Histology
lecture -2-
Connective tissue
Connective tissue
is the term traditionally applied
to a basic type of tissue of mesodermal origin which
provides structural and metabolic support for other
tissues and organs throughout the body.
In addition to a mechanical structural role,
connective tissues mediate the exchange of
nutrients, metabolites and waste products between
tissues and the circulatory system.
All supporting/connective tissues are composed of
a population of specialized support cells, some of
which produce an abundant extracellular matrix
Supporting tissues have important metabolic
roles such as the storage of fat (white adipose
tissue) and the regulation of body temperature
in the newborn (brown adipose tissue).
Cells of the immune system enter support
tissues where they assist in defense against
pathogenic microorganisms.
In response to tissue damage, the processes of
tissue repair are largely a function of
supporting tissues.
Loose Connective
Tissues
Embryonic
Connective Tissues
Connective Tissues
of Special Purposes
Dense Connective
Tissues
Connective
tissue
Embryonic
Connective
Tissues
Mesenchymal
Connective
Tissue
Mucoid
Connective
Tissue
Loose
Connective
Tissues
Areolar
Connective
Tissue
Adipose
Tissue
Reticular
Connective
Tissue
Dense
Connective
Tissues
Dense Regular
Connective
Tissue
Dense
Irregular
Connective
Tissue
Elastic
Connective
Tissue
Connective
Tissues of
Special
Purposes
Blood
Bone
Cartilage
Component of connective tissue
Cells
Fixed cells
Transient cells
Ground
substances
Glycosaminoglycan
Proteoglycan and
adhesive
glycoprotein
Fibers
Collagen
Ellastic
Reticular
Embryonic connective tissue
1.
Mesenchyme
Location
Under the skin of developing fetus
Around blood vessels in the adult
Function
Form other type of CT .
Histological criteria.
Irregular shaped mesenchymal cells
Ground substance of reticular fibers
Specialized cells.
Mesenchymal cells
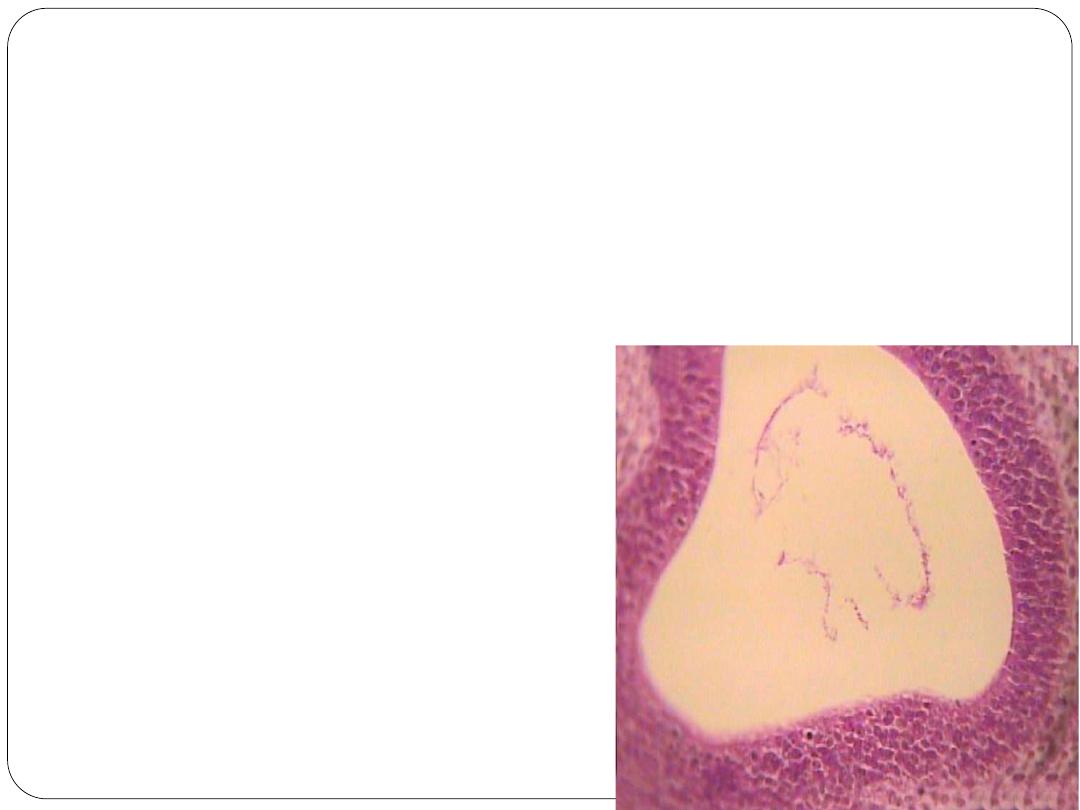
Mucous Connective Tissue .
Location
Umbilical cord
Function
Support
Histological Findings
Widely scattered Fibroblasts
o Spindle-shaped cells
Ground substance is viscous, jelly-like appearance (Wharton’s jelly)
Specialized cells.
fibroblasts.
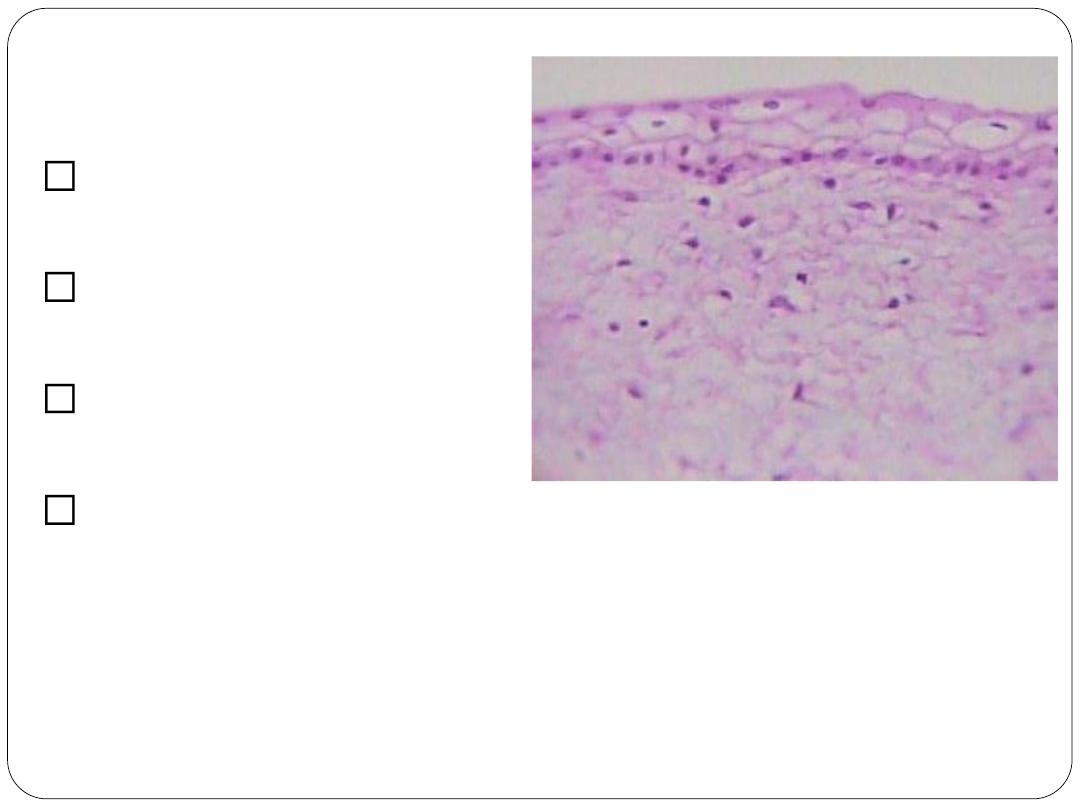
Connective tissue cells
Resident (fixed)cells.
1. Fibroblast-
Secrete both fibers and ground substance
of the matrix-elongated cells with ovoid (cigar-shaped)
nuclei and thin cytoplasm
2. Fibrocyte.
3. Myofibroblast-
have a contractile function as well as
a role in secretion of extracellular matrix.
4. Adipocytes-small condensed nucleus on the side,
very thin rim of cytoplasm-store fat.
5. Melanocyte (pigment cell) (originating
from the neural crest)
RESIDENT/PERMANENT CT CELLS
MATRIX-”FORMING” CELLS
Designated by suffix -blast
MATRIX-“MAINTAINING” CELLS
Designated by suffix -cyte
MATRIX-”REMOVING” CELLS
Designated by suffix -clast
Fibrocyte
Adipocytes

Melanocytes
Transient cells.
