Asthma
Dr Ghazi F. HajiIntervention cardiologist
Al kindi medical college
(Obstructive Lung Diseases )
Asthma ,COPD and Bronchiectasis
1
Regarding asthma ;True and False
1-Asthma is a irreversible chronic airway inflammation and increased airway hyper-responsiveness.2- The prevalence of asthma increased in last century.
3-The degree of inflammation is well related to disease severity.
4- Airway hyper-reactivity (AHR)is the tendency for airways to not contract to easily in response to triggers.
5- (10%) of asthmatic patients is externsic.
2
Regarding management of asthma :which is the following not correct.
1- Typical symptoms include recurrent episodes of wheeze, breathlessness and cough with diurnal pattern.
2- To diagnosed asthma patient should has clinical history plus FEV1 ≥ 15%* increase following administration of a bronchodilator .
3- Blood picture may shows peripheral blood Lymphocytosis.
4-Avoidance of aggravating factors is mandatory .
5-A stepwise approach to the management of asthma is applicable .
3
What is the asthma?
what is the prevalence ?what about pathology ?
what about pathophysilogy ?
what are the types of asthma?
what are the clinical features ?
What are the investigations?
what are the lines of treatment ?
What is the prognosis?
4
Introduction
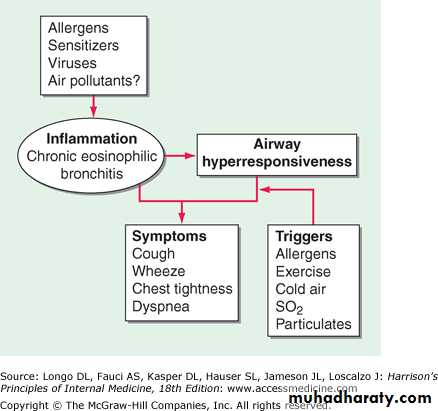
Asthma is a chronic airway inflammatory disease characterize by increased airway hyper-responsiveness.
Typical symptoms include: wheeze, cough, chest tightness and dyspnoea which is variable over short periods of time.
Narrowing of the airways is usually reversible
5
Prevalence
The prevalence of asthma increased in last century.Current estimates suggest that asthma affects 300 million people world-wide and an additional 100 million persons will be diagnosed by 2025.
The socio-economic state play a role control of disease (leads to days lost from school or work) .
Other factors might increase the risk of development of asthma: including duration of breast-feeding, prematurity and low birth weight
6
Risk Factors in Asthma
Endogenous Factors Environmental Factors
Genetic predisposition (twine) Indoor allergens
Atopy Outdoor allergens
Airway hyper responsiveness Occupational sensitizers
Gender Passive smoking
Ethnicity? Respiratory infections Obesity? Diet Early viral infections?
7
T riggers
Allergens ( House dust mites -Pets , cats ,dogs- and fungi (particularly Aspergillus )Upper respiratory tract viral infections
Exercise and hyperventilationCold air - Sulfur dioxide and irritant gases
Drugs (B-blockers, aspirin)
Stress - Irritants (household sprays, paint fumes)
8
Atopy (high level of IgE+ esnophilia + atopic dermitis or other allergic diseases)
@Atopy is the major risk factor for asthma
@Nonatopic individuals have a very low risk of developing asthma.
@Patients with asthma commonly suffer from other atopic diseases, particularly allergic rhinitis, which may be found in over 80% of asthmatic patients, and atopic dermatitis (eczema).@Atopy may be found in 40–50% of the population
9
10
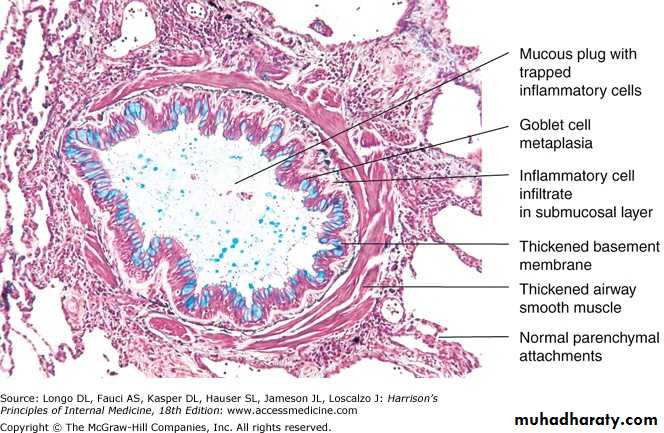
Pathology
@The airway mucosa is infiltrated with activated eosinophils and T lymphocytes, and there is activation of mucosal mast cells.@The degree of inflammation is poorly related to disease severity and may be found in atopic patients without asthma symptoms.
