Basic Anatomy
ent motor nerve fibers travel in the genital branch of
of the genitofemoral nerve (L1 and 2), and the effer
ent fibers of this reflex arc travel in the femoral branch
The affer
cremasteric reflex.
the thigh. This is called the
to contract by stroking the skin on the medial aspect of
nerve (see page 222). The cremaster muscle can be made
is supplied by the genital branch of the genitofemoral
from the fascia transversalis. The cremaster muscle
cle; and, finally, the internal spermatic fascia is derived
masteric fascia is derived from the internal oblique mus
the aponeurosis of the external oblique muscle; the cre
explained. The external spermatic fascia is derived from
anterior abdominal wall on each side, as previously
ficial fascia and are derived from the three layers of the
These three layers lie beneath the super
Spermatic fasciae.
and separates the testes from each other.
tribute to a median partition that crosses the scrotum
ischiopubic rami. Both layers of superficial fascia con
membrane (see Fig. 4.1). At the sides, it is attached to the
perineal body and the posterior edge of the perineal
wall (Scarpa’s fascia), and behind it is attached to the
with the membranous layer of the anterior abdominal
(often referred to as Colles’ fascia) is continuous in front
ing skin. The membranous layer of the superficial fascia
fibers and is responsible for the wrinkling of the overly
This is innervated by sympathetic nerve
dartos muscle.
fat is, however, replaced by smooth muscle called the
membranous layers of the anterior abdominal wall; the
This is continuous with the fatty and
Superficial fascia.
remain separate and form the labia majora.)
eral labioscrotal swellings. (In the female, the swellings
in the midline indicates the line of fusion of the two lat
mented and forms a single pouch. A slightly raised ridge
The skin of the scrotum is thin, wrinkled, and pig
Skin.
The wall of the scrotum has the following layers:
mides, and the lower ends of the spermatic cords (see Figs.
anterior abdominal wall. It contains the testes, the epididy
The scrotum is an outpouching of the lower part of the
Scrotum
Scrotum, Testis, and Epididymides
the uterus to the superficial inguinal nodes.
vessels convey a small amount of lymph from the body of
ligament of the uterus and a few lymph vessels. The lymph
inguinal canal from the abdominal cavity are the round
131
-
4.4 and 4.21).
-
-
-
-
-
-
-
-
-
the genitofemoral nerve. The function of the cremaster
cremaster muscles. It is now recognized that the testicular
be changed reflexly by the contraction of the dartos and
fully understood, but the surface area of the scrotal skin can
The control of testicular temperature in the scrotum is not
perature about 3°C lower than the abdominal temperature.
When they are located in the scrotum, they are at a tem
at a temperature lower than that of the abdominal cavity.
Normal spermatogenesis can occur only if the testes are
Fig. 4.21).
nect the rete testis to the upper end of the epididymis (see
con
efferent ductules
Small
rete testis.
channels called the
The tubules open into a network of
seminiferous tubules.
Lying within each lobule are one to three coiled
lobules.
of fibrous septa that divide the interior of the organ into
Extending from the inner surface of the capsule is a series
tunica albuginea.
fibrous capsule, the
level than the right. Each testis is surrounded by a tough
(see Figs. 4.5 and 4.21). The left testis usually lies at a lower
is a firm, mobile organ lying within the scrotum
testis
The
Testis
drains into the superficial inguinal lymph nodes (see Fig. 4.22).
Lymph from the skin and fascia, including the tunica vaginalis,
Lymph Drainage of the Scrotum
testis.
nalis is thus a closed sac, invaginated from behind by the
the processus and the peritoneal cavity. The tunica vagi
before birth, it becomes shut off from the upper part of
expanded part of the processus vaginalis; normally, just
medial, and lateral surfaces of each testis. It is the lower
within the spermatic fasciae and covers the anterior,
(see Figs. 4.4, 4.5, and 4.21). This lies
Tunica vaginalis
temperature and fertility, see below.
warmth and for protection against injury. For testicular
muscle is to raise the testis and the scrotum upward for
-
-
-
veins in the spermatic cord that form the pampiniform
plexus—together with the branches of the testicular
arteries, which lie close to the veins—probably assist in sta
stances to the seminal fluid to nourish the maturing sperm.
