167
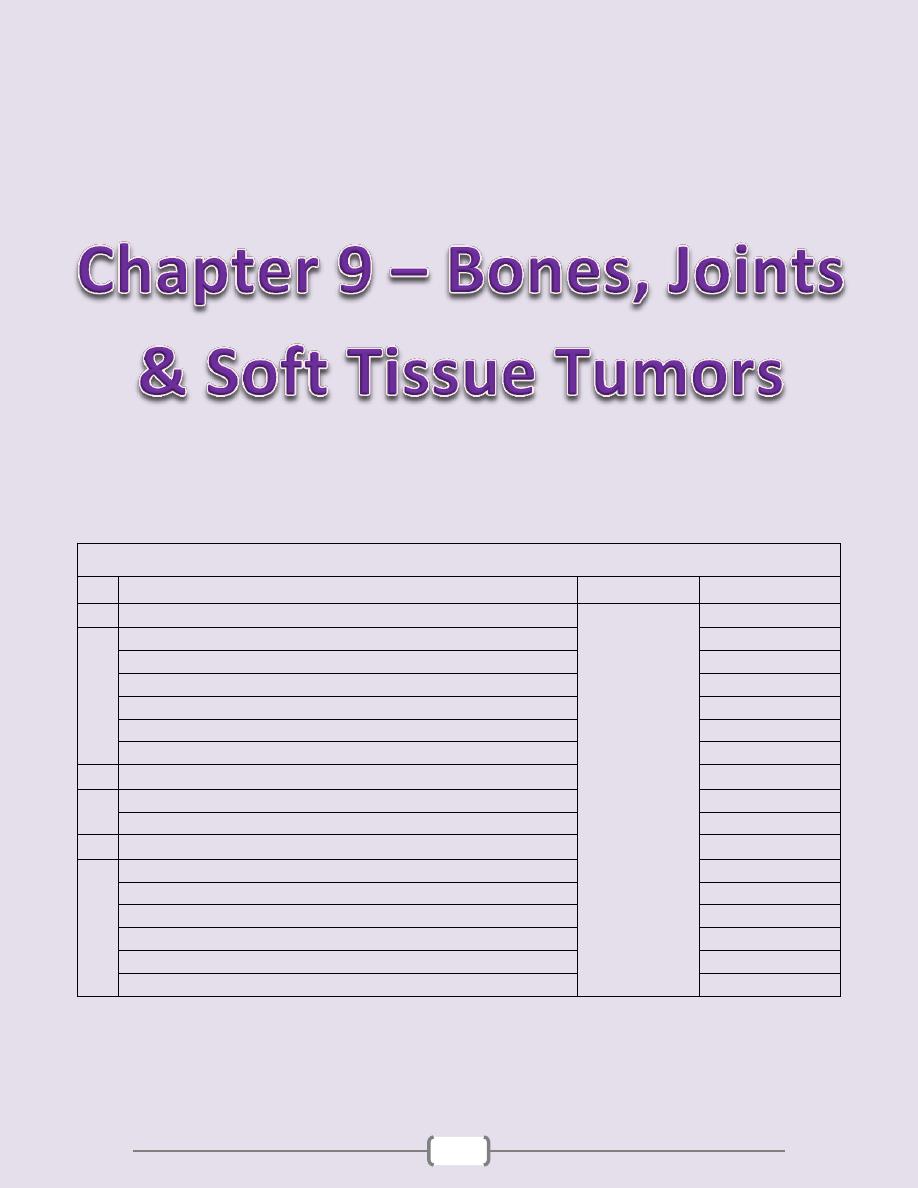
Chapter contents (167 –185)
Topics
Directed by
Page number
1
Bones
د. سالم
(168 - 178)
Congenital diseases of bone
168
Acquired diseases of bone development
168
Fractures
171
Osteonecrosis
172
Osteomyelitis
172
Bone tumors
173
2
Joints
(179 - 181)
Arthritis
179
Joint tumors and tumor-like lesions
181
3
Soft Tissue Tumors
(182
– 185)
Tumors of Adipose Tissue (Fatty Tumors)
182
Fibrous Tumors and Tumor-Like Lesions
182
Fibrohistiocytic Tumors
183
Skeletal Muscle Tumors
184
Smooth Muscle Tumors
184
Synovial Sarcoma
185
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
168
Bones
Congenital diseases of bone
Osteogenesis Imperfecta (OI) (Brittle bone diseases)
is a group of hereditary disorders
caused by gene mutations that eventuate in defective synthesis of and thus premature
degradation of type I collagen. The fundamental abnormality in all forms of OI is too little
bone, resulting in extreme susceptibility to fractures. The bones show marked cortical
thinning and attenuation of trabeculae.
Extraskeletal manifestations also occur because type I collagen is a major component of
extracellular matrix in other parts of the body. The classic finding of blue sclerae (Fig. 12-1)
is attributable to decreased scleral collagen content; this causes a relative transparency that
allows the underlying choroid to be seen. Hearing loss can be related to conduction defects in
the middle and inner ear bones, and small misshapen teeth are a result of dentin deficiency.
Achrondroplasia
is a major cause of dwarfism. The underlying etiology is a point mutation
in the fibroblast growth factor receptor, which causes inhibition of chondrocyte proliferation,
which is associated with suppression of the normal epiphyseal growth plate expansion. Thus,
long bone growth is markedly shortened. The most conspicuous changes include
disproportionate shortening of the proximal extremities, bowing of the legs, and a lordotic
posture. Microscopically, the cartilage growth plates are disorganized & hypoplastic.
Osteopetrosis
is a group of rare genetic disorders characterized by reduced osteoclast-
mediated bone resorption and therefore defective bone remodelling. The bones are solid and
heavy with no medullary canal, long ends are bulbous, small neural foramina compress
nerves. The affected bone is grossly dense but fractures occur readily like a piece of chalk.
Patients frequently have cranial nerve compressions by the surrouding bone, and recurrent
infections. The latter is attributable to diminished hematopoiesis resulting from reduced
marrow space with impressive hepatosplenomegaly due to extramedullary hematopoiesis.
Acquired diseases of bone development
Osteoporosis
is characterized by increased porosity of the skeleton resulting from reduced bone mass. The
disorder may be localized to a certain bone (s), as in disuse osteoporosis of a limb, or generalized
involving the entire skeleton. Generalized osteoporosis may be primary, or secondary.
Primary generalized osteoporosis: - Postmenopausal - Senile
Secondary generalized osteoporosis
Senile and postmenopausal osteoporosis are the most common forms. In the fourth decade in
both sexes, bone resorption begins to overrun bone deposition. Such losses generally occur in
areas containing abundant cancelloues bone such as the vertebrae & femoral neck. The
postmenopausal state accelerates the rate of loss; that is why females are more susceptible to
osteoporosis and its complications.
B. Neoplasia
Multiple myeloma
Carcinomatosis
A. Endocrine disorders
Hyperparathyroidism
Hypo or hyperthyroidism
Others
C. Gastrointestinal disorders
Malnutrition & malabsorption
Vit D & C deficiency
Hepatic insufficiency
D. Drugs
Corticosteroids
●
Anticoagulants
Chemotherapy
●
Alcohol
E. Miscellaneous
osteogenesis imperfecta
immobilization
pulmonary disease

Chapter 9 - Bones, Joints, and Soft Tissue Tumors
169
Gross features
Because of bone loss, the bony trabeculae are thinner and more widely separated than usual.
