
Basic Anatomy
619
Summary of the Branches
of the Cervical Plexus
and Their Distribution
T A B L E 1 1 . 7
Branches
Distribution
Cutaneous
Lesser occipital
Skin of scalp behind ear
Greater auricular
Skin over parotid salivary gland,
auricle, and angle of jaw
Transverse
cutaneous
Skin over side and front of neck
Supraclavicular
Skin over upper part of chest and
shoulder
Muscular
Segmental
Prevertebral muscles, levator scapulae
Ansa cervicalis
(C1, 2, 3)
Omohyoid, sternohyoid, sternothyroid
C1 fibers via
hypoglossal nerve
Thyrohyoid, geniohyoid
Phrenic nerve
(C3, 4, 5)
Diaphragm (most important muscle of
respiration)
Sensory
Phrenic nerve
(C3, 4, 5)
are summarized in Table 9.4.
The branches of the brachial plexus and their distribution
Branches
axillary sheath.
artery and vein are enclosed in the
(see Fig. 9.20). Here, the brachial plexus and the axillary
Pericardium, mediastinal parietal
pleura, and pleura and peritoneum
covering central diaphragm
Injury to the Brachial Plexus
ing a local anesthetic. The anesthetic solution is massaged
The roots and trunks of the brachial plexus occupy the antero-
inferior angle of the posterior triangle of the neck. Incomplete
lesions can result from stab or bullet wounds, traction, or
pressure injuries. The clinical findings in Erb-Duchenne and
Klumpke’s lesions are fully described on page 429.
Brachial Plexus Nerve Block
It will be remembered that the axillary sheath, formed from the
prevertebral layer of deep cervical fascia, encloses the bra-
chial plexus and the axillary artery. A brachial plexus nerve
block can easily be obtained by closing the distal part of the
sheath in the axilla with finger pressure, inserting a syringe
needle into the proximal part of the sheath, and then inject-
along the sheath, producing a nerve block. The syringe needle
C L I N I C A L N O T E S
(continued)
may be inserted into the axillary sheath in the lower part of the
posterior triangle of the neck or in the axilla.
page 89)
neck and ends in the cardiac plexus in the thorax (see
which descends in the
superior cardiac branch,
The
form the pharyngeal plexus
branches of the glossopharyngeal and vagus nerves to
which unite with the pharyngeal
Pharyngeal branches,
12th cranial nerves
which join the 9th, 10th, and
Cranial nerve branches,
carotid artery.
ies and are distributed along the branches of the external
arteries. These branches form a plexus around the arter
to the common and external carotid
Arterial branches
rami of the cervical nerves
to the upper four anterior
Gray rami communicantes
plexus.
branches around the artery to form the internal carotid
the carotid canal in the temporal bone. It divides into
onic fibers, accompanies the internal carotid artery into
consisting of postgangli
internal carotid nerve,
The
Branches
skull (Fig. 11.60).
The superior cervical ganglion lies immediately below the
rior, middle, and inferior cervical ganglia.
The sympathetic trunk possesses three ganglia: the supe
the prevertebral layer of deep fascia (Fig. 11.49).
embedded in deep fascia between the carotid sheath and
common carotid arteries (i.e., medial to the vagus) and is
sympathetic trunk. It lies directly behind the internal and
where it becomes continuous with the thoracic part of the
to the base of the skull and below to the neck of the 1st rib,
The cervical part of the sympathetic trunk extends upward
Cervical Part of the Sympathetic Trunk
exercise. Rarely, pressure on the first thoracic nerve causes
At the root of the neck, the brachial plexus and the subclavian
Compression of the Brachial Plexus and the
Subclavian Artery
artery enter the posterior triangle through a narrow muscu-
lar–bony triangle. The boundaries of the narrow triangle are
formed in front by the scalenus anterior, behind by the sca-
lenus medius, and below by the 1st rib. In the presence of a
cervical rib (see page XXX), the 1st thoracic nerve and the
subclavian artery are raised and angulated as they pass over
the rib. Partial or complete occlusion of the artery causes
ischemic muscle pain in the arm, which is worsened by
symptoms of pain in the forearm and hand and wasting of the
small muscles of the hand.
The Autonomic Nervous System in
the Head and Neck
Sympathetic Part
-
Superior Cervical Ganglion
■
■
-
■
■
■
■
-
■
■
■
■
■
■
620
CHAPTER 11
the vertebral artery (Fig. 11.57).
the 7th cervical vertebra and the neck of the 1st rib, behind
It lies in the interval between the transverse process of
stellate ganglion.
the first thoracic ganglion to form the
The inferior cervical ganglion in most people is fused with
and ends in the cardiac plexus in the thorax (see page 89)
which descends in the neck
The middle cardiac branch,
artery to the thyroid gland
which pass along the inferior thyroid
Thyroid branches,
5th and 6th cervical nerves
to the anterior rami of the
Gray rami communicantes
Branches
cartilage (Fig. 11.57).
