Unit 3 - Immunological factors in disease
20
Lecture 1 - Functional Anatomy &
Physiology of the immune system:
Functions of Host immune system:
1) To protect the host from pathogens while minimizing
damage to self-tissues.
2) Limits excessive responses that might lead to
autoimmune diseases.
Dysfunctions or deficiency of the immune response leads
to a variety of diseases involving every organ system in
the body.
The immune system consists of an intricately
Linked network of cells, proteins and lymphoid organs
which are strategically placed to ensure maximal
protection against infection.
Immune defenses are categorized into :
Innate & Adaptive immune response
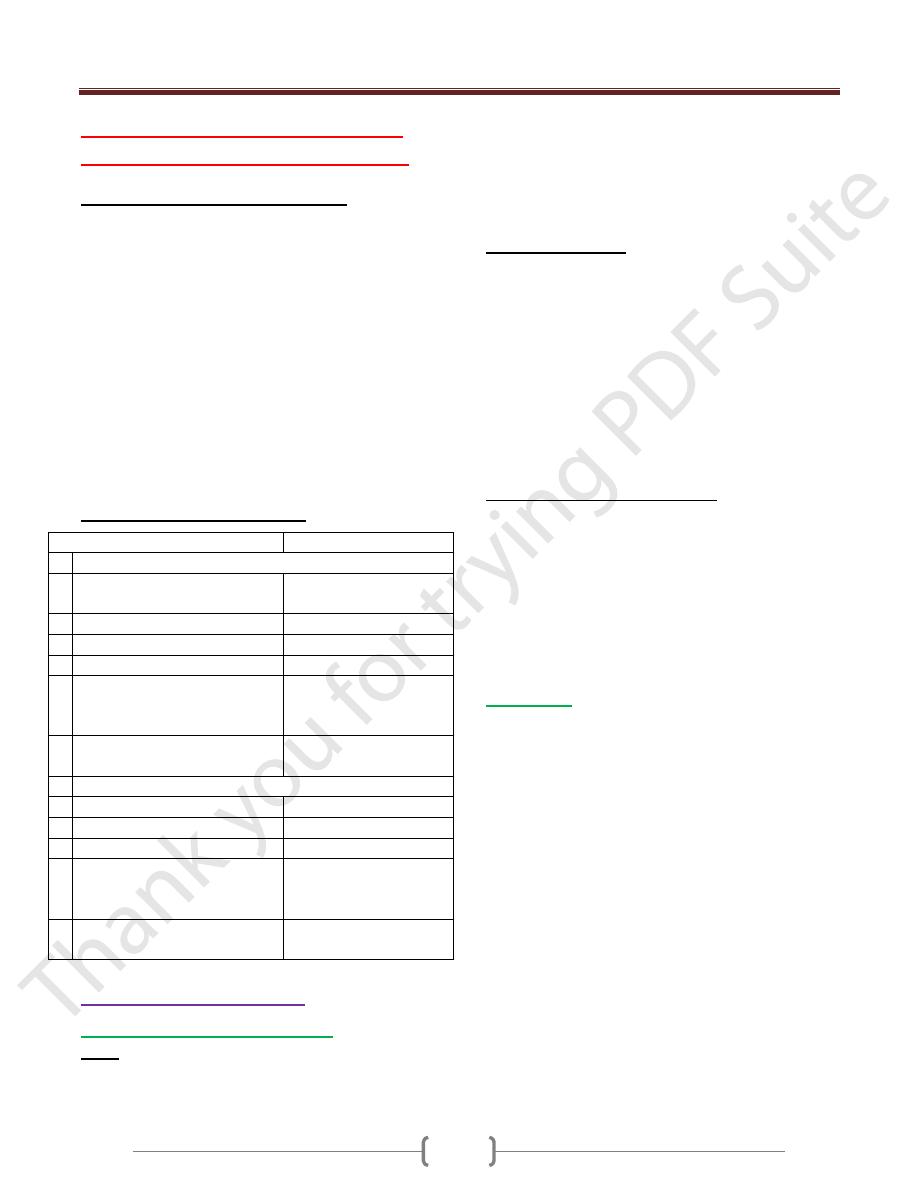
Properties of immune responses
Innate immune responses
Adaptive immune resp.
