Unit 8: Anti-inflammatory Drugs and Autacoids
844
Lecture 3+4 - Autacoids and
Autacoid Antagonists
Histamine
Autacoids (agonists and antagonists)
Are substances produced by a wide variety of cells in
body, having intense biological activity and generally
act locally at the site of synthesis and release.
Important Autacoids are: Histamine, 5-hydroxy-
tryptamine (5-HT, Serotonin), Bradykinin,
Prostaglandins (PGs), Plasma kinins, Angiotensin,
Slow reacting substances of anaphylaxis (SRS-A) and
platelet activating facter.
Histamine: Is a chemical mediator, which is
important in immune and inflammatory response. It
is synthesized and stored in most body tissues (e.g. the
skin and mucosal surfaces of the eye, nose, lungs, GI
tract and C.N.S). In these tissues, histamine is located
mainly in secretory granules of mast cells and
basophils.
Autacoids (agonists and antagonists)
Are substances produced by a wide variety of cells in
body, having intense biological activity and generally
act locally at the site of synthesis and release.
Important Autacoids are: Histamine, 5-hydroxy-
tryptamine (5-HT, Serotonin), Bradykinin,
Prostaglandins (PGs), Plasma kinins, Angiotensin,
Slow reacting substances of anaphylaxis (SRS-A) and
platelet activating facter.
Histamine: Is a chemical mediator, which is
important in immune and inflammatory response. It
is synthesized and stored in most body tissues (e.g. the
skin and mucosal surfaces of the eye, nose, lungs, GI
tract and C.N.S). In these tissues, histamine is located
mainly in secretory granules of mast cells and
basophils.
Histamine is discharged from mast cells and basophils
in
response to certain stimuli (e.g., allergic reactions,
cellular injury, bacterial toxin, trauma and extreme
cold). Allergies and anaphylaxis can also trigger
release of histamine.Various drugs can also release of
histamine (e.g tubocurarine, morphine) once released,
it diffuses rapidly into other tissues, where it interacts
with one or more of four types of histamine receptors
on target organs, called H
1
, H
2
, H
3
and H
4
receptors.
Inactivation of released histamine:
The inactivation of histamine is achieved by both:
1. Enzymatic metabolism
-histamine methyltransferase, the enzyme is present
in tissue but not in the blood.
-Diamine oxidase(histaminase), the enzyme is
present in tissues and in blood and it is present in
large concentration in food.
2. By transport processes that reduce the
concentration of the compound in the region of its
receptors.
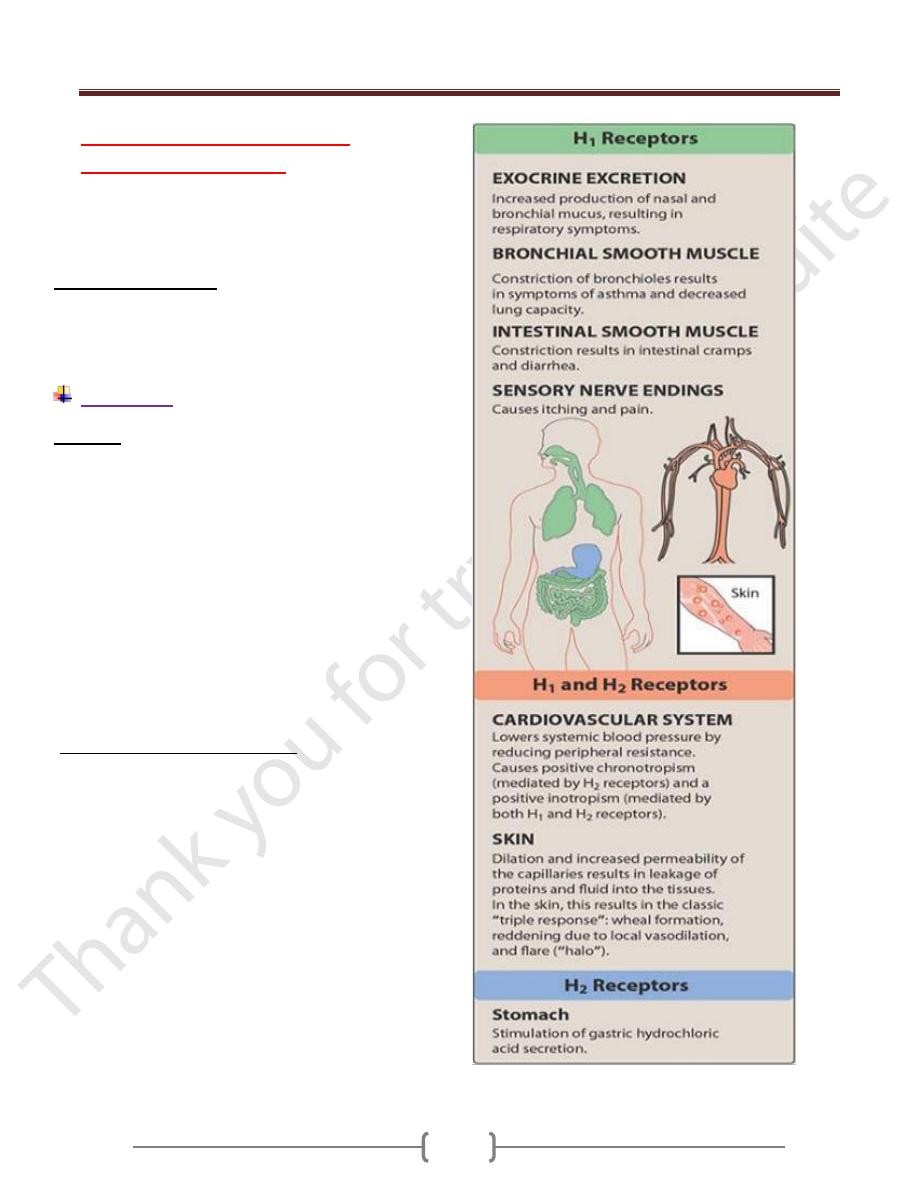
H
1
receptors are located mainly on smooth muscle
cells in blood vessels and the respiratory and GI
tracts. When histamine binds with these receptors
producing the following effects.
-Contraction of smooth muscle in the bronchi and
bronchioles producing bronchoconstraction.
-stimulation of vagus nerve endings to produce reflex
bronchoconstraction and cough.
Unit 8: Anti-inflammatory Drugs and Autacoids
842
-Increased permeability of veins and capillaries,
which allows fluid to flow into subcutaneous tissues
and form edema (little lower blood pressure).