tion of fluid. Another function may be the addition of sub
mature. A main function of the epididymis is the absorp
storage space for the spermatozoa and allows them to
The long length of the duct of the epididymis provides
enters the spermatic cord.
which
vas deferens,
from the tail of the epididymis as the
long, embedded in connective tissue. The tube emerges
The epididymis is a much coiled tube nearly 20 ft (6 m)
(see Fig. 4.21).
sinus of the epididymis
the inner visceral layer of the tunica vaginalis and is called
between the testis and the epididymis, which is lined with
inferiorly. Laterally, a distinct groove lies
and a pointed
body,
head,
Fig. 4.21). It has an expanded upper end, the
testis, with the vas deferens lying on its medial side (see
is a firm structure lying posterior to the
epididymis
The
blood ascending to the abdomen within the veins.
arriving in the artery from the abdomen loses heat to the
heat exchange mechanism. By this means, the hot blood
bilizing the temperature of the testes by a countercurrent
-
Epididymis
a
tail
the
-
-
Vasectomy
postoperative ejaculations, but that is simply an emptying process.
between ligatures. Spermatozoa may be present in the first few
upper part of the scrotal wall, and the vas deferens is divided
infertility. Under local anesthesia, a small incision is made in the
Bilateral vasectomy is a simple operation performed to produce
Now only the secretions of the seminal vesicles and prostate con-
stitute the seminal fluid, which can be ejaculated as before.
C L I N I C A L N O T E S
132
CHAPTeR 4
aorta (lumbar or para-aortic) nodes at the level of the 1st
matic cord and end in the lymph nodes on the side of the
The lymph vessels (see Fig. 4.22) ascend in the sper
Lymph Drainage of the Testis and Epididymis
cava, and the left vein joins the left renal vein.
canal. The right testicular vein drains into the inferior vena
reduced to a single vein as it ascends through the inguinal
This becomes
pampiniform plexus.
a venous network, the
testicular veins emerge from the testis and the epididymis as
The testicular artery is a branch of the abdominal aorta. The
Blood Supply of the Testis and Epididymis
The Abdomen: Part I—The Abdominal Wall
-
lumbar vertebra (i.e., on the transpyloric plane). This is
migrated from high up on the posterior abdominal wall,
to be expected because during development the testis has
Clinical Conditions Involving the Scrotum and Testis
should therefore always lead one to examine the left kidney.
exit of the testicular vein. A rapidly developing left-sided variocele
ease of the left kidney extends along the renal vein and blocks the
vein, in which the venous pressure is higher. Rarely, malignant dis
sure inferior vena cava, whereas the left vein joins the left renal
cents and young adults, with most occurring on the left side. This is
A varicocele is a condition in which the veins of the pampiniform
Varicocele
plexus are elongated and dilated. It is a common disorder in adoles-
thought to be because the right testicular vein joins the low-pres-
-
Malignant Tumor of the Testis
A malignant tumor of the testis spreads upward via the lymph
vessels to the lumbar (para-aortic) lymph nodes at the level of
the first lumbar vertebra. It is only later, when the tumor spreads
locally to involve the tissues and skin of the scrotum, that the
superficial inguinal lymph nodes are involved.
The process of the descent of the testis is shown in
Figure 4.23. The testis may be subject to the following congenital
anomalies.
the lower part of the anterior abdominal wall with the formation
The formation of the processus vaginalis and its passage through
Torsion of the testis is a rotation of the testis around the sper
Torsion of the Testis
-
matic cord within the scrotum. It is often associated with an
excessively large tunica vaginalis. Torsion commonly occurs in
active young men and children and is accompanied by severe
pain. If not treated quickly, the testicular artery may be occluded,
followed by necrosis of the testis.
Processus Vaginalis
of the inguinal canal in both sexes were described elsewhere
(see page 130). Normally, the upper part becomes obliterated just
before birth and the lower part remains as the tunica vaginalis.
The processus is subject to the following common congenital
anomalies:
1. It may persist partially or in its entirety as a preformed hernial
sac for an indirect inguinal hernia (Fig. 4.24).
