Motor & Sensory Function
of CNS
By
Dr. Mufeed Akram Taha
FIBMS Neurology
Clinical Attachment Turkey

Most volu tar ove e ts i itiated
the cerebral cortex are achieved when
the orte a tivates patter s of
function stored in lower brain areas
—the
cord, brain stem, basal ganglia, and
cerebellum. These lower centers, in turn,
send specific control signals to the
muscles.
The motor functions of CNS can be divided into:-
• Movement in which subdivided into 3 types of
movement
1. Voluntary movement like playing
piano&writing
2. Reflexes which are involuntary, rapid,
stereotyped movement like eye blinking,
Knee jerk.
3. Rhythmic motor pattern like chewing,
walking and running.
• Posture and balance
• communication

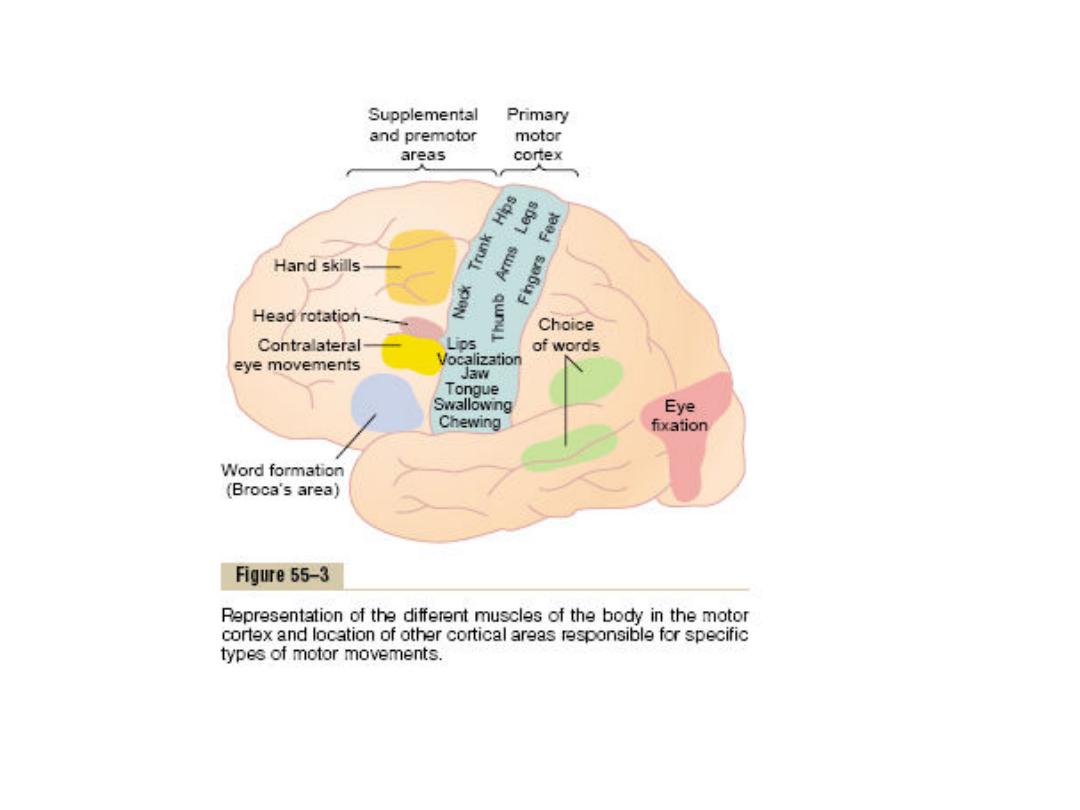
MOTOR CORTEX
The motor cortex occupies posterior third of
frontal lobe anterior to the central sulcus
(precentral gyrus).
The motor cortex itself is divided into three
subareas, each of which has its own
topographical representation of muscle
groups and specific motor functions:
(1) the primary motor cortex,
(2) the premotor area
(3) the supplementary motor area.
Primary Motor Cortex:-
The primary motor cortex lies in the first convolution of
the frontal lobes anterior to the central sulcus.This
area is responsible for conscious voluntary control of
precise, skilled movements of either individual
