Drugs for thyroid disorders
Thyroid glandThe thyroid secretes 2 types of hormones:
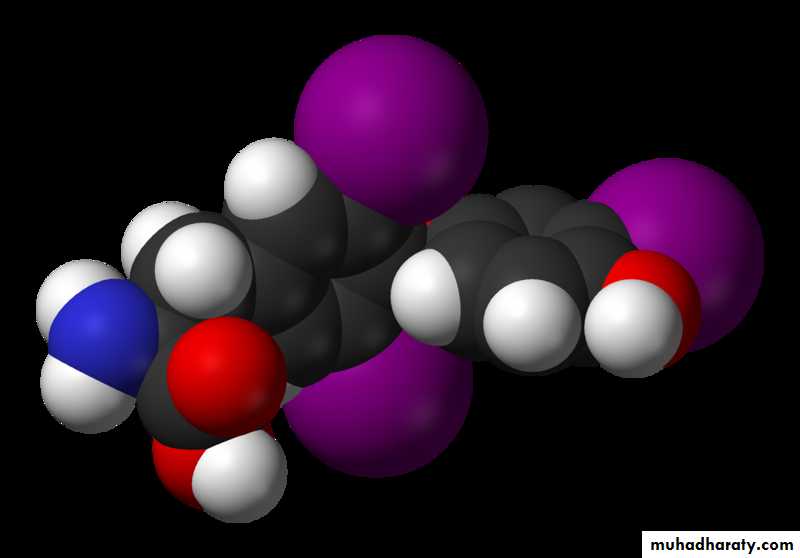
1- Iodine containing amino acids (are important for growth, development and metabolism) and these are: triiodothyronine, tetraiodothyronine
( thyroxine)
2- Calcitonin is important in the regulation of calcium level.
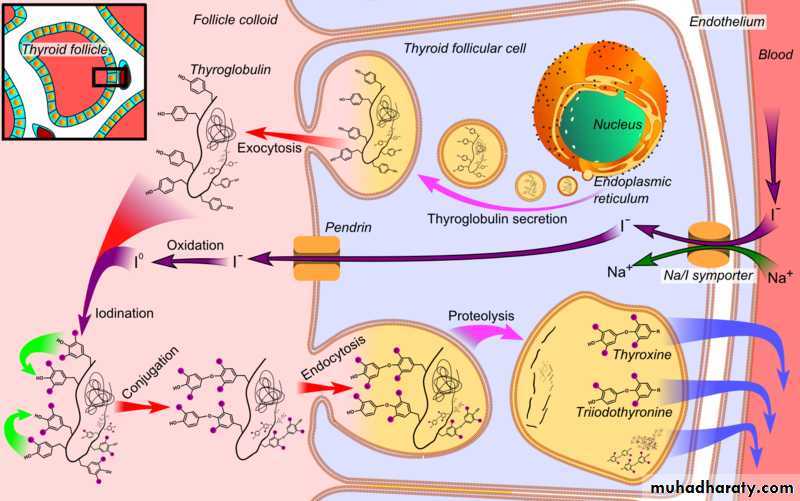
Thyroid hormones (TH) exists in two major forms:Levothyroxine (T4), with four iodine atoms per molecule, is an inactive form that can be converted into T3, and is produced exclusively by the thyroid gland.
Triiodothyronine (T3), with three iodine atoms per molecule, is eight times more effective than T4.
It is produced by conversion from T4, in the thyroid, brain, liver, bloodstream, and in various tissues of the body.
Triiodothyronine (T3)
Levothyroxine (T4)BIOSYNTHESIS, TRANSPORT & PERIPHERAL METABOLISM OFTHYROID HORMONES:
I. Thyroid hormone preparations for hypothyroidism:
1. Levothyroxine (T4):It is the drug of choice for most patients who require thyroid hormone replacement.
Pharmacokinetics:
Much of an administered dose of Levothyroxine is converted to T3 in the body.
The hormone has a prolonged half life (about 7 days)
Therapeutic uses:1. Levothyroxine is indicated for all forms of hypothyroidism, regardless of cause.
2. Levothyroxine is used to maintain proper levels of thyroid hormones following thyroid surgery, irradiation , & treatment with antithyroid drugs.
Adverse effects: 1. Thyrotoxicosis may result if the dosage is excessive. 2. Thyrotoxic crisis may occur if the dosage is especially large.
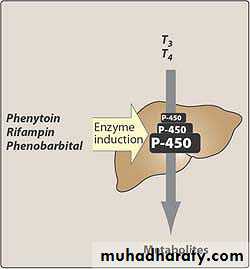
Drug interactions:
1. Drug that reduce Levothyroxine absorption:Cholestyramine, Colestipol, Calcium supplementation, Sucralfate, Aluminum –containing antacids, Iron.
2. Warfarine : Levothyroxine accelerates the degradation of vitamin K-dependant clotting factors.
3. Catecholamines: thyroid hormones increase cardiac responsiveness to catecholamines.
4. Levothyroxine can increase requirements for insulin & digitalis.Route of administration:
Levothyroxine is almost always administered by mouth.Oral dose should be taken on an empty stomach to enhance absorption.
Dosing is usually done in the morning before breakfast.IV administration is used for myxedama coma & for patients who cannot take Levothyroxine orally.
Duration of therapy:
For most hypothyroid patients, replacement therapy must be continued for life.Treatment provides symptomatic relief but does not produce cure.
