Unit 7: Chemotherapeutic Drugs
203
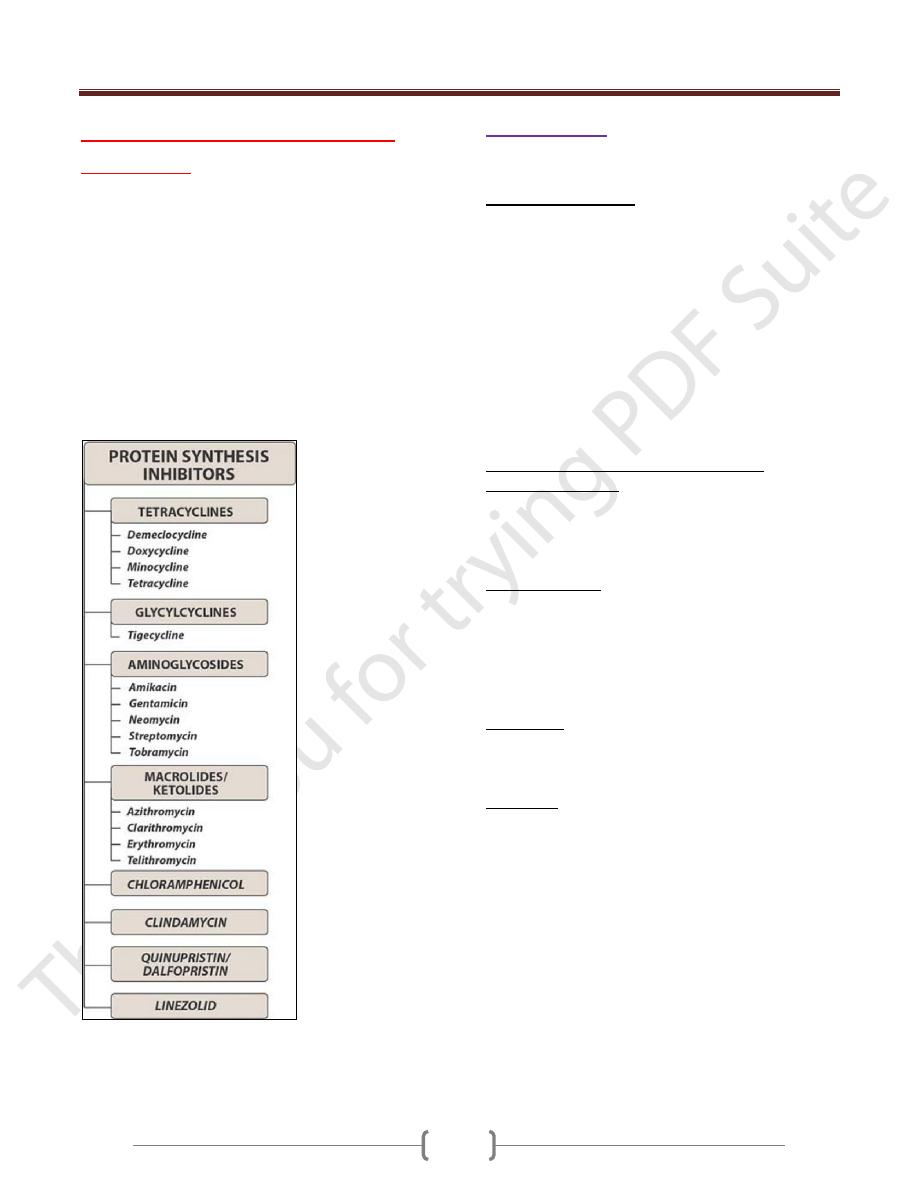
Lecture 4 - Protein synthesis
inhibitors
A number of antibiotics exert their antimicrobial effects
by targeting the bacterial ribosome. In general, the
bacterial ribosome is smaller (70S) than the mammalian
ribosome (80S). The mammalian mitochondrial ribosome,
however, more closely resembles the bacterial ribosome.
