Chapter 3 – Epidemiology of infectious diseases (Other infections)
233
“” Emporiatric medicine & the HIV-infected traveler “”
Issues for all travelers
Generally want at least 4-6 week lead time prior to departure to assess travel needs,
especially vaccines & need for malaria chemoprophylaxis
Get list of medical clinics from IAMAT www.iamat.org
Bring 30-35% DEET spray where biting insects are anticipated
Avoid piercings and tatoos, acupuncture, even shaving by a barber in many of these
developing areas
Be cautious of motor vehicle travel
Swim only in chlorinated water
Health insurance: both international insurance(try credit card companies, yellow pages,
internet) and air ambulance insurance: www.airambulancedirectory.com
Specific precautions for enteritis
Developing countries: especially important in patients with severe immunosuppression
Food and waterborne diseases: same precautions for all travelers regardless of HIV serostatus
If you can’t boil it, peel it, cook it, then forget it!!
No tap water, ice cubes. Bottled water, including for brushing teeth!
Portable water purifiers ( with absolute one micron filter)
Traveler’s diarrhea
If traveler’s diarrhea is severe: must seek medical attention (gi bleeding, fever, vomiting, prostration)
Enterotoxigenic E. coli probably no different in it’s presentation, but Salmonella,
Campylobacter, Shigella can be worse in HIV+ people
Occasional microsporidia (J Travel Med 1999 Dec;6(4):223-7), enteroaggregative E.
coli(CID 2001 Jun 15;32(12):1706-9), and Cryptosporidia
Other causes of enteritis eg,Cyclospora, Isospora belli, helminths, C. difficile, tropical sprue
Treatment for uncomplicated disease: cipro 500mg BID for three to seven days with first
day imodium.
Self-medication for other ailments
Options of self-medication: for respiratory tract infection, sinusitis, otitis media,UTI, cellulitis
International screening of travelers for HIV infection
Primarily aimed for those with extended stays: work visas, students. Approximately 50
countries may block entry of HIV+ travelers
Check with consular office(s) or go to www.travelstate.gov/hivtestingreqs.html
Our own calls to Brazilian, Canadian, and British consulates did not bear out any refusal
to have HIV+ travelers in their nation for short-term stay. However, long-term stay
decided on case by case basis.
Timing of HAART across time zones
Take more doses in the period than less.
East to West: extra dose of Nukes, viramune & PIs at bedtime
West to East: extra dose next morning
Chapter 3 – Epidemiology of infectious diseases (Other infections)
234
Efavirenz doesn’t need an extra dose (G. Moyle, personal comm.).
Viread has long intracellular half-life and may not need an extra dose
Debatable what to do with indinavir with respect to risk of nephrolithiasis
Drug and medical care issues
- Adequacy of supply of medications, including need for refrigeration and avoidance of
damp places. - Adequacy of medical care in destination, especially important in
prolonged stays-consult with IAMAT
- Avoid if possible, new medication changes just prior to travel
Malaria prevention
Same precautions and prophylaxis with all travelers
Review itinerary on www.cdc.gov malaria site
Disease presentation not different in HIV, except more severe in HIV-positive pregnant women
Mosquito bite prevention with 30-35% DEET, bed netting, permethrin spray, and
avoidance of dusk to dawn exposure
Drug interactions: mefloquine had variable effects on ritonavir, with decrease in Cmax,
Cmin, AUC. Despite strong inhibition of CYP3A4, mefloquine levels were not
affected by ritonavir (Khaliq et al, 7
th
Conf on Retro, abstract 92, 2000)
Malarone: Proguanil AUC increased possibly via CYP 2D6, Atovaquone AUC may be
decreased in presence of Ritonavir, mechanism unknown (Karp, Current Inf Dis Rep
2001, 3:50-8)
Despite these observations, there are currently no dose adjustments recommended at this time.
Measure patient’s glucose-6-phosphate dehydrogenase level prior to trip (possible need
for primaquine)
Malaria treatment
Quinidine: AUC increased by ritonavir via CYP3A4 inhibition. Quinidine reserved for
severe malaria and decrease in maintenance rate of drug required. Quinine probably
increased to lesser extent and should be avoided (risk of prolonged QT interval with
Torsades de pointes)
Treat non-severe malaria with malarone 4 pills/day for three days, or with lariam
(increased risk of seizures).