The middle cervical ganglion lies at the level of the cricoid
The Head and Neck
Middle Cervical Ganglion
■
■
■
■
■
■
Inferior Cervical Ganglion
dorsal scapular nerve
nerve to subclavius
suprascapular nerve
lateral pectoral nerve
thoracodorsal nerve
musculocutaneous nerve
axillary nerve
radial nerve
median nerve
ulnar nerve
medial cutaneous nerve of the forearm
medial cutaneous nerve of the arm
medial pectoral nerve
upper and lower
subscapular nerves
long thoracic nerve
T1
8
7
6
C5
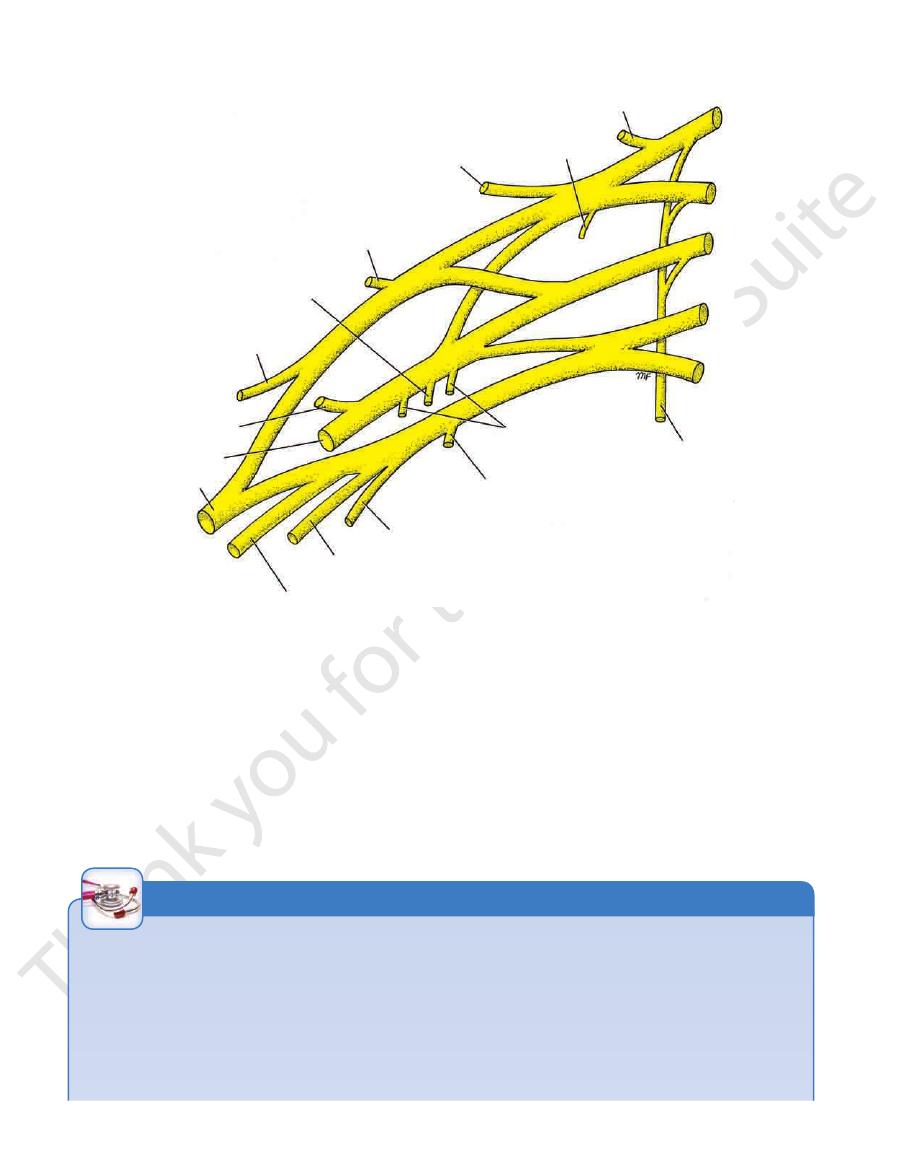
FIGURE 11.71
Brachial plexus and its branches.
Sympathectomy for Arterial Insufficiency of the Upper
produces not only vasodilatation of the skin vessels, but also
Removal of the stellate ganglion also removes the sym
removed to block the sympathetic pathway to the arm completely.
it is clear that the stellate and the 2nd thoracic ganglia should be
for the treatment of arterial insufficiency. From this information,
Sympathectomy of the upper limb is a relatively common procedure
fibers then join the roots of the brachial plexus as gray rami.
thoracic, stellate, and middle cervical ganglia. Postganglionic
rami, they ascend within the trunk and are relayed in the second
thoracic nerves. On reaching the sympathetic trunk via the white
preganglionic fibers leave the spinal cord in the 2nd to the 8th
The sympathetic innervation of the upper limb is as follows: The
Limb
-
pathetic nerve supply to the head and neck on that side. This
anhidrosis, nasal congestion, and Horner’s syndrome. For this
reason, the stellate ganglion is usually left intact in sympathecto-
mies of the upper limb.
C L I N I C A L N O T E S
(continued)
Basic Anatomy
621
Horner’s Syndrome
cle and the muscles that radiate from the lips into the face
stance of the lips is made up by the orbicularis oris mus
are lined on the inside by mucous membrane. The sub
(Fig. 11.72). They are covered on the outside by skin and
The lips are two fleshy folds that surround the oral orifice
and they are short in length.
testinal tract. The postganglionic fibers are nonmyelinated,
The last two plexuses are found in the gastroin
mucosal plexus (Meissner’s
(Auerbach’s plexus),
myenteric plexus
pulmonary plexus,
ganglion cells are placed in nerve plexuses, such as the
In certain locations, the
otic.
submandibular,
pterygopalatine,
ciliary,
asympathetic ganglia are the
located close to the viscera they innervate. The cranial par
These preganglionic fibers synapse in peripheral ganglia
within the cranial nerves.
myelinated preganglionic fibers that emerge from the brain
The axons of these connector nerve cells are
of the vagus.
dorsal nucleus
and that of the vagus nerve the
nucleus;
inferior salivary
that of the glossopharyngeal nerve the
superior salivary nuclei;
lacrimatory
nerve the
those of the facial
Edinger-Westphal nucleus;
is called the
The parasympathetic nucleus of the oculomotor nerve
vagus (10th) cranial nerves.
glossopharyngeal (9th),
oculomotor (3rd), facial (7th),
located in the nuclei of the
parasympathetic part of the autonomic nervous system is
The cranial portion of the craniosacral outflow of the
Parasympathetic Part
(Figs. 11.57 and 11.60).
ansa subclavia
is referred to as the
artery and then turns upward behind it. This anterior bundle
bundle crosses in front of the first part of the subclavian
resented by two or more nerve bundles. The most anterior
cervical ganglion to the inferior or stellate ganglion is rep
The part of the sympathetic trunk connecting the middle
cardiac plexus in the thorax (see page 89)
which descends to join the
inferior cardiac branch,
The
to the subclavian and vertebral arteries
Arterial branches
7th and 8th cervical nerves
to the anterior rami of the
Gray rami communicantes
Branches
The local anesthetic is then injected beneath the prevertebral
A stellate ganglion block is performed by first palpating the large
ment of the ganglion in cancerous growth, which may interrupt
include lesions of the brainstem or cervical part of the spinal cord;
of the sympathetic nerve supply to the orbit. Pathologic causes
the eyeball into the orbital cavity). It is caused by an interruption
(drooping of the upper eyelid), and enophthalmos (depression of
Horner’s syndrome includes constriction of the pupil, ptosis
traumatic injury to the cervical part of the sympathetic trunk; trac-
tion of the stellate ganglion caused by a cervical rib; and involve-
the peripheral part of the sympathetic pathway to the orbit.
