Unit 2: Bacteriology
95
Lecture 6 – Corynebacterium &
Diphtheroid
Corynebacteria are Gram-positive, aerobic, nonmotile,
rod-shaped bacteria classified as Actinobacteria.
Corynebacteria are related phylogenetically to
mycobacteria and actinomycetes. They do not form
spores or branch as do the actinomycetes, but they have
the characteristic of forming irregular, club-shaped or
V-shaped arrangements in normal growth. They undergo
snapping movements just after cell division, which
brings them into characteristic forms resembling Chinese
letters or palisades. The genus Corynebacterium consists
of a diverse group of bacteria including animal and
plant pathogens, as well as saprophytes. Some
corynebacteria are part of the normal flora of humans,
finding a suitable niche in virtually every anatomic site,
especially the skin and nares. The best known and most
widely studied species is Corynebacterium diphtheriae,
the causal agent of the disease diphtheria.
Corynebacterium diphtheriae:
Morphology and culturing
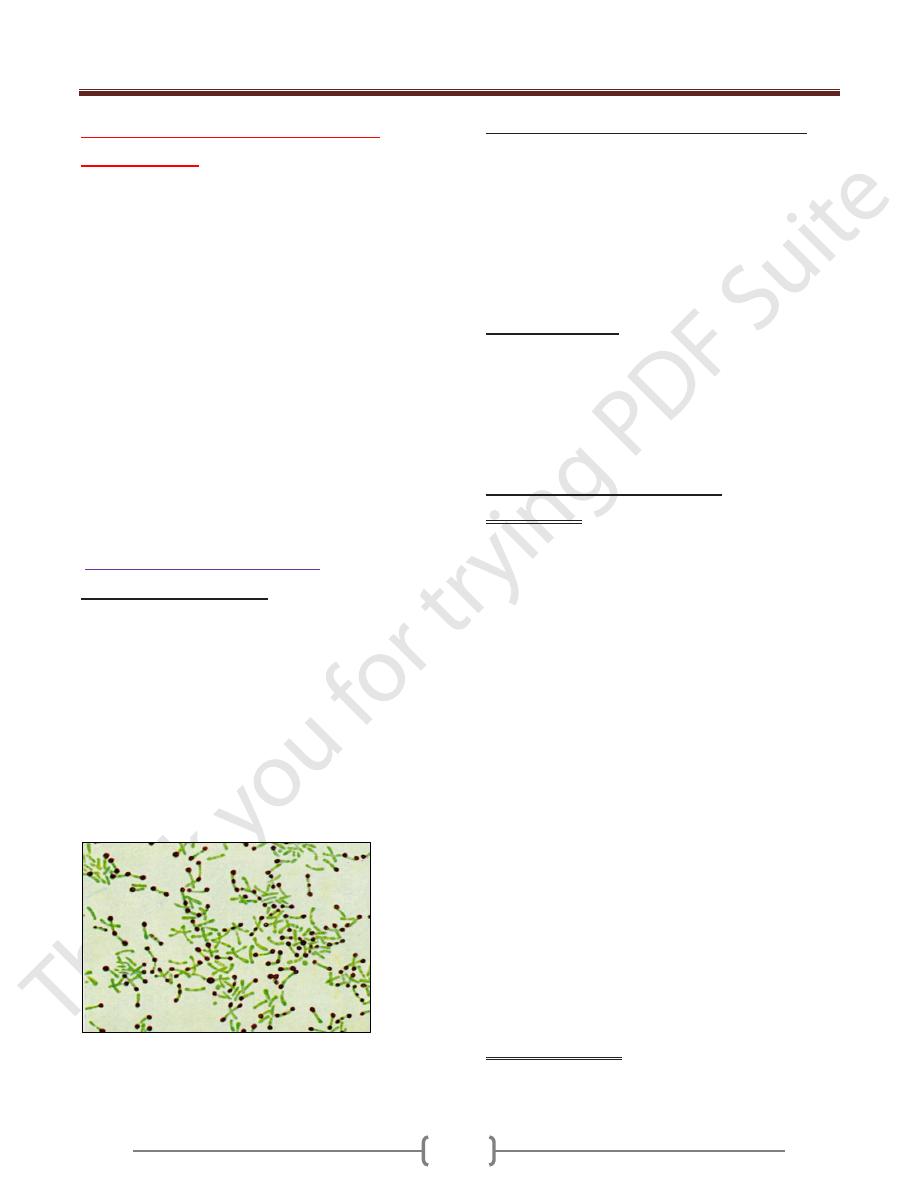
Diphtheria bacteria are Gram-positive, pleomorphic, often
club-shaped rods. The individual cells tend to group in
V, Y, or palisade arrangements. Neisser staining
reveals the polar bodies (polyphosphates stored at one
end of the rod). Lo¨ffler nutrient medium, which
consists of coagulated serum and nutrient broth, is still
used for the primary cultures. Selective indicator
mediums containing tellurite are used in selective
culturing. K tellurite is used to inhibit the accompanying
flora. The K tellurite is also reduced to tellurium,
coloring the colonies a brownish black.
