Resistance of
the Body to Infection
Leukocytes
Granulocytes
the Monocyte-macrophage System
and Inflammation
•
Our bodies are
exposed
continually to bacteria, viruses, fungi, and parasites, all of which
occur normally and to varying degrees
in the
skin, mouth, respiratory passage ways,
intestinal tract, lining membranes of the eyes, and even the urinary tract.
•
blood leukocytes (white blood cells) and tissue cells derived from leukocytes
work
together
in two ways to prevent disease:
(1) by actually
destroying
invading bacteria or viruses by
phagocytosis
,
(2) by
forming
antibodies
and
sensitized
lymphocytes,
one or both of which may destroy or
inactivate the invader.
Leukocytes (White Blood Cells)
They are
formed
partially in the
bone
marrow
(
granulocytes
and
monocytes
and a few
lymphocytes
) and partially in the
lymph
tissue
(
lymphocytes
and
plasma cells
).
After formation, they are
transported
in the blood to different parts of the body where they
are needed and to areas of serious infection and inflammation.
General Characteristic of leukosytes
A- Types of White Blood Cells.
Six
types
of white blood cells are normally present in the blood. They are
polymorphonuclear
neutrophils
, polymorphonuclear
eosinophils
, polymorphonuclear
basophils
,
monocytes
,
lymphocytes
,
and, occasionally ,
plasma
cells.
In addition, there are large numbers of
platelets
,
which are fragments of another type of cell similar to the white blood cells found in
the bone marrow, the
megakaryocyte.
The first three types of cells, the polymorphonuclear
cells, all have a
granular
appearance, ―
polys
,‖ because of the multiple nuclei.
The
granulocytes
and
monocytes
protect the body against invading organisms mainly by
ingesting them by
phagocytosis
.
The
lymphocytes
and
plasma
cells
function mainly in
connection with the
immune
system
; Finally, the function of
platelets
is specifically to
activate the blood clotting mechanism.

B- Concentrations of the Different White Blood Cells in the Blood.
•
The adult human being
has
about
4000-10000
white blood cells per
microliter
of blood (in
comparison with 5 million red blood cells).
•
neutrophils ~ 60 %
•
Lymphocytes 30 %
•
eosinophils 3 %
•
basophils 1 %
•
Monocytes 6 %
•
The number of platelets, which are only cell fragments, in each microliter of blood is
normally about
150,000-
400000
.
C- Genesis of the White Blood Cells
Formation
•
Aside from those cells committed to form red blood cells, two major lineages of
white blood
cells
are formed, the
myelocytic
and the
lymphocytic
lineages.
•
The
myelocytic lineage,
begins with the
myeloblast
;
the
lymphocytic lineage,
begin with the
lymphoblast
.
•
The granulocytes and monocytes are
formed
only in the
bone
marrow
. Lymphocytes and
plasma cells are produced mainly in the various
lymphogenous
tissues—especially the
lymph
glands,
spleen, thymus,
tonsils
, and various pockets of lymphoid tissue elsewhere in the
body, such as in the
bone
marrow
and in so-called
Peyer’s
patches underneath the epithelium
in the gut wall.
Storage
•
The
white
blood
cells
formed in the bone marrow are
stored
within the marrow until they are
needed in the circulatory system.
•
The
lymphocytes
are mostly
stored
in the various lymphoid tissues, except for a small
number that are temporarily being transported in the blood.
•
megakaryocytes
fragment in the bone marrow; the small fragments, known as
platelets
(or
thrombocytes
), then pass into the blood.

D- Life Span of the White Blood Cells
•
eThe
life
of the
granulocytes
after being released from the bone marrow is normally
4 to 8
hours
circulating in the blood and another
4 to 5 days
in tissues where they are needed.
•
The
monocytes
also have a short transit time,
10 to 20 hours
in the blood, before wandering
through the capillary membranes into the tissues. Once in the tissues, they swell to much
larger sizes to become
tissue macrophages
,
and, in this form, can live for
months
.
•
Lymphocytes
enter the circulatory system continually.
After
a
few
hours, they pass out of the
blood back into the tissues. The lymphocytes have life spans of
weeks
or
months
.
•
The
platelets
in the blood are replaced about once very
10
days
.
E- Neutrophils and Macrophages Defend Against Infections
•
T
he
neutrophils
are
mature cells that can attack and
destroy
bacteria even in the circulating
blood.
•
Conversely, the
tissue macrophages
begin
life as blood monocytes, which are immature cells
while still in the blood and have little ability to fight infectious agents at that time. However,
once they
enter
the tissues, they begin to
swell—sometimes
increasing their diameters as
much as fivefold.
F- White Blood Cells Enter the Tissue Spaces by Diapedesis
•
Neutrophils and monocytes can
squeeze
through the pores of the blood capillaries by
diapedesis.
