Unit 3: Helminthes (Nematodes)
86
Lecture 2+3+4+5 - Intestinal
nematodes
Enterobius vermicularis
Also called pinworm
It has a cosmopolitan distribution, but it is more common
in cool or temperate zone than in tropical areas.
Epidemiology:
Pinworm infection is prevalent in large family groups and
in schools and mental institution.
Contamination of clothing, bedding is a frequent cause of
familial outbreaks
The infection is more common in children than adults,
also prevalent where small children sleep together, and in
any population in which underclothing is worn day after
day and bathing is infrequent.
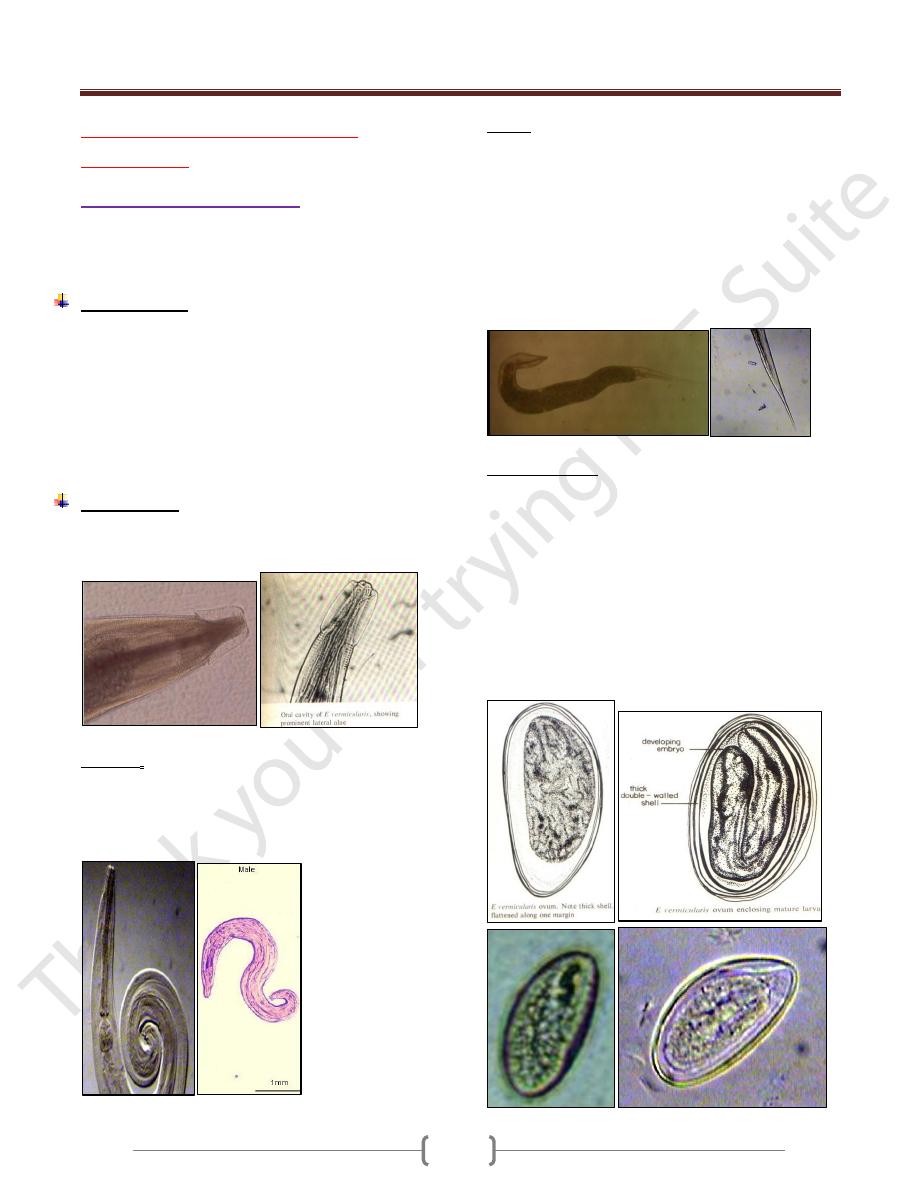
Morphology:
The adult male and female have an anterior expansion
from both side (ventral and dorsal) called (cervical alae).
The male measures up to 5 mm long with maximu m
width of 0.1- 0.2mm width.
The posterior end is strongly curved and the lateral view
of the worm forms an inverted question mark.
The male rarely seen as it die after female fertilization.
Female length 13 mm and 0.3-0.5 mm width. They are
light yellowish white.
The posterior end is sharply pointed and forming 1/3 of
the total length.
The male rarely seen as it die after female fertilization.
The adult worm inhabits the cecum and adjacent area of
the intestine.
Gravid female migrate down the bowel to the rectum and
during hosts sleep or relaxation, they crawl out of the anus
onto the perianal area and perineal skin.
Eggs morphology:
Eggs in utero are not fully embryonated when the female
worms migrate to the lower level of the colon.
Female discharge about 10,000 eggs. The eggs discharged
on the skin are essentially mature and within few hours
(about 6 hrs) contain a fully developed infective stage larva.
The eggs are flattened on one side and convex on the
other. It measures about 50-60µm by 20-30 µm. They
have a colorless inner double shell and an outer
albuminous layer that causes them to stick to each other
and to clothing and other objects.
Unit 3: Helminthes (Nematodes)
07
Mode of infection:
1) By swallowing fully developed eggs with food or water.
2) Inhalation of eggs (light infection).
3) Autoinfection
4) Retroinfection.