Thus, although drugs that interact with the bacterial target
usually spare the host cells, high levels of drugs such as
chloramphenicol or the tetracyclines may cause toxic
effects as a result of interaction with the mitochondrial
ribosomes. The following figure shows the drugs of
protein synthesis inhibitors
Summary of protein synthesis inhibitors
A.Tetracyclines
Are large group of antibiotics with common basic
structure and activity.
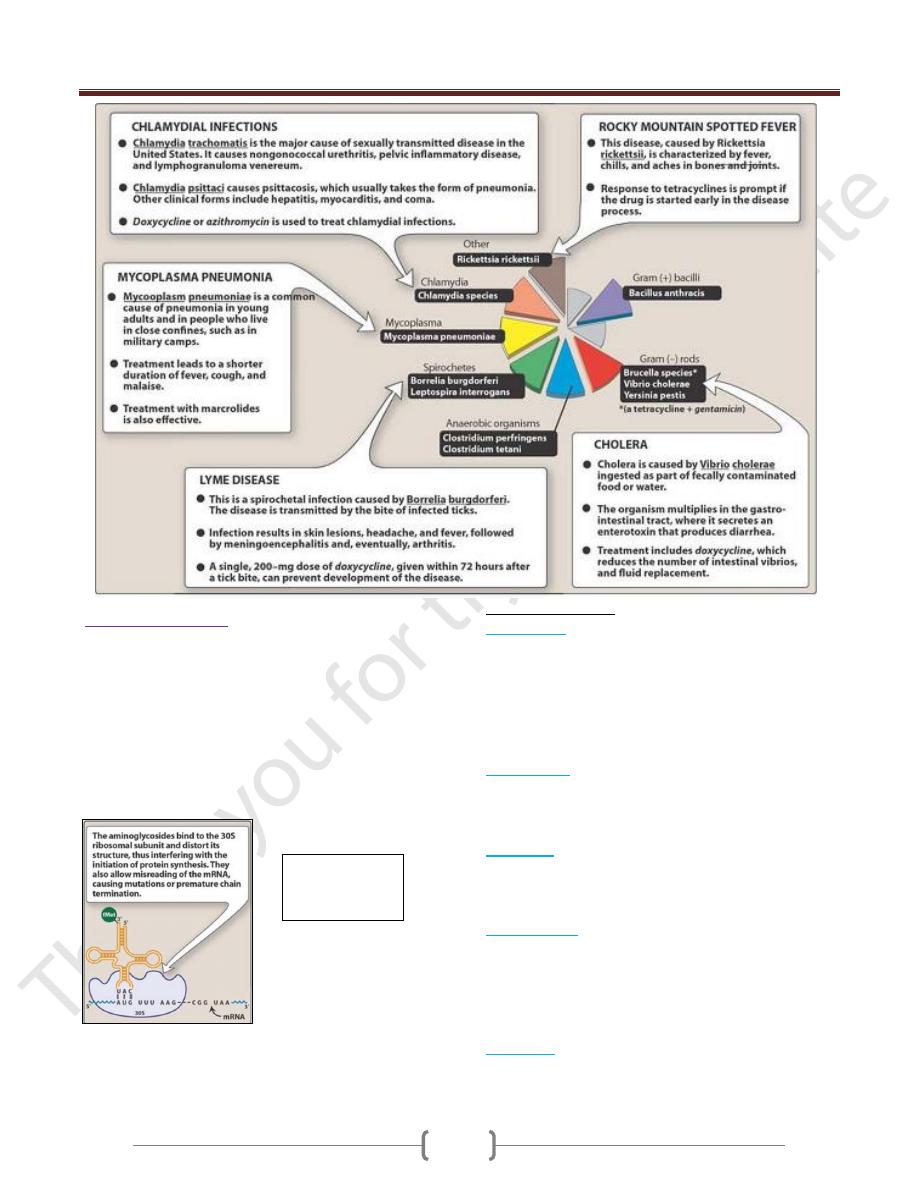
Antibacterial spectrum
Are broad spectrum antibiotics which act by inhibition of
protein synthesis so they are bacteriostatic. They are
effective against a wide range of m.o as G+ve including
corynebacterium acnes and G-ve including vibrio
cholerae infection, mycoplasma, rickettisia & Chlamydia.
