

80
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
Pericarditis
Pericardial fluid can be aspirated from the pericardial cavity
etrated. The blood escapes into the pericardial cavity and can
shot wounds when the chambers of the heart have been pen
heart during diastole. This compression of the heart is called
In inflammation of the serous pericardium, called pericarditis,
pericardial fluid may accumulate excessively, which can com-
press the thin-walled atria and interfere with the filling of the
cardiac tamponade.
Cardiac tamponade can also occur secondary to stab or gun-
-
restrict the filling of the heart.
Roughening of the visceral and parietal layers of serous peri-
cardium by inflammatory exudate in acute pericarditis produces
pericardial friction rub, which can be felt on palpation and heard
through a stethoscope.
should excessive amounts accumulate in pericarditis. This pro-
cess is called paracentesis. The needle can be introduced to the
left of the xiphoid process in an upward and backward direction
at an angle of 45° to the skin. When paracentesis is performed
at this site, the pleura and lung are not damaged because of the
presence of the cardiac notch in this area.
C L I N I C A L N O T E S
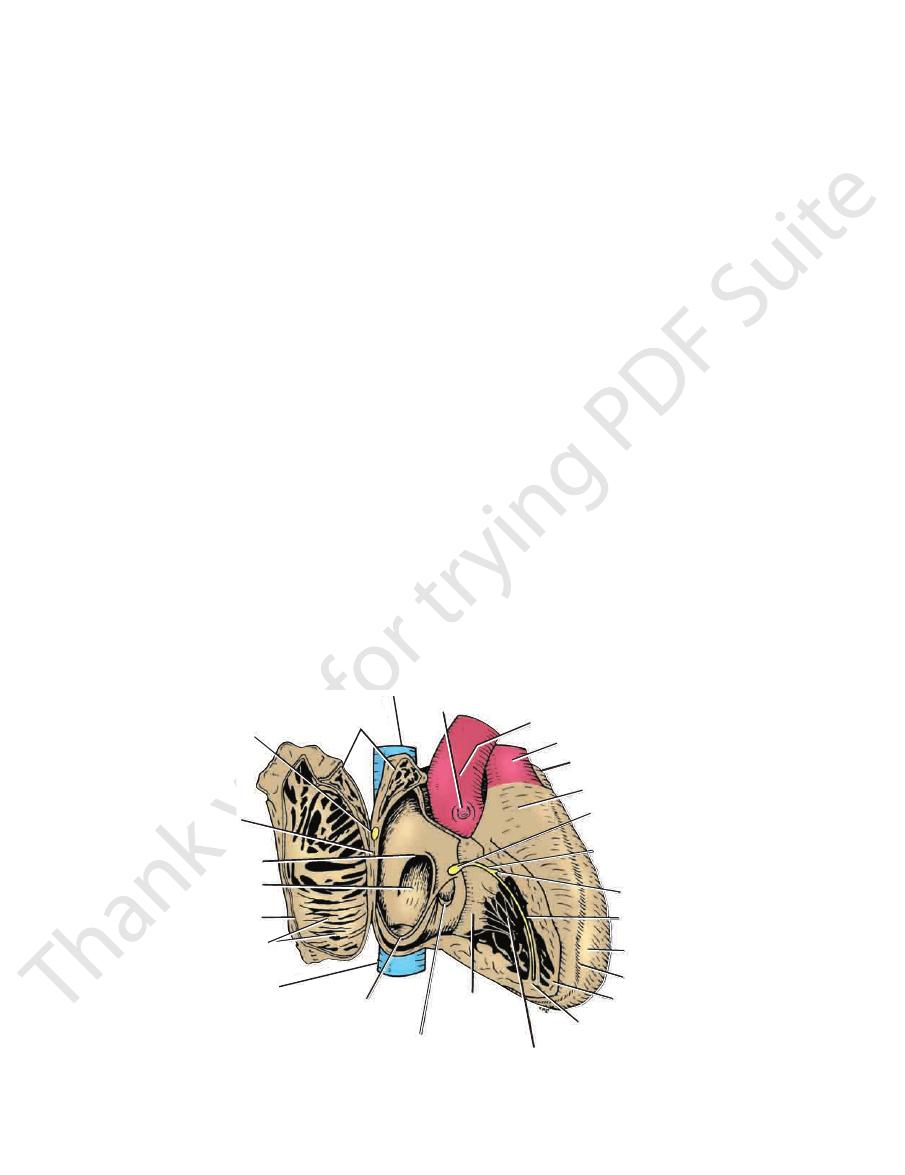
right common carotid artery
brachiocephalic artery
right subclavian artery
right
brachiocephalic vein
superior vena cava
transverse sinus
right pulmonary veins
reflection to left
atrium
inferior vena cava
fibrous pericardium
parietal layer of serous
pericardium
reflection of serous pericardium
left pulmonary vein
bronchus
left pulmonary artery
ligamentum arteriosum
left recurrent laryngeal nerve
left vagus nerve
left phrenic nerve
arch of aorta
left subclavian artery
left common carotid artery
left brachiocephalic vein
oblique sinus
FIGURE 3.32
The great blood vessels and the interior of the pericardium.
from each other by the vertical atrioventricular groove
right atrium and the right ventricle, which are separated
is formed mainly by the
sternocostal surface
The
(Fig. 3.34). The right border is formed by the right atrium;
It lies at the level of the fifth left intercostal space, 3.5 in.
directed downward, forward, and to the left (Fig. 3.34).
formed by the left ventricle, is
apex of the heart,
The
veins (Fig. 3.35). The base of the heart lies opposite the apex.
mainly by the left atrium, into which open the four pulmonary
or the posterior surface, is formed
base of the heart,
The
forms part of this surface.
right atrium, into which the inferior vena cava opens, also
terior interventricular groove. The inferior surface of the
mainly by the right and left ventricles separated by the pos
of the heart is formed
diaphragmatic surface
The
by the anterior interventricular groove.
cle. The right ventricle is separated from the left ventricle
the left border, by the left ventricle and part of the left auri-
-
(9 cm) from the midline. In the region of the apex, the apex
beat can usually be seen and palpated in the living patient.