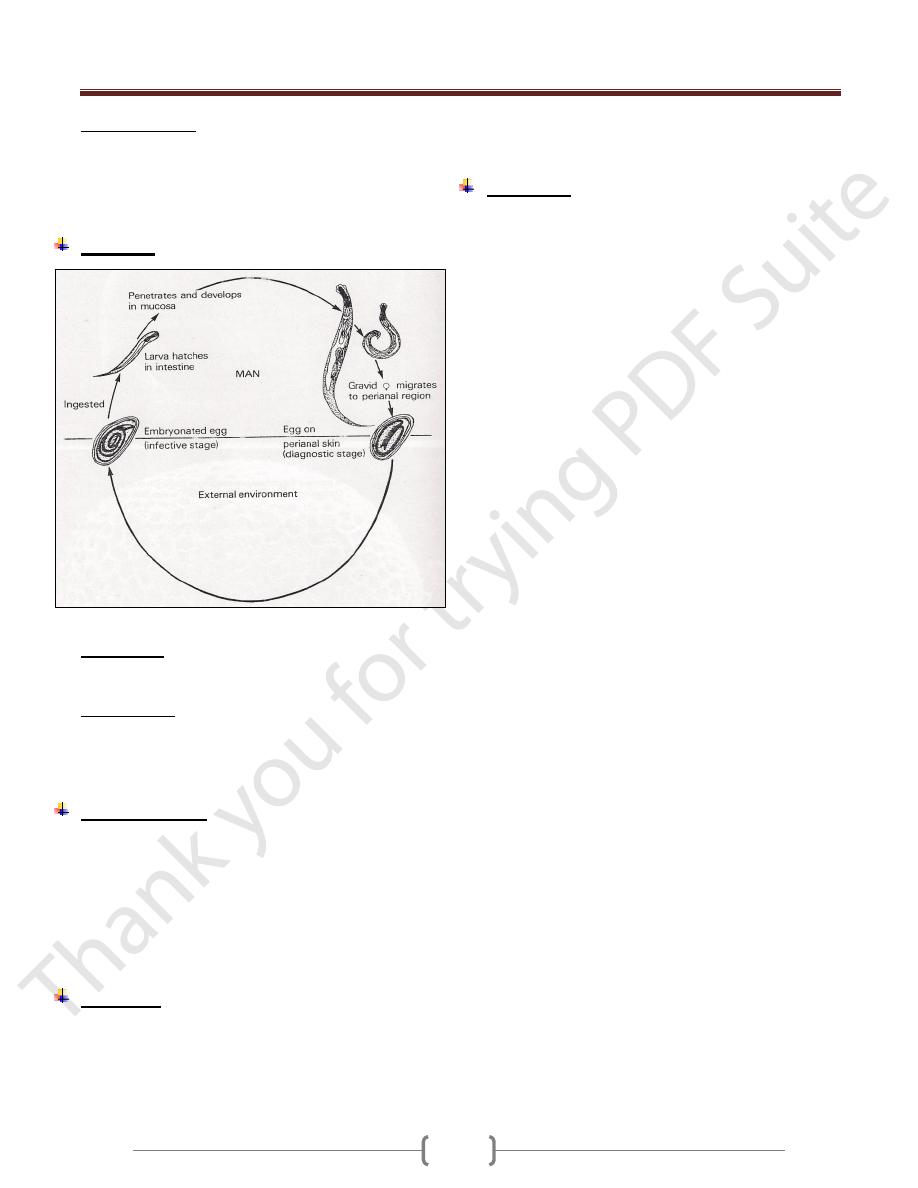
Life cycle
Development of the adult worms require about 6 weeks.
Autoinfection
It develops when the eggs are carried to the mouth by
fingers after scratching the itching skin.
Retroinfection:
It involves hatching of the embryonarted eggs after their
deposition in the perianal area and subsequent migration
back into the rectum and large intestine.
Clinical features
The first recognizable symptom is pruritus as the worms
emerge from the anus to the perianal skin.
Itching followed by scratching which predispose to
secondary bacterial infection.
The infection also induce sleep disturbance especially in
children.
In some cases, no symptoms appear.
Diagnosis:
The eggs are recovered from perianal skin by using scotch
tape technique and examined microscopically.
The technique preferably done at night or in the early
morning before bathing.
The eggs can't be seen in the stool, although the adult
female can be seen in the stool or near the anus.
Treatment:
A Single dose of mebendazole 100mg or albendazole
400mg or pyrantel pamoate 10mg/Kg .These drugs kill
only the adult worm in the colon but not the eggs, so the
treatment should be repeated after 2 weeks to kill any
adult worms that might have hatched from eggs present at
the time of initial treatment.
All family members should be treated. During this period
all night clothes and bed linen are laundered .Finger nails
must be kept short and hands washed carefully before
meals.
Reinfection after treatment is very common.
Unit 3: Helminthes (Nematodes)
07
Trichuris trichiura
Disease called Trichuriasis
It is a cosmopolitan and prevalent in worm or temperate
moist climates. In endemic area, the highest prevalence
occurs in children in of early school age, and adult also
have a high rates of infection.
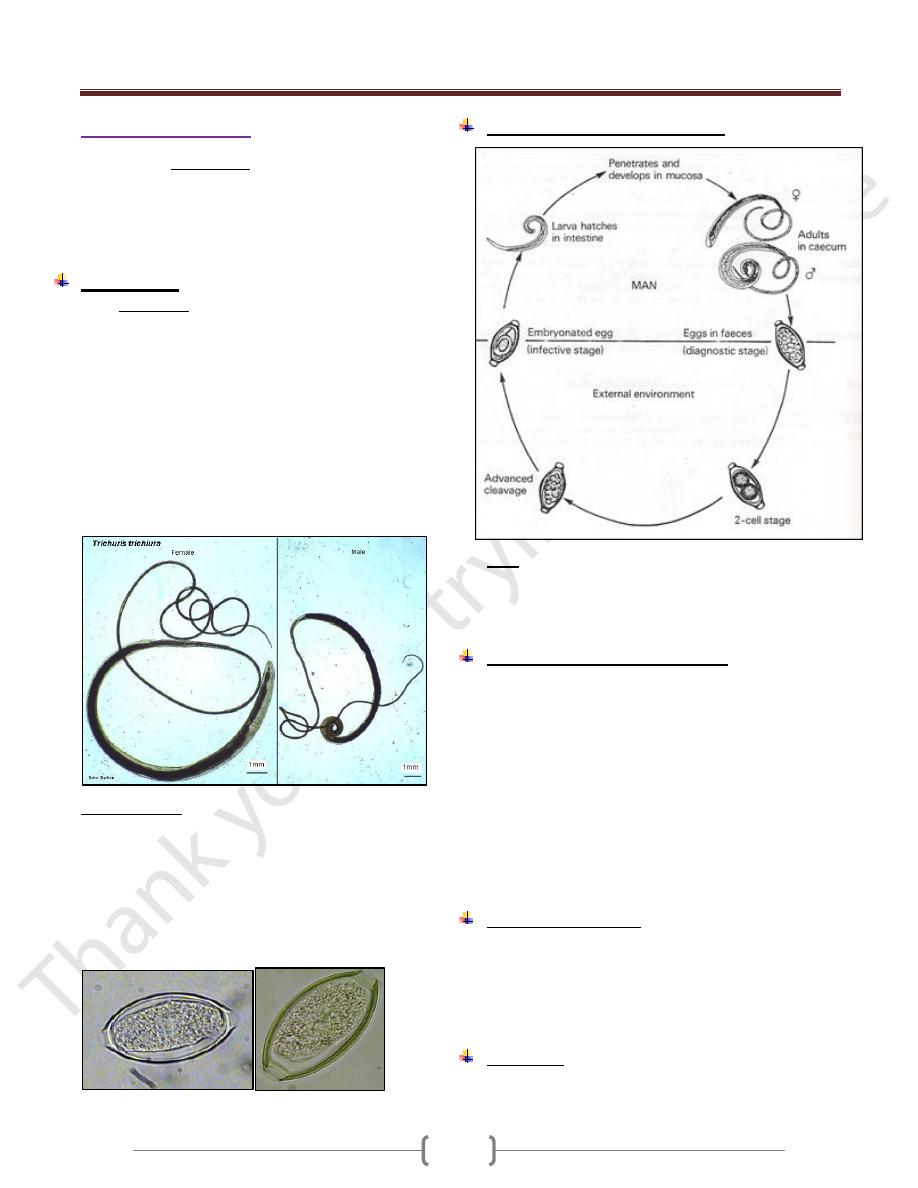
Morphology:
Adult whipworms are thread like in their anterior 3/5 of
the body and wider in the posterior portion.
The anterior end is threaded into the mucosal epithelium
of the cecum or the appendix but when the worm present
in large number , the worms are distributed posteriorly
throughout the colon , even in the rectum . Whipworms
live for several years.