Stained Corynebacterium cells. The "barred"
appearance and Note the characteristic "Chinese-
letter" arrangement of cells.
Three strains of Corynebacterium diphtheriae
are
recognized, gravis, intermedius and mitis. They are
listed here by falling order of the severity of the disease
that they produce in humans. All strains produce the
identical toxin and are capable of colonizing the throat.
The differences in virulence between the three strains can
be explained by their differing abilities to produce the
toxin in rate and quantity, and by their differing growth
rates.
Extracellular toxin
Diphtheria toxin consists of two functionally distinct
fragments, A and B, whereby B stands for binding to
receptors of target cells and A stands for toxic activity.
Fragment A irreversibly blocks protein synthesis
translation in the target cells, which then die. The toxin
gene is always a prophage genome component.
Pathogenesis and Clinical Picture
Local infection. Infection of the mucosa of tonsils,
pharynx, nose, and conjunctiva. Wounds and skin lesions
can also be infected. The pathogens invade the host
through these portals, reproduce, and produce
toxin, resulting in local cell damage. The inflammatory
reaction leads to collection of a grayish-white exudate, the
matrix of the “diphtherial pseudomembrane” consisting
of fibrin, dead granulocytes, and necrotic epithelial cells.
This coating adheres quite strongly to the mucosa. It may
extend into the larynx, thus eventually hindering
respiration. Regional lymph nodes are highly swollen.
Diphtheria is an upper respiratory tract illness
characterized by sore throat, low fever, and an adherent
membrane (called a pseudomembrane on the tonsils,
pharynx, and/or nasal cavity. Diphtheria toxin produced
by C. diphtheriae, can cause myocarditis, polyneuritis,
and other systemic toxic effects. A milder form of
diphtheria can be restricted to the skin. Diphtheria is a
contagious disease spread by direct physical contact or
breathing aerosolized secretions of infected individuals.
Once quite common, diphtheria has largely been
eradicated in developed nations through wide-spread use
of the DPT vaccine.Diphtheria is a serious disease, with
fatality rates between 5% and 10%. In children under 5
years and adults over 40 years, the fatality rate may be
as much as 20%. Outbreaks, although very rare, still
occur worldwide, even in developed nations.
Systemic intoxication. Parenchymal degeneration in the
cardiac muscle, liver, kidneys, and adrenal glands.
Motor cranial nerve paralysis. Late sequel damage due to
Unit 2: Bacteriology
96
the intoxication is frequently seen after the acute infection
has subsided.
Toxin-negative strains of C. diphtheriae are occasionally
observed as pathogens in endocarditis or dermal
infections. The pathogenicity of such strains corresponds
to that of commensal corynebacteria .
Diagnosis
The method of choice is detection and identification of the
pathogen in cultures from local infection foci. The
culture smear, which arrives at the laboratory in
transport medium, is plated out on Lo¨ffler medium
and a selective indicator medium. Identification is based
on both morphological and physiological characteristics.
The toxin is detected by the Elek-Ouchterlony
immunodiffusion test. A molecular method is now also
being used to identify the toxin gene. Toxin detection is
necessary for a laboratory diagnosis of diphtheria because
of the occurrence of toxin-negative strains.
Therapy
Antitoxic serum therapy is the primary treatment and it
must commence as soon as possible if diphtheria is
suspected. This treatment is supplemented by
administration of penicillin or erythromycin.
Epidemiology and prevention
Humans are the sole pathogen reservoir for diphtheria.
Infection sources include infected persons and carriers
(rare). The disease is usually transmitted by droplet
infection, or less frequently indirectly via contaminated
objects. The incubation period is two to five days.
Incidence levels in central Europe are low. From 1975 to
1984, only 113 cases were reported in Germany.
Incidence levels are higher in other countries (Russia).
Protective immunization with diphtheria toxoid is the
most important preventive measure . Exposure
prophylaxis involves isolation of infected persons until
two cultures from specimens taken at least 24 hours apart
are negative.