Basic Anatomy
81
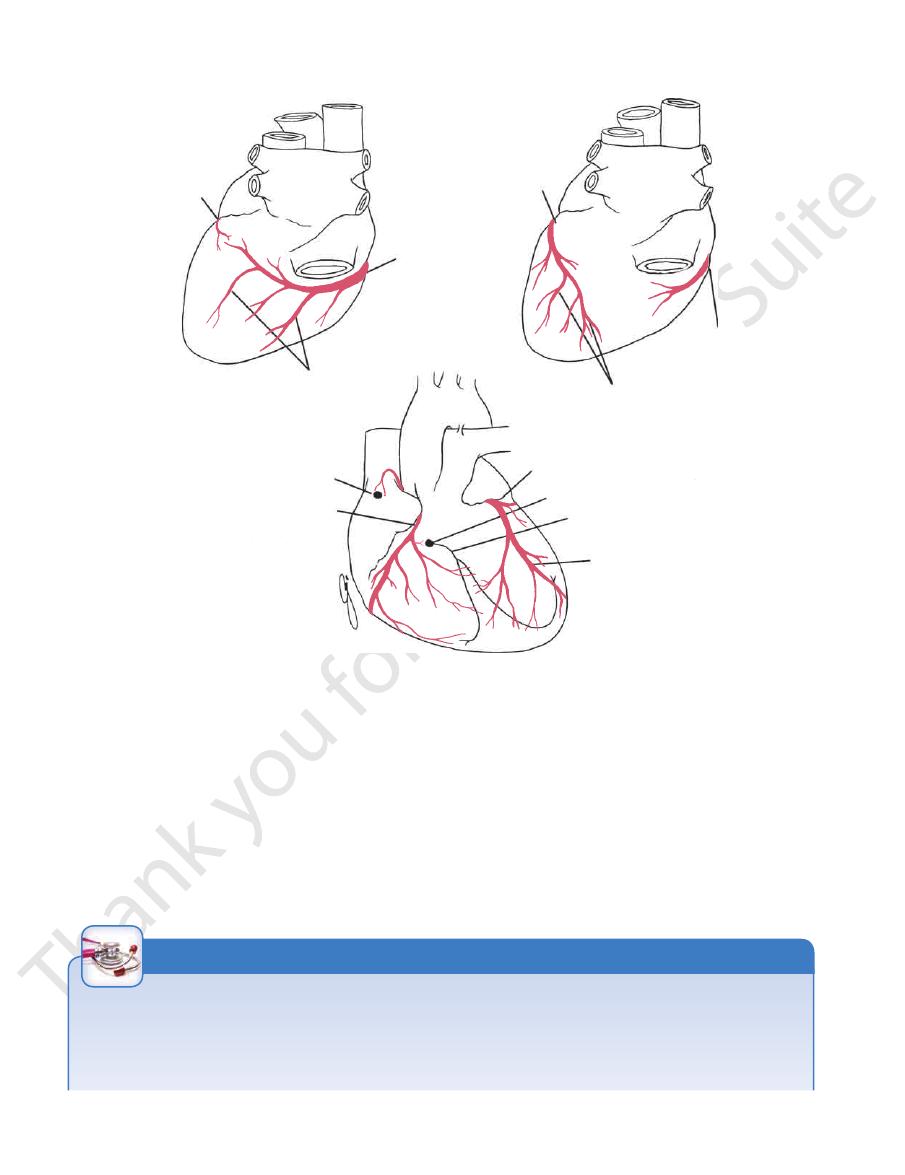
arch of aorta left common carotid artery
pulmonary trunk
left auricle
left coronary artery
circumflex branch
great cardiac vein
left ventricle
anterior
interventricular
artery
apex
interventricular groove
right ventricle
marginal
artery
atrioventricular
groove
anterior cardiac
vein
right
atrium
right coronary
artery
right auricle
ascending
aorta
right pulmonary
artery
superior vena cava
brachiocephalic
artery
left subclavian artery
ascending aorta
pulmonary trunk
(cut)
left auricle
right auricle
left
ventricle
right
ventricle
right
atrium
apex
superior vena cava
arch of aorta
(cut)
atrioventricular
groove
anterior
interventricular
groove
filled
with
fat
FIGURE 3.33
The anterior surface of the heart; the fibrous pericardium and the parietal serous pericardium have been
grooves. The coronary arteries are embedded in this fat.
removed. Note the presence of fat beneath the visceral serous pericardium in the atrioventricular and interventricular
FIGURE 3.34
The anterior surface of the heart and the great
the cardiac veins.
blood vessels. Note the course of the coronary arteries and
left common
carotid artery
left subclavian
artery
pulmonary
veins
left atrium
left ventricle
coronary sinus
inferior vena cava
right atrium
superior vena cava
bifurcation of pulmonary
trunk
ligamentum arteriosum
left recurrent laryngeal nerve
arch of
aorta
FIGURE 3.35
The posterior surface, or the base, of the heart.
82
CHAPTER 3
secundum (Fig. 3.37).
and the anulus is formed from the lower edge of the septum
the persistent septum primum of the heart of the embryo,
upper margin of the fossa. The floor of the fossa represents
in the fetus (Fig. 3.37). The anulus ovalis forms the
ovale
foramen
lis is a shallow depression, which is the site of the
right atrium from the left atrium (Fig. 3.36). The fossa ova
which separates the
atrial septum,
structures lie on the
These latter
anulus ovalis.
fossa ovalis
cava are the
In addition to the rudimentary valve of the inferior vena
Fetal Remnants
the heart and open directly into the right atrium.
Many small orifices of small veins also drain the wall of
valve (Fig. 3.36).
inferior vena caval opening and is guarded by the tricuspid
lies anterior to the
right atrioventricular orifice
The
fice. It is guarded by a rudimentary, nonfunctioning valve.
between the inferior vena cava and the atrioventricular ori
from the heart wall (Fig. 3.36), opens into the right atrium
which drains most of the blood
coronary sinus,
The
heart from the lower half of the body.
mentary, nonfunctioning valve. It returns the blood to the
the lower part of the right atrium; it is guarded by a rudi
(larger than the superior vena cava) opens into
vena cava
inferior
to the heart from the upper half of the body. The
part of the right atrium; it has no valve. It returns the blood
(Fig. 3.36) opens into the upper
superior vena cava
The
Openings into the Right Atrium
from the primitive atrium.
to the auricle. This anterior part is derived embryologically
which run from the crista terminalis
musculi pectinati,
is roughened or trabeculated by bundles of muscle fibers,
sinus venosus. The part of the atrium in front of the ridge
is smooth walled and is derived embryologically from the
The main part of the atrium that lies posterior to the ridge
crista terminalis.
which on the inside forms a ridge, the
sulcus terminalis,
the right auricle is a vertical groove, the
of the heart at the junction between the right atrium and
pouching, the auricle (Figs. 3.34 and 3.36). On the outside
The right atrium consists of a main cavity and a small out
Right Atrium
endocardium.
endothelium, the
and lined internally with a layer of
epicardium;
dium, the
covered externally with serous pericar
myocardium;
The walls of the heart are composed of cardiac muscle,
ventricle lies anterior to the left ventricle.
right atrium lies anterior to the left atrium, and the right
the right and left atria and the right and left ventricles. The
The heart is divided by vertical septa into four chambers:
when examining a radiograph of the heart.
the left ventricle. These borders are important to recognize
ventricle but also by the right atrium; the apex is formed by
(Fig. 3.34). The lower border is formed mainly by the right
border, by the left auricle; and below, by the left ventricle
The right border is formed by the right atrium; the left
matic (inferior) surface.
