Unit 3: Mycology
140
Lecture 2+3+4+5 - Fungal diseases
in humans (mycoses)
Fungal diseases are also called Mycoses. Mycoses are
classified as:
1) Superficial.
2) Cutaneous.
3) Subcutaneous.
4) Systemic.
5) Opportunistic.
Depending on the usual portal of entry and
initial site of involvement the Table below
shows the types of Mycoses, their causative
fungal agent and Diseases:-
Type of
Mycosis
Causative fungal agent
Mycosis
Superficial
Malassezia ,Hortaea
werneckii Trichosporon
species Piedraia hortae
Pityriases vericolor
Tinea nigra White
piedra Black piedra
Cutaneous
Microsporum species,
trichophyton species, and
Epidermophyton
floccosum
Candida albicans and other
Candida species
Dermatophytosis
candidiasis of skin,
mucosa or nails
Subcutaneous
Sporothrix schenckii
Phialophora verrucosa,
fonsecaea pedrosei,
others
Pseudallescheria boydii,
madurella mycetomatis,
others
Exophiala, bipolaris,
exserohilum, and others
Sorotrichosis
Chromobalstomy
cosis Mycosis
Phaeophomycosis
Endemic
(primary,
systemic)
Cocidioides immitis,
cposadasii Histoplasma
capsulatum Blastomyces
dermatitidis
Paracoccidioides
brasiliensis
Coccidioidomycos
is
Hhistoplasmosis
Blastomycosis
Paracoccidioidom
ycosis
Opportunistic
Candida albicans and
other Candida species
Cryptococcus neoformans
Aspergillus fumigataus
and other aspergillus
species
Species of Rhizoupus,
absidia, Mucor, and other
zygomycetes
Penicillium mameffei
Systemic
Candidiasis
Cryptococcosis
Aspergillosis
Mucormycosis
(zygomyccosis)
penicilliosis
Superficial mycosis
These are some of the most common infections in
humans; superficial infections of the skin and hair
(pityriasis versicolor. Tinea niger. Black and white
piedras) mainly cause cosmetic problems.
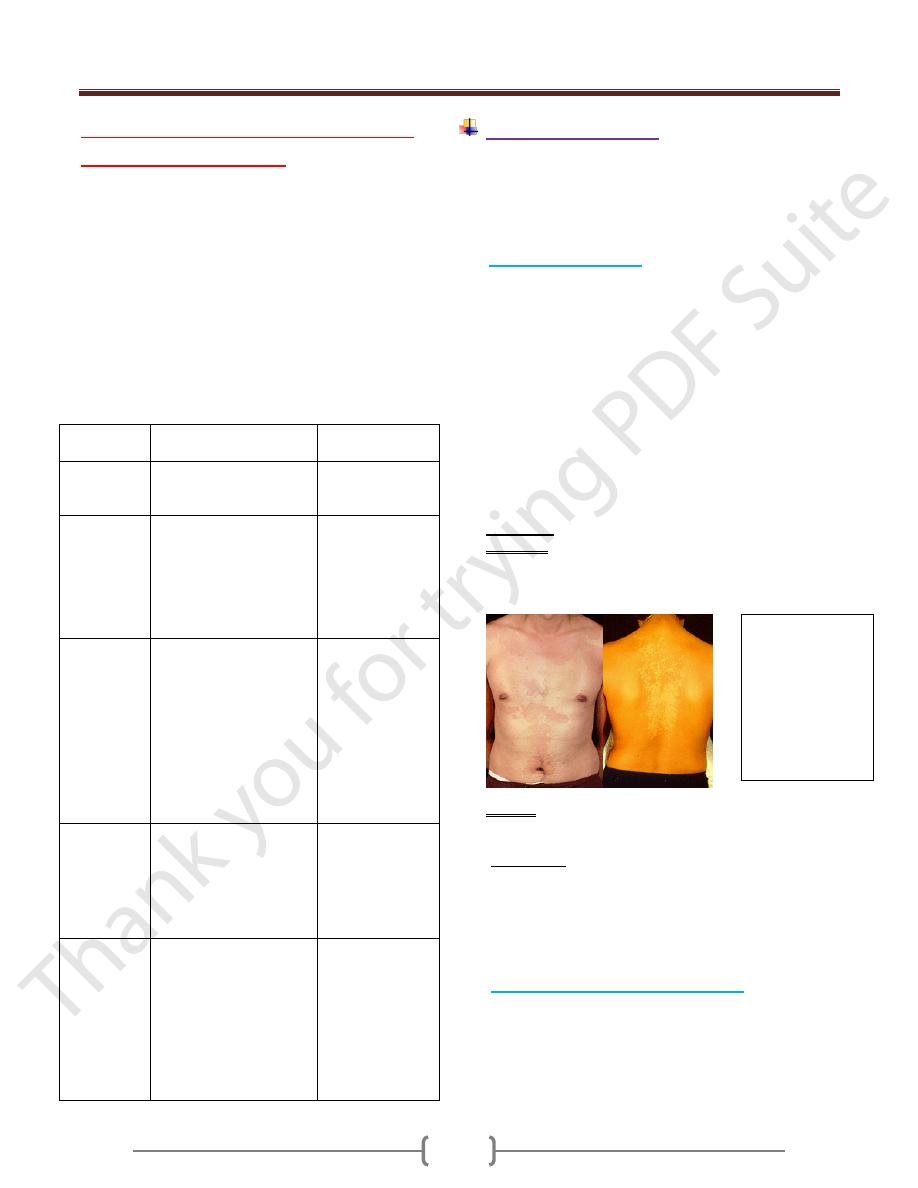
Pityriasis versicolor
Pityriasis versicolor is a chronic mild superficial
infection involves only the superficial keratin layer
(stratum corneum) of the skin caused by Malassezia
furfur. the yeast M.furfur is a common skin
inhabitant. Pityriasis (tinea) versicolor is a common
superficial mycosis, which characterized by discrete
hyper or hypopigmented macules of skin of the neck,
shoulder, chest, upper back arm or abdomen. The
lesions are chronic and may enlarged and coalesce to
from scaling plaque, the lesions are not usually itchy
and in some patients resolve spontaneously. it occur
more frequently in hot, humid weather.
