بسم ه الرحمن الرحيم
Reproductive system(male)
introduction
• The reproductive functions of the male can be
divided into three major subdivisions:
• (1)
spermatogenesis
, which means simply the
formation of sperm;
• (2) performance of the
male sexual act
; and
• (3)
regulation
of male reproductive functions by
the various
hormones
.
• Associated with these
reproductive functions
are
the effects of the male sex hormones on the
accessory sexual organs
,
cellular metabolism
,
growth
, and other functions of the body.
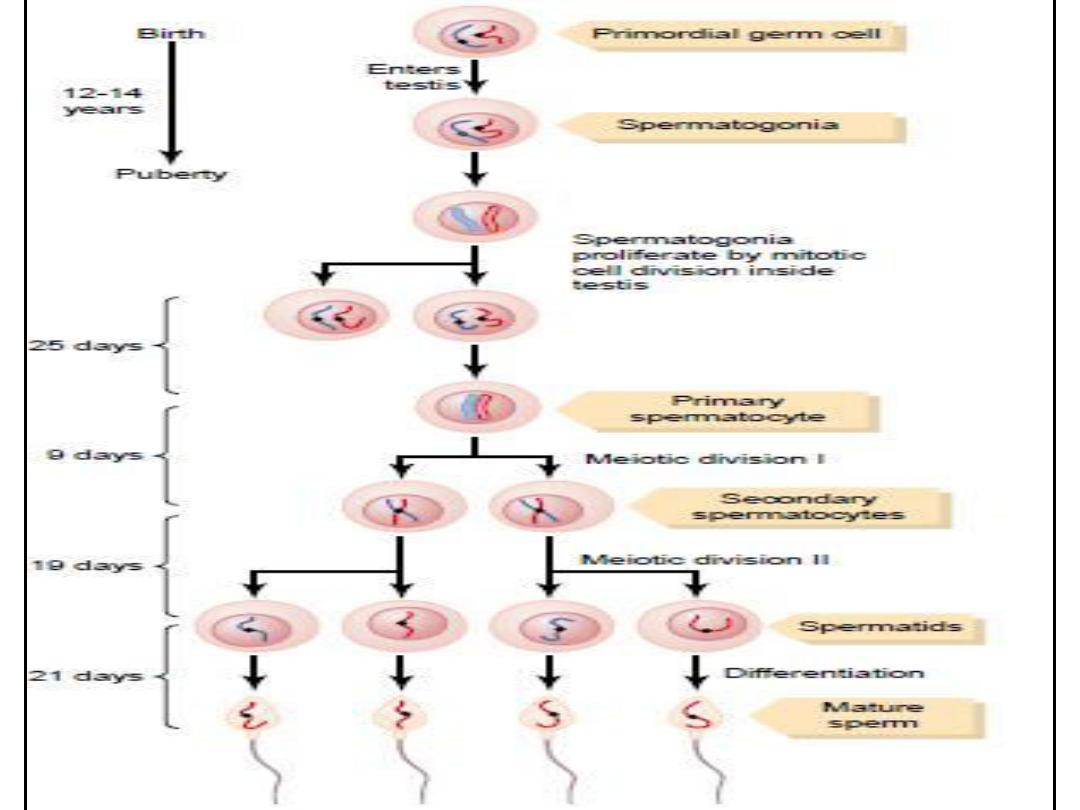
Spermatogenesis
• During formation of the embryo, the
primordial germ
cells migrate into the testes
and become immature germ cells called
spermatogonia
which lie in two or three layers
of the inner surfaces of the seminiferous
tubules ( Figure ).
• The spermatogonia begin to undergo
mitotic
division
, beginning at
puberty
, & continually
proliferate & differentiate through definite
stages of development to form sperm(Figure ).