muscles or small groups of muscles. The extremities
of the opposite side of the body are represented in
the precentral gyrus, with the feet at the top of the
gyrus and the face at the bottom.
The cortical representation of each part of the body is
proportional to the skill with which the part is used in
fine voluntary movement, so more than one half of
the entire primary motor cortex is concerned with
controlling the muscles of the hands and speech.
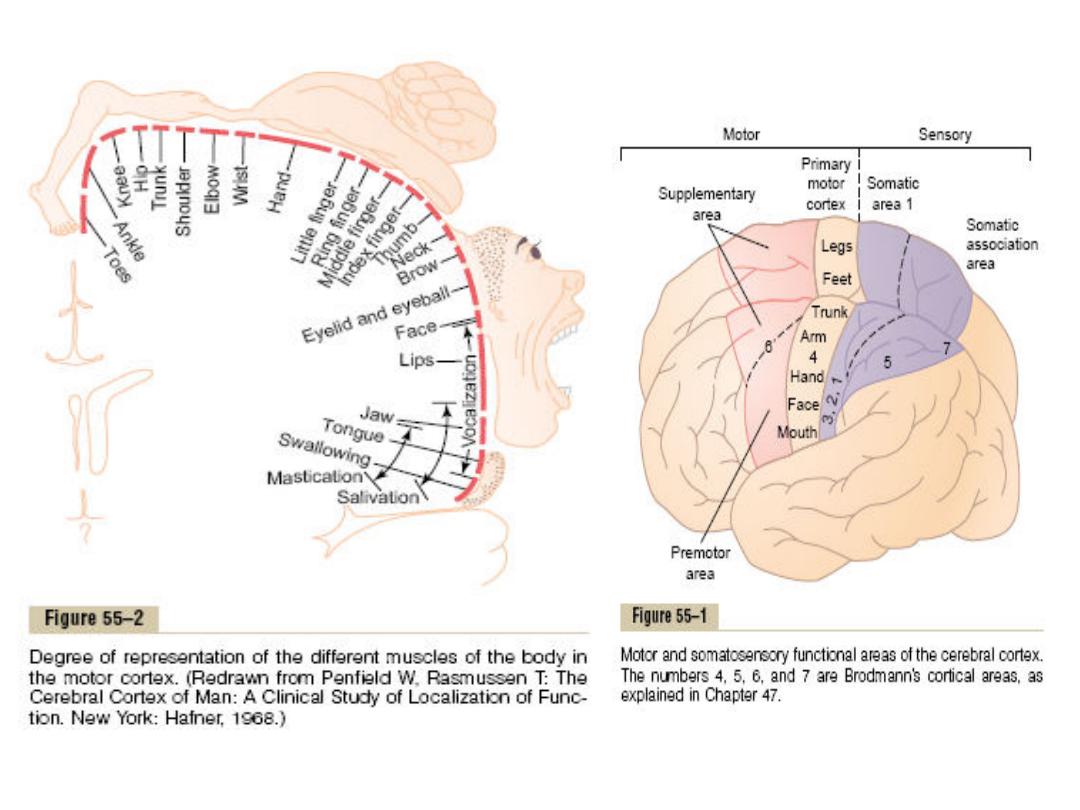
Supplementary Motor Area
This is located on medial surface of the
frontal lobe slightly anterior to the
primary motor cortex. it is responsible
for global mental planning of complex
motor sequences and sends these
instructions to the premotor area.
Premotor Area
This is located anterior to primary motor area and
below the supplementary motor area on the lateral
side of the hemisphere.Nerve signals generated in
the premotor area cause much more complex
patter s of ove e t tha the dis rete patter s
generated in the primary motor cortex. For instance,
the pattern may be to position the shoulders and
arms so that the hands are properly oriented to
perform specific tasks.The premotor area sends its
signals into the primary motor cortex to excite
multiple groups of muscle either directly or indirectly
(through basal ganglia thalamus primary
and premotor cortex.