Diagnosis
Specimen: Direct microscopical examination of scrapings
of infected skin treated with 10 - 20% KOH or stained
with Calcofluor white short unbranched hyphae and round
yeast dorm, other lesion also fluoresce under wood lamp.
Culture: malassezia furfur is lipophilic yeast (most require
lipid in the medium) for growth but culture is not is not done
Treatment
Daily application of selenium sulfide.
Topical or oral azoles are effective.
Lesion have tendency to recur and a permanent cure is
difficult to achieve.
Tinea nigra (tinea nigra palmris)
A superficial chronic and asymptomatic infection of the
outermost layer of stratum corneum caused by the
dermatiaceous fungus Hortaea (Exophiala weneckii)
which is found in soil and transmitted during injury.
Pityriasis
versicolor
showing
hyperpigmented
lesions in a
Caucasian and
hyphopigmented
lesions
Unit 3: Mycology
141
More prevalence in warm coastal regions (in USA mainly
in southern states) and among young women.
Tinea nigra most typically presents as a dark brown black
sliver nitrate like stain on the palm of the hands or sole of
the foot.
Diagnosis
Microscopical examination of scrapings of the periphery
of the skin lesions will reveal branched, septate hyphae
and budding yeast cells with melaninized cell wall.
Treatment
Response to keratolytic solution such as salicylic acid or
Azole antifungal drugs.
Piedra
Superficial fungal infection involves the cuticle of the
hair shaft and it is endemic in tropical underdevloped
countries.
Black piedra is a nodular infection of the hair shaft due to
piedra hortae which is manifested by a small form black
nodule involve hair shaft, by comparison, white piedra
due to trichosporon species is characterized by a large
soft, friable yellow nodule of the distal ends of hair shaft
Axillary, pubic scalp may be infected.
Treatment
Removal of the infected hair.
Application of topical antifungal agents.
Cutoeus mycoses
Cutaneous mycoses are caused by fungi that infect only
the superficial keratinized (skin, hair and nails).
The most important of these are dermatophytes that are
classified in three genera: Microsporum, Trichphyton and
Epidermophyton which are the main etiological agent of
the dermatophytosis, such cutaneous mycoses are referred
to as tinea (Latin word for ring worm). These infections
may be characterized by another latin noun according to
the area of the body involved eg. Tinea corporis (body),
tinea capitis (scalp and hair), tinea manum (hand and
finger) , tinea pedis (foot), tinea unguium (nail).
The dermatophytosis is characterized by anatomic site
specificity according to genera. For expmple ,
Epidermphyton floccosum infected only skin & nails
whereas microsporum Spp. Infected hair & skin but do not
involve nails. Trichphyton may infect hair, skin & nails.
Dermatophytosis are among the most prevalent infections
in world. Dermatophytosis are chronic infections favored
by heat and humidity eg: athlete’s foot (Tinea pedis) and
Jock itch (Tinea cruris).
Species of dermatophytes are calssified as anthropophilic
Zoophilic or geophilic depending upon their primary
source (humen, animal or soil). the anthropophilic Spp.
Are the most common causes of dermatophyte infection.
Geophilic are uncommon causes of human disease but are
seen in people who have appropriate exposure such as
gardener and cultural. Dermatophytes are acquired by
contact with contaminated soil or with infected animals or
humans
Identification
Dermatophytes are identified by their colonial appearance
and microscopic morphology after growth for a week at
25C on sabouraud’s dextrose agar..
Epidemiology
The incidence is higher in hot humid climates and under
crowded condition.
The source of infection is soil in case of geophilic
dermatophytes and other source is animal in Clinical
findings
Tinea pedis is the most prevalence of all dermatophytosis,
tinea unguinum: nail infection may follow prolonged tinea
pedis, one or more nails of the feet or hands may be
involved after hyphal invasion when the infection occurs
in the area also called jock itch involve hypersensitivity
reaction called kerion caused by tinea capitis, while
anthrophilic spp. May be transmitted by direct contact or
through fomites such as contaminated towels, clothing
and shared shower staff. Human to human transmittion
require close contact with infected human or animal.
Transmission take place within the family.