Self-treatment not generally advised
Vaccine issues in HIV+ traveler
Potential exposure to pathogen
Potential increase in side effects to vaccine
Potential decreased efficacy of vaccine
Vaccines
In most developing areas of world, following vaccine-preventable illnesses are addressed:
Measles, Hepatitis A, Typhoid Fever, Influenza, Yellow fever, Hepatitis B, Polio,
Japanese encephalitis, Rabies, Cholera, Meningococcus
Types of Vaccines
Killed (inactivated): Hepatitis A, Inactivated Polio (IPV), Rabies, Japanese encephalitis
Live (attenuated): MMR, Yellow fever, oral Typhoid
Chapter 3 – Epidemiology of infectious diseases (Other infections)
235
Subunit: Hepatitis B
Polysaccharide: Pneumococcal, Meningococccal, Typhoid Vi
Split antigen: Influenza
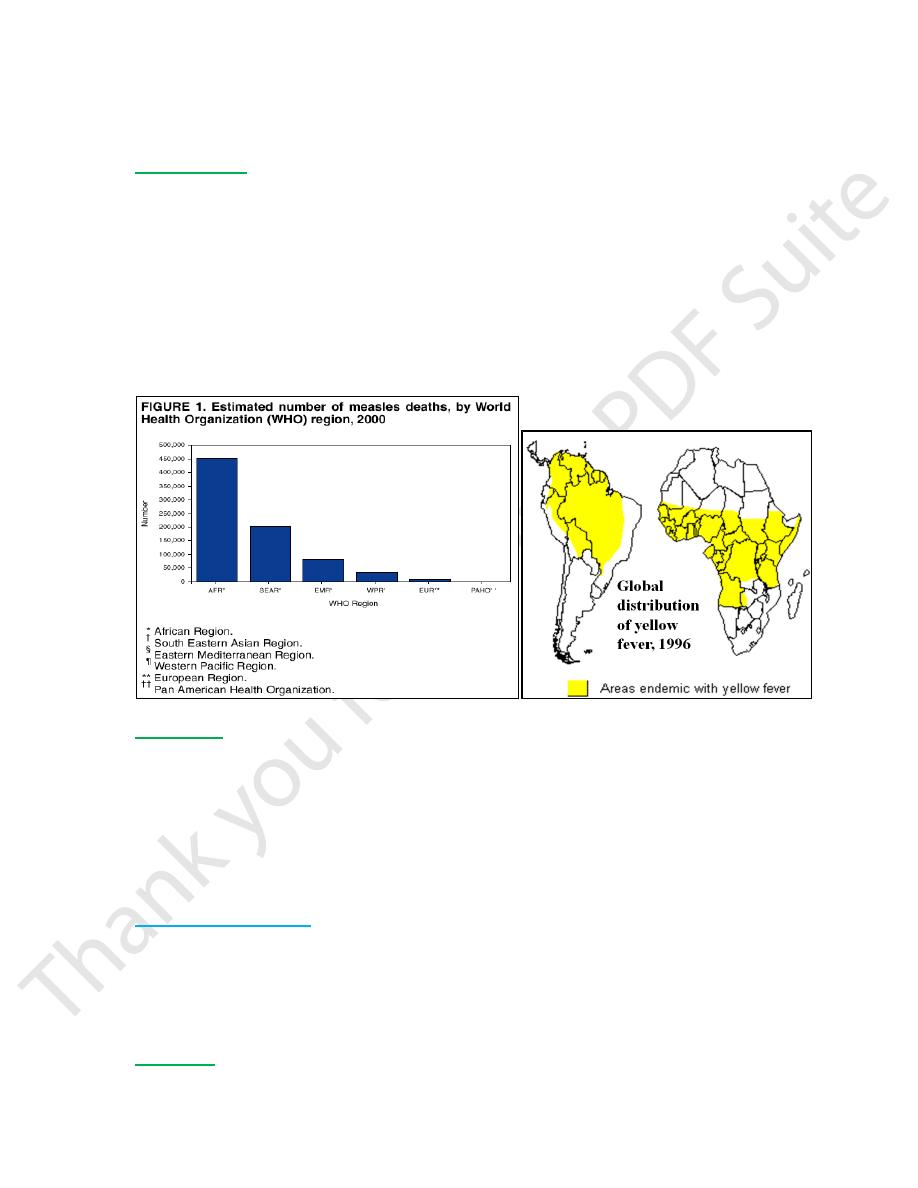
Measles vaccine
Increased prevalence of disease in SE Asia, Africa (especially sub-Saharan) based on
W.H.O. data on measles in children. Worse disease with increased morbidity and
mortality in HIV-infected people with pneumonitis & also encephalitis.
Increased risk of vaccine side effects in severely immunosuppressed: one known death in
patient with AIDS and deaths in other immunosuppressed recipients.
Vaccine considered safe in adults if T-helper count >200 &/or T-helper % >14%
If immune serum globulin prescribed to prevent Hep A, separate injections by at least
two weeks. Role of measuring serum IgG measles antibody
Use of gammaglobulin if inadequate antibody in AIDS, dose suggested is 15 ml IM.
