
222
CHAPTER 5
together.
tally arranged ganglia, the 1st and 2nd often being fused
The sympathetic trunk possesses four or five segmen
the left border of the aorta.
lies close to
left sympathetic trunk
inferior vena cava; the
lies behind the right border of the
right sympathetic trunk
vis below by passing behind the common iliac vessels. The
the medial arcuate ligament and gains entrance to the pel
vertebrae (Fig. 5.78). It enters the abdomen from behind
border of the psoas muscle on the bodies of the lumbar
the sympathetic trunk. It runs downward along the medial
above with the thoracic and below with the pelvic parts of
The abdominal part of the sympathetic trunk is continuous
Sympathetic Trunk (Abdominal Part)
tion are summarized in Table 5.1.
The branches of the lumbar plexus and their distribu
within the scrotum.
cremaster muscle and the drawing upward of the testis
of the thigh in the male results in reflex contraction of the
in which stimulation of the skin
cremasteric reflex,
the thigh (see page 450). It is the nervous pathway involved
which supplies a small area of the skin of
femoral branch,
the spermatic cord and supplies the cremaster muscle, and
which enters
genital branch,
the muscle and divides into a
anterior surface of the psoas. It runs downward in front of
(L1 and 2) emerges on the
genitofemoral nerve
The
sacrum and joins the 1st sacral nerve.
plexus (see page 255). It descends anterior to the ala of the
takes part in the formation of the sacral
lumbosacral trunk
4th lumbar root of the
and in the thigh see page 465.) The
(For a description of its course in the pelvis see page 455
