
Basic Anatomy
59
C H A P T E R O U T L I N E
(continued)
natomy
asic
B
a
Chest Cavity
vertebrae (see Fig. 3.2).
body of the sternum and behind by the lower eight thoracic
The inferior mediastinum is bounded in front by the
duct, (d) descending aorta, and (e) sympathetic trunks.
phrenic nerves on each side, (c) esophagus and thoracic
(a) Thymus, (b) heart within the pericardium with the
vertebrae (see Fig. 3.2).
manubrium sterni and behind by the first four thoracic
The superior mediastinum is bounded in front by the
(e) esophagus and thoracic duct, and (f) sympathetic trunks.
(a) Thymus, (b) large veins, (c) large arteries, (d) trachea,
the following order from anterior to posterior.
ber that the major mediastinal structures are arranged in
For purposes of orientation, it is convenient to remem
between the pericardium and the vertebral column.
which lies
posterior mediastinum,
and the sternum; and the
which is a space between the pericardium
mediastinum,
anterior
which consists of the pericardium and heart; the
middle mediastinum,
astinum is further subdivided into the
thoracic vertebra posteriorly (Fig. 3.2). The inferior medi
angle anteriorly to the lower border of the body of the 4th
by an imaginary plane passing from the sternal
mediastina
inferior
superior
The mediastinum is divided into
sympathetic trunks.
and lymph nodes, the vagus and phrenic nerves, and the
blood vessels, the trachea and esophagus, the thoracic duct
contains the remains of the thymus, the heart and large
to the sternum and posteriorly to the vertebral column. It
neck and inferiorly to the diaphragm. It extends anteriorly
extends superiorly to the thoracic outlet and the root of the
The mediastinum, though thick, is a movable partition that
lungs (Figs. 3.1, 3.2, and 3.3).
and the laterally placed pleurae and
mediastinum,
chest cavity can be divided into a median partition, called
that separates the chest from the abdominal viscera. The
only structure (apart from the pleura and the peritoneum)
Fig. 3.5). The diaphragm, which is a very thin muscle, is the
about one fingerbreadth above the clavicle on each side (see
the diaphragm. It extends upward into the root of the neck
The chest cavity is bounded by the chest wall and below by
the
Mediastinum
and
-
-
Superior Mediastinum
Inferior Mediastinum
C H A P T E R O B J E C T I V E S
To learn the structure of the heart, including its conducting
pericardial cavity,
thoracic cavity, pleural cavity
To be able to define what is meant by the term
To understand the general arrangement of the thoracic viscera
■
■
and their relationship to one another and to the chest wall.
■
■
mediastinum and
to learn the arrangement of the pleura relative to the lungs. This
information is fundamental to the comprehension of the function
and disease of the lungs.
■
■
Appreciating that the heart and the lungs are enveloped in
serous membranes that provide a lubricating mechanism for
these mobile viscera and being able to distinguish between
such terms as
(pleural space),
and costodiaphragmatic recess.
■
■
system and the arrangement of the different chambers and
valves, which is basic to understanding the physiologic and
pathologic features of the heart. The critical nature of the
blood supply to the heart and the end arteries and myocardial
infarction is emphasized.
Trauma to the chest wall can result in disruption of these
are located within the thoracic cavity, namely, the aorta, the
To understand that the largest blood vessels in the body
■
■
pulmonary arteries, the venae cavae, and the pulmonary veins.
vessels, with consequent rapid hemorrhage and death.
Because these vessels are hidden from view within the
thorax, the diagnosis of major blood vessel injury is often
delayed, with disastrous consequences to the
patient.