The heart does not rest on its base; it rests on its diaphrag
the heart is pyramid shaped; the base lies opposite the apex.
because
Note that the base of the heart is called the
The Thorax: Part II—The Thoracic Cavity
base
-
Borders of the Heart
Chambers of the Heart
the
-
-
the
-
-
and
-
superior vena cava
right auricle
sinuatrial node
crista terminalis
anulus ovalis
fossa ovalis
anterior wall of
right atrium
(reflected)
musculi pectinati
inferior vena cava
valve of inferior vena cava
valve of coronary sinus
chordae tendineae
septal cusp of
tricuspid valve
moderator band
right ventricle
interventricular
groove
left ventricle
right
branch of bundle
left
branch of bundle
atrioventricular bundle
infundibulum
left auricle
pulmonary trunk
ascending aorta
right coronary artery
atrioventricular node
FIGURE 3.36
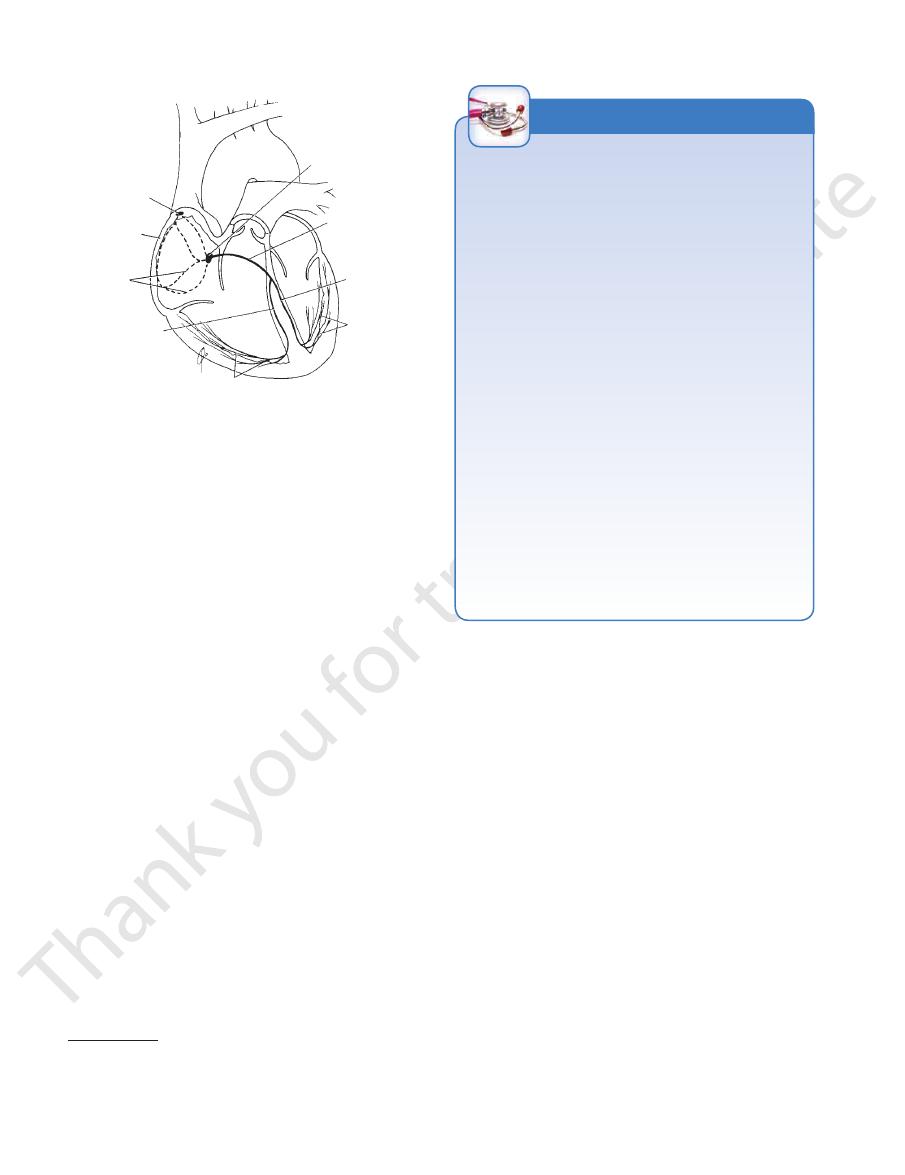
Interior of the right atrium and the right ventricle. Note the positions of the sinuatrial node and the atrioventricu-
lar node and bundle.

Basic Anatomy
83
septum secundum
septum primum
foramen ovale
A
B
pulmonary stenosis
hypertrophy of
right ventricle
C
septal defect
displaced aortic
opening
left recurrent laryngeal
nerve
D
E
FIGURE 3.37
gus (Figs. 3.32 and 3.39).
and the fibrous pericardium separates it from the esopha
Behind it lies the oblique sinus of the serous pericardium,
base or the posterior surface of the heart (see Fig. 3.35).
behind the right atrium and forms the greater part of the
main cavity and a left auricle. The left atrium is situated
Similar to the right atrium, the left atrium consists of a
Left Atrium
and close the pulmonary orifice.
cusps fill, come into apposition in the center of the lumen,
flows back toward the heart and enters the sinuses; the valve
nary trunk by the outrushing blood. During diastole, blood
cusps of the valve are pressed against the wall of the pulmo
of unnecessary confusion.) During ventricular systole, the
rotated to the left. This, unfortunately, causes a great deal
according to their position in the fetus before the heart has
(The cusps of the pulmonary and aortic valves are named
rior (left cusp) and two anterior (anterior and right cusps).
The three semilunar cusps are arranged with one poste
aortic valve
(see
and one is situated external to each cusp
sinuses,
called the
cle. At the root of the pulmonary trunk are three dilatations
rial wall prevent the cusps from prolapsing into the ventri
cusps; the attachments of the sides of the cusps to the arte
chordae or papillary muscles are associated with these valve
cusps are directed upward into the pulmonary trunk. No
are attached to the arterial wall. The open mouths of the
enclosed. The curved lower margins and sides of each cusp
by folds of endocardium with some connective tissue
(Fig. 3.38A) and consists of three semilunar cusps formed
guards the pulmonary orifice
pulmonary valve
The
the adjacent parts of two cusps.
chordae tendineae of one papillary muscle are connected to
intraventricular pressure rises. To assist in this process, the
being forced into the atrium and turning inside out as the
the papillary muscles contract and prevent the cusps from
When the ventricle contracts,
papillary muscles.
to the
The chordae tendineae connect the cusps
dae tendineae.