Unit 3: Mycology
142
Subcutaneous Mycoses
These are chronic, localized infections of the epidermis
and adjacent connective tissue and lymphatics following
the traumatic implantation of the organism. The causative
fungi are all soll saprophytes whose ability to adapt to the
tissue environment and elicit disease is extremely variable
Subcutaneous sporotrichosis, mycetoma, and
chromoblastomycosis are well characterized subcutaneous
mycoses
As you will see, these are clearly more significant than the
superficial and drmatophycoses
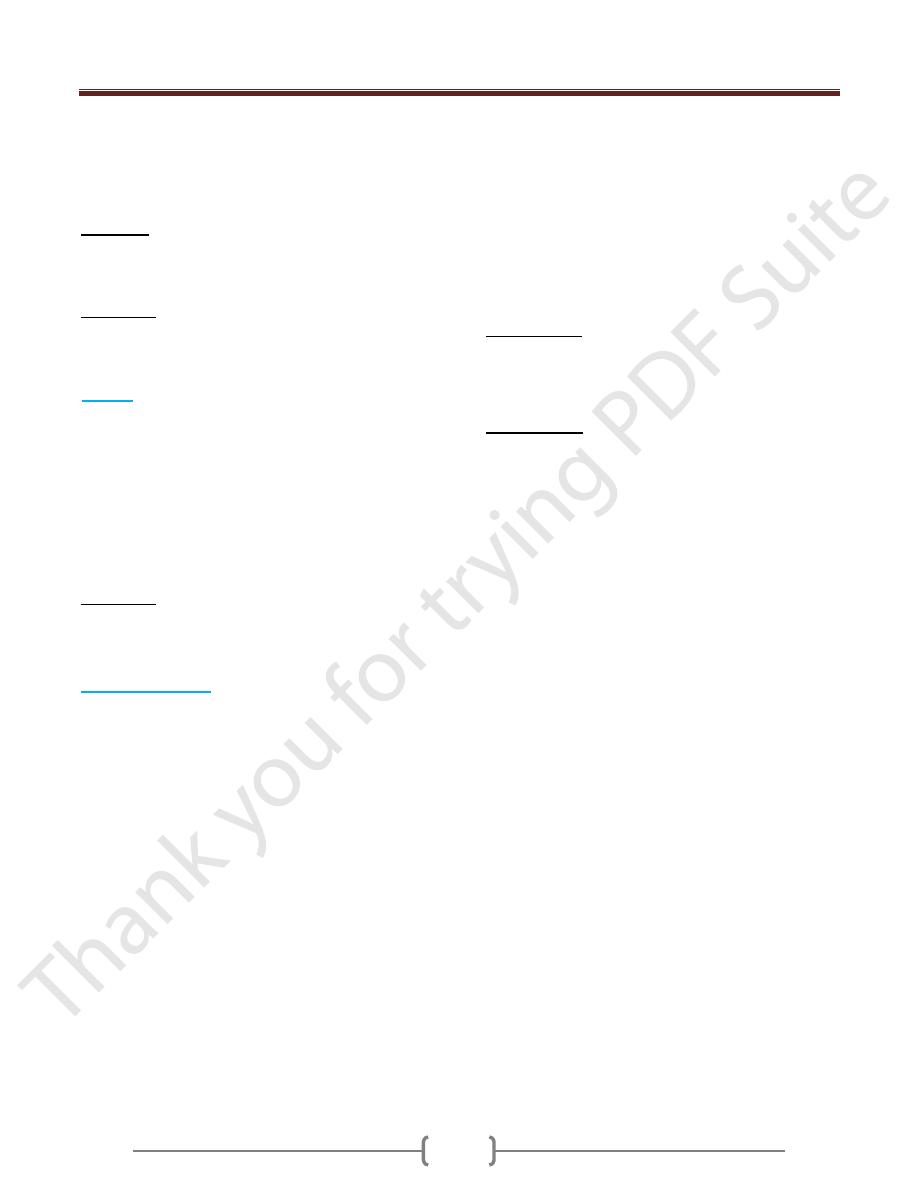
Sporotrichosis
Common name
: ‘Rose Gardener’s Disease’
Etiology
:
Sporothrix schenckii
Sporothrix schenckii is the only dimorphic fungus to
cause subcutaneous mycosis
Epidemiology:
Occurs worldwide and in all age groups, although it is
more common in tropical and subtropical areas
More infections occur in men due to occupational
exposure (foresters, gardeners, horticulturists)
Sporothrix schenckii grows frequently as an environmental
saprobe on woody plants & rich organic soll
They are well known to grow on roses
Most cases are traced to rose thorns, splinters or other
plant materials penetrating the skin
Many recent cases have been traced to sphagnum moss
purchased from commercial suppliers
Clinical manifestations
Most cases are cutaneous (relatively local/shallow &
mild) or lymphocutaneous
Primary “fixed” cutaneous lesions at site of injury are
small papules (colored raised area) most often occurring
on an extremity
Lymphocutaneous: lymph nodes become sequentially
infected as organisms are swept along the lymph channels
Lymph nodes become enlarged, firm, and discolored
(buboes)
Draining sinuses may develop from a lymph node and
terminate in the adjacent skin
One rare occasions disease occurs following when conidia
from environment are inhaled (in particular the recent
cases related to sphagnum moss exposure)
The rare pulmonary cases cause symptoms that range
from bronchitis to tuberculosis-like infections
The most common extracutaneous disorder is
osteoarticular in nature-confined to long bones near joints
Dissemination is rare and limited to
immunocompromised patients: many organs involved
Primary “fixed’
lesions of
cutaneous
sporotrichosis
Lymphocutaneous
Sporotrichosis
Sequential
infection of
lymph node
Unit 3: Mycology
143
Endemic mycoses (Primary or
systemic mycosis)
Four fungi causing systemic mycosis Coccidioidomycosis ,
Histoplasmosis, Blastomycosis & Paracoccidoidomycosis
Characteristic of Endemic Mycoses:-
1) Endemic mycoses is geographically restricted to specific
area of endemicity that why called endemic mycosis.
2) The fungi that cause Coccidioidomycosis and
Histoplasmosis exit in nature in dry soil while the agent of
blastomycosis and paracoccidioidomycosis reside in
nature but their habit are not clearly known.
3) All of these mycoses are caused by a thermally dimorphic
fungus.
4) Most of these infections are initiated in lungs following
inhalation of conidia.
5) Most of these infections are asymptomatic and self –
limiting, only few infections lead to disease which involve
dissemination from lungs to other organs.
6) Infected persons do not communicate these diseases to
others ( non – transmissible ).
7) The initial host defense mechanisms are provided by the
alveolar macrophage for all of these infections.
8) Within endemic areas, 90% or more occur in
immunocompetent individuals but persons with impaired
cellular immunity such as patients with AIDS/ HIV have a
new risk of serious infection.