1.
histocyte – macrophage
2.
granulocyte : neutrophilic-
eosinophilic-basophilic
3.
lymphocyte
4.
monocyte – precursor of macrophage
5.
plasma cell – effector of immune
response
6.
mast cell – heparin and histamin –
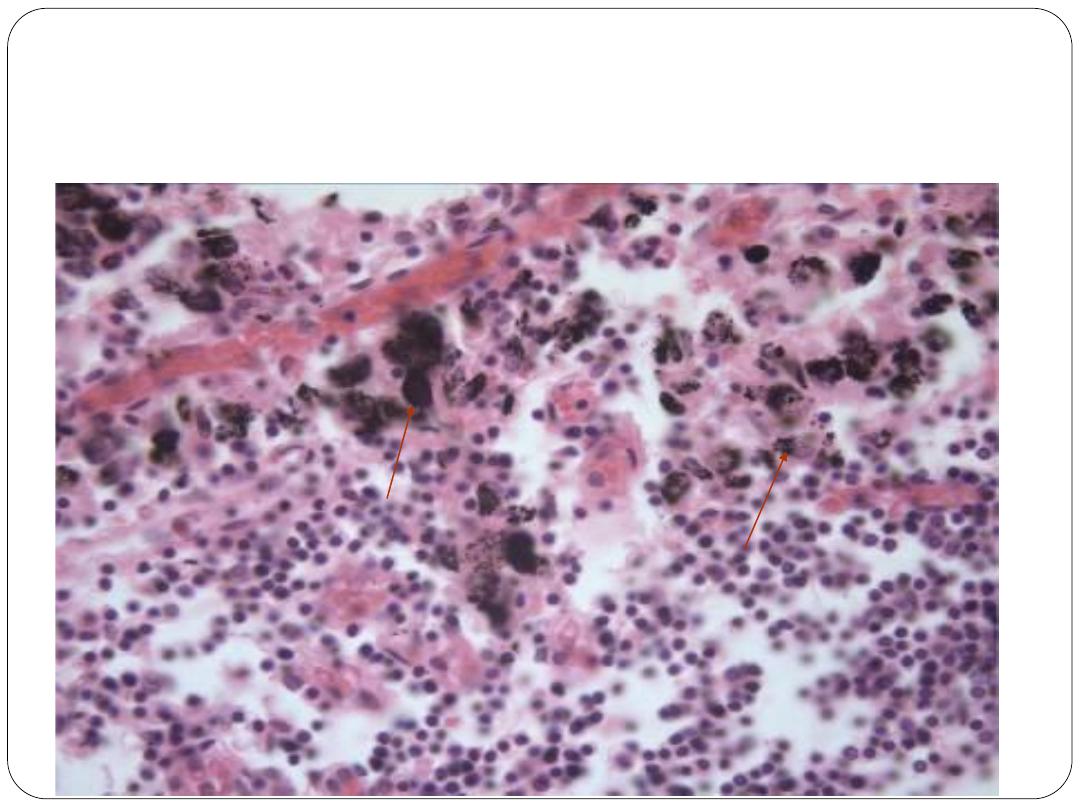
Macrophages in lymph node
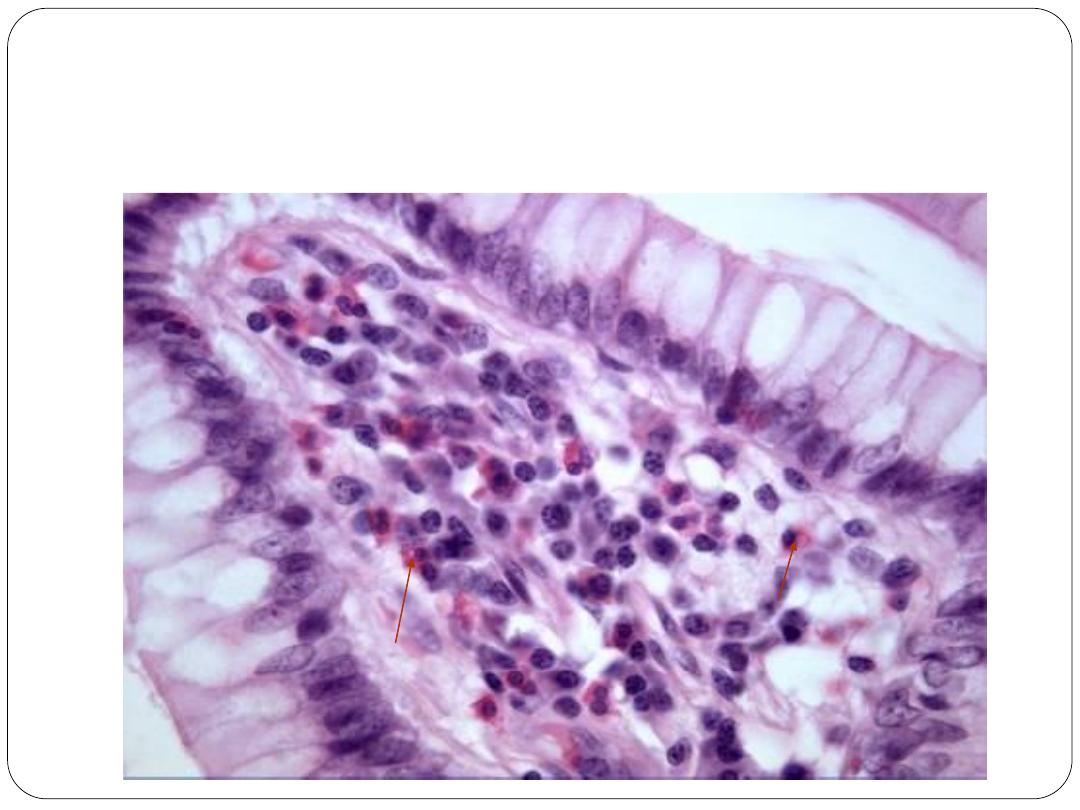
Eosinophils in lamina propria
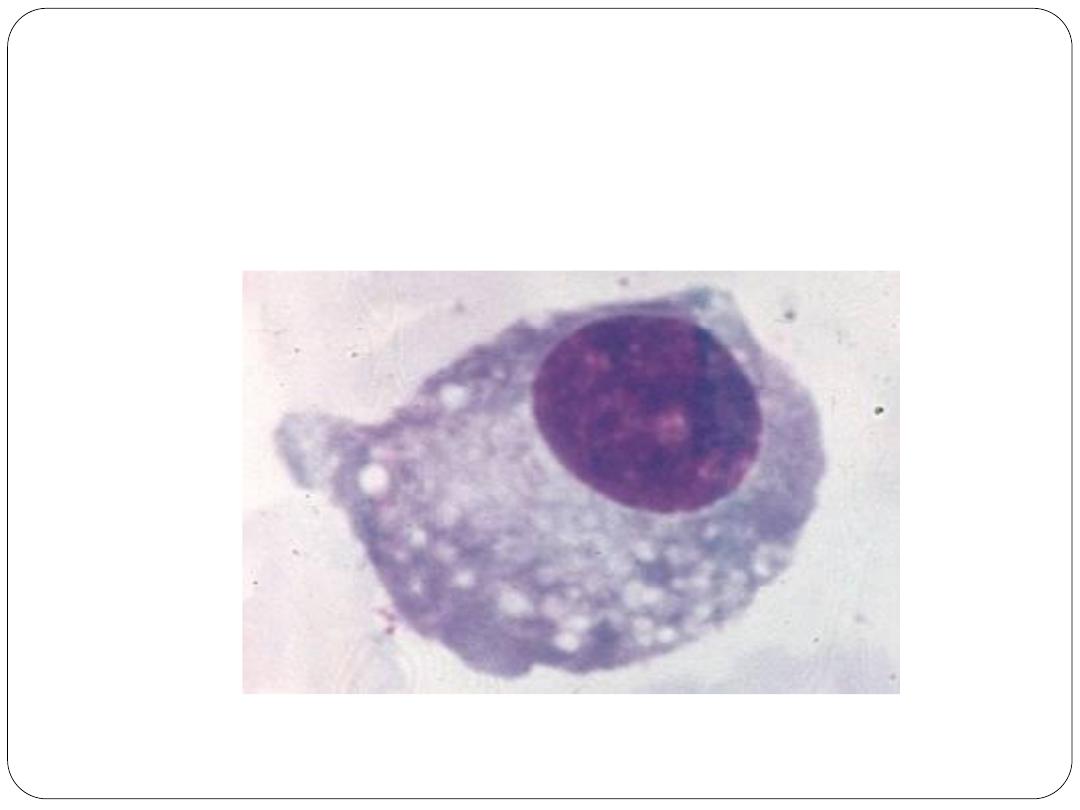
Plasma cells
Collagen
the main fiber type found in most supporting
tissues and is the most abundant protein in the
human body.
