INVESTIGATION OF RESPIRATORY DISEASES& PRESENTING PROBLEMS IN RESPIRATORY DISEASE
Dr Ghazi F.HajiInterventional cardiology
Al kindi Medical College
INVESTIGATION OF RESPIRATORY DISEASES
CXR PA,LATERAL --Computed tomography (CT) --High-resolution CT (HRCT) --CT pulmonary angiography (CTPA)Ventilation-perfusion imaging
Positron emission tomography (PET)
Pulmonary angiography -Right heart catheterisation
Endoscopic examination( Bronchoscopy)--- Abram's needle
Skin tests( The tuberculin test ,Skin hypersensitivity tests) Immunological and serological tests
Microbiological investigations Sputum, pleural fluid, throat swabs, blood and bronchial washings and aspirates can be examined for bacteria, fungi and viruses.
Histological and pathological examination
Respiratory function testing--- Exercise tests
Arterial blood gases and oximetry
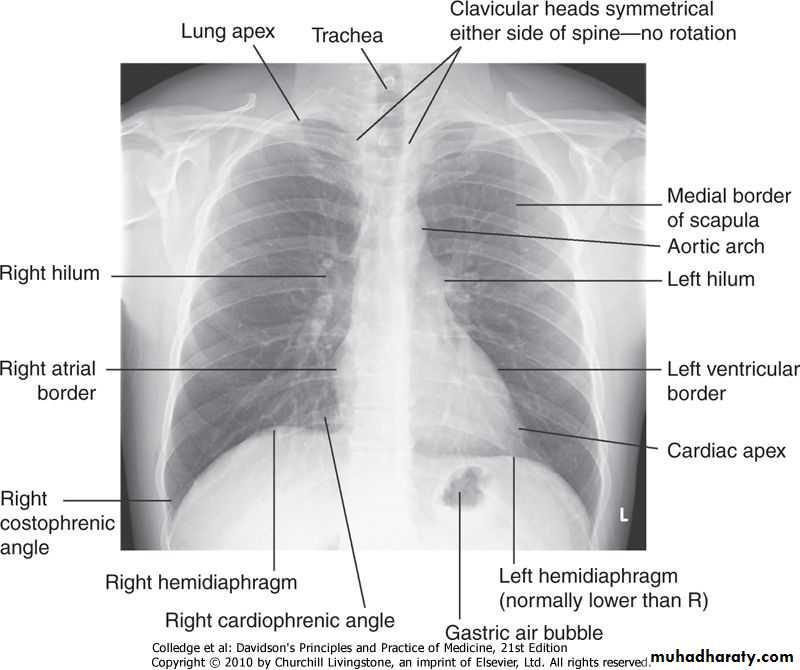
Imaging The 'plain' chest X-ray
This is performed on the majority of patients suspected of having chest disease.A postero-anterior (PA) film provides information on the lung fields, heart, mediastinum, vascular structures and the thoracic cage .
Additional information may be obtained from a lateral film, particularly if pathology is suspected behind the heart shadow or deep in the diaphragmatic
Common chest X-ray abnormalities Pulmonary and pleura
shadowing Consolidation: infection, infarction, inflammation, and rarely bronchoalveolar cell carcinomaLobar collapse:
Solitary nodule:
Multiple nodules: miliary tuberculosis (TB), dust inhalation, metastatic malignancy, healed varicella pneumonia, rheumatoid disease
Ring shadows, tramlines and tubular shadows: bronchiectasis
Cavitating lesions: tumour, abscess, infarct, pneumonia (Staphylococcus/Klebsiella), Wegener's granulomatosis
Reticular, nodular and reticulonodular shadows: diffuse parenchymal lung disease, infection
Pleural abnormalities: fluid, plaques, tumour
Increased translucency
BullaePneumothorax
Oligaemia
Hilar abnormalities :
Unilateral hilar enlargement: TB, bronchial carcinoma, lymphoma
Bilateral hilar enlargement: sarcoid, lymphoma, TB, silicosis
Other abnormalities :Hiatus hernia
Surgical emphysema
Computed tomography (CT)
CT provides detailed images of the pulmonary parenchyma, mediastinum, pleura and bony structures
The displayed range of densities can be adjusted to highlight different structures such as the lung parenchyma, the mediastinal vascular structures or bone
Computed tomography (CT)
High-resolution CT (HRCT)
To provide detailed images of the pulmonary parenchyma and is particularly useful in assessing diffuse parenchymal lung disease, identifying bronchiectasis and assessing the type and extent of emphysema.CT pulmonary angiography (CTPA)
is used increasingly in the diagnosis of pulmonary thromboembolism
w.