IVIG may also be okay.
Yellow fever
Mosquito-borne disease in tropical South America and Sub-Saharan Africa
Severity of illness from flu-like illness to severe hepatitis and hemorrhagic fever with a
classic biphasic illness. Fatality rate of severe disease ranges from 20% to 65%
Not known if HIV influences presentation of illness
Asymptomatic HIV+ recipients of vaccine without adverse effects
Lower antibody titers in HIV+ children
Consider measurement of antibody titer after vaccination. Vaccine not recommended in
symptomatic HIV-positive adults, certainly not if T-helper count <200.
Options to taking vaccine:
1. Avoiding areas of transmission altogether
2. If in an area of potential exposure, meticulously avoiding mosquito bites
3. Vaccine waiver letter-this may not be accepted at border. Need to arrange this with
consulate prior to leaving USA
4. Distinguish requirements of country from actual zones of endemicity
Hepatitis A
Vaccine response is lower in HIV+ patients, with dramatically low response rate in
patients with <200 cells/mm3 (Kemper et al, JID 2003 April 15; 187(8):1327-31)
Chapter 3 – Epidemiology of infectious diseases (Other infections)
236
Know if measurable IgG prior to travel. However, actual protective titer against infection
is unknown.
Generally, if less than one month prior to travel, give immune serum globulin with option
of starting Hepatitis A vaccine series at same time. There are no current
recommendations for an accelerated schedule.
Dose of immune serum globulin: 0.02 ml/kg body weight IM for trip less than 3 months.
If longer trip, give 0.06 ml/kg IM.
Prolonged viral shedding reported in HIV+ patients with acute Hep A
Hepatitis B
Know immune status prior to travel. Risk to international travelers generally low
Must warn susceptible patients of sexual risk of acquisition
Consider extra doses of vaccine if patient a non-responder (Rey et al Vaccine 2000 Jan
18; 18(13):1161-5)
Meningococcus
Endemic to sub-Sahara Africa during the dry season, occasional epidemics reported
elsewhere. Vaccine required for annual Hajj in Mecca. Very scant information on HIV
and disease. No mention on efficacy of vaccine in HIV infection
Japanese encephalitis
Caused by a flavivirus, transmitted by mosquito
Endemic to rural areas of SE Asia, varies often with season
Most cases are subclinical. Symptomatic disease presents as an acute encephalitis--
seizures, paralysis, coma, death; prolonged recovery in survivors and permanent brain
injury in some
It is a rare disease of travelers. Killed vaccine recommended for travelers with prolonged
stays in endemic areas. Vaccine occasionally causes severe allergic reaction requiring
emergent care. One study demonstrating reduced antibody titers in HIV+ children
vaccinated with JE vaccine
Alteration in presentation of illness in HIV-infected people not known
Polio
Most world transmission currently in south Asia and sub-Sahara Africa
Only inactivated polio vaccine (IPV) available in the USA