The Male measures 30 – 45 mm. Its posterior end is
curved ventrally into a coil of 360˚ or more. The Female
measures 35-50 mm. Its posterior end is club shape.
Egg/mature female = 3000-6000 daily.
Egg morphology: Narrow, barrel –shaped about 25*55
µm, laid in an unembryonated condition (one celled –
stage) and requires about 4weeks outside the body to
reach the infective stage. They have a thin, transparent
inner shell, a brownish outer shell and a transparent blister
like prominence at each pole.
Eggs remain infectious for few months under favorable
condition but shorter time under unfavorable condition.
In saline In iodine
Life cycle of Trichuris trichiura
Note:
1-All stages of development occur in the intestine
2-Development of Trichuris trichiura to the egg-laying
adult stage requires approximately 3 months.
Pathogenesis and clinical features
Light infections produce no symptoms.
Although adult worms burrow their hair like anterior end
into intestinal mucosa, they don’t cause significant anemia.
Heavy infection (tend to be between 1-5 years)
characterized by abdominal pain and distention, bloody or
mucoid chronic diarrhea, tenesmus, weight loss and
weakness and rectal prolapse which is due to increase
peristalsis that occur in an effort to expel the worms. The
whitish worms may be seen on prolapsed mucosa.
Entamoeba histolytica infection is frequently found in
association with trichuriasis.
Laboratory diagnosis
1) General stool examination to see the characteristic eggs.
2) Diarrheal or dysenteric stools contain eosinophils and
Charcot-Leyden crystals.
3) Adult or immature worms may be seen attached to the
prolapsed rectum or at sigmoidoscopy.
Treatment
Albendazole 400 mg/day for 3 days. Alternative is
Mebendazole 100 mg twice daily for 3 days or 500 mg once.
Unit 3: Helminthes (Nematodes)
07
Ascaris lumbricoides
The disease is called Ascariasis
It is the largest intestinal nematodes
With exception of Enterobius vermiculartis, Ascaris
lumbricoides is the most prevalent of all human
roundworms and occurs endemically in all parts of the
world except in cold, dry climates.
Morphology
Adult worm is elongated, cylindrical and tapers both
anteriorly and posteriorly to relatively blunt conical ends.
The heads is provided with three fleshy lips.
The mature male worm measures 12-31 cm in length by
2-4 mm in greatest diameter.
Its posterior end is somewhat curved ventrally.
The female measures 20-35cm in length by 3-6 mm in
greatest diameter but in certain cases, up to 45 cm may b e
observed.
Daily egg production per female averages about 200,000.
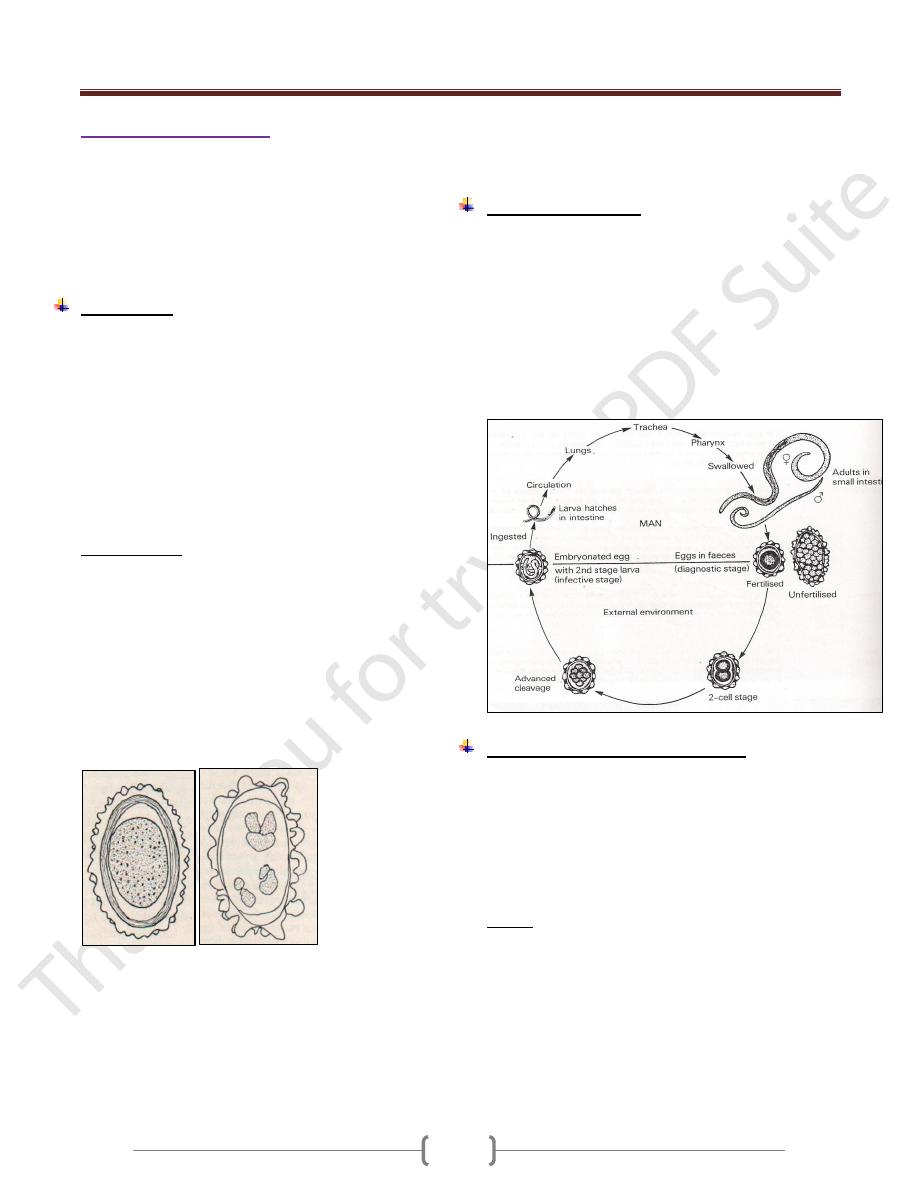
Egg morphology (Fig 1 &Fig 2)
The fertilized egg (figure 1) at the time of oviposition is
spherical or subspherical, measures 65-75 µ m by 35-50 µ
m and consists of the following:
1) a coarsely granular , spherical ovum that usually doesn’t
completely fill the shell
2) A thin innermost membrane that is highly impermeable.
3) A relatively thick, colorless middle layer that is smooth
on both inner and outer surfaces.
4) An outermost, coarsely mammilated, albuminoid layer
laid down in utero serving as a protective membrane.
Figure 1 fertilized egg Figure 2 unfertilized egg
Female worms without males produce infertile eggs that
are markedly subspherical.Interrnally they contain a mass
of disorganized granules and globules that completely fill
the shell (Figure 2).
Fertile eggs are passed in one cell stage. They survive
putrefaction and can withstand desiccation and cold. At
22 – 33C˚, development to the infective stage larva
usually occur s in 3-4 weeks. Eggs remain viable in soil
for more than a year.
