Unit 7: Chemotherapeutic Drugs
210
Lecture 6 - Antimycobacterial drugs
Mycobacterium infections are among the most difficult of
all bacterial infections to cure. Mycobacteria are slowly
growing organisms, making them relatively resistance to
antibiotics. Mycobacterial organisms are intracellular,
residing within macrophages and inaccessible to drug that
penetrate poorly. Combination of drugs rather than to any
single drug are required to overcome the resistance during
the course of therapy, and the treatment must be
administered for months to years depending on which
drugs are used.
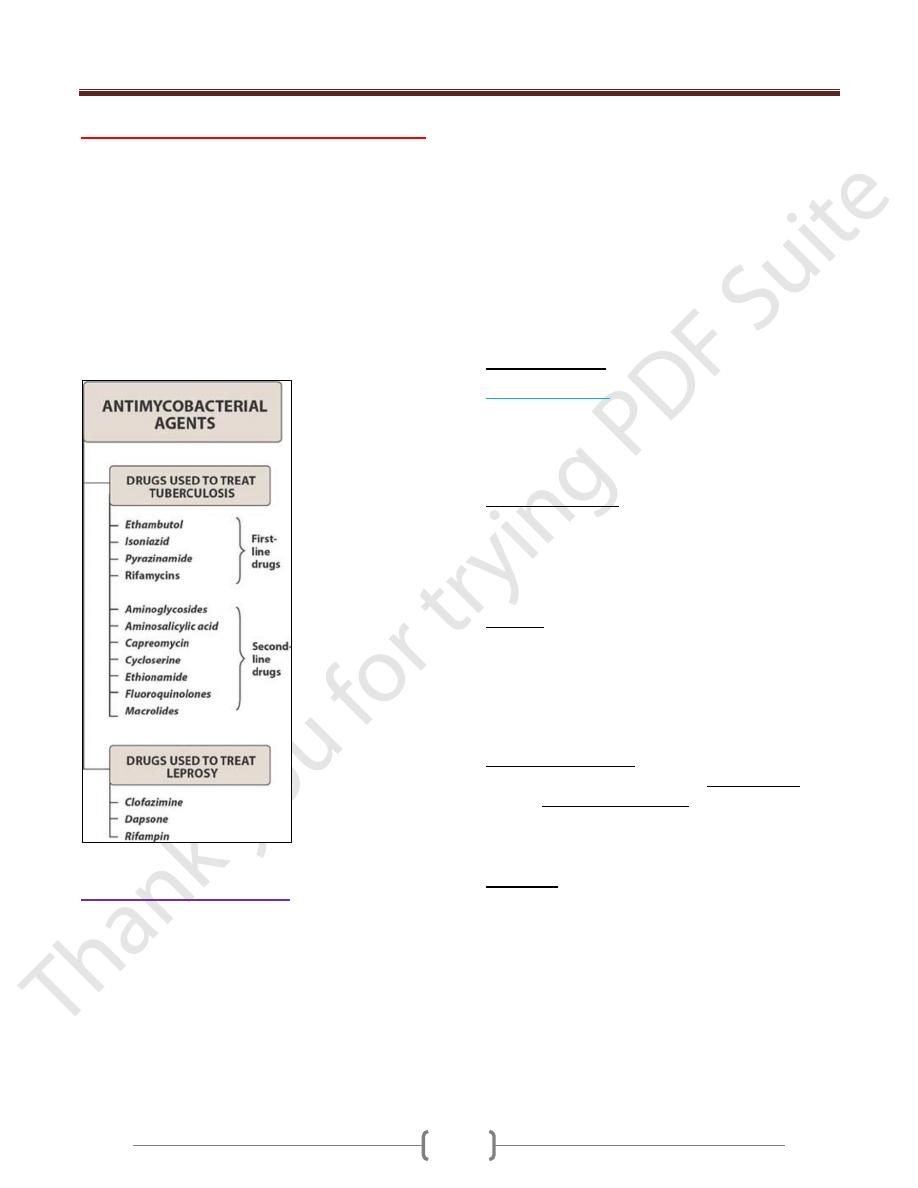
Summary of drugs used to treat mycobacterial infections.