Characteristics
1 recognize generic microbial
structure
Ag specific responses
2 immediate mobilized (minutes)
slow responses (days)
3 No memory
memory
4 Genetically encoded
Not genetically encoded
5 Identical responses in all
individuals
Aquired as an adaptive
immune response to
exposure to antigens
6 Present in invertebrates and
vertebrates
Presents in vertebrates
only
Immune components
1 Constitutive barriers (skin)
T and B lymphocytes
2 Phagocytes(N, Macro)
secreted molecules (Abs)
3 NK cell
Ag specific receptors
4 Soluble mediators
(Complement, Cytokines, acute
phase protein)
5 Pattern recognition molecules
(Toll like receptors)
The innate immune system
Constitutive barriers to infection
1) Skin:
Tightly packed highly keratinized cells of the skin which
limit colonization by microorganisms (MO).
Microbial growth is inhibited by physiological factors
such as low PH and low O2 tension and sebaceous glands
secrete hydrophobic oils that repel MO. Sweat contains
lysozyme that destroy bacterial cell wall. Ammonia has
antimicrobial activity. Defensine is also antimicrobial
peptides
2)
Mucous membrane
of the respiratory and
gastrointestinal and genitourinary tract provides a
constitutive barrier to infection.
Cilia and Secreted mucous trap invading pathogen.
Secretory IgA prevents bacteria and virus attaching to and
penetrating epithelial cells
Lysozyme and defensine
Lactoferrin acts to starve invading bacteria of iron
Physical manoeuvres such as sneezing and coughing
GIT: HCL, salivary amylase destroy bacteria
Induced vomiting or diarrhoea promotes clearance of
invading MO.
3) Endogenous commensal bacteria
About 10
14
bacteria normally reside at epithelial surface
in symbiosis with the human host and compete with
pathogenic bacteria for nutrients & space
They produce fatty acids and bactericidins that inhibits
growth of MO.
Eradication of these normal flora with broad spectrum
antibiotics commonly results in opportunistic infection
like candida
Phagocytes
They are specialized cells which ingest and kill MO and
produce inflammatory molecules which regulate other
components of the immune system
It includes Neutrophils, Macrophages & monocytes.
They are crucial for defense against bacterial & fungal
infections
They express a wide range of surface receptors to identify MO
These pattern recognition receptors include:
1- Toll-Like receptors
2- Mannose receptors
They recognize bacterial cell wall components, bacterial
DNA and Viral Double stranded RNA directly
Phagocytes recognize pathogen by these receptors alone.
Engulfment of microorganisms is greatly enhanced by
opsonisation.
Opsonins include acute phase proteins such as C reactive
protein, Abs, complement. This opsonin binds to pathogen
and phagocytes receptors acting as a bridge between the
two and facilitating phagocytosis
Unit 3 - Immunological factors in disease
21
Neutrophils
They are short lived cells with half-life of 6 hours
Kill MO directly
Facilitates the rapid transit of cells through tissues and
amplify the immune system
Killing mediated by enzymes contained in the granules
Changes in the damaged cells triggers inflammatory
molecules and cytokines to stimulate the production and
maturation of N in BM.
The transit of N. through the blood stream is responsible for
the rise in leukocyte count that occurs in early infection.
N. phagocytose the MO and fuse with cytoplasmic
granules to form phagolysosome.
Killing of MO ocuurs through a combination of oxidative
and non –oxidative pathways
1) Oxidative killing is also known as respiratory burst, is
mediated by NADPH oxidase enzyme complex which
converts oxygen into reactive oxygen species :
- Hydrogen peroxide - Superoxide
Myeloperoxidase enzyme
- Hypochlorous ions (HOCL
-
)
2) Non- oxidative (oxygen-independent killing)
Occurs through release of bactericidal enzymes including
lysozyme and lactoferrin
The process of phagocytosis deplete N glycogen reserves
and followed by N death
After N death, their content is released and lysosomal
enzymes degrade collagen & liquefaction of adjacent
tissues. The accumulation of dead and dying N. results in
the formation of pus. When the amount of pus is
extensive, result in abscess formation.