-Increased secretion of mucous glands. Mucosal
edema and increased nasal mucus produce the nasal
congestion characteristic of allergic rhinitis and the
common cold.
-Stimulation of sensory peripheral nerve endings to
cause pain and pruritus.
Histamine promotes vasodilation by causing vascular
endothelium to release nitric oxide. This chemical
signal diffuses to the vascular smooth muscle, where
it stimulates cyclic guanosine monophosphate
production, causing vasodilation.
H
2
-receptors present mostly in gastric glands and
smooth muscle of some blood vessels. When receptors
are stimulated, the main effects are increased
secretion of gastric acid and pepsin, increased rate
and force of myocardial contraction.
The H
3
-receptor functions as a negative-feedback
mechanism to inhibit histamine synthesis and release
in many body tissues. Stimulation of H3 receptors
opposes the effects produced by stimulation of H1
receptors.
The H
4
- receptor is expressed in only a few cell types,
and their role in drug action is unclear.
Drugs cause release of histamine:
Many drugs can cause release of histamine in the
body.
-Intracutaneouse morphine injection in humans
produced localized redness, localized edema and a
diffuse redness. This is due to release of histamine.
-I.V. inj of curare may cause bronchial constriction
due to release of histamine.
-codeine , papaverine, meperidine (pethedine),
atropine, hydralizine and sympathomimetic amines,
histamine releases by these drugs may not be
significant unless they are administered I.V in large
doses
Pharmacological effects of histamine.
Histamine taken by month has essentially no effect
because it is altered by the intestinal bacteria, the
gastrointestinal wall and also in the liver. If injected
I.V. (0.1 mg of histamine) causes a sharp decline in
the blood pressure, flushing of the face and headache.
There is also stimulation of gastric acid secretion. If
this injection is given to an asthmatic individual,
there will be a marked decrease in vital capacity and
a sever
attack of asthma. When large dose of histamine are
administered I.V, Which can be done only in animal,
the blood pressure remains low for a considerable
length of time and there is a marked elevation of the
hematocrit reading. Histamine shock may cause fatal
termination
Circulatory effects of histamine:
The two factors involved in the circulatory action of
histamine are:
Arteriolar dilatation and
Capillary permeability
So it leads to loss of plasma from circulation.
The injection of as little as 10ug of the histamine drug
produces triple response of Lewis. This response
consists of:
Localized redness,localized edema and diffused
redness.
Histamine increases the rat and force of contraction
of the heart. Both H
1
and H
2
receptors are present in
the heart. Large doses of histamine causes nor-
epinephrine release from the heart.
Effect on gastric secretion:
Histamine is a potent stimulant of gastric Hcl
secretion. As little as 0.025mg of the drug injected
subcutaneauslly in human will cause marked
increase in Hcl secretion but few other effect in the
body.