Its most notable function is the provision of tensile
strength.
Collagen is secreted into the extracellular matrix
in the form of tropocollagen which consists of
three polypeptide chains (alpha chains) bound
together to form a helical structure 300 nm long
and 1.5 nm in diameter.
In the extracellular matrix, the tropocollagen
molecules polymerise to form collagen. At least
27 different types of collagen have now been
delineated on the basis of morphology, amino acid
composition and physical properties.
Type I collagen
Found in fibrous supporting tissue, the dermis of the
skin, tendons, ligaments and bone, in a variable
arrangement from loose to dense according to the
mechanical support required.
The tropocollagen molecules are aggregated to form
fibrils strengthened by numerous intermolecular
bonds. Parallel collagen fibrils are further arranged
into strong bundles 2-10 μm in diameter which confer
great tensile strength to the tissue; these bundles are
visible with the light microscope
Type II Collagen
is found in hyaline cartilage and consists
of fine fibrils which are dispersed in the
ground substance
Type III collagen
makes up the fiber type known as reticulin which
was previously thought to represent a separate
species of fiber because of its affinity for silver
salts.
Reticulin fibers form the delicate branched
'reticular' supporting meshwork in highly cellular
tissues such as the liver, bone marrow and
lymphoid organs
Type IV collagen
does not form fibrils but rather a meshlike
structure and is an important constituent of
basement membranes.
Type VII
forms anchoring fibrils that link to
basement membrane.
remaining collagen types are present in
various specialised situations
Elastin
is an important structural protein which is arranged as
fibers and/or discontinuous sheets in the extracellular
matrix particularly of skin, lung and blood vessels where
it confers the properties of stretching and elastic recoil.
Elastin is synthesised by fibroblasts in a precursor form
known as tropoelastin which undergoes polymerisation
in the extracellular tissues.
Deposition of elastin in the form of fibers requires the
presence of microfibrils of the structural glycoprotein
fibrillin which become incorporated around and within
the elastic fibers
Reticulin fibers
Reticulin fibers form a delicate supporting
framework for many highly cellular organs such as
endocrine glands, lymph nodes and the liver.
In such organs, a fine network of branching fibres
ramifies throughout the parenchyma usually
anchored to a dense, collagenous capsule and septa
which traverse the tissue.
Reticulin is a nonbanded form of collagen designated
collagen type III.
usually poorly stained in standard preparations but are
able to adsorb metallic silver by which they are stained
black. This phenomenon led early histologists to
believe that reticulin had a completely different
chemical composition from that of collagen.
Reticulin is the earliest type of collagen fiber to be
produced during the development of all supporting
tissues and is also present in varying quantities in most
mature supporting tissues.
Ground substance
derived its name from being an amorphous
transparent material which has the properties of a
semifluid gel.
Tissue fluid is loosely associated with ground
substance, thereby forming the medium for passage
of molecules throughout supporting tissues and for
the exchange of metabolites with the circulatory
system.
mixture of long, unbranched polysaccharide chains
of seven different types, each composed of
repeating disaccharide units
One of the disaccharide units is usually a uronic acid and
the other an amino sugar, thus giving rise to the modern
term glycosaminoglycans (GAGs).
The glycosaminoglycans are acidic (negatively charged)
due to the presence of hydroxyl, carboxyl and sulphate
side groups on the disaccharide units.
Hyaluronic acid is the predominant GAG in the loose
supporting tissues and is the only one without sulphate
side groups.
Unlike many proteins, GAG molecules are not flexible
enough to form globular aggregates but remain in an
expanded form, thus occupying a huge volume for
relatively small mass
Their highly charged side groups render them
extremely hydrophilic, thus attracting a large
volume of water and positive ions, particularly
sodium, which constitute extracellular fluid. The
extracellular fluid imparts the characteristic
turgor of supporting tissue.
The structural glycoproteins
group of molecules composed principally of
protein
chains
bound
to
branched
polysaccharides.
The structural glycoproteins include two
fibrilforming
molecules,
fibrillin
and
fibronectin, and a number of nonfilamentous
proteins including laminin, entactin and
tenascin which function as links between cells
and extracellular matrix.
Fibrillin forms microfibrils 8-12 nm in diameter
which, in certain specialised situations, e.g. the
mesangium of the kidney , appear to enhance
adhesion
between
other
extracellular
constituents.
Fibrillin is a constituent of elastic fibers where it
appears to play a role in the orderly deposition of
the fibers.
Fibronectin plays a part in controlling the deposition
and orientation of collagen in extracellular matrix and
the binding of the cell to the extracellular material.
Cell membranes incorporate a group of transmembrane
protein complexes called integrins which act as cell
adhesion molecules. One of these, the fibronectin
receptor, establishes bonds within the cell to the actin
filaments of the cytoskeleton and binds with fibronectin
externally. The fibronectin in turn binds with collagen
and the glycosaminoglycan, heparin sulphate, thus
establishing
structural
continuity
between
the
cytoskeleton and the extracellular matrix.
Laminin is a major component of basement
membranes, binding with specific cell adhesion
molecules so as to form links between cell
membranes and other constituents of the basement
membrane.
Entactin, another nonfibrillary protein, has the
function of binding laminin to type IV collagen in
basement membranes.
Tenascin also binds to integrins and is important in
the embryo where it appears to be involved in
control of nerve cell growth.
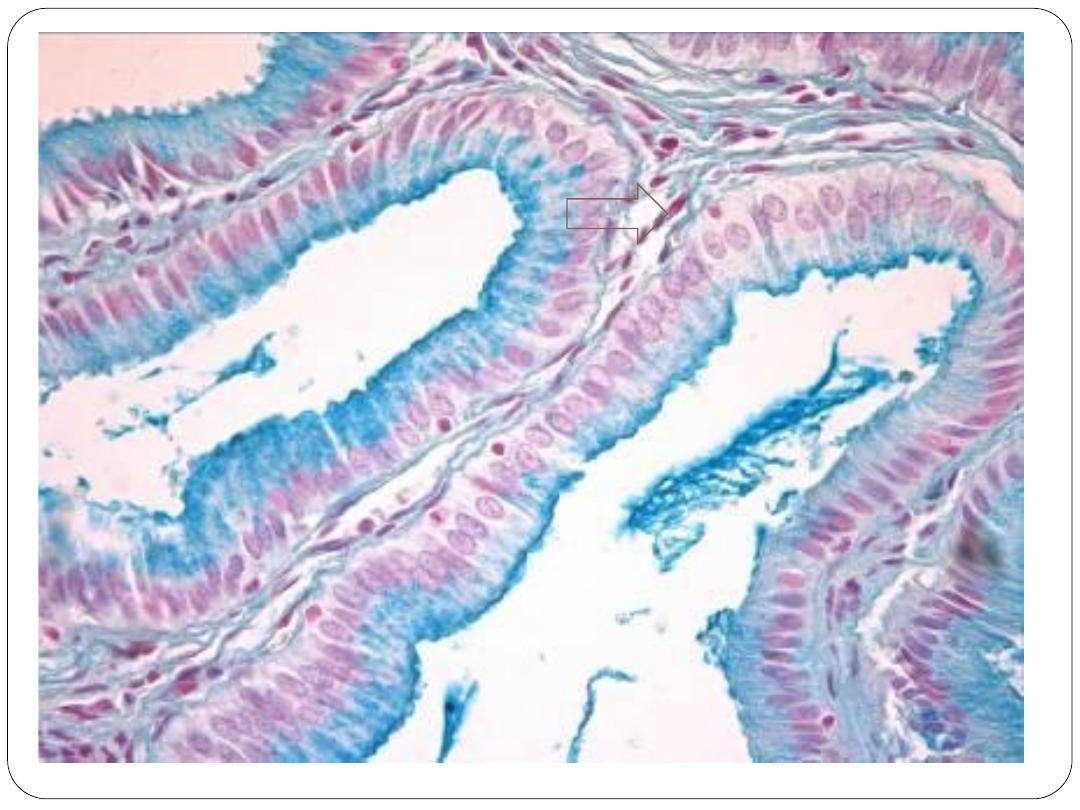
Basement membrane
sheetlike arrangements of extracellular matrix proteins
which act as an interface between the support tissues
and parenchymal cells.
associated with epithelial and muscle cells, as well as
forming a limiting membrane around the central
nervous system.
The term derives from the fact that the first basement
membranes to be recognized were those lying beneath
the basal cells of surface epithelia.
In the context of muscle and nervous tissue, the term
external lamina may also be applied.
Basement membrane is also involved in the control of
epithelial growth and differentiation, forming a barrier
to downward epithelial growth; this is only breached if
epithelia undergo malignant transformation.