Esophagus 100
Blood Supply of the Esophagus 100
Lymph Drainage of the Esophagus 100
Nerve Supply of the Esophagus 100
Thymus 100
Blood Supply 100
Cross-Sectional Anatomy of the Thorax 102
Radiographic Anatomy 102
Posteroanterior Radiograph 102
Right Oblique Radiograph 105
Left Oblique Radiograph 105
Bronchography and Contrast
Visualization of the Esophagus 105
Coronary Angiography 107
CT Scanning of the Thorax 107
60
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
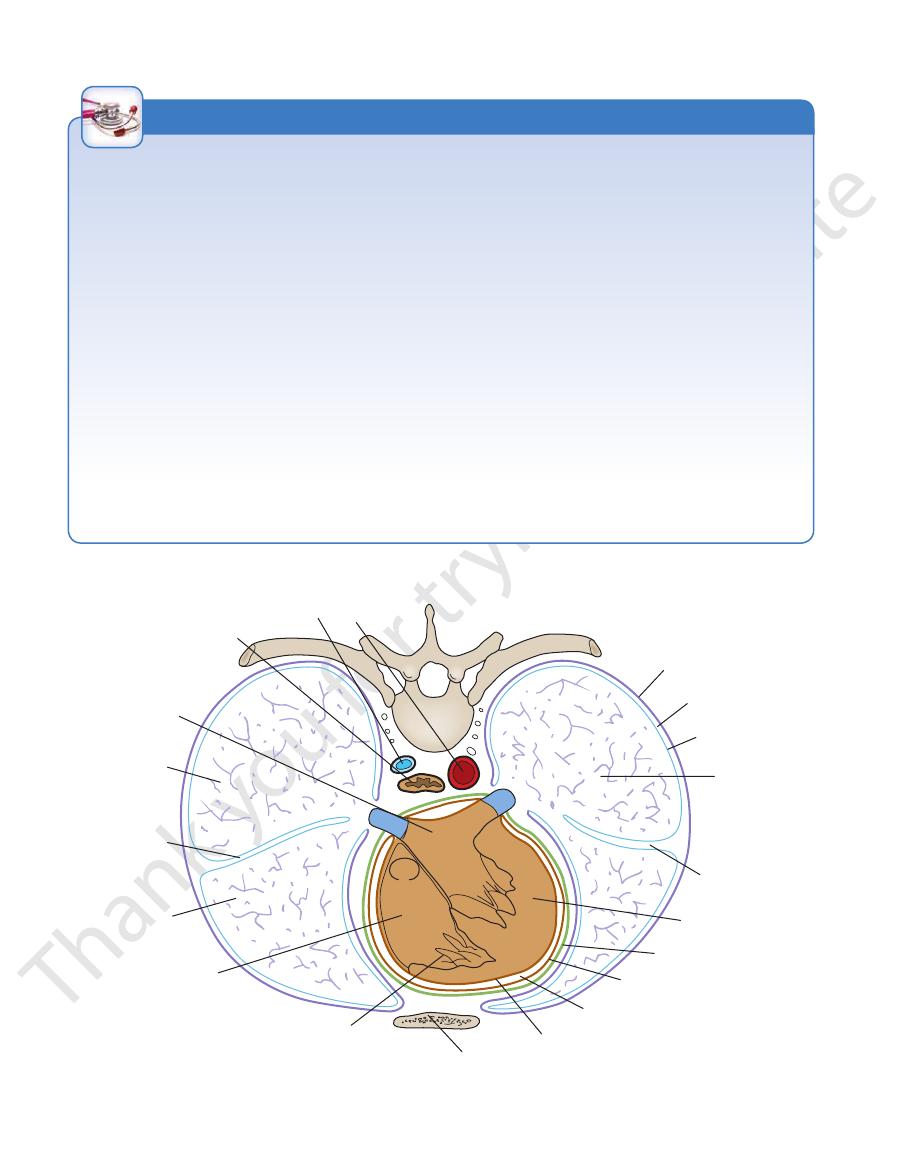
esophagus
aygos vein aorta
left atrium
right atrium
right ventricle
left ventricle
pleural space
parietal pleura
right lung,
lower lobe
left lung,
lower lobe
right lung,
upper lobe
right oblique
fissure
left oblique
fissure
visceral serous
pericardium
parietal serous
pericardium
fibrous pericardium
sternum
pericardial cavity
visceral pleura
FIGURE 3.1
Cross section of the thorax at the level of the eighth thoracic vertebra. Note the arrangement of the pleura and
pleural cavity (space) and the fibrous and the serous pericardia.
