
600
CHAPTER 11
this part.
vical arteries, the suprascapular arteries, or both arise from
has no branches. Occasionally, however, the superficial cer
The third part of the subclavian artery usually
Branches
the brachial plexus.
in the root of the neck, it is closely related to the nerves of
der of the 1st rib, where it becomes the axillary artery. Here,
across the posterior triangle of the neck to the lateral bor
lateral border of the scalenus anterior muscle (Fig. 11.57)
The third part of the subclavian artery extends from the
Third Part of the Subclavian Artery
deep muscles of the neck.
which supplies the
deep cervical artery,
spaces, and the
which supplies the 1st and the 2nd intercostal
tal artery,
superior intercos
dome of the pleura and divides into the
runs backward over the
costocervical trunk
The
Branches
scalenus anterior muscle (Fig. 11.57).
The second part of the subclavian artery lies behind the
Second Part of the Subclavian Artery
the superior epigastric and the musculophrenic arteries.
to the sternum; in the 6th intercostal space, it divides into
(Fig. 11.57). It descends vertically one fingerbreadth lateral
behind the 1st costal cartilage and in front of the pleura
descends into the thorax
internal thoracic artery
The
back of the scapula (Fig. 11.57).
chial plexus and follows the suprascapular nerve onto the
runs laterally over the bra
suprascapular artery
The
crosses the brachial plexus (Fig. 11.57).
is a small branch that
superficial cervical artery
The
inferior parathyroid glands.
recurrent laryngeal nerve. It supplies the thyroid and the
face of the thyroid gland, where it is closely related to the
ascends to the posterior sur
inferior thyroid artery
The
terminal branches (Fig. 11.57).
is a short trunk that gives off three
thyrocervical trunk
The
The Head and Neck
-
-
-
-
-
pressure is of great help, and the artery is compressed against
the subclavian artery. The use of a blunt object to exert the
strong pressure downward and backward on the third part of
remember that the hemorrhage can be stopped by exerting
In severe traumatic accidents to the upper limb involving lac
Palpation and Compression of the Subclavian
Artery in Patients with Upper Limb Hemorrhage
-
eration of the brachial or axillary arteries, it is important to
the upper surface of the 1st rib.
C L I N I C A L N O T E S
Veins of the Head and Neck
external jugular vein.
branch, which joins the posterior auricular vein to form the
anterior branch, which joins the facial vein, and a posterior
On leaving the parotid salivary gland, it divides into an
superficial temporal and the maxillary veins (Fig. 11.39).
The retromandibular vein is formed by the union of the
Retromandibular Vein
retromandibular vein.
illary vein joins the superficial temporal vein to form the
from the pterygoid venous plexus (Fig. 11.39). The max
The maxillary vein is formed in the infratemporal fossa
Maxillary Vein
retromandibular vein.
salivary gland, where it joins the maxillary vein to form the
and the auriculotemporal nerve and then enters the parotid
scalp (Fig. 11.39). It follows the superficial temporal artery
The superficial temporal vein is formed on the side of the
Superficial Temporal Vein
drains into the internal jugular vein.
by the anterior division of the retromandibular vein, and
side of the mouth. It then crosses the mandible, is joined
the face with the facial artery and passes around the lateral
with the cavernous sinus. The facial vein descends down
(Fig. 11.39). It is connected through the ophthalmic veins
supratrochlear veins
the union of the supraorbital and
The facial vein is formed at the medial angle of the eye by
Facial Vein
Veins of the Face and the Neck
spread of infection).
to the venous sinuses (and are an important route for the
skull bones (Fig. 11.9). They connect the veins of the scalp
The emissary veins are valveless veins that pass through the
Emissary Veins
vault of the skull (Fig. 11.9).