Drugs used in tuberculosis:
Therefore, multidrug therapy is employed when treating
tuberculosis in an effort to delay or prevent the emergence
of resistant strains.
The multidrug regimen is continued well beyond the
disappearance of clinical disease to eradicate any
persistent organisms. For example, the initial short-course
chemotherapy for tuberculosis includes isoniazid,
rifampin, ethambutol, and pyrazinamide for 2 months and
then isoniazid and rifampin for the next 4 months. Before
susceptibility data are available, more drugs may be added
to the first-line ones for patients who have previously had
tuberculosis or those in whom multidrug-resistant
tuberculosis is suspected. The added drugs normally
include an aminoglycoside (streptomycin, kanamycin, or
amikacin) or capreomycin (injectable agents), a
fluoroquinolone, and perhaps a second-line
antituberculosis agent such as cycloserine, ethionamide,
or para-aminosalicylic acid until we obtain one successful
strategy for achieving better treatment, it is known as
DOT“directly observed therapy,”.
First-line drugs
1) Isoniazide (INH):
It is hydrazide of isonicotinic acid the synthetic analogue
of pyridoxine. It is the most potent of the anti-tubercular
drugs, but is never given as a single agent in the treatment
of active tuberculosis.
Mechanism of action:
Is a prodrug that is activated by a mycobacterial catalase-
peroxidase (KatG). it inhibits the synthesis of mycolic
acids which is essential component of the mycobacterial
cell wall. Mycobacterium becomes resistance to drug by
reducing the ability of organism to accumulate the drug.
Kinetics:
Absorption of INH is readily after oral administration but
reduced in the presence of food and antacids thus it is
taken an hour before meals. Distribution is well into all
body fluid and tissues as CNS and CSF. Excretion is
mainly in the urine and also excreted in the saliva, sputum
and milk.
Antibacterial spectrum:
Isoniazid is specific for treatment of M. tuberculosis,
although Mycobacterium kansasii (an organism that
causes three percent of the clinical illness known as
tuberculosis) may be susceptible at higher drug levels.
When it is used alone, resistant organisms rapidly emerge.
Side effects
1) Allergic reaction including fever and skin rash.
2) Hepatitis occurs due to toxic metabolite which is the
monoacetylhydrazin. Incidence is increased by age.
3) Peripheral neuritis (paresthesia) is the most common
adverse effects due to a relative pyridoxine deficiency.
Most of the toxic reactions are corrected by pyridoxine
supplementation.
4) Drug interaction: INH can potentiate the adverse effects
of phenytoin because the INH inhibits metabolism of
phenytoin.
Unit 7: Chemotherapeutic Drugs
211
2) Rifamycins:
Rifampin, rifabutin
, and
rifapentine
are all considered to
be rifamycins, a group of structurally similar macrocyclic
antibiotics, which are first-line drugs for tuberculosis.
Any of these rifamycins must always be used in
conjunction with at least one other antituberculosis drug
to which the isolate is susceptible.
Rifampin:
It is a broad spectrum antimicrobial, active against G+ve
and G-ve cocci and some enteric bacteria, mycobacteria
(including M.tuberculosis and M.leprae) and Chlamydia.
Rifampin has a broader antimicrobial activity than
isoniazid . Because resistant strains rapidly emerge during
therapy, it is never given as a single agent in the treatment
of active tuberculosis.
Mechanism of action
Rifampin binds to the bacterial DNA dependent RNA
polymerase thus inhibiting RNA synthesis. Human RNA
is not affected. The administration of rifampin alone may
cause resistant to the mycobacteria. Resistance may be
due to chemical modification of microbial RNA-
polymerase.
Side effects
1) Harmless orange color to urine, sweat and tears.
2) Jaundice in patients with hepatic failure or alcoholics.