This leads to obvious porosity of otherwise spongy cancellous bones. (Fig. 12-3).
Microscopic features
There is thinning of the trabeculae and widening of Haversian canals.
The mineral content of the thinned bone is normal, and thus there is no alteration in the ratio
of minerals to protein matrix.
Etiology & Pathogenesis
o Osteoporosis involves an imbalance of bone formation, bone resorption, & regulation of
osteoclast activation. It occurs when the balance tilts in favor of resorption.
o Osteoclasts (as macrophages) bear receptors (called RANK receptors) that when stimulated
activate the nuclear factor (NFκB) transcriptional pathway. RANK ligand synthesized by
bone stromal cells and osteoblasts activates RANK. RANK activation converts macrophages
into bone-crunching osteoclasts and is therefore a major stimulus for bone resorption.
o Osteoprotegerin (OPG) is a receptor secreted by osteoblasts and stromal cells, which can bind
RANK ligand and by doing so makes the ligand unavailable to activate RANK, thus limiting
osteoclast bone-resorbing activity.
o Dysregulation of RANK, RANK ligand, and OPG interactions seems to be a major
contributor in the pathogenesis of osteoporosis. Such dysregulation can occur for a variety of
reasons, including aging and estrogen deficiency (Fig. 12-4).
o Influence of age: with increasing age, osteoblasts synthetic activity of bone matrix
progressively diminished in the face of fully active osteoclasts.
o The hypoestrogenic effects: the decline in estrogen levels associated with menopause
correlates with an annual decline of as much as 2% of cortical bone and 9% of cancellous
bone. The hypoestrogenic effects are attributable in part to augmented cytokine production
(especially interleukin-1 and TNF). These translate into increased RANK-RANK ligand
activity and diminished OPG.
o Physical activity: reduced physical activity increases bone loss. This effect is obvious in an
immobilized limb, but also occurs diffusely with decreased physical activity in older individuals.
o Genetic factors: these influence vitamin D receptors efficiency, calcium uptake, or PTH
synthesis and responses.
o Calcium nutritional insufficiency: the majority of adolescent girls (but not boys) have
insufficient dietary intake of calcium. As a result, they do not achieve the maximal peak bone
mass, and are therefore likely to develop clinically significant osteoporosis at an earlier age.
o Secondary causes of osteoporosis: these include prolonged glucocorticoid therapy (increases
bone resorption and reduce bone synthesis.)
The clinical outcome of osteoporosis depends on which bones are involved. Thoracic & lumbar
vertebral fractures are extremely common, and produce loss of height & various deformities,
including kyphoscoliosis that can compromise respiratory function. Pulmonary embolism &
pneumonia are common complications of fractures of the femoral neck, pelvis, or spine.
Paget Disease (Osteitis Deformans)
This unique bone disease is characterized by repetitive episodes of exaggerated, regional
osteoclastic activity (osteolytic stage), followed by exuberant bone formation (mixed
osteoclastic-osteoblastic stage), and finally by exhaustion of cellular activity (osteosclerotic
stage). The net effect of this process is a gain in bone mass; however, the newly formed bone
is disordered and lacks strength. Paget disease usually does not occur until mid-adulthood but
becomes progressively more common thereafter. The pathognomonic histologic feature is a
mosaic pattern of lamellar bone (likened to a jigsaw puzzle) due to prominent cement lines
that haphazardly fuse units of lamellar bone. (Fig. 12-5) The axial skeleton and proximal
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
170
femur are involved in the majority of cases. In patients with extensive disease,
hypervascularity of the marrow spaces can result in high-output congestive heart failure.
Cranial nerves impingement also occurs and can lead to head ache and auditory disturbances.
Rarely Paget disease is complicated by bone sarcoma (usually osteogenic).
Rickets and Osteomalacia
Rickets in growing children and osteomalacia in adults are skeletal diseases with worldwide
distribution. They may result from
1. Diets deficient in calcium and vitamin D 2. Limited exposure to sunlight (in heavily
veiled women, and inhabitants of northern climates with scant sunlight)
3. Renal disorders causing decreased synthesis of 1,25 (OH)
2
-D or phosphate depletion
4. Malabsorption disorders.
Although rickets and osteomalacia rarely occur outside high-risk groups, milder forms of
vitamin D deficiency (also called vitamin D insufficiency) leading to bone loss and hip
fractures are quite common in the elderly.
Whatever the basis, a deficiency of vitamin D tends to cause hypocalcemia. When
hypocalcemia occurs, PTH production is increased, that ultimately leads to restoration of the
serum level of calcium to near normal levels (through mobilization of Ca from bone &
decrease in its tubular reabsorption) with persistent hypophosphatemia (through increase renal
exretion of phosphate); so mineralization of bone is impaired or there is high bone turnover.
The basic derangement in both rickets and osteomalacia is an excess of unmineralized
matrix. This complicated in rickets by derangement of endochondral bone growth.
The following sequence ensues in rickets:
1. Overgrowth of epiphyseal cartilage with distorted, irregular masses of cartilage
2. Deposition of osteoid matrix on inadequately mineralized cartilage
3. Disruption of the orderly replacement of cartilage by osteoid matrix, with enlargement and
lateral expansion of the osteochondral junction
4. Microfractures and stresses of the inadequately mineralized, weak, poorly formed bone
5. Deformation of the skeleton due to the loss of structural rigidity of the developing bones
Gross features
o The gross skeletal changes depend on the severity of the disease; its duration, & the stresses
to which individual bones are subjected.
o During the nonambulatory stage of infancy, the head and chest sustain the greatest stresses. The
softened occipital bones may become flattened. An excess of osteoid produces frontal bossing.
Deformation of the chest results from overgrowth of cartilage or osteoid tissue at the
costochondral junction, producing the "rachitic rosary." The weakened metaphyseal areas of the
ribs are subject to the pull of the respiratory muscles and thus bend inward, creating anterior
protrusion of the sternum (pigeon breast deformity). The pelvis may become deformed.
o When an ambulating child develops rickets, deformities are likely to affect the spine, pelvis,
and long bones (e.g., tibia), causing, most notably, lumbar lordosis and bowing of the legs.
o In adults the lack of vitamin D deranges the normal bone remodeling that occurs throughout
life. The newly formed osteoid matrix laid down by osteoblasts is inadequately mineralized,
thus producing the excess of persistent osteoid that is characteristic of osteomalacia. Although
the contours of the bone are not affected, the bone is weak and vulnerable to gross fractures
or microfractures, which are most likely to affect vertebral bodies and femoral necks.
Microscopic features
The unmineralized osteoid can be visualized as a thickened layer of matrix (which stains pink
in hematoxylin and eosin preparations) arranged about the more basophilic, normally
mineralized trabeculae. (Fig. 12-7)
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
171
Hyperparathyroidism
Abnormally high levels of parathyroid hormone (PTH) cause hypercalcemia. This can result
from either primary or secondary causes. Primary hyperparathyroidism is caused usually
by a parathyroid adenoma, which is associated with autonomous PTH secretion. Secondary
hyperparathyroidism, on the other hand, can occur in the setting of chronic renal failure. In
either situation, the presence of excessive amounts of this hormone leads to significant
skeletal changes related to a persistently exuberant osteoclast activity that is associated with
increased bone resorption and calcium mobilization. The entire skeleton is affected. PTH is
directly responsible for the bone changes seen in primary hyperparathyroidism, but in
secondary hyperparathyroidism additional influences also contribute. In chronic renal failure
there is inadequate 1,25-(OH)
2
-D synthesis that ultimately affects gastrointestinal calcium
absorption. The hyperphosphatemia of renal failure also suppresses renal α
1
-hydroxylase,
which further impair vitamin D synthesis; all these eventuate in hypocalcemia, which
stimulates excessive secretion of PTH by the parathyroid glands, & hence elevation in PTH
serum levels.