• Within the premotor cortex the following
areas are present:-
1.
Broca’s area for speech(this is the word
formation area).
2. Voluntary Eye Movement area: Located in
the premotor area immediately above
Bro a’s
area. Damage to this area prevents a person
from voluntarily moving the eyes toward
different objects.
3. Head Rotation Area:This area is closely
associated with the eye movement field; it
directs the head toward different objects.

4. Hand Skills Area: Located in the
premotor area immediately anterior to
the primary motor cortex for the hands
and fingers when there is damage to this
area hand movements become
uncoordinated and nonpurposeful.

Transmission of Signals from the Motor
Cortex to the Muscles
Motor signals are transmitted directly from the
cortex to the spinal cord through the
corticospinal tract and indirectly through
multiple accessory pathways that involve the
basal ganglia, cerebellum, and various nuclei of
the brain stem.

The higher motor control systems
This control systems involve the structure control
all motor activities executed at the brain stem
level and spinal cord and these are :
1-The pyramidal system.
2- The extrapyramidal system.
3- The cerebellum.
The pyramidal and extrapyramidal systems called
upper motor neurons.
Corticospinal (Pyramidal) Tract:-
The corticospinal tract originates about 30%
from the primary motor cortex, 30% from the
premotor and supplementary motor areas,
and 40% from the somatosensory areas
posterior to the central sulcus. After leaving
the cortex, it passes through the posterior
limb of the internal capsule and then
downward through the brain stem forming the
pyramids of the medulla.

The majority of the pyramidal fibers 80% then cross in the
lower medulla to the opposite side and descend into
the lateral corticospinal tracts of the cord, finally
terminating on excitatory (for the agonist muscle) or
inhibitory (for the antagonist muscles) interneurons,
these fibers are concerned with distal limb muscles and
hence with skilled movements especially of hands &
fingers.
A few of the fibers do not cross to the opposite side in the
medulla but pass ipsilaterally down the cord in the
ventral corticospinal( these fibers are concerened with
axial and proximal limb muscle contraction).
Glutamate and or aspartate is the neurotransmitter of the
pyramidal system.
The extrapyramidal system:-
Which includes all those portions of the brain
and brain stem and their fibers that
contribute to motor control but that are not
part of the direct pyramidal system. This
system is concerned mainly with:
• Postural control and stability.
• Inhibits unwanted muscular activity.
• Maintains muscle tone.
Extrapyramidal system includes:
• Basal ganglia
• Reticular formation
• Vestibular nuclei
• Red nuclei
• Substantia nigra
• Tectum
• Subthalamic nucleus
• Cerebellum

When a firm tactile stimulus is applied to lateral
sole of the foot, two reflex arcs are stimulated at
the same time one through pyramidal system
and the other through extrapyramidal system, In
normal condition, the reflex arc of the pyramidal
system suppresses that of extrapyramidal system
and therefore downward bending of the toes is
elicited when tactile stimulus is applied to lateral
sole of foot. When pyramidal system is
dammaged without extrapyramidal system there
will be extension of great toe and fanning of
other toes called Babinski sign.

The main spinal extrapyramidal tracts include
the subcorticospinal pathways which are:-
1. Tectospinal tract(from the superior
colliculus of the tectum and is involved in
the control of neck muscles).
2. Vestibulospinal tract(from vestibular
nuclei)
3. Reticulospinal tracts(from pontine and
medullary reticular formation)
4. Rubrospinal tract(from the red nucleus)
The red nucleus:-
It’s oval u leus, pi k i fresh spe i e s bec. of an
iron containing pigment in many of the cells and
its centrally placed in the upper mesencephalic
reticular formation.It receives fibers from the
deep cerebellar nuclei and cerebral cortex and
the most important efferent projection of the red
nucleus is to the contralateral spinal cord. It
operates in close association with the pyramidal
tract. This nucleus give rise to rubrospinal tract
that cross to opposite side in lower brain stem
and follows a course parallel to the lateral
corticospinal tract and it acts as an accessory

route for the transmition of discrete signals
from the motor cortex to the spinal cord.
This tract is involved in large movements of
proximal musculature of the limbs. It
inhibits activity of extensors and increases
activity of flexors.

