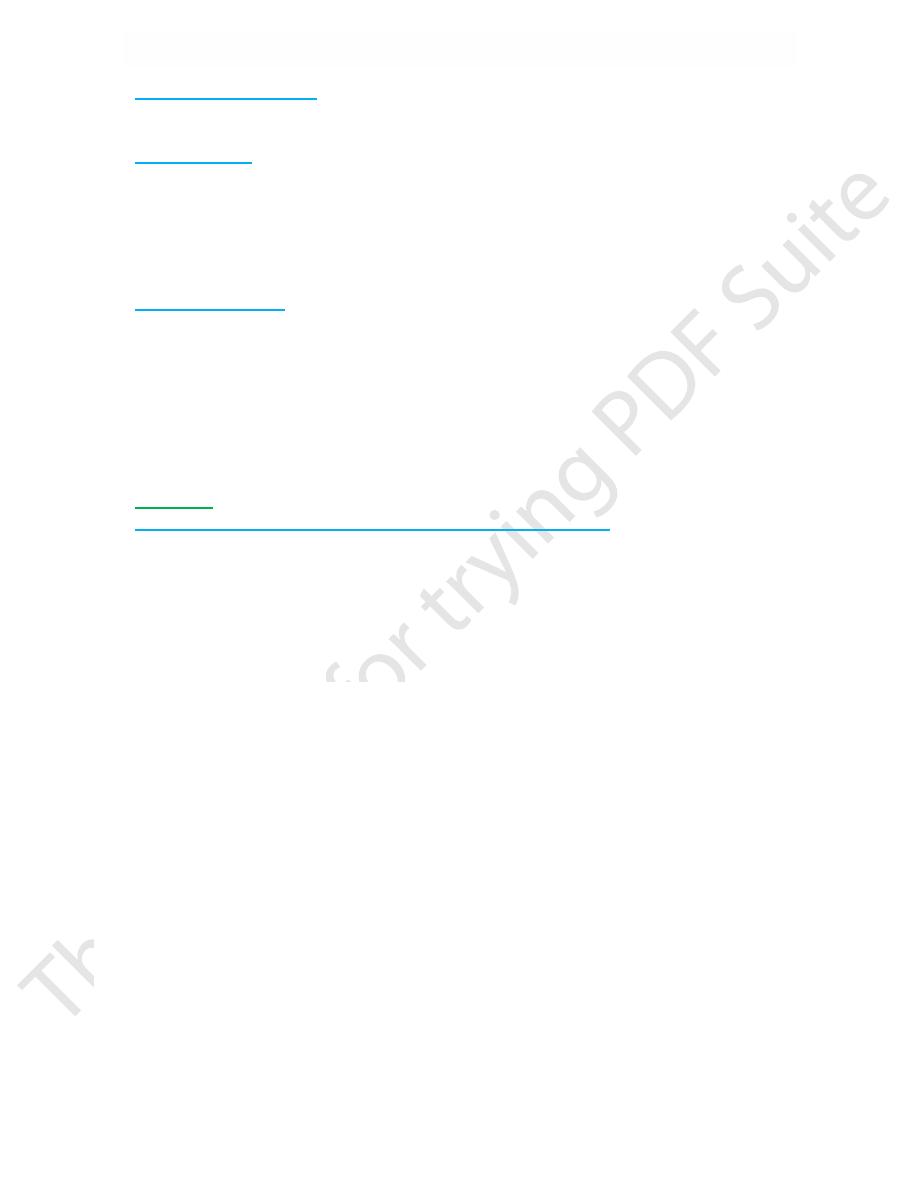
Components of hypertension: Renin - Sodium
o @ Renin
Is an enzyme secreted from specialized cells
in the efferent arteriole of the glomerulus
(JGA). Maintains blood pressure through
vasoconstriction when there is inadequate salt
to maintain volume.
RAS: has a central role in acute & chronic
regulation of BP. RAS blockade was one of the
stunning successes of 20
th
century medicine.
Clinical assessment
Hypertension is a frequent finding in both
acute & chronic renal disease, Depends on type of renal disease & its duration. --
Glomerular – Vascular
Chapter 4 – Kidney & Urinary tract disease
65
Acute glomerular disease:
Patients with acute glomerular disease, such as
poststreptococcal glomerulonephritis or membranous nephropathy, tend to be volume
expanded and edematous due to sodium retention.
Vascular disease
HP is also common in acute vascular diseases, such as vasculitis or scleroderma. In these
settings, the elevation in BP results from ischemia-induced activation of the renin-
angiotensin system rather than volume expansion.
A patient presenting with acute renal failure, hypertension, & red cells and red cell casts
in the urine sediment almost certainly has either glomerulonephritis or vasculitis.
The absence of
edema
in this setting would point strongly toward a primary vascular disease.
Chronic renal failure
Hypertension is present in approximately 80-85% of patients with chronic renal failure.
Data from the Modification of Diet in Renal Disease Study, showed that the prevalence
of hypertension rose progressively from 65 to 95 percent as the GFR fell from 85 to 15
mL/min per 1.73 m
2
Hypertension may occur or be exacerbated in patients with advanced chronic renal failure
treated with erythropoietin.
Patients with end-stage renal disease are more likely to have an increase in pulse pressure
and isolated systolic hypertension (? increased aortic stiffness).
Treatment
Targets of antihypertensive treatment in patients with renal disease
o
130/80 mmHg. if proteinuria > 1g/day lower target values lowering proteinuria to
values as near to normal as possible . to reduce proteinuria ACEI, ARB or combination
are required
o
The desired degree of blood pressure control can usually be safely achieved with
combined therapy: - ACE inhibitor or angiotensin II receptor blocker
- a diuretic - a calcium channel blocker & -a beta blocker.
Acute renal failure
Refers to a sudden and usually reversible loss of renal function, which develops over a
period of days or weeks & is usually accompanied by a reduction in urine volume. There
are many possible causes and it is frequently multifactorial. If cause cannot be rapidly
corrected & renal function restored, temporary renal replacement therapy may be required.
Causes of acute renal failure
Pre-renal:
o
Systemic: - HF - Blood or fluid loss
o
Local: - Renal artery occlusion/stenosis - Diseases affecting arterioles
Intrinsic Renal Disease
o
Acute tubular necrosis/toxic/septic renal failure (85%)
o
Glomerular disease (5%): - Primary - Component of systemic disease
o
Interstitial disease (10%)
Post-renal:
Obstruction (e.g. Stones, Tumour, Prostatic enlargement)
Reversible pre-renal acute renal failure
Because haemodynamic disturbances can initially produce acute renal dysfunction that
has the potential to be rapidly reversed, prompt recognition and treatment are important.