11
12
13
14
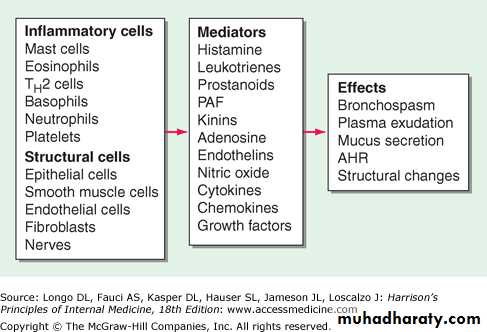
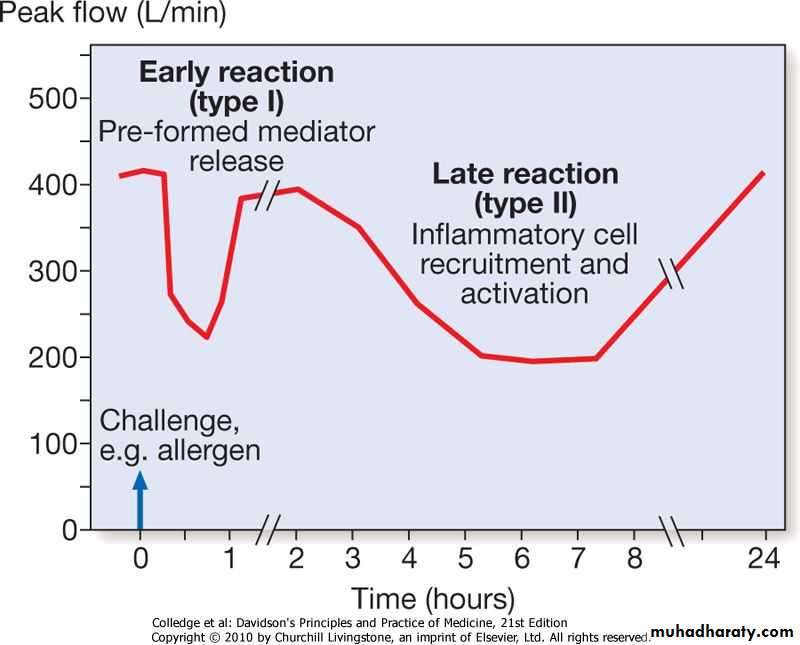
Pathophysiology
Airway hyper-reactivity (AHR)- It is the tendency for airways to contract too easily and too much in response to triggers that have little or no effect in normal individuals.With increasing severity and chronicity of the disease, remodelling of the airway occurs, leading to fibrosis of the airway wall, fixed narrowing of the airway and a reduced response to bronchodilator medication.
Inhalation of an allergen into the airway is followed by a two-phase bronchoconstrictor response with both an early and a late-phase response
15
16
Types of asthma
Externesic asthma (atopic)Intrinsic Asthma (nonatopic )
Aspirin-sensitive asthma
Exercise-induced asthma
‘Nocturnal asthma'.
‘Cough-variant asthma‘
Occupational asthma
17
18
Intrinsic Asthma ( nonatopic )
#A minority of asthmatic patients (approximately10%)#Negative skin tests to common inhalant allergens
#Normal serum concentrations of IgE.
#Later onset of disease (adult-onset asthma),
#Commonly have concomitant nasal polyps, and may be aspirin-sensitive
19
Aspirin-sensitive asthma
Asthma is triggered by medications including:
Asprin (foods containing salicylates. ) NSAID
Alcohol (in particular white wine)
β-adrenoceptor antagonists and
Oral contraceptive pills
These inhibit the cyclo-oxygenase, which leads to shunting of arachidonic acid metabolism through the lipoxygenase pathway, resulting in the production of the cysteinyl leukotrienes
The classical aspirin-sensitive patient is female and presents in middle age which present either with asthma, rhinosinusitis and nasal polyps.
.
20
. Exercise-induced asthma,
hyperventilation results in water loss from fluid of the respiratory mucosa, which in turn triggers mediators to be release.‘Nocturnal asthma'.
symptoms such as cough and wheeze during sleep and disturb sleep
‘Cough-variant asthma'
Cough may be the dominant symptom in some patients, and the lack of wheeze or breathlessness may lead to a delay in reaching the diagnosis
.