Role of the Brain Stem in Controlling Motor Function
The brain stem consists of the medulla, pons, and mesencephalon.
it is an extension of the spinal cord upward into the cranial cavity,
The brain stem provides many special control functions, such as
the following:
1. Control of respiration
2. Control of the cardiovascular system
3. Partial control of gastrointestinal function
4. Control of many stereotyped movements of the body
5. Control of equilibrium
6. Control of eye movements.

Motor Functions of the Spinal Cord
"Spinal Cord Reflexes“
The basic unit of integrated reflex activity is the reflex
arc. This arc consists of a sense organ, an afferent
neuron, one or more synapses in a central
integrating station or sympathetic ganglion, an
efferent neuron, and an effector. The connection
between afferent and efferent somatic neurons is
generally in the brain or spinal cord. The afferent
neurons enter via the dorsal roots or cranial nerves
and have their cell bodies in the dorsal root ganglia
or in the homologous ganglia on the cranial nerves.
The efferent fibers leave via the ventral roots or
corresponding motor cranial nerves

The sensory signals enter the cord almost entirely
through the sensory (posterior) roots. After
entering the cord, sensory signal travels to two
separate destinations:
(1) One branch terminates in the gray matter of the
cord to elicits local segmental cord reflexes and
other local effects.
(2) Branch transmits signals to higher levels (Brain
stem, cerebral cortex).

Sensation

• Input to the nervous system is provided
by the sensory receptors that detect
sensory stimuli.
• Sensory receptors are specialized cells or
neurons that trasduce environmental
signals (mechanical forces, light, sound,
chemicals and temperature) into
neuronal signals (action potential) in
neuron attached to it.

• There are separate warm and cold
receptors.
• Hair receptors associated with skin hairs
allow you to feel the displacement of
hairs.
• Several types of pain receptors respond to
mechanical trauma or very high or low
temperatures.
According to the type of energy or stimulus that stimulates
receptors, there are 5 different types of sensory receptors:-
1.
Mechanoreceptors: which detect mechanical deformation of
the receptor or of cells adjacent to the receptor which include
tactile sensations (touch, pressure, vibration, itch), hearing,
equilibrium and the position sense.
2.
Thermoreceptors:- which detect changes in temperature, some
receptors detecting cold and others warmth.
3.
Pain receptors(nociceptors):- which detect damage in the
tissues, whether it be physical or chemical damage.
4.
Electromagnetic receptors(photoreceptors):- such as rods and
cones which detect light on the retina of the eye.
5.
Chemoreceptors:-which detect taste in the mouth(taste
receptor), smell in the nose (olfactory receptors), O2& CO2
concentrations in the blood(carotid body receptors), osmolality
of body fluids(osmoreceptors).
General properties of receptors:
1. The sensitivity of receptors: each type of
receptor is very highly sensitive to one type of
stimulus or particular type of energy for which
its designed.
2. The specificity of nerve fiber attached to the
receptor: Each nerve fibers is specialized to
transmit only one modality of sensation .
3. The ability to generate a receptor potential
(generator potential): the mechanism used by
the receptor to produce the receptor potential
varies depending on the type of receptor as the
impulse rate is proportional to the stimulus
intensity.

The brain can recognize the intensity of the
stimulus that is transmitted to it by:
A- Variation in the frequency of the action
potential generated by the activity in a given
receptor (called temporal summation and
B- By variation in the number of receptor
activated (called spatial summation)
4-Adaptation or desensitization of receptors: It is
a progressive decrease of receptor response to the
continuous application of a constant sensory stimulus.
When a continuous sensory stimulus is applied, the
receptors respond at first with a very high impulse
rate, then at a progressively lower rate until finally
many of them no longer respond at all.