Gross features
There is increased osteoclastic activity, with bone resorption. Cortical and trabecular bone are
lost and replaced by loose connective tissue. (Fig. 12-8)
Bone resorption is especially pronounced in the subperiosteal regions and produces
characteristic radiographic changes, best seen along the radial aspect of the middle phalanges
of the second and third fingers.
o Microscopical features
o There is increased numbers of osteoclasts and accompanying erosion of bone surfaces.
o The marrow space contains increased amounts of loose fibrovascular tissue.
o Hemosiderin deposits are present, reflecting episodes of hemorrhage resulting from
microfractures of the weakened bone.
o In some instances, collections of osteoclasts, reactive giant cells, and hemorrhagic debris
form a distinct mass, termed "brown tumor of hyperparathyroidism". (Fig. 12-8 B) Cystic
change is common in such lesions (hence the name osteitis fibrosa cystica).
Patients with hyperparathyroidism have reduced bone mass, and hence are increasingly
susceptible to fractures and bone deformities.
Fractures
Fractures are classified into the following types
Complete or incomplete fractures: the fracture line either extends through the whole or part
of the thickness of the bone involved.
Closed when the overlying tissue is intact, or compound when the fracture extends into the
overlying skin
Comminuted when the bone is splintered into small fragments
Displaced, when the fractured bone ends are not aligned
Pathologic fracture refers to bone break that occurs at the site of previous disease (e.g., a
bone cyst, a malignant tumor, etc).
Stress fracture develops slowly over time as a collection of micro-fractures associated with
increased physical activity, especially with repetitive weight on bone (as in military boot camps).
The fracture mechanically ruptures associated blood vessels; the resulting blood hematoma
creates a fibrin mesh scaffold to recruit inflammatory cells, fibroblasts, and endothelium. This
soft tissue callus is able to hold the ends of the fractured bone in apposition, but it is non-
calcified and cannot support weight bearing. Bone progenitors in the medullary cavity deposit
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
172
new foci of woven bone, and activated mesenchymal cells at the fracture site to differentiate
into cartilage-synthesizing chondroblasts. In uncomplicated fractures, this early repair process
peaks within 2-3 weeks. The newly formed cartilage acts as a nidus for endochondral
ossification. This connects the trabeculae in adjacent bone. With ossification, the fractured
ends are bridged by a bony callus. Although excess fibrous tissue, cartilage, and bone are
produced in the early callus, subsequent weight-bearing leads to resorption of the callus from
non-stressed sites; at the same time there is strengthening of regions that support greater load
stresses. This callus remodeling restores the original size and shape of the bone. (Fig. 12-9)
The healing of a fracture can be disrupted by many factors:
Displaced and comminuted fractures frequently result in some deformity; devitalized
fragments of splintered bone require resorption, which delays healing, enlarges the callus, and
requires long periods of remodeling that may never completely normalize.
Inadequate immobilization permits constant movement at the fracture site so that the normal
constituents of callus do not form. In this case, the healing site is composed mainly of fibrous
tissue and cartilage. This causes instability and resulting in delayed union or even nonunion.
Also too much movement along the fracture gap causes the central portion of the callus to
undergo cystic degeneration that may become lined by synovial-like cells, creating a false
joint, (pseudoarthrosis).
Infection (a risk in comminuted and open fractures) is a serious obstacle to fracture healing.
Inadequate levels of calcium or phosphorus, vitamin deficiencies, systemic infection,
diabetes, and vascular insufficiency all cause impairment of bone repair.
Osteonecrosis (avascular necrosis)
(Fig. 12-10)
Ischemic necrosis with resultant bone infarction occurs mostly due to fracture or after
corticosteroid use. Microscopically, dead bon trabevulae (characterized by empty lacunae) are
interspersed with areas of fat necrosis. The cortex is usually not affected because of collateral
blood supply; in subchondral infarcts, the overlying articular cartilage also remains viable
because the synovial fluid can provide nutritional support. With time, osteoclasts can resorb
many of the necrotic bony trabeculae; any dead bone fragments that remain act as scaffolds
for new bone formation, a process called creeping substitution. Symptoms depend on the size
and location of injury. Subchondral infarcts often collapse & can lead to severe osteoarthritis.
Osteomyelitis
This refers to inflammation of the bone and related marrow cavity almost always due to
infection. Osteomyelitis can be acute or a chronic. The most common etiologic agents are
pyogenic bacteria and Mycobacterium tuberculosis.
Pyogenic Osteomyelitis
The offending organisms reach the bone by one of three routes:
1. Hematogenous dissemination (most common)
2. Extension from a nearby infection (in adjacent joint or soft tissue)
3. Traumatic implantation of bacteria (as after compound fractures or orthopedic procedures).
Staphylococcus aureus is the most frequent cause. Mixed bacterial infections, including
anaerobes, are responsible for osteomyelitis complicating bone trauma. In as many as 50% of
cases, no organisms can be isolated.
Pathologic features (Fig. 12-11)
o The offending bacteria proliferate & induce an acute inflammatory reaction.
o Entrapped bone undergoes early necrosis; the dead bone is called sequestrum.
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
173
o The inflammation with its bacteria can permeate the Haversian systems to reach the
periosteum. In children, the periosteum is loosely attached to the cortex; therefore, sizable
subperiosteal abscesses can form and extend for long distances along the bone surface.
o Lifting of the periosteum further impairs the blood supply to the affected region, and both
suppurative and ischemic injury can cause segmental bone necrosis.
o Rupture of the periosteum can lead to an abscess in the surrounding soft tissue and eventually
the formation of cutaneous draining sinus. Sometimes the sequestrum crumbles and passes
through the sinus tract.
o In infants (uncommonly in adults), epiphyseal infection can spread into the adjoining joint to
produce suppurative arthritis, sometimes with extensive destruction of the articular cartilage
and permanent disability.
o After the first week of infection chronic inflammatory cells become more numerous.
Leukocyte cytokine release stimulates osteoclastic bone resorption, fibrous tissue ingrowth,
and bone formation in the periphery, this occurs as a shell of living tissue (involucrum)
around a segment of dead bone. Viable organisms can persist in the sequestrum for years after
the original infection.
