1
Malpositions and malpresentations
Learning Objectives
:
By the end of this lect., the students should be able to:
1- Define lie (normal & abnormal), malposition & malpresentation.
2- List complications of malposition and malpresentation.
3- State management of different types of malpositions.
4- Determine management of different types of malpresentations.
5- Describe cord prolapse management.
Lie:
Is the relation of the long axis of the fetus with the long axis of the mother.
Normal lie is longitudinal (may be either cephalic or breech).
Abnormal lie
Where the long axis of the fetus is not lying along the long axis of the mother
- Transverse
- Oblique
- Unstable
Position:
The relationship of the dominator of the presenting part to fixed points of
the maternal pelvis. Fixed points of maternal pelvis are: sacrum, sacro-iliac J, ileo-
pectineal eminences & symphysis pubis.
Denominator:
Is the most definable peripheral point in the presenting part. They are:
- Occiput in vertex
- Sacrum in breech
-
Mentum in face presentation
The vertex:
The area bounded by the anterior and posterior fontanelles and the parietal
eminences.
Malposition:
In about 90% of women in the late first stage of labour at term, the vertex present in
OA (occiput anterior). Right, left or direct occiput anterior, which is normal position.
In this case the head is well flexed allowing the smallest anteroposterior diameter
(suboccipito-brigmatic) diameter and transverse (biparietal) diameter, both 9.5 cm. to
pass through the pelvis.
Malposition: Where the fetus is lying longitudinally and the vertex is presenting, but
it is not in OA (occiput anterior) position.
- OT occiput transverse (LOT, ROT)
- OP occiput posterior
Malpositions characterized by minor degree of deflection of the head and thus present
a larger anteroposterior diameter (occipito-frontal) of 11.5 cm. this larger diameter
associated with malposition is the cause of longer and difficult labours and more
operative deliveries. With effective uterine activity malposition corrects to normal
position with flexion of the head at the atlanto-occiptal joint and rotation forward of
the occiput.
2
EMalpresentation
Where the fetus presents in any manner other than vertex.
i. Breech
ii. Face
iii. Brow
iv. Shoulder
Malpositions and Malpresentations complications:
1. Carry increased risk for both Mother and Fetus.
2. Must be managed by experienced personnel.
Maternal Risks:
Fetal Risks:
•Prolonged labor
•Infection
•Obstructed labor
•Injury to bladder, vagina and rectum
•Maternal hemorrhage
•Thromboembolism
•Ruptured uterus
•Perinatal mortality and morbidity
•Cord prolapse
•Perinatal infection and meconium
aspiration
•Traumatic injury
OCCIPITO POSTERIOR POSITION:
Occiput usually lateral when head engages and in 80% will rotate to anterior position
during labor. Posterior position causes delay in 1
st
stage. Treatment if inefficient
uterus action, which may result in rotation to anterior.
Mechanism of labour:
With head engagement, occiput usually lateral, but rotate anterior during labour in 4
cases out of 5 and in 1/5 will rotate posterior
More common in the RT oblique diam.
If flexion increase during labour, the occiput will be the leading part and will rotate
anteriorly long rotation 3/8 of the circle
If deflexion persist the bregma will be the part which touch the pelvic floor first and
will rotate forward and the occiput backward (short backward rotation 1/8 of the cycle
and get (persistant occiput posterior) which may descend and born face to pubis.
Early in labour 15% were in OP position, where at the time of delivery 5% will have
persistent OP.
Etiology of Occipitoposterior Position:
Anteriorly situated placenta
Anthropoid pelvis
Flat Sacrum
Pendulous abdomen
Chance
R.O.P. three times as common as L.O.P.
Diagnosis and features of labour:
Abdominal palpation: flatting of the abdomen
below the umbilicus, limbs felt anterior, and the
3
back in the flank where the fetal heart best heard, deflexion revealed when the
prominence of sinciput and occiput felt at the same level above the symphysis pubis
with large head
Vaginal examination: accurate assessment of descend, flexion, and position.
May lead to:
- Deep Transverse Arrest
- Prolong 1
st
and 2
nd
stage of labour
- Early rupture of membranes with cord prolapse
- Skull usually engaged in occipito frontal diameter, if great compression may
cause intracranial hemorrhage and fetal death.
Management:
Severe “Back Labor” may warrant epidural anesthesia
Slow progress may need oxytocin
12% will deliver spontaneously O.P.
Transverse arrest may require operative intervention
Lack of progress may warrant C-section
The usual mode of labour will be:
- Spontaneous delivery as face to pubis.
- Delivery as face to pubis; assisted or not by forceps or ventous.
- Manual rotation and delivery as occiput anterior.
- Rotation with forceps and delivery as occiput anterior
Large episiotomy is usually needed.