2.
It may become very much narrowed, but its lumen remains
in communication with the abdominal cavity. Peritoneal fluid
accumulates in it, forming a congenital hydrocele (Fig. 4.24).
3.
The upper and lower ends of the processus may become
spermatic fascia, cremasteric fascia, internal spermatic fascia,
The tunica vaginalis is closely related to the front and sides
obliterated, leaving a small intermediate cystic area referred
to as an encysted hydrocele of the cord (see Fig. 4.24).
of the testis. It is therefore not surprising to find that inflam-
mation of the testis can cause an accumulation of fluid within
the tunica vaginalis. This is referred to simply as a hydrocele
(Fig. 4.25). Most hydroceles are idiopathic.
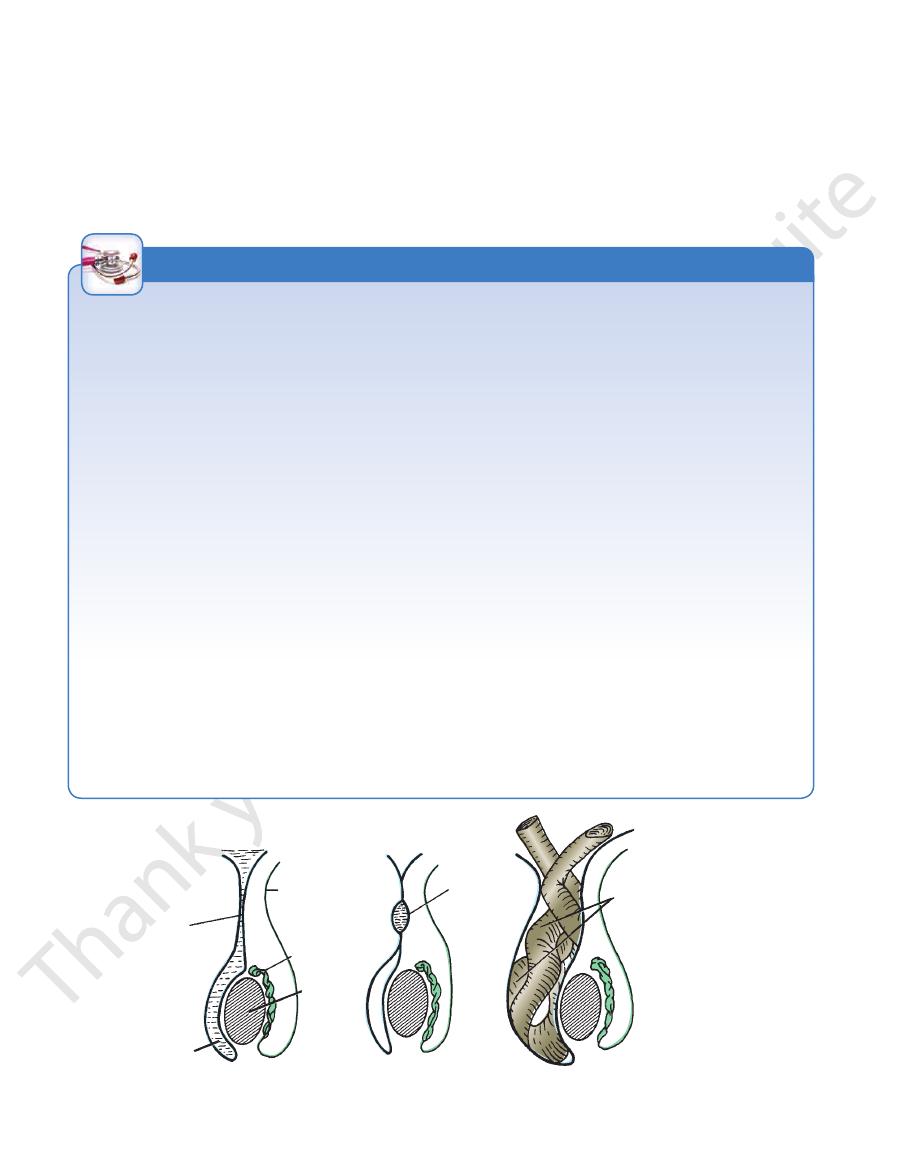
To remove excess fluid from the tunica vaginalis, a proce-
dure termed tapping a hydrocele, a fine trocar and cannula are
inserted through the scrotal skin (see Fig. 4.25). The following
anatomic structures are traversed by the cannula: skin, dartos
muscle and membranous layer of fascia (Colles’ fascia), external
and parietal layer of the tunica vaginalis.