Referred pain: That is the pain felt in a part of
the body considerably remote from the tissues
causing the pain. Usually the pain is initiated
in one of the visceral organs and referred to
an area on the body surface or deep area of
the body not exactly coincident with the
location of the viscus producing the pain. The
best known example is referral of cardiac pain
to the inner aspect of the left arm. Other
examples include pain in the tip of the
shoulder owing to irritation of the central
portion of the diaphragm and pain in the
testicle due to distortion of the ureter
The mechanism of the referred pain is as follow: The visceral pain
fibers enter the spinal cord and synapse with second order
neuron that also receives pain fiber from the skin. When the
visceral pain fibers are stimulated, pain signals from the viscera
are then conducted through the same neurons that conduct
pain signals from the skin, and person has the feeling that the
sensations actually originate in the skin itself. The rules that
determine the areas to which the pain is referred are:
1- Dermatomal rules:In which the pain is usually referred to a
structure that developed from the same embryonic segment or
dermatome in which the pain originates. For example, during
embryonic development, the diaphragm migrates from the neck
region to its adult location in the abdomen and takes its nerve
supply the phrenic nerve with it. The afferent fibers of the
phrenic nerve enter the spinal cord at the level of the second to
fourth cervical segments, the same location at which afferents
from the tip of shoulder enter.

2- Brain interpretation rule: Pain signals from visceral
structure may converge on the same spinothalamic
tract that receives sensory somatic signals from the
peripheral structures. Since somatic pain is much more
common than visceral pain, the brain has learned that
activity arriving in a given pathway is caused by a pain
stimulus in a particular somatic area.
3- Facilitation effects rule: In which the incoming impulse
from visceral structures lower the threshold of
spinothalamic neurons receiving afferent from somatic
areas, so that minor activity in the pain pathways from
the somatic areas passes on to the brain.

Visceral pain: It is the pain from different viscera
of the abdomen and chest. The true visceral
pain is transmitted through type C nerve fibers
that run in the sympathetic or
parasympathetic nerves. The viscera have
somatic receptors for pain sensation only.
Because there are relatively few pain
receptors in the viscera, visceral pain is poorly
localized. Visceral pain is different from
surface pain and that is a highly localized
types of damage to the viscera rarely cause
pain.

Central inhibition of pain:-Pain perception is affected by
a variety of psychological factors such as mood and
emotional motivational state. For example, under
"fight and flight" condition, the threshold for pain
increases such that stimuli that usually produce pain
are not perceived as painful. Opposite phenomenon
also occurs. For example, when a subject is anxious, a
nonpainful stimulus may perceived as painful. The
degree to which each person reacts to pain varies . The
variation of patient's reaction to pain is due to partly
from the capability of the brain itself to control the
degree of input of pain signals to the CNS by activation
of a pain control system, called analgesia system and
partly by stimulation of large sensory fibers from the
peripheral tactile receptors.

1- Analgesia system: It consists of three major
components and these are:
(A)The neurons of periaqueductal gray area.
(B) Neurons of raphe magnus nucleus.
(C) Pain inhibitory complex located in the dorsal
horns of the spinal cord.
(D) plus other accessory components (such as
periventricular nuclei around the third
ventricle and medial forebrain bundle in the
hypothalamus).

2- Stimulation of peripheral sensory fiber (gate
control theory): Cells in substantia gelatinosa
(SG) act as the "gate". Stimulation from large
fibres (A fibers) causes the gate to close (cells
in SG stimulated, decrease pain signal).
Stimulation from small fibres (C fibers) opens
gate (cells in SG inhibitted, increase pain
signal).

3- Thermal sensations; Thermal sensations are detected
by two different types of subcutaneous sensory
receptors. There are two types of thermal receptors
and these are:
(1) The cold receptors which respond maximally to
temperature slightly below body temperature and the
signals are conducted through A and C nerve fibers.
(2)The warmth receptors which respond maximally to
temperature slightly above body temperature and the
signals are conducted through C nerve fibers.
Because the number of cold or warmth receptors in any
one surface area of the body is very slight, it is difficult
to judge gradations of temperature when small areas
are stimulated. The judgment of gradation is increased
as the stimulated surface area increases.