Epithelium is devoid of blood vessels and the basement
membrane must therefore permit the flow of nutrients,
metabolites and other molecules to and from the
epithelium.
The main constituents of basement membranes and
external laminae are the glycosaminoglycan heparan
sulphate, the fibrous protein collagen type IV, and the
structural glycoproteins fibronectin, laminin and
entactin.
With the electron microscope, the basement membrane
is seen to consist of three layers. A relatively
electronlucent layer, the
lamina lucida
(ranging from
10 to 50 nm in width), abuts the basal cell membrane of
the parenchymal tissue. The intermediate layer is
electrondense and is thus known as the
lamina densa
;
depending on the tissue, this varies from 20 to 300 μm
in thickness. Beyond the lamina densa is a broad,
relatively electronlucent layer known as the
lamina
fibroreticularis
which merges with the underlying
supporting tissue.
Copyright © 2010 Pearson Education, Inc.
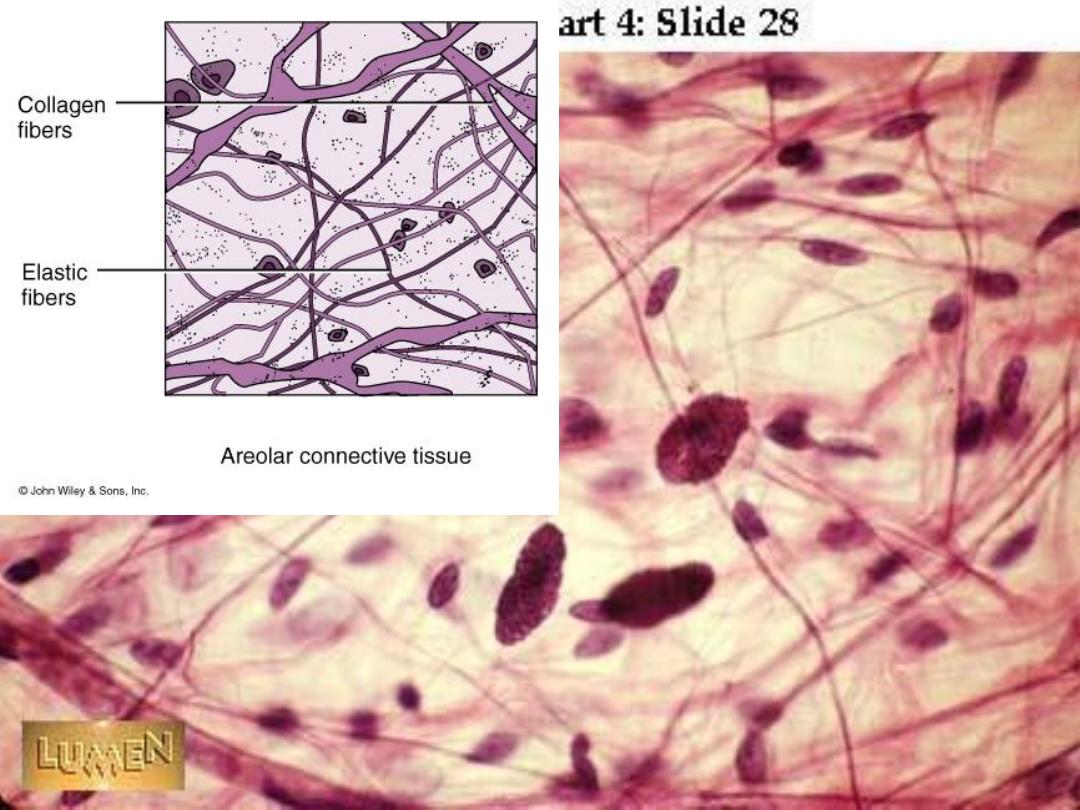
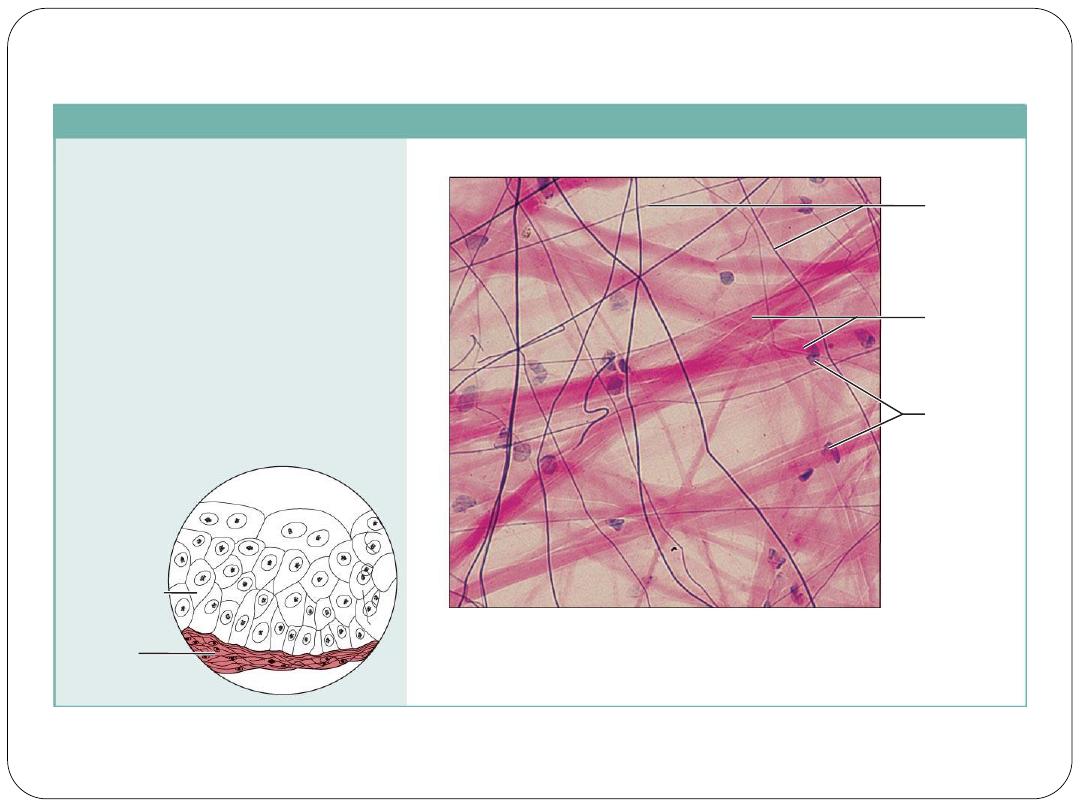
(a) Connective tissue proper: loose connective tissue, areolar
Description: Gel-like matrix with all
three fiber types; cells: fibroblasts,
macrophages, mast cells, and some
white blood cells.
Function: Wraps and cushions
organs; its macrophages phagocytize
bacteria; plays important role in
inflammation; holds and conveys
tissue fluid.
Location: Widely distributed under
epithelia of body, e.g., forms lamina
propria of mucous membranes;
packages organs; surrounds
capillaries.
Photomicrograph: Areolar connective tissue, a
soft packaging tissue of the body (300x).
Epithelium
Lamina
propria
Fibroblast
nuclei
Elastic
fibers
Collagen
fibers
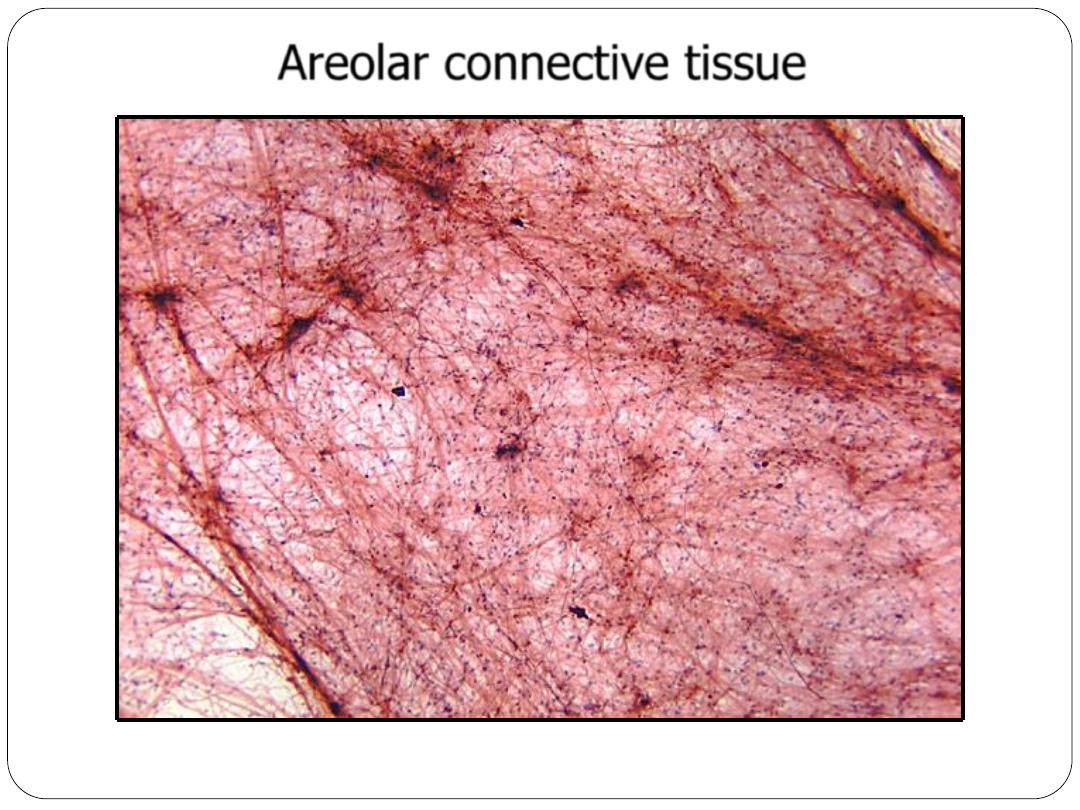
Mesentery spread – Verhoeff – 4x objective
This is a loose connective tissue. See how widely spread the fibers and cells
are separated from one another.