The diploic veins occupy channels within the bones of the
Diploic Veins
are described on page 544.
and inferior petrosal sinuses (Fig. 11.9). All these sinuses
the occipital sinus, the cavernous sinuses, and the superior
straight sinus, the transverse sinuses, the sigmoid sinuses,
include the superior and inferior sagittal sinuses, the
bones, the orbit, and the internal ear. The venous sinuses
no valves. They receive tributaries from the brain, the skull
page 544). They have thick, fibrous walls, but they possess
the meningeal layer of the dura mater (Fig. 11.37A; see also
The venous sinuses are situated between the periosteal and
Venous Sinuses
neighboring venous sinuses.
and the veins of the brainstem, all of which drain into the
They consist of the cerebral veins, the cerebellar veins,
The veins of the brain are thin walled and have no valves.
Veins of the Brain
The veins of the scalp, face, and neck
emissary veins
The veins of the brain, venous sinuses, diploic veins, and
The veins of the head and neck may be divided into
■
■
■
■
-
Basic Anatomy
part is covered by the sternothyroid, sternohyoid, and
omastoid, and the parotid salivary gland. Its lower
The skin, the fascia, the sternocleid
Anterolaterally:
Relations of the Internal Jugular Vein
Directly above the inferior bulb is a bicuspid valve.
rior bulb.
infe
and another near its termination called the
rior bulb
supe
The vein has a dilatation at its upper end called the
deep cervical lymph nodes.
course, it is closely related to the
brachiocephalic vein (Figs. 11.39 and 11.57). Throughout its
vian vein behind the medial end of the clavicle to form the
and common carotid arteries. It ends by joining the subcla
the carotid sheath lateral to the vagus nerve and the internal
the jugular foramen. It then descends through the neck in
tinuation of the sigmoid sinus and leaves the skull through
from the brain, face, and neck (Fig. 11.39). It starts as a con
The internal jugular vein is a large vein that receives blood
Internal Jugular Vein
sternocleidomastoid muscle.
rior jugular vein joins the external jugular vein deep to the
is joined to the opposite vein by the jugular arch. The ante
close to the midline (Fig. 11.39). Just above the sternum, it
The anterior jugular vein descends in the front of the neck
Anterior Jugular Vein
Anterior jugular vein
from the back of the scapula
Suprascapular vein
the posterior triangle
from the skin and the fascia over
Transverse cervical vein
from the back of the scalp
Posterior external jugular vein
Tributaries
vian vein behind the middle of the clavicle.
beneath the platysma muscle, and it drains into the subcla
It descends across the sternocleidomastoid muscle and
posterior division of the retromandibular vein (Fig. 11.39).
jaw by the union of the posterior auricular vein with the
The external jugular vein is formed behind the angle of the
External Jugular Vein
601
-
-
-
-
-
-
■
■
-
omohyoid muscles, which intervene between the vein
The upper surface of the 1st rib
Inferiorly:
phrenic nerve
The scalenus anterior muscle and the
Posteriorly:
The clavicle
Anteriorly:
Relations
phatic duct on the right.
receives the thoracic duct on the left side and the right lym
it receives the external jugular vein. In addition, it often
internal jugular vein to form the brachiocephalic vein, and
at the outer border of the 1st rib (Fig. 11.57). It joins the
The subclavian vein is a continuation of the axillary vein
Subclavian Vein
(Fig. 11.110)
Middle thyroid vein
(Fig. 11.55)
Superior thyroid vein
Lingual vein
Pharyngeal veins
(Fig. 11.39)
Facial vein
(Fig. 11.30)
Inferior petrosal sinus
Tributaries of the Internal Jugular Vein
common carotid artery and the vagus nerve.
9th, 10th, 11th, and 12th cranial nerves. Below lie the
Above lie the internal carotid artery and the
Medially:
thoracic duct.
(Fig. 11.57). On the left side, it passes in front of the
bral vein, and the first part of the subclavian artery
the phrenic nerve, the thyrocervical trunk, the verte
medius, the scalenus anterior, the cervical plexus,
vical vertebrae, the levator scapulae, the scalenus
The transverse processes of the cer
Posteriorly:
the vein.