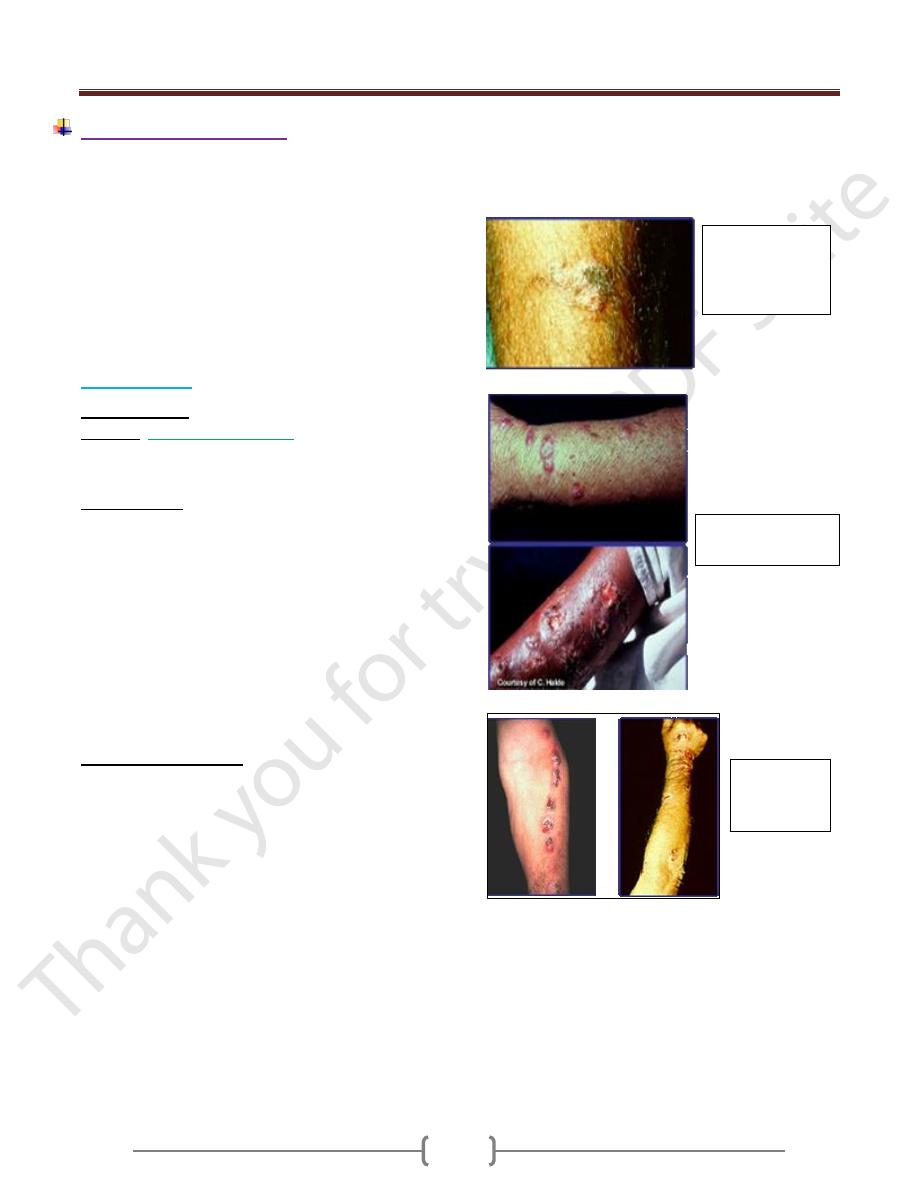
Coccidioidomycosis
The etiological is
coccidioides immitus.
The infection is endemic in the desert southwestern of
US, Maxico Central and South America.
Coccidoicdomycosis is acquired by inhalation of
arthroconidia of C. immitis.
Approximately 60% of the cases are usually
asymptomatic and self – limited respiratory infection.
The infection may become disseminated to meninges,
bone and skin dissemination occurs most frequently in
person with dark skin.
Coccidioides immitis is a dimorphic fungus but instead of
a yeast phase, a large, distinctive, round walled spherule
is produced in the invasive tissue form, spherule are also
be produced in the laboratory by cultivation, this structure
unique among the pathogenic fungi. Development of
spherule and with production of multiple endospores
within each spherule, the spherule eventually rupture,
releasing 200-300 endospores, each of which can
differentiate into another species.
In alkaline soil and in culture, Coccidioides immitis grow
only as a mold regardless the temperature. Growth
become visible in 2-5 days , the hayphae are septated and
produce thick walled barrel shaped arthroconidia which
are the infection unit in nature and highly infection unit in
nature and highly infection in the laboratory. Spherule has
been produced from arthroconidia in vitro under
specialized condition.
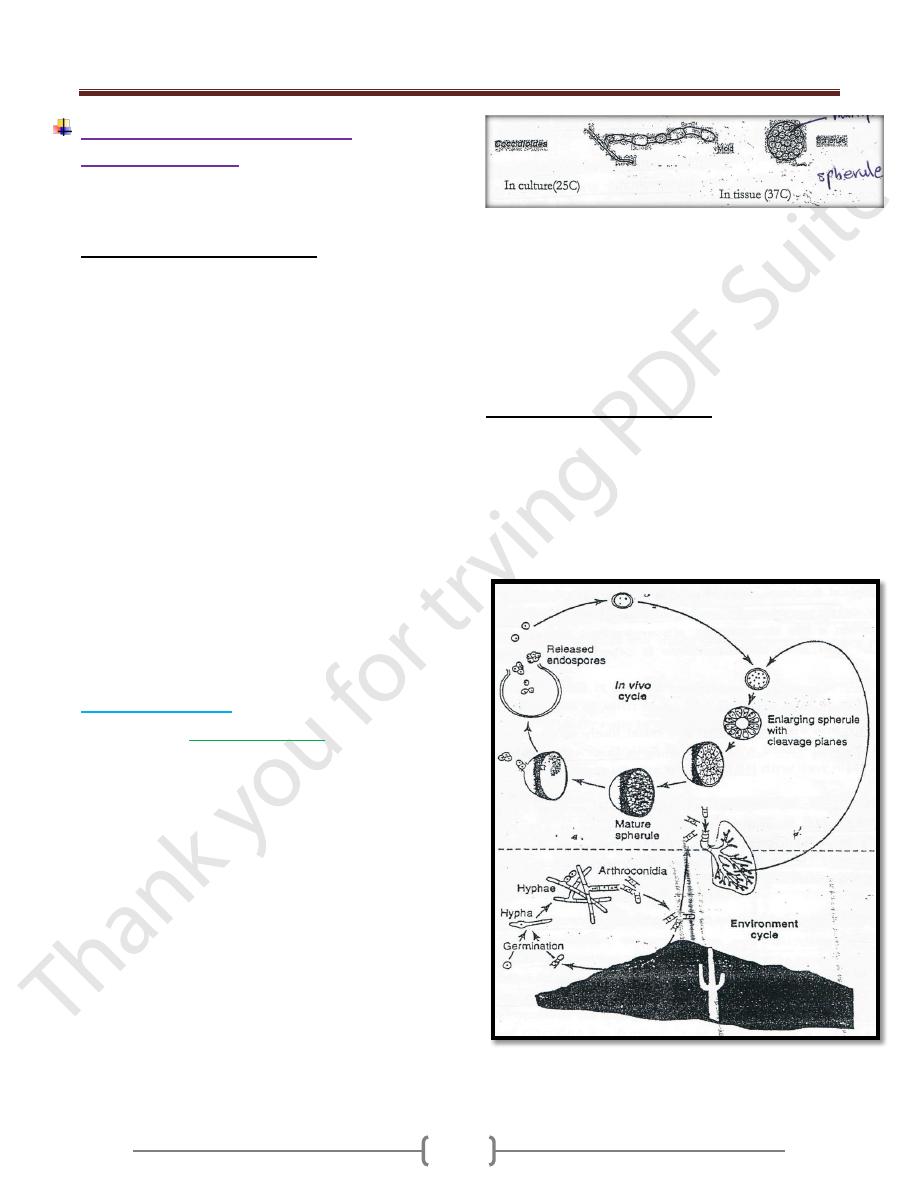
Life cycle Coccydioides immitus
The nature cycle take place in desert climates with modest
rainfull. Hyphae differentiate into arthroconidia which
break loose and may be suspended in the air. Soil disruption
and wind facilltate spread and probably of inhalation into
human lungs. In human host environment in vivo
differentiation produce spherules. The spherules releasing
endospores which can be repeat the in vivo cycle.