The antibiotic range of all tetracyclines is the same,
except that some tetracycline-resistant strain might remain
susceptible to minocycline. The differences in clinical
efficacy between members of this group are minor and
attributed largely to features of absorption, distribution
and excretion of the drug so they are pharmacokinetic
rather than antimicrobials.
The therapeutic application of tetracyclines
Mechanism of action
Tetracyclines act by inhibiting bacterial protein synthesis
by binding to 30S ribosomal subunit thus preventing
binding of aminoacyl transfer RNA to the a site on the
50S ribosomal unit.
Pharmacokinetics
Usually tetracyclines are given by oral route but it can be
given also intravenously when it is required. Calcium,
magnesium, iron preparation can form chelates with
tetracyclines thus avoid their simultaneous administration.
These ions will impair the absorption of tetracycline & they
stay in the intestine and inhibit normal intestinal flora.
Distribution
The tetracyclines are readily distributed through all body
tissues in the liver, kidney, spleen& skin & bind to tissues
undergoing calcification (for example, teeth and bones).
Side effects
Discoloration of teeth in the young and should not be
given to children up to 8 years of age and in pregnant or
lactating women.
Phototoxicity for example, sever sunburn occurs when
the patient receiving a tetracycline is exposed to sun or
ultraviolet rays
Vestibular problems, this may lead to dizziness, vertigo,
nausea and vomiting and this is remarkable for
minocyclin.
Superinfection: Overgrowths of Candida (for example in
the vagina) or of resistant staphylococci (in the intestine)
may occur.
local tissue injury I.V injection thrombophlebitis
I.M injection local irritation
Unit 7: Chemotherapeutic Drugs
204
B. Aminoglycoside
They are bactericidal antibiotics acting on the 30S
ribosomal subunit thus disrupting bacterial protein
synthesis. They are effective only against aerobic
organisms, since anaerobes lack the oxygen-requiring
transport system.
One of the mechanisms of resistance of bacteria to
aminoglycoside antibiotic includes plasmid-mediated
formation of enzymes as acetylate, phosphorylate or
adenylate to inactivate the drug.
Clinical indications:
1) Gentamicin:
It is effective against G-ve m.o as pseudomonas
aeruginosa and G+ve m.o. It is not effective against
anaerobes and usually it may be given alone or in
combination with penicillin or vancomycin in the
treatment of streptococcal endocarditis or meningitis.
It is used topically for skin and eye infections.
2) Tobramycin:
It is similar to gentamycin in activity as antibiotic
spectrum. Slightly more effective against pseudomonas in
patient with cystic fibrosis.
3) Amikacin:
Is used in serious infections with G-ve organisms that are
resistance to gentamycin and in systemic infection with
pseudomonas.
4) Streptomycin:
Is active for T.B as a second line therapy. It is used with
tetracycline for plague, tularemia and brucellosis.
Side effects: vestibulotoxicity, allergic manifestations,
used by pregnant women it may lead to deafness of the
newborn.
5) Neomycin:
Active against G+ve and G-ve microorganisms. It is used
topically for skin infection and can be taken orally.