Ventilation-perfusion imaging
In this technique, the lungs are imaged using a gamma camera that is able to distinguish two isotopes, inhaled 133Xe (yielding ventilation images) and injected macroaggregates of 99mTc-albumin (yielding perfusion images).Pulmonary emboli appear as perfusion defects with preserved ventilation. However, the utility of this technique is limited in patients with underlying lung disease, in whom up to 70% of scans may be indeterminate. (pulmonary embolism)I.
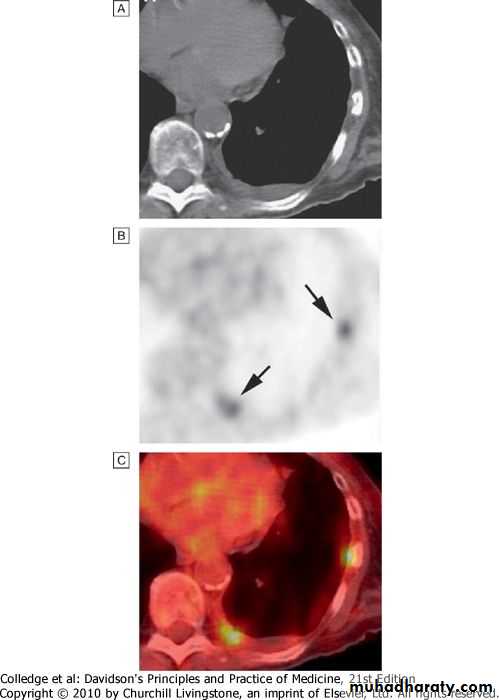
Positron emission tomography (PET)
PET scanners exploit the avid ability of malignant tissue to absorb and metabolise glucose..
Pulmonary angiography
Images taken with contrast medium in the main pulmonary artery are rarely used, particularly now that CTPA is widely available.Right heart catheterisation
remains useful in the investigation of patients with pulmonary hypertension, providing information on pulmonary and right heart pressures.
Endoscopic examination Laryngoscopy The larynx may be inspected indirectly with a mirror or directly with a laryngoscope. Fibreoptic instruments allow a magnified view to be obtained.
Bronchoscopy
1-Flexible bronchoscopy may be performed under local anaesthesia with sedation on an outpatient basis. Structural changes, such as distortion or obstruction, can be seen. Abnormal tissue in the bronchial lumen or wall can be biopsied, and bronchial brushings, washings or aspirates can be taken for cytological or bacteriological examination.
Transbronchial needle aspiration (TBNA) may be used to sample mediastinal lymph nodes and in the staging of lung cancer.
2- Rigid bronchoscopy requires general anaesthesia and is reserved for specific situations such as massive haemoptysis or removal of foreign bodies
..
Investigation of pleural disease
The traditional method of pleural biopsy using an Abram's needle is largely being replaced by the use of core biopsy guided by either ultrasound or CT.Thoracoscopy, which involves the insertion of an endoscope through the chest wall, facilitates biopsy under direct vision and is practised by many surgeons and an increasing number of physicians.
Skin tests --The tuberculin test may be of value in the diagnosis of tuberculosis. Skin hypersensitivity tests are useful in the investigation of allergic diseases .
Immunological and serological tests
The presence of pneumococcal antigen (revealed by counter-immunoelectrophoresis) in sputum, blood or urine may be of diagnostic importance in pneumonia.In blood, high or rising antibody titres to specific organisms (such as Legionella, Mycoplasma, Chlamydia or viruses) may eventually clinch a diagnosis suspected on clinical grounds.
Precipitating antibodies may be found as a reaction to fungi such as Aspergillus.
Microbiological investigations
Of Sputum, pleural fluid, throat swabs, blood and bronchial washings and aspirates can be examined for bacteria, fungi and viruses.:Induced sputum
The use of hypertonic saline to induce expectoration of sputum is useful in facilitating the collection of specimens for microbiology, particularly in patients in whom more invasive procedures such as bronchoscopy are not possible.
Histopathological and cytological examination
Histopathological examination of biopsy material obtained from pleura, lymph node or lung often allows a 'tissue diagnosis' to be made. ( in suspected malignancy or in interstitial lung disease, organisms, such as M. tuberculosis, (Pneumocystis or fungi.
Cytological examination of exfoliated cells in sputum, pleural fluid or bronchial brushings and washings, or of fine needle aspirates from lymph nodes or pulmonary lesions can support a diagnosis of malignancy.
