Unit 3: Drugs Affecting the Central Nervous System
71
Lecture 4+5 - Anesthetics
Local Anesthetics Drugs
Unit 3: Drugs Affecting the Central Nervous System
72
Unit 3: Drugs Affecting the Central Nervous System
73
Unit 3: Drugs Affecting the Central Nervous System
74
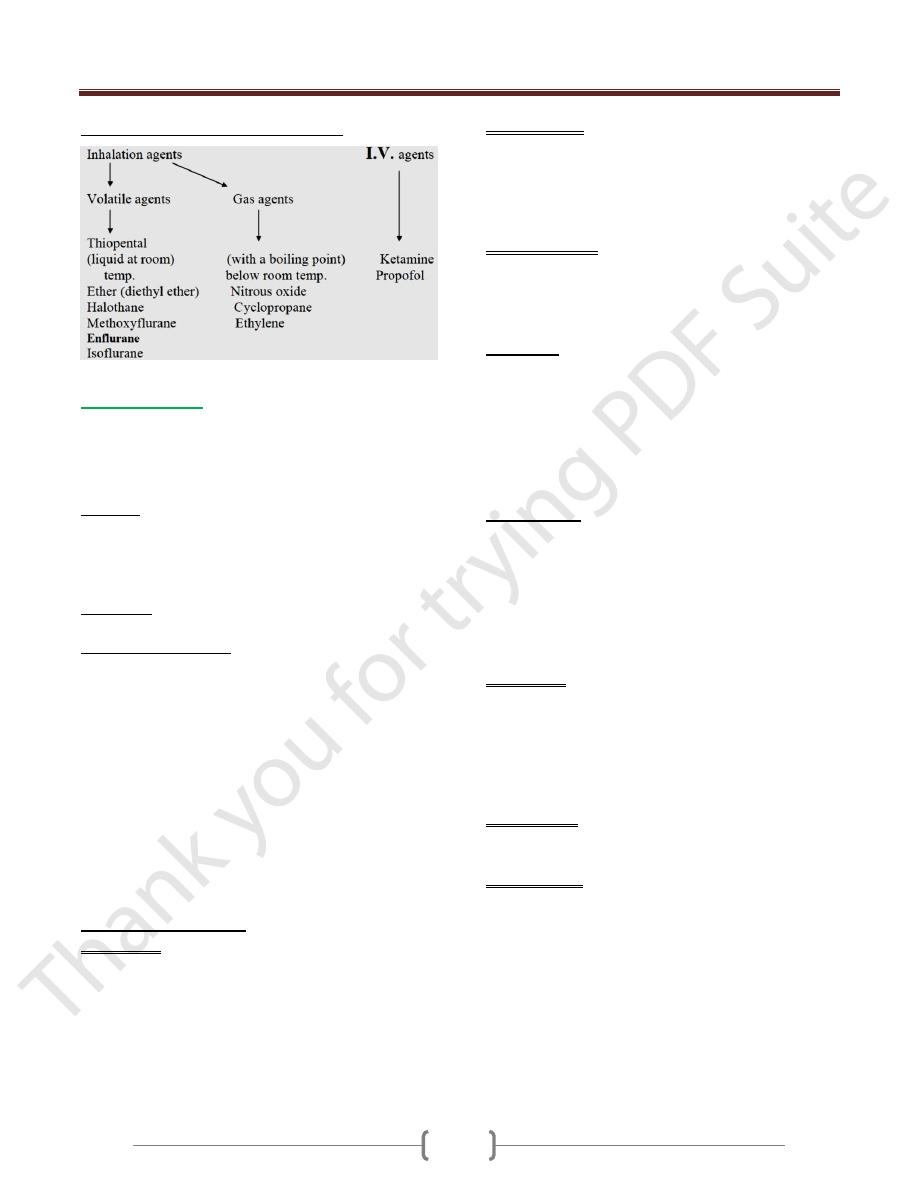
General anesthetic drugs
Anesthesia: Is a Greek Word meaning lack of
sensation.
Anesthesia is divided into 2 parts:
A. General anesthetic drugs B. Local anesthetic drugs
General anesthetic drugs
Are drugs which produce reversible loss of Sensation and
consciousness. General anesthetic agents can be
administered by different routes:
Oral administration
Subcutaneous
Rectal suppository
Intravenous injection anti inhalation
But l.V or inhalational administration is preferred. The
drugs which are given as anesthetics b l.V
administration are used for specific purpose as quickly
acting general anesthetics for few minutes or as a
supplement with another general anesthetic agents as:
Thiopental (i.v anesthetic agent), (Nitrous oxide, ether
and halothane (Inhalation agent).
As a supplement in order to produce the induction of
anesthesia in a short period, because the inhalational
anesthetic agents need a time about 15-20 minutes for
production of induction.
During this 15—20 minutes, the patients will start into
what we called stages of general anesthesia.
1) Stage I (Analgesia): The subject is conscious but
drowsy. Responses to painful stimuli are reduced. It is
pronounced with ether and nitrous oxide but not with
Halothane.
2) Stage II (Excitement): This stage starts when the patient
is unconscious. The respiratory rate is increased and
irregular. There is a rise and irregularity in B.P. During
this stage the pupils are dilated. This stage may be
prolonged leading to increase risks of sudden death. To
avoid this stage of anesthesia, a short acting barbiturate
such as Pentothal is given l.V before inhalation anesthesia
is administered.
3) Stage III (Surgical anesthesia).
The patients are not responded to surgical stimulation.
Pupils become to dilate again and the eyes are dry.
The skeletal muscle becomes relax.
Corneal and laryngeal reflexes are absent.
Light reflex is lost.