Medical uses of histamine:
(No therapeutic uses but only diagnostic uses).
Histamine is useful as a diagnostic of a chlorhydria.
It is also used in diagnosis of Phenochromocytoma,
since it stimulates the output of catecholamines from
the adrenal medullary tumor which cause rise in
blood
pressure in stead of fall in B.P(dangerous test).
Subcutaneous injection of histamine may be used to
estimate the blood supply to an area.
Unit 8: Anti-inflammatory Drugs and Autacoids
842
Types of Anti-histamine drugs:
A- Selected H1 antagonist drugs:
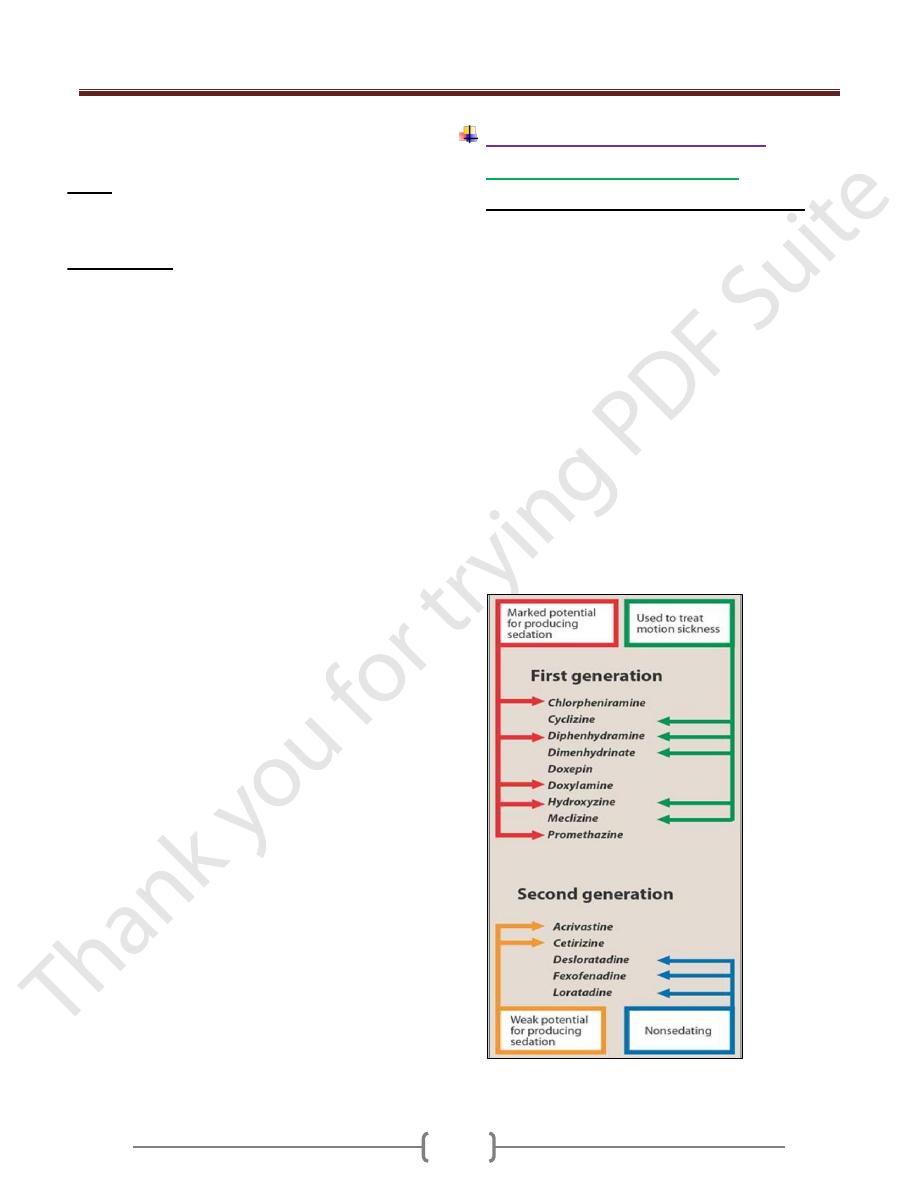
1) First-generation H1 receptor antagonists:
These drugs bind to both central and peripheral H
1
receptors and can cause CNS depression or stimulation.
They usually cause CNS depression (drowsiness,
sedation) with usual therapeutic doses and may cause
CNS stimulation (anxiety, agitation) with excessive doses,
especially in children. They also have Anticholinergic
effects (e.g. dry mouth, urinary retention, constipation,
blurred vision).
Chlorpheniramine (Histadin) & Dexchlorpheniramine
(Polaramine)
cause minimal drowsiness.