Deflection of Mediastinum
mine the diagnosis and degree of spread of carcinoma of the
bifurcation of the trachea. The procedure can be used to deter
superior mediastinum is explored down to the region of the
midline in the neck just above the suprasternal notch, and the
opening the pleural cavities. A small incision is made in the
mens of tracheobronchial lymph nodes are obtained without
phrenic nerves, and sometimes the trachea, main bronchi, and
Other pressure effects can be seen on the sympathetic trunks,
severe congestion of the veins of the upper part of the body.
tumor can partially occlude the superior vena cava, causing
producing paralysis of the left vocal fold. An expanding cyst or
enlargement may compress the left recurrent laryngeal nerve,
idly spread to involve the mediastinal lymph nodes, which on
enlarging tumor or organ. A tumor of the left lung can rap
the mediastinum, their functions can be interfered with by an
Because many vital structures are crowded together within
itself by the patient’s being breathless and in a state of shock; on
astinum is displaced to the opposite side. This condition reveals
in rhythmic pulsation, and the esophagus distends as each bolus
effect of the preserving fluids, is an inflexible, fixed structure. In
In the cadaver, the mediastinum, as the result of the hardening
the living, it is very mobile; the lungs, heart, and large arteries are
of food passes through it.
If air enters the pleural cavity (a condition called pneumotho-
rax), the lung on that side immediately collapses and the medi-
examination, the trachea and the heart are found to be displaced
to the opposite side.
Mediastinitis
The structures that make up the mediastinum are embedded in
loose connective tissue that is continuous with that of the root
of the neck. Thus, it is possible for a deep infection of the neck
to spread readily into the thorax, producing a mediastinitis.
Penetrating wounds of the chest involving the esophagus may
produce a mediastinitis. In esophageal perforations, air escapes
into the connective tissue spaces and ascends beneath the fas-
cia to the root of the neck, producing subcutaneous emphysema.
Mediastinal Tumors or Cysts
-
esophagus.
Mediastinoscopy
Mediastinoscopy is a diagnostic procedure whereby speci-
-
bronchus.
C L I N I C A L N O T E S
Basic Anatomy
of the suprapleural membrane at the thoracic outlet; and a
extends into the root of the neck to line the undersurface
phragm and the lateral aspect of the mediastinum and
the thoracic wall, covers the thoracic surface of the dia
which lines
parietal layer,
Each pleura has two parts: a
the development of the lungs in Figure 3.4.
pleurae, it might be helpful to look at the illustrations of
num within the chest cavity (Fig. 3.3). Before discussing the
The pleurae and lungs lie on either side of the mediasti