chor
free edges and ventricular surfaces are attached to the
ring of the skeleton of the heart (see below), whereas their
inferiorly. The bases of the cusps are attached to the fibrous
ventricular septum, and the inferior or posterior cusp lies
rior cusp lies anteriorly, the septal cusp lies against the
(posterior) cusps. The ante
inferior
anterior, septal,
fold of endocardium with some connective tissue enclosed:
(Figs. 3.36 and 3.38) and consists of three cusps formed by a
guards the atrioventricular orifice
tricuspid valve
The
heart. The third type is simply composed of prominent ridges.
tricular bundle, which is part of the conducting system of the
the anterior wall. It conveys the right branch of the atrioven
crosses the ventricular cavity from the septal to
erator band,
mod
tricular wall, being free in the middle. One of these, the
(Fig. 3.36). The second type is attached at the ends to the ven
) to the cusps of the tricuspid valve
chordae tendineae
ventricular wall; their apices are connected by fibrous chords
which project inward, being attached by their bases to the
cles,
papillary mus
of three types. The first type comprises the
The trabeculae carneae are composed
trabeculae carneae.
the ventricular wall a spongelike appearance and are known
ridges formed of muscle bundles. The projecting ridges give
those of the right atrium and show several internal projecting
The walls of the right ventricle are much thicker than
dibulum.
funnel shaped, at which point it is referred to as the
As the cavity approaches the pulmonary orifice, it becomes
nary trunk through the pulmonary orifice (see Fig. 3.36).
through the atrioventricular orifice and with the pulmo
The right ventricle communicates with the right atrium
Right Ventricle
Coarctation of the aorta.
relationship to the left recurrent laryngeal nerve).
Patent ductus arteriosus (note the close
Tetralogy of Fallot.
Atrial septal defect.
Normal fetal heart.
A.
B.
C.
D:
E.
-
infun-
as
-
(the
-
-
-
and
-
-
-
-
).
-
-
-

84
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
pulmonary
valve
tricuspid valve
aortic sinus
A
B
D
E
C
F
G
H
LV
RV
FIGURE 3.38
Fibrous skeleton
Path taken by the cardiac impulse from the sinuatrial node to the Purkinje network.
Path taken by the blood
Cross section of the ventricles of the heart.
Semilunar cusps of the aortic valve.
Mitral cusps with valve
Mitral cusps with valve open.
Position of the tricuspid and pulmonary valves.
A.
B.
C.
closed. D.
E.
F.
through the heart. G.
H.
of the heart.
right atrium
left atrium
middle lobe of
right lung
right oblique
fissure
lower lobe
of right lung
esophagus
azygos vein
thoracic
duct
sympathetic trunk
splanchnic nerves
hemiazygos vein
descending aorta
oblique sinus
pulmonary vein
lower lobe of
left lung
left oblique fissure
upper lobe of left lung
pericardium
pericardial cavity
left ventricle
right ventricle
sternum
T8
FIGURE 3.39
Cross section of the thorax at the eighth thoracic vertebra, as seen from below. (Note that all computed tomog
raphy scans and magnetic resonance imaging studies are viewed from below.)
-
Basic Anatomy
The atrioventricular bundle (bundle of His) is the only
Atrioventricular Bundle
tricles before the ventricles start to contract.
ficient time for the atria to empty their blood into the ven
the atrioventricular node (about 0.11 seconds) allows suf
The speed of conduction of the cardiac impulse through
atrial myocardium.
stimulated by the excitation wave as it passes through the
by the atrioventricular bundle. The atrioventricular node is
From it, the cardiac impulse is conducted to the ventricles
the septal cusp of the tricuspid valve (Figs. 3.37 and 3.38).
lower part of the atrial septum just above the attachment of
The atrioventricular node is strategically placed on the
Atrioventricular Node
muscle of the atria and cause the muscle to contract.
impulses that spread in all directions through the cardiac
The node spontaneously gives origin to rhythmic electrical
the opening of the superior vena cava (Figs. 3.36 and 3.40).
in the upper part of the sulcus terminalis just to the right of
The sinuatrial node is located in the wall of the right atrium
Sinuatrial Node
that form the conducting system of the heart).
(specialized cardiac muscle fibers
Purkinje fibers
plexus of
its right and left terminal branches, and the subendocardial
atrioventricular bundle
atrioventricular node,
sinuatrial node,
ized cardiac muscle present in the
The conducting system of the heart consists of special
into the ventricles before the ventricles contract.
the ventricles allows time for the atria to empty their blood
slight delay in the passage of the impulse from the atria to
later by the contractions of both ventricles together. The
heart, so the atria contract first and together, to be followed
system and the impulse travels to different regions of the
tractile process originates spontaneously in the conducting
beats per minute in the resting adult. The rhythmic con
The normal heart contracts rhythmically at about 70 to 90
nuity between the atria and the ventricles.
skeleton of the heart forms the basis of electrical disconti
valves from stretching and becoming incompetent. The
rings support the bases of the valve cusps and prevent the
but provide attachment for the muscle fibers. The fibrous
the muscular walls of the atria from those of the ventricles
fibrous rings around the atrioventricular orifices separate
the membranous upper part of the ventricular septum. The
pulmonary, and aortic orifices and are continuous with
sists of fibrous rings that surround the atrioventricular,
(Fig. 3.38) con
skeleton of the heart
The so-called
nous and attached to the fibrous skeleton.
The smaller upper part of the septum is thin and membra
lower part of the septum is thick and formed of muscle.
by the anterior and posterior interventricular grooves. The
the left. Its position is indicated on the surface of the heart
ward and to the right and the other facing backward and to
The septum is placed obliquely, with one surface facing for
into the right and left ventricles.
(interventricular) septum
ventricular
the heart has thick walls and is divided by the
heart backward and to the right. The ventricular portion of
and left atria. The septum runs from the anterior wall of the
into the right
atrial (interatrial) septum
divided by the
atrial portion of the heart has relatively thin walls and is
epicardium and lined internally by the endocardium. The
diac muscle, the myocardium, covered externally by the
The walls of the heart are composed of a thick layer of car
the left coronary artery.
coronary artery, and the left posterior sinus gives origin to
The anterior aortic sinus gives origin to the right
tic sinus.
aor
Behind each cusp, the aortic wall bulges to form an
are located on the posterior wall (left and posterior cusps).
cusp is situated on the anterior wall (right cusp) and two
similar in structure to the pulmonary valve (Fig. 3.38). One
guards the aortic orifice and is precisely
aortic valve
The
the papillary muscles is similar to that of the tricuspid valve.
The attachment of the chordae tendineae to the cusps and
intervenes between the atrioventricular and aortic orifices.
of the tricuspid valve. The anterior cusp is the larger and
posterior, which have a structure similar to that of the cusps
(Fig. 3.38). It consists of two cusps, one anterior and one
guards the atrioventricular orifice
mitral valve
The
aortic vestibule.
aortic orifice is called the
but no moderator band. The part of the ventricle below the
developed trabeculae carneae, two large papillary muscles,
the cavity of the right ventricle (Fig. 3.38). There are well-
tic because of the bulging of the ventricular septum into
section, the left ventricle is circular; the right is crescen
times higher than that inside the right ventricle.) In cross
ventricle. (The left intraventricular blood pressure is six
(Fig. 3.38) are three times thicker than those of the right
through the aortic orifice. The walls of the left ventricle
through the atrioventricular orifice and with the aorta
The left ventricle communicates with the left atrium
Left Ventricle
valve.