21
Occupational asthma
@This type is common in adults, symptoms occur during a particular period of employment and improve during time away from work, e.g. weekends or holidays. Atopic individuals and smokers appear to be at increased risk.
@The most frequently reported causative agents commonly are (Isocyanates -Flour and grain dust -Latex –Animals- Aldehydes –Wood-dust ). Paint sprayers -Bakers -Chemical workers –Animal handlers Welders -Food processing
@The diagnosis of occupational asthma is difficult and requires specialist assessment. Early diagnosis and removal from exposure often results in significant improvement
22
Persistent asthma
@A chronic and complex inflammatory response.@Smooth muscle hypertrophy and hyperplasia, @Thickening of the basement membrane,
@Mucous plugging and epithelial damage result.
@ sputum samples demonstrates eosinophilia,
@In some patients neutrophilic inflammation predominates, and in others, scant inflammation is observed: so-called 'pauci-granulocytic' asthma.23
Clinical features of asthma
Typical symptoms include recurrent episodes of wheeze, chest tightness, breathlessness and cough.Asthma characteristically displays a diurnal pattern, with symptoms and lung function being worse in the early morning.
Classical precipitants include exercise, particularly in cold weather, exposure to airborne allergens or pollutants, and viral upper respiratory tract infections.
An inspection for nasal polyps and eczema should be performed. Rarely, a vasculitic rash may be present in Churg-Strauss syndrom
24
Physical finding
Shortness of breathing ,tachypenia, cyanosis
Tachycardia ,sweating ,wheezy chest
Might be seen deformity of the chest ,use of accessory muscle
Hyperresonance on percussion during attack .
All over chest there is wheezing and rhonchi on auscultation, prolong expiratory phase
Some time ,absent breathing sound occur due to pneumothorax as complication of disease
25
Diagnosis
Pulmonary function test (FEV1,VC,FEF)by spirometery if not available use peak flow meterChallenge test(adenosine)
Skin prick test
CBP
CXR
Sputum
26
Making a diagnosis of asthma Compatible clinical history plus either/or
@FEV1 ≥ 15%* (and 200 mL) increase following administration of a bronchodilator/trial of corticosteroids(( A trial of corticosteroids (e.g. 30 mg daily for 2 weeks))@> 20% diurnal variation on ≥ 3 days in a week for 2 weeks on PEF (the lowest values typically being recorded in the morning) of more than 20% is considered diagnostic
@FEV1 ≥ 15% decrease after 6 min. of exercise
27@Challenge tests using (adenosine &exercise ) develop symptom and drop in lung function
@ Skin prick tests: demonstrated The presence of atopy
@Blood picture may show peripheral blood eosinophilia
@Radiological examination. normal or show hyperinflation of lung fields. Lobar collapse may be seen if mucus occludes a large bronchus, allergic bronchopulmonary aspergillosis
@An induced sputum differential eosinophil count of greater than 2%
@Measurement of total and allergen-specific IgE.
28
Management
1-Asthma education :Whenever possible, patients should be encouraged to take responsibility for managing their own disease. And Encourage to understand the nature of the condition, the relationship between symptoms and inflammation,2-The use of PEF to guide management decisions.
3-Enviromental control :Avoidance of aggravating factors.(reducing exposure to relevant antigens, e.g. a pet animal, House dust mite ,reduce fungal exposure ,Smoking cessation)
29
30
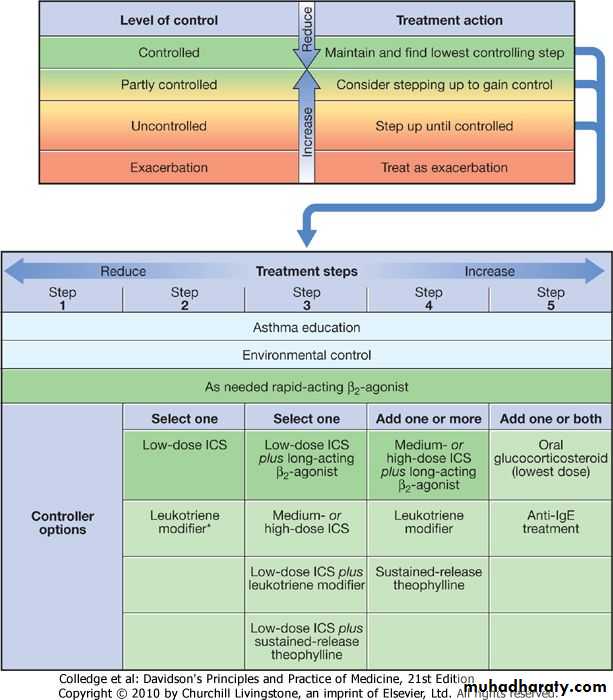
A stepwise approach to the management of asthma
Step 1: Occasional use of inhaled short-acting β2-adrenoreceptor agonist bronchodilators@For patients with mild intermittent asthma (symptoms less than once a week for 3 months and fewer than two nocturnal episodes/month), it is usually sufficient to prescribe an inhaled short-acting β2-agonist (salbutamol or terbutaline), to be used on an as-required basis.