61
Pleurae
-
-
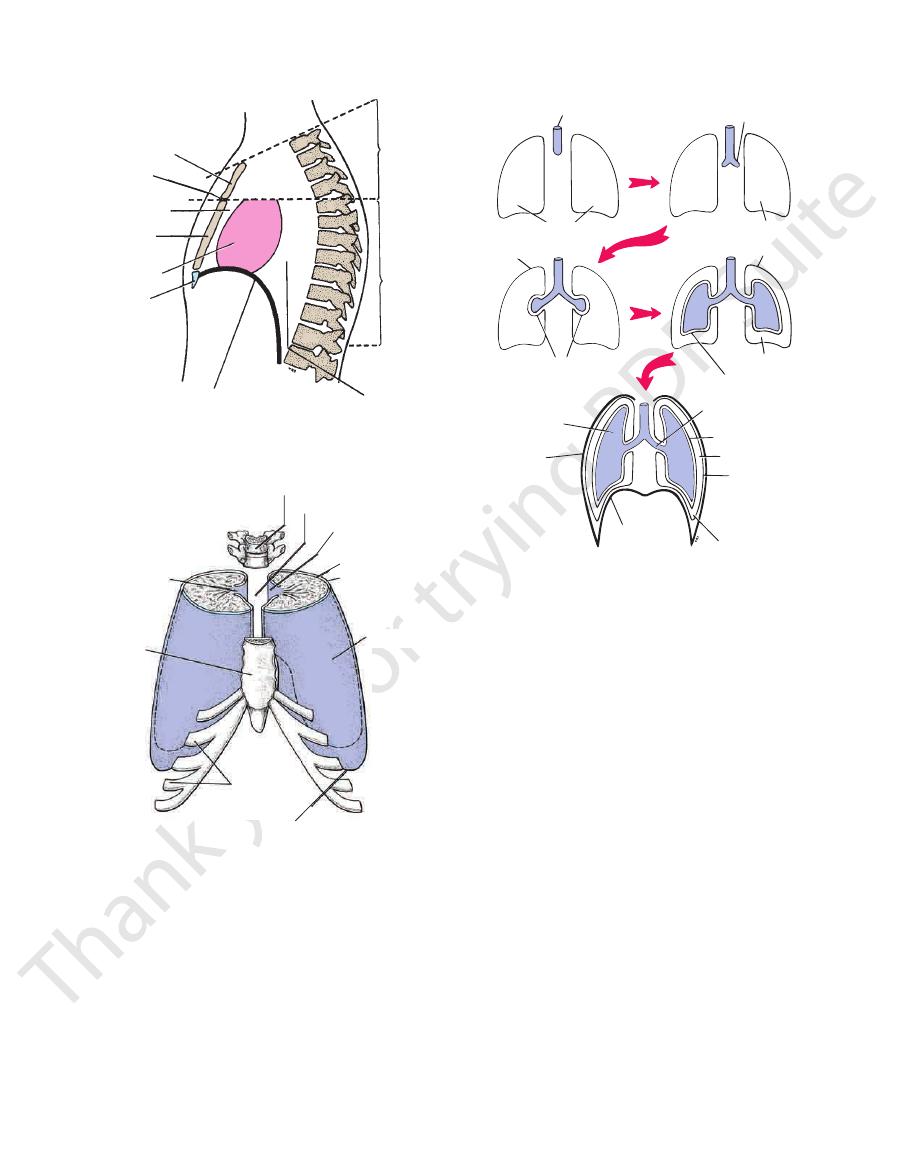
T1
4
5
T12
manubrium
sternal
angle
body of
sternum
xiphoid
process
posterior
mediastinum
inferior
mediastinum
superior
mediastinum
diaphragm
anterior
mediastinum
middle
mediastinum
FIGURE 3.2
Subdivisions of the mediastinum.
vertebral column
mediastinum
mediastinal pleura
(parietal pleura)
visceral pleura
pleural cavity
(space)
costal pleura
(parietal pleura)
body of
sternum
hilum of lung
costal
cartilages
diaphragmatic pleura
(parietal pleura)
FIGURE 3.3
Pleurae from above and in front. Note the posi
tion of the mediastinum and the hilum of each lung.
-
laryngotracheal tube
coelomic cavity
lung bud
coelomic cavity
parietal pleura
visceral pleura
parietal pleura
pleural cavity
lung
thoracic
wall
diaphragm
costodiaphragmatic
recess
parietal pleura
pleural cavity
visceral pleura
root of lung
visceral pleura
FIGURE 3.4
Formation of the lungs. Note that each lung bud
the surface that it covers. The cervical pleura extends up
parietal pleura according to the region in which it lies or
For purposes of description, it is customary to divide the
each other with the minimum of friction.
pleura as a thin film and permits the two layers to move on
which covers the surfaces of the
pleural fluid,
sue fluid, the
The pleural cavity normally contains a small amount of tis
pleural cavity [slitlike] space and the larger chest cavity.)
This is probably to avoid the confusion between the
cavity.
pleural
instead of the anatomic term
pleural space
term
(Figs. 3.3 and 3.4). (Clinicians are increasingly using the
pleural cavity
from one another by a slitlike space, the
The parietal and visceral layers of pleura are separated
(Fig. 3.5).
nary ligament
pleural cuff hangs down as a loose fold called the
monary vessels and large bronchi during respiration, the
(Figs. 3.3, 3.4, and 3.5). To allow for movement of the pul
entering and leaving the lung at the hilum of each lung
by means of a cuff of pleura that surrounds the structures
The two layers become continuous with one another
fissures (Figs. 3.1, 3.3, 3.4, 3.5, and 3.6).
of the lungs and extends into the depths of the interlobar
which completely covers the outer surfaces
visceral layer,
growth of the lung.
to a slitlike space called the pleural cavity as a result of the
with parietal pleura. The original coelomic cavity is reduced
covered with visceral pleura and the thoracic wall is lined
to fill a greater part of the cavity. Note also that the lung is
invaginates the wall of the coelomic cavity and then grows
-
pulmo-
-

62
CHAPTER 3
left costodiaphragmatic recesses and the right and left
fully occupy the pleural cavities at four sites: the right and
ties. However, during quiet inspiration, the lungs do not
full inspiration, the lungs expand and fill the pleural cavi
During
lung root.