by passing through the obturator foramen into the thigh.
and behind the common iliac vessels. It leaves the pelvis
and 4) crosses the pelvic brim in front of the sacroiliac joint
(L2, 3,
obturator nerve
psoas at the brim of the pelvis. The
lumbosacral trunk emerge from the medial border of the
The obturator nerve and the 4th lumbar root of the
men, it supplies the iliacus muscle.
to the femoral vessels and the femoral sheath. In the abdo
enters the thigh behind the inguinal ligament and lateral
and laterally between the psoas and the iliacus muscles and
the largest branch of the lumbar plexus. It runs downward
(L2, 3, and 4) is
femoral nerve
surface of the thigh. The
ment (see page 450). It supplies the skin over the lateral
enters the thigh behind the lateral end of the inguinal liga
crosses the iliac fossa in front of the iliacus muscle and
The Abdomen: Part II—The Abdominal Cavity
-
-
a
in the
-
-
-
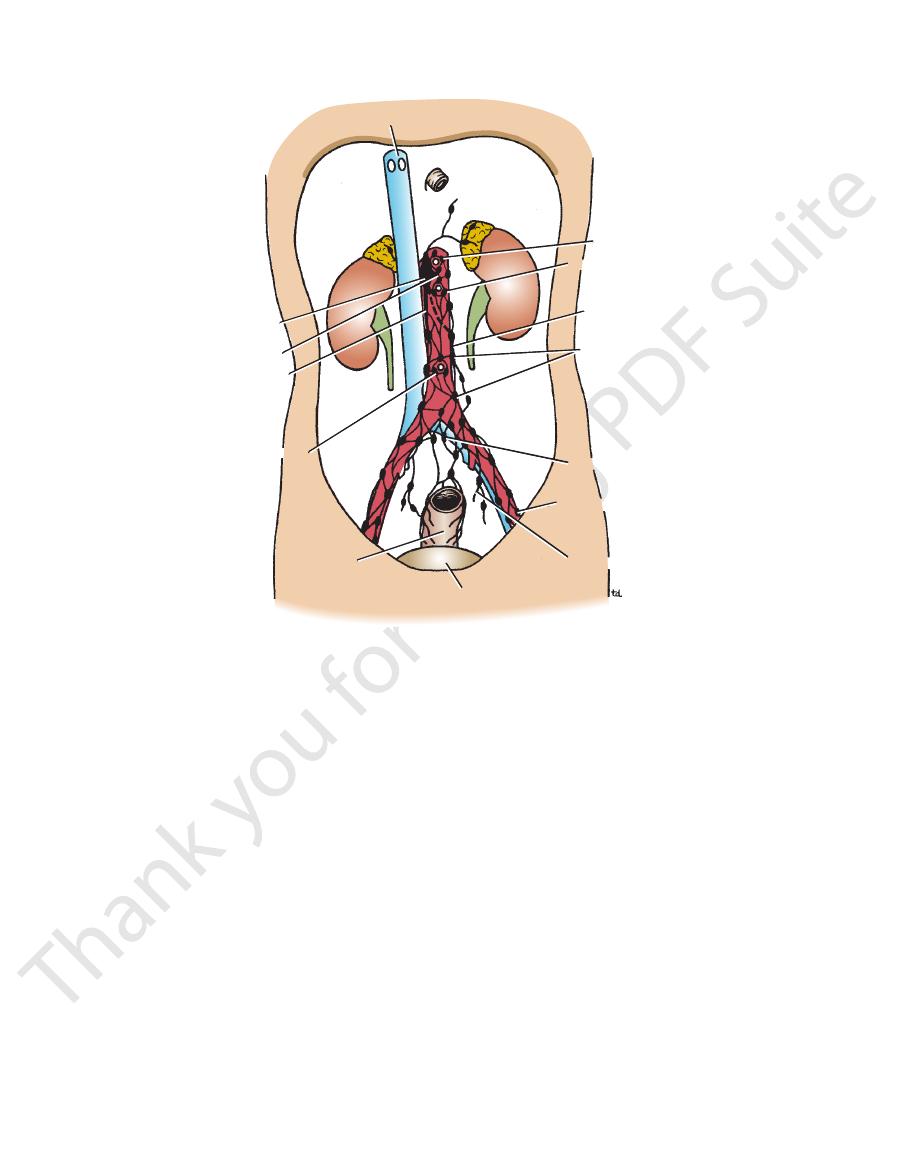
inferior vena cava
cisterna chyli
right lumbar trunk
inferior mesenteric nodes
rectum
bladder
internal iliac nodes
external iliac nodes
common iliac nodes
lateral aortic
(para-aortic) nodes
left lumbar trunk
superior mesenteric nodes
celiac nodes
intestinal trunk
FIGURE 5.76
Lymph vessels and nodes on the posterior abdominal wall.
Basic Anatomy
223
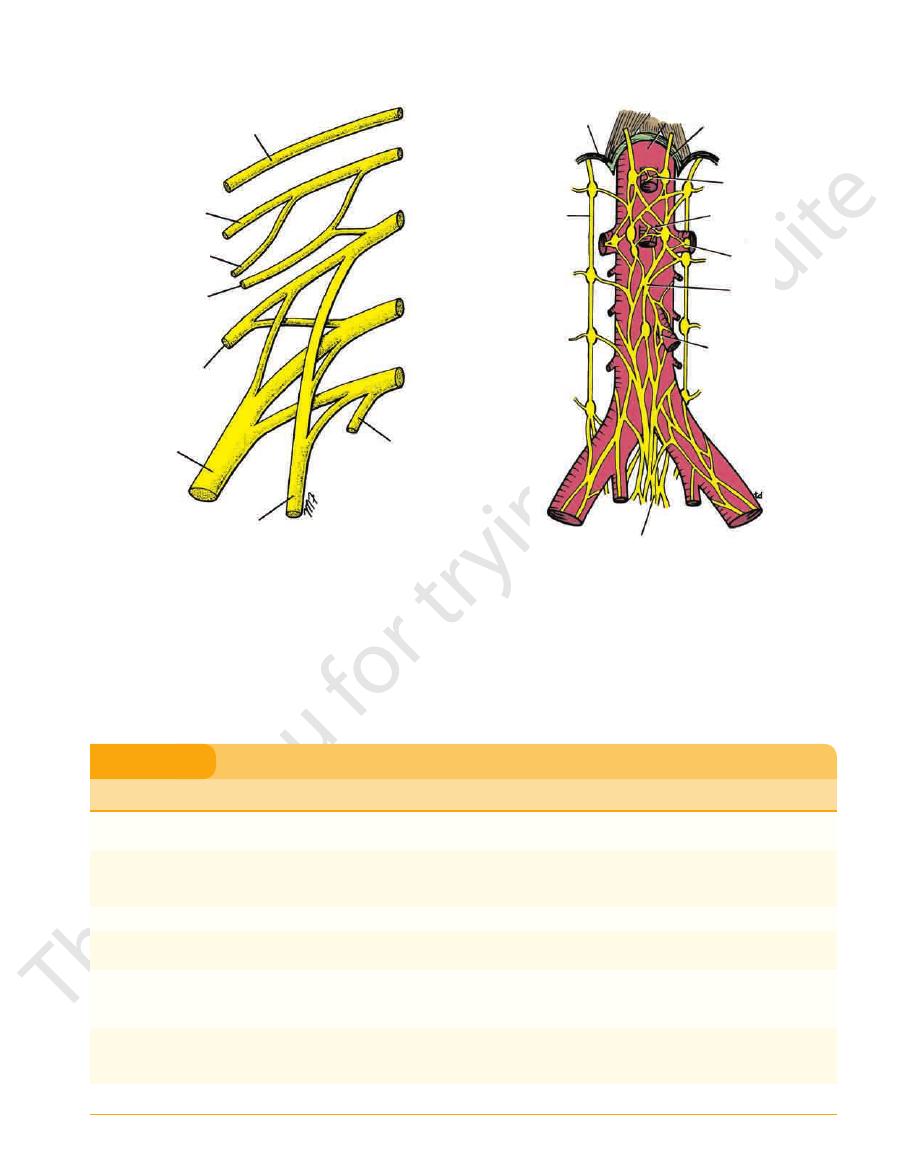
subcostal nerve
iliohypogastric nerve
ilioinguinal nerve
genitofemoral nerve
lateral cutaneous
nerve of the thigh
femoral nerve
obturator nerve
to lumbosacral trunk
T12
L1
L2
L3
L4
FIGURE 5.77
Lumbar plexus of nerves.