Liothyronine (T3):Liothyronine is a synthetic preparation of T3. Liothyronine differs from levothyroxine in 3 important ways:
1. Liothyronine has a shorter half life & shorter duration of action.
2. Liothyronine has a more rapid onset of action.
3. Liothyronine is more expensive.These preparations make Liothyronine less desirable than levothyroxine for long-term use.
Liotrix:
Liotrix is a mixture of synthetic T4 plus synthetic T3 in a 4:1 fixed ratio ( this ratio is similar to the ratio of these hormones in plasma).Since levothyroxine alone produces the same ratio of T4 to T3, liotrix offers no advantages over levothyroxine for most indications.
Π. Drugs for hyperthyroidism:
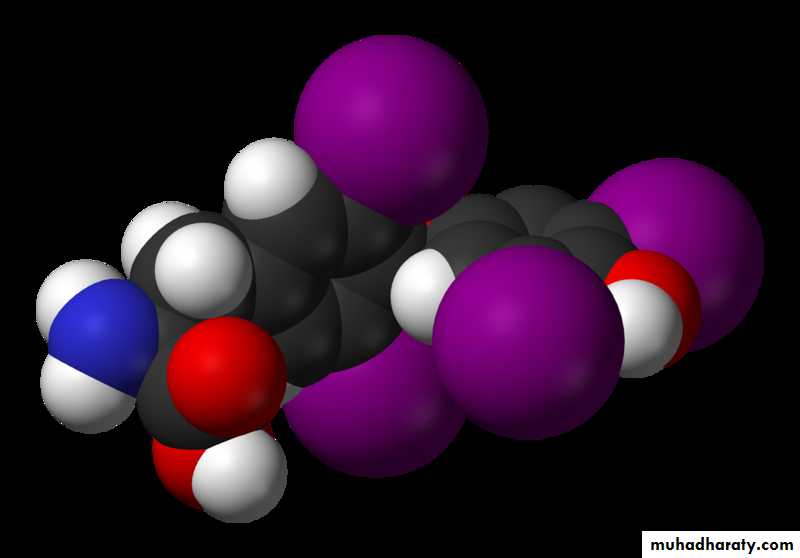
1. Propylthiouracil:Therapeutic response to PTU result primarily from blockade of thyroid hormone synthesis. Blockade occurs in two ways:
1. PTU prevents the oxidation of iodide, thereby inhibiting incorporation of iodine into tyrosine.
2. PTU prevents iodinated tyrosines from coupling. Both effects results from inhibiting peroxidase, the enzyme that catalyzes both reactions.
In addition, PTU acts in the periphery to suppress conversion of T4 to T3.
BIOSYNTHESIS, TRANSPORT & PERIPHERAL METABOLISM OFTHYROID HORMONES:
Pharmacokinetics:
PTU is rapidly absorbed following oral administration.Therapeutic actions begin within 30 minutes.
The plasma half life is short (about 2 hours).The drug can across the placenta & can enter breast milk.
Therapeutic uses:PTU has four applications in hyperthyroidism:
1. PTU can be used alone as the sole form of therapy for Graves diseases.
2. PTU can be employed as an adjunct to radiation therapy.
3. PTU can be given to suppress thyroid hormone synthesis in preparation for thyroid gland surgery.4. PTU is given to patients experiencing thyrotoxic crisis.
Adverse effects:1. Agranulocytosis.
2. Hypothyroidism.
3. Neonatal hypothyroidism & goiter.
4. Rash.
5. Nausea, arthralgia, headache, dizziness, & parasthesia.
2. Methimazole:
Methimazole is similar to PTU.
However, in contrast to PTU, Methimazole does not block conversion of T4 to T3 in the periphery.
It crosses the placenta more readily than PTU , therefore PTU is preferred.
3. Iodide products ( Non radioactive):A. Strong iodine solution (Lugol,s solution):
Lugol,s solution is a mixture containing 5% elemental iodine & 10% potassium iodide.
The iodine undergoes reduction to iodide within the GIT prior to absorption.
Mechanism of action:When present in high concentration, iodide has a paradoxical suppressant effect on the thyroid which is brought about in three ways:
1. High concentration of iodide decreases iodine uptake by the thyroid.
2. High concentration of iodine inhibit thyroid hormone synthesis by suppressing both the iodination of tyrosine & the coupling of iodinated tyrosine residues.
3. High concentration of iodine inhibit release of thyroid hormone into blood stream.
Therapeutic uses:
Lugol,s solution is given in preparation for thyroidectomy.Plasma levels of thyroid hormones are reduced with PTU before initiating Lugol,s solution.
Then Lugol,s solution along with PTU is administered for the last 10 days prior to surgery.
Adverse effects:
Chronic ingestion of iodine can produce iodism.Sign & symptoms include a brassy taste,
a burning sensation in the mouth & throat,
soreness of the teeth & gums, frontal headache,
coryza, salivation & skin eruption.
B. Sodium iodide(IV):
IV sodium iodide is employed for the acute management of thyrotoxic crisis.Benefits derive from the ability of high concentration of iodide to rapidly suppress thyroid hormone release.
It is used in combination with PTU & propranolol.
C. Potassium iodide: potassium iodide can be used to treat graves disease & thyrotoxic crisis. it has the same effects as lugol,s solution.4. Propranolol:
Propranolol can suppress tachycardia & other symptoms of Graves disease .Benefits derived from B-adrenergic blockade, not from reducing levels of T3 & T4.