Chronicity may develop when there is delay in diagnosis, extensive bone necrosis, and
improper management. Complications of chronic osteomyelitis include
1. A source of acute exacerbations
2. Pathologic fracture
3. Secondary amyloidosis
4. Endocarditis
5. Development of squamous cell carcinoma in the sinus tract (rarely osteosarcoma).
Tuberculous Osteomyelitis
(Fig. 12-12)
Bone infection complicates up to 3% of those with pulmonary tuberculosis. Young adults or
children are usually affected. The organisms usually reach the bone hematogenously. The
long bones and vertebrae are favored sites. The lesions are often solitary (multifocal in AIDS
patients). The infection often spreads from the initial site of bacterial deposition (the
synovium of the vertebrae, hip, knee, ankle, elbow, wrist, etc) into the adjacent epiphysis,
where it causes typical granulomatous inflammation with caseous necrosis and extensive
bone destruction. Tuberculosis of the vertebral bodies (Pott disease), is an important form of
osteomyelitis. Infection at this site causes vertebral deformity and collapse, with secondary
neurologic deficits. Extension of the infection to the adjacent soft tissues with the
development of psoas muscle abscesses is fairly common in Pott disease. Advanced cases are
associated with cutaneous sinuses, which cause secondary bacterial infections. Diagnosis is
established by synovial fluid direct examination, culture or PCR.
Bone tumors
Primary bone tumors are classified according to their normal cell of origin or line of
differentiation. Among the benign mass lesions, osteochondroma and fibrous cortical defect
occur most frequently. Osteosarcoma is the most common primary bone cancer, followed by
chondrosarcoma and Ewing sarcoma. Benign tumors markedly outnumber their malignant
counterparts, particularly before age 40; bone tumors in the elderly are much more likely to
be malignant.
Most bone tumors develop during the first few decades of life and tend to originate in the
long bones of the extremities. Nevertheless, specific tumor types target certain age groups and
anatomic sites; such clinical information is often critical for the appropriate diagnosis. For
instance, most osteosarcomas occur during adolescence, with half arising around the knee,
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
174
either in the distal femur or proximal tibia. In contrast, chondrosarcomas tend to develop
during mid- to late adulthood and involve the trunk, limb girdles, and proximal long bones.
Benign lesions are frequently asymptomatic and are detected as incidental findings. Others
produce pain or a slowly growing mass. Occasionally, a sudden pathologic fracture is the first
manifestation. Radiologic imaging is important in the evaluation of bone tumors; however,
biopsy and microscopic evaluations are necessary for the final diagnosis.
Bone-Forming Tumors
1)
Osteoma
is a benign lesion of bone that in many cases represent a developmental abnormaly or
reactive growth rather than true neoplasms. They are most common in the head, including the
paranasal sinuses. Microscopically, there is a mixture of woven and lamellar bone. They may
cause local mechanical problems (e.g., obstruction of a sinus cavity) & cosmetic deformities.
2)
Osteoid Osteoma and Osteoblastoma
are benign neoplasms with very similar histologic
features. Both lesions typically arise during the 2
nd
& 3
rd
decades. They are well-
circumscribed lesions, usually involving the cortex. The central area of the tumor, termed the
nidus, is characteristically radiolucent. Osteoid osteomas arise most often in the proximal
femur and tibia, and are by definition less than 2 cm, whereas osteoblastomas are larger.
Localized pain is an almost universal complaint with osteoid osteomas, and is usually relieved
by aspirin. Osteoblastomas arise most often in the vertebral column; they also cause pain,
which is not responsive to aspirin. Malignant transformation is rare unless the lesion is
treated with radiation.
Gross features (Fig. 12-13)
Both lesions are round-to-oval masses of hemorrhagic gritty tan tissue.
A rim of sclerotic bone is present at the edge of both types of tumors.
Microscopic features
There are interlacing trabeculae of woven bone surrounded by osteoblasts. The intervening
connective tissue is loose, vascular & contains variable numbers of giant cells.
3) Osteosarcoma
This is “a bone-producing malignant mesenchymal tumor.” Excluding myeloma and
lymphoma, osteosarcoma is the most common primary malignant tumor of bone (20%). The
peak age of incidence is 10-25 years with 75% of the affected patients are younger than age
20 years; there is a second peak that occurrs in the elderly, usually secondary to other
conditions, e.g. Paget disease, bone infarcts, and prior irradiation. Most tumors arise in the
metaphysis of the long bones of the extremities, with 60% occurring about the knee, 15%
around the hip, & 10% at the shoulder. The most common type of osteosarcoma is primary,
solitary, intramedullary, and poorly differentiated, producing a predominantly bony matrix.
Gross features (Fig. 12-14 A)
The tumor is gritty, gray-white, often with foci of hemorrhage and cystic degeneration.
It frequently destroys the surrounding cortex to extend into the soft tissue.
There is extensive spread within the medullary canal, with replacement of the marrow.
However, penetration of the epiphyseal plate or the joint space is infrequent.
Microscopic features
o Tumor cells are pleomorphic with large hyperchromatic nuclei; bizarre tumor giant cells are
common, as are mitoses.
o The direct production of mineralized or unmineralized bone (osteoid) by malignant cells is
essential for diagnosis of osteosarcoma. The neoplastic bone is typically fine, lace-like but
can also be deposited in broad sheets. (Fig. 12-14 B)
o Cartilage can be present in varying amounts. When malignant cartilage is abundant, the tumor
is called a chondroblastic osteosarcoma.
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
175
Pathogenesis
o Several genetic mutations are closely associated with the development of osteosarcoma. In
particular, RB gene mutations that occur in both sporadic tumors, and in individuals with
hereditary retinoblastomas. In the latter there are germ-line mutations in the RB gene (inherited).
o Spontaneous osteosarcomas also frequently exhibit mutations in genes that regulate the cell
cycle including p53, cyclins, etc.
Osteosarcomas typically present as painful enlarging masses. Radiographs usually show a
large, destructive, mixed lytic and blastic mass with infiltrating margins. The tumor
frequently breaks the cortex and lifts the periosteum. The latter results in a reactive periosteal
bone formation; a triangular shadow on x-ray between the cortex and raised periosteum
(Codman triangle) is characteristic but not specific of osteosarcomas. Osteosarcomas
typically spread hematogenously; 10% to 20% of patients have demonstrable pulmonary
metastases at the time of diagnosis.
Cartilage-Forming Tumors
1)
Osteochondroma (Exostosis)
is a relatively common benign cartilage-capped outgrowth attached by a bony stalk to the
underlying skeleton. Solitary osteochondromas are usually first diagnosed in late adolescence
and early adulthood (male-to-female ratio of 3:1); multiple osteochondromas become
apparent during childhood, occurring as multiple hereditary exostosis, an autosomal dominant
disorder. Inactivation of both copies of the EXT gene (a tumor suppressor gne) in
chondrocytes is implicated in both sporadic and hereditary osteochondromas.
Osteochondromas develop only in bones of endochondral origin arising at the metaphysis
near the growth plate of long tubular bones, especially about the knee. They tend to stop
growing once the normal growth of the skeleton is completed. Occasionally they develop
from flat bones (pelvis, scapula, and ribs). Rarely, exostoses involve the short tubular bones
of hands and feet.
Pathological features (Fig. 12-15)
Osteochondromas vary from 1-20cm in size. The cap is benign hyaline cartilage.
Newly formed bone forms the inner portion of the head and stalk, with the stalk cortex
merging with the cortex of the host bone.
Osteochondromas are slow-growing masses that may be painful. Osteochondromas rarely
progress to chondrosarcoma or other sarcoma, although patients with the multiple hereditary
exostoses are at increased risk of malignant transformation.
2)
Chondroma
is a benign tumor of hyaline cartilage. When it arises within the medullary cavity, it is termed
enchondroma; when on the bone surface it is called juxtacortical chondroma.