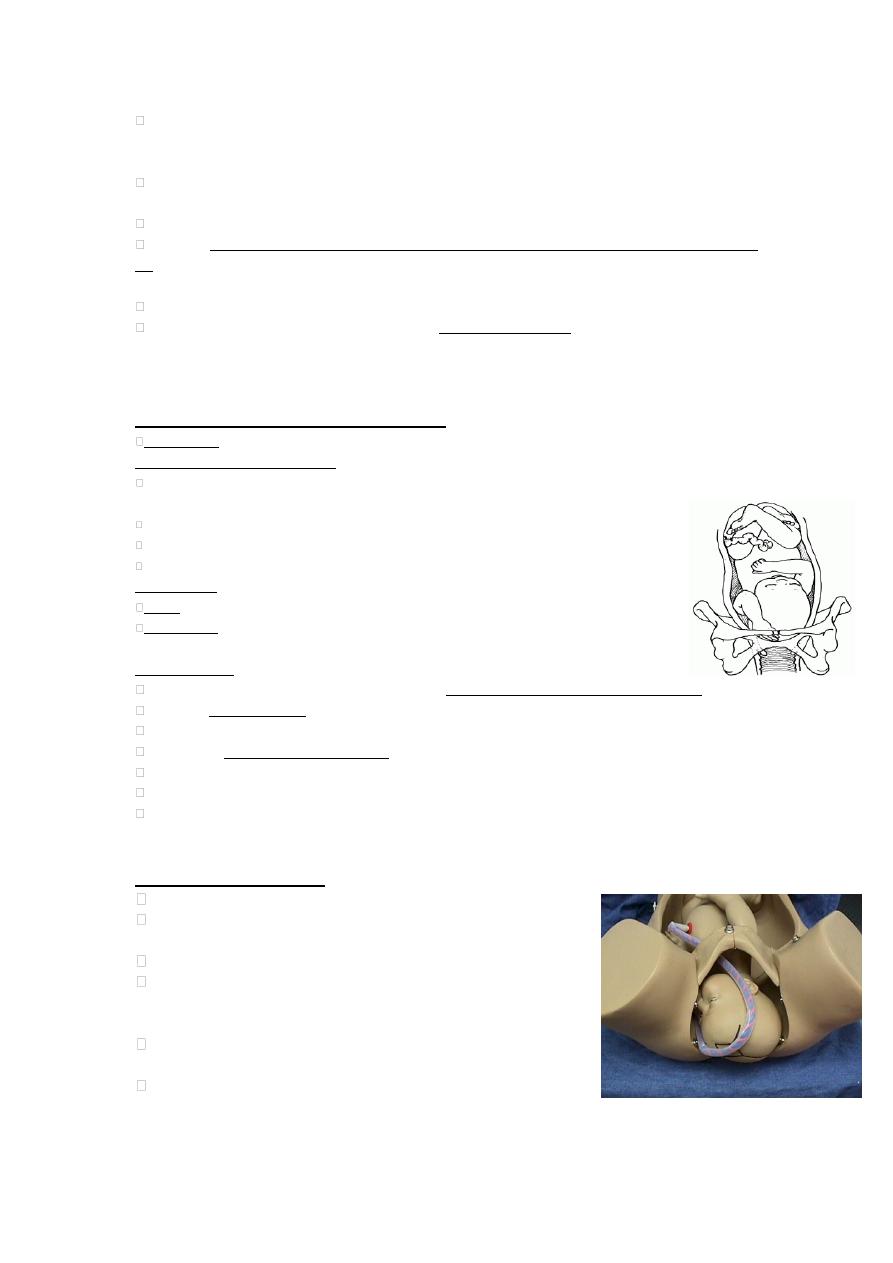
DEEP TRANSVERSE ARREST:
.
Arrest of labour when the fetal head has descend to
the level of ischial spine and the sagittal
sutures lies in the transverse diameter of the pelvis.
Diagnosis during the second stage and may end with
obstructed labour, especially occurs in android pelvis.
Treatment rotation manually, or with kielland’s
forceps or ventous then traction, otherwise C/S.