3) Nausea, vomiting, skin rashes and fever.
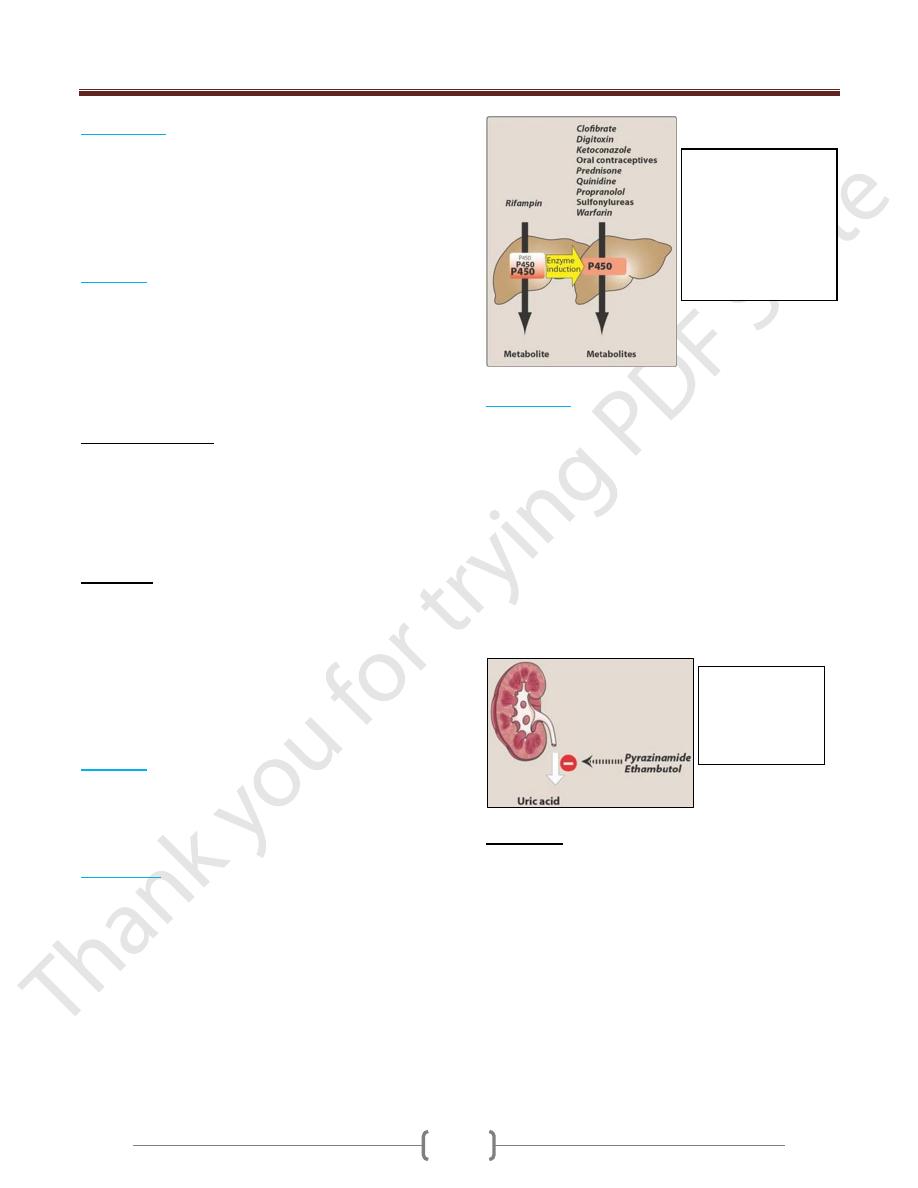
4) Rifampin can induce the cytochrome P-450, it can
decrease the half-lives of other drugs (as warfarin,
prednisone, oral contraceptives) that are coadministered
and metabolized by this system. This may lead to
higher dosage requirements for these agents.