Enchondromas are usually diagnosed in persons between ages 20 and 50 years; they are
typically solitary and located in the metaphyseal region of tubular bones, the favored sites
being the short tubular bones of the hands and feet. Ollier disease is characterized by
multiple chondromas preferentially involving one side of the body. Chondromas probably
develop from slowly proliferating rests of growth plate cartilage.
Pathological features (Fig. 12-16)
Enchondromas are gray-blue, translucent nodules usually smaller than 3 cm. Microscopically,
there is well-circumscribed hyaline matrix and cytologically benign chondrocytes.
Most enchondromas are detected as incidental findings; occasionally they are painful or cause
pathologic fractures. Solitary chondromas rarely undergo malignant transformation, but those
associated with enchondromatosis are at increased risk.
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
176
3)
Chondrosarcomas
are malignant tumors of cartilage forming tissues. They are divided into conventional
chondrosarcomas and chondrosarcoma variants. Each of these categories comprises several
distinct types, some defined on microscopic grounds & others on the basis of location within
the affected bone, for e.g. they are divided into central (medullary), peripheral (cortical), and
juxtacortical (periosteal). The common denominator of chondrosarcoma is the production of a
cartilaginous matrix and the lack of direct bone formation by the tumor cells (cf
osteosarcoma). Chondrosarcomas occur roughly half as frequently as osteosarcomas; most
patients age 40 years or more, with men affected twice as frequently as women.
Pathological features (Fig. 12-17)
Conventional chondrosarcomas arise within the medullary cavity of the bone to form an
expansile glistening mass that often erodes the cortex. They exhibit malignant hyaline or
myxoid stroma. Spotty calcifications are typically present. The tumor grows with broad
pushing fronts into marrow spaces and the surrounding soft tissue. Tumor grade is determined
by cellularity, cytologic atypia, and mitotic activity. Low-grade tumors resemble normal
cartilage. Higher grade lesions contain pleomorphic chondrocytes with frequent mitotic
figures with multinucleate cells and lacunae containing two or more chondrocytes.
Dedifferentiated chondrosarcomas refers to the presence of a poorly differentiated
sarcomatous component at the periphery of an otherwise typical low-grade chondrosarcoma.
Other histologic variants include myxoid, clear-cell and mesenchymal chondrosarcomas.
Chondrosarcomas commonly arise in the pelvis, shoulder, and ribs. A slowly growing low-
grade tumor causes reactive thickening of the cortex, whereas a more aggressive high-grade
neoplasm destroys the cortex and forms a soft tissue mass. There is also a direct correlation
between grade and biologic behavior. Size is another prognostic feature, with tumors larger
than 10 cm being significantly more aggressive than smaller tumors. High-grade
Chondrosarcomas metastasize hematogenously, preferentially to the lungs and skeleton.
Fibrous and Fibro-Osseous Tumors
Fibrous tumors of bone are common and comprise several morphological variants.
1) Fibrous Cortical Defect and Nonossifying Fibroma
(Fig. 12-18)
Fibrous cortical defects occur in 30% to 50% of all children older than 2 years of age; they
are probably developmental rather than true neoplasms. The vast majority are smaller than 0.5
cm and arise in the metaphysis of the distal femur or proximal tibia; almost half are bilateral
or multiple. They may enlarge in size (5-6 cm) to form nonossifying fibromas. Both lesions
present as sharply demarcated radiolucencies surrounded by a thin zone of sclerosis.
Microscopically are cellular and composed of benign fibroblasts and macrophages, including
multinucleated forms. The fibroblasts classically exhibit a storiform pattern. Fibrous cortical
defects are asymptomatic and are usually only detected as incidental radiographic lesions.
Most undergo spontaneous differentiation into normal cortical bone. The few that enlarge into
nonossifying fibromas can present with pathologic fracture; in such cases biopsy is necessary
to rule out other tumors.
2) Fibrous Dysplasia
is a benign mass lesion in which all components of normal bone are present, but they fail to
differentiate into mature structures. Fibrous dysplasia occurs as one of three clinical patterns:
A. Involvement of a single bone (monostotic)
B. nvolvement of multiple bones (polyostotic)
C. Polyostotic disease, associated with café au lait skin pigmentations and endocrine
abnormalities, especially precocious puberty (Albright syndrome).
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
177
Monostotic fibrous dysplasia accounts for 70% of cases. It usually begins in early
adolescence, and ceases with epiphyseal closure. It frequently involves ribs, femur, tibia &
jawbones. Lesions are asymptomatic and usually discovered incidentally. However, fibrous
dysplasia can cause marked enlargement and distortion of bone, so that if the face or skull is
involved, disfigurement can occur.
Polyostotic fibrous dysplasia without endocrine dysfunction accounts for the majority of the
remaining cases. It tends to involve the shoulder and pelvic girdles, resulting in severe
deformities and spontaneous fractures.
Albright syndrome accounts for 3% of all cases. The bone lesions are often unilateral, and the
skin pigmentation is usually limited to the same side of the body. The cutaneous macules are
classically large, dark to light brown (café au lait), and irregular.
Gross features (Fig. 12-19)
The lesion is well-circumscribed, intramedullary; large masses expand and distort the bone.
On section it is tan-white and gritty.
Microscopic features
There are curved trabeculae of woven bone (mimicking Chinese characters), without
osteoblastic rimming. The above are set within fibroblastic proliferation
Individuals with monostotic disease usually have minimal symptoms. By x-ray, lesions
exhibit a characteristic ground-glass appearance with well-defined margins. Polyostotic
involvement is frequently associated with progressive disease, and more severe skeletal
complications (e.g., fractures, long bone deformities, and craniofacial distortion). Rarely,
polyostotic disease can transform into osteosarcoma, especially following radiotherapy.
Miscellaneous Bone Tumors
1)
Ewing Sarcoma & Primitive Neuroectodermal Tumor (PNET)
are primary malignant small round-cell tumors of bone and soft tissue. They are viewed as
the same tumor because they share an identical chromosome translocation; they differ only in
degree of differentiation. PNETs demonstrate neural differentiation whereas Ewing sarcomas
are undifferentiated. After osteosarcomas, they are the second most common pediatric bone
sarcomas. Most patients are 10 to 15 years old. The common chromosomal abnormality is a
translocation that causes fusion of the EWS gene with a member of the ETS family of
transcription factors. The resulting hybrid protein functions as an active transcription factor to
stimulate cell proliferation. These translocations are of diagnostic importance since almost
all patients with Ewing tumor have t(11;22).
Pathological features (Fig. 12-20)
o Ewing sarcoma and PNETs arise in the medullary cavity but eventually invade the cortex and
periosteum to produce a soft tissue mass. The tumor is tan-white, frequently with foci of
hemorrhage and necrosis.
o Microscopic features
There are sheets of uniform small, round cells that are slightly larger than lymphocytes with
few mitoses and little intervening stroma. The cells have scant glycogen-rich cytoplasm.
The presence of Homer-Wright rosettes (tumor cells circled about a central fibrillary space)
indicates neural differentiation, and hence indicates by definition PNET.
Ewing sarcoma and PNETs typically present as painful enlarging masses in the diaphyses of
long tubular bones (especially the femur) and the pelvic flat bones. The tumor may be
confused with osteomyelitis because of its association with systemic signs & symptoms of
infection. X-rays show a destructive lytic tumor with infiltrative margins and extension into
surrounding soft tissues. There is a characteristic periosteal reaction depositing bone in an
onionskin fashion.