of the medial side of the leg and foot; articular branches to hip and knee joints
Iliacus, pectineus, sartorius, quadriceps femoris muscles, and intermediate cutaneous
Cremaster muscle in scrotum in male; skin over anterior surface of thigh; nervous pathway for
skin of upper medial aspect of thigh; root of penis and scrotum in the male; mons pubis and
External oblique, internal oblique, transversus abdominis muscles of anterior abdominal wall;
External oblique, internal oblique, transversus abdominis muscles of anterior abdominal wall;
Branches
Distribution
Iliohypogastric nerve
skin over lower anterior abdominal wall and buttock
Ilioinguinal nerve
labia majora in the female
Lateral cutaneous nerve of the thigh
Skin of anterior and lateral surfaces of the thigh
Genitofemoral nerve (L1, 2)
cremasteric reflex
Femoral nerve (L2, 3, 4)
branches to the skin of the anterior surface of the thigh and by saphenous branch to the skin
Obturator nerve (L2, 3, 4)
Gracilis, adductor brevis, adductor longus, obturator externus, pectineus, adductor magnus
(adductor portion), and skin on medial surface of thigh; articular branches to hip and knee
joints
Segmental branches
Quadratus lumborum and psoas muscles
Branches of the Lumbar Plexus and their Distribution
T A B L E 5 . 1
responding lumbar spinal nerve. A gray ramus contains
join each ganglion to a cor
Gray rami communicantes
nerve fibers.
contains preganglionic nerve fibers and afferent sensory
to the first two lumbar spinal nerves. A white ramus
join the first two ganglia
White rami communicantes
Branches
■
■
■
■
-
medial arcuate
ligament
sympathetic
trunk
aorta
aortic opening in
diaphragm
celiac plexus
superior mesenteric
plexus
renal plexus
aortic plexus
inferior mesenteric
plexus
hypogastric plexus
FIGURE 5.78
Aorta and related sympathetic plexuses.
receive fibers from splanchnic nerves and the vagus.)
abdominal aorta and its branches. (These plexuses also
Fibers pass medially to the sympathetic plexuses on the
cles of the skin (see Fig. 1.4).
to the blood vessels, sweat glands, and arrector pili mus
are distributed through the branches of the spinal nerves
postganglionic nerve fibers. The postganglionic fibers
-
■
■
224
CHAPTER 5
from the sacral parasympathetic.
enteric plexus is similar but receives parasympathetic fibers
branches of the corresponding arteries. The inferior mes
than the celiac plexus. They are distributed along the
The renal and superior mesenteric plexuses are smaller
the branches of the artery.
distribution. Parasympathetic vagal fibers also accompany
the branches of the celiac artery and follow them to their
sympathetic fibers). Postganglionic branches accompany
the greater and lesser splanchnic nerves (preganglionic
rounds the origin of the celiac artery. The ganglia receive
connected together by a large network of fibers that sur
celiac ganglia
The celiac plexus consists mainly of two
respectively.
inferior mesenteric
superior mesenteric plexus,
celiac plexus, renal plexus,
mesenteric arteries form the
gins of the celiac, renal, superior mesenteric, and inferior
Regional concentrations of this plexus around the ori
around the abdominal part of the aorta (Fig. 5.78).