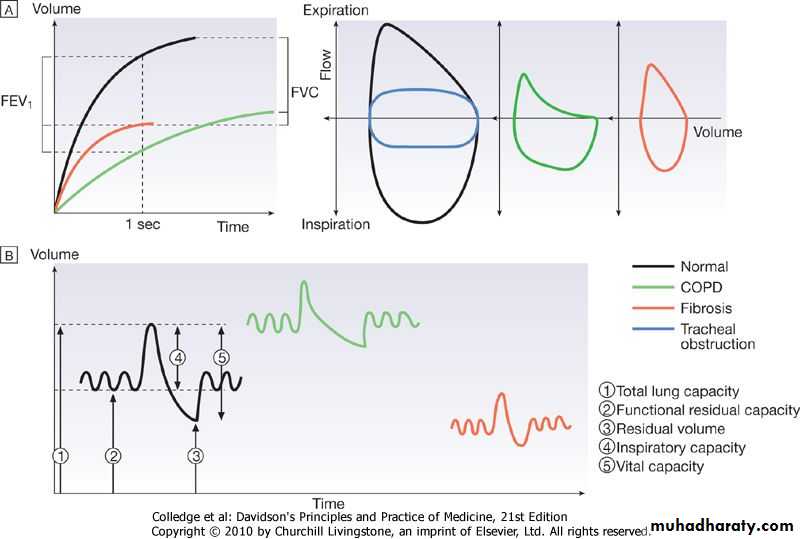
Respiratory function testing
Respiratory function tests are used to aid diagnosis, assess functional impairment, and monitor treatment or progression of disease. Airway narrowing, lung volume and gas exchange capacity are quantified and compared with normal values adjusted for age, gender, height and ethnic origin.Airway narrowing is assessed by asking patients to blow out as hard and as fast as they can into a peak flow meter or a spirometer.
Peak flow meters are cheap and convenient for home monitoring of peak expiratory flow (PEF) in the detection and monitoring of asthma, but values are effort-dependent.
The FEV1 and FVC are obtained from a maximal forced expiration into a spirometer. FEV1 is disproportionately reduced in airflow obstruction, resulting in FEV1/FVC ratios of less than 70%.
When airflow obstruction is seen, spirometry should be repeated following inhaled short-acting β2-adrenoceptor agonists (e.g. salbutamol); reversibility to normal is suggestive of asthma
Lung volume,
Tidal volume and vital capacity (VC) can be measured by spirometry. Total lung capacity (TLC) can be measured by asking the patient to rebreathe an inert non-absorbed gas (usually helium) and recording the dilution of test gas by lung gas. This measures the volume of intrathoracic gas which mixes quickly with tidal breaths. Alternatively, lung volume may be measured by body plethysmography, which determines the pressure/volume relationship of the thorax.Transfer factor
:To measure the capacity of the lungs to exchange gas, patients inhale a test mixture of 0.3% carbon monoxide, which is avidly bound to haemoglobin in pulmonary capillaries. After a short breath-hold, the rate of disappearance of CO into the circulation is calculated from a sample of expirate, and expressed as the TLCO or carbon monoxide transfer factor..Asthma
Chronic bronchitis
Emphysema
Pulmonary fibrosis
FEV1
↓↓
↓↓
↓↓
↓
VC
↓
↓
↓
↓↓
FEV1/VC
↓
↓
↓
→/↑
TLCO
→
→
↓↓
↓↓
TLC
→/↑
↑
↑↑
↓
Arterial blood gases and oximetry
The measurement of hydrogen ion concentration, PaO2 and PaCO2, and derived bicarbonate concentration in an arterial blood sample is essential in assessing the degree and type of respiratory failure and for measuring acid-base status.
Pulse oximeters with finger or ear probes allow non-invasive continuous assessment of oxygen saturation in patients, in order to assess hypoxaemia and its response to therapy.
Exercise tests
Exercise testing with spirometry before and after can be helpful in demonstrating exercise-induced asthma.Walk tests include the self-paced 6-minute walk .
PRESENTING PROBLEMS IN RESPIRATORY DISEASE
OriginCommon causes
Clinical features
Pharynx
Post-nasal drip
History of chronic rhinitis
Larynx
Laryngitis, tumour, whooping cough, croup
Voice or swallowing altered, harsh or painful cough
Paroxysms of cough, often associated with stridor
TracheaTracheitis
retrosternal pain with cough
Bronchi
Bronchitis (acute) and COPD
Dry or productive, worse in mornings
BRONCHI
Asthma
Usually dry, worse at night
Eosinophilic bronchitis
Features similar to asthma but no airway hyper-reactivity (AHR)
Bronchial carcinoma
Persistent (often with haemoptysis)
Lung parenchyma
Tuberculosis
Productive, often with haemoptysis
Pneumonia
Dry initially, productive later
Bronchiectasis
Productive, changes in posture induce sputum production
Pulmonary oedema
Often at night (may be productive of pink, frothy sputum)
Interstitial fibrosis
Dry, irritant and distressing
Drug side-effect
ACE inhibitors
Dry cough
Cough :- Cough is the most frequent symptom of respiratory disease. It is caused by stimulation of sensory nerves in the mucosa of the pharynx, larynx, trachea and bronchi. Acute sensitisation of the normal cough reflex occurs in a number of conditions, and it is typically induced by changes in air temperature or exposure to irritants such as cigarette smoke or perfumes.