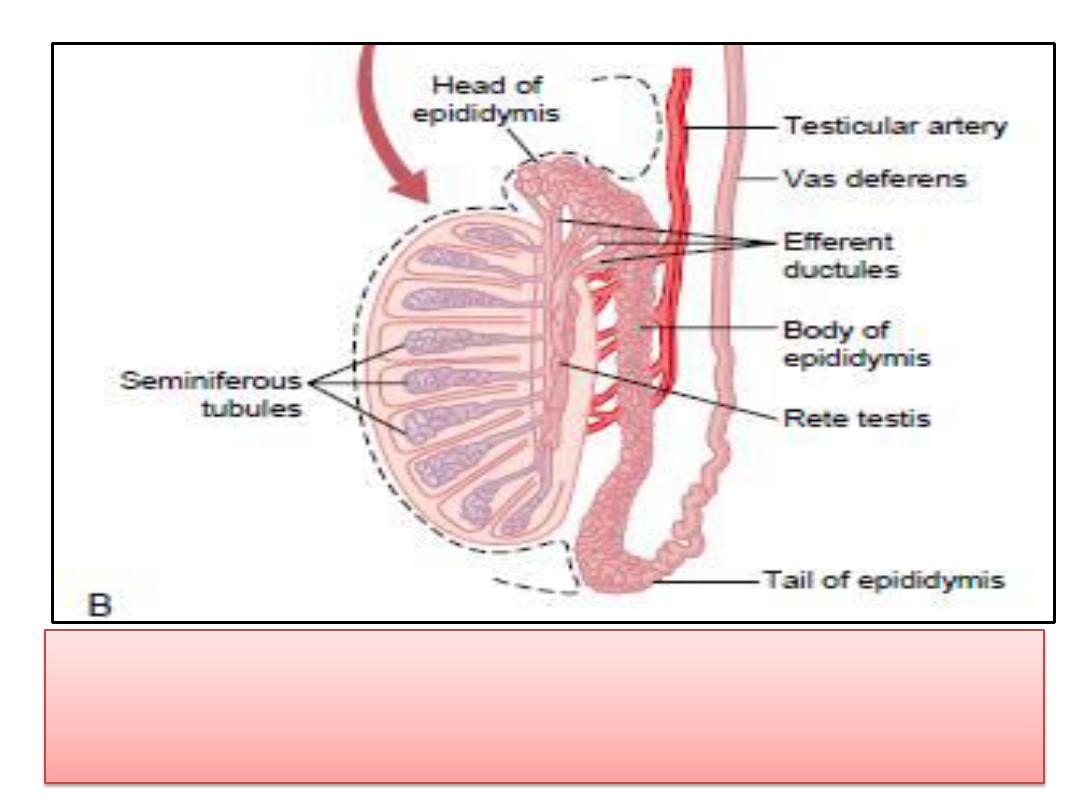
Internal structure of the testis and relation of the
testis to the epididymis
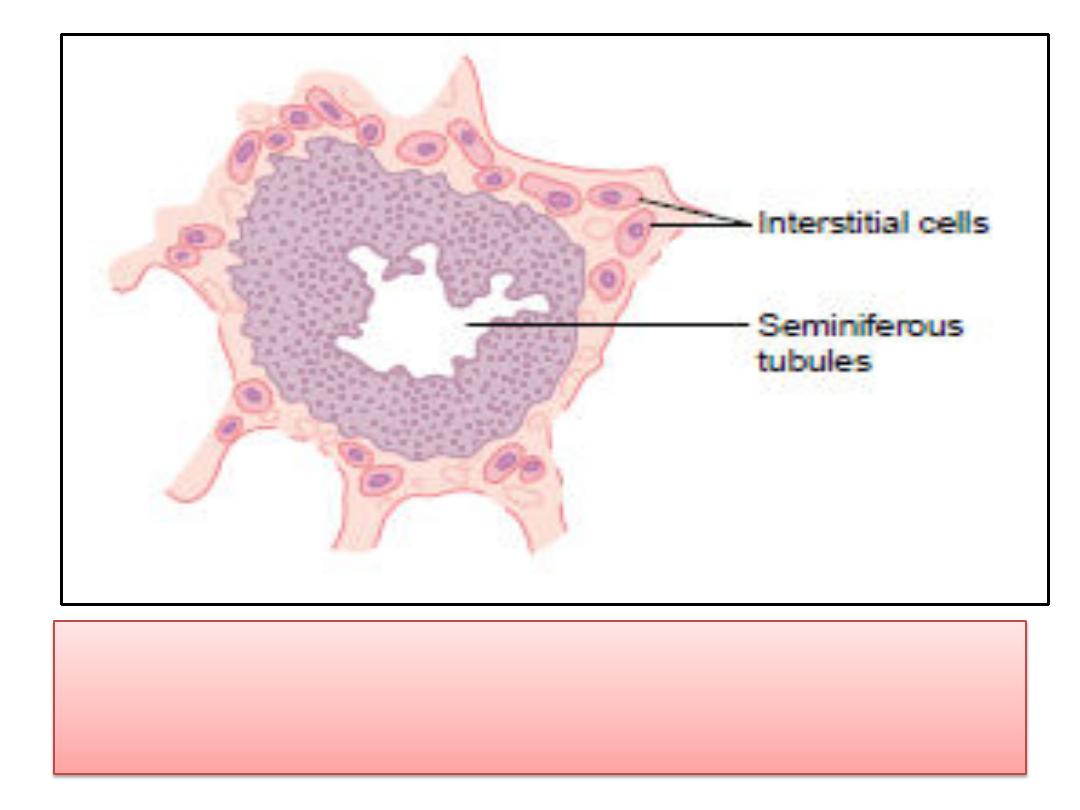