Areolar connective tissue
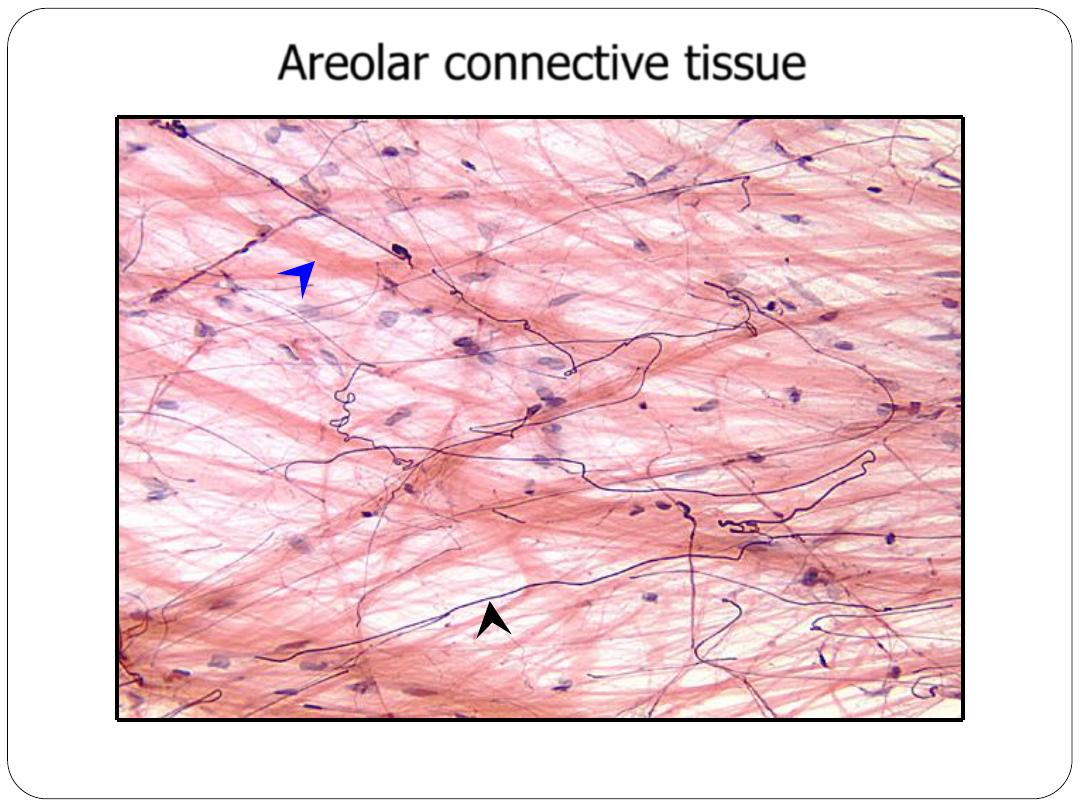
Elastin fiber (black arrowhead);
collagen fiber (blue arrowhead); the nuclei are of
various cell types, some of which are permanent and others that wander through
Mesentery spread – Verhoeff – 10x objective
Areolar connective tissue
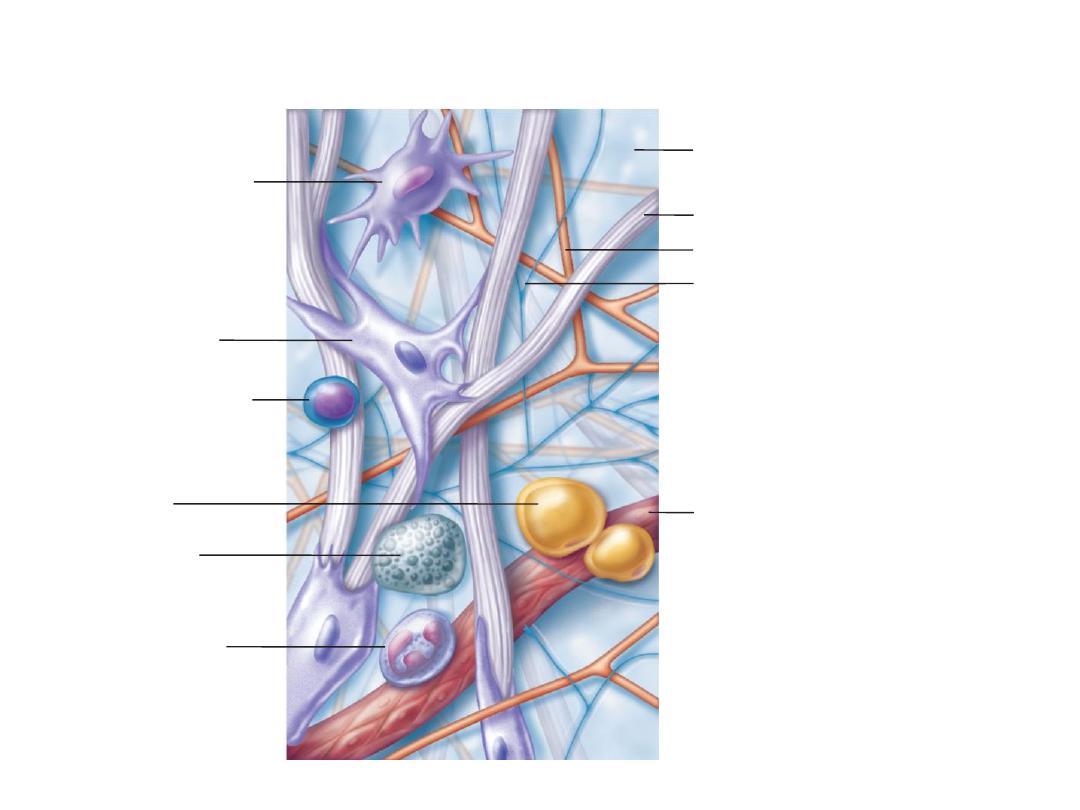
Copyright © 2010 Pearson Education, Inc.
Areolar connective tissue: A prototype (model) connective tissue.
Macrophage
Fibroblast
Lymphocyte
Fat cell
Mast cell
Neutrophil
Capillary
Cell types
Extracellular
matrix
Fibers
• Collagen fiber
• Elastic fiber
• Reticular fiber
Ground substance
Copyright © 2010 Pearson Education, Inc.