Life cycle (Figure 3)
Ingestion of emryonated eggs in food or water
contaminated with human feces , eggs hatch in the small
intestine , larva migrate through the gut wall into the
blood stream and then to the lungs. On about the 9
th
day
of infection, they, pass up the bronchi and trachea and are
swallowed. Within small intestine, they become adults 8-
12 weeks after exposure. They live in the lumen don’t
attach to the wall, and derive their substance from
ingested food.
Pathogenesis and clinical features
1) In the stage of larval migration, passage through the liver
and lungs in the initial infection provokes no remarkable
pathologic changes unless hundreds of larvae are
migrating simultaneously.
2) Large No. of larvae in subsequent infection lead to intense
tissue reaction in the liver and lungs even if few larvae are
involved.
Liver:
In the early stage, focal eosinophilic infiltration and
granuloma formation around and in the paths of migrating
larvae and general inflammation around the portal tract.
Later, fibrosis of the periportal and interlobular space.
The cardinal symptoms associated with Ascaris
pneumonitis consist of fever ( moderate – 40C),
productive cough, dyspnoea and high transient peripheral
eosinophila and Chest x-rays shows scattered, s hifting
mottling of the lungs (these picture is variable from day to
Unit 3: Helminthes (Nematodes)
07
day and spontaneously clears after a few days to 2 weeks).
Pulmonary infiltration and peripheral eosinophilia is
called Loffler's syndrome. Migrating larvae may also be
seen in the sputum. Pulmonary Ascariasis appears to be
most common and severe in endemic area and sometime
fatal, even in adults.
When adult worms present in the small intestine in small
No., usually cause no symptoms.
Average infection in children cause intermittent colic, loss
of appetite, and nervous symptoms.
The nutritional demands and space requirements of
massive infection may be great and the total mass of
worms may reach to 1 liter and may lead to nutritional
impairment especially in children.
From time to time worms are passed spontaneously,
unassociated with illness and these events are of no
special significance. If there is an febrile illness, the
worms migrate outward in both directions or aggregate in
closely packed masses that will obstruct the bowel.
Sometimes the worms may enter and block the biliary and
pancreatic ducts or sometimes reach the liver and form
liver abscess which is more common than that of
E.histolytica sometimes the worm may reach the lung
from the intestine or may reach the nasopharynx and
emerge from the nares.
NOTE:
1- The survival time of mature A.lumbricoides in human
intestine is short and not exceeds a year.
2- Ascariasis is frequently associated with whipworm
infection as well as diseases due to other causes.
Diagnosis:
In the early stage of disease, diagnosis is difficult unless
there is an immature worm passed.
Once the worm in the intestine and eggs are passed by the
mature worms, the diagnosis can be made with ease by
detecting eggs in the stool. Sometime the patient sees
adult worms in the stool.
Treatment:
Albendazole 400mg on1ce
Mebendazole 100 mg twice daily for 3 days.
Pyrantel pamoate.
Epidemiology:
1) Endemicity is maintained by fecal contamination of soil.
2) Eggs are relatively resistant to desiccation, and
embryonation takes place in clay soil as well as in loam.
3) Infective stages eggs remain viable for weeks, months, or
even years.
4) Dirt eating is responsible for heavy infection in small
children.
5) Hogs infected with Ascaris sum probably an occasional
source of intestinal ascariasis in man and the larva make
lung migration and sometimes develop to adult stage in
man.
6) Ascaris of human origin may develop to adult stage in
pigs.
Control
1) Anthelmintic drugs.
2) Home and community sanitation
3) Mass treatment repeated at intervals of 2 months – 2 years.
Unit 3: Helminthes (Nematodes)
07
Hook worms
Belong into 2 genera: Necator and Ancylostoma
Ancylostoma duodenale (Ancylostomiasis)
"Old world hookworm"
Morphology
Adult worm are grayish white or pinkish. The body is
narrowed anteriorly.The head has a slight bend dorsally.
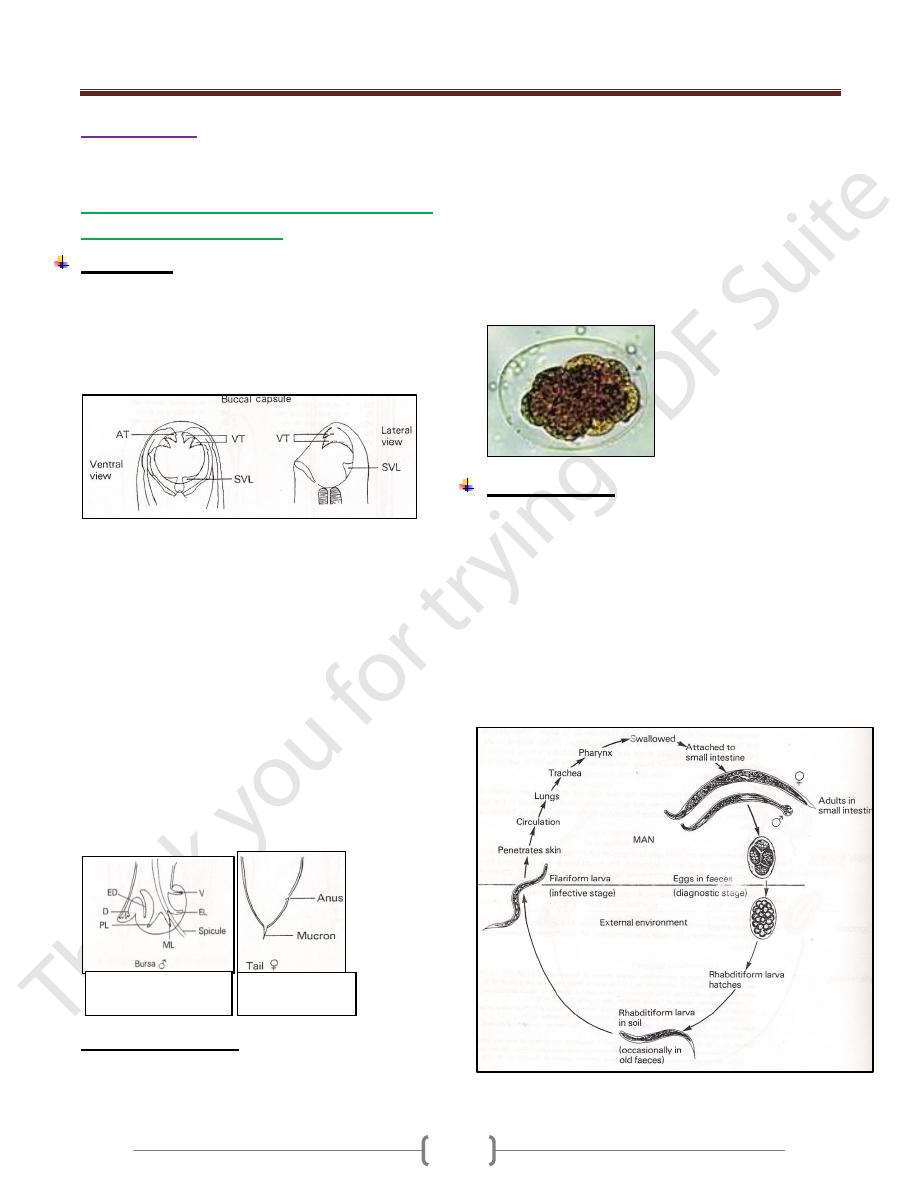
The mouth (figure 1) is well developed, with a pair of
teeth on either side of the median line and a smaller pair
in the depth of the buccal capsule.