Monocytes and Macrophages
Monocytes are the precursors of tissue macrophages
They produced in the BM and exported to circulation
constitutes about 5% of leukocytes
After 7-10 Hrs in the blood stream , they migrate to
peripheral tissues where they differentiate into tissue
macrophages. They do not die after killing pathogens.
In the liver----- Kupffer cell
In the lung-----alveolar macrophages
In the kidney----mesangial cells
In the brain-----microglial cells
Functions of Macrophages:
1) Initiation and amplification of the inflammatory response
by cytokines secretions (IL-1, IL-6, IL-8, TNF alpha)
2) Killing of MO by phagocytosis (oxidative and non-
oxidative pathways)
3) Resolution and repair of inflammation by:
a. Scavenging of necrotic and apoptotic cell
b. Tissue remodelling by elastase and collagenase enzymes
c. Scar formation by IL-1 , platelet derived growth factor,
fibroblast growth factor
4) Link between innate and adaptive by presentation of Ag
to T cells and T cells secreted cytokines act on
macrophages that enhance phagocytosis.
Natural killer cells (NK) cell
Is large granular lymphocytes
Acts against tumor cell and virally infected cell
It is not Ag specific cell and generate memory cell
It kills target cell by Ab dependent cell mediated
cytotoxicity (ADCC) and perforin –granzyme pathway
Produce the following cytokines (TNF-α, IFN-α , IFN- γ)
Mast cell and Basophils
1) they are derived from BM 7 play an important role in allergy
2) Mast cell reside in the tissues that are exposed to external
stimuli like skin and gut
3) Basophiles reside in the circulation and recruited to
tissues in response to inflammation.
Both had a cytoplasmic granules containing histamine and
other mediators
Other mediators synthesized after activation
(Leukotrienes, prostaglandins)
Local release of these mediators initiates inflammatory
cascades that lead to increase local blood flow, vascular
permeability, stimulate smooth muscle contraction and
increase secretion at mucosal surface.
Cytokines
Are soluble proteins that acts as multipurpose chemical
messengers. More than 100 cytokines have been described
with overlapping complex roles in modifying the immune
response
IL-1 secreted from macrophages and stimulates N
recruitment, T cell and macrophages activation; induce
fever and acute phase reactant.
IL-2 secreted from Th 1 , stimulate proliferation and
differentiation of Ag specific T cell
IL-4 secreted from Th2 , and mast cell , stimulates
maturation of T and B cell and enhance IgE production
IL-6 secreted from Th2 and macrophages,stimulate
maturation of B cell to plasma cell
Il-12 secreted from macrophages and activate NK cell and
stimulates IFN gamma and TNF alpha release by T cell
Unit 3 - Immunological factors in disease
22
IFN alpha secreted from Th1 and macrophages and NK
cell and had antiviral activity & activates TCD8 cell, NK ,
macrophages
IFN gamma secreted from Th1cell that increases
antitumor and antimicrbial activity of macrophages
TNF alpha secreted from macrophages and it is pro
inflammatory and had direct cytotoxic, increase apoptosis
Complement system:
It is a group of more than twenty tightly regulated
functionally linked proteins that act to promote
inflammation and elimenate pathogens
It is synthesis in the liver
It is circulate in inactive form
It is activated by three pathways:
1) Classical pathway: is initiated when IgG or IgM
binds Ag forming immune complex
2) Alternative pathway: is initiated by binding C3 to
LPS of G –ve bacterial cell wall, C3 to teichoic acid of
G + ve bacteria
3) Lectin pathway: is activated by the direct binding of
mannose-binding lectin to microbial cell surface
carbohydrates(mannose on the pathogen surface)
This mimics the binding of C1 to immune complex, thus
bypassing the need for immune complex formation
Activation of the complement by any one of these
pathways results in activation of C3 ending in a final
common pathway
C5-C9 (MAC) membrane attack complex ending with
pores formation on the cell surface
It is important in defense mechanisms against encapsulated
bacteria (Neisseria & Haemophilus influenzae)
Fragments of complement act as an opsonin. naphylotoxins
The adaptive immune system:
When the innate immune system failed to eradicate the
pathogen the adaptive immunity will be stimulated
It is characterized by specificity, highly adaptive & can
respond to unlimited number of molecules & had a memory
There are two major arms of adaptive immunity:
1) Humoral immunity mediated by Abs which is produced
by B cells. 2) Cellular immunity mediated by T cells that
secrete cytokines
Lymphoid organs
Primary lymphoid organs that involved in lymphocytes
development which include BM where both T and B
lymphocytes are derived from haemopoietic stem cell and
where lymph.mature. The second organ is thymus
Thymus:
Is bilobed structure that active during fetal and neonatal
period and involuted after puberty. In the thymus
immature T cell undergoes selection and maturation.
