Unit 2: Bacteriology
91
Lecture 5 - Anaerobic Spore-Former
Bacteria (Pathogenic Clostridia)
The genus Clostridium consists of relatively large,
Gram-positive, rod-shaped bacteria. All species
form endospores and have a strictly fermentative type
of metabolism. Most clostridia will not grow under
aerobic conditions and vegetative cells are killed by
exposure to O
2
, but their spores are able to survive long
periods of exposure to air.
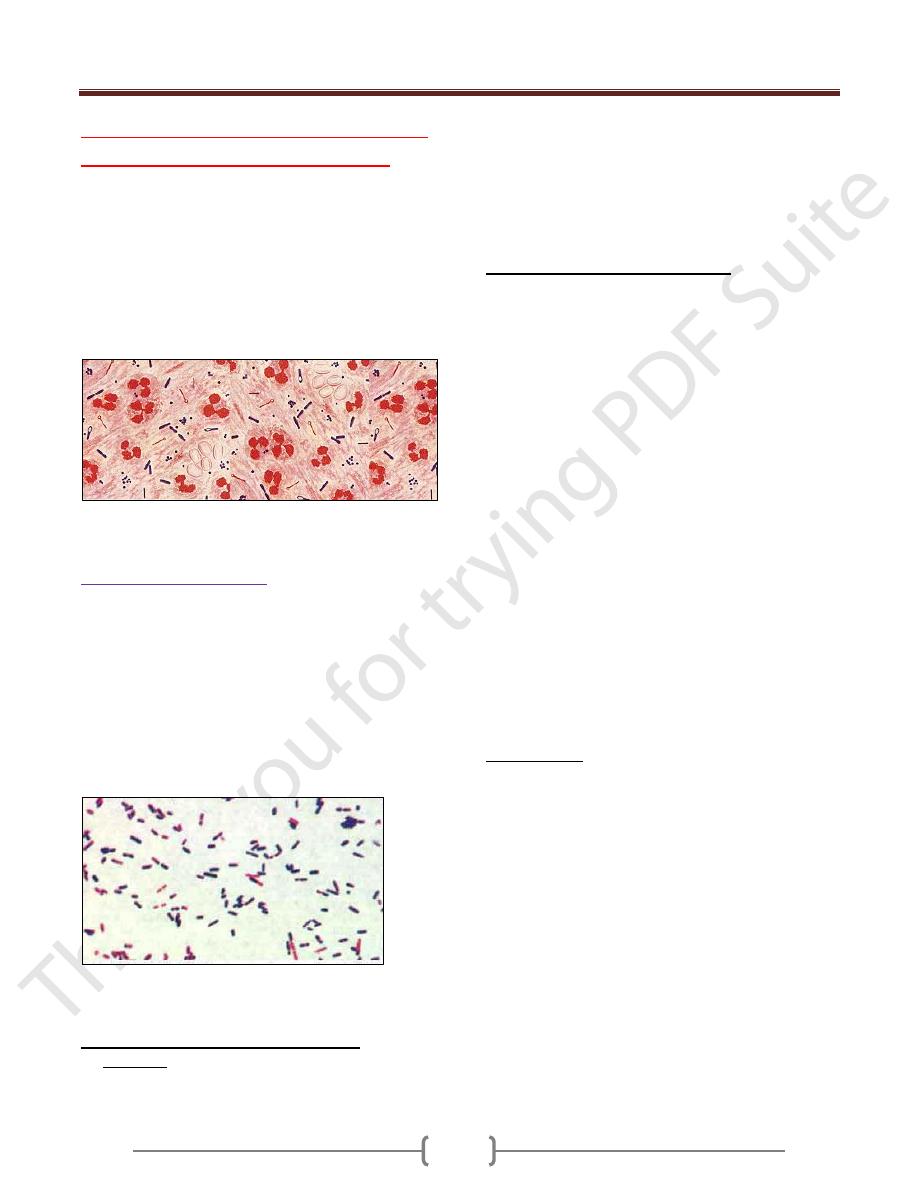
Stained pus from a mixed anaerobic infection. At least
three different clostridia are apparent
Clostridium perfringens
:
Clostridium perfringens (formerly known as
Clostridium welchii) is a Gram-positive, rod-shaped,
anaerobic, spore-forming bacterium of the genus
Clostridium. C. perfringens is ubiquitous in nature and
can be found as a normal component of decaying
vegetation, marine sediment, the intestinal tract of humans
and other vertebrates, insects, and soil. Virtually every
soil sample ever examined, with the exception of the
sands of the Sahara, has contained C. perfringens.