Figure 1: mouth part of adult worm (male and female)
Male measures 8-11 * 0.4-0.5 mm in width.
The posterior end (figure 2) is provided with a prominent
copulatory bursa that is broader than it is long and is
supported by rays having the following pattern for each
half: a dorsal, single at its root but bifurcated at the tip,
externodorsal ,arising from the root of the dorsal; three
laterals separated from one another and two ventral close
to each other.
Female measures 120-13*0.6mm in width and tapered at
the posterior end (figure 3). The anus lies ventrally near the
caudal tip and the vulvar opening is situated mid-ventrally
at the beginning of the posterior third of the body.
Female lies around 20,000 eggs daily. Man is probably
the only normal host of
Ancylostoma duodenale.
Eggs morphology (Fig 4)
The egg is broadly ovoid measures 60 by 40 m , have a
thin , transparent shell , and are in the 2-8 cell stage of
cleavage when evacuated.
Embryonation to the first rhabditiform larval stage takes
place in 24-48 hr on moist sandy loam in a shaded
environment and 25 c .The rhabditiform larva measures
0.25-0.3 µm in length by 17 µµm in maximu m diameter.
It feeds on bacteria and organic debris, grows, sheds its
cuticle and continues to feed and increase in size.
After 5-8 days the rhabditiform larva stop feeding,
becomes inactive, and transforms into a more slender
filariform larva which has closed mouth, an elongated
esophagus and a sharply pointed tail.
Life cycle (Fig 5)
In Ancylostoma duodenale, the filariform larva is adapted to
enter the body by the oral as well as by the skin. After skin
penetration , the larva carried by blood to the lungs ,
migrate into the alveoli and up the bronchi and trachea and
then swallowed to reach the small intestine and develop
into adults and attached to the wall of the intestine with the
aid of the teeth. They feed on blood from capillaries of the
intestinal villi.6 weeks is required from the time filariform
larva enter the skin until the worms become mature in the
intestine , copulate and begin to lay eggs which passed with
feces to repeat the cycle.
Figure 3 posterior
e nd of female
Figure 2 Bursa
(posterior end) of male
Unit 3: Helminthes (Nematodes)
07
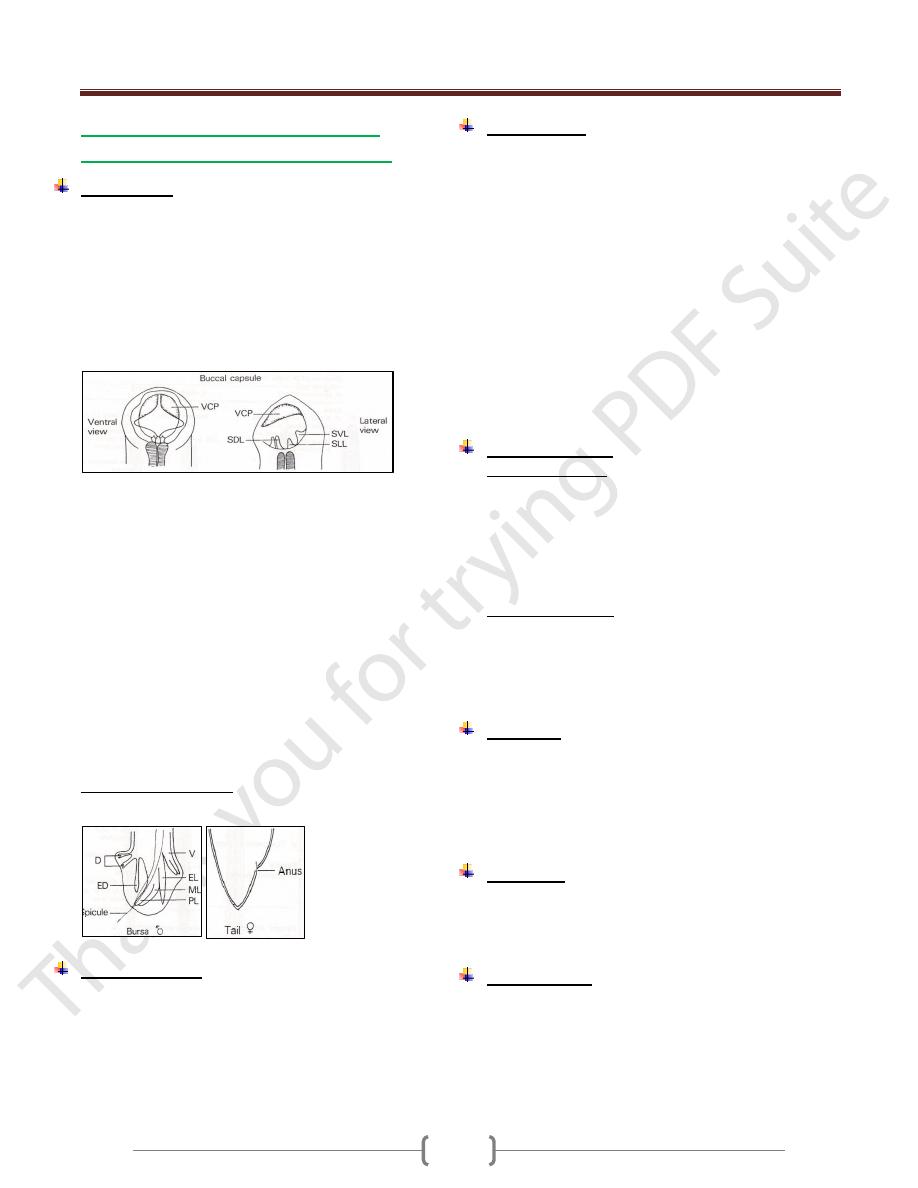
Necatror americanus (Uncinariasis,
necatoriasis), New world hook worm.
Morphology
The adult worm is strongly flexed dorsally at the ant. end.
The small buccal (figure 6) capsule is provided with 2
ventral cutting plates,2 poorly developed dorsal
plates((median dorsal )and in the depth of the mouth
cavity a pair of short triangular lancets. A pair of cephalic
glands opens into the buccal capsule that secretes an
anticoagulant. The esophagus bears a pair of ventrolateral
glands and dorsal gland which secrete proteolytic enzyme.
Figure 6: mouth part of adult worm (male and female)
The male measures 7-9 mm in length by 0.3 mm in width.
The copulatory bursa is symmetrical. The supporting rays
for each half consist of a small separated dorsal,
bifurcated at the tip; a slender, unbranched externodorsal;
three larterals arising from a large fleshy trunk; 2 ventral
fused half way or more to the tip; and short prebursal ray.
The two copulatory spicules are long that are fused at
their outer ends terminating in a barb [figure 7: Bursa
(posterior end) of male].