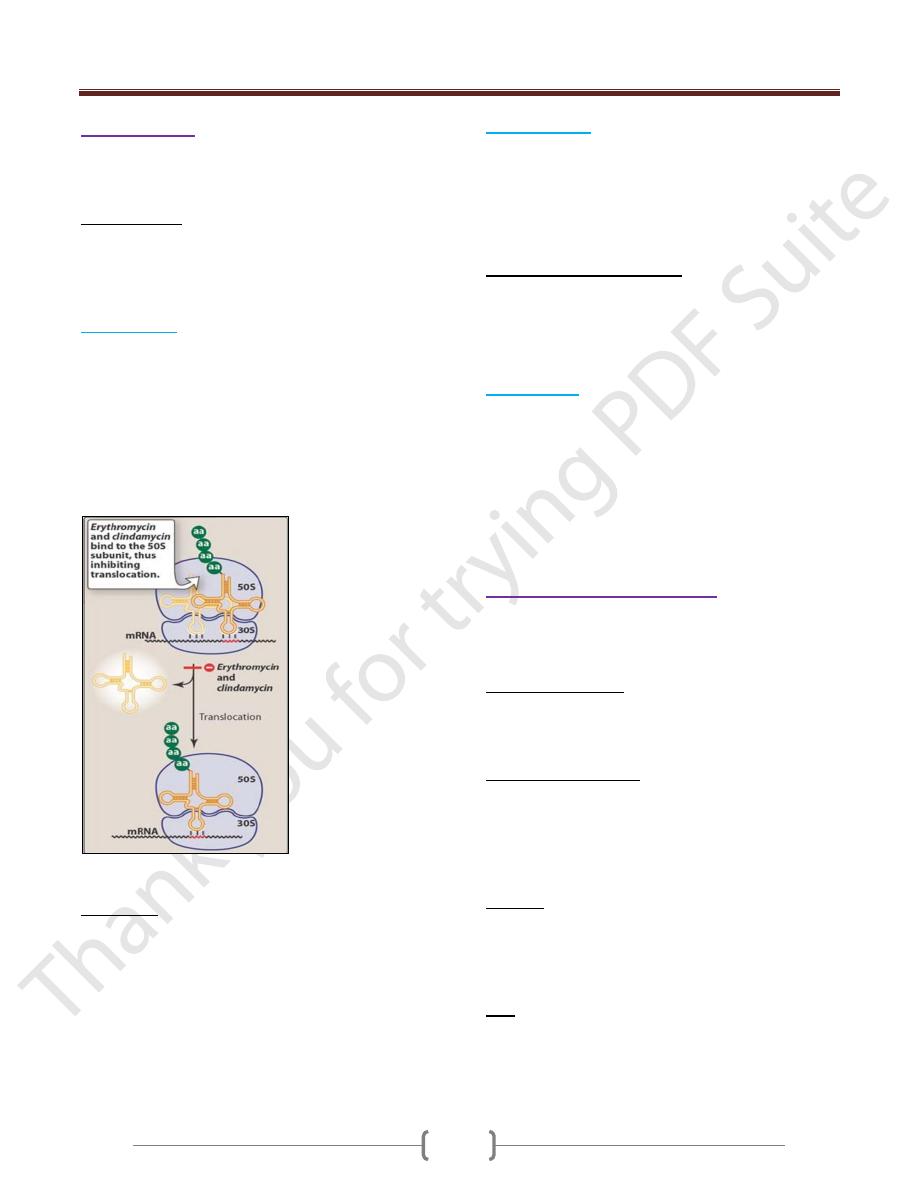
Mechanism of
action of
aminoglycosides
Unit 7: Chemotherapeutic Drugs
205
C. Macrolides:
Are group of closely related compounds characterized by
a macrocyclic lactone ring to which deoxy sugars are
attached.
Mode of action:
Macrolides bind irreversibly to a site on the 50s subunit of
the bacterial ribosome, thus inhibiting the translocation
steps of protein synthesis. Generally considered to be
bacteriostatic, they may be cidal at higher doses.
1) Erythromycin:
It is effective against G+ve organisms including
pneumococci, streptococci, staphylococci and
corynebacterium.
It is effective against other organisms on which β-lactam
antibiotics are not effective as mycoplasma, legionella,
Chlamydia and ureaplasma. G-ve organisms such as
neisseria species, some rickettsia species, treponema
pallidum and campylobacter species.
Mechanism of action of erythromycin and clindamycin
Side effects:
GIT problems (nausea, vomiting and diarrhea).
Liver toxicity (this occurs especially with estolate salt
form of erythromycin.
Ototoxicity: transient deafness especially at high doses.
Interactions: erythromycin inhibits the hepatic
metabolism of theophylline, warfarin (oral
anticoagulants), estemizole, carbimazipine and
cyclosporine which can lead to toxic accumulation of
these drugs.