• Signs of lesions of peripheral sensory pathways:
With complete lesion of peripheral sensory
nerves all forms of sensation are lost in the area
supplied by the affected nerve but without
following the dermatemal pattern due to the fact
that neighboring nerves overlap into the territory
of the affected nerve.
• If the afferent fibers of a reflex arc affected, the
reflex concerned is lost. With lesions of the
posterior root of the spinal cord all forms of
sensation are lost but the distribution of the loss
follows a dermatomal pattern, and loss of
reflexes subserved by the involved root.

The course of the somatic sensations through
the spinal cord
(The somatosensory system)
Almost all the afferent sensory somatic
information of the body enters the spinal cord
through the dorsal roots of the spinal nerves
or the brain stem via the cranial nerves. On
entering the spinal cord the sensory signals
are carried to the brain by one of two sensory
pathways:

1
— the dorsal column pathway (lemmiscal system); in which:
first order neurons (dorsal root sensory fibers) enter the
dorsal column of the spinal cord and then pass up on the
same side of its entrance in the spinal cord to the medulla,
where they synapse in the cuneate and gracile nuclei.
From the cuneate and gracile nuclei the second order neurons
are originated and decussate immediately to the opposite
side and then pass upward to the thalamus through medial
leminisci pathways which is joined by additional decussated
fibers from the sensory nucleus of the trigeminal nerve.
From thalamus, third order neurons project mainly to the
somatic sensory area located at postcentral gyrus and
occupy the cerebral cortex of the anterior portion of the
parietal lobe.
So The dorsal column carries the following sensations: fine
touch and pressure (including weight, shape, Size, texture),
vibration, proprioception.
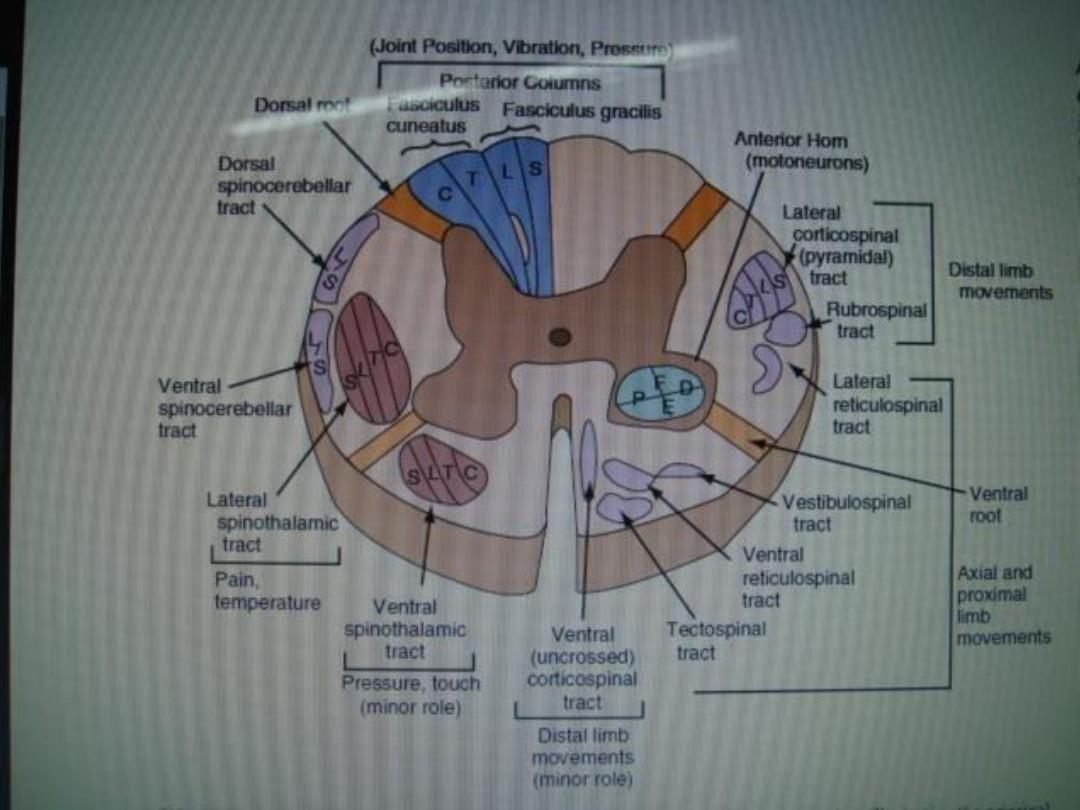