Diphenhydramine (Allermine),
the prototype of first
generation antihistamines causes a high incidence of
drowsiness and anticholinergic effects.
Promethazine (Phenergan)
is strong CNS depressants
and cause extensive drowsiness.
Cyproheptadine (Periactin).
It has the unusual effect of
increasing appetite, via an action on serotonin receptors in
hypothalamus (by blocking the serotonergic receptors).
Summary of therapeutic advantage and disadvantage of
some H
1
histamine-receptor blocking agents.
There is an agent which stimulate the gastric acid
secretion but has only 2% the potency of histamine, it
is called
Betazol: it is an isomer of histamine, it has less effect
than histamine on cardiovascular system and may be
safer for determination of gastric acidity, However
Betazol is dangerous to use in asthmatic patients.
Anti-Histamines:
The effect of histamine can be opposed in three ways:
1. Physiological antagonism: by using a drug to oppose
the effect (e.g adrenaline). Histamine constricts bronchi,
causes vasodilatation which increases capillary
permeability. Adrenaline opposes this effect by a
mechanism unrelated to histamine.
2. By preventing histamine from reaching its site of
action (receptors), By competition with H
1
-H
2
receptors
(Drug antagonisms).
3. By preventing the release of histamine. (adrenal
steroids and sodium-cromoglycate can suppress the
effect on the tissues)
Unit 8: Anti-inflammatory Drugs and Autacoids
842
2) Second-generation H
1
receptor antagonists
(non-sedating) agents:
They were developed mainly to produce less sedation
than the first generation drugs. They cause less CNS
depression because they are selective for peripheral H
1
receptors and do not cross the blood brain barrier.
Terfenadine:
is metabolized to the active metabolite
fexofenadine by a specific cytochrome P-450. This
enzyme is inhibited by certain antibiotic as by
erythromycin and antifungal agents (ketoconazole). The
parent drug can interfere with cardiac potassium channels
producing ventricular tachycardia.
Fexofenadine
: has been approved as a safer antihistamine
of this class
Loratadine:
has poor CNS penetration.
Acravistine and Cetirizine
: are not associated with
cardiac effect.
Astemizole
: there are reports of ventricular tachycardia
associated with astemizole.
Mechanism of action
Antihistamines are structurally related to histamine, which
prevents histamine from acting on target tissues . They
have no ability to block histamine release.
Indications for use
The drugs can relieve symptoms but don’t relieve
hypersensitivity.
1) Allergic rhinitis. Some relief of sneezing, rhinorrhea,
nasal airway obstruction and conjunctivitis are with the
use of antihistamine.
2) Anaphylaxis. Antihistamine is helpful in treating urticaria
and pruritus.
3) Allergic conjunctivitis. This condition, which is
characterized by redness, itching and tearing of the eyes.
4) Drug allergies. Antihistamines may be given to prevent
or treat reactions to drugs (e.g, before a dignostic test that
uses an iodine preparation).
5) Transfusions of blood and blood products.
6) Dermatologic conditions. Antihistamines are the drug of
choice for treatment of allergic contact dermatitis and
acute Urticaria. Urticaria often occurs because the skin
has many mast cells to release histamine.
7) Miscellaneous. Some antihistamines are commonly used
for non-allergic disorder such as motion sickness, nausea,
vomiting, sleep, cough or add to cough mixtures.
Contraindication to use:
Contraindication or must be used with caution in clients
with hypersensitivity to the drugs, narrow-angle
glaucoma, prostatic hypertroph, stenosing peptic ulcer,
bladder neck obstruction, during pregnancy and lactating
women (these drugs pass readily into breast milk and may
adversely affect newborn infant) .