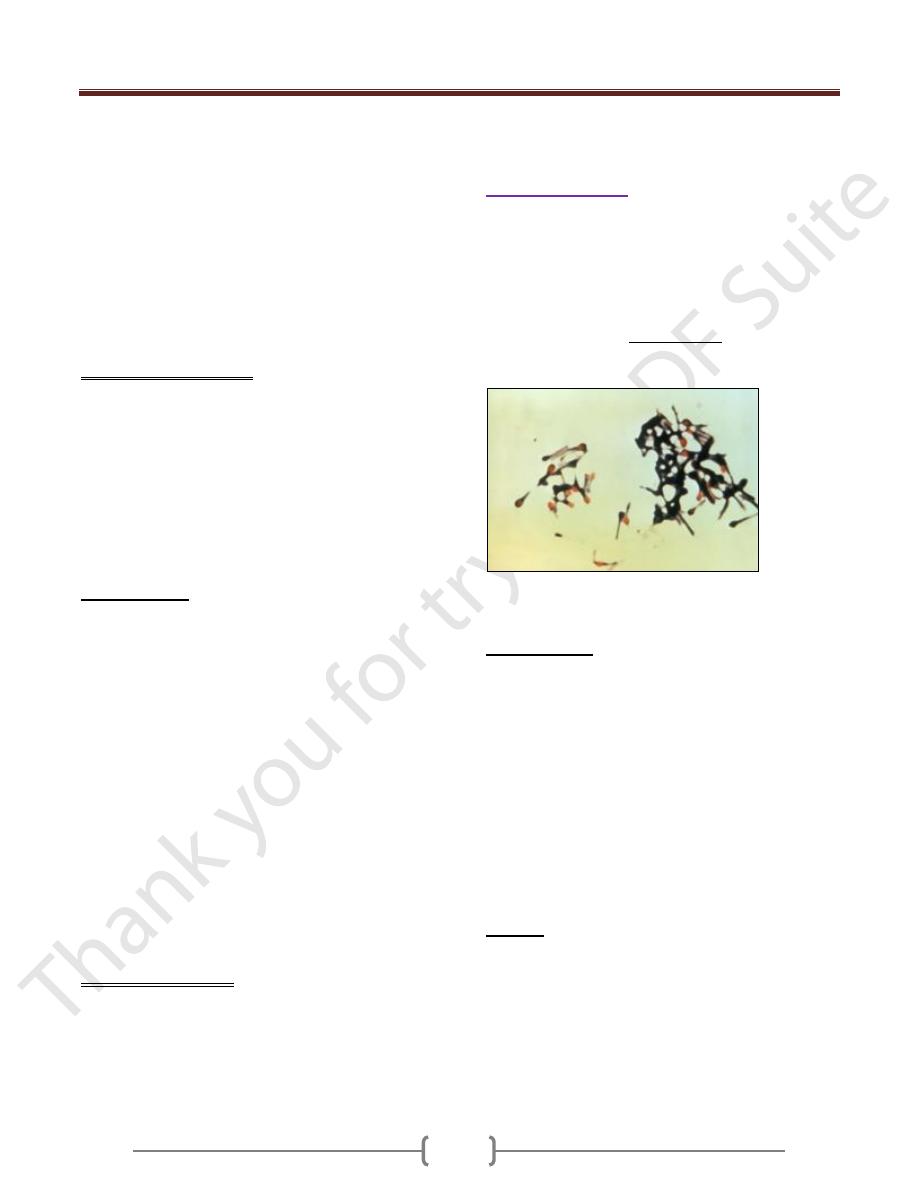
Photomicrograph of large, Gram-positive, rod-shaped
Clostridium perfringens bacilli.