Rifabutin:
it is a derivative of rifampin, is the preferred
drug for use in tuberculosis. it is a less potent inducer of
cytochrome P450 enzymes. Rifabutin has adverse effects
similar to those of rifampin but can also cause uveitis,
skin hyperpigmentation, and neutropenia.
Rifapentine:
it has activity comparable to that of
rifampin but has a longer half-life than rifampin and
rifabutin, which permits weekly dosing. However, for the
intensive phase (initial 2 months) of the short-course
therapy for tuberculosis, rifapentine is given twice
weekly. In the subsequent phase, rifapentine is dosed
once per week for 4 months. To avoid resistance issues,
rifapentine should not be used alone.
3)
Ethambutol
:
It is bacteriostatic and specific for most strains of
mycobacterium cell wall. Resistance is not a serious
problem if the drug is employed with other
antituberculous agents. Ethambutol is well absorbed
orally, well distributed to all body fluids even to CSF and
that is why used in tubercular meningitis.. Ethambutol
inhibits arabinosyl transferase—an enzyme that is
important for the synthesis of the mycobacterial
arabinogalactan cell wall. Resistance is not a serious
problem if the drug is employed with other antitubercular
agents Both parent drug and metabolites are excreted by
glomerular filtration and tubular secretion.
Side effects:
1) The most important side effect is optic neuritis, which
results in diminished visual acuity and loss of ability to
discriminate between red and green. Visual acuity should
be periodically examined. Discontinuation of the drug
results in reversal of the optic symptoms. In addition,
urate excretion is decreased by the drug; thus, gout may
be exacerbated.
2) May cause urate retention and gouty attacks.
Figure 34.8 Rifampin
induces cytochrome
P450, which can
decrease the half-
lives of
coadministered drugs
that are metabolized
by this system.
Pyrazinamide
and ethambutol
may cause urate
retention and
gouty attacks.
Unit 7: Chemotherapeutic Drugs
212
4) Pyrazinamide
: it is bactericidal to actively dividing
organisms. It is enzymatically hydrolyzed to pyrazinoic
acid which is the active form of the drug,
but the
mechanism of its action is unknown The drug is well
absorbed after oral administration from gut; well
distributed into body tissues including CSF. The main
side effects include hepatic toxicity and gouty attack due
to urate retention.
Second-line drugs:
A number of drugs aminosalicylic acid, ethionamide,
cycloserine are considered second-line drugs because they
are no more effective than the first-line agents and their
toxicities are often more serious.
1) Aminosalicylic acid
: it is derivative of salicylic acid with
similar structure to p-aminobenzoic acid (PABA). It is a
bacteriostatic agent that acts as a competitive inhibitor for
PABA in folate biosynthesis.
2) Ethionamide
: it is chemically related to isoniazid and
also blocks the synthesis of mycolic acids. It is effective
after oral administration and is widely distributed
throughout the body, including the CSF. Side effects that
limit its use include gastric irritation, hepatotoxicity,
peripheral neuropathies and optic neuritis.
3) Cycloserine
: it is orally effective tuberculostatic agent
appears to antagonize the step in bacterial cell wall
synthesis involving D-alanine. It distributes well
throughout body fluids, including CSF. Side effects:
peripheral neuropathy and CNS disturbances including
depression and psychotic reactions.
Drugs used in the treatment of leprosy:
Leprosy (Hansen’s disease) is caused by M.leprae. Bacilli
from skin lesions or nasal discharges of infected patients
enter susceptible individual via the skin or respiratory
tract. The recommended drug treatment by WHO is triple
drug regimen that consists of dapsone, clofazimine and
rifampin for at least 2 years and until skin biopsy is
negative for the causative bacilli.
1) Dapsone:
structurally similar to sulfonamides. It acts a
competitive inhibitor of folic acid synthesis. Dapsone is
also employed in the treatment of pneumocystis carinii in
HIV patients. Side effects include hemolysis especially in
patients with G-6PD deficiency, methemoglobinemia,
peripheral neuropathy and the possibility of developing
erythema nodosum leprosum.