Unit 3: Mycology
144
Clinical findings
Acute primary infection with C.immitis is either a
symptomatic in 60% of cases or present as a complex
called valley fever or desert rheumatism by resident of
endemic areas. Valley fever includes fever, malaise, dry
joint pain & headache after 1-2 weeks. 15% of these
patients may develop rash due to hypersensitivity reaction
There are physical or radiological findings, less than 1%
of persons infected with C. immitis develop secondary or
disseminated Coccidiomycosis ( occur a year after
primary infection) which is ofter a life threatening.
Dissemination disease involve lesions in the bone, joints
or skin. the clinical course is often characterized by
remission and relapses.
Diagnosis
Expectorated sputum, skin & visceral lesions are most
likely to demonstrate spherule by direct examination mixed
with KOH or Calcofluor white while CSF is least likely,
spherules stain well with H& E stain or special stain.
Culture of C. immitis from sputum, visceral lesions or skin
lesions on mold agar, Sabouraud’s dextrose agar, incubated
at room temp. or at 37C Culture must be examined only in a
biological safety cabinet because the culture conidia are
highly infectious. Identification may be confirmed by
animal inoculation use specific DNA probe.
Skin test become positive within 2-4 weeks but is often
negative in patients with disseminated disease.
In serological test 1gM and 1gG precipitin within 2-4
weeks of infection then decline in the subsequent months
and then rise greatly in dissemination occur.
Treatment
In most of person, symptomatic infection is a self –
limited and requires only supportive treatment.
IV Amphteracin B is required in severe disease followed by
several months of oral therapy with itraconazol. Coccidioidal
meningitis have been treated with oral fluconazol.
Histoplasmosis
The causative organism is
histoplasma capsulatum.
Histoplaxmosis is the most prevalence pulmonary
mycotic infection in human and animals.
Hisplasmosis is limited to the endemic area where the
majority of cases are symptomatic or with fever and
cough. H capsulatum received its name from the
appearance of yeast cells in histopathologic section.
In the USA it is endemic in central and eastern states
especially Ohio and Mississippi river.
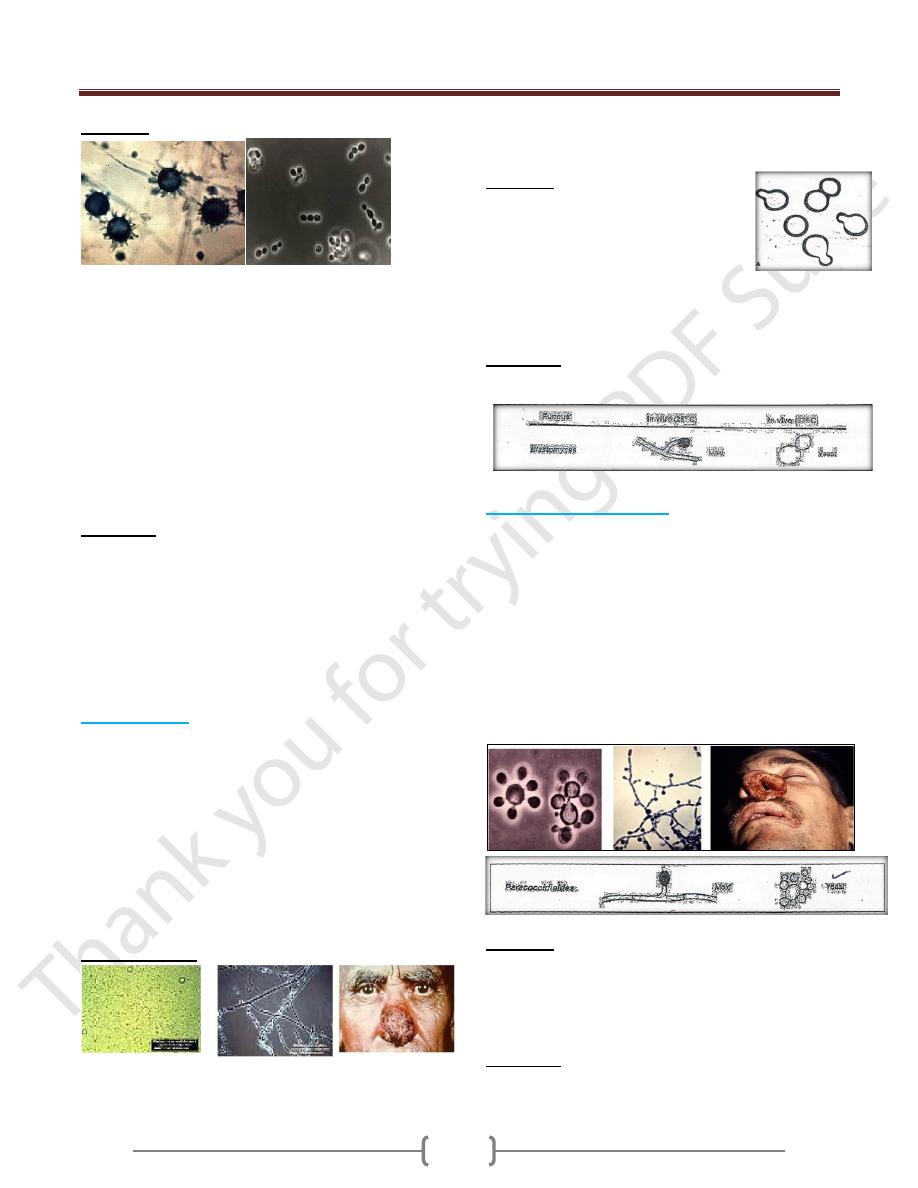
H. capsulatum a dimorphic fungus that grows in soil and
humid climatic conditions, particularly soil containing
bird or bat droppings. This dimorphic fungi exists as a
mold in soil the mold is hyaline, septate hyphae produce
microconidia and large thick walled macroconidia with
peripheral projections of cell wall material. Microconidia
are small enough to reach the terminal bronchioles and
alveoli and believe to the mode of infection.