The female measures 9-11 mm in length by 0.4 mm in
width. The vulvar opening is midventral anterior to the
midline (figure 8: posterior end of female). the female
lay 5000 eggs /day
Egg morphology (fig. 4)
Similar to that of Ancylostoma duodenale
Life cycle (Fig 5)
Similar to that of Ancylostoma duodenale but the
filatiform larva is adapted to enter the body only through
skin penetration of the epidermis , where they remain
relatively inactive for 1 or 2 days before moving deeper to
the cutaneous blood vessels.
Pathogenesis
1) Larva may cause allergic inflammation at the site of entry
through the skin and in heavy infection, passage through
the lungs may cause pulmonary eosinophilia.
Anemia as the worm suck blood from the intestine. blood
loss of Ancylostoma duodenale =0.15 ml /worm/day while
in Necatror americanus = 0.03 ml / worm/day. It is of
hypochromic microcytic anemia. In light and moderate
infection with good nutrition, blood loss can be
compensated .In severe infection anemia is inevitable.
2) A complete normal mucosal pattern of the small intestine.
3) Malabsorption is uncommon and it is not a characteristic
of pure hook worm infection.
4) Necatror americanus may survive as long as 18 years and
Ancylostoma duodenale lives for 1-5 years.
Clinical features
A. In acute infection :
1) Skin penetration by the larva cause allergic reaction
known as ground itch which is more severe in
Necatror americanus than Ancylostoma duodenale.
2) Pneumonia in case of heavy infection.
3) When the worm reach the small intestine, vomiting,
epigastric pain and sometime diarrhea.
B. In chronic infection.
1) Sign and symptoms due to iron deficiency anemia.
2) Hypoprotenemia due to long term complication of
IDA manifested by facial and peripheral edema.
3) Pica, ingestion of nonfood constituent as a result of IDA.
Diagnosis
General Stool Examination for eggs demonstration.
In a stool sample that is not fresh, the eggs may have
hatched to release rhabditiform larvae, which need to be
differentiated from those of Strongyloides stecolaris.
Test for occult blood in the stool in case of heavey infection.
Treatment
Albendazole single dose of 400 mg for both n and a
Mebendazole 100 mg twice daily for 3 days.
Correction of anemia.
Epidemiology.
Hook worms infection is widespread in tropics & subtropics.
Ancylostoma duodenale is endemic in the Far East and
Mediterranean coastal and in Africa
Necatror americanus endemic in west, east and central
Africa and central & south America as well as in Far East.
Unit 3: Helminthes (Nematodes)
08
A Human Hookworm Vaccine is currently being
developed by the Sabin Vaccine Institute & is in phase 1
clinical testing.
The candidate vaccine is comprised of two recombinant
antigens known as Na-GST-1 and Na-APR-1, each of
which is an important parasite enzyme required for
hookworms to successfully utilize host blood as a source
of energy. Na-GST-1 is a 24 kDa recombinant N.
americanus glutathione- S-transferase , while Na-APR-1
is a 45 kDa recombinant N. americanus aspartic protease.
Strongyloides and other Rhabditoidea
The rhabditoidea is a large group containing mostly,
small, free-living forms, some of which may be
encountered as pseudoparasites in human feces, urine,
gastric washing, or sputum. The parasitic members of
rhabditoidea are unique in that they have an alternation of
free-living and parasitic generations. Adults of the free
living generation are dioecious, while in the parasitic
generation the adult is parthenogenetic.
Strongyloides stercoralis (Strongyloidiasis)
Morphology
The slender parasitic female measures up to 2.7 mm in
length by 30- 40 µm in diameter.
The normal habitat is the mucosal epithelium of the upper
small intestine
Reproduction is parthenogenetic.
Egg morphology
Thin- shelled ovoid eggs, 50-58 µm by 30-34 µm are laid
in the epithelium .Each female producing < 50 eggs /day.
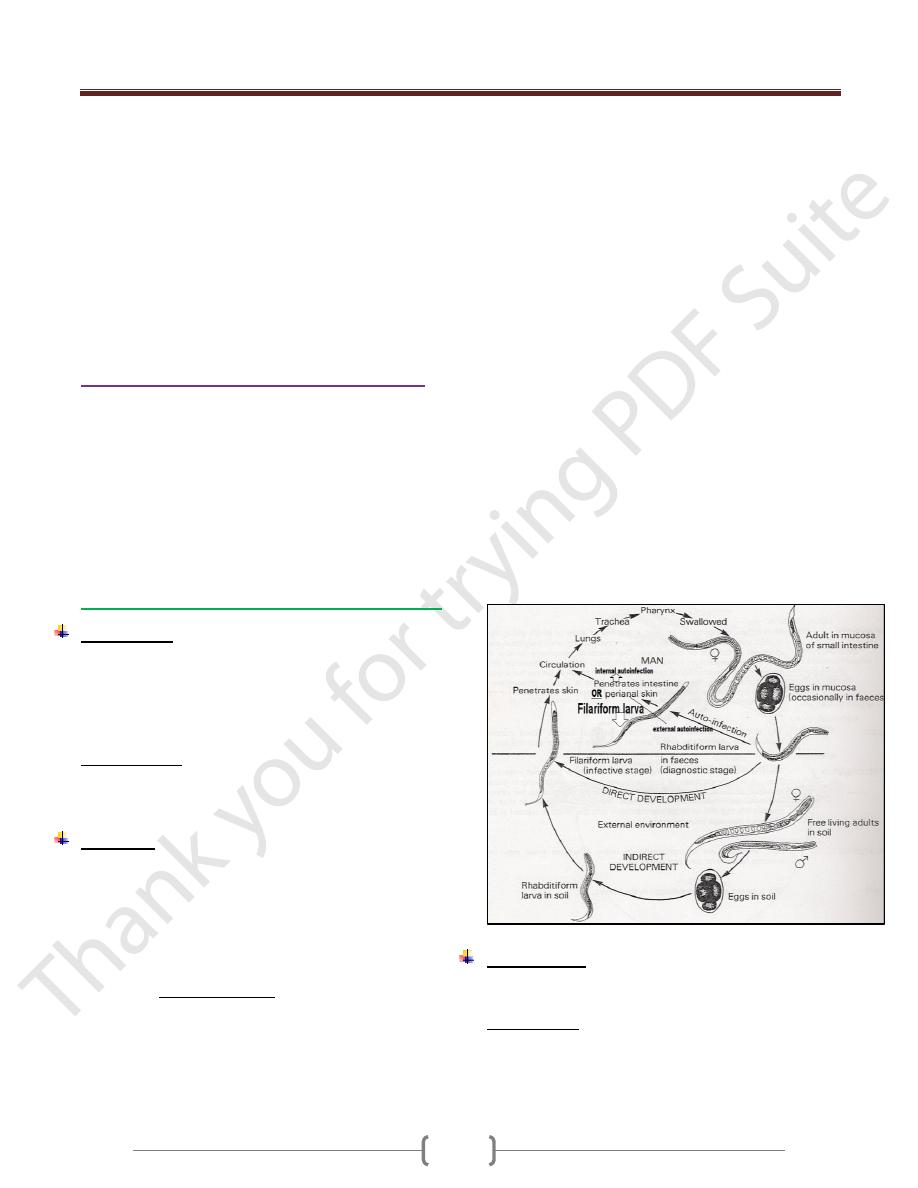
Life cycle
There are direct and indirect developments.