The skeletal muscle becomes marked relax. Surgery may
proceed during this plane.
4) Stage IV (Medullary paralysis):
The medullary center becomes completely paralysis
failure of ventilation and circulation, marked fall in B.P.
Death can rapidly ensue.
General aspects of anesthesia:
The practice of anesthetist has three main parts:
Before surgery (pre-medication):
The principle is to provide:
A. Sedation and amnesia (to reduce anxiety and stress).
-The patient who is going to do operation is normally
afraid, -Sedation and amnesia may produce by a drug like
diazepain.
B. Analgesia.
e.g. of drug produces analgesia pethedine or morphine.
C. Inhibition of para-sympathetic autonomic system
(Antimuscari.nic agent)....
1) To reduce bronchial secrçtion. Mostly happen with the
use of an irritating drug such as ether. Bronchial
secretion may cause bronchospasm.
2) To reduce secretion of salivary glands, because the
saliva may enter the larynx causes laryngospasm.
3) To reduce reflex bradycardia and hypotension. E.g. of
drug produces inhibition of para-sympathetic.
Atropine or 1-lyoscine.
So Typical combination drugs used in premedication
Include:
Morphine Hyoscine These combination
or + or } usually given
lhr.before
pethedine Atropine operation
During surgery:
The most important is to produce sleep, analgesia & muscle
relaxation by using a single drug or more than one drug.
After surgery:
The anesthetist ensures that the effects of hypnotic,
analgesic and muscle relaxant are adequate.
The patient must never be left alone until he is conscious
Unit 3: Drugs Affecting the Central Nervous System
75
Types of general anesthetic agents
Inhalation agents
Pharmacokinetics:
The level of anesthetic is determined by the tension
(concentration) of anesthetic in the brain tissue. It is
influenced by:
1) Solubility
An anesthetic agent with high solubility in blood as ether
will provide slow induction because blood will act as a
reservoir or store for the drug, so that it does not enter the
brain easily until the reservoir has been filled.
2) Elimination
It depends mainly on the lungs
3) Metabolism and toxicity.
Some of the inhalation anesthetics are metabolized to
certain toxic effects as:
Chloroform: produces hepatotoxicity associated with free
radical formation in liver cells.
Methoxyflurane: is now very rarely used because 5O%
of Methoxyflurane is metabolized, generating fluoride and
oxalate which cause renal toxicity.
Enflurane: also generates fluoride but at much lower
level (non-toxic).
Halothane: is metabolized (about 30%) to bromide,
trifluoracetic acid and other metabolites which may be
responsible for the rare occurrence of liver toxicity.
1)
Halothane (Fluothane):
Advantages:
Potent and nonflammable.
Induction is smooth and rapid. The surgical anesthesia
is produced within 2-5 minute.
No effect on bronchial and salivary secretion.
recovery is rapid and incidence of post-operative
nausea and vomiting is low.
Disadvantages:
Muscle relaxation is not enough.
Potent respiratory depressant.
Induces cardiac arrhythmia.
Sever hepatitis which may be fetal.
Expensive.
Drug interaction:
Potentiate the response to antihypertensive drugs.
Sensitizes the heart to adrenaline (when adrenaline is
used to obtain bloodless filed of surgery).
2)
Isoflurane
Is an isomer of Enflurane. It is a new non-flammable
agent.
Its intermediate in potency with Halogenated agents and
the heart rhythm is stable during its use.
It has a good muscle relaxation effect.
It has low blood/gas solubility.
3)
Nitrous oxide
It is non-flammable agent
It is mixed with oxygen 50% for surgical anesthesia; this
mixture is added to another inhalation agent to reduce the
requirement of the inhalation agent by 50%.
Anoxia may occur if mixed with less than 20% oxygen
Euphoria and hallucination during induction called
laughing gas.
Advantages:
It has strong analgesic action.
induction is rapid.
Produces light anesthesia without depressing the
respiratory or vasomotor center.
Recovery time rarely exceeds 4 mm even after
prolonged administration.
Disadvantage:
It must be used with more effective anesthesia and muscle
relaxants to produce a state of full surgical anesthesia.
Adverse effects
Nausea and vomiting.
Bone marrow depression with repeated uses and
teratogenic risk.
Unit 3: Drugs Affecting the Central Nervous System
76
Intravenous anesthetic agents:
Produce rapid induction, because the blood
concentration can be raised rapidly.
Are used in short minor operation or as a supplement with
inhalational anesthetic to produce the induction for the
major operation.
The I.V Anesthetic agents are mainly the:
1) Very short acting barbiturate: like
Thiopental
Methohexital
Thiamylal
Thiopental in a single dose exerts its effect within 30
second and it remains for about 4-7 mm. It is quickly
take up from the plasma into the fat depots of the
body. After many injection have been given. The fat
depots become saturated and a further dose produces a
prolonged effect.
Great care is necessary to avoid over dose which results in
depression of respiratory activity
Laryngospasm and increased bronchial secretion are
common.
Insignificant analgesic effect and the muscle
relaxation is too short.
2) Ketamine
It is hallucinogen drug. In anesthetic doses, it produces a
trance-like state known as dissociation anesthesia
(sedation, amnesia and analgesia). The effect of ketamine
is on the superficial pain but not on visceral pain. So for
this reason ketamine uses to induce anesthesia for the
patient who has superficial pain as a minor operation.
Advantages:
Anesthesia remains for up to 15 mm. after a single I.V
injection & is characterized by a good analgesic action
It does not induce bronchospasm, so it is used to
anesthetist patient suffering from asthma.
Disadvantages:
It lacks of muscle relaxation.
It raises heart rate, intracranial & intraocular
Pressure.
Its recovery is very slow and may be a companied by
hallucination.