@A history of a severe exacerbation should lead to a step up in treatment.
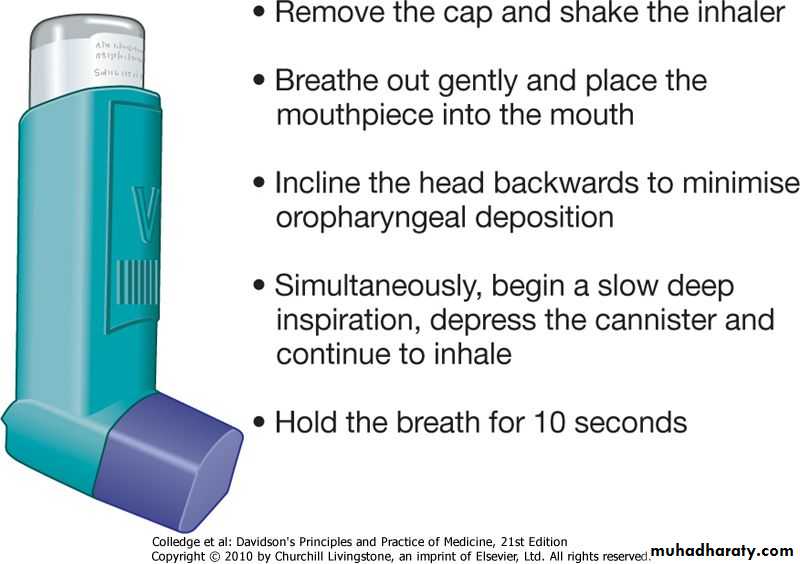
@A variety of different inhaled devices are available ,The metered-dose inhaler remains the most widely prescribed .
31
32
Step 2: Introduction of regular 'preventer' therapy Regular anti-inflammatory therapy (preferably inhaled corticosteroids (ICS) such as beclometasone, budesonide, fluticasone or ciclesonide) should be started in addition to inhaled β2-agonists taken on an as-required basis in any patient who
1-Has experienced an exacerbation of asthma in the last 2 years
2-Who used inhaled β2-agonists three times a week or more
3-Who reports symptoms three times a week or more4-Who was wakened by asthma one night per week.
33Step 3: Add-on therapy
If a patient remains poorly controlled despite regular use of ICS, a review should be undertaken focusing on adherence, inhaler technique and on-going exposure to modifiable aggravating factors.Add-on therapy should be considered in adults taking 800 μg/day BDP (or equivalent)in dose ICS.
Long-acting β2-agonists (LABAs), such as salmeterol and formoterol,(least 12 hours), represent the first choice of add-on therapy.
34
cont.
Fixed combination inhalers of ICS and LABAs have been developed; these are more convenient, increase compliance, and prevent patients using a LABA as monotherapy (which may be accompanied by an increased risk of life-threatening attacks or asthma death).
Oral leukotriene receptor antagonists (e.g. montelukast 10 mg daily) may facilitate a reduction in the dose of ICS and control exacerbations.
Oral theophyllines may be considered in some patients
35
Step 4: Poor control on moderate dose of inhaled steroid and add-on therapy: addition of a fourth drug
#Regular therapy with low-dose budesonide reduces the risk of severe exacerbations in patients with mild persistent asthma.
In adults, the dose of ICS may be increased to 2000 μg BDP/budesonide (or equivalent) daily.
#A nasal corticosteroid preparation should be used in patients with prominent upper airway symptoms.
#Oral therapy with leukotriene receptor antagonists, theophyllines or a slow-release β2-agonist may be considered.