Morphology and Colony characteristics
On blood agar plates, C. perfringens grown anaerobically
produces β-haemolytic, flat, spreading, rough, translucent
colonies with irregular margins. A Nagler agar plate,
containing 5-10% egg yolk, is used to presumptively
identify strains which produce α-toxin, a diffusible
lecithinase which interacts with the lipids in egg yolk to
produce a characteristic precipitate around the colonies.
One half of the plate is inoculated with antitoxin to act as
a control in the identification.
Pathogenesis and Clinical Finding:
Clostridium perfringens, which produces a huge array of
invasins and exotoxins, causes wound and surgical
infections that lead to gas gangrene, in addition to severe
uterine infections. Clostridial hemolysins and
extracellular enzymes such as proteases, lipases,
collagenase and hyaluronidase, contribute to the
invasive process. Clostridium perfringens also produces
an enterotoxin and is an important cause of food
poisoning. Usually the organism is encountered in
improperly sterilized (canned) foods in which endospores
have germinated. C. perfringens is commonly
encountered in infections as a benign component of the
normal flora. In this case, its role in disease is minor.
Infections due to C. perfringens show evidence of tissue
necrosis, bacteremia, emphysematous cholecystitis, and
gas gangrene, which is also known as clostridial
myonecrosis. The toxin involved in gas gangrene is
known as α-toxin, which inserts into the plasma
membrane of cells, producing gaps in the membrane
which disrupt normal cellular function. The action of
C. perfringens on dead bodies is known to mortuary
workers as tissue gas and can only be halted by
embalming.
Gas gangrene:
Is a bacterial infection that produces gas within tissues in
gangrene. It is a deadly form of gangrene usually caused
by Clostridium bacteria. It is a medical emergency. Gas
gangrene generally occurs at the site of trauma or a recent
surgical wound. The onset of gas gangrene is sudden and
dramatic. About a third of cases occur on their own.
Patients who develop this disease in this manner often
have underlying blood vessel disease (atherosclerosis or
hardening of the arteries), diabetes, or colon cancer.
Clostridium perfringens produces many different toxins,
four of which (alpha, beta, epsilon, iota) can cause
potentially deadly syndromes. The toxins cause damage to
tissues, blood cells, and blood vessels. Gas gangrene is
marked by a high fever, brownish pus, gas bubbles
under the skin, skin discoloration, and a foul odor.
Pathophysiology of Gas gangrene is caused by exotoxin-
producing Clostridial species (most often Clostridium
Unit 2: Bacteriology
92
perfringens, but less commonly C. septicum or
C. ramnosum ), which are mostly found in soil but also
found as normal gut flora, and other anaerobes (e.g.
Bacteroides and anaerobic streptococci). The exotoxin is
commonly found in C. perfringens type A strain and is
known as alpha toxin. These environmental bacteria may
enter the muscle through a wound and go on to
proliferate in necrotic tissue and secrete powerful
toxins. These toxins destroy nearby tissue, generating gas
at the same time. Other organisms may rarely cause gas
gangrene (for example, Klebsiella pneumoniae in the
context of diabetes).
Treatment of gas gangrene
Treatment of gas gangrene is usually by
amputation
if necessary in many cases.
alone are not effective because they do not
penetrate ischaemic
However,
penicillin
is given as an adjuvant treatment to
surgery
. In addition to surgery and antibiotics,
(HBOT) is used and acts to
inhibit the growth of and kill the anaerobic C.
perfringens.
Food poisoning
Some strains of C. perfringens produce toxins (which
cause gas gangrene) if ingested. In the United Kingdom
and United States they are the third most common cause
of food-borne illness, with poorly prepared meat and
poultry the main culprits in harboring the bacterium. The
clostridial enterotoxin mediating the disease is often heat-
resistant and can be detected in contaminated food and
feces. Incubation time is between 6 and 24 (commonly
10-12) hours after ingestion of contaminated food.