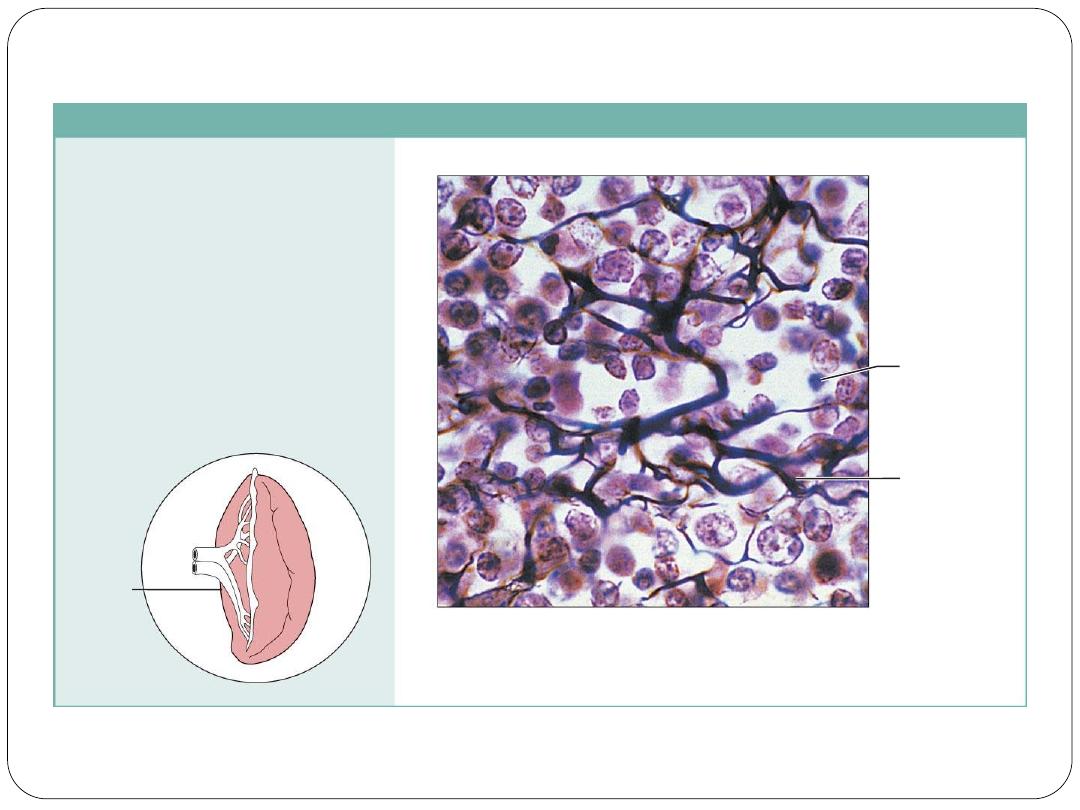
(c) Connective tissue proper: loose connective tissue, reticular
Description: Network of reticular
fibers in a typical loose ground
substance; reticular cells lie on the
network.
Function: Fibers form a soft internal
skeleton (stroma) that supports other
cell types including white blood cells,
mast cells, and macrophages.
Location: Lymphoid organs (lymph
nodes, bone marrow, and spleen).
Photomicrograph: Dark-staining network of reticular
connective tissue fibers forming the internal skeleton
of the spleen (350x).
Spleen
White blood
cell
(lymphocyte)
Reticular
fibers
Spleen – section – silver – 10x objective
Reticular tissue consists of very small collagenous fibers. They are visualized as
brownish-black fibers with the silver stain.
Reticular connective tissue
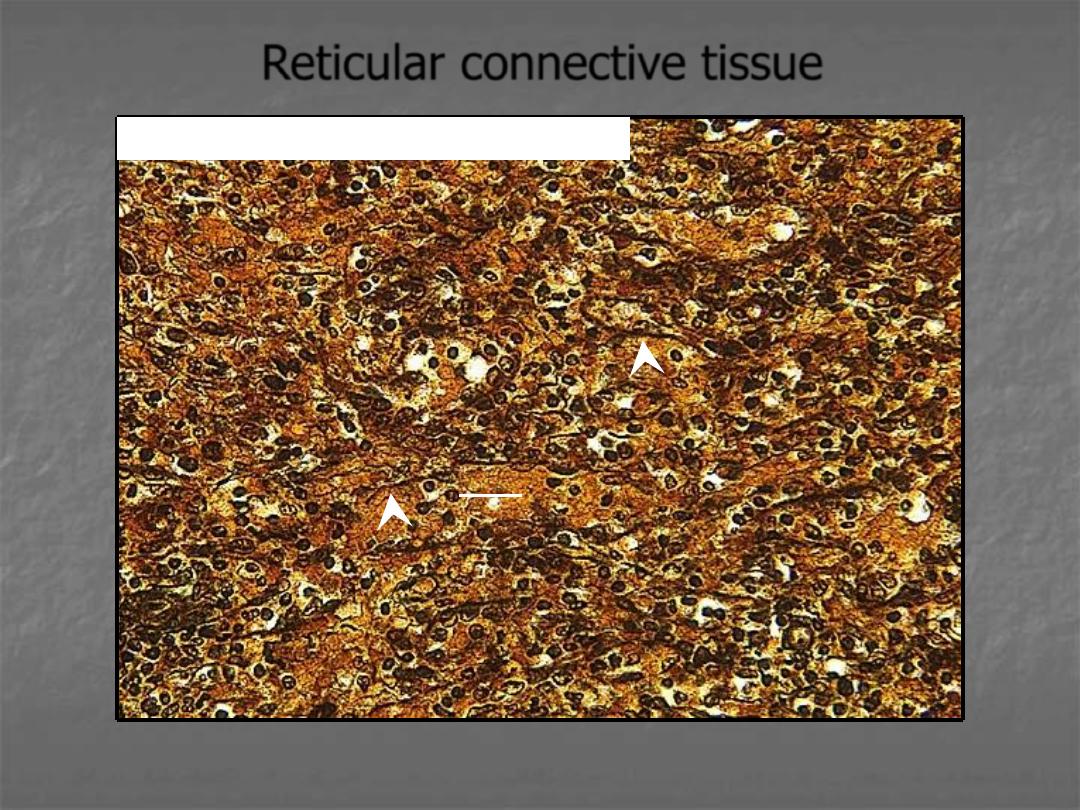
Arrowheads point out reticular fibers. The rounded nuclei are of lymphocytes
residing in the organ.
lymphocyte
Spleen – section – silver – 40x objective
Reticular connective tissue
Copyright © 2010 Pearson Education, Inc.
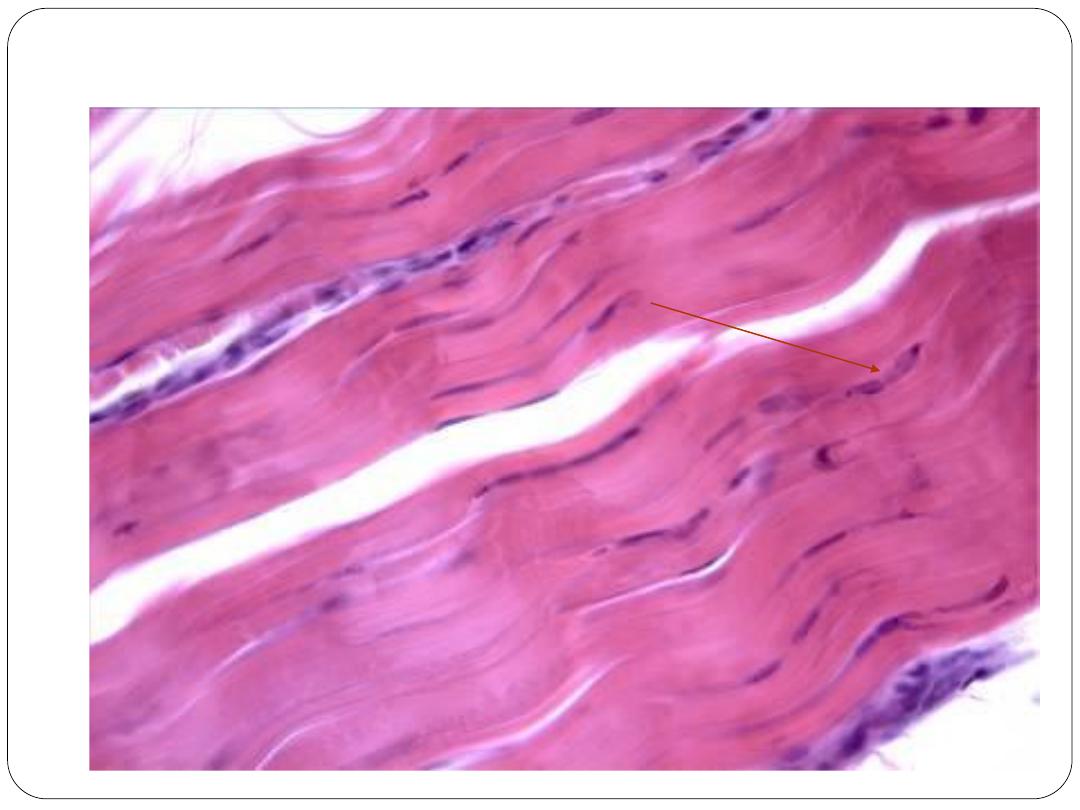
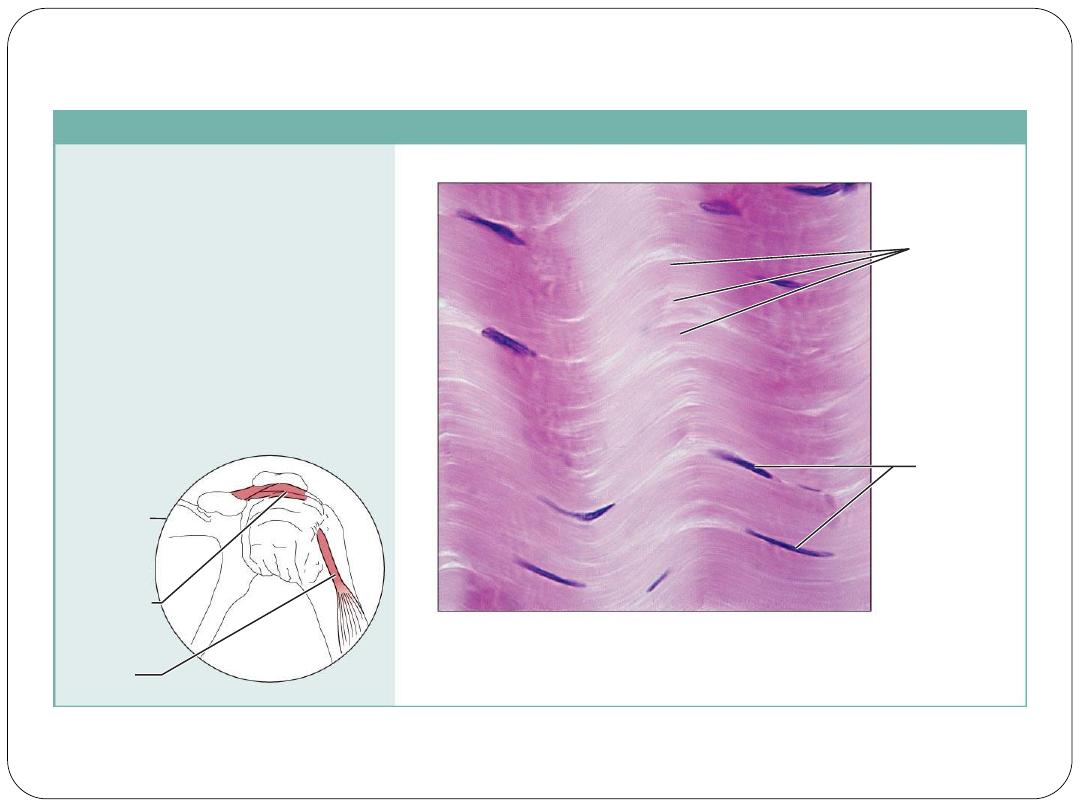
(d) Connective tissue proper: dense connective tissue, dense regular
Description: Primarily parallel
collagen fibers; a few elastic fibers;
major cell type is the fibroblast.