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
178
2)
Giant-Cell Tumor of Bone (GCT)
(Fig. 12-21)
is dominated by multinucleated osteoclast-type giant cells, hence the synonym osteoclastoma.
GCT is benign but locally aggressive, usually arising in individuals in their 20s to 40s. Current
opinion suggests that the giant cell component is likely a reactive macrophage population and
the mononuclear cells are neoplastic. Tumors are large and red-brown with frequent cystic
degeneration. They are composed of uniform oval mononuclear cells with frequent mitoses,
with scattered osteoclast-type giant cells that may contain 30 or more nuclei.
The majority of GCTs arise in the epiphysis of long bones around the knee (distal femur and
proximal tibia). Radiographically, GCTs are large, purely lytic, and eccentric; the overlying
cortex is frequently destroyed, producing a bulging soft tissue mass with a thin shell of
reactive bone. Although GCTs are benign, roughly 50% recur after simple curettage; some
malignant examples (5%) metastasize to the lungs.
3)
Metastatic Tumors
(Fig. 12-22)
These are the most common malignant tumor of bone. Certain tumors exhibit a distinct
skeletal prediliction. In adults more than 75% of skeletal metastases originate from cancers
of the prostate, breast, kidney, and lung. In children, neuroblastoma, Wilms' tumor,
osteosarcoma, Ewing sarcoma, and rhabdomyosarcoma are the common sources of bony
metastases. Most metastases involve the axial skeleton (vertebral column, pelvis, ribs, skull,
sternum), proximal femur, and humerus. The radiologic appearance of metastases can be
purely osteolytic, purely osteoblastic, or mixed osteolytic-osteoblastic (majority of cases). In
lytic lesions (e.g., kidney& lung), the metastatic cells secrete substances such as
prostaglandins, interleukins, etc. that stimulate osteoclastic bone resorption; the tumor cells
themselves do not directly resorb bone. Similarly, metastases that elicit a blastic response
(e.g., prostate adenocarcinoma) do so by stimulating osteoblastic bone formation.
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
179
Joints
Arthritis
Osteoarthritis (Degenerative joint disease)
is the most common joint disorder. It is a frequent consequence of aging and is an important
cause of physical disability in individuals over the age of 65. The fundamental feature of
osteoarthritis is degeneration of the articular cartilage.
In most cases, osteoarthritis appears insidiously with age and without apparent initiating
cause (primary osteoarthritis). When osteoarthritis manifests in youth, there is typically some
predisposing condition, such as previous traumatic injury, developmental deformity, or
marked obesity. In these osettings the disease is called secondary osteoarthritis. Gender has
some influence; knees and hands are more commonly affected in women, whereas hips are
more commonly affected in men.
Pathological features (Fig. 12-23)
o Early changes include proliferation with disorganization of the chondrocytes in the superficial
part of the articular cartilage; (this is accompanied by increasing water content of the matrix
thus decreasing concentration of the proteoglycans with subsequent reduction of elasticity).
o As the superficial part of the cartilage are degraded vertical and horizontal fibrillation and
cracking of the matrix occur.
o Eventually, full-thickness portions of the cartilage are lost, and the subchondral bone plate is
exposed. Friction smooths and polishes the exposed bone (eburnation).
o Small fractures displace pieces of cartilage and subchondral bone into the joint, forming loose
bodies (joint mice). The fracture gaps are filled with synovial fluid to form eventually fibrous
walled cysts.
o Mushroom-shaped osteophytes (bony outgrowths) develop at the margins of the articular surface.
o In severe disease, a fibrous synovial pannus covers the peripheral portions of the articular surface.
Pathogenesis
o Regardless of the inciting stimulus (wear & tear of aging, estrogens in females, and genetic
susceptibility), early osteoarthritis is marked by degenerating cartilage containing more water
and less proteoglycan. The collagen network is also diminished, presumably as a result of
decreased local synthesis and increased breakdown; chondrocyte apoptosis is increased.
o Overall, cartilage tensile strength and resilience are reduced. In response to these degenerative
changes, chondrocytes in the deeper layers proliferate and attempt to "repair" the damage by
synthesizing new collagen and proteoglycans. Although these reparative changes are initially
able to keep pace, matrix changes and chondrocyte loss eventually predominate.
Osteoarthritis predominantly affects patients beginning in their 50s and 60s. Characteristic
symptoms include deep, aching pain exacerbated by use, morning stiffness, and limited range
of movement. Osteophyte impingement on spinal foramina can cause nerve root compression
with radicular pain, muscle spasms, muscle atrophy, and neurologic deficits. Hips, knees,
lower lumbar and cervical vertebrae, proximal and distal interphalangeal joints of the fingers
are commonly involved. Heberden nodes in the fingers, representing prominent osteophytes
at the distal interphalangeal joints, are characteristic in women. With time, significant joint
deformity can occur, but unlike rheumatoid arthritis, fusion does not take place.
Gout
This is a disorder caused by the tissue accumulation of excessive amounts of uric acid, an end
product of purine metabolism. It is marked by recurrent episodes of acute arthritis, sometimes
accompanied by the formation of large crystalline aggregates called tophi & chronic joint
deformity. All of these are the result of precipitation of monosodium urate crystals from
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
180
supersaturated body fluids. Not all individuals with hyperuricemia develop gout; this indicates
that influences besides hyperuricemia contribute to the pathogenesis. Gout is traditionally
divided into primary (90%) and secondary forms (10%). Primary gout designates cases in
whom the basic cause is unknown or when it is due to an inborn metabolic defect that causes
hyperuricemia. In secondary gout the cause of the hyperuricemia is known.
Pathologic features (Fig. 12-24)
The major morphologic manifestations of gout are
1. Acute arthritis 2. Chronic tophaceous arthritis
3. Tophi in various sites, and 4. Gouty nephropathy
o Acute arthritis: The synovium is edematous and congested,
There is an intense infiltration of the synovium & synovial fluid by neutrophils.
Long, slender, needle-shaped monosodium urate crystals are frequently found in the
cytoplasm of the neutrophils as well as in small clusters in the synovium.
o Chronic tophaceous arthritis:
This evolves from repetitive precipitation of urate crystals during acute attacks. The urates
can heavily encrust the articular surfaces and form visible deposits in the synovium.
The synovium becomes hyperplastic, fibrotic, and thickened by inflammatory cells, forming a
pannus that destroys the underlying cartilage, and leading to erosions of subjacent bone.
In severe cases, fibrous or bony ankylosis occurs, resulting in loss of joint function.
o Tophi
These are the pathognomonic hallmarks of gout.
Tophi can appear in the articular cartilage, periarticular ligaments, tendons, and soft tissues,
including the ear lobes. Superficial tophi can lead to large ulcerations of the overlying skin.
Microscopically, they are formed by large aggregations of urate crystals surrounded by an
intense inflammatory reaction of lymphocytes, macrophages, and foreign-body giant cells,
attempting to engulf the masses of crystals.
o Gouty nephropathy
This refers to the renal complications associated with urate deposition including medullary
tophi, intratubular precipitations and renal calculi. Secondary complications such as
pyelonephritis can occur, especially when there is urinary obstruction.