The chain of deep cervical lymph nodes runs alongside
digastric, and the spinal part of the accessory nerve.
is crossed by the stylohyoid, the posterior belly of the
and the sternocleidomastoid (Fig. 11.55). Higher up, it
■
■
-
-
■
■
■
■
■
■
■
■
■
■
■
■
■
■
-
■
■
■
■
■
■
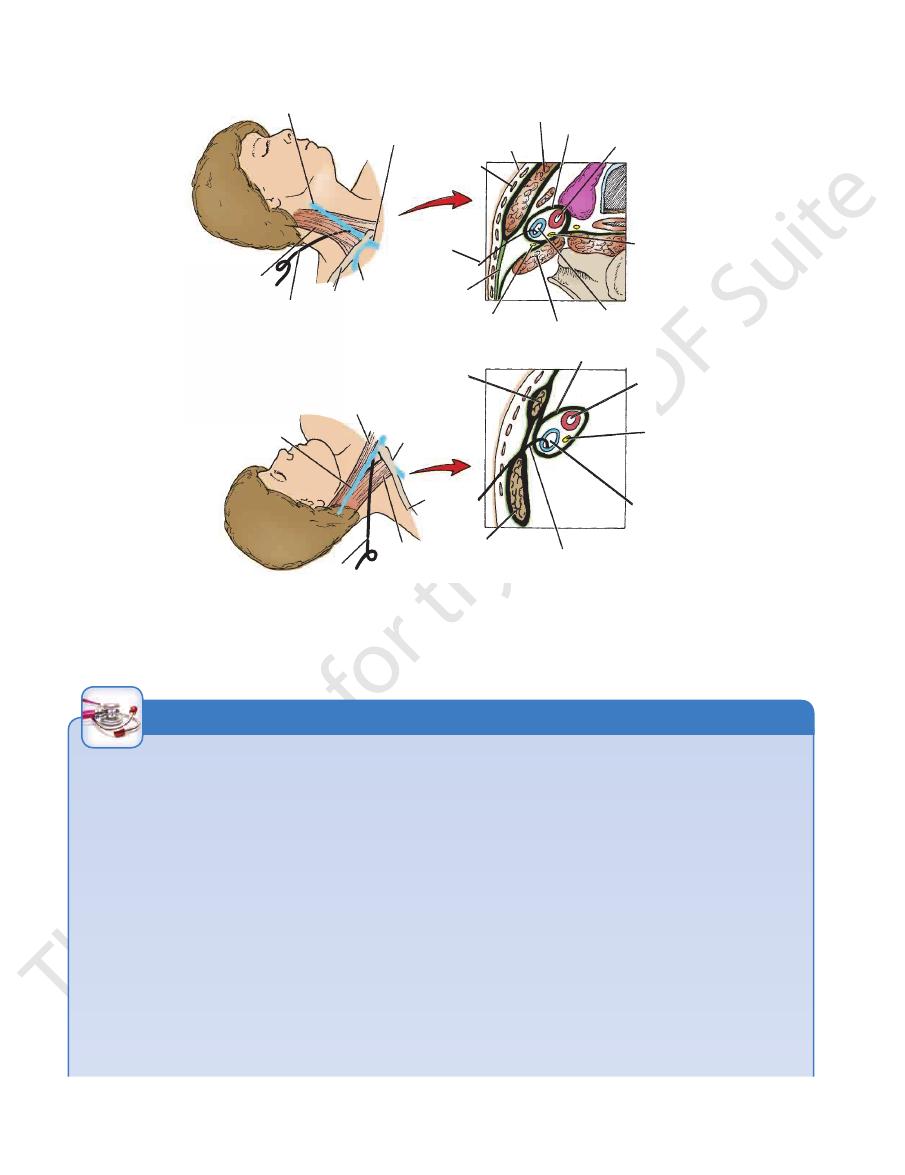
Penetrating Wounds of the Internal Jugular Vein
the tip of the mastoid process and the angle of the jaw to the
It descends through the neck from a point halfway between
The internal jugular vein is remarkably constant in position.
tains little smooth muscle, its injury is not followed by contrac
The hemorrhage of low-pressure venous blood into the loose
connective tissue beneath the investing layer of deep cervical
fascia may present as a large, slowly expanding hematoma. Air
embolism is a serious complication of a lacerated wall of the
internal jugular vein. Because the wall of this large vein con-
-
tion and retraction (as occurs with arterial injuries). Moreover,
the adventitia of the vein wall is attached to the deep fascia of
the carotid sheath, which hinders the collapse of the vein. Blind
clamping of the vein is prohibited because the vagus and hypo-
glossal nerves are in the vicinity.