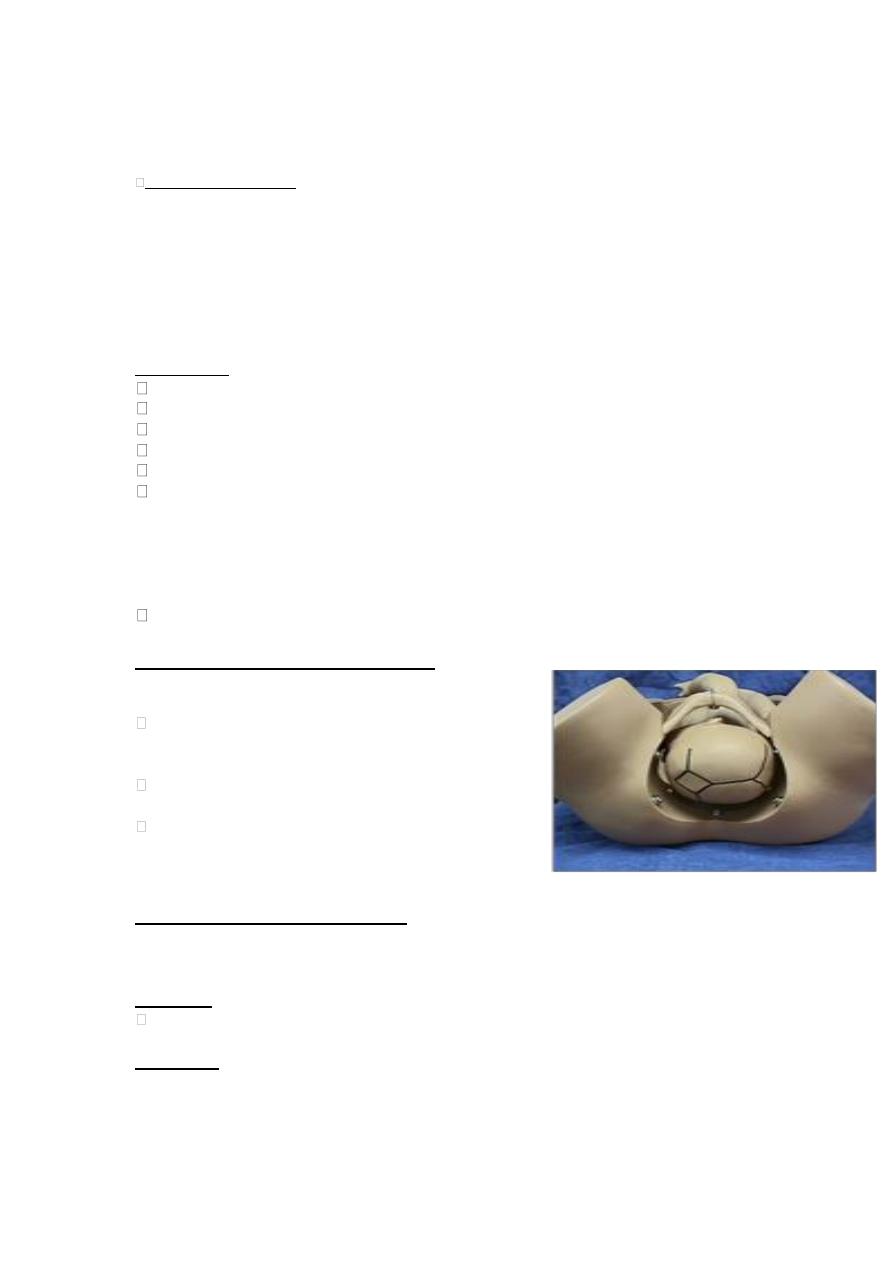
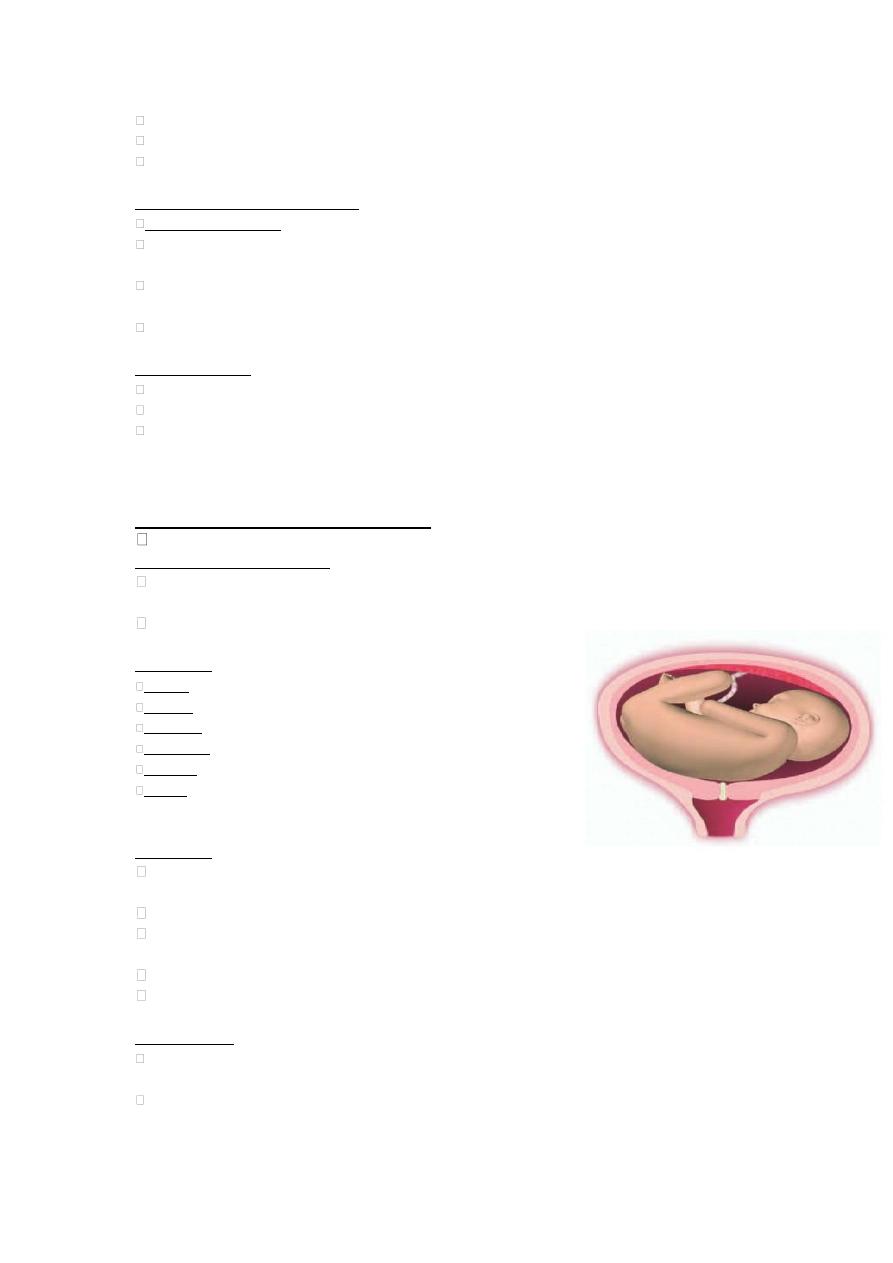
BREECH PRESENTATION:
At term, the head is usually the presenting part because of its smallest diameter is
match with the lower segment and because of its heaviness so tend to occupy the
lower segment of the uterus.
Definition
Where the fetal buttocks occupy the
lower part of the uterus.
Incidence: vary according to the gestation.
- 40 % at 26 weeks
- 20% 30Weeks
- 3% at term
4
AETIOLOGY: FLUPP
Fetal: prematurity, multiple pregnancy, anomalies: often those that restrict the ability
of the fetus to assume a vertex presentation, major malformation:hydrocephaly,
anencephaly, meningomyemocoele and most common malformation:congenital
dislocation of the hip.
Liquor: oligohydramnios/polyhydramnios
Uterine: anomalies (bicornuate, fibroid)
Placenta: praevia
Pelvis: contraction, pelvic tumours obstructing birth canal
TYPES OF BREECH:
- Frank (breech with extended legs): 65%
both fetal thighs flexed
both lower limbs extended at the knee
- Complete (fully flexed): 25%
when both fetal thighs and knees are flexed
- Footling (incomplete): 10%
One leg is flexed and the other leg is
extended, or one or two feet may present and
lie below the buttocks.
Because of the smaller and irregular presenting part of a breech compared with
a vertex labour, there is a greater incidence of cord prolapse which is higher
with foot presentations where it may be as high as 10%.
Diagnosis: most cases are recognized on antenatal clinical examination, where
identification being easier at later gestations and if the mother is maltiparous or has a
thin abdominal wall.