Inhaled spores are engulfed by macrophages and develop
into yeast form. In tissue H capsulatum occurs as an oval
budding yeast inside macrophage , the organism spread
widely throughout the body to reticuloendothelial tissues
such as liver, spleen, bone marrow and lymph node but
most of infections remain asymptomatic because of initial
inflammatory reaction as a small granulomatous foci.
Birds themselves do not carry the disease, but their
dropping provides nutrents as a source of nitrogen for
fungus. Bats which have a lower body temperature than
bird carry the fungus, shed it in the feces and probably
infect new soil sites.
Unit 3: Mycology
145
Diagnosis
In tissue biopsies or bone marrow aspirates, oval yeast
cells within macrophages are seen microsocopically after
stain with fungal stain or Geimsa stain for blood bone
marrow smears.
Specimen for culture including sputum, bone marrow
aspirates to be inoculated on sabouraud’s dextrose agar of
inhibitory mold agar at 25 – 30C for 4-12 weeks.
Two serological test are useful for diagnosis; complement
fixation test (CF) and immunodiffusion (ID) test. The ID
test is more specific but less sensitive than the CF test.
Skin test is no useful for diagnosis.
Treatment
Acute pulmonary infection is managed with supportive
therapy and rest.
In mild to moderate infection, itroconazol is the drug of
choice.
Amphotericin B is used for treatment of disseminated
systemic infection.
Prolonged treatment may be needed, relapse may occur.
Blastomycosis
Caused by fungus: blastomyces dermatitidis.
It is a dimorphic fungi with some characteristic similar to
those of H. capsulatum. Growth develop in the yeast
phase in tissue, the yeast are typically larger than those of
H. capsulatum with broad based buds and a thick wall.
The mold phase appears in culture at 25C. Hyphae are
septate and sufficiently similar to the macroconidia
produce by H. capsulatum. Most of the cases occur in the
us and Canada but blastomycosis has been documented in
Africa and Asia.
Clinical findings
Most of clinical features of blastomycosis are similar to
hsitoplasmosis asymptomatic or mild cases are rarely
recognized. Dissemination may result in ulcerated
granuloma on exposed area of the skin, bone or other sites.
Diagnosis
Wet mount of specimen such as sputum,
exudates and biopsies from lesions may
show broady attached buds in thick walled
yeast cells.
Colonies develop on sabouraud’s agar at 30C and
confirmed by detection of B.dermatitids specific antigen
of by specific DNA probe.
Treatment
Amphtericin B are used for sever cases.
Paraconcciioidomycosis
Paracoccidioides braziliensis cause paracoccidiomycosis.
P. braziliensis is a dimorphic fungi that exist as mold in
soil and as a yeast in tissue. The yeasts are larger and have
thinner walls than those of B . dermatiditis and buds are
multiple and attached by narrow connection.
It is endemic in south America
The spores are inhaled and early lesions occur in the
lungs. A symptomatic infection is common alternatively,
oral mucous membrane lesions, lymph node enlargement,
some tissue dissemination may occur.
Diagnosis
In pus or tissue yeast cell with multiple buds are seen
microscopically specimen culture for 2-4 weeks may
grow typical organism. Serology is most useful for
diagnosis, skin test are rarely helpful.
Treatment
Itraconzol is the most effective drug. And trimethoprim
and sulfamethoxazol are also effective.
Unit 3: Mycology
146
Opportunistic Mycosis
Opportunistic Mycosis is a group of fungal infection that
occurs almost exclusively in immune compromised
patients. Patients with compromised host defenses are
susceptible to ubiquitous fungi to which healthy people
are expose but usually resistant many causes type of
fungus and the natural history of the mycotic infection are
determined by the underlying predisposing condition
.Candida and related yeast as member of normal flora are
endogenous opportunists. Other opportunistic mycosis are
caused by exogenous fungi present in soil, water and air.
The type of patient who acquire an opportunistic fungal
infection is one who is compromised by some underlying
disease such as AIDS, Lymphoma, Leukemia, diabetes
also any patients treated with corticosteroid cytotoxic
drugs or other immunosuppressive drugs are exposed to
opportunistic mycosis.
Common etiologic agents are
1) Yeasts
Candida spp. Cryptococcus spp
2) Mycelial or Filamentous Fungi
Aspergillus spp. Zygomycetes, Rhizopus
3) Protozoan-like fungi
Pneumocystis carinii
Candida (Candidiasis)
Candida albicans, the most important sp. of candida
Is an oval yeast with asingle buds, it is a part of the
normal flora in the upper respiratory tract, gastrointestinal
tract, femal genital tracts.