2
— the anterolateral pathways (spinothalamic pathway): In which
[A]First order neurons (dorsal root sensory fibers) enter the dorsal
horns of the spinal cord and synapse with the second order
neurons.
[B]The second order neurons cross to the opposite anterolateral white
column where, they turn upward toward the thalamus through
anterior and lateral spinothalamic tracts. Some of the second order
neuron of the anterolateral system, which carry signals from slow C
pain fibers, pass to the reticular formation of the medulla, pons,
and mesencephalon through a spinoreticular pathway and through
spinotectal tract, From these areas, higher order neurons are
transmitted from reticular formation to the cortex.
[C] From thalamus, third order neurons project mainly to the somatic
sensory area of the cortex along with the neurons of the dorsal
column.
The anterolateral system carries the following sensations: crude
touch and pain, thermal sensation.

Signs of lesions of the central sensory pathways
[1] A lesion confined to the posterior column of the spinal cord
will cause:
Loss of position and vibration sense on the same side, but the sensation
of pain, touch, temperature will be preserved.
[2] Lesions of the spinothalamic tracts cause impairment of the ability to
appreciate pain and temperature on the contralateral side of the body
below the level of the lesion. Touch is usually modified (it feels
different) but not abolished because of its alternative pathway in the
posterior columns.
[3] In the brain stem, the spinothalamic tract and medial lemniscus run
close together. Therefore, lesion of the upper brain stem usually
affects all forms of sensation on the contralateral side ofthe body.
[4] Lesions of the main sensory nuclei of the thalamus may cause:
Loss of various modalities of sensation on the opposite side of the body,
And spontaneous pain of most unpleasant quality in the opposite side
of the body which often causes considerable emotional reaction.