sels and bronchi that constitute the
except at its hilum, where it is attached to the blood ves
the visceral pleura. It is thus seen that each lung lies free
vessels and bronchi and here becomes continuous with
the hilum of the lung, it is reflected as a cuff around the
boundary of the mediastinum (see Figs. 3.3 and 3.5). At
covers and forms the lateral
mediastinal pleura
The
(Figs. 3.4 and 3.5).
costodiaphragmatic recess
inspiration is referred to as the
area of the pleural cavity into which the lung expands on
the costal and diaphragmatic pleurae separate. This lower
ration, the margins of the base of the lung descend, and
other below the lower border of the lung. In deep inspi
costal and diaphragmatic pleurae are in apposition to each
the diaphragm (Figs. 3.3 and 3.5). In quiet respiration, the
covers the thoracic surface of
diaphragmatic pleura
The
tebral bodies, and the back of the sternum (Fig. 3.3).
costal cartilages, the intercostal spaces, the sides of the ver
lines the inner surfaces of the ribs, the
costal pleura
The
to 4 cm) above the medial third of the clavicle.
membrane (see Fig. 2.13). It reaches a level 1 to 1.5 in. (2.5
into the neck, lining the undersurface of the suprapleural
The Thorax: Part II—The Thoracic Cavity
-
-
-
-
costomediastinal recesses.
six intercostal nerves.
the phrenic nerve and around the periphery by the lower
The diaphragmatic pleura is supplied over the domes by
nerve.
The mediastinal pleura is supplied by the phrenic
costal nerves.
The costal pleura is segmentally supplied by the inter
ture, touch, and pressure and is supplied as follows:
The parietal pleura (Fig. 3.7) is sensitive to pain, tempera
described on pages 54 and 55.
The surface markings of the lungs and pleurae were
lungs slide in and out of the recesses.
inspiration and expiration, the anterior borders of the
are separated by a capillary layer of pleural fluid. During
between the costal and mediastinal parietal pleurae, which
anterior margins of the pleura. They are slitlike spaces
are situated along the
costomediastinal recesses
The
come together again.
lungs ascend so that the costal and diaphragmatic pleurae
the recesses. During expiration, the lower margins of the
ing inspiration, the lower margins of the lungs descend into
are separated only by a capillary layer of pleural fluid. Dur
between the costal and diaphragmatic parietal pleurae that
are slitlike spaces
costodiaphragmatic recesses
The
-
Nerve Supply of the Pleura
-
■
■
-
■
■
■
■
cervical pleura
(parietal pleura)
mediastinal pleura
(parietal pleura)
cuff of pleura
diaphragmatic pleura
(parietal pleura)
pulmonary ligament
lower lobe
upper lobe
bronchi
costal pleura
(parietal pleura)
oblique fissure
left lung
visceral pleura
pulmonary veins
FIGURE 3.5
Different areas of the parietal pleura. Note the cuff of pleura (
Arrows
and leaving the hilum of the left lung. It is here that the parietal and the visceral layers of pleura become continuous.
) that surrounds structures entering
dotted lines
indicate the position of the costodiaphragmatic recess.
Basic Anatomy
by dividing into right and left principal (main)
carina
line of the neck. In the thorax, the trachea ends below at
level of the 6th cervical vertebra. It descends in the mid
the larynx at the lower border of the cricoid cartilage at the
tube (Fig. 3.9). It begins in the neck as a continuation of
The trachea is a mobile cartilaginous and membranous
Trachea
monary plexus (Fig. 3.7).