2) Clofazimine
: it binds to DNA and inhibits template
function. It has anti-inflammatory effect that can prevent
erythema nodosum leprosum that happen with dapsone.
Adverse effects include a red-brown discoloration of the
skin and eosinophilic enteritis.
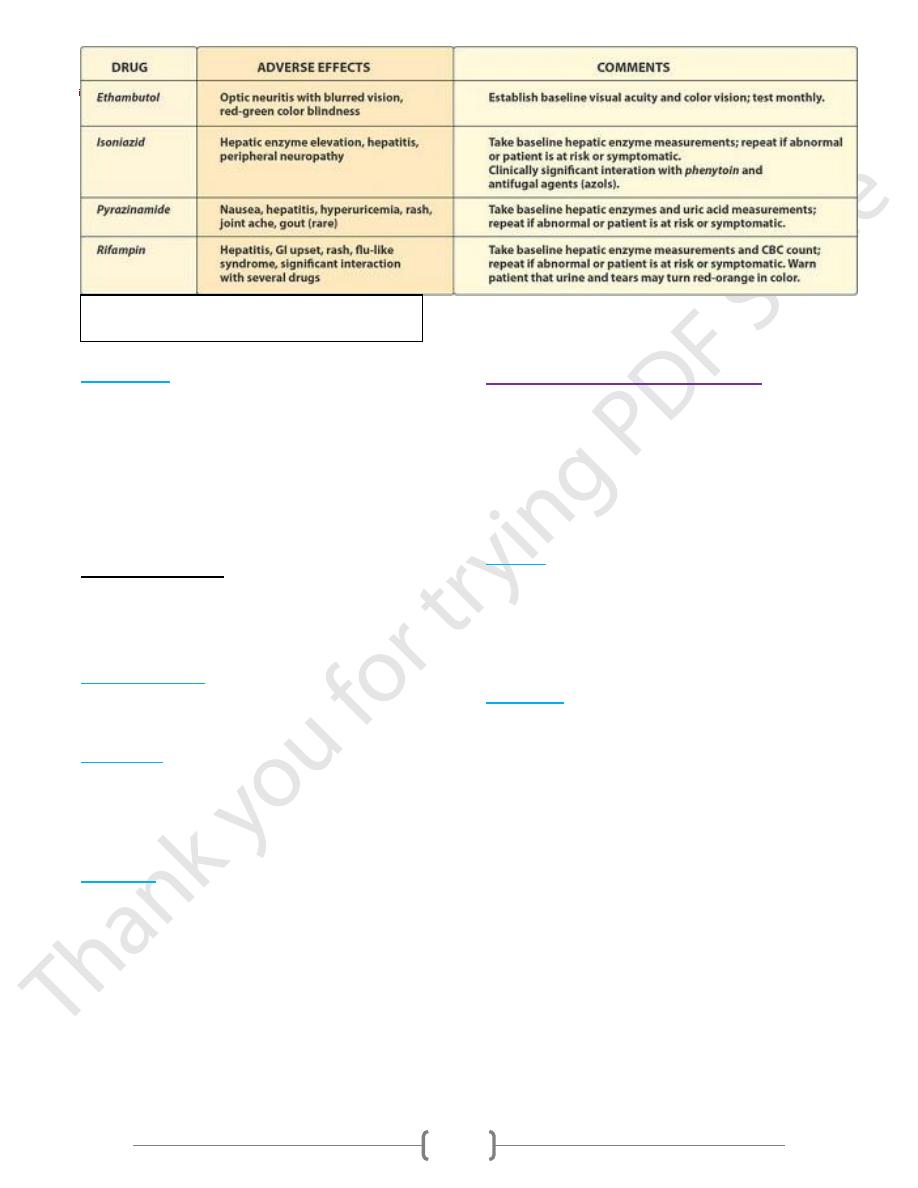
Some characteristics of first-line drugs used in
treating tuberculosis. CBC = complete blood count.