Stellate Ganglion Block
anterior tubercle (carotid tubercle) of the transverse process of
the 6th cervical vertebra, which lies about a fingerbreadth lat-
eral to the cricoid cartilage. The carotid sheath and the sterno-
cleidomastoid muscle are pushed laterally and the needle of the
anesthetic syringe is inserted through the skin over the tubercle.
layer of deep cervical fascia. This procedure effectively blocks
the ganglion and its rami communicantes.
■
■
■
■
■
■
-
and
and the
-
the
the
and the
car-
diac plexus, the
the
and the
plexus).
-
The Digestive System in the Head
and Neck
The Mouth
The Lips
-
-
hard palate
soft palate
uvula
palatopharyngeal
fold
palatine tonsil
palatoglossal fold
sulcus terminalis
vallate papillae
foramen cecum
posterior wall
of oral part of
pharynx
mucous
membrane
lining vestibule
buccinator
muscle
opening of
parotid duct
upper second
molar tooth
lingual
vein
lingual
nerve
lingual
artery
opening of
submandibular duct
openings of ducts
of sublingual gland
sublingual fold
frenulum of
tongue
plica fimbriata
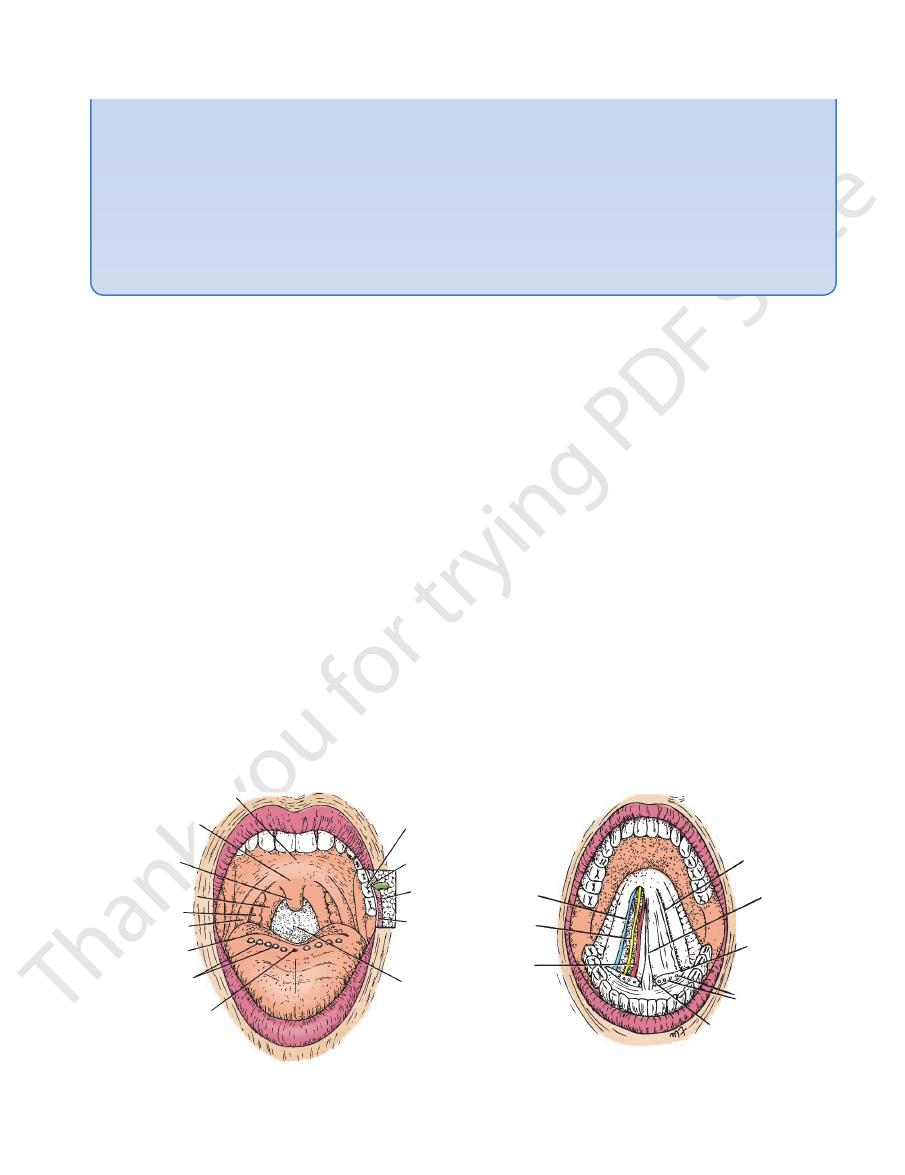
A
B
FIGURE 11.72
A.
Undersurface of the tongue.
Cavity of the mouth. Cheek on the left side of the face has been cut away to show the buccinator muscle
and the parotid duct. B.
622
CHAPTER 11
opens onto the floor of the mouth on the summit of a small
The submandibular duct of the submandibular gland
(Fig. 11.72).
plica fimbriata
the frenulum, the mucous membrane forms a fringed fold,
midline to the floor of the mouth (Fig. 11.72). Lateral to
connects the undersurface of the tongue in the
tongue
frenulum of the
A fold of mucous membrane called the
from the sides of the tongue to the gum of the mandible.
the tongue and by the reflection of the mucous membrane
The floor is formed largely by the anterior two thirds of
and the soft palate behind (Fig. 11.72).
The roof of the mouth is formed by the hard palate in front
Roof of Mouth
The mouth proper has a roof and a floor.
Mouth Proper
opposite the upper second molar tooth (Fig. 11.72).
opens on a small papilla into the vestibule
salivary gland
duct of the parotid
bule in contact with one another. The
that of the muscles of the lips keeps the walls of the vesti
mucous membrane. The tone of the buccinator muscle and
which is made up by the buccinator muscle and is lined with
The lateral wall of the vestibule is formed by the cheek,
the mucous membrane from the lips and cheeks to the gums.