The left atrioventricular orifice is guarded by the mitral
through the posterior wall (Fig. 3.35) and have no valves.
The four pulmonary veins, two from each lung, open
Openings into the Left Atrium
auricle possesses muscular ridges as in the right auricle.
The interior of the left atrium is smooth, but the left
85
-
-
Structure of the Heart
-
-
-
-
-
Conducting System of the Heart
-
-
the
the
and
-
-
band, where it crosses to the anterior wall of the right
side of the ventricular septum to reach the moderator
The right bundle branch (RBB) passes down on the right
tum, it divides into two branches, one for each ventricle.
tum. At the upper border of the muscular part of the sep
border of the membranous part of the ventricular sep
septal cusp of the tricuspid valve to reach the inferior
The atrioventricular bundle then descends behind the
dle descends through the fibrous skeleton of the heart.
travel from the atria to the ventricles (Fig. 3.40). The bun
thus the only route along which the cardiac impulse can
of the atria and the myocardium of the ventricles and is
pathway of cardiac muscle that connects the myocardium
-
-
-
86
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
sinuatrial
node
right atrium
internodal
pathways
right branch
of atrioventricular
bundle
Purkinje
plexus
Purkinje
plexus
left branch of
atrioventricular
bundle
atrioventricular
bundle
atrioventricular
node
FIGURE 3.40
The conducting system of the heart. Note the
the superior vena caval opening. It descends on the atrial
posterior end of the sinuatrial node and passes posterior to
leaves the
middle internodal pathway
tricular node. The
descends on the atrial septum and ends in the atrioven
and passes anterior to the superior vena caval opening. It
leaves the anterior end of the sinuatrial node
pathway
anterior internodal
ordinary cardiac muscle cells. The
a structure consisting of a mixture of Purkinje fibers and
special pathways in the atrial wall (Fig. 3.40), which have
phenomenon has been explained by the description of
can travel by passing along the ordinary myocardium. This
travel to the atrioventricular node more rapidly than they
Impulses from the sinuatrial node have been shown to
Internodal Conduction Paths
have the opposite effect.
rate of conduction of the impulse; the sympathetic nerves
parasympathetic nerves slow the rhythm and diminish the
enced by the autonomic nerve supply to the heart. The
The activities of the conducting system can be influ
chambers contract in a coordinated and efficient manner.
throughout the myocardium of the heart so that the different
impulses, but also for conducting these impulses rapidly
is responsible not only for generating rhythmic cardiac
It is thus seen that the conducting system of the heart
Purkinje plexus of the left ventricle.
which eventually become continuous with the fibers of the
usually divides into two branches (anterior and posterior),
passes down on its left side beneath the endocardium. It
The left bundle branch (LBB) pierces the septum and
the Purkinje plexus (Fig. 3.40).
ventricle. Here, it becomes continuous with the fibers of
internodal pathways.
-
*
-
Failure of the Conduction System of the Heart
likely to occur if the blow occurs during the upstroke of the T
the young is most likely due to the compliant chest wall due
mic contraction of the ventricles (arrhythmias) or, if complete
spread from the atria to the ventricles. Failure of the bundle to
The sinuatrial node is the spontaneous source of the cardiac
impulse. The atrioventricular node is responsible for picking
up the cardiac impulse from the atria. The atrioventricular
bundle is the only route by which the cardiac impulse can
conduct the normal impulses results in alteration in the rhyth-
bundle block occurs, complete dissociation between the atria
and ventricular rates of contraction. The common cause of
defective conduction through the bundle or its branches is
atherosclerosis of the coronary arteries, which results in a
diminished blood supply to the conducting system.
Commotio Cordis
This condition results in ventricular fibrillation and sudden
death and is caused by a blunt nonpenetrating blow to the
anterior chest wall over the heart. It occurs most commonly
in the young and adolescents and is often sports-related. The
sudden blow is frequently produced by a baseball, baseball
bat, lacrosse ball, or fist or elbow. The common incidence in
to the flexible ribs and costal cartilages and the thin undevel-
oped chest muscles. Apparently, timing of the blow relative
to the cardiac cycle is critical; ventricular fibrillation is most
wave of the electrical activity of the cardiac muscle.
C L I N I C A L N O T E S
septum to the atrioventricular node. The
Branches
and left ventricle and the atrioventricular septum.
right atrium and right ventricle and parts of the left atrium
lowing branches from the right coronary artery supply the
nary artery in the posterior interventricular groove. The fol
the atrioventricular groove to anastomose with the left coro
the inferior border of the heart it continues posteriorly along
almost vertically in the right atrioventricular groove, and at
pulmonary trunk and the right auricle (Fig. 3.34). It descends
sinus of the ascending aorta and runs forward between the
arises from the anterior aortic
right coronary artery
The
face of the heart, lying within subepicardial connective tissue.
arteries and their major branches are distributed over the sur
immediately above the aortic valve (Fig. 3.41). The coronary
left coronary arteries, which arise from the ascending aorta
The arterial supply of the heart is provided by the right and
valve of the inferior vena cava to the atrioventricular node.
node and descends through the crista terminalis and the
leaves the posterior part of the sinuatrial
nodal pathway
posterior inter-
The Arterial Supply of the Heart
-
-
-
1.
The
ventricle.
and the upper part of the anterior wall of the right
pulmonary conus (infundibulum of the right ventricle)
supplies the anterior surface of the
right conus artery
conduction.