Palpation: the fetus will be in a longitudinal lie with the head palpable as a spherical
hard mass in the upper pole and the lower fetal pole is broader and is felt above or
within the pelvis.
Fetal heart auscultation, in the maternal upper abdomen usually above the umbilicus
because of the higher position.
Ultrasound
Vaginal Examination if she is in labour.
Mechanism of labour:
4 positions LSA ( left sacro-anterior) ,RSA, LSP, RSP
Mostly the bitrochanteric diameter 10cm engaged in a transverse diam. of pelvic
brim with the back anteriorly.
During labour the breech descends into the pelvic cavity, internal rotation brings the
bitrochanteric diameter into the ant. Post. Diam, of pelvic outlet.
The breech born by lateral flexion of the trunk
1
st
the anterior buttock app., and rest of the trunk born by further descend, with the
arm remain flexed, Then the ant. shoulder appear
The flexed head engaged, and then internal rotation occurs, occiput become anterior
and born.
Post rotation of the head occur to less extend, which is less favorable.
THE PROBLEM WITH BEING A BREECH:
FOUR FOLD INCREASE IN PERINATAL MORTALITY DUE TO…..
5
(1) Problems associated with the malpresentation
(2) problems of asphyxia and trauma due to the malpresentation.
PROBLEMS ASSOCIATED WITH THE MALPRESENTATION:
(1) prematurity and preterm PROM
(2) fetal anomalies
(3) placenta praevia and abruption
PROBLEMS
OF
ASPHYXIA
AND
TRAUMA
DUE
TO
THE
MALPRESENTATION:
(1)Cord prolapsed especially with footling and to less extent with flexed breech.
Which can cause rapid and sever hypoxia.
(2) Increased risk of CTG abnormalities: cord compression is common during a
breech vaginal delivery.