That is, even though a pore is much
smaller
than a cell, a small portion of the cell
slides
through the pore at a time.
•
Both neutrophils and macrophages Move Through Tissue Spaces by Ameboid Motion.
•
Some cells move at velocities as great as 40 mm/min.
G- White Blood Cells Are Attracted to Inflamed Tissue Areas by Chemotaxis
•
Many
different
chemical substances in the tissues
cause
both neutrophils and macrophages to
move toward the source of the chemical. This phenomenon is known as
chemotaxis
.
•
They include:
(1) Some of the bacterial or viral
toxins
,
(2)
degenerative
products of the inflamed tissues themselves,
(3) several reaction products of the ―
complement
complex‖ activated in inflamed tissues,
and
(4) several reaction products caused by plasma
clotting
in the inflamed area,

Phagocytosis
•
means cellular
ingestion
of the offending agent by neutrophils and macrophages. Phagocytes
must be selective
of the material that is phagocytized; otherwise, normal cells and structures
of the body might be ingested. Whether
phagocytosis
will occur depends especially on three
selective
procedures
.
•
First
, most
natural
structures in the tissues have
smooth
surfaces
, which resist phagocytosis.
•
Second
, most natural substances of the body have
protective
protein
coats that repel the
phagocytes.
•
Third
, the immune system of the body develops
antibodies
against infectious agents such as
bacteria. The antibodies then
adhere
to the bacterial membranes and thereby make the
bacteria especially susceptible to phagocytosis. To do this, the antibody molecule
also
combines
with the
C3
product of the
complement cascade,
which is an additional part of the
immune system. The C3 molecules, in turn,
attach
to receptors on the phagocyte membrane,
thus initiating phagocytosis. This selection and phagocytosis process is called
opsonization
.
•
Phagocytosis
by
Neutrophils
.
the neutrophil
first
attaches
itself to the particle and then
projects
pseudopodia
in all directions around the particle. The pseudopodia meet one another
on the opposite side and fuse. This creates an
enclosed chamber
that contains the
phagocytized particle.
•
Then the chamber
invaginates
to the inside of the cytoplasmic cavity and
breaks
away from
the outer cell membrane to form a free-floating
phagocytic
vesicle
(also called a
phagosome
)
inside the cytoplasm.
•
Phagocytosis
by
Macrophages
.
When activated by the immune system they are much more
powerful
phagocytes than neutrophils,
Once Phagocytized, Most Particles Are Digested by Intracellular Enzymes.
•
lysosomes
and other cytoplasmic granules in the neutrophil or macrophage come in
contact
with the phagocytic vesicle, and their
membranes
fuse
,
thereby dumping many digestive
enzymes and bactericidal agents into the vesicle. Thus, the phagocytic vesicle now becomes
a
digestive
vesicle
,
•
The
lysosomes
of
macrophages
(but not of neutrophils) also contain large amounts of
lipases
,
which digest the thick lipid membranes possessed by some bacteria such as the tuberculosis
bacillus.
Both Neutrophils and Macrophages Can Kill Bacteria.
•
Much of the killing
effect
results
from several powerful
oxidizing
agents.
These oxidizing
agents include large quantities of
superoxide
(
O2
–),
hydrogen peroxide
(
H2O2
), and
hydroxyl ions
(–
OH
–), all of which are lethal to most bacteria, even in small quantities. Also,
one of the lysosomal enzymes,
myeloperoxidase
, catalyzes the reaction between H2O2 and
chloride ions to form
hypochlorite
, which is exceedingly bactericidal.
Monocyte-Macrophage Cell System (Reticuloendothelial System)
After entering the tissues and becoming macrophages,
another
large portion of monocytes
becomes
attached
to the tissues and remains attached for
months
or
even
years
until they are
called on to perform specific local protective functions.
They have the
same
capabilities as the mobile macrophages to
phagocytize
large quantities of
bacteria, viruses, necrotic tissue, or other foreign particles in the tissue. And, when
appropriately
stimulated
, they can
break
away
from their attachments and once again
become
mobile
macrophages that respond to chemotaxis and all the other stimuli related to the
inflammatory process.
Thus, the body has a widespread ―
monocyte-macrophage
system
‖ in virtually all tissue areas.
The total
combination of
monocytes
,
mobile
macrophages,
fixed
tissue macrophages, and a
few specialized
endothelial
cells in the bone marrow, spleen, and lymph nodes is
called
the
reticuloendothelial system.
1. Tissue Macrophages in the Skin and Subcutaneous Tissues (Histiocytes).
when the skin is broken infection begins in a subcutaneous tissue and local inflammation
ensues, local tissue
macrophages
can
divide
in situ and form more macrophages. Then they
perform the usual functions.