#Oral itraconazole should be contemplated in patients with allergic bronchopulmonary aspergillosis (ABPA)'
36
Step 5: Continuous or frequent use of oral steroids
@At this stage prednisolone therapy (usually administered as a single daily dose in the morning) should be prescribed in the lowest amount necessary to control symptoms.@Patients on long-term oral corticosteroids (> 3 months) or receiving more than three or four courses per year will be at risk of systemic side-effects.
@Osteoporosis can be prevented in this group of patients by using bisphosphonates .
@Steroid-sparing therapies such as methotrexate, ciclosporin or oral gold may be considered.
@New therapies, such as omalizumab, a monoclonal antibody directed against IgE, may prove helpful in atopic patients.
37
Indications for Short courses of 'rescue' oral corticosteroids (prednisolone 30-60 mg daily) Tapering of the dose to withdraw treatment is not necessary unless given for more than 3 weeks
1-Symptoms and PEF progressively worsening day by day
2-Fall of PEF below 60% of the patient's personal best recording
3-worsening of sleep disturbance by asthma4-Persistence of morning symptoms until midday
5-Progressively diminishing response to an inhaled bronchodilator6-Symptoms severe enough to require treatment with nebulised or injected bronchodilators
38Step-down therapy
#Once asthma control is established, the dose of inhaled (or oral) corticosteroid should be titrated to the lowest dose at which effective control of asthma is maintained.#Decreasing the dose of ICS by around 25-50% every 3 months is a reasonable strategy for most patients
39
40
41
A metered-dose inhaler (MDI) is a device that delivers a specific amount of medication to the lungs, in the form of a short burst of aerosolized medicine that is inhaled by the patient..
The medication in a metered dose inhaler is most commonly a bronchodilator, corticosteroid or a combination of both for the treatment of asthma and COPD. Other medications less commonly used but also administered by MDI are mast cell stabilizers, such as cromoglicate or nedocromil.
42
43
44
Asthma in pregnancy
Unpredictable clinical course: 1/3 worsen, 1/3remain stable and 1/3 improve.Labour and delivery: 90% have no symptoms.
Safety data: good for β2-agonists, inhaled steroids, theophyllines, oral prednisolone, and chromones.
Oral leukotriene receptor antagonists: no evidence that these harm the fetus
Steroids: women on maintenance prednisolone > 7.5 mg/day should receive hydrocortisone 100 mg 6-8-hourly during labour.
Prostaglandin F2α: may induce bronchospasm and should be used with extreme caution.
Breastfeeding: use medications as normal.
Uncontrolled asthma represents the greatest danger to the fetus: Associated with maternal (hyperemesis, hypertension, pre-eclampsia, vaginal haemorrhage, complicated labour) and fetal (intrauterine growth restriction and low birth weight, preterm birth, increased perinatal mortality, neonatal hypoxia) complications.
45
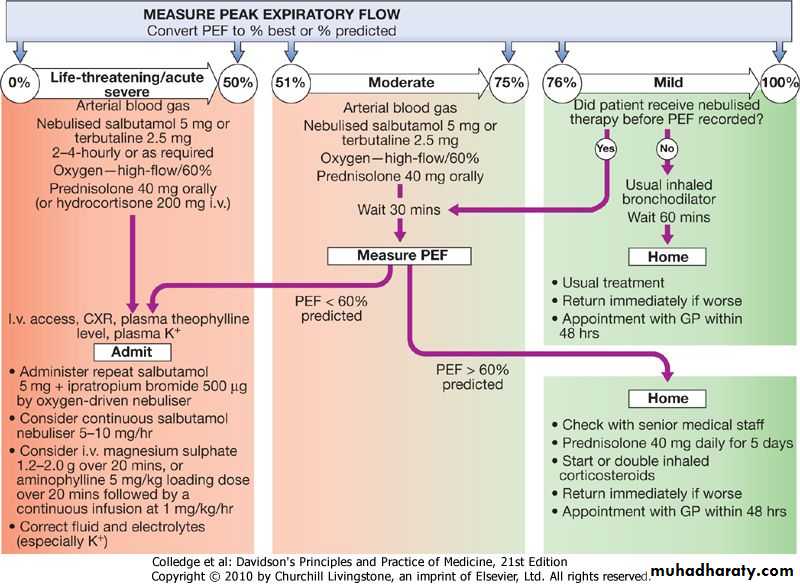
Acute severe asthma
Immediate assessment of acute severe asthma1-PEF 33-50% predicted (< 200 L/min)
2-Respiratory rate ≥ 25/min
3-Heart rate ≥ 110/min
5-Inability to complete sentences in 1 breath
Arterial blood gas analysis is essential to determine the PaCO2, a normal or elevated level being particularly dangerous.