Internal Jugular Vein Catheterization
sternoclavicular joint. Above, it is overlapped by the anterior
caudal direction (Fig. 11.61).
eter are inserted into the vein at the apex of the triangle in a
and the medial end of the clavicle are identified. A shallow skin
sternal and clavicular heads of the sternocleidomastoid muscle
head turned to the opposite side, the triangle formed by the
muscle (Fig. 11.61). In the anterior approach, with the patient’s
the clavicle at the posterior border of the sternocleidomastoid
are introduced into the vein about two fingerbreadths above
the posterior approach, the tip of the needle and the catheter
nal and clavicular heads of the sternocleidomastoid muscle. In
ered laterally by this muscle. Just above the sternoclavicular
border of the sternocleidomastoid muscle, and below, it is cov-
joint, the vein lies beneath a skin depression between the ster-
depression usually overlies the triangle. The needle and cath-
C L I N I C A L N O T E S
602
CHAPTER 11
The Head and Neck
internal jugular vein
right brachiocephalic
vein
subclavian
vein
clavicle
catheter
sternocleidomastoid muscle
catheter
deep
fascia
phrenic
nerve
scalenus anterior muscle
internal jugular vein
vagus nerve
common carotid artery
carotid sheath
sternocleidomastoid muscle
skin
platysma
muscle
internal jugular vein
catheter
clavicular origin of
sternocleidomastoid muscle
clavicle
subclavian
vein
sternal origin of
sternocleidomastoid muscle
catheter
internal jugular vein
vagus nerve
common carotid artery
carotid sheath
A
B
sternal origin of
sternocleidomastoid muscle
FIGURE 11.61
Catheterization of the right internal jugular vein.
and the clavicle.
into the vein close to the apex of the triangle formed by the sternal and clavicular heads of the sternocleidomastoid muscle
Anterior approach. Note that the catheter is inserted
to the sternocleidomastoid muscle and the common carotid artery.
Posterior approach. Note the position of the catheter relative
A.
B.
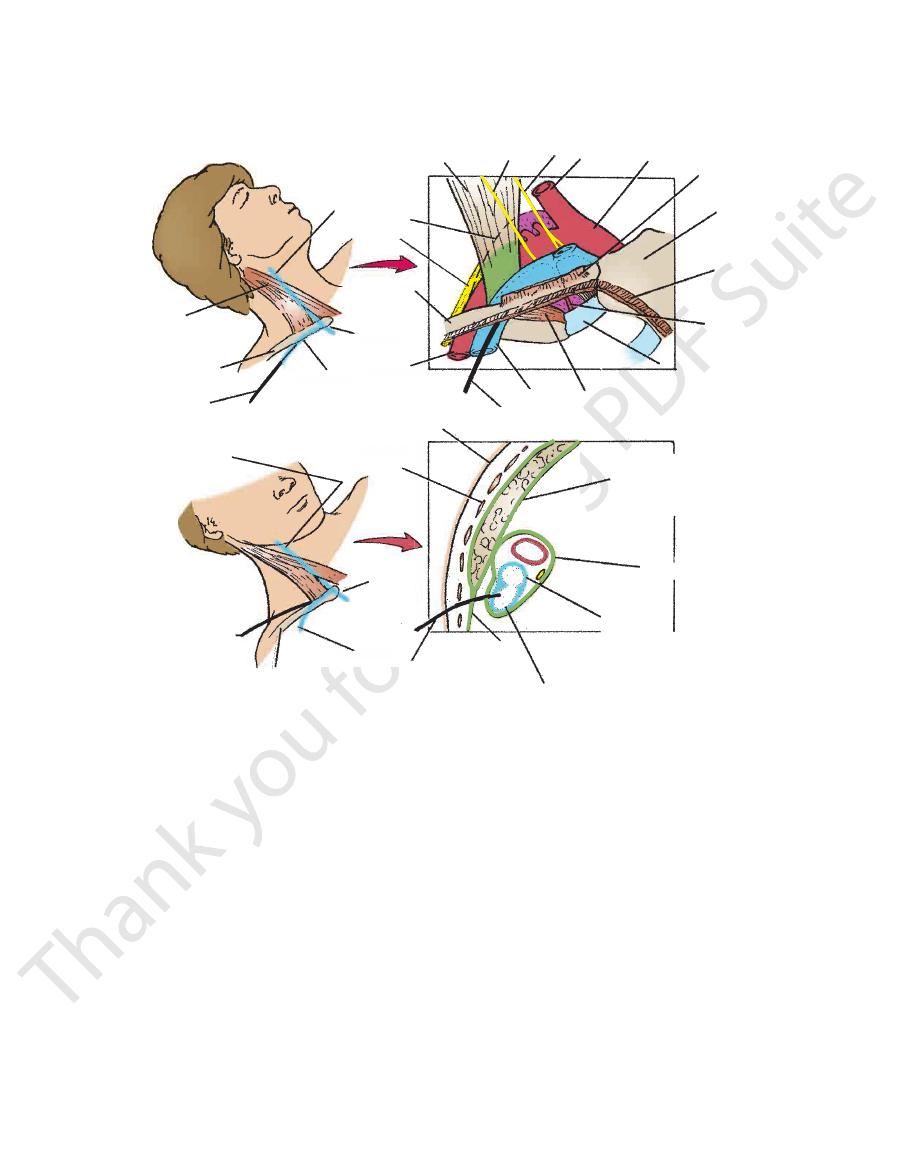
Subclavian Vein Thrombosis