(3) Entrapment of the fetal head
- Through partly dilated cervix
- Unrecognized disproportion >10 min
(3) Traumatic injuries
CNS, intra-abdominal organs, nerve palsies (brachial plexus), muscle injuries. An
uncontrolled rapid delivery of the head may occur with a smaller fetus and this
predisposes to tentorial tears & intracranial bleeding
(4) Extension of fetal arms (nuchal arms)
MANAGEMENT OF BREECH PRESENTATION AT TERM:
A large trial comparing planned vaginal delivery and planned C/S for delivery of a
term breech baby, showed that C/S had better outcome with no difference in maternal
complications.
Management options:
(1) External cephalic version ECV.
(2) Elective caesarean section.
(3) Assisted vaginal delivery.
The current approach to management of breech presentation involves identification of
patients who may be a candidate for ECV. Patients who are at highest risk for
complications are delivered by Caesarean section. Patients who are carefully chosen
(after thorough discussion with them of options and risks) are candidates for vaginal
breech delivery.
EXTERNAL CEPHALIC VERSION:
The manipulative transabdominal conversion of breech to cephalic presentation
Benefit to the mother to avoid mortality and morbidity associated with breech
vaginal delivery and decrease the need for C/S
May be performed at 36 – 37 weeks.
The couple should receive counseling about the procedure, success rates,
complications, and subsequent management of persistent breech presentation.
Provided that there is no contraindications, it should be offered to all antenatal
women who have a breech presentation at term.
CONTRAINDICTAIONS:

6
Placenta previa
Uterine anomalies
Oligohydramnios or polyhadraminous.
Indicated vaginal delivery (fetal death, anomaly best delivered as breech)
Previous C/S or myomectomy scar.
Multiple gestations.
Pre – eclampsia or hypertension
Plan to deliver by Caesarean section for any other reasons.
* SUCCESS
60-70%
* TECHNIQUE
Should be performed in a setting where emergency C/S is available should there is
evidence of fetal compromised during or soon after ECV.
Ultrasound is needed to confirm the diagnosis, fetal attitude, position of the placenta
and the quantity of amniotic fluid.
After 36W
Cardiotocography (CTG) prior and after the procedure to confirm fetal health
Tocolytic drugs may be needed to stop uterine contactions.
Disengaging the breech by moving the fetus up and away from the pelvis, shifting it
to the sideways position, followed by forward somersault to move the head to the
lower pole
Anti D (if Rh negative)
* Complications of External Cephalic Version:
Placental Abruption
Cord accident
Rh Sensitization – transplacental hemorrhage.
“Fetal Distress”
Neurological Injury
Premature Delivery or premature rupture of the membranes.
7
* Theoretical Benefits of Late ECV:
Low Reversion Rate
Few Unnecessary External Cephalic Versions
A Prompt Delivery with Healthy Child Can Occur if There is a Complication during
the External Version
* Factors Influencing Successful External Cephalic Version:
Experienced Operator
Earlier Gestation
Unengaged Breech
Complete or Incomplete Breech
Normal Amniotic Fluid Volume
Cooperative, Relaxed Patient
Multiparous Patient
Infant not Macrosomic
Mother not Obese
Factors that strengthen recommendations for a Caesarean
Section
:
Fetal weight <2500g; >3500g
Small pelvis on pelvimetry or very flat sacrum.
Pimigravida
Previous Caesarean section
Preterm breech
Hyperextended fetal head
Placenta praevia
Oligohydramnios
footling breech
If any complication with breech presentation, ex PET, OR IUGR
Factors that increase the likelihood of a successful vaginal
breech delivery:
Frank or complete breech
Good pelvimetry (Judged clinically)
Flexed neck
Maltiparous
EFW 2500-3500g
Breech deeply engaged
Gestational age >36 weeks
No other maternal or fetal indication for CS
Experienced obstetrician, anesthetist and pediatrician
present at delivery
Spontaneous onset of labour
Management of vaginal breech delivery:
As soon as the memb. Rupture vag. Ex done to exclude cord prolapsed.
If any maternal or fetal distress, change to C/S.
8
Successful outcome depends on normal rate of cervical dilation; descend of the
breech and a normal fetal heart rate. With poor progress of labour, cephalo-pelvic
disproportion should be considered.
Second stage of labour need full cooperation of the mother, epidural anesthesia
provide pain relieve in labour and prevent the mother from bearing down before
cervical full dilation.
So should not be placed in Lithotomy position until anterior buttock and the anus
are in view over the mother perineum with no retraction between contractions.
Episiotomy done as soon as the anus is visible in primiparous.
Delivery of the feet and leg spontaneously by mother effort, pulsation in the cord
observed.
Once the ant. scapula appear, the anterior arm hooked out then posterior arm
Lovset’s manoeuvre for delivery of extended arms may be needed.
Baby’s body allowed hanging down, as soon as the nape of the neck appears.