Pathogenesis
(Fig. 12-25)
o Although the cause of excessive uric acid biosynthesis in primary gout is unknown in most
cases, rare patients have identifiable enzymatic defects or deficiencies that are associated with
excess production of uric acid.
o In secondary gout, hyperuricemia can be caused by increased urate production (e.g., rapid cell
lysis during chemotherapy for lymphoma or leukemia) or decreased excretion (chronic renal
failure), or both. Reduced renal excretion may also be caused by drugs such as thiazide
diuretics, because of their effects on uric acid tubular transport.
o Whatever the cause, increased levels of uric acid in the blood and other body fluids (e.g.,
synovium) lead to the precipitation of monosodium urate crystals. The precipitated crystals
are chemotactic to neutrophils & macrophages through activation of complement components
C3a and C5a fragments. This leads to a local accumulation of neutrophils and macrophages in
the joints and synovial membranes to phagocytize the crystals. The activated neutrophils
liberate destructive lysosomal enzymes. Macrophages participate in joint injury by secreting a
variety of proinflammatory mediators such as IL-1, IL-6, and TNF. While intensifying the
inflammatory response, these cytokines can also directly activate synovial cells and cartilage
cells to release proteases (e.g., collagenases) that cause tissue injury.
o Repeated bouts of acute arthritis, however, can lead to the permanent damage seen in chronic
tophaceous arthritis.b
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
181
Pseudogout (chondrocalcinosis) (Calcium pyrophosphate crystal deposition disease).
Pseudogout typically first occurs in the age 50 years or older. It involves enzymes that lead to
accumulation and eventual crystallization of pyrophosphate with calcium. The pathology in
pseudogout involves the recruitment and activation of inflammatory cells, and is reminiscent of
gout. The knees, followed by the wrists, elbows, shoulders, and ankles, are most commonly
affected. Approximately 50% of patients experience significant joint damage.
Infectious Arthritis
can cause rapid joint destruction and permanent deformities. Microorganisms can lodge in
joints during hematogenous dissemination, by direct inoculation or by contiguous spread
from osteomyelitis or a soft tissue abscess.
Suppurative Arthritis is a subtype of infectious arthritis in which the bacteria seed the joint
during episodes of bacteremia. Haemophilus influenzae predominates in children under age 2
years, S. aureus is the main causative agent in older children and adults, and gonococcus is
prevalent during late adolescence and young adulthood. There is sudden onset of pain,
redness, and swelling of the joint with fever, leukocytosis, and elevated ESR. In 90% of
nongonococcal suppurative arthritis, the infection involves only a single joint-usually the
knee. Joint aspiration is typically purulent, and allows identification of the causal agent.
Joint tumors and tumor-like lesions
Ganglion and Synovial Cysts
(Fig. 12-27)
A ganglion is a small (<1.5 cm) cyst located near a joint capsule or tendon sheath; the wrist is
an especially common site. It is firm to fluctuant pea-sized nodules. Because they arise by
cystic degeneration of connective tissue they are grossly translucent and microscopically lack
a true cell lining. They are usually asymptomatic.
Synovial cyst occurs due to herniation of synovium through a joint capsule or massive
enlargement of a bursa. (Fig. 12-28) A good example is the Baker cyst that occurs in the
popliteal fossa.
Pigmented Villonodular Tenosynovitis (PVNS) & Giant-Cell Tumor (GCT) of
Tendon Sheath
(Fig. 12-30)
These are closely related benign neoplasms of synovium. PVNS tends to involve joints
diffusely, whereas GCT usually occurs as a single tendon sheath nodule.
Grossly, both lesions are red-brown to orange-yellow. In PVNS the joint synovium is diffusely
converted into red-brown finger-like projections, and nodules. In contrast, GCT is well
circumscribed and contained. Microscopically, Tumor cells in both lesions resemble
synoviocytes. In PVNS they spread along the surface and infiltrate the subsynovial
compartment. In GCT the cells grow in a solid nodular aggregate. Other typical findings include
hemosiderin deposits, foamy macrophages, & multinucleated giant cells. PVNS usually affects
the knee (80% of cases). Patients typically complain of pain, locking, and recurrent swelling. In
contrast, GCT manifests as a solitary, slowly growing mass frequently involving wrist and
finger tendon sheaths. GCT is the most common soft tissue tumor of the hand.
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
182
Soft Tissue Tumors
Tumors of Adipose Tissue (Fatty Tumors)
1)
Lipomas
are benign tumors of fat, and are the most common soft tissue tumors of adulthood. Most
lipomas are solitary lesions. Lipomas can be subclassified based on their histologic features
(e.g., conventional, myolipoma, spindle cell, myelolipoma, pleomorphic, angiolipoma),
and/or characteristic chromosomal rearrangements. Most lipomas are mobile, slowly
enlarging, painless masses. They are usually seen in adults age 40+; associated with obesity;
there are no gender differences. They are rare in children. Multiple lipomas are more common
in women. The condition is often familial, & may be associated with neurofibromatosis &
multiple endocrine neoplasia syndromes. Lipomas mostly involve the subcutaneous tissue of
the trunk, back, shoulder, neck, proximal extremities but are rare on hands, feet, face, &in
retroperitoneum
Pathological features (Fig. 12-35)
Conventional lipomas (the most common subtype) are soft, yellow, well-encapsulated
masses. They can vary considerably in size.
Microscopically, they consist of mature fat cells with no pleomorphism.
2)
Liposarcoma
is a malignant neoplasm of adipocytes. These tumors occur most commonly in the 40 to 60
years of age & mostly in the deep soft tissues (cf. lipoma) or in visceral sites. The prognosis
of liposarcomas is greatly influenced by the histologic subtype; well-differentiated and
myxoid variants tend to grow in a fairly indolent fashion and have a more favorable outlook
than do the more aggressive round cell and pleomorphic variants, which tend to recur after
excision and metastasize to lungs. A t(12;16) chromosomal translocation is associated with
myxoid liposarcomas; the rearrangement affects a transcription factor that plays a role in
normal adipocyte differentiation.
Pathological features (Fig. 12-36)
Usually they are relatively well-circumscribed large masses.
Several different histologic subtypes are recognized, including two low-grade variants, the
well-differentiated liposarcoma and the myxoid liposarcoma, the latter characterized by
abundant, mucoid extracellular matrix.
Some well-differentiated lesions can be difficult to distinguish histologically from lipomas,
whereas very poorly differentiated tumors can resemble various other high-grade malignancies.
In most cases, cells indicative of fatty differentiation are present. Such cells are known as
lipoblasts; they recapitulate fetal fat cells with cytoplasmic lipid vacuoles that scallop the nucleus.
Fibrous Tumors and Tumor-Like Lesions
Reactive Proliferations
1)
Nodular Fasciitis
is a self-limited, reactive fibroblastic proliferation that typically occurs in
adults on the volar aspect of the forearm. Patients characteristically present with a several-week
history of a solitary, rapidly growing mass. Preceding trauma is noted in up to 15% of cases.
Pathological features (Fig. 12-37)
Characteristically, the lesion is several centimeters in greatest dimension and nodular.
Mcroscopically, it is richly cellular and consists of plump, randomly arranged, immature-
appearing fibroblasts in an abundant myxoid stroma. The cells vary in size and shape (spindle
to stellate) and have conspicuous nucleoli and numerous mitoses.