Manifestions typically include abdominal cramping and
diarrhea - vomiting and fever are unusual. The whole
course usually resolves within 24 hours. Very rare, fatal
cases of clostridial necrotizing enteritis have been
known to involve "Type C" strains of the organism,
which produce a potently ulcerative β-toxin. It is likely
that many cases of C. perfringens food poisoning remain
subclinical, as antibodies to the toxin are common
amongst the population.
Treating food poisoning:
In most cases, food poisoning
can be treated at home without seeking medical advice. It
is very important that the patient do not become
dehydrated because it will make him feel worse and slow
down his recovery. Oral rehydration salts (ORSs) are
recommended for people vulnerable to the effects of
dehydration, such as the elderly and those with a pre-
existing health condition.
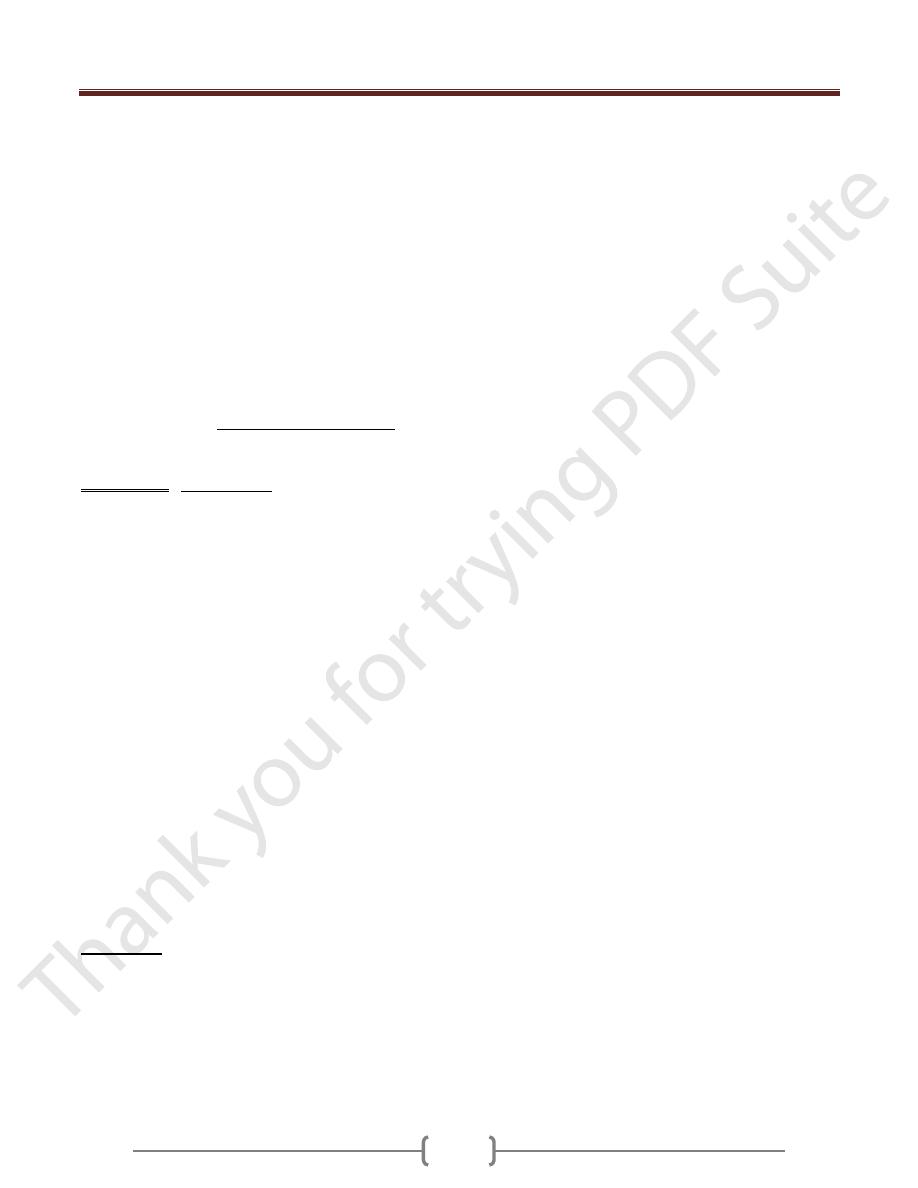
Clostridium tetani
Clostridium tetani is a rod-shaped, anaerobic bacterium
of the genus Clostridium. Like other Clostridium species,
it is Gram-positive, and its appearance on a gram stain
resembles tennis rackets or drumsticks. C. tetani is
found as spores in soil or as parasites in the
gastrointestinal tract of animals. C. tetani produces a
potent biological toxin, tetanospasmin, and is the
causative agent of tetanus.