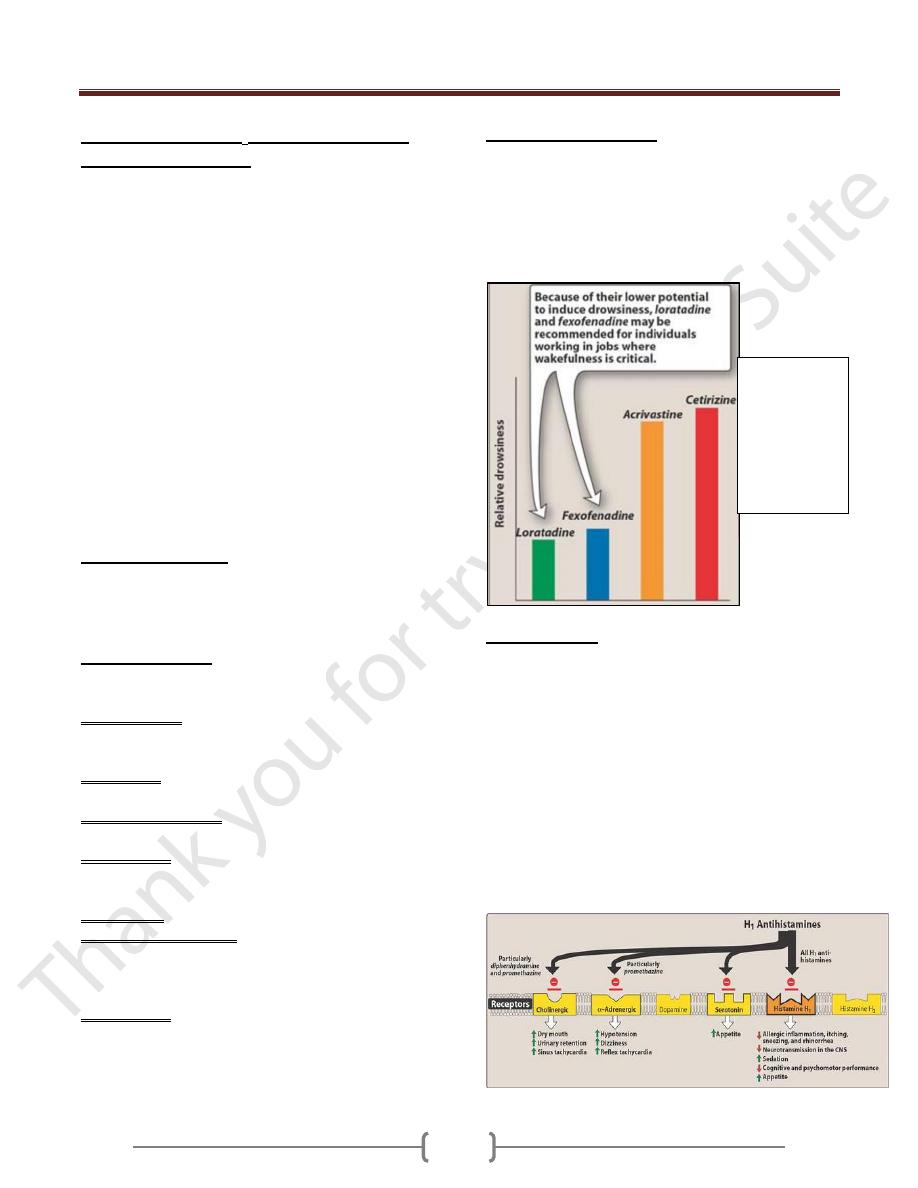
Adverse effects:
1) Drowsiness and sedation, some antihistamines appear to
cause more drowsiness and sedation than other.
2) Anticholinergic
3) Some antihistamines may cause dizziness, fatigue,
hypotention, headache, epigastric distress and
photosensitivity (exaggerated response to brief exposure
to the sun, resulting in moderatic distress and
photosensitivity (exaggerated response to brief exposure
to the sun, resulting in moderately sever to sun burn).
4) Even these drugs are used to treat allergy, but some time
may cause skin rash.
5) Serious adverse reaction including cardiac arrest & death,
have been reported in patients receiving high dose astemizole.
Effect of H
1
antihistamines
Relative
potential for
causing
drowsiness in
patients
receiving
second-
generation H
1
anti-histamines.
Unit 8: Anti-inflammatory Drugs and Autacoids
842
B- H
2
-receptor antagonists
These are Cimetidine
(Tagamate), Ranitidine (Zantac),
Fomatidine, Nizatidine
. All are equally effective in
producing healing, but they differ in structure and the
pharmacokinetic, potency and side effects.
Mechanism of action
Numerous factors influence acid secretion by the
stomach, including food, physiological condition and
drugs. H2 receptor blockers reduce basal acid-secretion
by about 95% and food stimulated acid-secretion by about
70%. Both conc. and vol. of H ions will decrease.
Pharmacokinetics:
1) They are all well absorbed after oral dose.
2) Antacids decrease their absorption in about 10-20%.
3) Peak serum conc. is reached within 1-2hrs.
4) All cross BBB and placenta and they are excreted in milk.
5) Bioavailabilty of
cimetidine, rantidine and fomatidine
is reduced to about 70% by 1st pass metabolism while
nizatidine has no 1st pass metabolism.
6) Efficacy is the same for all, but potency differs (different
doses are used).
Uses
Cimetidine
is used for conditions
In Which reduction of gastric secretion is beneficial,
these are in main duodenal ulcer, benign gastric ulcer,
stomach ulcer and reflux eosophagitis.
Is given before anesthesia in case of surgery and
before labor to decrease gastric acid.
Is also used to prevent peptic ulcer induced by
NSAIDs in high-risk patients e.g elderly patient.