In tissues may appear as yeast or pseudohyphae
Pseudohyphae are elongated yeast that resemble hyphae
but are not true hyphae. Candida species colonize the
mucosal surface of all humans during or soon after birth.
Candidiasis may be caused by:
Candida albicans
C. tropicalis
C. krusei
C. pseudotropicalis
C. albicans var. stellatoida
C. parapsilosis
C. guilliermondii
C. glabrata
Clinical manifestation of Candidiasis
A. Mucocutaneous involvement
1) Oral Candidiasis (thrush)
Appearance of milk curds as they crumble
Common in older people, diet deficiencies. Premature
babies, first sign of clinical AIDS
2) Vaginitis
Predisposing factors
Pregnant women (growth promoted by secretion of
glycogen and progesterone) –obesity –diabetes (high
sugar content in urine) –may be sexually transmitted but
rarely infects the penis (balanitis).
3) Bronchial and pulmonary (not common)
Difficult to diagnose because organism is common in
most chronic lung conditions
4) Alimentary candidiasis
Infection resides in the esophagus, intestine and anus
B. Cutaneous involvement
Often associated with skin that is kept moist and hair
abrasions occur
inter digital between the fingers groin, axillary regions
(under arms),umbilicus, feet and nails• bacteria may be
involved in a secondary invader nail infections
onychomycosis
diaper rash may be caused by a species of Candida
C. Systemic involvement
1) Endocarditis - heart
Predisposing conditions: drug addicts using unclean needles
preexisting valvular disease people treated with antibiotics
intravenous infusion = gets into tubes of machine
2) Urinary Tract
Bladder and kidney included more common in women
than men, yeast can be found in urine with no obvious
infection present
Unit 3: Mycology
147
3) Meningitis relatively rare.
4) Septicemia
In blood and potentially fatal patients often predisposed
through antibiotic therapy or a result of having leukemia
D. Allergic Diseases
Candidiasis- similar to the dermatophytosis reaction
caused by dermatophytes
Eczema- Reddening and itching of skin, may become
crusty and scaly
Gastritis
Cryptococcus
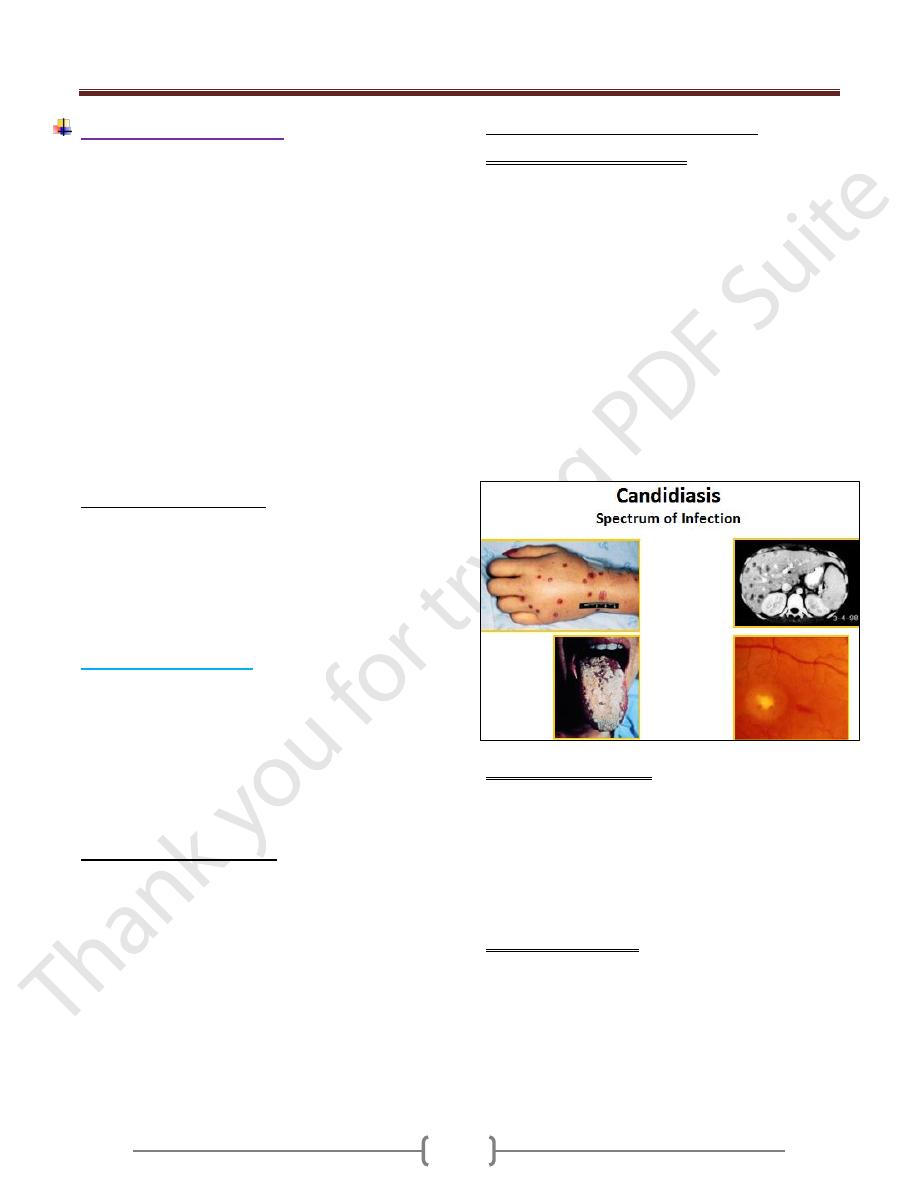
The genus Cryptococcus contain different Spp.,
Cryptococcus neoformans
is considered the most
important human pathogen.Cryptococcus neoformans is
an encapsulated fungus ,this yeast occur widely nature
and found abundantly in dry pigeon feces. C.neoformans
cause cryptococcosis after inhalation of yeast from lung,
these yeast migrate to the CNS but also involve other
organs (skin,eye,prostat).Cryptococcosis is usually
associated with immunocompromized person especially in
AIDS patients.
