Unit 2: Bacteriology
98
Lecture 7 – Mycobacteria
Tuberculosis Bacteria (TB)
Tuberculosis is unquestionably among the most
intensively studied of all human diseases. In view of the
fact that tuberculosis can infect practically any organ in
the body.
Tuberculosis (TB) is the leading cause of death
in the world from a bacterial infectious disease. The
disease affects 1.8 billion people/year which is equal to
one-third of the entire world population.
Mycobacterium tuberculosis is the etiologic agent of
tuberculosis in humans. Humans are the only reservoir
for the bacterium. Mycobacterium bovis is the etiologic
agent of TB in cows and rarely in humans. Both cows
and humans can serve as reservoirs. Humans can also be
infected by the consumption of unpasteurized milk.
This route of transmission can lead to the development of
extrapulmonary TB, exemplified in history by bone
infections that led to hunched backs.
Other human pathogens belonging to the
Mycobacterium genus include
Mycobacterium avium
which causes a TB-like disease especially prevalent in
AIDS patients, and Mycobacterium leprae, the causative
agent of leprosy.
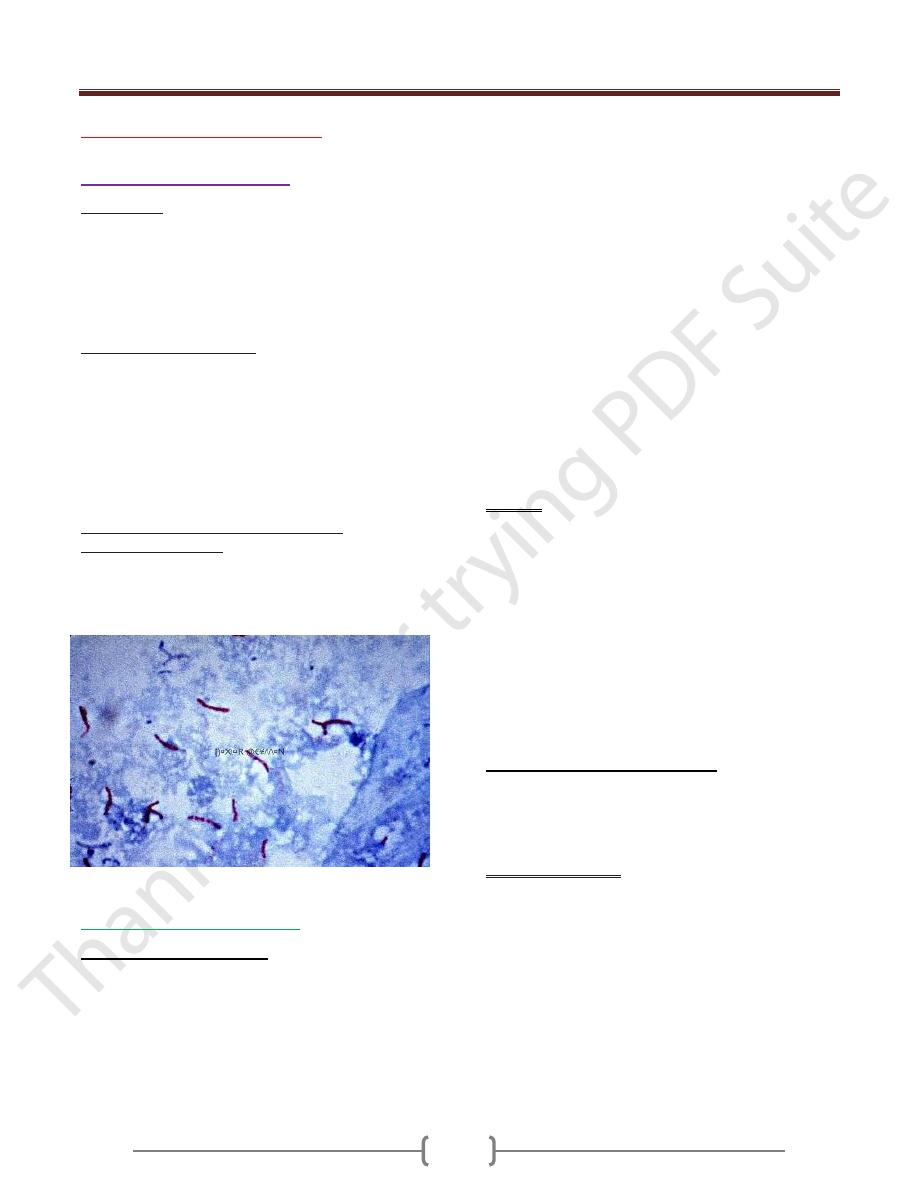
Mycobacterium tuberculosis (Ziehl Neilson Stain)
Mycobacterium tuberculosis
Morphology and culturing
TB are slender, acid-fast rods, 0.4 µm wide, and 3–4 µm
long, nonsporing and nonmotile. They can be stained with
special agents (Ziehl-Neelsen, Kinyoun, fluorescence).