Clostridium tetani with characteristic 'tennis racket'
appearance.
Characteristics
C. tetani is a rod-shaped, obligate anaerobe which stains
Gram positive in fresh cultures; established cultures may
stain Gram negative. During vegetative growth, the
organism cannot survive in the presence of oxygen, is
sensitive to heat and has flagella which provide limited
mobility. As the bacterium matures, it develops a
terminal spore, which gives the organism its
characteristic appearance. C. tetani spores are extremely
hardy and are resistant to heat and most antiseptics.
The spores are distributed widely in manure-treated soils,
and can also be found on human skin and in contaminated
heroin .
Toxicity
C. tetani usually enters a host through a wound to the skin
and then it replicates. Once an infection is established, C.
tetani produces two exotoxins, tetanolysin and
tetanospasmin. Eleven strains of C. tetani have been
identified, which differ primarily in flagellar antigens
and in their ability to produce tetanospasmin. The genes
that produce toxin are encoded on a plasmid which is
present in all toxigenic strains, and all strains that are
Unit 2: Bacteriology
93
capable of producing toxin produce identical toxins.
Tetanolysin serves no known function to C. tetani, and the
reason the bacteria produce it is not known with certainty.
Tetanospasmin is a neurotoxin and causes the clinical
manifestations of tetanus. Tetanus toxin is generated in
living bacteria, and is released when the bacteria lyses,
such as during spore germination or during vegetative
growth. A minimal amount of spore germination and
vegetative cell growth are required for toxin production.
On the basis of weight, tetanospasmin is one of the most
potent toxins known. The estimated minimum human
lethal dose is 2.5 nanograms per kilogram of body
weight, or 175 nanograms in a 70 kg (154 lb) human. The
only toxins more lethal to humans are botulinum toxin,
produced by close relative Clostridium botulinum and the
exotoxin produced by Corynebacterium diphtheriae, the
causative agent of diphtheria.
Toxin Action: Tetanospasmin is distributed in the blood
and lymphatic system of the host. The toxin acts at
several sites within the central nervous system,
including peripheral nerve terminals, the spinal cord,
and brain, and within the sympathetic nervous system.
The toxin is taken up into within the nerve axon and
transported across synaptic junctions, until it reaches the
central nervous system, where it is rapidly fixed to
gangliosides at the presynaptic junctions of inhibitory
motor nerve endings. The clinical manifestations of
tetanus are caused when tetanus toxin blocks inhibitory
impulses, by interfering with the release of
neurotransmitters, including glycine and gamma-
aminobutyric acid. This leads to unopposed muscle
contraction and spasm. Characteristic features are Risus
Sardonicus (a rigid smile), Trismus (commonly known
as lock-jaw), and Opisthotonus (rigid, arched back).
Seizures may occur, and the autonomic nervous system
may also be affected. Tetanospasmin appears to prevent
the release of neurotransmitters by selectively cleaving
a component of synaptic vesicles called synaptobrevin
II.
Treatment:
When a tetanus infection becomes established, treatment
usually focuses on controlling muscle spasms, stopping
toxin production, and neutralizing the effects of the
toxin. Treatment includes administration of tetanus
immune globulin (TIG), which comprises antibodies
that inhibit tetanus toxin (also known as tetanus
antitoxins), by binding to and removing unbound
tetanus toxin from the body. Binding of the toxin to the
nerve endings appears to be an irreversible event, and
TIG is ineffective at removing bound toxin. Large doses
of antibiotic drugs (such as metronidazole or
intramuscular penicillin G) are also given once tetanus
infection is suspected, to halt toxin production.