Cross section of a seminiferous tubule.
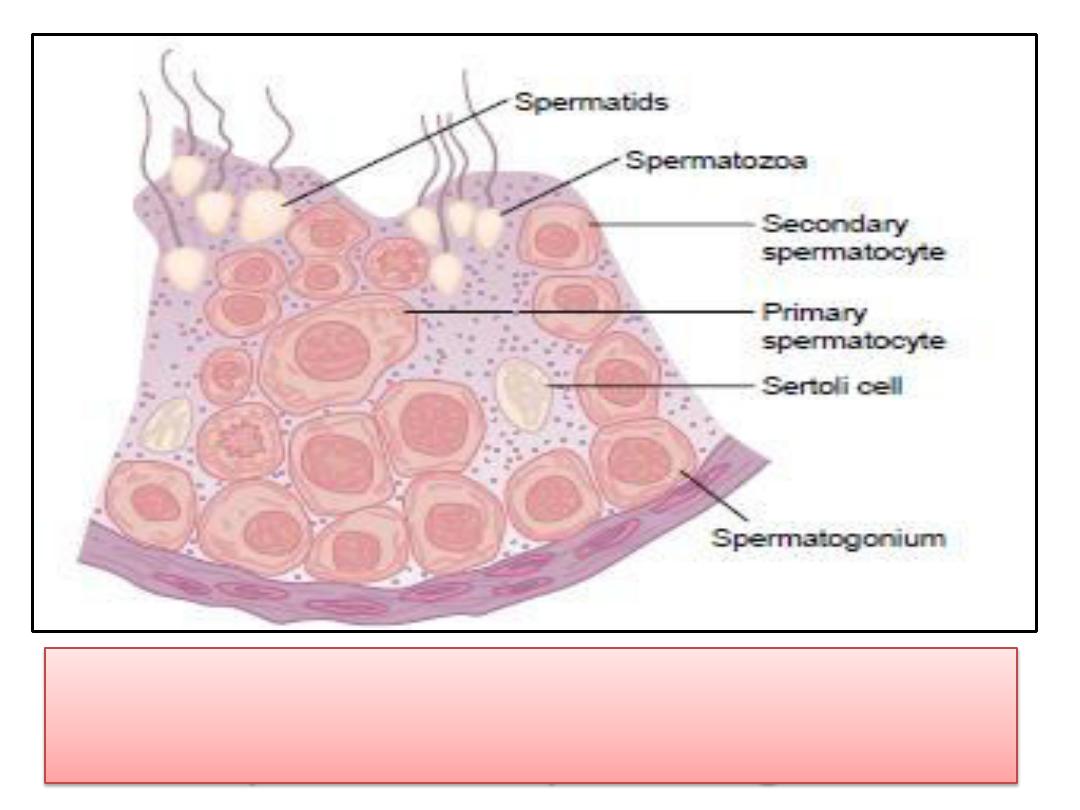
Stages in the development
of sperm from spermatogonia.