The eggs after being laid by the female, they undergo
development and are sloughed into the lumen of crypts of
lieberkuhn, where the first stage rhabditoid larva hatches.
Larvae then migrate into the intestinal lumen and are
evacuated in the stool. If deposited in a warm, moist,
shaded, site, direct development to the third stage
filariform larva may occur 24-36 hrs in the fecal mass or
in the soil. This larva initiates infection by skin
penetration.
Under certain condition, the first stage larva develops to
the infective stage within the intestinal tract , and the larva
can reinfect the host by penetrating the mucosa of the
colon without leaving the body (internal autoinfection) or
by penetrating the perianal or perineal skin after being
passed in the stool (external autoinfection). Autoinfection
occurs at low level in healthy individual and at high level
in immunodeficient patient resulting in a disseminated,
fatal infection.
After the first stage larva reaches the external
environment in feces, it will develop to free living
rhabditoid adults in 2-4 days (indirect development). The
male which is about 0.9 mm long with caudal end curved
ventrally. The female is about 1.2 mm long and contains
up to 28 eggs in its two uteri. After the eggs are deposited
by the female, they rapidly develop to the infective
filariform larval stage.
On contact with skin, the filariform larvae (in direct or
indirect development ) penetrate the epidermis to the
small blood vessels and are carried to the lungs, then they
reach the pulmonary capillaries , break out into the
alveoli, then via trachea, to the intestine, where they
invade the epithelium of the glands , molt twice, and
reach maturity in about 2 weeks. The most common level
of the intestine parasitized by Strongyloides stercoralis is
the duodenum, followed by the jejunum.
Pathogenesis
Minor local lesions occur on penetration of the larv a into
the skin.
Larva currens: a transient itchy linear urticarial wheels
across abdomen and buttocks.
The pulmonary response to larval migration is not so
severe but in heavy infection, pneumonitis may occur and
Unit 3: Helminthes (Nematodes)
00
the larva may be seen in sputum and even s ometimes the
eggs or adult form may be seen in sputum.
The adult female produces extensive ulceration and
sloughing of the mucosa and fibrosis and inflammatory
infiltration of the submucosal layers and granulomas
surrounding the larvae and these pathological changes
may be found in other affected organs.
Eosinophilia of 10-40%.
Total serum IgE is usually elevated.
Clinical features
Entry of the larva through the skin produces mild needling
sensation.
Pneumonitis may be produced by the larvae but it is less
severe than that of ascariasis.
The adult in the small intestine may give rise to no
demonstrable symptom or to moderate to severe diarrhea.
Malabsorption syndrome with steatorrhoea may occur.
Heavy infection may give rise to symptoms similar to
duodenal ulcer.
If the GIT and lungs are involved, the condition is
referred to as the hyperinfection syndrome which
present with dyspnoea, fever, GIT symptom, wheezing,
hemoptysis and cough.
When the numbers of migrating larvae are so great as to
injure other organ such as the liver , heart , adrenals,
pancreas , kidneys or central nervous system , this
referred as disseminated strongyloidiasis , seen
primarily in patients whose normal defenses have been
compromised e.g. HIV, chemotherapy, corticosteroid. It is
fatal unless diagnosed and treated early.
Diagnosis
Finding larvae in the stool. Repeated examination is
required as the excretion of the larvae is intermittent.
Treatment
- Ivermectin 200 µgm /Kg single dose.
- Albendazole 15 mg/Kg twice daily for 3 days. In
hyperinfection syndrome, 400 mg for 15 days.
S trongyloides
Hookworm
2
nd
stage larva
a) Rhabditiform esophagus
with a small buccal capsule.
a) Rhabditiform esophagus
with a large buccal capsule
b)Genital premordium large
b) Genital premordium small.
3
rd
stage larva
a) Esophagus 40% of the
length
a) Esophagus 25% of the
length
b) No sheath.
b) Sheath.
c) Tail forked
C) Tail pointed
Trichostrongylus sp.
The adults are 5-10 mm in length and are located in the
Small intestine.
They are mostly parasites of ruminants and infect humans
living in close proximity to these animals
Infection may occur by ingestion of the infective larvae or
by penetration of the skin.
The eggs are similar to that of hookworms but the ends
are more pointed and the ovum is passed in an advanced
cleavage stage.
Clinical features
Light infections are a symptomatic. In heavy infections
there may be anemia, abdominal pain and diarrhea.
Diagnosis
Eggs in the stool.
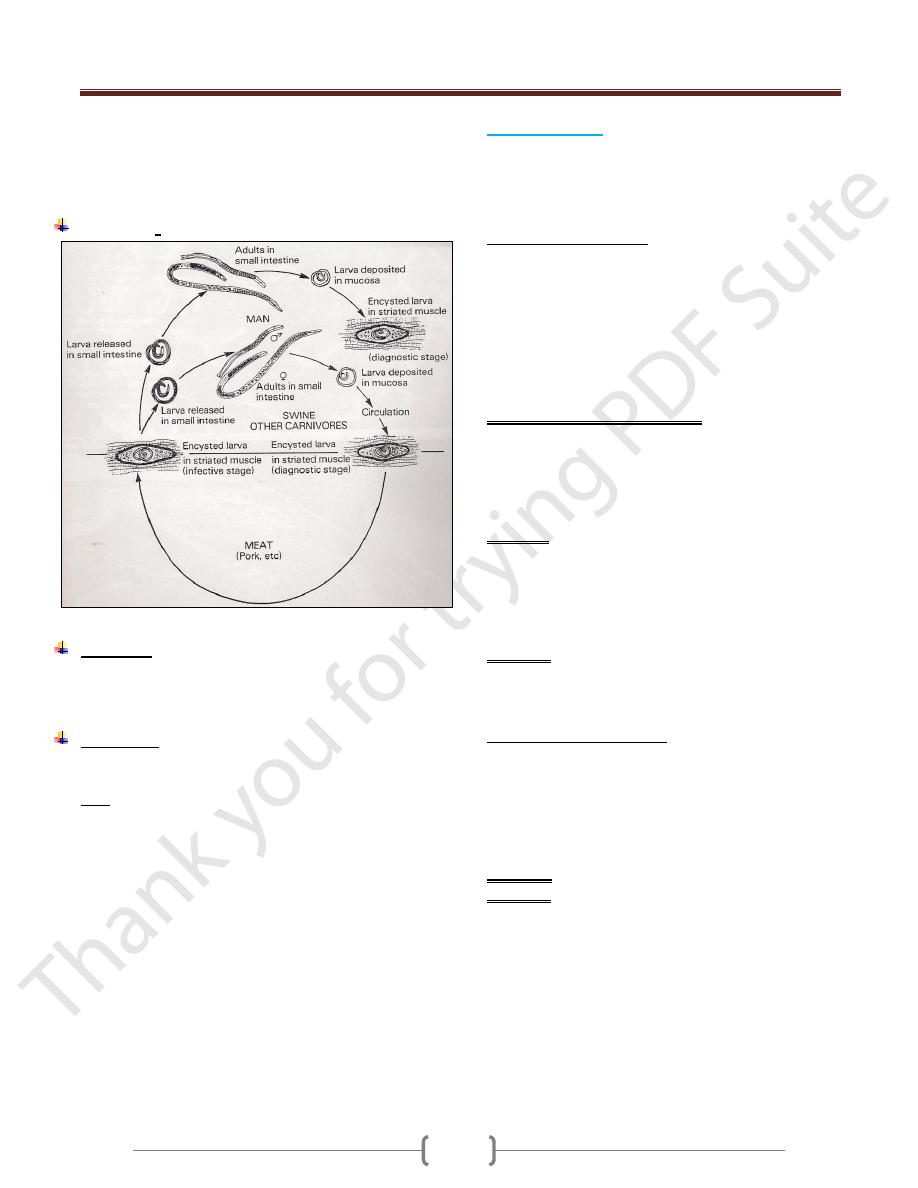
Trichinella spiralis (Trichinosis)
Trichinella spiralis is a parasite of rats and pigs and is
transmitted to humans by eating partially cooked pork
meat. The main tissue invaded is the striated muscle.