The vestibule is limited above and below by the reflection of
mouth proper behind the third molar tooth on each side.
the lips. When the jaws are closed, it communicates with the
municates with the exterior through the oral fissure between
and the gums and the teeth internally. This slitlike space com
The vestibule lies between the lips and the cheeks externally
Vestibule
cavity proper.
The mouth is divided into the vestibule and the mouth
formed on each side by the palatoglossal fold (Fig. 11.72).
oropharyngeal isthmus,
entrance into the pharynx, the
The mouth extends from the lips to the pharynx. The
The Mouth Cavity
inner surface of the lips to the gums.
—connect the
labial frenulae
of mucous membrane—the
midline on the outer surface of the upper lip. Median folds
is the shallow vertical groove seen in the
philtrum
The
nerves, connective tissue, and many small salivary glands.
(Fig. 11.73). Also included are the labial blood vessels and
The Head and Neck
is
-
-
Floor of Mouth
the
papilla on either side of the frenulum of the tongue (Fig. 11.72).
sublingual fold.
ing a low fold of mucous membrane, the
The sublingual gland projects up into the mouth, produc-
Numerous ducts of the gland open on the summit of the fold.
The greater palatine and nasopalatine nerves
Roof:
Sensory Innervation of the Mouth
attached to the alveolar periosteum.
The mucous membrane of the gingiva, or gum, is strongly
being bitten between the teeth when the jaws are closed.
that prevent redundant folds of mucous membrane from
the buccinator muscle by elastic fibers in the submucosa
In the vestibule, the mucous membrane is tethered to
Mucous Membrane of the Mouth
(Fig.
lary division of the trigeminal
11.74) from the maxil
nerve
levator labii
superioris
levator labii
superioris
alaeque nasi
infraorbital
nerve (V2)
buccal
nerve (V3)
mental
nerve (V3)
levator anguli oris
zygomaticus minor
zygomaticus major
risorius
orbicularis oris
platysma
depressor anguli oris
depressor labii inferioris
mentalis
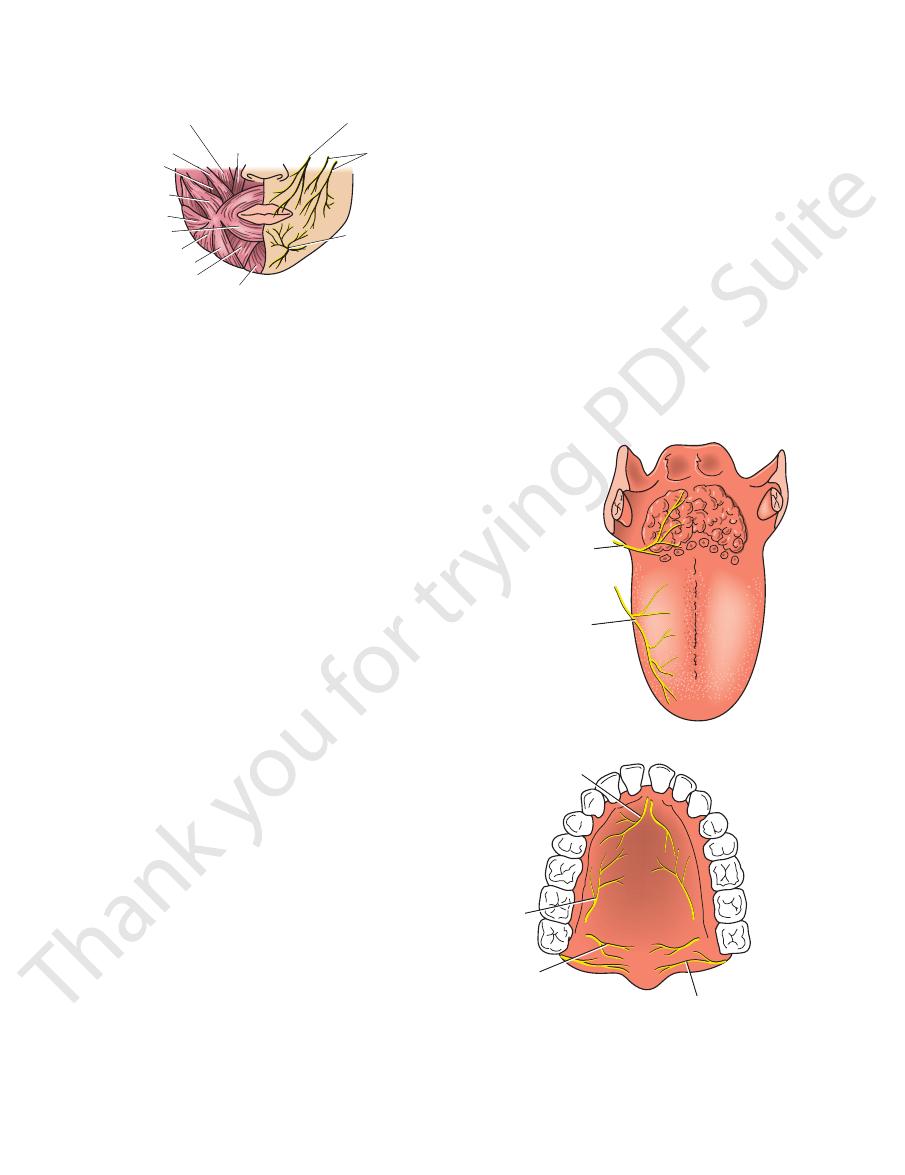
FIGURE 11.73
Arrangement of the facial muscles around the
lips; the sensory nerve supply of the lips is shown.
glossopharyngeal
nerve (all sensations)
glossopharyngeal nerve (IX)
nasopalatine
nerve (V2)
greater
palatine
nerve (V2)
lesser
palatine
nerve (V2)
lingual nerve (V3)
(common sensation)
chorda tympani (VII)
(taste)
A
B
FIGURE 11.74
A.
greater petrosal branch of the facial nerve.
run with branches of the maxillary nerve (V2) and join the
mucous membrane of the hard and soft palate; taste fibers
Sensory nerve supply to the
Sensory nerve supply to the mucous
membrane of the tongue. B.