Dose with
Cimetidine
, 400mgx2/day with breakfast and
at bedtime in case of peptic ulcer. Patients with duodenal
ulcer may receive 800mg as a single dose at bedtime.
Most patient become symptoms free in about 8dayes but
treatment should continuo for 6-8 weeks.
Dose for
rantidine
,
150mgx2/day. Taken in the morning
and in the evening. A single dose 300mgx2/day at
bedtime may be used as alternative for duodenal ulcer.
Treatment lasts at least 4 weeks. If the ulcer is not healed
at this duration of time, a further 4 weeks of therapy the
patient is needed.
Adverse effects:
Are few in short term uses, but more with high term uses,
includes-headache, dizziness, constipation, diarrhoea,
tiredness and muscular pain. H
3
-receptor agonists and
antagonists are being investigated, but none is available
for clinical use.
Serotonin or 5-hydroxytryptamine (5-HT)
It is a neurotransmitter, widely distributed in the CNS,
beginning in the midbrain and projecting into thalamus,
hypothalamus, cerebral cortex, and spinal cord. CNS
serotonin is usually an inhibitory neurotransmitter and is
associated with mood, the sleep-wake cycle. Serotonin is
thought to produce sleep by inhibiting CNS activity. In
the blood, 5-HT is present in high concentration in
platelets (regulator of platelets function) and also high
concentration in intestine. There are 7 molecular subtype
receptors. Some of these types used for treatment of acute
migraine attack and anxiety.
Biosynthesis:
The biosynthesis of 5-HT follows a pathway similar to
that of nor-adrenaline, except that the precursor amino
acid is tryptophan instead of tyrosin. Tryptophan is
converted to 5-hydroxy trytophan by tryptophan
hydroxylase then to 5-hydroxytryptamine by dopa-
decarboxylase.
Degradation:
Occurs mainely by MAO, forming 5-hydroxyindolacetic
acid (5-HIAA), which is excreted in urine.
Pharmacological effects:
Smooth muscles. 5-HT stimulates the G.I smooth muscle;
it increases the peristaltic movement of intestine.
Serotonin contracts the smooth muscle of bronchi; this
contraction effect is less than the effect of histamine.
Blood vessels. If serotonin is injected i.v, the blood
pressure usually first rises, because of the contraction of
large vessels and then falls because of arteriolar dilatation.
Serotonin causes aggregation of platelets.
Classification of serotonin receptors.
There are 7 types of serotonin receptors:
1) 5-HT1 receptors (5-HT1A, B, C & D)
Occur mainly in CNS. Effects are neurotransmitter
inhibition, contraction and relaxation of smooth muscles.
Specific agonists
Include: 5HT has no clinical application as a drug.
o
Sumatriptan
a selective 5-HT1D used in treatment of
acute migraine.
o
Buspirone
a selective 5-HT1A used in anxiety (it has
non-benzodiazepine anxiolytic activity).
o
Ergotamine
is a partial agonist used in migraine. It
acts on 5-HT1A receptor.
Nonspecific 5-HT receptor agonist
o
Dexfenfluramine
used as appetite suppressant.
Unit 8: Anti-inflammatory Drugs and Autacoids
842
Specific antagonists
o
Spiperone
(acts on 1A receptor) and
o
Methiothepin
(acts on 1A, 1B, 1D receptors).
2) 5-HT2 (2A, 2B and 2C receptors)
Occurs in CNS and many peripheral sites.
Specific ligand
o
Lysergide
(LSD) [agonist in CNS (main effect
behavioural), antagonist in periphery main effect smooth
muscle contraction]
Specific antagonists
o
Ketanserin
: it blocks 5-HT1C, 5-HT2A , and vascular
α
1
adrenoreceptor. It prevents platelets aggregation by
blocking 5-HT
2
receptors on platelets.
o
Ritanserin
. 5HT2 antagonist with a little or no effect
α
effect.
o Cyproheptadine.
3) 5-HT3 receptors
Occur in peripheral nervous system. Effects are excitatory
Specific agonists
2-methyl-5-HT.
Specific antagonists
o
Ondansetron
used to prevent nausea and vomiting
associated with cancer chemotherapy.
o
Granisetron
can reduce or prevent sever nausea and
vomiting associated with cancer chemotherapy.
4) 5-HT4 receptors
Occur mainly in the enteric nervous system (also in CNS).
Effects are excitatory, causing increase G.I motility.
Specific agonist
o
Metoclopramide
(used to stimulate gastric emptying).
5)
Little is known so far about the functions & pharmacology
of
5-HT5-7 receptors
. Many new receptors selective
agonists and antagonists are being developed.