Actinomyces
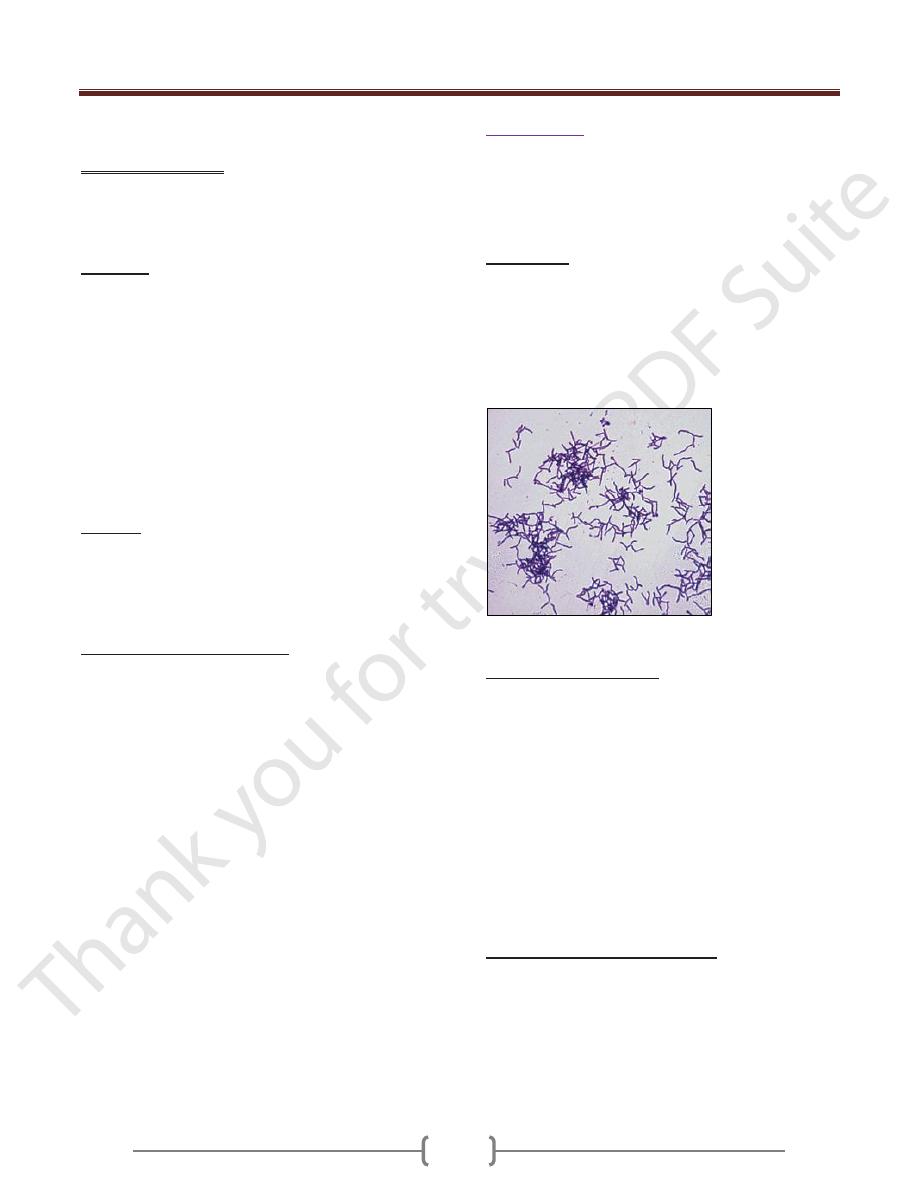
Actinomycetes are Gram-positive bacteria that tend to
grow in the form of branched filaments. The resulting
mycelial masses are, however, not observed in older
cultures, which strongly resemble those of corynebacteria
in their morphology.
Occurrence
.
Actinomycetes are part of the normal mucosal flora in
humans and animals. They colonize mainly the oral
cavity, and an actinomycosis infection is therefore always
endogenous. Ninety percent of actinomycetes infections
in humans are caused by A. israelii, with far fewer cases
caused by A.naeslundii and other species.
Actinomyces israelii
Morphology and culture
Actinomycetes are Gram-positive, pleomorphic rod
bacteria that sometimes also show genuine branching.
The yellowish sulfur granules, measuring 1–2 mm, can
be observed macroscopically in actinomycetes pus.
These particles are conglomerates of small Actinomyces
colonies surrounded by a wall of leukocytes. Mycelial
filaments extend radially from the colonies (actinium =
Greek for raylike). Culturing the organism requires
enriched mediums and an anaerobic milieu containing
5–10% CO2. Mycelial microcolonies form only during
the first days. Whitish macrocolonies, often with a
rough surface, begin to appear after two weeks.