Basic Anatomy
innervated by the buccal branch of the facial nerve)
sion of the trigeminal nerve (the buccinator muscle is
The buccal nerve, a branch of the mandibular divi
Cheek:
of the facial nerve.
taste fibers travel in the chorda tympani nerve, a branch
of the mandibular division of the trigeminal nerve. The
The lingual nerve (common sensation), a branch
Floor:
623
-
bered. The close relation of the submandibular duct to the floor
medical professional is called on to examine. Needless to say,
Clinical Significance of the Examination of the
Mouth
The mouth is one of the important areas of the body that the
the physician must be able to recognize all the structures vis-
ible in the mouth and be familiar with the normal variations
in the color of the mucous membrane covering underlying
structures. The sensory nerve supply and lymph drainage of
the mouth cavity should be known. The close relation of the
lingual nerve to the lower third molar tooth should be remem-
of the mouth may enable one to palpate a calculus in cases of
periodic swelling of the submandibular salivary gland.
C L I N I C A L N O T E S
Development of the Mouth
topharyngeal folds, and most of the soft palate are entodermal
the teeth are ectodermal structures. The secretory epithelium
pears during the third week of development (Fig. 11.75). If this
The cavity of the mouth is formed from two sources: a depres-
sion from the exterior, called the stomodeum, which is lined
with ectoderm, and a part immediately posterior to this,
derived from the cephalic end of the foregut and lined with
entoderm. These two parts at first are separated by the buc-
copharyngeal membrane, but this breaks down and disap-
membrane were to persist into adult life, it would occupy an
imaginary plane extending obliquely from the region of the
body of the sphenoid, through the soft palate, and down to the
inner surface of the mandible inferior to the incisor teeth. This
means that the structures that are situated in the mouth ante-
rior to this plane are derived from ectoderm. Thus, the epithe-
lium of the hard palate, sides of the mouth, lips, and enamel of
and cells lining the ducts of the parotid salivary gland also are
derived from ectoderm. On the other hand, the epithelium of
the tongue, the floor of the mouth, the palatoglossal and pala-
in origin. The secretory and duct epithelia of the sublingual
and submandibular salivary glands also are believed to be of
entodermal origin.
E M B R Y O L O G I C N O T E S
mandibular
process
olfactory pit
maxillary
process
buccopharyngeal
membrane
brain
buccopharyngeal
membrane
stomodeum
region of
developing neck
pericardial cavity
notochord
second pharyngeal
arch
pharynx
four pharyngeal pouches
A
B
FIGURE 11.75
A.
fibrous septum.
right and left halves by a median
dible and the hyoid bone below. The tongue is divided into
the styloid process and the soft palate above and to the man
membrane (Fig. 11.77). The muscles attach the tongue to
The tongue is a mass of striated muscle covered with mucous
The Tongue
upper jaw.
30. The teeth of the lower jaw appear before those of the
third molar, which may happen between the ages of 17 and
to erupt at 6 years of age. The last tooth to erupt is the
molars, and 6 molars in each jaw (Fig. 11.76). They begin
There are 32 permanent teeth: 4 incisors, 2 canines, 4 pre
Permanent Teeth
those of the upper jaw.
2 years. The teeth of the lower jaw usually appear before
6 months after birth and have all erupted by the end of
and four molars in each jaw. They begin to erupt about
There are 20 deciduous teeth: four incisors, two canines,
Deciduous Teeth
The Teeth
developing embryo showing the buccopharyngeal membrane breaking down.
The face of the
Sagittal section of the embryo showing the position of the buccopharyngeal membrane. B.
-
-
624
CHAPTER 11
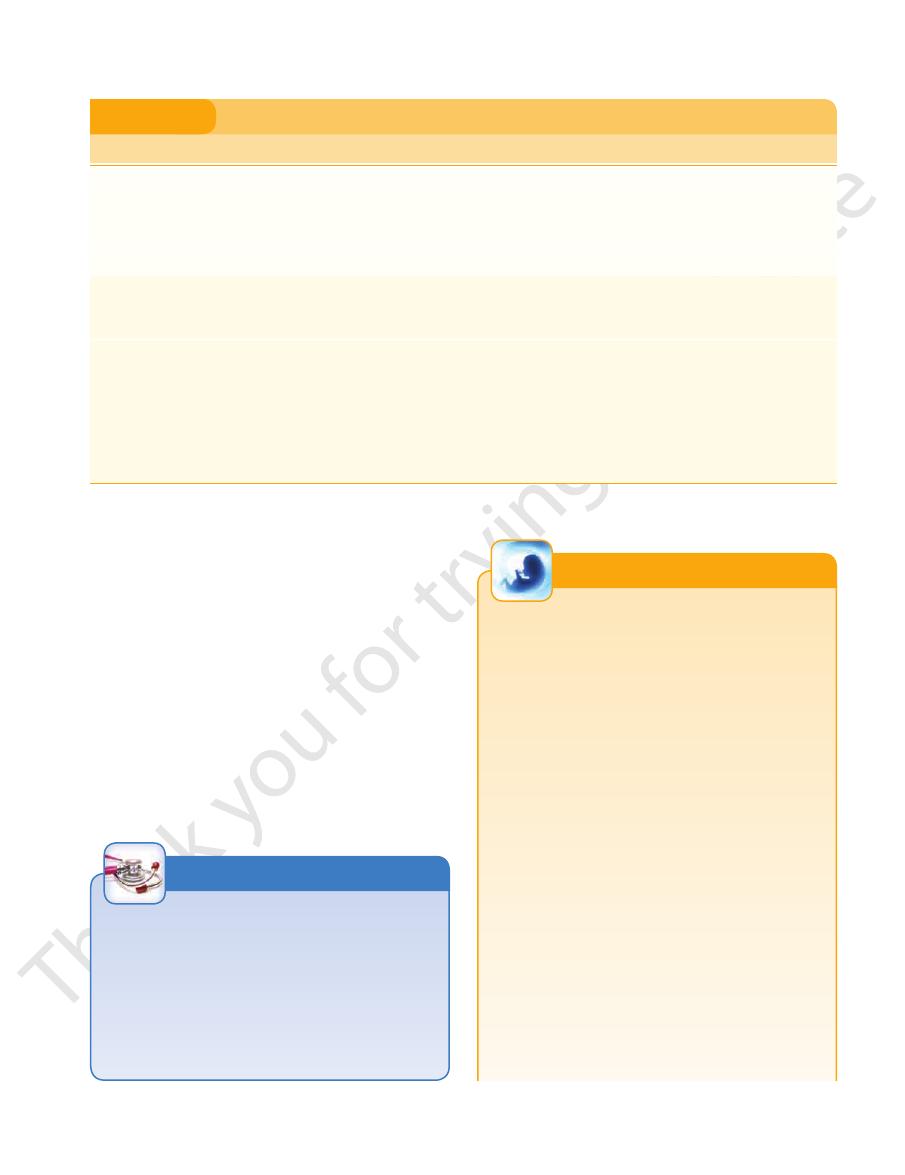
sulcus terminalis
by a V-shaped sulcus, the
tongue can be divided into anterior and posterior parts
The mucous membrane of the upper surface of the
Mucous Membrane of the Tongue
The Head and Neck
(Fig. 11.77).