C L I N I C A L N O T E S
peritoneal cavity
vas deferens
epididymis
testis
cyst
peritoneal fluid
persistent
processus
vaginalis
A
B
C
coils of small intestine inside
persistent processus vaginalis,
which forms hernial sac
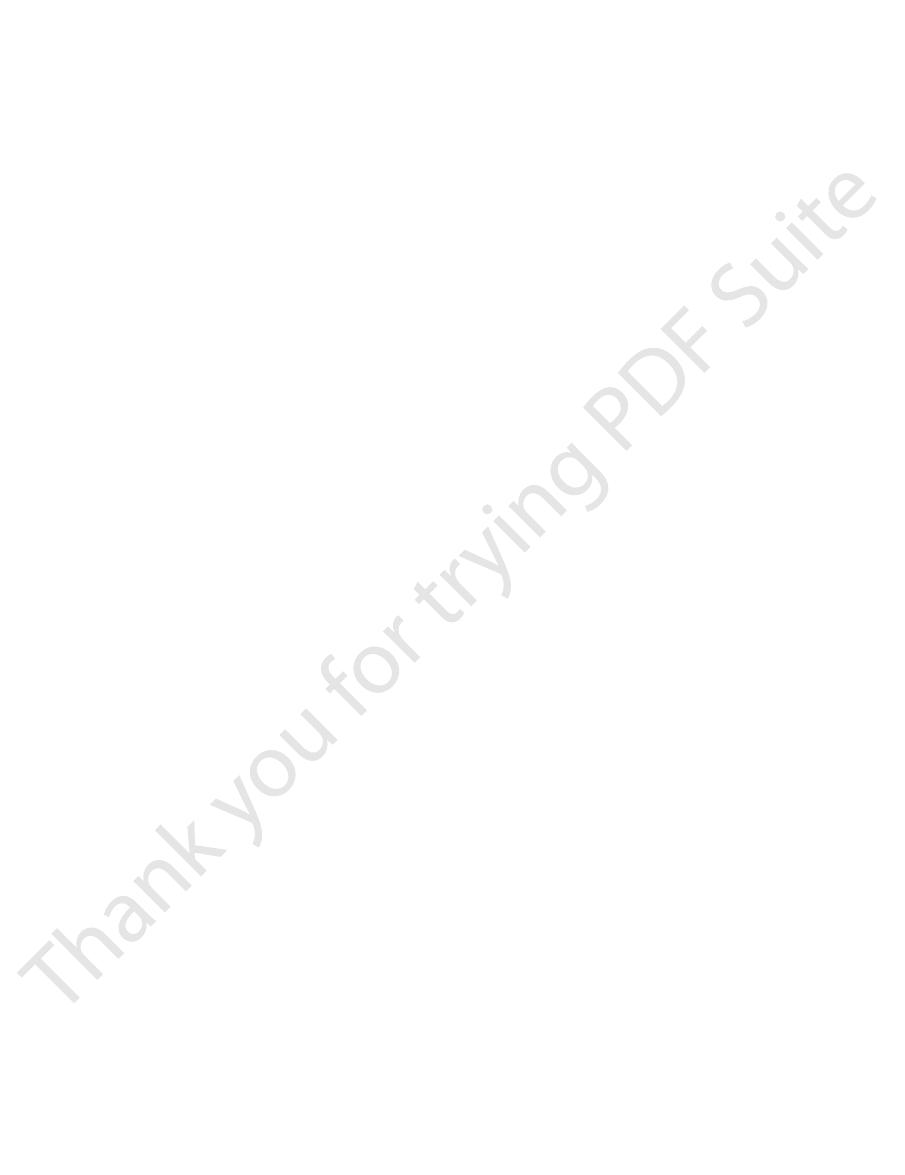
FIGURE 4.24
Common congenital anomalies of the processus vaginalis.