ordinary atrial myocardial fibers that are responsible for the more rapid
some researchers, who claim that it is the packaging and arrangement of
*The occurrence of specialized internodal pathways has been dismissed by
Basic Anatomy
87
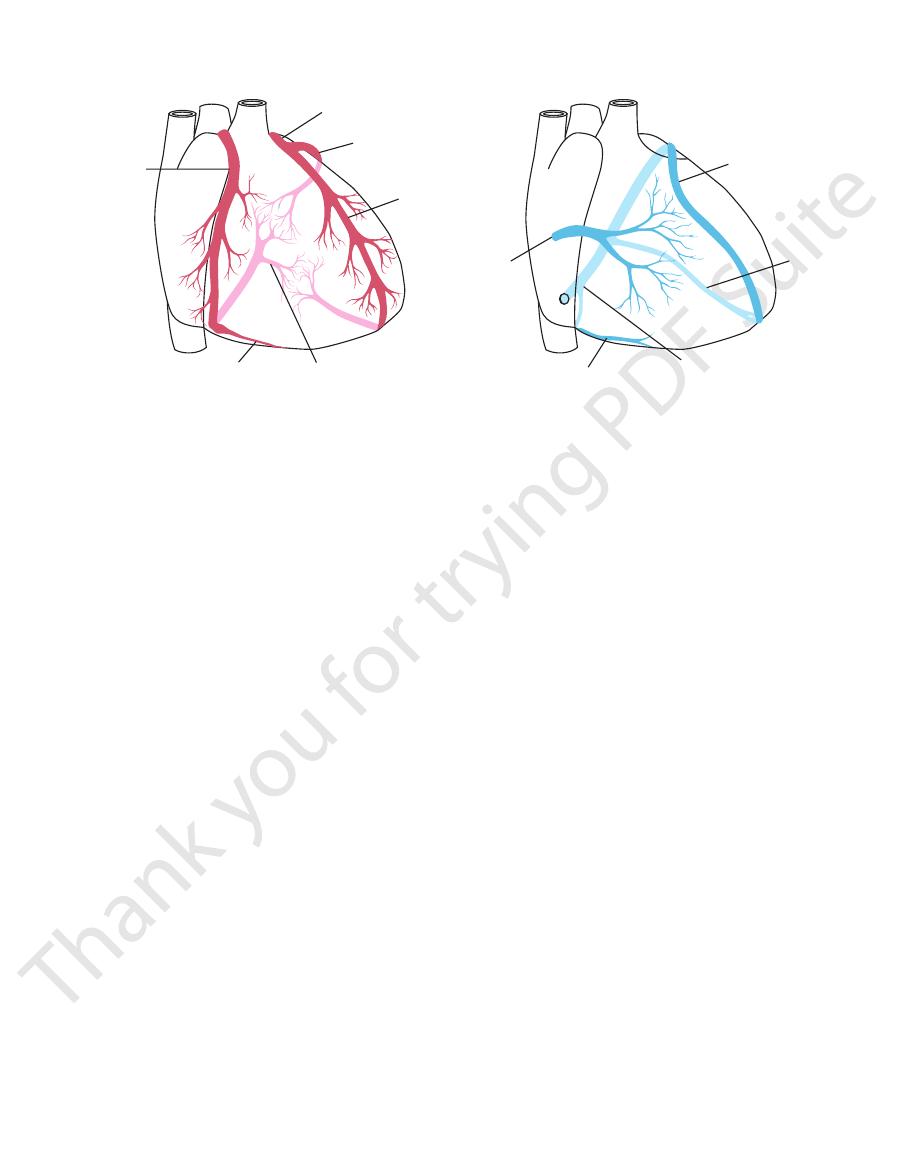
right
coronary
artery
left coronary artery
circumflex branch
anterior
interventricular
branch
posterior interventricular branch
marginal branch
great cardiac
vein
middle
cardiac
vein
coronary sinus
small cardiac vein
anterior
cardiac
vein
FIGURE 3.41
Coronary arteries and veins.
2.
The
the lower margin of the costal surface to reach the apex.
is the largest and runs along
marginal branch
tricle. The
number and supply the anterior surface of the right ven
are two or three in
anterior ventricular branches
-
3.
The
right ventricle.
number and supply the diaphragmatic surface of the
are usually two in
posterior ventricular branches
4.
The
is replaced by a branch from the left coronary artery.
In 10% of individuals, the posterior interventricular artery
atrioventricular node.
A large septal branch supplies the
rior interventricular branch of the left coronary artery.
the apical part, which receives its supply from the ante
the posterior part of the ventricular septum but not to
cles, including its inferior wall. It supplies branches to
groove. It gives off branches to the right and left ventri
runs toward the apex in the posterior interventricular
posterior interventricular (descending) artery
-
-
5.
The
Branches
rior interventricular branch and a circumflex branch.
enters the atrioventricular groove and divides into an ante
the pulmonary trunk and the left auricle (Fig. 3.34). It then
tic sinus of the ascending aorta and passes forward between
and ventricular septum. It arises from the left posterior aor
including the greater part of the left atrium, left ventricle,
right coronary artery, supplies the major part of the heart,
which is usually larger than the
left coronary artery,
The
coronary artery.
and left atria; in 35% of individuals it arises from the left
supplies the node and the right
of the sinuatrial node
artery
terior surface of both the right and left atria. The
faces of the right atrium. One branch supplies the pos
supply the anterior and lateral sur
atrial branches
-
-
-
-
1.
The
supplies the pulmonary conus.
left conus artery
A small
arise directly from the trunk of the left coronary artery.
may
(left diagonal artery)
of these ventricular branches
supply the anterior part of the ventricular septum. One
and left ventricles with numerous branches that also
The anterior interventricular branch supplies the right
one third of individuals, it ends at the apex of the heart.
the terminal branches of the right coronary artery. In
posterior interventricular groove and anastomoses with
it then passes around the apex of the heart to enter the
to the apex of the heart (Fig. 3.41). In most individuals,
runs downward in the anterior interventricular groove
anterior interventricular (descending) branch
2.
The
(except for the small area to the right of the anterior inter
supplies all of the right ventricle
right coronary artery
The
Heart in Most Individuals
Summary of the Overall Arterial Supply to the
sustain the muscle.
although sometimes the collateral circulation is enough to
ally leads to myocardial death (myocardial infarction),
one of the larger branches of either coronary artery usu
branches become blocked by disease. A sudden block of
blood supply to the cardiac muscle should one of the large
to provide an adequate
not large enough
they are usually
and left coronary arteries (collateral circulation) exist, but
Anastomoses between the terminal branches of the right
Coronary Artery Anastomoses
left coronary artery (10%).
tricular artery is a branch of the circumflex branch of the
the posterior interven
left dominance,
viduals (90%). In
coronary artery. Right dominance is present in most indi
terior interventricular artery is a large branch of the right
the pos
right dominance,
artery are variable (Fig. 3.42). In
gin, size, and distribution of the posterior interventricular
the diaphragmatic surface of both ventricles. Here the ori
the most common variations affect the blood supply to
Variations in the blood supply to the heart do occur, and
Variations in the Coronary Arteries
supply the left atrium.