Sex Chromosomes
• In each
spermatogonium
, one of the
23 pairs
of
chromosomes carries the genetic information
that
determines the sex
of each eventual off
spring.
• This pair is composed of
one X chromosome
,
which is called the
female chromosome
, and
one
Y chromosome
, the
male chromosome
.
• During
meiotic division
, the male
Y chromosome
goes to one spermatid that then becomes a
male
sperm
, and the female
X chromosome
goes to
another spermatid that becomes
a female sperm
.
• The sex of the eventual offspring is determined by
which of these two types of sperm fertilizes the
ovum.
• At
puberty
(usually 12 to14 years after birth),
the spermatogonia proliferate rapidly by
mitosis
.
• Some begin meiosis to become
primary
spermatocytes
and continue through meiotic
division I to become
secondary
spermatocytes
.
• After completion of meiotic division II, the
secondary spermatocytes produce
spermatids
, which differentiate to form
spermatozoa.

Hormonal Factors That Stimulate
Spermatogenesis
• several hormones play essential roles in
spermatogenesis. Some of these are as
follows:
• 1.
Testosterone
, secreted by the Leydig cells
located in the interstitium of the testis, is
essential forgrowth and division of the
testicular germinalcells, which is the first stage
in forming sperm.
• 2.
Luteinizing hormone
, secreted by the
anterior pituitary gland, stimulates the
Leydig
cells
to secrete
testosterone
.

Hormonal Factors That Stimulate
Spermatogenesis
3
. Follicle-stimulating hormone
, also secreted by the
anterior pituitary gland, stimulates the
Sertoli cells
;
without this stimulation, the conversion of the
spermatids to sperm (the process of spermiogenesis)
will not occur.
4.
Estrogens
, formed from testosterone by the Sertoli cells
when they are stimulated by follicles timulating
hormone, are probably also essential for
spermiogenesis.
5.
Growth hormone
specifically promotes early division
of the spermatogonia themselves; in its absence, as in
pituitary dwarfs, spermatogenesis is severely deficient
or absent, thus causing
infertility
.
semen
• Semen, is composed of the
fluid and sperm
from the
vasdeferens
,
fluid from the
seminal vesicles
, fluid from the prostate gland , and
small amounts from the
mucous glands
, especially the
bulbourethral glands.
• Thus, the bulk of the semen is seminal vesicle fluid, which is the
last to be ejaculated and serves to wash the sperm through the
ejaculatory duct and urethra.
• The average
pH
of the combined semen is about
7.5
, the alkaline
prostatic fluid having more than neutralized the mild acidity of the
other portions of the semen.
• The
prostatic
fluid gives the semen
a milky
appearance, and fluid
from the
seminal vesicles
and mucous glands gives the semen
a
mucoid
consistency
• Also,
a clotting enzyme
from the prostatic fluid causes the
fibrinogen of the seminal vesicle fluid to form
a weak fibrin
coagulum
that
holds the semen
in the deeper regions of the vagina
where the uterine cervix lies.
• The coagulum then dissolves during the next 15 to 30 minutes
because of lysis by fibrinolysin formed from the prostatic
profibrinolysin.
semen
• In the early minutes after ejaculation, the sperm
remain relatively immobile, possibly because of
the
viscosity of the coagulum
.
• As the coagulum dissolves, the sperm
simultaneously become highly motile.
• Although sperm can live for
many weeks
in the
male genital ducts, once they are ejaculated in
the semen, their
maximal life span
is only
24 to
48 hours
at body temperature.
• At lowered temperatures, however, semen can be
stored for
several weeks
, and when frozen at
temperatures below
-100°C
, sperm have been
preserved for years.

Secretion of Testosterone by the Interstitial Cells of
Leydig in the Testes
• The testes secrete several male sex hormones,
which are collectively called
androgens
, including
testosterone
,
dihydrotestosterone
, and
androstenedione
.
• Testosterone is so much
more abundant
than the
others that one can consider it to be the
significant testicular hormone, although ,much, if
not most, of the testosterone is eventually
converted into the more active hormone
dihydrotestosterone
in the target tissues.