Preformed hernial sac for indirect inguinal hernia.
Encysted hydrocele of
Congenital hydrocele.
A.
B.
the cord. C.
Basic Anatomy
133
acquired
hydrocele
scrotal skin
dartos muscle
membranous layer of
superficial fascia
external spermatic fascia
cremasteric fascia
internal spermatic fascia
tunica vaginalis
testis
hydrocele fluid
FIGURE 4.25
The tunica vaginalis distended with fluid (hydrocele). Also shown are the various anatomic layers traversed by a
trocar and a cannula when a hydrocele is tapped.
Development of the Testis
developing normally, is susceptible to traumatic injury and, for
and function normally. A maldescended testis, although often
down into the scrotum by surgery before puberty, it will develop
because the temperature there retards the normal process of
mal path and fails to reach the scrotum. It may be found in the
found within the abdomen, within the inguinal canal, at the
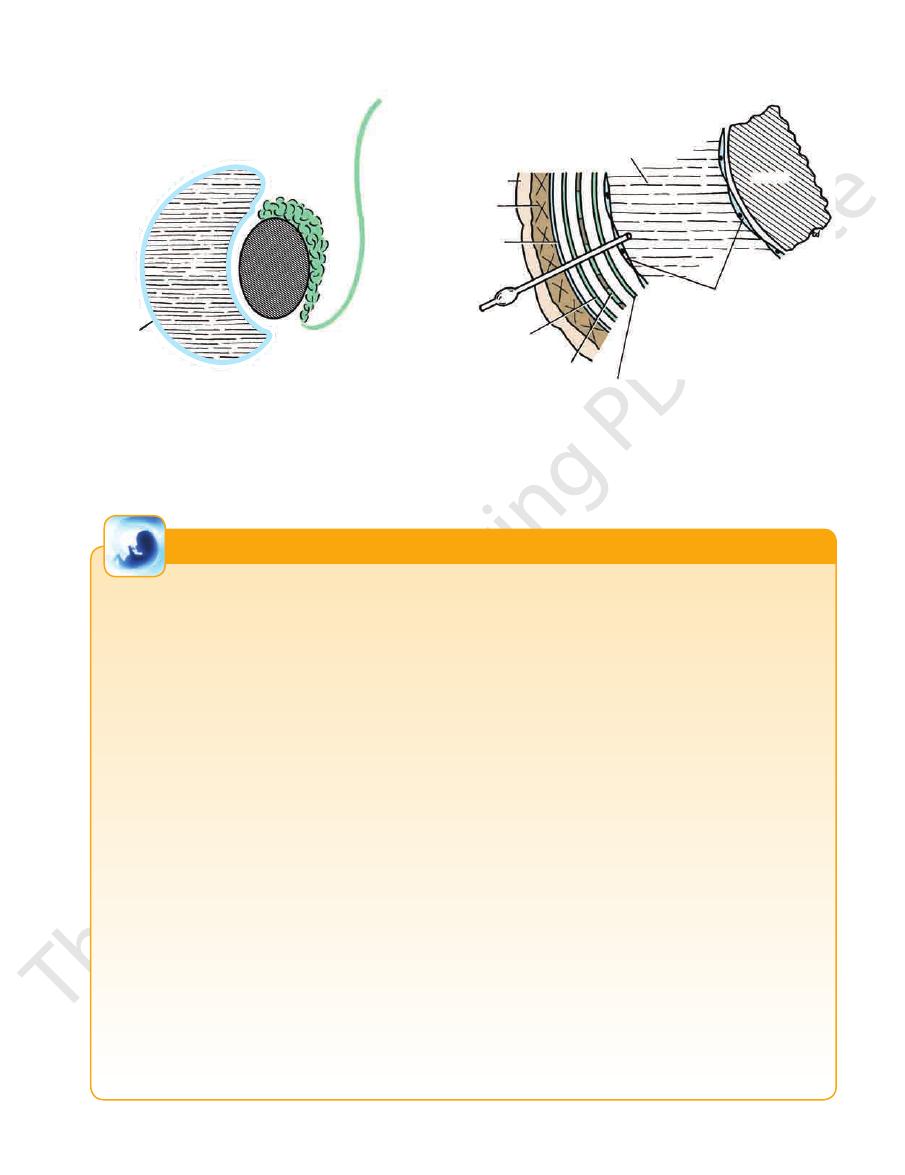
The sex cords become
tunica albuginea.
dense fibrous layer, the
The male sex chromosome causes the genital ridge to secrete
testosterone and induces the development of the testis and the
other internal and external organs of reproduction.