Atrial branches
the left ventricle.
supply
posterior ventricular branches
and
ventricular
Anterior
margin of the left ventricle down to the apex.
is a large branch that supplies the left
marginal artery
left
margin of the heart in the atrioventricular groove. A
terventricular artery (Fig. 3.41). It winds around the left
is the same size as the anteriorin
circumflex artery
-
-
-
-
-
-
-
ventricular groove), the variable part of the diaphragmatic
88
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
circumflex
branch of
left coronary
artery
branches of posterior
interventricular artery
sinuatrial
node
right coronary artery
anterior
interventricular
artery
atrioventricular bundle
atrioventricular node
left coronary artery
branches of posterior
interventricular artery
right
coronary
artery
circumflex branch
of left coronary
artery
right
coronary
artery
A
B
C
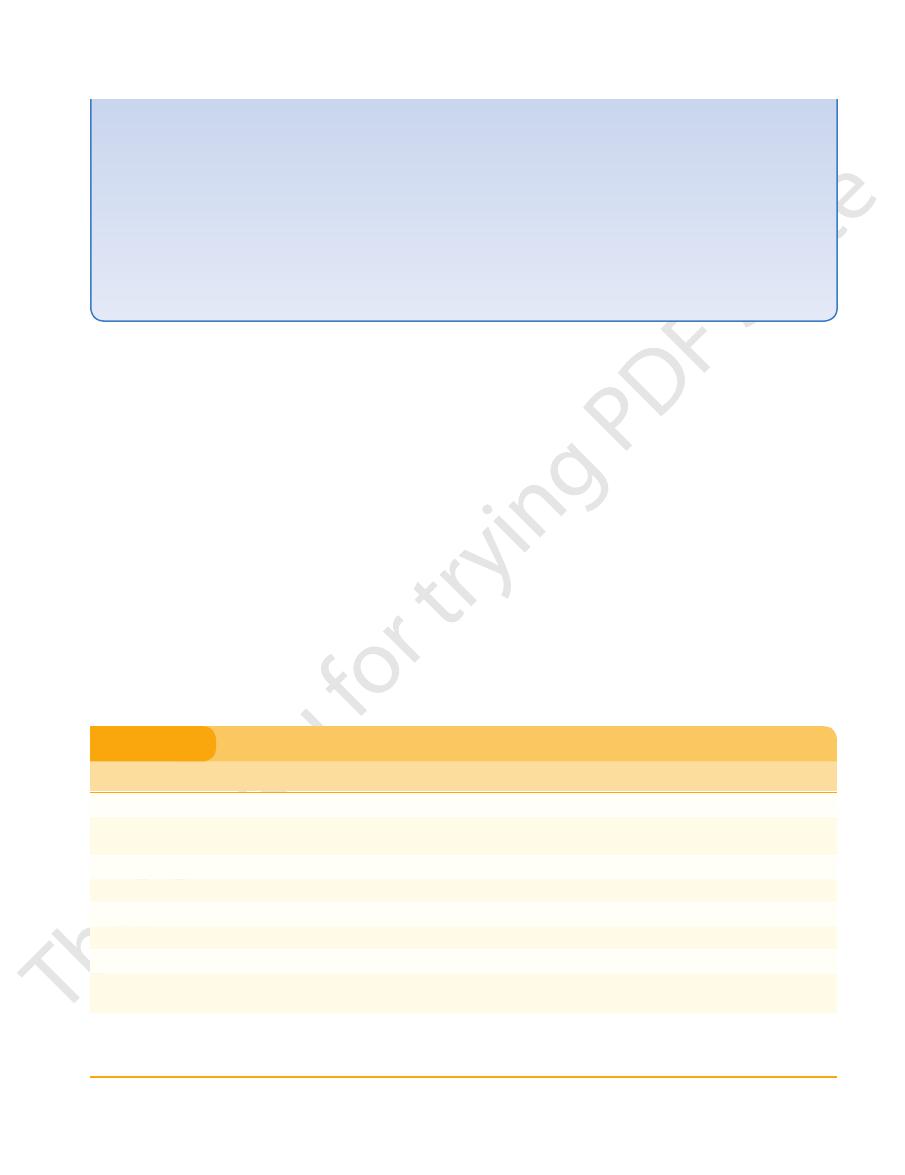
FIGURE 3.42
(Fig. 3.42).
LBB is supplied by the right and left coronary arteries
ular bundle is supplied by the left coronary artery; the
the right coronary artery. The RBB of the atrioventric
lar node and the atrioventricular bundle are supplied by
sometimes by the left coronary artery. The atrioventricu
The sinuatrial node is usually supplied by the right but
Arterial Supply to the Conducting System
LBB.
tricular septum, most of the left atrium, the RBB, and the
interventricular groove, the anterior two thirds of the ven
tricle, a small area of the right ventricle to the right of the
supplies most of the left ven
left coronary artery
The
node and bundle. The LBB also receives small branches.
atrium, and the sinuatrial node and the atrioventricular
ventricular septum, the right atrium and part of the left
surface of the left ventricle, the posteroinferior third of the
Anterior view of the heart showing the relationship of the blood supply to the conducting system.
the left dominance.
Posterior view of the heart showing the origin and distribution of the posterior interventricular artery in
Posterior view of the heart showing the origin and distribution of the posterior interventricular artery in the
A.
right dominance. B.
C.
-
-
-
-
Coronary Artery Disease
blockage are caused by an acute thrombosis on top of a chronic
The myocardium receives its blood supply through the right
and left coronary arteries. Although the coronary arteries have
numerous anastomoses at the arteriolar level, they are essen-
tially functional end arteries. A sudden block of one of the large
branches of either coronary artery will usually lead to necrosis
of the cardiac muscle (myocardial infarction) in that vascular
area, and often the patient dies. Most cases of coronary artery
atherosclerotic narrowing of the lumen.
C L I N I C A L N O T E S
(continued)
Basic Anatomy
89
Arteriosclerotic disease of the coronary arteries may pres
that have been carried out before treatment. For this reason, a
coronary artery stenting are now commonly accepted methods
Because coronary bypass surgery, coronary angioplasty, and
infarction, the artery involved, and the electrocardiographic
be helpful when attempting to correlate the site of myocardial
the different areas of the myocardium. This information can
Table 3.1 shows the different coronary arteries that supply
occurs when coronary flow is suddenly
Myocardial infarction
that myocardial ischemia occurs on exertion but not at rest. (3)
rest. In this condition, the coronary arteries are so narrowed
is cardiac pain that occurs on exertion and is relieved by
the myocardium occur over many years and are caused by a
lumina of the arteries: (1) General degeneration and fibrosis of
ent in three ways, depending on the rate of narrowing of the
-
gradual narrowing of the coronary arteries. (2) Angina pecto-
ris
reduced or stopped and the cardiac muscle undergoes necro-
sis. Myocardial infarction is the major cause of death in indus-
trialized nations.
signature.
of treating coronary artery disease, it is incumbent on the student
to be prepared to interpret still- and motion-picture angiograms
working knowledge of the origin, course, and distribution of the
coronary arteries should be memorized.
Coronary Artery
Infarct Location
ECG Signature
Proximal LAD
Large anterior wall
ST elevation: I, L, V1–V6
More distal LAD
Anteroapical
Inferior wall if wraparound LAD
ST elevation: V2–V4
ST elevation: II, III, F
Distal LAD
Anteroseptal
ST elevation: V1–V3
Early obtuse, marginal
High lateral wall
ST elevation: I, L, V4–V6
More distal marginal branch, circumflex
Small lateral wall
ST elevation: I, L, or V4–V6, or no abnormality
ECG, electrocardiographic; LAD, left anterior descending (interventricular); RCA, right coronary artery.