At this point, delivery of the head is assisted by one of the three methods:
1- The body of the baby is swung over the maternal abdomen until the mouth and
nose of the fetus become visible.
2- Two fingers are press over the maxilla to flex the head and delivery is
accomplished by shoulder traction (Mauriceau-Smellie-Veit maneuver).
3- Forceps are applied to the head from below while an assistant holds the baby just
below the horizontal.
BREECH EXTRACTION:
Where the obstetrician completely removes the entire body from the uterus.
ONLY used for operative delivery of the second twin (usually in conjunction with
an internal podalic version) at caesarean section.
Spontaneous or assisted breech delivery is the only acceptable method for delivering
a singleton breech vaginally
“It is now well accepted as the standard in the medical profession that a vaginal
breech delivery should be undertaken only under very limited circumstances.”
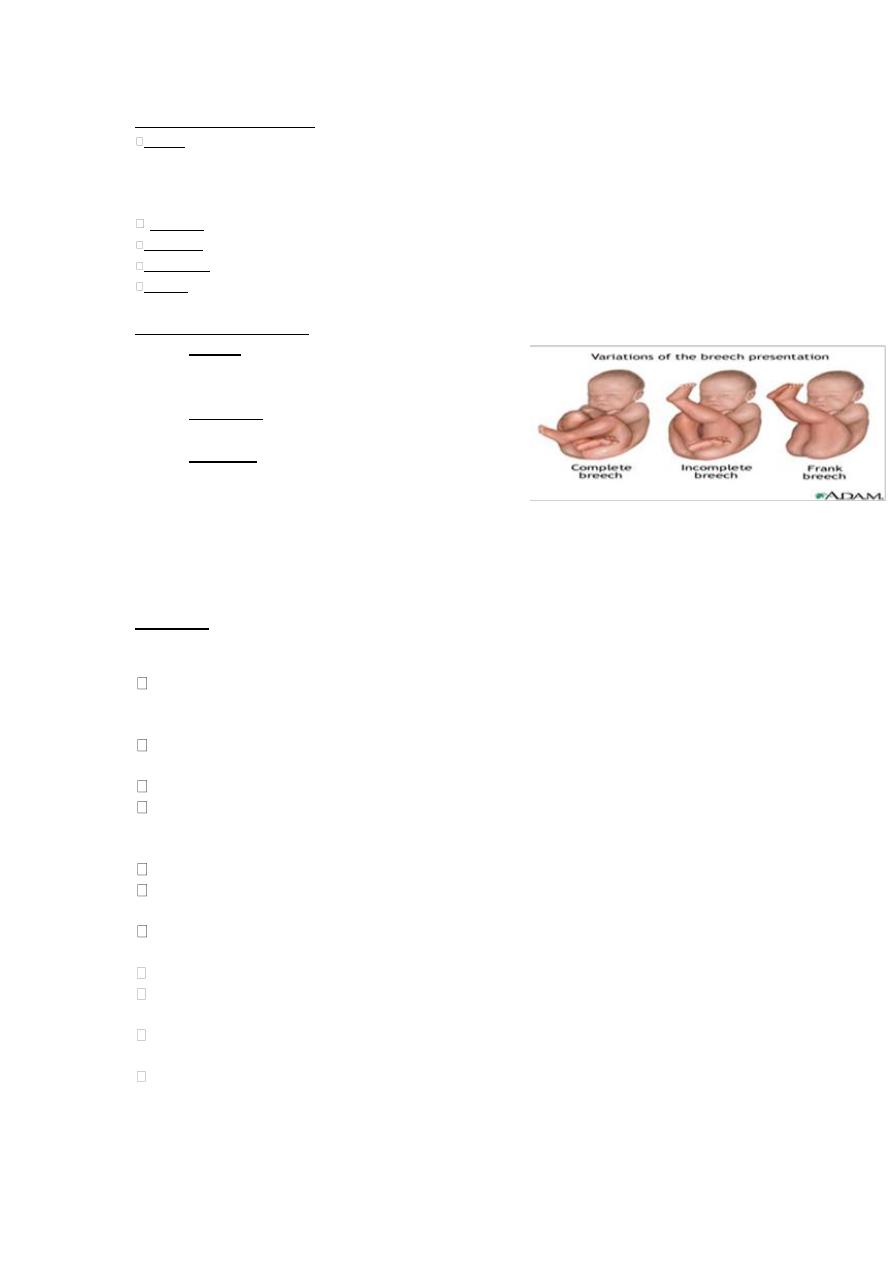
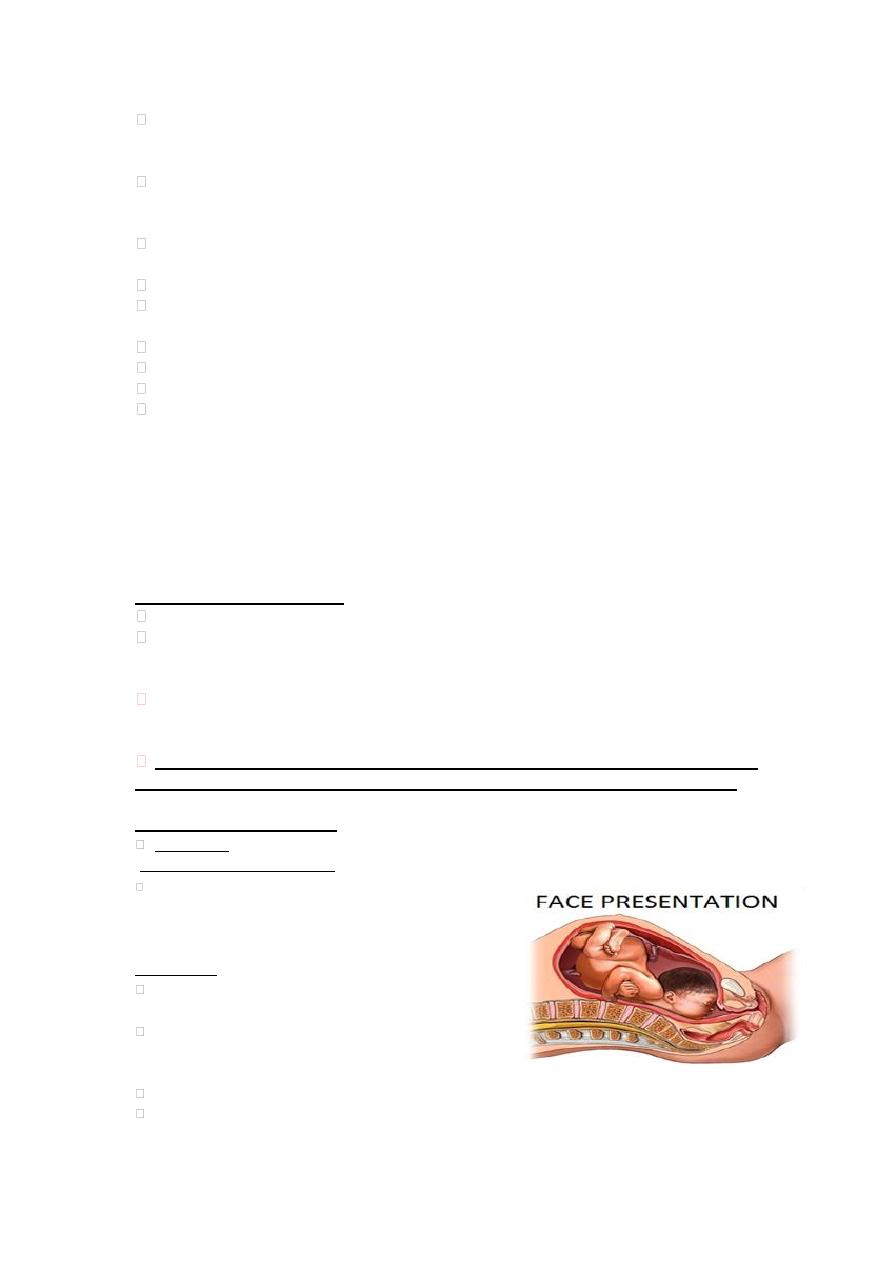
FACE PRESENTATION:
Incidence: 1 in 500-1000 deliveries
Mechanics of presentation:
Characterized by extreme extension of the fetal
head so the face (rather than the skull) presents to
the birth canal.
Aetiology:
The general causes of malpresentation apply for
face presentation.
Any factor that favors extension such as fetal
goitre, anencephaly, several loop of cord around