Function: Attaches muscles to
bones or to muscles; attaches bones
to bones; withstands great tensile
stress when pulling force is applied
in one direction.
Location: Tendons, most
ligaments, aponeuroses.
Photomicrograph: Dense regular connective
tissue from a tendon (500x).
Shoulder
joint
Ligament
Tendon
Collagen
fibers
Nuclei of
fibroblasts
Copyright © 2010 Pearson Education, Inc.
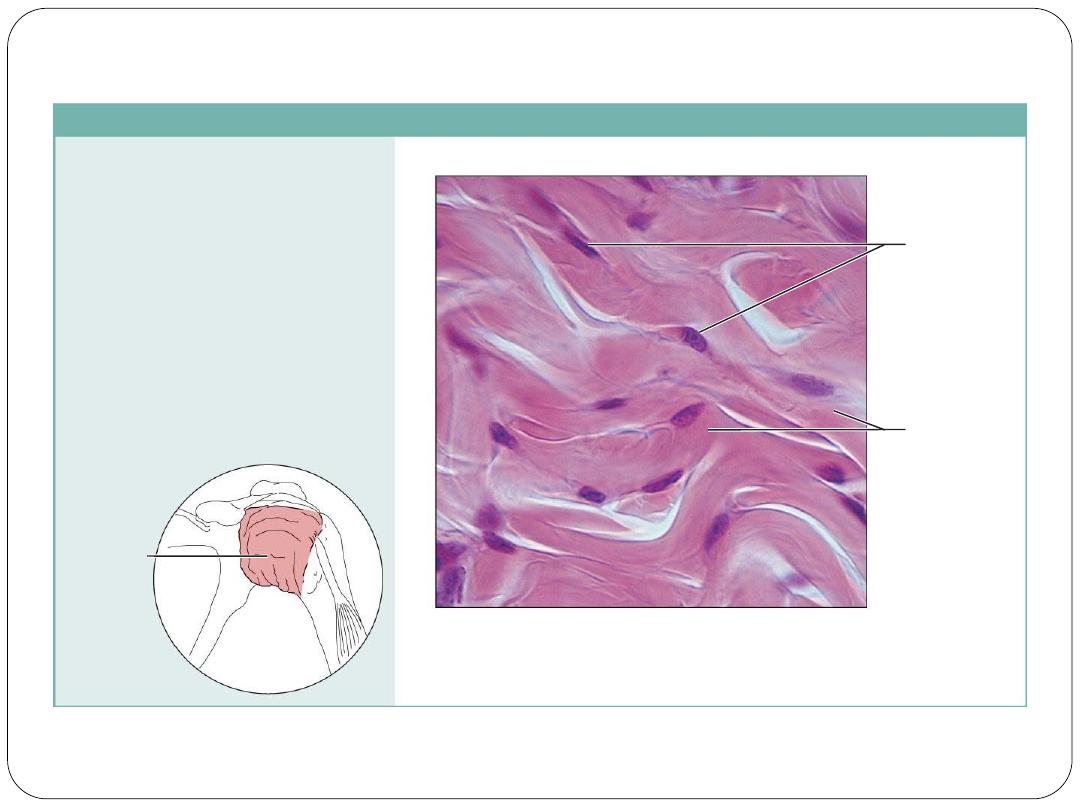
(e) Connective tissue proper: dense connective tissue, dense irregular
Description: Primarily
irregularly arranged collagen
fibers; some elastic fibers;
major cell type is the fibroblast.
Function: Able to withstand
tension exerted in many
directions; provides structural
strength.
Location: Fibrous capsules of
organs and of joints; dermis of
the skin; submucosa of
digestive tract.
Photomicrograph: Dense irregular
connective tissue from the dermis of the
skin (400x).
Collagen
fibers
Nuclei of
fibroblasts
Fibrous
joint
capsule
Copyright © 2010 Pearson Education, Inc.
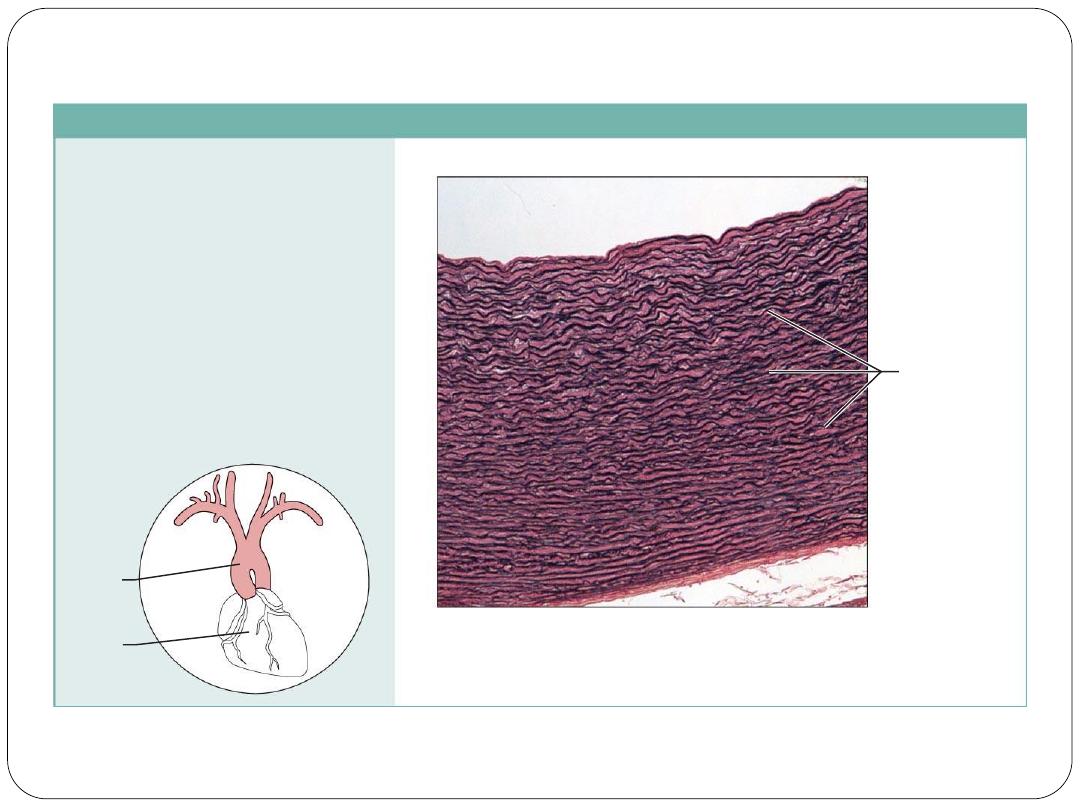
(f) Connective tissue proper: dense connective tissue, elastic
Description: Dense regular
connective tissue containing a high
proportion of elastic fibers.