Circumflex
Posterolateral
ST elevation: V4–V6; ST depression: V1–V2
Distal RCA
Small inferior wall
ST elevation: II, III, F; ST depression: I, L
Proximal RCA
Large inferior wall and posterior wall
Some lateral wall
ST elevation: II, III, F; ST depression: I, L, V1–V3
ST elevation: V5–V6
RCA
Right ventricular
Usually inferior
ST elevation: V2R–V4R; some ST elevation: V1;
or ST depression V2, V3
ST elevation: II, III, F
Coronary Artery Lesions, Infarct Location, and ECG Signature
T A B L E 3 . 1
reflexes.
ning with the vagus nerves take part in cardiovascular
consciousness via this pathway. Afferent fibers run
myocardium become impaired, pain impulses reach
sciousness. However, should the blood supply to the
carry nervous impulses that normally do not reach con
Afferent fibers running with the sympathetic nerves
arteries.
traction of the heart and a constriction of the coronary
nerves results in a reduction in the rate and force of con
coronary arteries. Activation of the parasympathetic
on the sinuatrial and atrioventricular nodes and on the
The postganglionic parasympathetic fibers terminate
coronary arteries.
contraction of the cardiac muscle, and dilatation of the
nerves results in cardiac acceleration, increased force of
fibers, and on the coronary arteries. Activation of these
sinuatrial and atrioventricular nodes, on cardiac muscle
The postganglionic sympathetic fibers terminate on the
pathetic supply comes from the vagus nerves.
racic portions of the sympathetic trunks, and the parasym
sympathetic supply arises from the cervical and upper tho
situated below the arch of the aorta. The
thetic fibers of the autonomic nervous system via the
The heart is innervated by sympathetic and parasympa
that open directly into the heart chambers.
(Fig. 3.41) and by small veins
anterior cardiac vein
by the
The remainder of the blood is returned to the right atrium
are tributaries of the coronary sinus.
middle cardiac veins
small
atrium to the left of the inferior vena cava. The
It opens into the right
great cardiac vein.
tinuation of the
posterior part of the atrioventricular groove and is a con
through the coronary sinus (Fig. 3.41), which lies in the
Most blood from the heart wall drains into the right atrium
Venous Drainage of the Heart
-
and
Nerve Supply of the Heart
-
car-
diac plexuses
-
-
-
-
-
90
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
Cardiac Pain
matic surface of the heart often gives rise to discomfort in the
costobrachial nerve communicates with the medial cutaneous
areas supplied by the upper four intercostal nerves and by the
Pain originating in the heart as the result of acute myocardial
ischemia is assumed to be caused by oxygen deficiency and the
accumulation of metabolites, which stimulate the sensory nerve
endings in the myocardium. The afferent nerve fibers ascend to
the central nervous system through the cardiac branches of the
sympathetic trunk and enter the spinal cord through the poste-
rior roots of the upper four thoracic nerves. The nature of the
pain varies considerably, from a severe crushing pain to nothing
more than a mild discomfort.
The pain is not felt in the heart, but is referred to the skin
areas supplied by the corresponding spinal nerves. The skin
intercostobrachial nerve (T2) are therefore affected. The inter-
nerve of the arm and is distributed to skin on the medial side of
the upper part of the arm. A certain amount of spread of nervous
information must occur within the central nervous system, for
the pain is sometimes felt in the neck and the jaw.
Myocardial infarction involving the inferior wall or diaphrag-
epigastrium. One must assume that the afferent pain fibers from
the heart ascend in the sympathetic nerves and enter the spinal
cord in the posterior roots of the seventh, eighth, and ninth tho-
racic spinal nerves and give rise to referred pain in the T7, T8,
and T9 thoracic dermatomes in the epigastrium.
Because the heart and the thoracic part of the esophagus
probably have similar afferent pain pathways, it is not surprising
that painful acute esophagitis can mimic the pain of myocardial
infarction.
C L I N I C A L N O T E S
Action of the Heart
opposite the 3rd intercostal space.
lies behind the left half of the sternum
aortic valve
The
sternum.
third left costal cartilage and the adjoining part of the
lies behind the medial end of the
pulmonary valve
The
opposite the 4th costal cartilage.
lies behind the left half of the sternum
mitral valve
The
num opposite the 4th intercostal space.
lies behind the right half of the ster
tricuspid valve
The
(Fig. 3.14):
56. The surface markings of the heart valves are as follows
The surface projection of the heart was described on page
Surface Anatomy of the Heart Valves
aortic and pulmonary orifices.
The cusps float into apposition and completely close the
and immediately fills the pockets of the semilunar valves.
systole, blood begins to move back toward the ventricles
is ejected from the heart. At the conclusion of ventricular
the semilunar valve cusps are pushed aside, and the blood
present in the large arteries (aorta and pulmonary trunk),
Once the intraventricular blood pressure exceeds that
the same time throughout the ventricles.
fibers, ensures that myocardial contraction occurs at almost
(Fig. 3.38) and its terminal branches, including the Purkinje
of the cardiac impulse along the atrioventricular bundle
tracting and the atrioventricular valves close. The spread
chordae tendineae. Meanwhile, the ventricles start con
muscles then begin to contract and take up the slack of the
tricular bundle and its branches (Fig. 3.38). The papillary
node, is conducted to the papillary muscles by the atrioven
The cardiac impulse, having reached the atrioventricular
this means, blood does not reflux into the veins.
large veins and milks the blood toward the ventricles. By
in the atria, which commences around the openings of the
tricles. The sinuatrial node initiates the wave of contraction
forces the remainder of the blood in the atria into the ven
When the ventricles are nearly full, atrial systole occurs and
passively flows from the atria to the ventricles (Fig. 3.38).
ation) occurs, the atrioventricular valves open, and blood
in the large veins and atria. Once ventricular diastole (relax
valves are closed, the blood is temporarily accommodated
ventricular systole (contraction), when the atrioventricular
Blood is continuously returning to the heart; during
150 times per minute in the newborn child.
70 to 90 times per minute in the resting adult and 130 to
The normal heart beats
cardiac cycle.
referred to as the
take place within it as it fills with blood and empties is
The heart is a muscular pump. The series of changes that
-
-
-
-
■
■
-
■
■
■
■
■
■
Auscultation of the Heart Valves
produced at each valve with the minimum of distraction or
the chest wall so that he or she will be able to hear sounds
for a physician to know where to place the stethoscope on
closure of the aortic and pulmonary valves. It is important
and mitral valves. The second sound is produced by the sharp
contraction of the ventricles and the closure of the tricuspid
The first sound is produced by the
lu¯b-du˘p.
two sounds:
On listening to the heart with a stethoscope, one can hear
interference.
C L I N I C A L N O T E S
(continued)