Three types of papillae are present on the upper
(see page 659).
marks the site of the upper end of the thyroglossal duct
The foramen cecum is an embryologic remnant and
oral part, and the posterior third, or pharyngeal part.
to divide the tongue into the anterior two thirds, or
by a small pit, the foramen cecum. The sulcus serves
The apex of the sulcus projects backward and is marked
surface of the anterior two thirds of the tongue: the
and the
fungiform papillae,
filiform papillae, the
vallate papillae.
The mucous membrane on the inferior surface of
lingual tonsil.
nodules, the
(Fig. 11.77), caused by the presence of underlying lymph
the tongue is devoid of papillae but has an irregular surface
The mucous membrane covering the posterior third of
the tongue is reflected from the tongue to the floor of the
Deep cervical lymph nodes
Posterior third:
cervical lymph nodes
Submandibular and deep
Sides of the anterior two thirds:
Submental lymph nodes
Tip:
Lymph Drainage
The veins drain into the internal jugular vein.
and the ascending pharyngeal artery supply the tongue.
The lingual artery, the tonsillar branch of the facial artery,
muscles are summarized in Table 11.8.
The origin, insertion, nerve supply, and action of the tongue
Hypoglossal nerve
Nerve supply:
and the palatoglossus.
They are the genioglossus, the hyoglossus, the styloglossus,
These muscles are attached to bones and the soft palate.
Alter the shape of the tongue
Action:
Hypoglossal nerve
Nerve supply:
and vertical fibers.
attached to bone. They consist of longitudinal, transverse,
These muscles are confined to the tongue and are not
intrinsic and extrinsic.
The muscles of the tongue are divided into two types:
Muscles of the Tongue
(Fig. 11.72).
plica fimbriata
vein, the mucous membrane forms a fringed fold called the
seen through the mucous membrane. Lateral to the lingual
lateral side of the frenulum, the deep lingual vein can be
frenulum of the tongue.
mucous membrane, the
tongue is connected to the floor of the mouth by a fold of
mouth. In the midline anteriorly, the undersurface of the
On the
Intrinsic Muscles
Extrinsic Muscles
Blood Supply
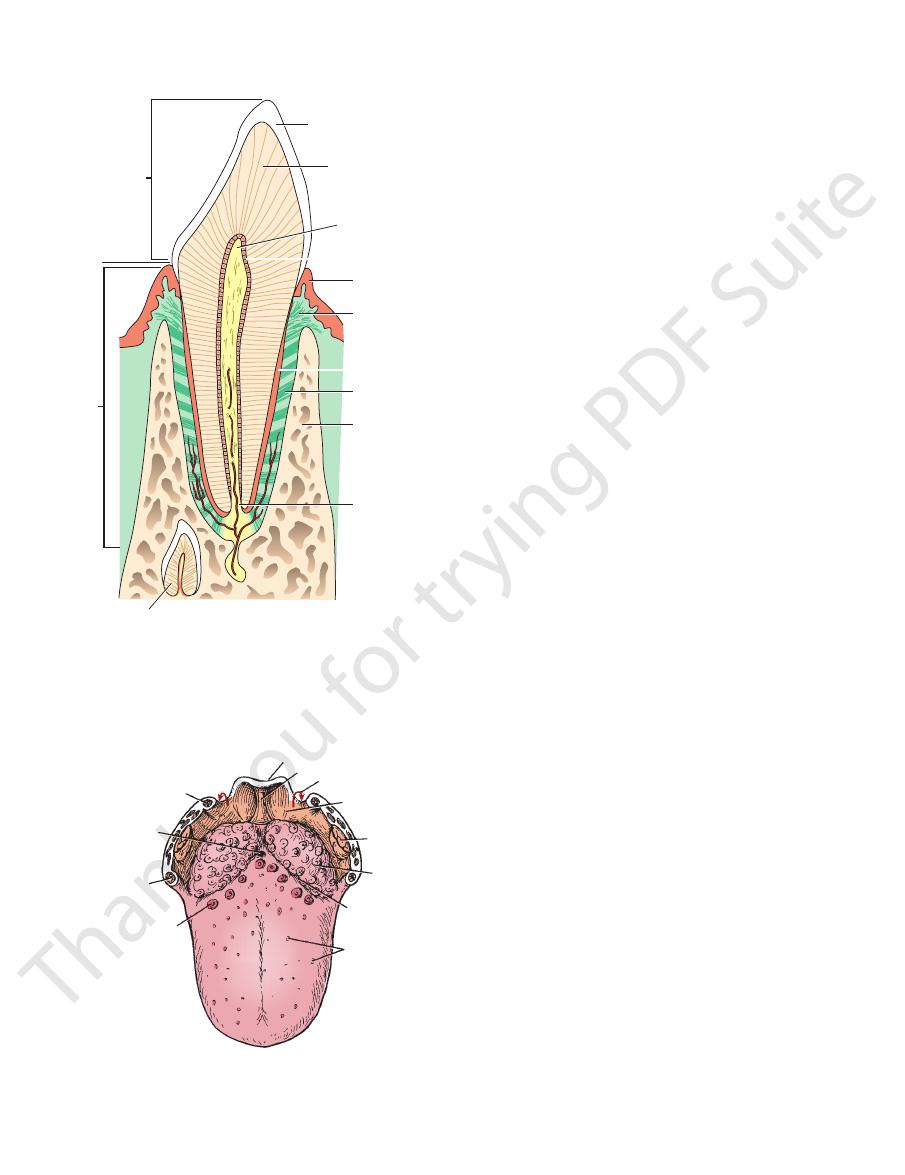
crown
enamel
dentine
pulp in
pulp cavity
gingiva
odontoblasts
periodontal
ligament
periodontal
ligament
alveolar
bone
root canal
cementum
neck
root
permanent tooth
FIGURE 11.76
Sagittal section through the lower jaw and
developing permanent tooth.