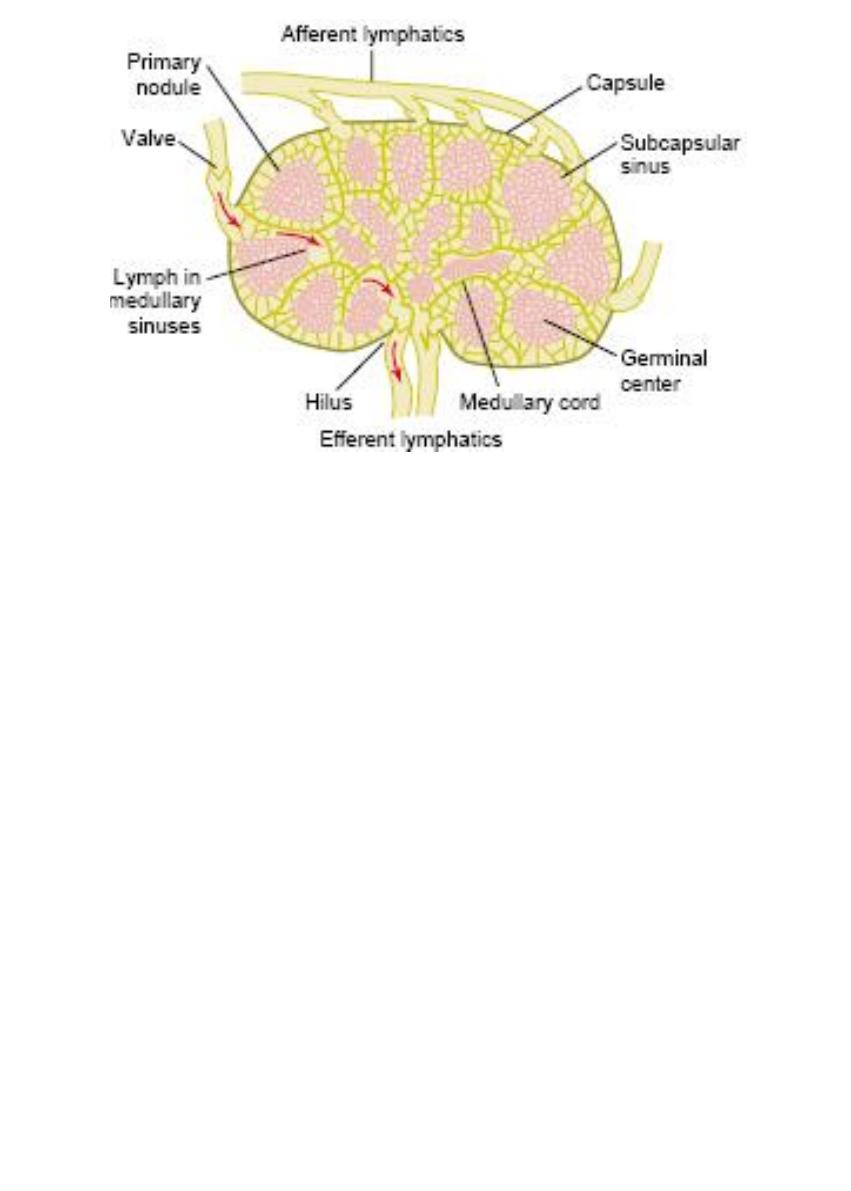
2. Macrophages in the Lymph Nodes.
Essentially
no
particulate matter that enters the tissues, such as
bacteria
, can be
absorbed
directly through the capillary membranes into the blood. Instead, if the particles are not
destroyed locally in the tissues, they
enter
the lymph and flow to the lymph nodes
located
intermittently along the course of the lymph flow. The foreign particles are then
trapped
in
these nodes in a meshwork of
sinuses lined
by
tissue macrophages.
3. Alveolar Macrophages in the Lungs.
If the particle is
not
digestible
, the macrophages often form a ―
giant
cell
‖
capsule
around the
particle until it can be slowly dissolved. Such capsules are frequently
formed
around tuberculosis
bacilli
,
silica dust particles
,
and even carbon particles.
4. Macrophages (Kupffer Cells) in the Liver Sinusoids.
These cells form such an effective
filtration
system
that almost none of the bacteria from the
gastrointestinal
tract succeeds in passing from the
portal
blood into the general
systemic
circulation.
5. Macrophages of the Spleen and Bone Marrow.
The spleen is
similar
to the lymph nodes, except that blood, instead of lymph, flows through the
tissue spaces of the spleen.
a small
artery
penetrates from the splenic capsule into the
splenic pulp
and
terminates
in small
capillaries
. The capillaries are highly
porous
, allowing whole blood to pass out of the capillaries
into
cords
of red pulp.
The blood then gradually
squeezes
through the
trabecular
meshwork
of
these cords and eventually returns to the circulation through the endothelial walls of the
venous
sinuses
.