A chest X-ray is not immediately necessary unless pneumothorax is suspected.
46
Life-threatening features of acute severe asthma
1-PEF < 33% predicted (< 100 L/min)2-SpO2 < 92% or PaO2 < 8 kPa (60 mmHg) (especially if being treated with oxygen)
3-Normal or raised PaCO2
4-Silent chest -Cyanosis -Feeble respiratory effort
5-Bradycardia or arrhythmias -Hypotension
6-Exhaustion -Confusion -Coma
47
Treatment
@Admission to hospital
@Oxygen
@High doses of inhaled
bronchodilators.
@Ipratropium bromide
@Systemic corticosteroids
@Intravenous aminophylline
@Intravenous magnesium
@Endotracheal intubation and intermittent positive pressure ventilation(mechanical ventilator )
48
49
Treatment of Life-threatening
@Oxygen. High concentrations of oxygen (humidified if possible).@High doses of inhaled bronchodilators. Short-acting β2-agonists are the agent of first choice. administered via a nebuliser driven by oxygen.
@Ipratropium bromide should be added to salbutamol in patients with acute severe or life-threatening attacks.
@Systemic corticosteroids. administered orally as prednisolone, but intravenous hydrocortisone may be given in patients who are vomiting or unable to swallow
50
@Intravenous fluids. (?)
@Potassium supplements may be necessary because repeated doses of salbutamol can lower serum potassium.@Intravenous magnesium is bronchodilatation whose presenting PEF is < 30% predicted.
@Some patients benefit from the use of intravenous aminophylline but careful monitoring is required.
@Intravenous leukotriene receptor antagonists (remains (under investigation
51@Monitoring of treatment : PEF should be recorded every 15-30 minutes and then every 4-6 hours.
@Pulse oximetry should ensure that SaO2 remains > 92%, but repeat arterial blood gases are necessary if :
the initial PaCO2 measurements were normal or raised,
the PaO2 was < 8 kPa (60 mmHg) or
the patient deteriorates
@ CXR : to exclude Pnuemothorax
52
Indications for endotracheal intubation and intermittent positive pressure ventilation acute severe asthma
Coma
Respiratory arrest
Deterioration of arterial blood gas tensions despite optimal therapy
PaO2 < 8 kPa (60 mmHg) and falling
PaCO2 > 6 kPa (45 mmHg) and rising
pH low and falling (H+ high and rising)
Exhaustion, confusion, drowsiness
53
54
55
Prognosis
The outcome from acute severe asthma is generally good. Death is fortunately rare
#Failure to recognise the severity of an attack, on the part of either the assessing physician or the patient, contribute to undertreatment and delay in delivering appropriate therapy.
#Prior to discharge, patients should be stable on discharge medication (nebulised therapy should have been discontinued for at least 24 hours) and the PEF should have reached 75% of predicted or personal best.
#The acute attack provides an opportunity to look for and address any trigger factors, for the delivery of asthma education and for the provision of a written self-management plan.
.
56
Byssinosis
Byssinosis occurs as a result of exposure to cotton brack (dried leaf and plant debris) in cotton and flax mills.An acute form of the disease occurs in about one-third of individuals on first exposure to cotton dust and is characterised by an acute bronchiolitis with symptoms and signs of airflow obstruction.
.
The condition is more common in smokers.
Typical symptoms include chest tightness or breathlessness accompanied by a drop in lung function; classically, these are most severe on the first day of the working week ('Monday fever') or following a period away from work.
Affected workers should be offered alternative employment. Continued exposure leads to the development of persistent symptoms and a progressive decline in FEV1.
57
Regarding asthma ;True and False
1-Asthma is a irreversible chronic airway inflammation and increased airway hyper-responsiveness. F2- The prevalence of asthma increased in last century. T
3-The degree of inflammation is well related to disease severity. F
4- Airway hyper-reactivity (AHR)is the tendency for airways to not contract to easily in response to triggers. F
5- 10% of asthmatic patients is externsic. F
58
Regarding management of asthma :which is not correct.
1- Typical symptoms include recurrent episodes of wheeze, breathlessness and cough with diurnal pattern.2- To diagnosed asthma patient should has clinical history plus FEV1 ≥ 15%* increase following administration of a bronchodilator.
3- Blood picture may show peripheral blood Lymphocytosis.
4-Avoidance of aggravating factors is mandatory .
5-A stepwise approach to the management of asthma is applicable .
59
60