Aging:
Aging can be defined as a progressive and generalized impairment of function resulting in the loss of adaptive response to stress and increased risk of age related diseases.The overall effect of these alterations is an increase in the probability of declining health and dying and which is also often associated with social, emotional and financial marginalization in old age
Heterogeneity
As people age, they become more dissimilar than similar in terms of individual physiology. For example:
-A group of 30 year olds has similar cardiovascular endurance, lung capacity, cognitive ability
-A group of 80 year olds may differ much more in basic physiology
With this heterogeneity in function, must know what’s normal to recognize disease
Normal Changes with Aging:
Skeleton
Decreased height and weight (after age 80)
Loss of bone substance (osteopenia)
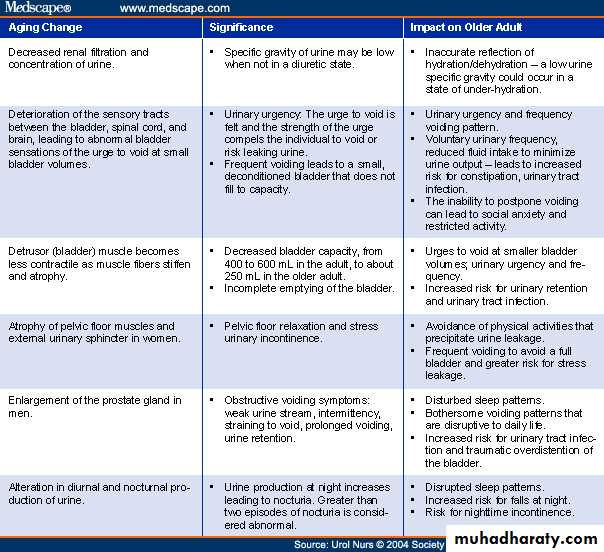
Kidney
Decreased creatinine, renal blood flow and concentration ability
Gastrointestinal Tract
Decreased acid (Vitamin B12 related)
Fewer taste buds
Eyes
Arcus senilis
Decreased acuity, accommodation, color sensitivity, depth perception
Hyperopia (far-sightedness)
Hearing
Degenerative changes of ossicles
Obstruction of eustachian tube
Atrophy of cochlear hair cells
High frequency hearing loss and pitch discrimination
Nervous system
Increased motor response time
Slower psychomotor performance
Slowing intellectual performance
Decreased complex learning
Decreased hours of sleep
Common versus Normal:
Just because a finding is common in the elderly doesn’t mean it’s normal
Hypertension, osteoarthritis, and dementia are common in the elderly but not normal
Patients only discuss things with you that they feel are abnormal
If your patient considers incontinence a “normal” part of aging, he/she won’t bring it up during a clinic visit.
Patient expectations are often wrong
Disability and Disease:
Geriatric disorders are usually disabilities rather than discretely defined diseasesADL (Activities of Daily Living) and IADL (Instrumental Activities of Daily Living) difficulties increase with age
Less than 10 percent of those 65-69 need help with IADL/ADL
60% of females over 85 living in the community needed help with IADLs, and 40% required help with ADLs
Activities of Daily Living (ADL):
Activities of Daily Living (ADL) include
Dressing
Eating
Walking
Going to the bathroom
Bathing
These are severe functional disabilities and define dependency
Instrument Activities of Daily Living (IADL):
IADL include:
Shopping
Housekeeping
Accounting/bill paying
Food/meal preparation
Travel/driving
These are less severe than ADL, but clearly cause dysfunction and lead to dependency
Weak Link Concept:
Many elderly have one system that is their “weak link”. Examples:
CNS – dementia, hx of strokes, etc.
Neuromuscular – neuropathy, osteoarthritis, deconditioning, etc.
Genitourinary – incontinence, prostatism, etc.
This weak link influences the presentation of diseases
Disease presents differently:
A 90 yo with dementia who develops pneumonia
may present with delirium
A 90 yo with osteoarthritis and neuropathy who develops pneumonia
may present with a fall
A 90 yo with no “weak link” who develops pneumonia
may present “typically” – fever, chills, productive cough, etc.
Hard to Cure Syndromes:
Geriatric syndromes may be perceived as difficult or impossible to treat and cure.
However, a thorough evaluation often reveals many minor contributing disorders that can be improved, resulting in overall effective treatment
Our job may not be to cure disease in the elderly, but to improve function
For Instance…
In a patient complaining of nocturia x3 who has an enlarged prostate, an internist may start an alpha blocker
A geriatrician would
Evaluate his medication list and move the diuretic to morning dosing or eliminate it
Address sleep hygiene issues (no caffeine before bedtime, no water within 2 hours, etc)
Discuss timed voiding
Multiple “tweaks” may result in improved function
Anticipatory Management:
Identification of a geriatric syndrome can lead to anticipation and avoidance of complications
After diagnosis of dementia, anticipate delirium with psychoactive drugs or infections
After diagnosis of neuropathy, anticipate falls or hip fracture.
Look for vitamin D deficiency
Start bisphosphonate
Counsel caregiver
Might not completely avoid these, but can at least prepare the patient and family
Mental Status Changes:
Dementia is a disease of aging, but not a normal consequence of agin.There are many types
Delirium occurs as a complication of many disease states in the elderly
Changes in mental status are the hallmark of dementia and delirium
Familiarity with the mini-mental status examination is essential to be able to evaluate mental status!
Geriatric medicine: main issues
Understanding basic concepts
Approaching the older patient
Age related physiological & pathological states
Demographic impact on geriatric health care
National programmes and services
Basic concepts:
Multiple diseases and multiple drugs.
Diseases often chronic, progressive with adverse consequences. Focus on functional independence
Prevention is more productive and rewarding
Disease profile influenced by socioeconomic emotional status
Symptoms may be silent: no pain in MI, no fever in infection or may be atypical & unrelated. Weak link organ symptoms: confusion, incontinence, faints, falls, depression, heart failure-Geriatric Syndromes
Features like reduced jerks, bacteriuria, common
Approaching the older patient
Do not be an ageist
Have patience in history taking
Optimize communication
Make the patient safe & comfortable
Get a full medication list
Assess family’s cooperation & attitude
Assess care giver’s stress
Physiological changes and their impact:
Change: decrease in
Impact: decrease in
Basal metabolic rateCalorie needs
Pulmonary functionExercise capacity
Renal functionAbility to conc./dilute urine
Bone mineralFracture resistance
Gastro-intestinal function
Bowel motility
SightIndependence
DentitionEating ability
TasteAppetite
Common geriatric disorders:CVS: hypertension, IHD, heart failure, PVD, syncope
Resp: pneumonia, tuberculosis, asthma, COPD
CNS: stroke, dementia, meningitis, encephalopathy
Endo: diabetes, thyroid, sexual, metabolic diseases
Musculoskeletal: osteoporosis, OA, RA, falls, fracture
GIT: dyspepsia, constipation, NSAID gastrop, GERD
Urogenital: UTI, BPH, menopause, incontin., prolaps
Cancers: breast, lung, prostate, cervical, haematol.
Spl senses & iatrogenic: eye, ear, taste, skin, ADRs
Unclassified symptoms in old age:
Weakness, Fatigue , Anorexia, Constipation, Altered taste, Breathlessness, Low muscle strength, Body aches ,Confusion, Insomnia, Impotence, Faints/ Falls