gum showing an erupted temporary incisor tooth and a
palatopharyngeal
fold
epiglottis median glossoepiglottic
fold arrow leading into
piriform fossa
vallecula
tonsil
lymphoid
tissue
sulcus
terminalis
fungiform
papillae
vallate papillae
palatoglossal
fold
foramen cecum
FIGURE 11.77
Dorsal surface of the tongue showing the
arrows
fossa on each side (
valleculae, the epiglottis, and the entrance into the piriform
).
Basic Anatomy
625
Muscles of Tongue
T A B L E 1 1 . 8
Intrinsic muscles
Shape changes:
and palatoglossus muscles on both sides acting together
Styloglossus
Retraction and elevation of the posterior third:
together
Hyoglossus muscles on both sides acting
Depression:
sides acting together
Styloglossus and hyoglossus muscles on both
Retraction:
together (Fig. 11.78)
The genioglossus muscles on both sides acting
Protrusion:
Movements of the Tongue
tion and taste)
Glossopharyngeal nerve (general sensa
Posterior third:
chorda tympani branch of the facial nerve (taste)
lar division of trigeminal nerve (general sensation) and
Lingual nerve branch of mandibu
Anterior two thirds:
Sensory Innervation
Vertical
Transverse
Muscle
Origin
Insertion
Nerve Supply
Action
Intrinsic Muscles
Longitudinal
Median septum and
submucosa
Mucous membrane
Hypoglossal nerve
Alters shape of tongue
Extrinsic Muscles
Genioglossus
Superior genial spine of
mandible
Blends with other muscles
of tongue
Hypoglossal nerve
Protrudes apex of tongue
through mouth
Hyoglossus
Body and greater cornu
of hyoid bone
Blends with other muscles
of tongue
Hypoglossal nerve
Depresses tongue
Styloglossus
Styloid process of tem-
poral bone
Blends with other muscles
of tongue
Hypoglossal nerve
Draws tongue upward and
backward
Palatoglossus
Palatine aponeurosis
Side of tongue
Pharyngeal plexus
Pulls roots of tongue upward
and backward, narrows
oropharyngeal isthmus
-
-
Development of the Tongue
At about the fourth week, a median swelling called the
end of each first pharyngeal arch), appears on each side of the
floor of the pharynx (Fig. 11.79). A little later, another swelling,
appears in the entodermal ventral wall or
tuberculum impar
called the lateral lingual swelling (derived from the anterior
tuberculum impar. The lateral lingual swellings now enlarge,
grow medially, and fuse with each other and the tuberculum
impar. The lingual swellings thus form the anterior two thirds
of the body of the tongue, and since they are derived from the
first pharyngeal arches, the mucous membrane on each side
will be innervated by the lingual nerve, a branch of the man-
dibular division of the 5th cranial nerve (common sensation).
The chorda tympani from the seventh cranial nerve (taste)
also supplies this area.
Meanwhile, a second median swelling, called the
innervated by the 9th cranial nerve (common sensation and
the tongue is formed from the third pharyngeal arches and is
pears. Thus, the mucous membrane of the posterior third of
arch on each side overgrow the other arches and extend
arches are entering this region. The anterior ends of the third
anterior ends of the second, third, and fourth pharyngeal
culum impar and becomes V shaped. At about this time, the
appears in the floor of the pharynx behind the tuberculum
copula,
impar. The copula extends forward on each side of the tuber-
into the copula, fusing in the midline. The copula now disap-
taste).
E M B R Y O L O G I C N O T E S
(continued)
Laceration of the Tongue
truded from the mouth. It can also occur when a patient acci
A wound of the tongue is often caused by the patient’s teeth
following a blow on the chin when the tongue is partly pro-
-
dentally bites the tongue while eating, during recovery from
an anesthetic, or during an epileptic attack. Bleeding is halted
by grasping the tongue between the finger and thumb pos-
terior to the laceration, thus occluding the branches of the
lingual artery.
C L I N I C A L N O T E S
626
CHAPTER 11
The Head and Neck
The anterior two thirds of the tongue is separated from the
soft palate.
foramen. The glossopharyngeal nerve also supplies the
enters the front of the hard palate through the incisive
nasopalatine nerve, also a branch of the maxillary nerve,
the greater and lesser palatine foramina (Fig. 11.74). The
division of the trigeminal nerve enter the palate through
The greater and lesser palatine nerves from the maxillary
Nerve Supply of the Palate
nerve supply, and actions are summarized in Table 11.9.
The muscles of the soft palate, their origins, insertions,
a tense sheet.
that the soft palate may be moved upward or downward as
cles of the two sides contract, the soft palate is tightened so
expands to form the palatine aponeurosis. When the mus
The tendon, together with the tendon of the opposite side,
don, which turns medially around the pterygoid hamulus.
as they descend from their origin to form a narrow ten
The muscle fibers of the tensor veli palatini converge
nerve as it passes downward and forward in the carotid tri
ing hindbrain and later migrate inferiorly and anteriorly around
the mucous membrane just anterior to the sulcus terminalis,
of the tongue becomes free. Some of the entodermal cells remain
lying mesenchyme. Later, these cells degenerate so that this part
arches. Around the edge of the anterior two thirds of the tongue,
ryngeal arches and the anterior ends of the third pharyngeal
posterior third by a groove, the sulcus terminalis, which repre-
sents the interval between the lingual swellings of the first pha-
the entodermal cells proliferate and grow inferiorly into the under-
in the midline and help form the frenulum of the tongue.