Pathogenesis and clinical picture
The pathogens breach mucosa (perhaps normal dermis
as well) and are able to establish themselves in tissue in
the presence of a low redox potential. The factors
responsible for these conditions include poor blood
perfusion and, above all, contributing bacterial
pathogens. Genuine actinomycoses are actually always
polymicrobial. The mixed flora found includes mainly
Unit 2: Bacteriology
97
the anaerobes of the oral cavity. Actinobacillus
actinomycetemcomitans is frequently isolated along with
various species of Bacteroidaceae. Facultative anaerobes
such as staphylococci, streptococci, and
Enterobacteriaceae are, however, also found among the
contributing flora.
Cervicofacial actinomycosis. This is the most frequent
form of actinomycetes infection (>90%). The abscesses
are hard and tumor-like at first, then they necrotize.
They may also break through to the dermal surface to
create fistulae.
Thoracic actinomycosis. This rare form results from
aspiration of saliva; sometimes this type also develops
from an actinomycosis in the throat or hematogenous
spread.
Abdominal actinomycosis. This type results from
injuries to the intestine or female genitals.
Genital actinomycosis. May result from use of
intrauterine contraceptive devices.
Canaliculitis. An inflammation of the lacrimal canaliculi
caused by any of several Actinomyces species.
Caries. The Actinomyces species involved in caries
development are A. viscosus, A. naeslundii, and A.
odontolyticus . A possible contribution to periodontitis is
also under discussion.
Diagnosis
Involves identification of the pathogen by microscopy and
culturing in pus, fistula secretion, granulation tissue, or
bronchial secretion. The samples must not be
contaminated with other patient flora, in particular from
the oral cavity and must be transported to the laboratory
in special anaerobe containers. Microscopic detection of
branched rods suffices for a tentative diagnosis. Detection
of mycelial microcolonies on enriched nutrient mediums
after one to two weeks further consolidates this diagnosis.
Final identification by means of direct
immunofluorescence, cell wall analysis, and metabolic
analysis requires several weeks.
Therapy
: Treatment includes both surgical and
antibiotic measures. The antibiotic of choice is an
aminopenicillin. Antibiosis that also covers the
contributing bacterial pathogens is important.
Epidemiology and prevention
. Actinomycoses occur
sporadically worldwide. Average morbidity (incidence)
levels are between 2.5 and five cases per 100 000
inhabitants per year. Men are infected twice as often as
women. Prophylactic considerations are irrelevant due to
the endogenous nature of actinomycetes infections.
Diphtheroid
Lists of gram-positive rod bacteria that are rarely
involved in infections and normally infect only persons
with defective immune defenses. Recent years have seen
considerable changes in their classification and
nomenclature—still an ongoing process. Some of these
bacteria are designated by collective terms such as
“diphtheroid rods” or “coryneform bacteria.” Many of
these bacteria are part of the normal dermal and mucosal
flora. They are frequently found in sampled materials as
contaminants, but also occasionally cause infections.
Summary:
Corynebacterium (Diphtheria bacteria) are pleomorphic,
club-shaped rod bacteria that often have polar bodies and
group in V, Y, or palisade forms. They can be grown on
enriched nutrient media. Their pathogenicity derives from
diphtheria toxin, which binds to receptors of sensitive cells
with the B fragment. Once the binding process is completed,
the active A fragment invades the cell. This substance
irreversibly blocks translation in the protein biosynthesis
chain. The toxin gene is a component of the β-prophage.
Local and systemic intoxications are differentiated when
evaluating the clinical picture. Local infection usually affects
the tonsils, on which the diphtherial pseudomembrane
develops. Systemic intoxications affect mainly the liver,
kidneys, adrenal glands, cardiac muscle, and cranial nerves.
Laboratory diagnosis is based on pathogen identification.
The most important treatment is antitoxin therapy.
Diphtheria occurs only in humans. Thanks to extensive
diphtheria toxoid vaccination programs, it is now rare.
Actinomycetes are part of the normal mucosal flora.
These are Gram-positive rods that often occur in the form of
branched filaments in young cultures. Conglomerates of
microcolonies in pus form so-called sulfur granules.
Actinomycetes are obligate anaerobes. The pathogens enter
body tissues through mucosa defects. Monoinfections are
rare, the most frequent case being actinomycetes-dominated
endogenous polyinfections. Cervicofacial actinomycosis,
caused by oral cavity colonizer A. israelii, is the most
frequent form of actinomycosis. Treatment includes surgical
procedures and antibiosis with aminopenicillins.
The group of Gram-positive, irregular (pleomorphic),
nonsporing rod bacteria includes many different genera that
are normal components of the skin and mucosal flora .
Pathogens in this group cause two characteristic
diseases: diphtheria, caused by Corynebacterium diphtheriae
and actinomycosis, caused mainly by Actinomyces israelii.