lower border of the clavicle at the junction of the medial third
for catheterization. The vein is slightly more medially placed on
The subclavian vein is located in the lower anterior corner of the
the condition may follow a radical mastectomy with a block dis
Spontaneous thrombosis of the subclavian and/or axillary
veins occasionally occurs after excessive and unaccustomed
use of the arm at the shoulder joint. The close relationship of
these veins to the 1st rib and the clavicle and the possibility of
repeated minor trauma from these structures are probably fac-
tors in its development.
Secondary thrombosis of subclavian and/or axillary veins is a
common complication of an indwelling venous catheter. Rarely,
-
section of the lymph nodes of the axilla. Persistent pain, heavi-
ness, or edema of the upper limb, especially after exercise, is a
complication of this condition.
Anatomy of Subclavian Vein Catheterization
posterior triangle of the neck (Fig. 11.62), where it lies immedi-
ately posterior to the medial third of the clavicle.
Infraclavicular Approach
Since the subclavian vein lies close to the undersurface of the
medial third of the clavicle (Fig. 11.62), this is a relatively safe site
the left side than on the right side.
Anatomy of Procedure
The needle should be inserted through the skin just below the
and outer two thirds, coinciding with the posterior border of the
origin of the clavicular head of the sternocleidomastoid mus-
cle on the upper border of the clavicle (Fig. 11.62). The needle
pierces the following structures:
■
■
Skin
■
■
Superficial fascia
■
■
Pectoralis major muscle (clavicular head)
■
■
Clavipectoral fascia and subclavius muscle
■
■
Wall of subclavian vein
C L I N I C A L N O T E S
(continued)
Basic Anatomy
603
The needle is pointed upward and posteriorly toward the middle
posterior to the scalenus anterior muscle and perforated the
bright red blood flow indicate that the needle has passed
The needle may hit the 1st rib, if the needle
Hitting the 1st rib:
The needle may be “walked” along the
of the suprasternal notch.