BradyKinin
An endogenous vasodilator occurring in blood vessel
walls, it has an effect somewhat similar to the histamine
on vascular smooth muscles, bronchial and intestinal
smooth muscles. At least two distinct receptor types, B1
and B2, appear to exist for BradyKinin.
Roles of bradykinin:
1) Mediator of inflammation and pain.
2) Regulation of microcirculation.
3) Their production is interrelated with clotting and
fibrinolysin systems.
4) Responsible for circulatory change after birth.
5) Involved in shock and some immune reactions.
Kinins
Peptide that are mediated in the inflammation.
Action of kinin:
On CVS: vasodilatation in the kidneys, heart,
intestine, skin, and liver. It is 10 times active than
histamine as vasodilator.
On exocrine and endocrine glands: kinin modulate
the tone of pancreas and salivery glands and help
regulate GIT motility, also affect the transport of water
and electrolytes, glucose and amino acids through
epithelial cell transport. They regulate transport of
substrates through kidneys and GIT.
Angiotensin
It is generated in the plasma from a precursor plasma
globulin. It is involved in the electrolyte balance, plasma
volume and B.P.
Angiotensin I:
Renin is an enzyme produced by the kidney in response to
a number of factors including adrenergic activity (β
1
-
receptor) and sodium depletion. Renin converts a
circulating glycoprotein (angiotensinogen) into an
inactive material angiotensin-I. It gets activation during
passage through pulmonary circulation to angiotensin II
by (ACE). ACE is located on the luminal surface of
capillary endothelial cells, particularly in the lungs & also
present in many organ (e.g brain).
Angiotensin II:
Is an active agent, has a vasoconstrictor action on blood vessels
& sodium and water retention. Vasoconstriction effect by
direct action. It is more potent presser agent than NA
Eicosanoid compounds
They are very large family of compounds with a wide
spectrum of biological actions. They have very short half-
life (seconds to minutes). Most important of these
compounds are:
Prostaglandines, Leukotriens and Thromboxanes.
They are produced in minute amounts by all cells except
RBCs and they act locally at the same site of synthesis.
These agents have many physiological processes as
mediators and modulators of inflammatory reactions.
They are inactivated locally by the tissues.
Unit 8: Anti-inflammatory Drugs and Autacoids
822
Prostaglandines:
The Prostaglandines (PG
s
), so named because they were
first isolated from seminal fluid, represent a series of
acidic lipids having powerful pharmacological activity.
Many series of compounds are present; starting from PGA
to I. Practically every cell in the body is capable of
synthesizing one or more types of PG
S
. The four major
group of PG
s
are E, F, A, and B.
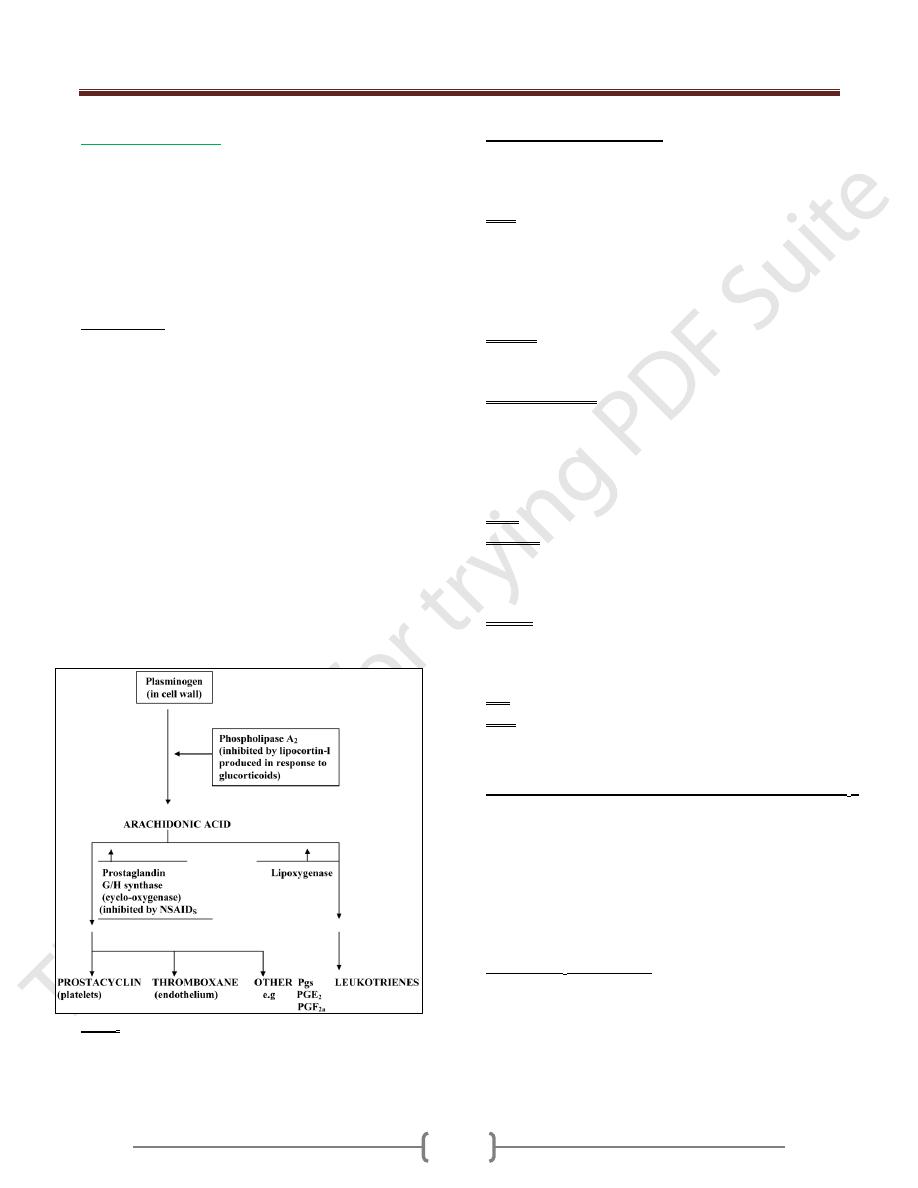
Biosynthesis:
There are no performed stores of PG