Higher interpretation of sensory signals
This is achieved by the cerebral cortex in the following areas :
[1] Primary sensory areas.
[2] Sensory association areas.
[3] Wernicke's area.
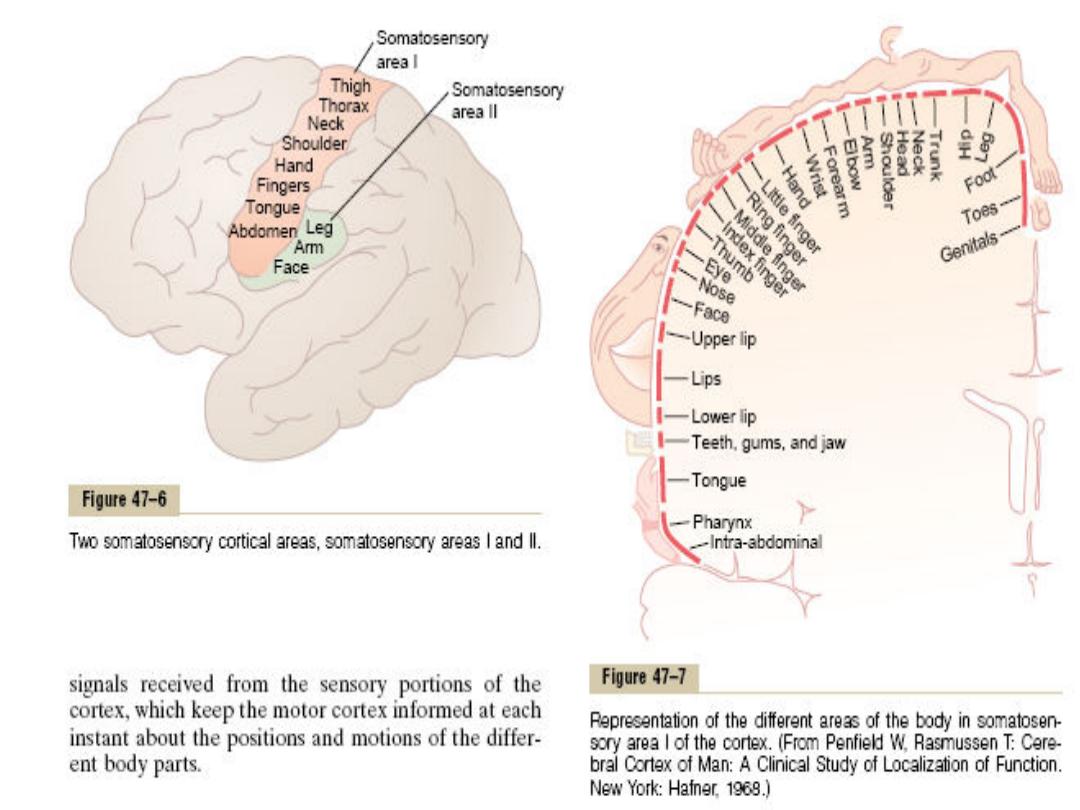
[1] Primary sensory areas: which include :
Primary somatic sensory area.
Primary visual sensory area.
Primary auditory sensory area.
They are the areas of the cerebral cortex to which the respective
sensory signals are projected. They have spatial localization of
signals from peripheral receptors., These, areas analyze only the
simple aspects of sensations and that is to inform the brain that a
sensory signal is actually arrived to the
cerebral cortex but they are
not able of complete analysis of complicated sensory patterns.

In the primary somatic sensory area the spatial
orientation of the different parts of the opposite side
of body were represented. The size of the area of
representation is directly proportional to the number
of specialized sensory receptors in each respective
peripheral area of the body. For instances, the lips by
far the greatest of all, followed by the face and thumb
where as the entire trunk and lower part of the body
are represented by relatively small areas.
Yet orti al lesio s do ’t a olish so ati se satio . Thus,
perception may occur at subcortical level and it is
possible in the absence of the cortex. Wide spread
excision of primary somatic sensory area does not
abolish and present following signs:

• The person is unable to localize discretely the
different sensations in the different parts of
the body.
• He is unable to judge exactly the degrees of
pressure against his body.
• He is unable to judge exactly the weights of
objects.
• He is unable to judge shapes or forms of
objects.
• He is unable to judge texture of materials.

[2] Sensory association areas:
Which include:
Somatic sensory association area.
Visual sensory association area.
Auditory sensory association area.
Around the borders of the primary sensory area are
regions called sensory association area. the
general function of the sensory association areas
is to provide a higher level of interpretation of
the sensory signals. In these areas interpretation
of sensory signals is achieved by giving the
simplest meaning and characteristic of the
sensory signal. Destruction of the sensory
association greatly reduces the capability of the
brain to analyze and interpretate different
characteristics of sensory experiences.

[3] Wernicke's area:
It is the area where the sensory association
areas all meet one another in the posterior
part of the temporal lobe where the temporal,
parietal, and occipital lobes all come together.
This area is called Wernicke's area which
converge the different sensory interpretative
areas.

It is highly developed in the dominant side of
the brain and plays the greatest role in
interpretation of the complicated meanings of
different sensory experiences. It is important
to note that the left hemisphere is usually
dominant with respect to language, even in
left handed people

Following severe damage to this area in the
dominant side of t he brain:
A person might hear perfectly well and even
recognize different words but still might be
unable to arrange these words into a coherent
thought. Likewise the person may be able to
read words from the printed page but be
unable to recognize the thought that is
conveyed.

Thank you