Mycobacterium tuberculosis (MTB) is distantly related
to the Actinomycetes. Many nonpathogenic mycobacteria
are components of the normal flora of humans, found
most often in dry and oily locales. Mycobacterium
tuberculosis is an obligate aerobe. For this reason, in the
classic case of tuberculosis, MTB complexes are always
found in the well-aerated upper lobes of the lungs. The
bacterium is a facultative intracellular parasite, usually
of macrophages, and has a slow generation time, 15-20
hours, a physiological characteristic that may contribute
to its virulence.
Two media are used to grow MTB Middlebrook's
medium which is an agar based medium and
Lowenstein-Jensen medium which is an egg based
medium. MTB colonies are small and buff colored when
grown on either medium. Both types of media contain
inhibitors to keep contaminants from out-growing MT. It
takes 4-6 weeks to get visual colonies on either type of
media. TB are obligate aerobes. Their reproduction is
enhanced by the presence of 5–10% CO2 in the
atmosphere. Cultures must be incubated for three to six or
eight weeks at 37 ºC until proliferation becomes
macroscopically visible.
Cell wall.
Many of the special characteristics of TB are
ascribed to the chemistry of their cell wall, which features
a murein layer as well as numerous lipids, the most
important being the glycolipids (e.g.,
lipoarabinogalactan), the mycolic acids, mycosides, and
wax D . For example
Glycolipids and wax D are
r
esponsible for resistance to chemical and physical
noxae. Also they have adjuvant effect (wax D), i.e.,
enhancement of antigen immunogenicity. Tuberculin is
partially purified tuberculin contains a mixture of small
proteins (10 kDa). Tuberculin is used to test for TB
exposure (Delayed allergic reaction).
Pathogenesis and clinical picture
It is necessary to differentiate between primary and
secondary tuberculosis (reactivation or postprimary
tuberculosis) . The clinical symptoms are based on
reactions of the cellular immune system with TB antigens.
Primary tuberculosis.
In the majority of cases, the pathogens enter the lung in
droplets, where they are phagocytosed by alveolar
macrophages. TB bacteria are able to reproduce in these
macrophages due to their ability to inhibit formation of
the phagolysosome. Within 10–14 days an inflammatory
focus develops the so-called
primary focus
from which
the TB bacteria move into the regional lymph nodes,
where they reproduce and stimulate a cellular immune
response, which in turn results in clonal expansion of
specific T lymphocytes and attendant lymph node
swelling. The primary complex (Ghon’s complex)

Unit 2: Bacteriology
99
develops between six and 14 weeks after infection. At the
same time,
granulomas
form at the primary infection
site and in the affected lymph nodes, and macrophages
are activated by the cytokine
MAF
(
macrophage
activating factor
).
A tuberculin allergy
also develops in
the macroorganism The further course of the disease
depends on the outcome of the battle between the TB and
the specific cellular immune defenses.
Postprimary
dissemination foci
are sometimes observed as well, i.e.,
development of
local tissue defect foci
at
other
localizations
, typically the
apices
of the lungs.
Mycobacteria may also be transported to other organs
via the lymph vessels or bloodstream and produce
dissemination foci there. The host eventually prevails in
over 90% of cases: the granulomas and foci fibrose,
scar, and calcify, and the infection remains clinically
silent.
Secondary tuberculosis.
In about 10% of infected persons the primary
tuberculosis reactivates to become an
organ tuberculosis
,
either within months (5 %) or after a number of years (5
%). Exogenous reinfection is rare in the populations of
developed countries.
Reactivation
begins with a
caseation necrosis
in the center of the granulomas (also
called
tubercles
) that may progress to
cavitation
(formation of caverns). Tissue destruction is caused by
cytokines, among which tumor necrosis factor a (TNFa)
appears to play an important role. This cytokine is also
responsible for the
cachexia
associated with tuberculosis.
Reactivation frequently stems from old foci in the lung
apices.The body’s immune defenses have a hard time
containing necrotic tissue lesions in which large numbers
of TB cells occur (e.g., up to 109 bacteria and more per
cavern); the resulting lymphogenous or hematogenous
dissemination may result in infection foci in other organs.
Virtually all types of organs and tissues are at risk for this
kind of secondary TB infection. Such infection courses
are subsumed under the term
extrapulmonary
tuberculosis
.