Clinical features
Common causesOrigin
History of chronic rhinitis
Post-nasal drip
Pharynx
Voice or swallowing altered, harsh or painful cough
Laryngitis, tumour, whooping cough, croup
Larynx
Paroxysms of cough, often associated with stridor
retrosternal pain with cough
Cough(asthma like) -GERDTracheitis
• Heart burnTrachea
Eosephageal
Dry or productive, worse in morningsBronchitis (acute) and COPD
Bronchi
Usually dry, worse at night
Asthma
Features similar to asthma but no airway hyper-reactivity (AHR)
Eosinophilic bronchitisProductive, often with haemoptysis
TuberculosisLung parenchyma
Dry initially, productive later
Pneumonia
Productive, changes in posture induce sputum production
BronchiectasisOften at night (may be productive of pink, frothy sputum)
Pulmonary oedema
Dry, irritant and distressing
Interstitial fibrosisDry cough
ACE inhibitorsDrug side-effect
Breathlessness
Breathlessness or dyspnoea can be defined as the feeling of an uncomfortable need to breathe. It is unusual among sensations in having no defined receptors, no localised representation in the brain, and multiple causes both in health (e.g. exercise) and in diseases of the lungs, heart or muscles.Pathophysiology
Respiratory diseases can stimulate breathing and dyspnoea by: stimulating intrapulmonary sensory nerves (e.g. pneumothorax, interstitial inflammation and pulmonary embolus)
Chronic exertional dyspnoea
Acute dyspnoeaSystem
Chronic heart failure
Acute pulmonary oedema ()
Cardiovascular
Myocardial ischaemia (angina equivalent)
COPD
Acute severe asthma
Respiratory
Chronic asthma
Acute exacerbation of COPD
Bronchial carcinoma
PneumothoraxInterstitial lung disease (sarcoidosis, fibrosing alveolitis, extrinsic allergic alveolitis, pneumoconiosis)
Pneumonia*Pulmonary embolus
Chronic pulmonary thromboembolism
Acute respiratory distress syndrome (ARDSLymphatic carcinomatosis (may cause intolerable breathlessness)
Inhaled foreign body (especially in the child)Lobar collapseRespiratory
Large pleural effusion(s)
Laryngeal oedema (e.g. anaphylaxis)
Severe anaemiaObesityDeconditioning
Metabolic acidosis (e.g. diabetic ketoacidosis, lactic acidosis, uraemia, overdose of salicylates, ethylene glycol poisoning)
Others
Psychogenic hyperventilation (anxiety or panic-related)
Chest painCardiac
Myocardial ischaemia (angina)Myocardial infarction
Myocarditis
Pericarditis
Mitral valve prolapse
Aortic
Aortic dissection
Aortic aneurysm
Musculoskeletal2 Osteoarthritis
Rib fracture/injury
Costochondritis (Tietze's syndrome)
Intercostal muscle injury
Epidemic myalgia (Bornholm disease)
Oesophageal Oesophagitis
Oesophageal spasm -Mallory-Weiss syndrome
Massive pulmonary embolus Anxiety/emotion1
Peripheral Lungs/pleura Pulmonary infarct
Pneumonia Pneumothorax Malignancy
Tuberculosis Connective tissue disorders
Neurological Prolapsed intervertebral disc
Herpes zoster
Thoracic outlet syndrome
Malignancy
Haemoptysis: Coughing up blood, irrespective of the amount, is an alarming symptom and patients nearly always seek medical advice. A history should be taken to establish that it is true haemoptysis and not haematemesis, or gum or nose bleeding.1-Carcinoma* Bronchiectasis* Acute bronchitis* foreign body
2-Parenchymal disease
Tuberculosis* Suppurative pneumonia Lung abscess Parasites (e.g. hydatid disease, flukes) Trauma
Actinomycosis Mycetoma
3-Lung vascular disease
Pulmonary infarction* Goodpasture's syndrome
Polyarteritis nodosa
Idiopathic pulmonary haemosiderosis
4-Cardiovascular disease
Acute left ventricular failure* Mitral stenosis - Aortic aneurysm
5-Blood disorders
Leukaemia Haemophilia Anticoagulants