Usually give one adult dose, unless primary series never done or completed
Other vaccines
- Typhoid: two vaccines available: one live and one killed-use only the latter in HIV+ patients.
- Typhim Vi has lower antibody response rate in patients with less than 200 CD4+ T
lymphs (Vaccine 1999 Aug 6;17(23-24):2941-45)
- Influenza-year-round endemicity in the tropics and April - September in southern
hemisphere. No recommendations on revaccinating prior to travel
- Diptheria/Tetanus - Pneumococcus
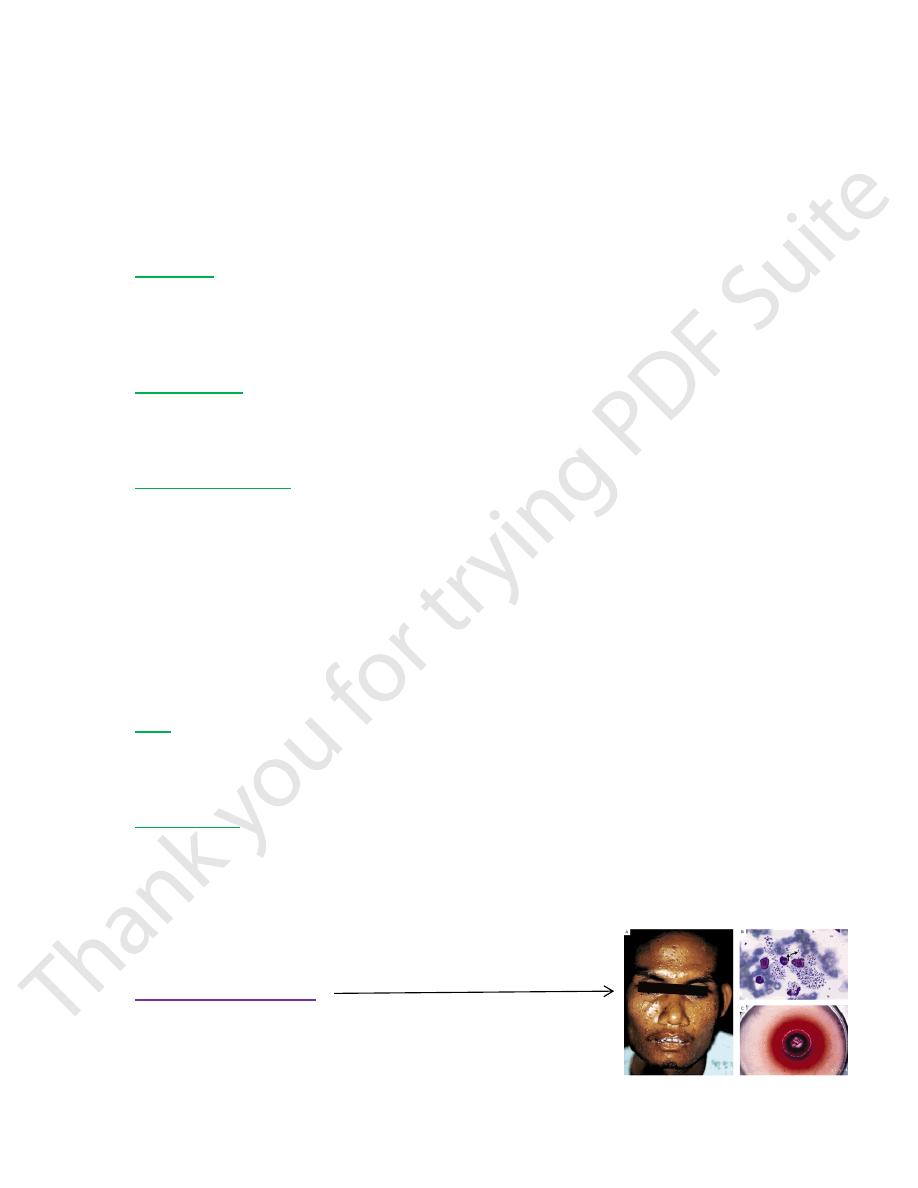
Penicillium marneffei
Fungal infection endemic to SE Asia, acquired by inhaling spores.
Opportunistic infection in AIDS. Chronic illness with fever, weight loss,
anemia, generalized lymphadenopathy, hepatomegaly, umbilicated
papules. Other organ systems can also be involved. Diagnosis: bone
marrow, skin lesion, blood culture. Treatment: Ampho B, followed by itraconazole
Chapter 3 – Epidemiology of infectious diseases (Other infections)
237
Visceral leishmaniasis
Protozoan parasite transmitted by sandflies. 90% world cases acquired in India,
Bangladesh, Sudan, Nepal, Brazil; & also endemic in Mediterranean countries
Typically a chronic illness with prolonged incubation period Typically have
hepatosplenomegaly, fevers, weight loss
In AIDS, worse cytopenias, and atypical presentations: pleuropulmonary, GI
Serologic tests less sensitive in AIDS. Lower treatment response in AIDS
HAART and secondary prophylaxis improves survival
Tuberculosis
Know PPD status prior to trip
Repeat PPD after return, especially after prolonged trip.
Risk of acquisition might be much higher in health care setting
Approach to the returning HIV-positive traveler
Review dates and itinerary
More aggressive evaluation of asymptomatic patient if visit to developing areas was prolonged
For symptomatic patients, check incubation periods for the more common diseases of travelers:
Short (less than one week):bacterial diarrhea, Cryptosporidium, hemorrhagic fevers
Medium (up to one month): Giardia, Entamoeba, Malaria, Salmonella typhi, leptospirosis
Long: Malaria, Visceral leishmaniasis, viral hepatitis, amoebic liver abscess, Schistosomiaisis
Eosinophilia
May see this anyway in HIV-infected persons
However, in setting of travel to indigenous areas, helminthic infections should be looked
for in fecal smears
Summary
Precautions generally same for HIV & non-HIV infected travelers
Decisions regarding live vaccines are very weighted to patient’s immune status
May anticipate lower response to all vaccines and hence increased risk of disease
Incomplete information currently on need for dose or drug changes for malaria
prevention in patients taking ritonavir
Patients taking proper precautions and not severely immunocompromised should do well.
Sometimes, travel itinerary should be modified to avoid potential exposures
Differential diagnosis of illness in returning HIV-positive traveler can be very broad both
in short term and long term follow-up