Predisposing factors for TB infection include:
Close contact with large populations of people, i.e.,
schools, nursing homes, dormitories, prisons, etc.
Poor nutrition
IV drug use
Alcoholism
HIV infection is the number 1 predisposing factor for
MTB infection. 10 percent of all HIV-positive individuals
harbor MTB. This is 400-times the rate associated with
the general public. Only 3-4% of infected individuals will
develop active disease upon initial infection, 5-10%
within one year. These percentages are much higher if the
individual is HIV+.
Immunity
Humans show a considerable degree of genetically
determined resistance to TB. Besides this inherited
faculty, an organism acquires an (incomplete) specific
immunity during initial exposure (first infection). This
acquired immunity is characterized by localization of the
TB at an old or new infection focus with limited
dissemination (Koch’s phenomenon). This immunity is
solely a function of the T lymphocytes. The level of
immunity is high while the body is fending off the
disease, but falls off rapidly afterwards.It is therefore
speculated that resistance lasts only as long as TB or the
immunogens remain in the organism (= infection
immunity).
Tuberculin reaction.
Parallel to this specific immunity,
an organism infected with TB shows an altered reaction
mechanism, the tuberculin allergy, which also develops
in the cellular immune system only. The tuberculin
reaction, positive six to 14 weeks after infection, confirms
the allergy. The tuberculin proteins are isolated as purified
tuberculin (PPD = purified protein derivative). Five
tuberculin units (TU) are applied intracutaneously in the
tuberculin test. If the reaction is negative, the dose is
sequentially increased to 250 TU. A positive reaction
appears within 48 to 72 hours as an inflammatory
reaction (induration) at least 10mm in diameter at the
site of antigen application. A positive reaction means that
the person has either been infected with TB or
vaccinated with BCG. It is important to understand that a
positive test is not an indicator for an active infection or
immune status. While a positive test person can be
assumed to have a certain level of specific immunity, it
will by no means be complete. One-half of the clinically
manifest cases of tuberculosis in the population are
secondary reactivation tuberculoses that develop in
tuberculin positive persons.
Diagnosis
R
equires microscopic and cultural identification of the
pathogen or pathogen-specific DNA.
Traditional method
Workup of test material, for example with N-acetyl-L-
cysteine-NaOH (NALC-NaOH method) to liquefy
viscous mucus and eliminate rapidly proliferating
Unit 2: Bacteriology
100
accompanying flora, followed by centrifugation to enrich
the concentration.
Microscopy. Ziehl-Neelsen and/or auramine fluorescent
staining . This method produces rapid results but has a
low level of sensitivity (>104–105/ml) and specificity
(acid-fast rods only).
Culture on special solid and in special liquid mediums.
Time requirement: four to eight weeks.
Identification. Biochemical tests with pure culture if
necessary. Time requirement: one to three weeks.
Resistance test with pure culture.
Time requirement: three
weeks.
Rapid methods.
A number of different rapid TB diagnostic methods have
been introduced in recent years that require less time than
the traditional methods.
Culture.
Early-stage growth detection in liquid mediums
involving identification of TB metabolic products with
highly sensitive, semi-automated equipment. Time
requirement: one to three weeks. Tentative diagnosis.
Identification.
Analysis of cellular fatty acids by means of
gas chromatography and of mycolic acids by means of
HPLC. Time requirement: 12 days with a pure culture.
DNA probes.
Used to identify M. tuberculosis complex
and other mycobacteria. Time requirement: several hours
with a pure culture.
Resistance test.
Use of semi-automated equipment .
Proliferation/ nonproliferation determination in liquid
mediums containing standard antituberculotic agents.
Time requirement: 7–10 days.
Direct identification in patient material.
Molecular methods used for direct detection of the M.
tuberculosis complex in (uncultured) test material. These
methods involve amplification of the search sequence.
Therapy
The previous method of long-term therapy in sanatoriums
has been replaced by a standardized chemotherapy often
on an outpatient basis.
Epidemiology and prevention
Tuberculosis is endemic worldwide. The disease has
become much less frequent in developed countries in
recent decades. Tuberculosis is still a major medical
problem. It is estimated that every year approximately 15
million persons contract tuberculosis and that three
million die of the disease. The main source of infection is
the human carrier. There are no healthy carriers. Diseased
cattle are not a significant source of infection in the
developed world. Transmission of the disease is generally
direct, in most cases by droplet infection. Indirect
transmission via dust or milk (udder tuberculosis in cattle)
is the exception rather than the rule. The incubation
period is four to 12 weeks.