Prevention of tetanus includes vaccination, and
cleaning the primary wound. Prophylaxis is effective,
in the form of a tetanus toxoid vaccine, which is given
with or without passive immunization with tetanus
immune globulin. Very few cases of tetanus have
occurred in individuals with up-to-date tetanus
vaccinations. DPT vaccine (diphtheria-pertussis-tetanus)
may provide protection from tetanus for many years (
about 10 years), and every 10 years thereafter, a booster
shot of tetanus vaccine is recommended. Tetanus is not
contagious from person to person, and is the only
vaccine-preventable disease that is infectious but not
contagious. A C.tetani infection does not result in
tetanus immunity, and tetanus vaccination should be
given as soon as the patient has stabilized.
Unit 2: Bacteriology
94
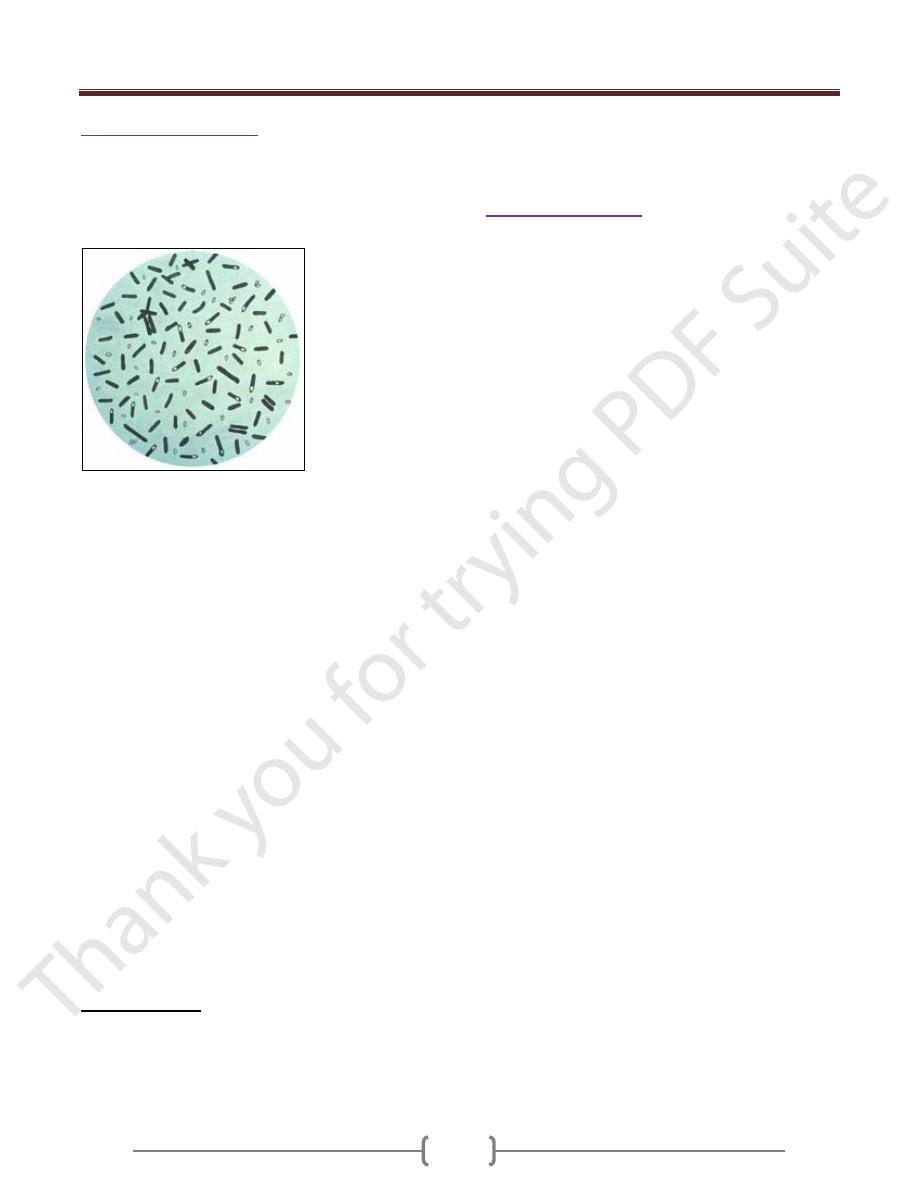
Clostridium botulinum
Clostridium botulinum is a Gram-positive, rod shaped
bacterium that produces the neurotoxin botulin, which
causes the flaccid muscular paralysis seen in botulism.