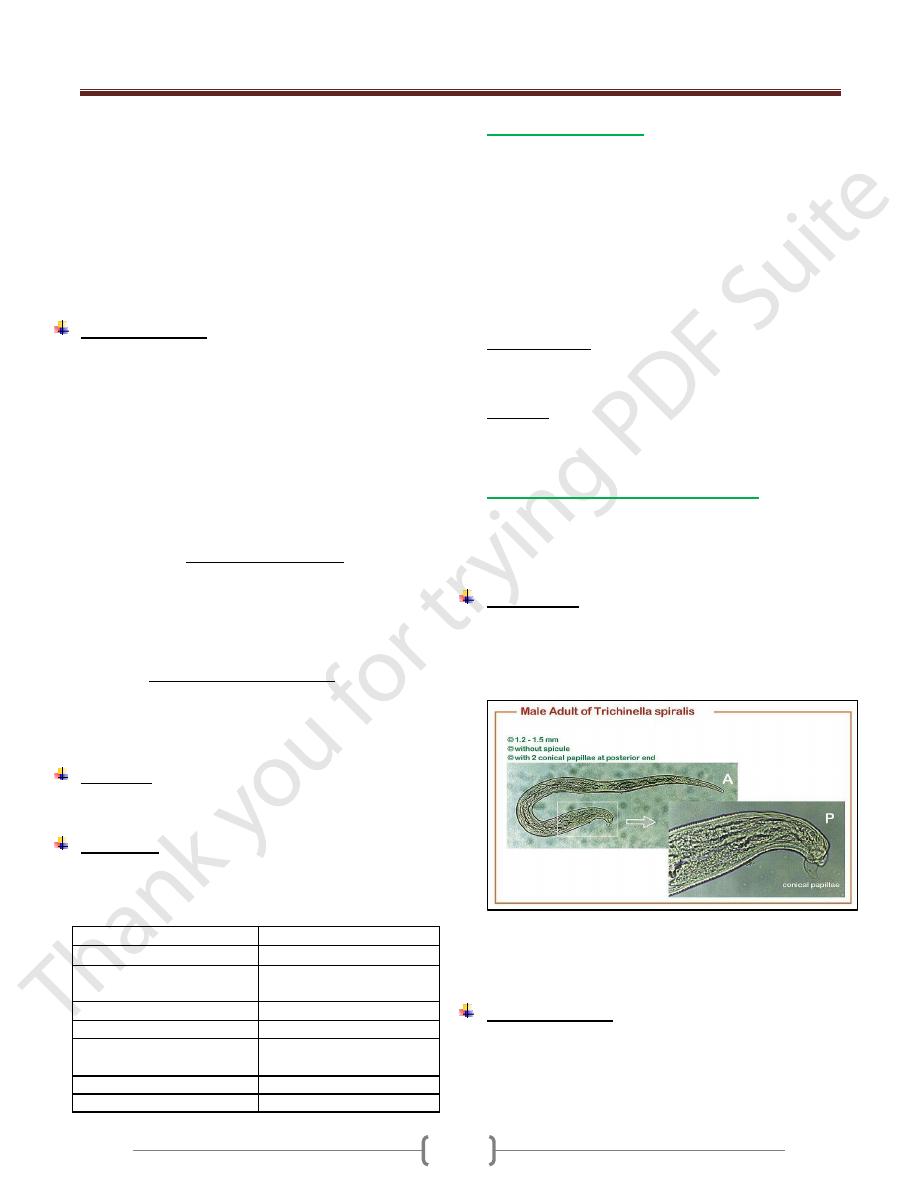
Morphology
The adult is minute, barely visible to the unaided eye. The
male measures 1.4-1.6 mm in length by 30-40 µ m in
diameter. The cloacal opening is terminal and is guarded
by a pair of conical papillae.
The female is viviparous measures 2.2 -3.5 mm by 50-60
µm in diameter. The vulva lies midventrally approximately
one fifth the body lengths from the anterior end.
Clinical features
A few days after eating undercooked meat, the patient
experiences diarrhea followed 1-2 weeks later by fever,
muscle pain, periorbital edema and
eosinophilia.Subconjunctival hemorrhage. Signs of
Unit 3: Helminthes (Nematodes)
06
cardiac and central nervous system disease are frequent
because larvae migrate to these tissues as well. Death
which is rare is due to congestive heart failure (CHF) or
respiratory paralysis.
Life cycle:
Diagnosis
1) muscle biopsy reveals larvae within striated muscle
2) Serological tests, (bentonine flocculation test), become
positive 3 weeks after infection.
Treatment
- Albendazole 20 mg/Kg for 7 days
- Steroid to control the effects of acute inflammation.
Note: there is no established specific therapy for tissue
phase of Trichinosis.
Larva Migrans
It is a term applied to the migration of larval helminths in
hosts that are suitable for long survival but are unsuitable
for their development to the mature adult stage. There are
2 types of larva migrans:
1) Visceral larva migrans
Toxocara canis is the major cause of visceral larva
migrans
The definitive host for T.canis is the dog .Humans ingest
soil containing the eggs, which hatch into larvae in the
small intestine. The larvae migrate to many organs
especially, the liver, brain, and eyes. The larvae
encapsulated and die. The life cycle is not completed in
humans; humans are therefore accidental dead –end host.
Pathogenesis and clinical features
- Granuloma around the larvae as a result of delay type
hypersensitivity reaction (DTH).
- The most serious clinical finding is blindness associated
with retinal involvement, fever, splenomegaly and
eosinophilia.
Diagnosis
- Definitive diagnosis depends on visualization of the
larvae in tissue.
- Serologic tests are commonly used
- The presence of hypergammaglobulinemia and
eosinophilia support the diagnosis.
Treatment
- Albendazole or mebendazole.
- Many patients recover without treatment.
2) Cutaneous larva migrans
It is caused by the filariform larvae of Ancylostoma
caninum (dog hookworm) and Ancylostoma braziliense
(cat hookworm).
The larvae penetrate the skin and migrate through the
subcutaneous tissue causing an inflammatory response.
The lesions (creeping eruption) are extremely pruritic.
Diagnosis: clinically.
Treatment: Oral or topical thiabendazole is effective.