Absence of thymus is associated with profound T cell
immune deficiency.
Secondary lymphoid organs include spleen, LN, mucosa
associated lymphoid tissue and gut associated lymphoid
tissue where the pathogen interacts with lymphocytes.
Spleen
:
Is highly effective in filtration of blood and important site
of phagocytosis of aged RBC, bacteria, immune
complexes and other debris
It is important defense against encapsulated bacteria
(Streptococcus pneumonia and H influenzae infection)
Lymph node
It consists from:
1) Cortex (B cell) primary follicles
2) Para cortex (T cell and dendritic cell)
3) Medulla (plasma cell) & contains sinuses hat rich in
macrophages
MALT
Includes Peyer’s patches, Appendix, tonsils & Adenoids
Lymphatics
Functions
1) Provide access to LN
2) 2-return tissue fluid to venous system
3) Transport fat from small intestine to the blood stream
It begins as blind ended capillaries & then form lymphatic
ducts then enter LN (Afferent) and leave LN (Efferent)
and drain into thoracic duct then superior vena cava
Humoral Immunity
B cells:
They arise in the BM stem cells and found as mature B
cells in BM, LN, spleen and to lesser extent blood stream.
It encountered soluble Ag usually in LN by Ab that found
on its surface and presented to T cells. Stimulated B cells
by Ag respond by proliferation known as clonal expansion
and differentiate into either plasma cell and memory cells
Immunoglobulins:
Are soluble proteins consists from two heavy and two
light chains. The heavy chain determins the isotypes IgG,
IgM, IgA, IGE,IgD
Functions: * Opsonins, ADCC
Unit 3 - Immunological factors in disease
23
* Actvation classical pathway of complement
* Present in the secretions (Sec IgA) and deficiency of
this leads to recurrent resp and GIT infection
First exposure to Ag leads to IgM production (longer lag
phase) and for short period of time
Second exposure to AG leads to large titer of IgG
production with higher affinity (shorter lag phase)
Cellular immunity:
T cells are important against virus ,fungi, intracellular
bacteria
It arise in the bone marrow and exported as immature
cells to thymus undergo differentiation and selection
Ag in order to recognized by T cells , must be processed
into smaller fragment and combined to HLA (human
leukocyte antigens)
HLA molecules are highly polymorphic to ensure
diversity in recognition of Ags within the population.
T cells can be divided according to its function,
recognition of HLA molecules and expression of cell
surface proteins.
Leukocytes cell surface molecules are named
systematically by assigning them a cluster of
differentiation (CD) Ag numbe
T cytotoxic (CD8)
They recognize Ag peptide in association with MHC class I
Kill target cell by perforin granzyme
Secret IFN gamma
T helper (CD4)
They recognize Ag peptide in association with MHC class II
Produce cytokines and provide co -stimulatory signals
that support the activation of Tc
Assist production of mature Ab by B cells
Th cells can be divided into subsets according to
cytokines they produced :
* Th1 (IL-2, IFN- gamma, TNF-alpha), support
development of delayed type hypersensitivity
* Th2 (IL-4, IL-5, IL-10) promote allergic response
* Regulatory CD4+ lymphocytes, important in the
regulation of other CD4 cells and prevention of
autoimmune diseases