The
trabeculae
of the red pulp are
lined
with vast numbers of macrophages, and the
venous
sinuses
are also lined with macrophages.
phagocytizing
unwanted debris in the blood, including especially
old and abnormal
red blood
cells.

Inflammtion Role of Neutrophils and Macrophages
When tissue
injury
occurs, whether caused by bacteria, trauma, chemicals, heat, or any
other phenomenon,
multiple
substances are
released
by the injured tissues and cause
dramatic
secondary
changes
in the surrounding uninjured tissues. This entire complex of
tissue changes is
called
inflammation
.
Inflammation is characterized by
(1)
vasodilation
of the local blood vessels, with consequent excess local blood flow;
(2) increased
permeability
of the capillaries, allowing
leakage
of large quantities of fluid into the
interstitial spaces;
(3) often
clotting
of the fluid in the interstitial spaces because of excessive amounts of
fibrinogen
and other proteins leaking from the capillaries;
(4)
migration
of large numbers of granulocytes and monocytes into the tissue;
(5)
swelling
of the tissue cells.
Some of the many tissue
products
that
cause
these reactions are
histamine
,
bradykinin
,
serotonin
,
prostaglandins
,
several different
reaction products of the
complement
system
,
reaction products of the blood
clotting
system
,
and multiple substances called
lymphokines
that are
released
by sensitized T cells.

“Walling-Off” Effect of Inflammation.
One of the first results of inflammation is to ―
wall
off
‖ the area of injury from the remaining
tissues. The
tissue spaces and the lymphatics
in the inflamed area are
blocked
by fibrinogen
clots. This walling-off process delays the spread of bacteria or toxic products.
1. Tissue Macrophage Is a First Line of Defense Against Infection.
When the macrophages activated by the products of infection and inflammation, the first
effect is rapid
enlargement
of each of these cells. Next, many of macrophages break loose
from their attachments and
become
mobile
.
2. Neutrophil Invasion of the Inflamed Area Is a Second Line of Defense.
the products from the inflamed tissues initiate the following reactions:
(1) They
alter
the inside surface of the capillary
endothelium
, causing neutronphils to stick to
thecapillary walls in the inflamed area. This effect is called
margination
.
(2) They cause the
intercellular
attachments
between the endothelial cells of the capillaries
andsmall venules to
loosen
, allowing
openings
large enough for neutrophils to pass by
diapedesis
.
(3) Then cause
chemotaxis
of the neutrophils toward the injured tissues.
The
products
of inflammation also
mobilize the stored
neutrophils of the marrow into the
circulating blood increasing its count to fourfold to fivefold this is called Neutrophilia
3. Second Macrophage Invasion into the Inflamed Tissue Is a Third Line of Defense.
Along with the invasion of neutrophils, monocytes from the blood
enter
the inflamed tissue
and
enlarge
to become macrophages.
4. Increased Production of Granulocytes and Monocytes by the Bone Marrow Is a Fourth
Line of Defense.
This results from
stimulation
of the granulocytic and monocytic progenitor cells of the
marrow.
Feedback Control of the Macrophage and Neutrophil Responses
(1)
tumor necrosis factor
(
TNF
),
(2)
interleukin-1
(
IL-1
),
(3)
granulocyte-monocyte colony-stimulating factor
(
GM-CSF
),
(4)
granulocyte colony-stimulating factor
(
G-CSF
),
(5)
monocyte colony-stimulating factor
(
M-CSF
).
These factors are
formed
by
activated macrophage
cells in the inflamed tissues and in smaller
quantities by other
inflamed tissue cells
.
Formation
of Pus
•
When neutrophils and macrophages engulf large numbers of bacteria and necrotic tissue,
eventually die
.
After several days, a
cavity
is often excavated in the inflamed tissues that
contains
varying
portions of
necrotic
tissue, dead
neutrophils
, dead
macrophages
, and tissue
fluid
.
This mixture is commonly known as
pus
.
After the infection has been suppressed, the dead cells and necrotic tissue in the pus
gradually
autolyze
over a period of
days
, and the end products are eventually absorbed into
the surrounding tissues and lymph
Eosinophils
1-
produced
in large numbers in people with
parasitic
infections
,
eosinophils
attach
themselves to the parasites by way of special surface molecules and
release
substances that kill many of the parasites.
e.g. a highly
larvacidal
polypeptide called
major
basic
protein
.
2- The
mast cells and basophils release
an
eosinophil
chemotactic
factor
that causes
eosinophils to
migrate
toward the inflamed
allergic
tissue
.
The eosinophils are believed to
detoxify
some of the inflammation-inducing substances
released by the mast cells and basophils and probably also to
phagocytize
and destroy
allergen-antibody complexes, thus preventing excess
spread
of the local inflammatory
process.