2) Clarithromycin:
More acid stable and the absorption is better than
erythromycin
Clarithromycin is more effective against Haemophilus
influenzae
Similar indication to erythromycin with added use against
toxoplasma gondii and mycobacterium intracellular.
Advantages of clarithromycin:
1) It has longer half-life this permits a twice daily dosing.
2) It penetrates well to the most tissues.
3) It is metabolized to active metabolite which has an
antibiotic activity.
3) Azithromycin:
Less active against streptococci and staphylococci than
erythromycin but more active against respiratory
infections due to haemophilus influenzae. It is now the
preferred therapy for urethritis caused by Chlamydia
trachomatis.
It penetrates into most tissues except CSF with half life 2-
3 days, this allows a single daily dose and shortening of
the course of therapy.
D- Lincosamide antibacterials
Include
lincomycin
and
Clindamycin
Both agents resemble erythromycin in the antibiotic
activity.
Mechanism of action:
Inhibit protein synthesis by binding to 50S ribosomal
subunit at a binding site close to the binding sites of
erythromycin.
Antimicrobial spectrum
They are bacteriostatics active against infections caused
by anaerobic bacteria such as bacteroids fragilis which
often causes abdominal infections associated with trauma.
They are active against staphylococci, streptococci except
enterococci.
Kinetics:
Distribution is well to most body tissues and fluid except
CSF even when the meninges are inflamed. They attain
high concentrations in bone so they are very effective in
bone and joint infections.
Uses
Clindamycin is preferred over lincomycin because of
enhanced absorption, more effectiveness and less toxicity;
but because clindamycin use may result in
pseudomembraneous colitis therefore its use is also
Unit 7: Chemotherapeutic Drugs
206
limited to those patients who can not tolerate other
antibiotics. Clindamycin is used primarily to treat
anaerobic infections caused by B.fragilis. It is used as
alternative to penicillin but not effective in endocarditis.
Clindamycin is useful topically in cystic facial acne but
take care to avoid colitis development. Clindamycin and
lincomycin are not effective against aerobic G-ve bacilli.
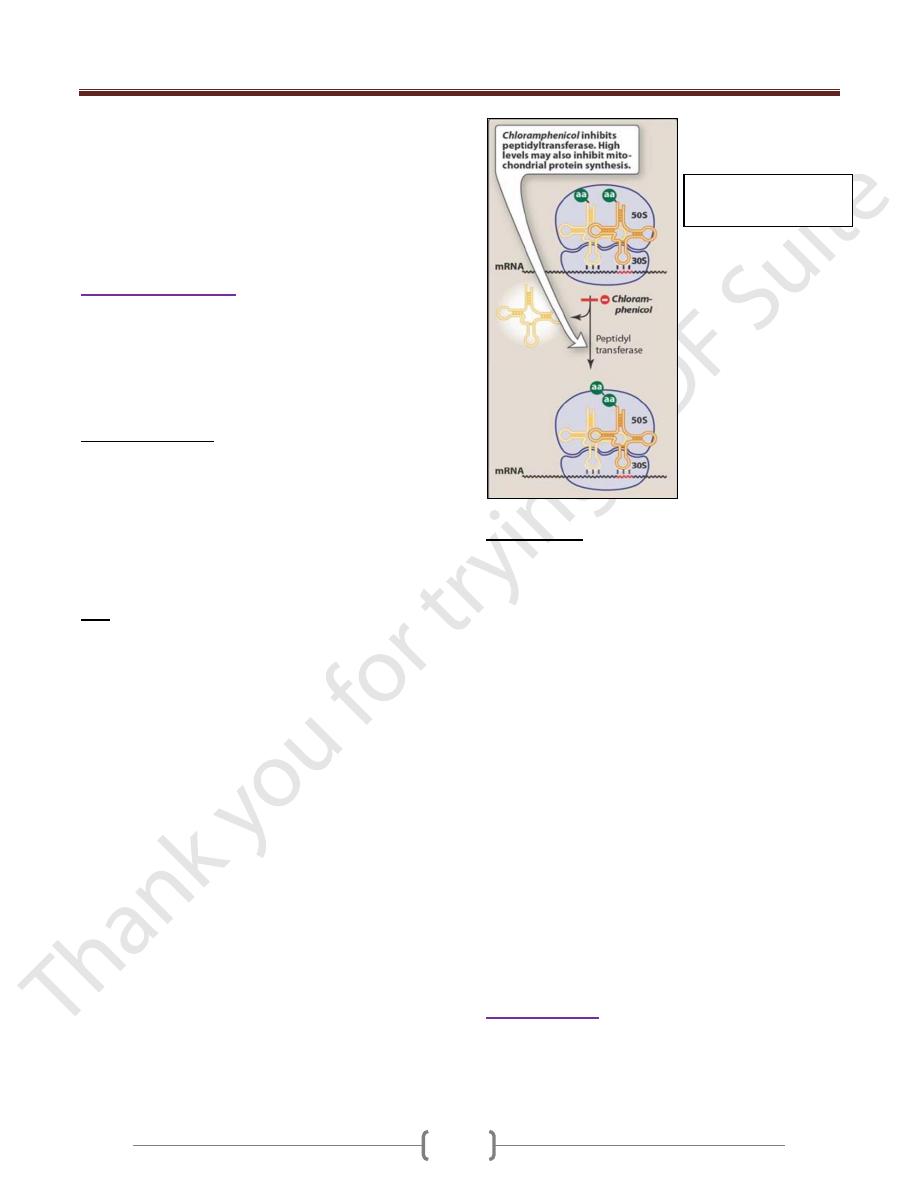
E. Chloramphenicol
Is active against a wide range of G+ve and G-ve organism
including Rickettsia, Mycoplasma and Chlamydia. It’s
also effective against anaerobic bacteria as B.fragilis. It is