touch. It receives an autonomic nerve supply from the pul
but is insensitive to common sensations such as pain and
The visceral pleura covering the lungs is sensitive to stretch
63
-
-
the
nerve
first rib
trachea
cervical dome of
pleura
right vagus
right phrenic
nerve
brachiocephalic
artery
infrahyoid
muscles
thymus left common carotid artery
left internal jugular vein
internal thoracic artery
left phrenic nerve
left vagus nerve
left subclavian artery
left recurrent laryngeal
nerve
first thoracic nerve
thoracic duct
sympathetic trunk
esophagus
T1
superior vena
cava
right phrenic
nerve
right lung
azygos vein
right vagus nerve
trachea
esophagus
sympathetic
trunk
thoracic duct
left recurrent laryngeal
nerve
left lung
left vagus nerve
left phrenic nerve
arch of aorta
manubrium sterni
thymus
T4
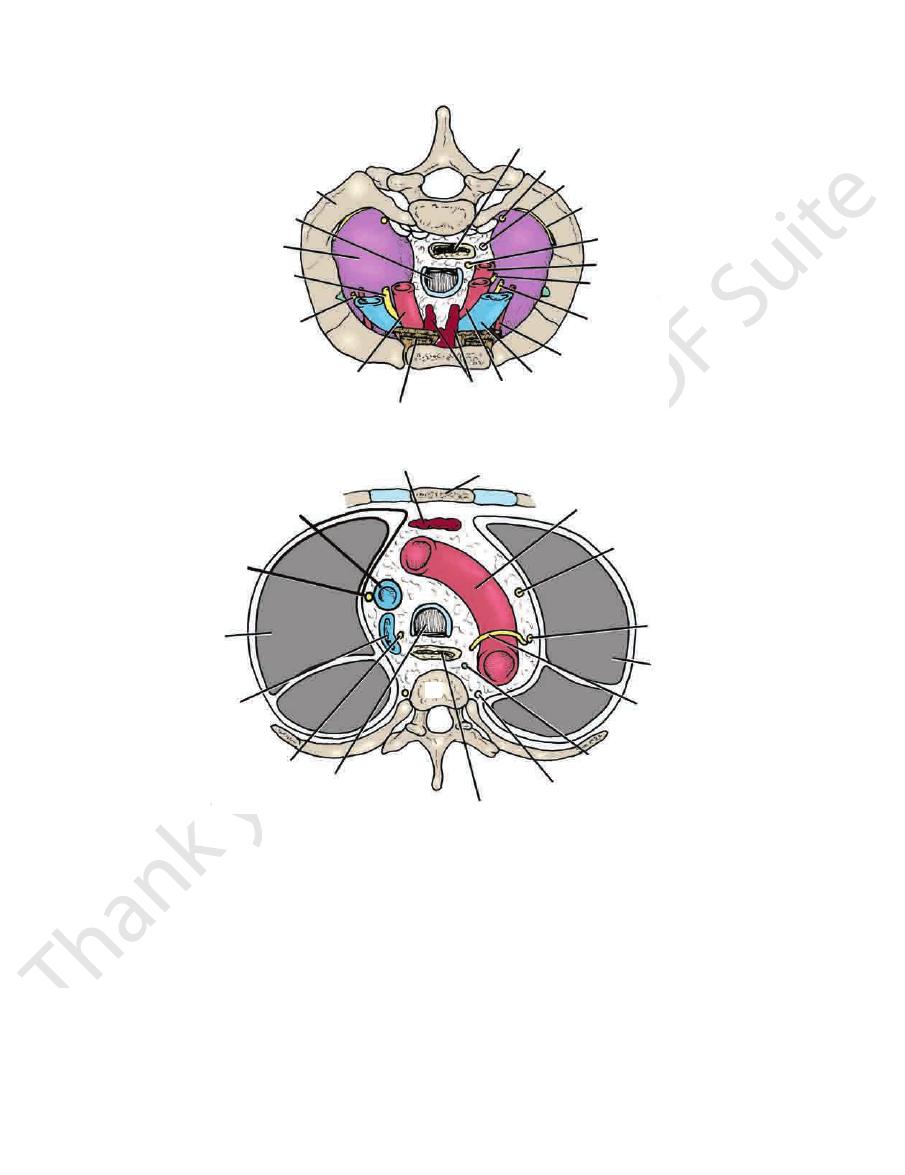
A
B
FIGURE 3.6
Cross section of the thorax.
below.
At the 4th thoracic vertebra, as seen from
At the inlet, as seen from above.
A:
B:
Phrenic nerves
(C3, C4, and C5)
Intercostal
nerves
(T1-T11)
Parietal pleura
Visceral pleura
Nerves of
pulmonary plexus
(vagus and
sympathetic)
FIGURE 3.7
Diagram showing the innervation of the parietal
and visceral layers of pleura.