It is also the main paralytic agent in botox.
C. botulinum stained with gentian violet
It is an anaerobic spore-former, which produces oval,
subterminal endospores and is commonly found in soil.
C. botulinum is arod-shaped microorganism. It is an
obligate anaerobe, meaning that oxygen is poisonous to
the cells. However, they tolerate very small traces of
oxygen due to an enzyme called superoxide dismutase
(SOD) which is an important antioxidant defense in
nearly all cells exposed to oxygen. Under unfavorable
circumstances they are able to form endospores that
allow them to survive in a dormant state until exposed to
conditions that can support their growth. In laboratory the
microorganism is usually isolated in Tryptose Sulfite
Cycloserine (TSC) growth media, always in an anaerobic
environment with less than 2% of Oxygen. This can be
achieved by several commercial kits that use a chemical
reaction to replace O
2
with CO
2
(E.J. GasPak System). C.
botulinum is lipase negative microorganism, it grows
between pH values of 4.8 and 7 and it can't use lactose
as a primary carbon source, characteristics important
during biochemical identification. C. botulinum strains
that do not produce a botulin toxin are referred to as
Clostridium sporogenes. The complete genome of C.
botulinum has now been sequenced.
Phenotypic types
The current nomenclature for C. botulinum recognises
four physiological groups (I-IV). This is mostly based
on the ability of the organism to digest complex proteins.
Most outbreaks of human botulism are caused by group I
(proteolytic) or II (non-proteolytic) C. botulinum.
Group III organisms mainly cause diseases in animals.
There has been no record of Group IV C. botulinum
causing human or animal disease.
Clostridium difficile
This bacterium is a very important cause of diarrhea and
more severe intestinal disease in people, and is also
possibly an important cause of diarrhea in some animals
(dogs and cats). Clostridium difficile toxin A is a toxin
generated by Clostridium difficile. It is usually described
as a enterotoxin, but it also has some activity as a
cytotoxin. C. difficile occurs in the fecal flora of 1–4%
of healthy adults and in 30–50% of children during the
first year of life. The factors that lead to development of
the disease are not known with certainty. Cases of
pseudomembranous colitis are observed frequently
under treatment with clindamycin, aminopenicillins, and
cephalosporins (hence the designation antibiotic-
associated colitis), but also occur in persons not taking
antibiotics. Occasional outbreaks are seen in hospitals.
The pathological mechanism is based on formation of two
toxins. Toxin A is an enterotoxin that causes a
dysfunction characterized by increased secretion of
electrolytes and fluids. Toxin B is a cytotoxin that
damages the mucosa of the colon.
The clinical course
includes fever, diarrhea, and spasmodic abdominal
pains. Coloscopy reveals edematous changes in the colon
mucosa, which is also covered with yellowish-whitish
matter. Laboratory diagnosis involves culturing the
pathogen from patient stool and detection of the
cytotoxin in bacteria-free stool filtrates on the basis of a
cytopathic effect (CPE) observed in cell cultures, which
CPE is then no longer observed after neutralization with
an antiserum. Toxins A and B can also be detected with
immunological test kits (ELISA tests). A specific therapy
is not required in many cases. Antibiotic treatment is
indicated in severe cases. The agent of choice is currently
metronidazole.