aortic plexus,
ent fibers form a plexus of nerves, the
preganglionic parasympathetic fibers, and visceral affer
Preganglionic and postganglionic sympathetic fibers,
(Fig. 5.78).
hypogastric plexus
superior
they form a large bundle of fibers called the
branches from sympathetic nerves in front of the aorta,
mon iliac vessels into the pelvis, where, together with
Fibers pass downward and medially in front of the com
The Abdomen: Part II—The Abdominal Cavity
■
■
-
Aortic Plexuses
-
-
and
plexus,
-
-
Lumbar Sympathectomy
ticipate in reflex activity. Reflex sweating, salivation, nausea,
nal obstruction as in intestinal obstruction, in the passage of a
cera later move laterally as development proceeds, taking their
line structures and receive a bilateral nerve supply; many vis
probably because the viscera develop embryologically as mid
neum is chemically irritated, produces the same symptoms and
is inflamed. Any movement of that inflamed peritoneum, even
by the same nerves, it is not surprising to find cutaneous
Intercostal nerves
from the abdomen reach the central nervous system in the fol
skin, fascia, muscles, and parietal peritoneum. It can be severe
physician. This section provides an anatomic basis for the differ
the limb as branches of these nerves. Additional postganglionic
supply the vessels of the lower limb leave the spinal cord from
Lumbar sympathectomy is performed mainly to produce a vaso-
dilatation of the arteries of the lower limb in patients with vaso-
spastic disorders. The preganglionic sympathetic fibers that
segments T11 to L2. They synapse in the lumbar and sacral gan-
glia of the sympathetic trunks. The postganglionic fibers join the
lumbar and sacral nerves and are distributed to the vessels of
fibers pass directly from the lumbar ganglia to the common and
external iliac arteries, but they follow the latter artery only down
as far as the inguinal ligament. In the male, a bilateral lumbar
sympathectomy may be followed by loss of ejaculatory power,
but erection is not impaired.
Abdominal Pain
Abdominal pain is one of the most important problems facing the
-
ent forms of abdominal pain found in clinical practice.
Three distinct forms of pain exist: somatic, visceral, and
referred pain.
Somatic Abdominal Pain
Somatic abdominal pain in the abdominal wall can arise from the
and precisely localized. When the origin is on one side of the
midline, the pain is also lateralized. The somatic pain impulses
-
lowing segmental spinal nerves:
■
■
Central part of the diaphragm: Phrenic nerve (C3, 4, and 5)
■
■
Peripheral part of the diaphragm:
(T7 to 11)
■
■
Anterior abdominal wall: Thoracic nerves (T7 to 12) and the
1st lumbar nerve
■
■
Pelvic wall: Obturator nerve (L2, 3, and 4)
The inflamed parietal peritoneum is extremely sensitive, and
because the full thickness of the abdominal wall is innervated
hypersensitivity (hyperesthesia) and tenderness. Local reflexes
involving the same nerves bring about a protective phenomenon
in which the abdominal muscles increase in tone. This increased
tone or rigidity, sometimes called guarding, is an attempt to rest
and localize the inflammatory process.
Rebound tenderness occurs when the parietal peritoneum
when that movement is elicited by removing the examining hand
from a site distant from the inflamed peritoneum, brings about
tenderness.
Examples of acute, severe, localized pain originating in the
parietal peritoneum are seen in the later stages of appendicitis.
Cutaneous hyperesthesia, tenderness, and muscular spasm or
rigidity occur in the lower right quadrant of the anterior abdomi-
nal wall. A perforated peptic ulcer, in which the parietal perito-
signs but involves the right upper and lower quadrants.
Visceral Abdominal Pain
Visceral abdominal pain arises in abdominal organs, visceral
peritoneum, and the mesenteries. The causes of visceral pain
include stretching of a viscus or mesentery, distention of a hol-
low viscus, impaired blood supply (ischemia) to a viscus, and
chemical damage (e.g., acid gastric juice) to a viscus or its cov-
ering peritoneum. Pain arising from an abdominal viscus is dull
and poorly localized. Visceral pain is referred to the midline,
-
-
nerve supply with them.
Colic is a form of visceral pain produced by the violent
contraction of smooth muscle; it is commonly caused by lumi-
gallstone in the biliary ducts, or in the passage of a stone in the
ureters.
Many visceral afferent fibers that enter the spinal cord par-
vomiting, and increased heart rate may accompany visceral
pain.
C L I N I C A L N O T E S
(continued)