Anatomy of Problems
■
■
Hitting the clavicle:
lower surface of the clavicle until its posterior edge is reached.
■
■
is pointed downward and not upward.
■
■
Hitting the subclavian artery: A pulsatile resistance and
subclavian artery.
Anatomy of Complications
Refer to Figure 11.62.
■
■
Pneumothorax: The needle may pierce the cervical dome of
the pleura, permitting air to enter the pleural cavity. This com-
plication is more common in children, in whom the pleural
reflection is higher than in adults.
■
■
Hemothorax: The catheter may pierce the posterior wall of
the subclavian vein and the pleura.
■
■
Subclavian artery puncture: The needle pierces the wall of
the artery during its insertion.
■
■
Internal thoracic artery injury: Hemorrhage may occur into
the superior mediastinum.
■
■
Diaphragmatic paralysis: This occurs when the needle
damages the phrenic nerve.
(except the tip); the floor of the mouth and vestibule;
lower incisors); the anterior two thirds of the tongue
ethmoid sinuses; the upper and lower teeth (except the
lip (except the central part); the frontal, maxillary, and
scalp; the nose; the cheek; the upper lip and the lower
of the jaw. They receive lymph from the front of the
mandibular salivary gland just below the lower margin
These lie superficial to the sub
Submandibular nodes:
mately passes into the submandibular nodes.
over the buccinator muscle. They drain lymph that ulti
One or two nodes lie in the cheek
Buccal (facial) nodes:
gland, the auricle, and the external auditory meatus.
scalp above the parotid gland, the eyelids, the parotid
parotid salivary gland. They receive lymph from the
These are situated on or within the
Parotid nodes:
auditory meatus.
the scalp above the ear, the auricle, and the external
ear over the mastoid process. They receive lymph from
These lie behind the
Retroauricular (mastoid) nodes:
the back of the scalp.
bone on the back of the skull. They receive lymph from
These are situated over the occipital
Occipital nodes:
The regional nodes are arranged as follows:
that is embedded in the carotid sheath in the neck (Fig. 11.55).
to the back of the head and as a deep vertical terminal group
arranged as a regional collar that extends from below the chin
The lymph nodes of the head and neck (Fig. 11.40) are
Lymph Drainage of the Head and Neck
the pleura and/or internal thoracic artery by the needle pass
toid is attached to the upper border of the clavicle. At this point,
The site of penetration of the vein wall is larger, since it lies
to enter the subclavian vein at the point where the clavicle and
cm from the clavicle. The catheter is tunneled beneath the skin
The needle pierces the skin in the deltopectoral groove about 2
The Procedure in Children
the first rib cross. The more oblique approach in children mini-
mizes the possibility of entering the subclavian artery.
Supraclavicular Approach
This approach (Fig. 11.62) is preferred by many for the following
anatomic reasons.
■
■
at the junction of the internal jugular vein and the subclavian
vein, which makes the procedure easier.
■
■
The needle is pointed downward and medially toward the
mediastinum, away from the pleura, avoiding the complica-
tion of pneumothorax.
■
■
The catheter is inserted along a more direct course into the
brachiocephalic vein and superior vena cava.
Anatomy of the Procedure
With the patient in the Trendelenburg position (patient supine
with head tilted downward) or simple supine position and the
head turned to the opposite side, the posterior border of the
clavicular origin of sternocleidomastoid muscle is palpated (Fig.
11.62). The needle is inserted through the skin at the site where
the posterior border of the clavicular origin of sternocleidomas-
the needle lies lateral to the lateral border of scalenus anterior
muscle and above the 1st rib. The needle pierces the following
structures (Fig. 11.62):
■
■
Skin
■
■
Superficial fascia and platysma
■
■
Investing layer of deep cervical fascia
■
■
Wall of the subclavian vein
The needle is directed downward in the direction of the opposite
nipple. The needle enters the junction of the internal jugular vein
and the subclavian vein. It is important that the operator under-
stands that the pleura is not being penetrated and that it is pos-
sible for the needle to lie in a zone between the chest wall and
the cervical dome of the parietal pleura but outside the pleural
space (cavity).