the neck
Fetalmuscloskeletal abn.
High maternal parity.
9
At diagnosis:
60% mento-anterior MA
15% mento-transverse MT
25% mento-posterior MP
Diagnosis:
Abd. Ex. The prominence of the head is palpable at a higher level on the opposite
side of the fetal spine.
Generally diagnosed on vaginal examination in labour, avoid damaging the eyes by
fingers or antiseptic. Palpation of the nose, eyes and the hard gum margins should
confirm the presentation.
May be confused with breech presentation…REMEMBER
Anus is in line with the ischial tuberosities; mouth forms a traingle with the molar
prominence.
MANAGEMENT
Submentobregmatic diameter equals suboccipitobregmatic diameter of vertex
presentations.
labour occurs by internal rotation with the chin delivering under the symphysis, and
the head then delivers by FLEXION under the symphysis.
60-80% of face presentations deliver spontaneously (approximately 50% of MP
presentations will undergo rotation during labour, and most MT presentations will
rotate to MA)
If MP, even thought the diameters are the same as MA, the diameters of large
frontal bones prevent descent behind the narrow retropubic arch, and in this situation
C/S is indicated.
If MT or MA, with poor progress in the first or second stage , then the safer option
is C/S, which also indicated in case of contracted pelvis, or cord prolapsed.