Exposure prophylaxis. Patients with open tuberculosis
must be isolated during the secretory phase. Secretions
containing TB must be disinfected. Tuberculous cattle
must be eliminated.
Disposition prophylaxis. An active vaccine is available
that reduces the risk of contracting the disease by about
one-half. It contains the live vaccine BCG (lyophilized
bovine TB of the Calmette-Gue´rin type). Vaccination of
tuberculin-negative persons induces allergy &
(incomplete) immunity that persist for about five to 10
years.
Leprosy Bacteria (LB)
Morphology and culture
Mycobacterium leprae (Hansen, 1873) is the causative
pathogen of leprosy. In morphological terms, these acid-
fast rods are identical to tuberculosis bacteria. They differ,
however, in that they cannot be grown on nutrient
mediums or in cell cultures.
Pathogenesis
The pathomechanisms of LB are identical to those of TB.
The host organism attempts to localize and isolate
infection foci by forming granulomas. Leprous
granulomas are histopathologically identical to
tuberculous granulomas. High counts of leprosy bacteria
are often found in the macrophages of the granulomas.
Immunity
The immune defenses mobilized against a leprosy
infection are strictly of the cellular type. The lepromin
skin test can detect a postinfection allergy.
This test is not, however, very specific (i.e., positive
reactions in cases in which no leprosy infection is
present). The clinically differentiated infection course
forms observed are probably due to individual immune
response variants.
Clinical picture
Leprosy is manifested mainly on the skin, mucosa, and
peripheral nerves. A clinical differentiation is made
between tuberculoid leprosy and lepromatous leprosy
(LL). There are many intermediate forms. TL is the
benign, nonprogressive form characterized by spotty
Unit 2: Bacteriology
101
dermal lesions. The LL form, on the other hand, is
characterized by a malignant, progressive course with
nodular skin lesions and cordlike nerve thickenings
that finally lead to neuroparalysis. The inflammatory
foci contain large numbers of leprosy bacteria.
Diagnosis
Detection of the pathogens in skin or nasal mucosa
scrapings under the microscope using Ziehl-Neelsen
staining . Molecular confirmation of DNA sequences
specific to leprosy bacteria in a polymerase chain reaction
is possible.
Therapy
Paucibacillary forms are treated with dapson plus
rifampicin for six months. Multibacillary forms require
treatment with dapson, rifampicin, and clofazimine over a
period of at least two years.
Epidemiology and prevention
Leprosy is now rare in socially developed countries,
although still frequent in developing countries. There are
an estimated 11 million victims worldwide. Infected
humans are the only source of infection. The details of the
transmission pathways are unknown. Discussion of the
topic is considering transmission by direct contact with
skin or mucosa injuries and aerogenic transmission.
The incubation period is 2–5–20 years.
Isolation of patients under treatment is no longer required.
An effective epidemiological reaction requires early
recognition of the disease in contact persons by means of
periodical examinations every six to 12 months up to five
years following contact.
Nontuberculous Mycobacteria (NTM)
Mycobacteria that are neither tuberculosis nor leprosy
bacteria are categorized as atypical mycobacteria (old
designation), nontuberculous mycobacteria (NTM) or
MOTT (mycobacteria other than tubercle bacilli).
Morphology and culture
In their morphology and staining behavior, NTM are
generally indistinguishable from tuberculosis bacteria.
With the exception of the rapidly growing NTM, their
culturing characteristics are also similar to TB. Some
species proliferate only at 30 °C. NTM are frequent
inhabitants of the natural environment (water, soil) and
also contribute to human and animal mucosal flora. Most
of these species show resistance to the antituberculoid
agents in common use.
Clinical pictures and diagnosis
Some NTM species are apathogenic, others can cause
mycobacterioses in humans that usually follow a chronic
course
NTM infections are generally rare. Their occurrence is
encouraged by compromised cellular immunity. Frequent
occurrence is observed together with certain
malignancies, in immunosuppressed patients and in
AIDS patients, whereby the NTM isolated in 80% of
cases are M. avium or M. intercellulare. As a rule, NTM
infections are indistinguishable from tuberculous lesions
in clinical, radiological, and histological terms. Diagnosis
therefore requires culturing and positive identification.
The clinical significance of a positive result is difficult to
determine due to the ubiquitous occurrence of these
pathogens. They are frequent culture contaminants. Only
about 10% of all persons in whom NTM are detected
actually turn out to have a mycobacteriosis.
Therapy
Surgical removal of the infection focus is often
indicated. Chemotherapy depends on the pathogen
species, for instance a triple combination (e.g., INH,
ethambutol, rifampicin) or, for resistant strains, a
combination of four or five antituberculoid agents.