Function: Allows recoil of tissue
following stretching; maintains
pulsatile flow of blood through
arteries; aids passive recoil of lungs
following inspiration.
Location: Walls of large arteries;
within certain ligaments associated
with the vertebral column; within the
walls of the bronchial tubes.
Elastic fibers
Aorta
Heart
Photomicrograph: Elastic connective tissue in
the wall of the aorta (250x).
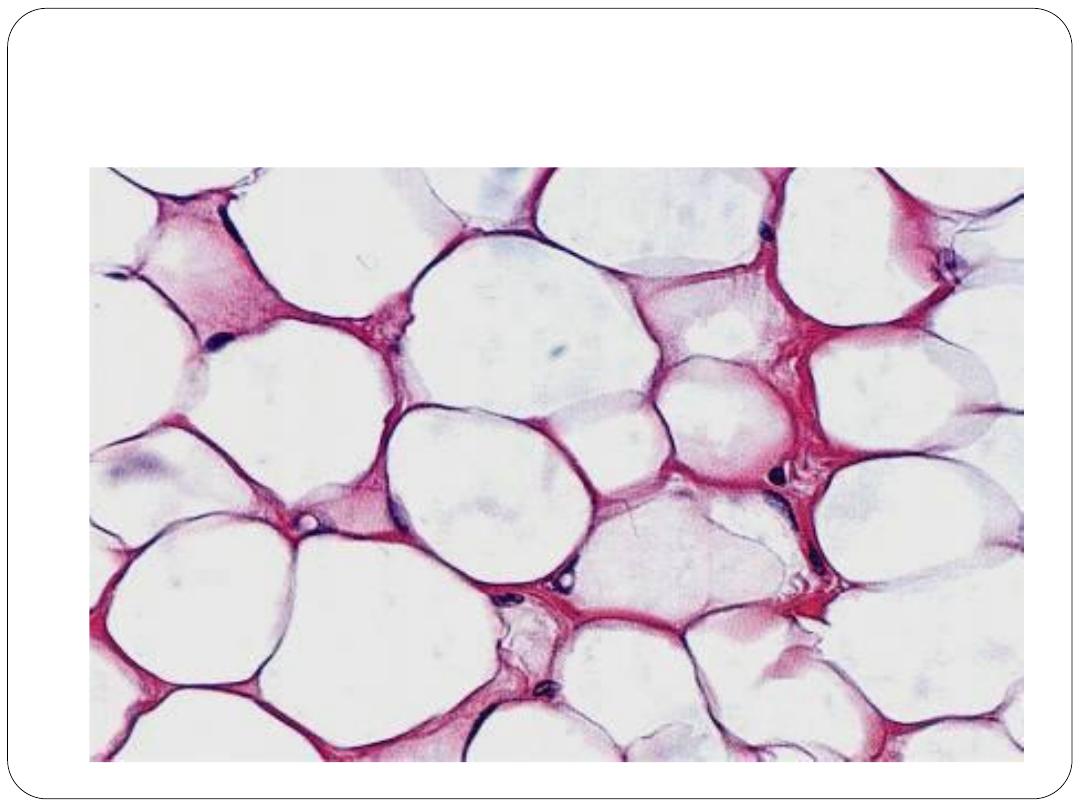
Adipose tissue
Most supporting tissues contain cells which are adapted
for the storage of fat; these cells, called adipocytes, are
derived from primitive mesenchyme where they develop
as lipoblasts.
Adipocytes are found in isolation or in clumps
throughout loose supporting tissues or may constitute the
main cell type as in adipose tissue.
Stored fat within adipocytes is derived from three main
sources: dietary fat circulating in the bloodstream as
chylomicrons; triglycerides synthesised in the liver and
transported in blood; and triglycerides synthesised from
glucose within adipocytes
Adipose tissue is often regarded as an inactive
energy store, however it is an extremely important
participant in general metabolic processes in that it
acts as a temporary store of substrate for the
energy deriving processes of almost all tissues.
Adipose tissue, therefore, generally has a rich
blood supply. The rate of fat deposition and
utilisation within adipose tissue is largely
determined by dietary intake and energy
expenditure, but a number of hormones and the
sympathetic nervous system profoundly influence
the fat metabolism of adipocytes
In addition to their energy storage role adipocytes
have an important endocrine role. Through
secretion of several proteins adipocytes modulate
energy
metabolism
and
influence
general
metabolism in coordination with hormones such as
insulin to regulate body mass. Adipose tissue is
responsible for the secretion of several proteins,
collectively known as adipocytokines. These
include leptin, adipsin, resistin, adiponectin, tumor
necrosis factor alpha, and plasminogenactivator
inhibitor type 1
Two main types of adipose tissue
White adipose tissue.
This type of adipose tissue
comprises up to 20% of total body weight in normal,
well nourished male adults and up to 25% in females.
It is distributed throughout the body particularly in the
deep layers of the skin.
In addition to being an important energy store, white
adipose tissue acts as a thermal insulator under the skin
and functions as a cushion against mechanical shock in
such sites as around the kidneys.
Brown adipose tissue.
This highly
specialized type of adipose tissue is found in
newborn mammals and some hibernating
animals, where it plays an important part in
body temperature regulation.
Only small amounts of brown adipose tissue
are found in human adults
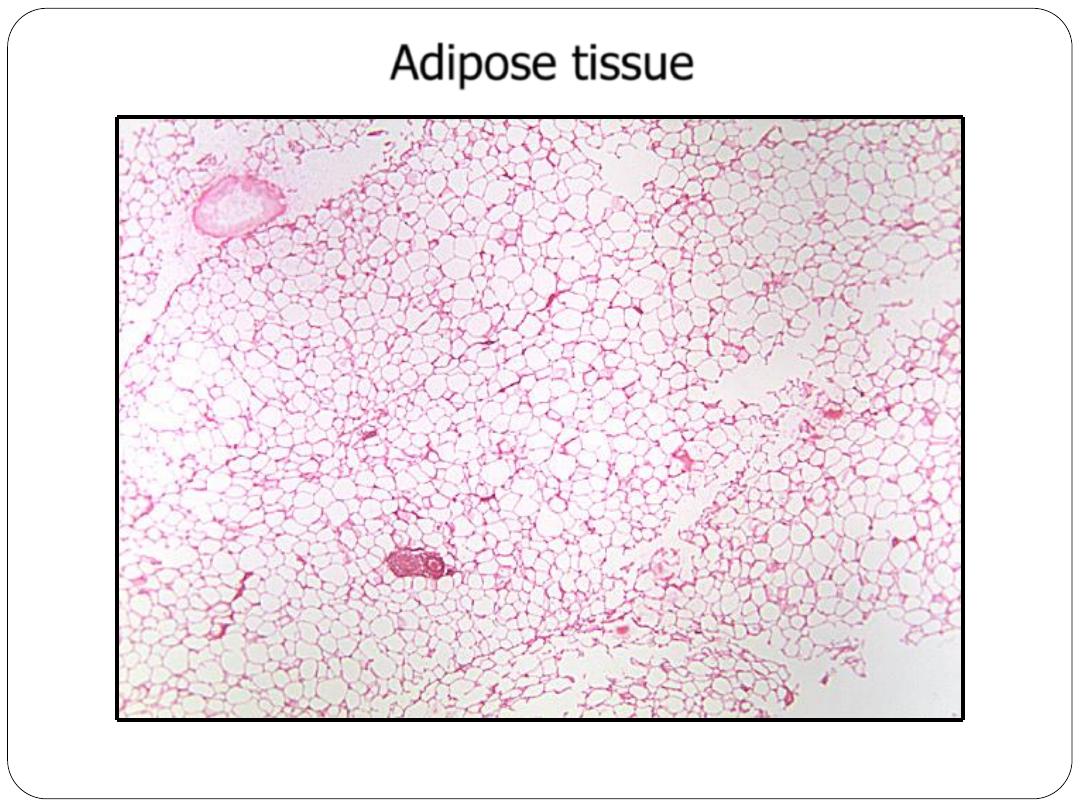
Adipose tissue – section – H&E – 4x objective
This honey-combed appearance is characteristic of adipose tissue.
Adipose tissue