a bacteriostatic with wide range of activity and may
become bacteriocidal against some micro-organisms.
Mechanism of action
It binds to 50S segment of the ribosome and inhibits
peptidyl transferase enzyme responsible for peptide bound
formation leads inhibition of protein synthesis. Because of
the similarity of mammalian mitochondrial ribosomes to
those of bacteria, protein synthesis in these mammalian
may be inhibited at high circulating chlormphenicol levels
producing bone marrow toxicity.
Uses
As drug of choice for treating ampicillin-resistant typhoid
fever, paratyphoid fever and other salmonella infections,
and infection caused by H.influenzae as meningitis,
arthritis and osteomylitis. Chlormphenicol is used against
β-lactam producing strains of H.influenzae but third
generation cephalosporins as ceftriaxone is preferred.
Chloromphenicol is widely used as topical treatment of
both eye and ear infections. It’s very effective because of
its broad spectrum activity and ability to penetrate ocular
tissues. Chloromphenicol is an alternative for tetracycline
in treating Rickettsial infection. It’s
also used in serious anaerobic infections (as cerebral
abscess caused by anaerobic bacteria).
Adverse effects
1) Gray baby syndrome: this syndrome occurs in neonates
if the dosage regimen of chloramphenicol is not properly
adjusted. Neonates have a low capacity to glucuronidate
the antibiotic and they have under developed renal
function. They therefore have a decreased ability to
excrete the drug, which accumulates to levels that
interfere with the function of mitochondrial ribosomes.
This leads to poor feeding, depressed breathing,
cardiovascular collapse, cyanosis and death.
2) Anemia: hemolytic anemia occurs in patients with low
levels of glucose 6-posphate dehydrogenase.
Chlormphenicol may lead to inhibition of the RBC
maturation in the bone marrow, this effect is dose
dependent and it is reversible. Aplastic anemia which is
idiosyncratic reaction, non dose related and irreversible
and may be fatal.
3) Chloramphenicol inhibits metabolism of several drugs
as phenytoin (anticonvulsant), chlorpropamide and
tolbutamide (hypoglycemic agents), coumarin and
warfarin (anticoagulants agents).
4) GIT disturbances
F. Fusidic acid
It inhibits protein synthesis as chloramphenicol. It has
antimicrobial activity against S.aureus infection. It’s
usually used topically.
Mechanism of action of
chloramphenicol