Anatomic Complications
The following complications may occur as the result of damage
to neighboring anatomic structures (Fig. 11.62):
■
■
Paralysis of the diaphragm: This is caused by injury to the
phrenic nerve as it descends posterior to the internal jugular
vein on the surface of the scalenus anterior muscle.
■
■
Pneumothorax or hemothorax: This is caused by damage to
-
ing posteriorly and downward.
■
■
Brachial plexus injury: This is caused by the needle passing
posteriorly into the roots or trunks of the plexus.
Regional Nodes
■
■
■
■
■
■
■
■
-
■
■
-
and the gums.
604
CHAPTER 11
The Head and Neck
sternocleidomastoid
muscle
internal
jugular
vein
carotid sheath
clavicular head of
sternocleidomastoid
muscle
platysma
muscle
skin
internal
jugular vein
clavicle
A
B
clavicle
clavicle
catheter
catheter
catheter
investing
layer
of deep
cervical
fascia
catheter
first costal
cartilage
internal thoracic
artery
pectoralis
major (cut)
right
common
carotid
artery
vagus
nerve
phrenic
nerve
scalenus
anterior
muscle
cervical
pleura
brachial
plexus
manubrium
sterni
sternocleidomastoid
muscle (cut)
subclavian
vein
subclavian
vein
subclavian
vein
subclavian
vein
subclavius
muscle
subclavian
artery
right
brachio-
cephalic
vein
right
brachio-
cephalic
vein
brachiocephalic
artery
stoid
internal
jugular
vein
cervical
pleura
brachial
plexus
platysma
muscle
s
clavicle
heter
catheter
cat
subclavian
vein
subclavian
i
subclavian
artery
right
brachio-
cephalicc
vein
clavicle
clavicle
b l i
right
brachio-
cephalic
vein
internal
jugular
vein
FIGURE 11.62
Subclavian vein catheterization.
Supraclavicular approach. The catheter enters the subclavian vein close to its junction with the
Infraclavicular approach. Note the many important anatomic structures
A.
located in this region. B.
internal jugular vein to form the brachiocephalic vein.
thoracic duct or the right lymphatic duct (Fig. 11.40).
nodes join to form the jugular trunk, which drains into the
The efferent lymph vessels from the deep cervical lymph
muscle, is mainly associated with drainage of the tongue.
which is situated close to the omohyoid
omohyoid node,
jugulo-
with drainage of the tonsil and the tongue. The
below and behind the angle of the jaw, is mainly concerned
which is located
jugulodigastric node,
regional nodes. The
(Fig. 11.49). They receive lymph from all the groups of
course of the internal jugular vein within the carotid sheath
The deep cervical nodes form a vertical chain along the
tures, including the thyroid gland.
trachea. They receive lymph from neighboring struc
These lie alongside the
Tracheal (paratracheal) nodes:
receive lymph from the larynx.
These lie in front of the larynx. They
Laryngeal nodes:
the vertebral column.
lymph from the nasal pharynx, the auditory tube, and
ynx and in front of the vertebral column. They receive
These lie behind the phar
Retropharyngeal nodes:
lobe of the ear.
skin over the lower part of the parotid gland, and the
drain lymph from the skin over the angle of the jaw, the
the external jugular vein on the side of the neck. They
These lie along the course of
Superficial cervical nodes:
front of the neck.
receive lymph from the skin and superficial tissues of the
the anterior jugular veins in the front of the neck. They
These lie along the course of
Anterior cervical nodes:
skin over the chin.
the incisor teeth, the center part of the lower lip, and the
the tongue, the floor of the anterior part of the mouth,
just below the chin. They drain lymph from the tip of
These lie in the submental triangle
Submental nodes:
■
■
■
■
■
■
■
■
-
■
■
■
■
-
Deep Cervical Nodes