Augmentation for poor progress may be used on a face presentation
Forceps may be used on a MA or MT if it is at the outlet with episiotomy and the
need for skilled personal. Vacuum is contraindicated.
BROW PRESENTATION:
Incidence: 1:1500 -3000, prematurity is important risk factor.
Mechanics of presentation:
Head is half extended such that attitude is halfway between
flexion (vertex) and hyperextension (face).
Usually transitional- when the head is in the process of converting
from a vertex to a face or vice versa.
Presenting part is between the facial orbits and anterior fontanelle.
Mentovertical diameter is presenting diameter 13cm; while its 9.5cm
for suboccipitobregmatic (vertex) or submentobregmatic (face).
DIAGNOSIS:
- On abdominal, ex, head above the brim, cephalic prominence on the same side
as the back
- On vaginal examination, palpate:
Anterior fonatnelle
Orbital ridges
Eyes
11
Nose, mouth and chin cant felt
Nasion more often found anterior
In labour large caput succedaneum may make diagnosis impossible
MANGEMENT IN LABOUR:
Initially expectant;
50-75% will either flex to a vertex, or extend to a face with contractions from behind
meeting soft tissue and bony resistance below and will therefore deliver vaginally
High incidence of prolonged labour and dysfunctional labour, cord prolapse when
the membranes rupture with high incidence of uterine rupture in neglected cases
Agumentation with oxytocin is not advisable
Persistent brow:
The diameter is undeliverable vaginally
Delivery by caesarean section
Some time with dead fetus, extreme prematurity and capacious pelvis, vag. delivery
happened. Although vaginal delivery is possible in the preterm fetus, there is small
risk of spinal cord injury and C/S is preferred.
SHOULDER PRESENTATION:
Incidence at term: 1 in 200.
Mechanics of presentation:
long axis of the fetus is perpendicular to long axis of mother (i.e. occurs in
transverse lie)
Mostly the back is anterior
Aetiology:
Fetal : Prematurity, multiple pregnancy
Liquor: Polyhydramnios
Uterine :Anomaly
Placenta: Praevia
Pelvis :contraction, tumour
Parity :high maternal parity (80% of cases occur in women
who are para3 or more)
Diagnosis:
On abdominal palpation, no fetal pole is presenting to the pelvis, and the head is
palpable in either the right or left iliac fossa.
Fundus is lower than normal.
On vaginal examination, elongated bag of membrane, or may palpate ribs, scapula,
clavicle.
In advanced labour, fetal hand and arm may prolapse into the vagina.
If late presentation, may present with obstetrical ring.
Management:
With the onset of labour most cases of transverse lie will be converted to
longitudinal lie due to increase muscular tone of the uterus.
If rupture of the membranes occur with the fetus in transverse lie or with cord or arm
prolapsed, then C/S should be performed.
11
If late diagnosis, the fetus may be impacted in the transverse lie then C/S with
midline vertical incision is advised to avoid fetal trauma or lateral extension of
transverse incision of the uterus.
If early preterm fetus or small macerated dead, then spontaneous expulsion occurs
by extreme flexion of the body.
In neglected case uterine rupture may occurs.
Consider ECV prior to labour, if its early in labour or at 41 weeks if still transverse
lie, by stimulation of contraction with oxytocine and artificial rupture of the
membranes (Stabilizing induction).
If polyhydraminous, do amniocentesis to maintain successful version.
If diagnosed late in labour, deliver by Caesarean section (as fetal head and trunk
would have to enter pelvis at the same time to deliver vaginally). Decapitation in dead
fetus to avoid C/S.
COMPOUND PRESENTATION:-
Incidence: 0.1%
Mechanism of presentation:
When a fetal extremity prolapses alongside the presenting part, and both enter the
maternal pelvis at the same time.
Vertex-hand
Breech-hand
Vertex-arm-foot
Aetiology :
Fetal : Multiple, premature
Maternal : Multiparity
Management:
Usually have early rupture of membrane, diag. after rupture of the membrane
Exclude cord prolapse
Occurs in up to 20% of cases
Otherwise expectant management
Mostly doesn’t interfere with normal delivery
Vertex-foot: try to gently reposition the lower extremity
If arm prolapses in vertex-hand, wait and see if it moves as head descends; if it
converts to shoulder presentation, deliver by CS
CORD PROLAOSE:
Incidence 0.2% of all birth
Causes: low birth wt <2.5, prematurity,
malpresentation, 2
nd
twin, multiparous.
Outcome: increase PNM and morbidity
Management: alive baby with viable gestation, elevate the
presenting part and rapid C/S (the dx-C/S interval is
important).
Viable fetus and advance in labour (late 1
st
stage or 2
nd
stage), assisted delivery as forceps or ventous.
To elevate the presenting part( knee-chest position,
trendelenburge position, or manual elevation).
………………………………………………………………………………………...