Morphology and identification
C.neoformans grow at 35C to 37C,. Whitish mucoid is
produced within 2-3 days. The microscopical examination
of colony or clinical materials appears as spherical, single
or multiple budding thicked wall yeast surrounded by
thick unstained capsule. All members of genus are
encapsulated and produce urease by its ability to grow at
37C .There are 5 serotypes of Cneoformans (A-D and
AD), A and D are the most common worldwide.
Pathogenesis
Initial cryptococcal infection begins by inhalation of fungus
into the lung initially followed by hematogenous spread to
the brain meninges .Development of meningitis being the
first indication of the disease. The primary pulmonary
infection may be asymptomatic or mimic flu like influenza
respiratory infection, resolve spontaneously. Involvement
of the eye, skin, prostate are seen. The inflammatory
reaction is minimal & granulomatous.
Diagnosis Lab. test
Specimen: CSF,exudate,sputum,blood and serum. CSF is
centrifuged before microscopical examination & culturing
Microscopical examination: The diagnosis of
Cryptococcus depends on demonstrating the organism or
its capsule in tissue or body fliud The specimen mixed
with India Ink,the yeast cell is seen microscopically by a
wide, unstained capsule .Demontsration of the pathogen
on an India Ink preparation is pathognomonic for
C.neoformans.
Culture: The organism can be cultured from CSF or other
specimen on most fungal media at room temperature or
37C. The diagnosis ofthis organism is confirmed by
urease test
Serology: test for capsular antigen can be performed on
CSF or serum.
The latex slide agglutination test for cryptococcal antigen
is positive in 90% of patients with cryptococcal
meningitis.
Treatment and prevention
Amphotericin B with or without flucytocin is curative in
most of the cases of meningitis or disseminated disease.
There is no specific mean of prevention.Fluconazol is
used in AIDS patients for long term suppression of
cryptococcal meningitis.
Epidemiology
Birds (pigeons) are considered to serve as reservoir of
infection but the birds are not infected .The organisms are
transmitted by respiratory droplets
Aspergillosis
Aspergillosis is a spectrum of human disease that may be
caused by Aspergillus Spp .these species are saprophytic
organism and widely distributed in nature and found
throughout the world .The most common human pathogen
is Aspergillus fumigatus,and to lesser extent A.niger,
A.ilayus and A.terreus.
This mold produce abundant conidia that easily dispersed
into environment Human become infected by inhaling
them. A topic individual may develop severe allergic
reaction to the conidial antigen. The conidia may
germinate to produce hyphae and invade the lung or other
tissue ,these may occur in immunocompromized patients
but also causing invasive lung infection including external
otomycosis ,mycotic keratitis, OnychomycosiS, Sinusitis
and CNS infection.
Morphology and Identification
Aspergillus spp. Exist only as mold,they are not
dimorphic ,these Spp. Are grow rapidly producing aerial
septate hyphae that form V shaped branches and long
conidiophore expand in vesicle and phialides are
produced directly from the vesicle surface and phialides
Unit 3: Mycology
148
produce besipetal chain of conidia .The Spp, Are
identified according to morphologic differences in these
structure including the size, Shape, texture and color of
conidia.
Aspergillus
Moulds
True hyphae
Exogenous, airborne
o Soil
o Water / storage tanks in hospitals etc
o Food
o Compost and decaying vegetation
o Fire proofing materials
o Bedding, pillows
o Ventilation and air conditioning systems
o Computer fans
Portal of entry: nasal passages, respiratory tract
Potential for hospital outbreaks
Pathogenesis
In the lung, alveolar macrophage are able to engulf and
destroy conidia,in immune compromized patients
especially leukemia ,bone marrow transplant the conidia
may smell and germinate to produce hyphae that invade
the preexisting cavities (Aspergilloma or fungal ball) or
blood vessel.
Clinical findings
A. Allergic form A topic individual often develop severe
allergic reaction to conidial antigen elicits an immediate
asthmatic reaction and after subsequent exposure in
another hand the conidia germinate and hyphae colonize
the bronchial tree without invading the lung parenchyma
,this phenomena is characteristic allergic
bronchpulmonary aspergillosis presented with asthma,
chest infiltration ,eosinophilia with type one and type
three skin test hypersensitivity
B. Aspergilloma and Extra pulmonary colonization:
Patients who have already a chronic pulmonary disease
(TB and Sarcoidosis) Fungus ball called aspergilloma
within a preexisting cavity.
C. Invasive Aspergillosis
Following inhalation and germination of conidia,invasive
disease develop as an acute pneumonic process
characterized by fever, cough ,hemoptysis from the lung,
the disease may spread to the GIT ,kidney, liver ,brain or
other organ producing abscess and necrotic lesion even
when hyphae invade the wall of the blood vessel. Patients
at risk are those with lymphoma and leukemia.
Diagnostic Lab. Test
A. Specimen: sputum or other respiratory secretions or lung
biopsy.
B. Microscopical examination: Sputum treated with KOH
or Calcofuor white should examined directly under
microscope show septate,branching hyaline hyphae.
C. Culture: Culture show colonies which differ according to
the morphology of their conidial structure when grow
within few days on media at room temp.
D. Serology:-The Intradermal test for precipitin to
A.fumigatus is positive in over 80% of patients with
Aspergillosis or allergic form of Aspergillosis.
Treatment
Aspergilloma treated with Itraconazol with Amphotericin
B and surgery Invasion Aspergillosis require rapid
adminstration of Amphotericin B,vericonazol,flucytocin
also used.Allergic form treated with corticosteriod or
sodium cromoglycate.
Epidemiology:
Avoid exposure to the conidia in person at risk for allergic
disease leukemic; lemphoma patients with bone marrow
transplant should minimize their risk of exposure to conidia