The sex cords of the genital ridge become separated from the
coelomic epithelium by the proliferation of the mesenchyme (Fig.
4.26). The outer part of the mesenchyme condenses to form a
U-shaped and form the seminiferous tubules. The free ends of
the tubules form the straight tubules, which join one another in
the mediastinum testis to become the rete testis. The primordial
sex cells in the seminiferous tubules form the spermatogonia,
and the sex cord cells form the Sertoli cells. The mesenchyme
in the developing gonad makes up the connective tissue and
fibrous septa. The interstitial cells, which are already secret-
ing testosterone, are also formed of mesenchyme. The rete testis
becomes canalized, and the tubules extend into the mesonephric
tissue, where they join the remnants of the mesonephric tubules;
the latter tubules become the efferent ductules of the testis. The
duct of the epididymis, the vas deferens, the seminal vesicle,
and the ejaculatory duct are formed from the mesonephric duct
(see Fig. 4.26).
Descent of the Testis
The testis develops high up on the posterior abdominal wall, and
in late fetal life it “descends” behind the peritoneum, dragging its
blood supply, nerve supply, and lymphatic drainage after it (for
details, see page 130). The process of the descent of the testis is
shown in Figure 4.23.
Congenital Anomalies of the Testis
The testis may be subject to the following congenital anomalies.
■
■
Anterior inversion, in which the epididymis lies anteriorly and
the testis and the tunica vaginalis lie posteriorly
■
■
Polar inversion, in which the testis and epididymis are com-
pletely inverted
■
■
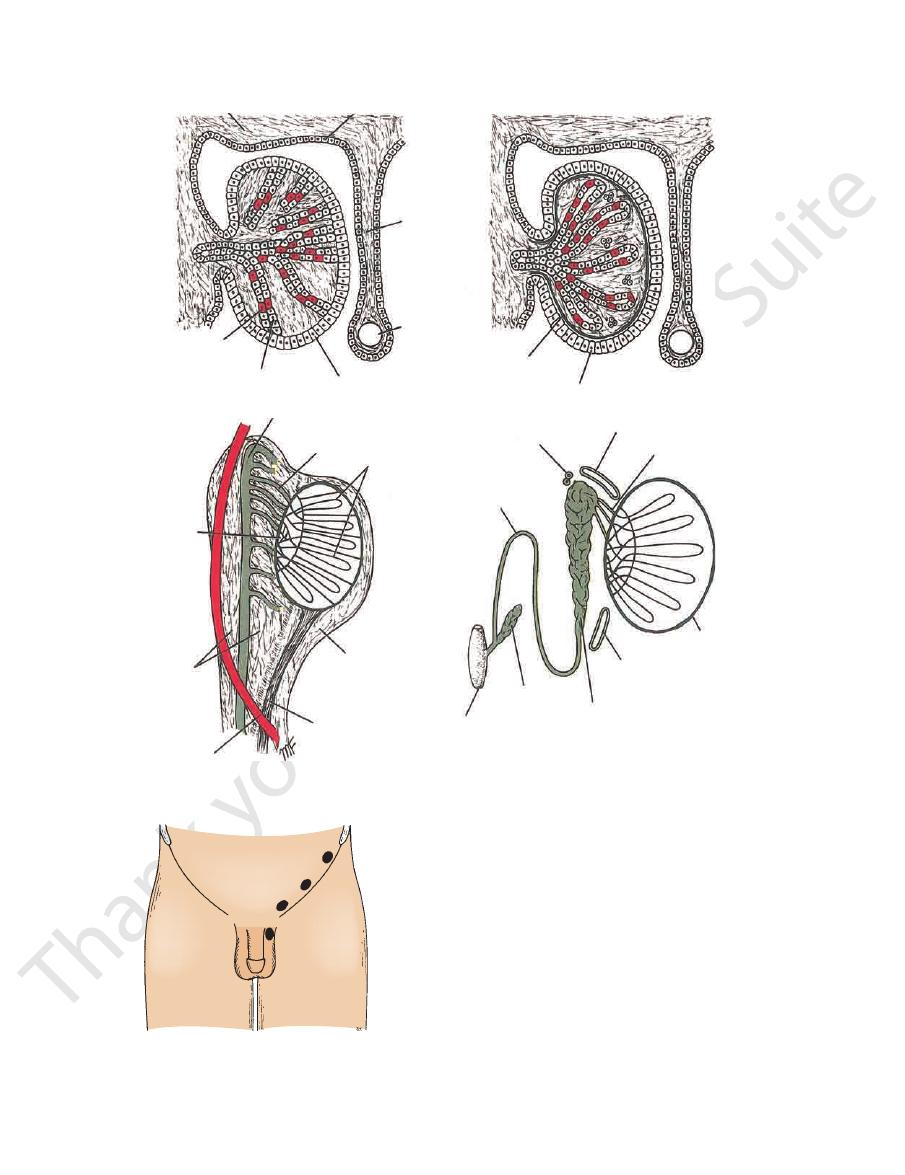
Imperfect descent (cryptorchidism): Incomplete descent
(Fig. 4.27), in which the testis, although traveling down its
normal path, fails to reach the floor of the scrotum. It may be
superficial inguinal ring, or high up in the scrotum.
■
■
Maldescent (Fig. 4.28), in which the testis travels down an abnor-
superficial fascia of the anterior abdominal wall above the ingui-
nal ligament, in front of the pubis, in the perineum, or in the thigh.
It is necessary for the testes to leave the abdominal cavity