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
183
2)
Myositis Ossifican
is distinguished from other fibroblastic proliferations by the presence of
metaplastic bone. It usually develops in the proximal muscles of the extremities in athletic
adolescents and young adults after trauma. The involved area is initially swollen and painful,
eventually evolving into a painless, hard, well-demarcated mass. It is vital to distinguish the
lesion from extra-skeletal osteosarcoma.
3)
Fibromatoses
are a group of fibroblastic proliferations distinguished by their tendency to
grow in an infiltrative fashion and, in many cases, to recur after surgical removal. Although
some lesions are locally aggressive, they do not metastasize. The fibromatoses are divided
into two major clinicopathologic groups: superficial and deep.
The superficial fibromatoses arise in the superficial fascia and include such entities as
palmar fibromatosis (Dupuytren contracture) (Fig. 12-38) and penile fibromatosis (Peyronie
disease). Superficial lesions are genetically distinct from their deep-seated cousins and are
generally more innocuous; they also come to clinical attention earlier, because they cause
deformity of the involved structure. The deep fibromatoses include the so-called desmoid
tumors that arise in the abdominal wall & muscles of the trunk and extremities, and within
the abdominal cavity (mesentery and pelvic walls). Deep fibromatoses tend to grow in a
locally aggressive manner and recur after excision. These tumors are gray-white, firm to
rubbery, poorly demarcated, infiltrative masses 1 to 15 cm in greatest dimension.
Microscopically, they are composed of plump cells arranged in broad sweeping fascicles that
penetrate the adjacent tissue.
Fibrosarcoma
is a malignant neoplasm composed of fibroblasts. Most occur in adults, typically in the deep
tissues of the thigh and retroperitoneal area. As with other sarcomas, fibrosarcomas often
recur locally after excision (>50% of cases) and can metastasize hematogenously (>25% of
cases), usually to the lungs.
Pathological features (Fig. 12-39)
These unecapsulated, infiltrative sarcomas show frequently areas of hemorrhage and necrosis.
Microscopically, the low-grade tumors may closely resemble fibromatosis; less differentiated
examples show densely packed spindled cells growing in a herringbone fashion, there are
frequent mitoses, and necrosis.
Fibrohistiocytic Tumors
These are composed of a mixture of fibroblasts and phagocytic, lipid-laden cells resembling
activated macrophages. The neoplastic cells are most likely fibroblasts. Nevertheless, a
significant number of such tumors actually derive from other mesenchymal cell types. Thus,
the term fibrohistiocytic, especially in regard to the malignant variants, should be considered
descriptive and not necessarily referring to a specific cellular origin. These tumors are divided
into benign, of intermediate malignant potential, frankly malignant.
1)
Benign Fibrous Histiocytoma (Dermatofibroma)
are relatively common benign lesions in adults presenting as small (<1 cm) mobile nodules in
the dermis or subcutaneous tissue. Microscopically, the lesion consists of bland, interlacing
spindle cells admixed with foamy, lipid-rich histiocyte-like cells. The borders of the lesions
tend to be infiltrative. The pathogenesis of these lesions is uncertain.
2)
Malignant Fibrous Histiocytoma (MFH)
is a term rather loosely applied to a variety of soft tissue sarcomas characterized by
considerable cytologic pleomorphism, the presence of bizarre multinucleate cells, and
storiform architecture. (Fig. 12-40) Despite the name, the phenotype of many such tumors is
fibroblastic and not histiocytic. Nevertheless, it is also important to note that several tumors
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
184
diagnosed as MFH actually exhibit markers for cells of other origin (e.g., smooth muscle
cells, adipocytes, skeletal muscle cells) and are therefore more appropriately classified as
leiomyosarcomas, liposarcomas, etc. MFH exhibiting fibroblastic differentiation are usually
large (5-20 cm), gray-white unencapsulated masses that often appear deceptively
circumscribed. They usually arise in the musculature of the proximal extremities or in the
retroperitoneum. Most of these tumors are extremely aggressive, recur unless widely excised,
and have a metastatic rate of 30% to 50%.
Skeletal Muscle Tumors
Rhabdomyosarcoma
Rhabdomyosarcoma is the most common soft tissue sarcoma of childhood and adolescence,
usually appearing before age 20. They occur most commonly in the head and neck or
genitourinary tract.
Chromosomal translocations are found in most cases; the more common t(2;13) translocation
fuses the PAX3 gene (controls skeletal muscle differentiation & development) on
chromosome 2 with the FKHR gene on chromosome 13. The hybrid PAX3-FKHR protein
probably involves dysregulation of muscle differentiation.
Gross features (Fig. 12-34)
Tumors arising near the mucosal surfaces of the bladder or vagina, can present as soft,
gelatinous, grapelike masses, designated sarcoma botryoides. In other cases they are
deceptively demarcated or infiltrative grayish-white to brownish masses.
Microscopical features
o Rhabdomyosarcoma is histologically subclassified into the embryonal, alveolar, and
pleomorphic variants.
o The rhabdomyoblast is the diagnostic cell in all types; it exhibits granular eosinophilic
cytoplasm, and may be round or elongated; the latter are known as tadpole or strap cells and
may contain cross-striations visible by light microscopy.
o The diagnosis of rhabdomyosarcoma is based on the demonstration of skeletal muscle
differentiation, either in the form of sarcomeres under the electron microscope or by
immunohistochemical demonstration of muscle-associated antigens such as desmin and
muscle-specific actin.
Rhabdomyosarcomas are aggressive neoplasms. Location and the histologic variant of the
tumor influence survival; embryonal, pleomorphic, and alveolar variants have progressively
worsening prognoses. The malignancy is curable in almost two-thirds of children, but adults
do much more poorly.
Smooth Muscle Tumors
1)
Leiomyomas
are common, well-circumscribed neoplasms that can arise from smooth muscle cells
anywhere in the body, but are encountered most commonly in the uterus.
2)
Leiomyosarcomas
(15% of soft tissue sarcomas).
They occur in adults, more commonly females. Deep soft tissues of the extremities and
retroperitoneum are common sites. Microscopically, they show spindle cells with cigar-
shaped nuclei arranged in interweaving fascicles. (Fig. 12-41)Superficial leiomyosarcomas
are usually small and have a good prognosis, whereas retroperitoneal tumors are large, cannot
be entirely excised, and cause death by both local extension and metastatic spread.
Chapter 9 - Bones, Joints, and Soft Tissue Tumors
185
Synovial Sarcoma
(10% of all soft tissue sarcomas)
The cell of origin is unclear and is most certainly not a synoviocyte. Reflecting a non-joint
origin, 90% of synovial sarcomas are not intra-articular but rather paraarticular. They are
typically seen in the 20-40 years of age. Most develop in deep soft tissues around the large
joints of the extremities, especially around the knee (Fig. 12-42). Most synovial sarcomas
show a characteristic t(X;18) translocation, which relates to prognosis. Microscopically,
synovial sarcomas may be biphasic or monophasic. Classic biphasic synovial sarcoma
exhibits differentiation of tumor cells into both epithelial-like cells and spindle cells. The
epithelial cells are cuboidal to columnar and form glands or grow in solid cords or aggregates.
The spindle cells are arranged in densely cellular fascicles that surround the epithelial cells.
Immunohistochemistry is helpful, because the tumor cells are positive for keratin and
epithelial membrane antigen. Common metastatic sites are lung, bone, and regional lymph
nodes. Only 10% to 30% live for more than 10 years.