s
. They are
synthesized locally by the release of Arachidonic acid
from tissue phospholipids by the action of phospholipase
A
2
of the cell walls, in response to appropriate stimuli. So
the Arachidonic acid is the source of Eicosanoids.
Glucocorticoids prevent the formation of arachidonic
acid by inducing the synthesis of an inhibitory
polypeptide called lipocortin-1; the capacity to inhibit the
subsequent formation of both prostaglandins and
leukotrienes.
Arachidonic acid is further metabolised by cyclo-
oxygenase (COX, also called PGH synthase), which
changes the linear fatty acids into the cyclical structures
of the prostaglandins. This reaction is blocked by NSAID
s
as aspirin.
Note: The inhibition of cyclo-oxygenase enzyme by
NSAID
s
leaving Leukotriences which will be formed
more since all the formed Arachidonic acid is shifted
toward their synthesis.
Pharmacological actions:
The mechanism of action of PG
s
involve for the
stimulation of cyclic
AMP
production and calcium use by
various cells.
CVS
PGE
2
acts as vasodilator; it is more potent hypotensive
than Ach and histamine.
PGI
2
acts as vasodilator more potent hypotensive than PGE
2.
Thromboxane A
2
and PGF
2α
act mostly as
vasoconstrictor (especially in veins).
Uterous
PGE
2
and PGF
2α
Contract human uterus (that means
intiation and progression of labour).
Bronchial muscle
PGF
2α
and thromboxan A
2
cause bronchial muscle
contraction. PGE
2
& PGI
2
cause bronchial muscle dilatation
(so asthma some time happen due to imbalance between the
dilatation & contraction effect of PG
s
. so Aspirin can
induce asthma in some persons & relive in others.
GIT: PGE
2
and PGF
2α
cause colic and watery diarrhoea.
Platelets
Thromboxan A
2
is potent induce of platelets aggregation
PGI
2
is potent anti-aggregation to the platelets while
PGE
1
and PGI
2
inhibit platelet aggregation.
Kidney
PGE
2
and PGI
2
increase water, Na ion and K ion excretion
(act as diuresis) that cause renal vasodilatation and inhibit
tubular reabsorption.
Eye: PGE
2
and PGF
2α
cause miosis.
CNS
Fever: PGE
1
and PGE
2
increase the body temperature
Sleep: PGD
2
when infused into cerebral ventricles induces sleep
“Diseases assoociated with excess production of PG
s
”
Various diseases may be associated with excessive PG
s
production. So it is possible to improve the patients from
such diseases by prostaglandin synthase inhibitor.
Some of these diseases as dysmenorrhea, Bartters
syndrome, threatened abortion, pancreatic cholera,
hypercalcemia of cancer, idiopatheic orthostatic
hypotention and inflammation.
Uses of PG
s
in medicine
1) PGI
2
:
Epoprostenol
(inhibits platelets aggregation)
2) PGE
1
:
Alprostadil
(used to maintain the potency of
arterioles in neonates with congenital heart defects).
3) PGE
2
:
Dinoproste
(used as pessaries to induce labor)
4) Synthetic analogue of PGE
1
:
Misoprostol
(inhibit the
secretion of HCl).