spermatogenesis. If an incompletely descended testis is brought
this reason, should be placed in the scrotum. Many authorities
believe that the incidence of tumor formation is greater in testes
that have not descended into the scrotum.
The appendix of the testis and the appendix of the epididy-
mis are embryologic remnants found at the upper poles of these
organs that may become cystic. The appendix of the testis is
derived from the paramesonephric ducts, and the appendix of
the epididymis is a remnant of the mesonephric tubules.
E M B R Y O L O G I C N O T E S
134
CHAPTeR 4
The Abdomen: Part I—The Abdominal Wall
posterior abdominal wall
coelomic epithelium
dorsal
mesentery
gut
primordial sex cells
sex cords
genital ridge
tunica albuginea
coelomic epithelium
mesonephric duct
mesonephric tubule
U-shaped sex cords
rete testis
mesonephros
paramesonephric duct
genital ridge
gubernaculum
appendix of epididymis
superior aberrant ductules
efferent ductules
tunica albuginea
vas deferens
inferior aberrant ductules
canal of epididymis
seminal
vesicle
prostatic
urethra
A
B
C
D
FIGURE 4.26
The formation of the testis and the ducts of the testis.
1
2
3
4
FIGURE 4.27
Four degrees of incomplete descent of the
the five lumbar vertebrae and their intervertebral discs and
The posterior abdominal wall is formed in the midline by
Structure of the Posterior Abdominal Wall
ligaments of the uterus. (For further details, see page 288.)
of adipose tissue and the terminal strands of the round
to form the scrotum.) Within the labia are a large amount
fetus. (In the male, the genital swellings fuse in the midline
formed by the enlargement of the genital swellings in the
The labia majora are prominent, hair-bearing folds of skin
dragging its blood supply and lymph vessels after it.
down through the inguinal canal, and into the scrotum,
In the upper part of scrotum.
ring.
At the superficial inguinal
ring.
In the abdominal cavity close to the deep inguinal
testis. 1.
2. In the inguinal canal. 3.
4.
Labia Majora
laterally by the 12th ribs, the upper part of the bony pelvis
(Fig. 4.29), the psoas muscles, the quadratus lumborum