Remember that the circumvallate papillae are situated on
and that their taste buds are innervated by the ninth cranial
nerve. It is presumed that during development the mucous
membrane of the posterior third of the tongue becomes pulled
anteriorly slightly, so that fibers of the ninth cranial nerve cross
the succus terminalis to supply these taste buds (Fig. 11.79).
The muscles of the tongue are derived from the occipital
myotomes, which at first are closely related to the develop-
the pharynx and enter the tongue. The migrating myotomes
carry with them their innervation, the 12th cranial nerve, and
this explains the long curving course taken by the 12th cranial
-
angle of the neck (see page 616).
-
-
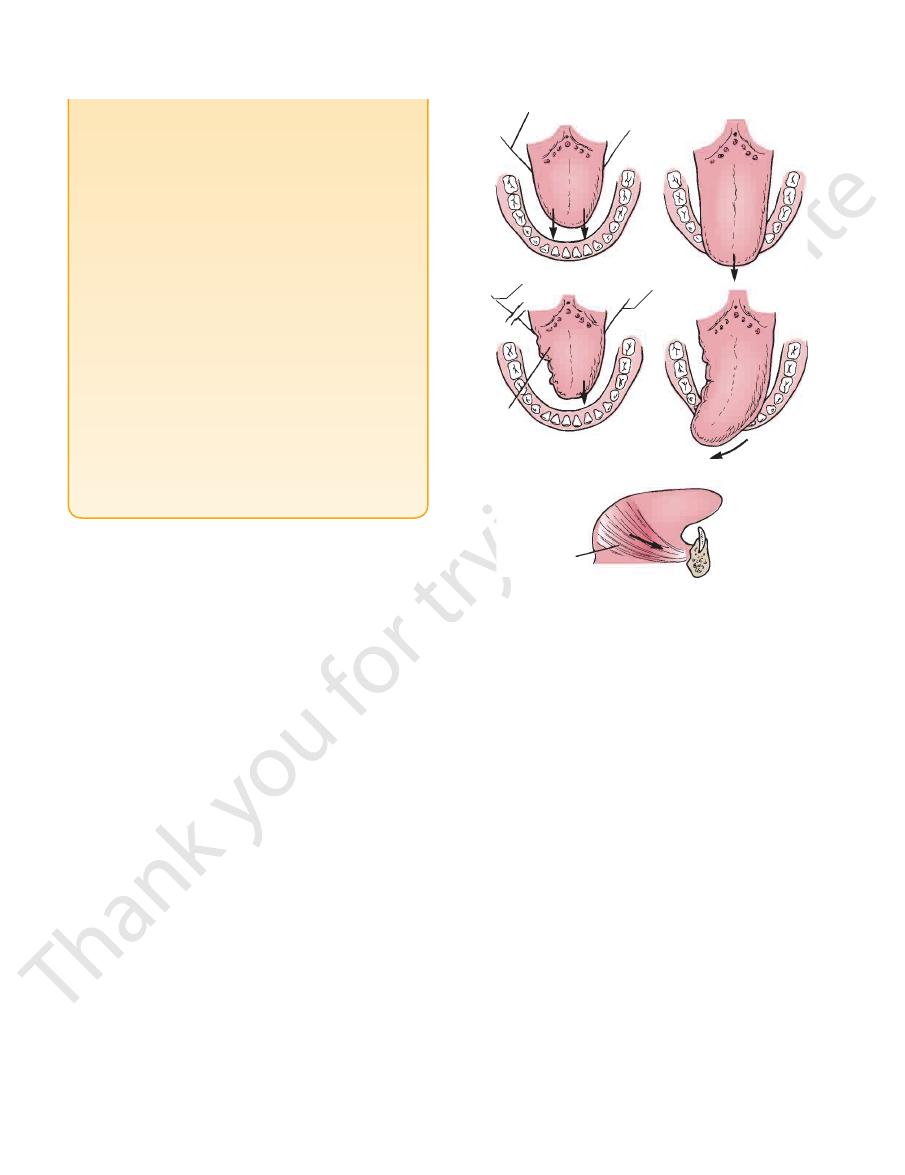
right hypoglossal nerve
cut right hypoglossal
nerve
intact
hypoglossal
nerve
right half
of tongue
atrophied
genioglossus muscle
A
B
C
D
E
FIGURE 11.78
Diagrammatic representation of the action of
geus, and the musculus uvulae (Fig. 11.81).
levator veli palatini, the palatoglossus, the palatopharyn
The muscles of the soft palate are the tensor veli palatini, the
Muscles of the Soft Palate
don of the tensor veli palatini muscle.
posterior border of the hard palate. It is the expanded ten
The palatine aponeurosis is a fibrous sheet attached to the
Palatine Aponeurosis
faces of the soft palate.
The mucous membrane covers the upper and lower sur
Mucous Membrane
tine aponeurosis, and muscles.
The soft palate is composed of mucous membrane, pala
lateral wall of the pharynx.
The soft palate is continuous at the sides with the
uvula.
der presents in the midline a conical projection called the
border of the hard palate (Fig. 11.81). Its free posterior bor
The soft palate is a mobile fold attached to the posterior
(Fig. 11.80). It is continuous behind with the soft palate.
maxillae and the horizontal plates of the palatine bones
The hard palate is formed by the palatine processes of the
front and the soft palate behind.
nasal cavity. It is divided into two parts: the hard palate in
The palate forms the roof of the mouth and the floor of the
The origin and insertion and direction of
the nerve lesion.
asked to protrude the tongue, the tip points to the side of
When the patient is
The right hypoglossal nerve (which innervates
the tip of the tongue is protruded in the
The right and left muscles contract equally together
the right and left genioglossus muscles of the tongue.
A.
and as a result (B)
midline. C.
the genioglossus muscle and the intrinsic tongue muscles
on the same side) is cut and as a result the right side of the
tongue is atrophied and wrinkled. D.
E.
pull of the genioglossus muscle.
The Palate
Hard Palate
Soft Palate
-
-
-
-
-