• Testosterone is formed by the interstitial cells of
Leydig
, which lie in the interstices between the
seminiferous tubules
• Effect of Testosterone on Development of Adult
Primary and Secondary Sexual Characteristics
• Effect on the Distribution of Body Hair(Baldness)
• Effect on the Voice.
• Testosterone Increases Thickness of the Skin and Can
Contribute to Development of Acne.
• Testosterone Increases Protein Formation and Muscle
Development.
• Testosterone Increases Bone Matrix and Causes
Calcium Retention.
• Testosterone Increases Basal Metabolism
• Effect on Red Blood Cells.
• Effect on Electrolyte and Water Balance.
Function of the testesteron
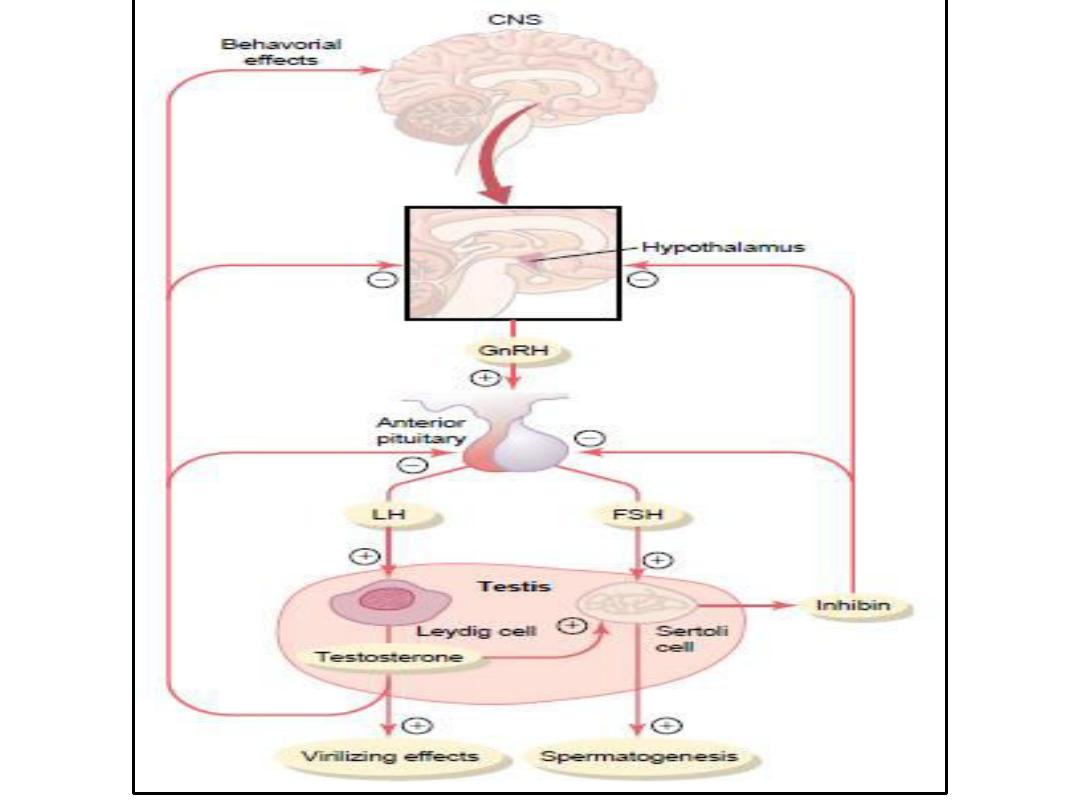
Control of Male Sexual Functions by Hormones from the
Hypothalamus and Anterior Pituitary Gland
• A major share of the control of sexual functions in both
the male and the female begins with secretion
• of
gonadotropin-releasing hormone
(GnRH) by the
hypothalamus .
• This hormone in turn stimulates the
anterior pituitary
gland to secrete two other hormones called
gonadotropic hormones
:
(1) luteinizing hormone (LH) and
(2) follicle-stimulatinghormone (FSH).
• In turn,
LH
is the primary stimulus for the secretion of
testosterone by the testes, and
FSH
mainly stimulates
spermatogenesis.
Thank you
