
Basic Anatomy
241
bones) anteriorly. Above the brim is the
The true pelvis has an inlet, an outlet, and a cavity.
bony canal through which the child passes during birth.
vis is of great importance for obstetrics, because it is the
Knowledge of the shape and dimensions of the female pel
True Pelvis
the true pelvis.
During the early stages of labor, it helps guide the fetus into
3rd month of pregnancy helps support the gravid uterus.
nal cavity. It supports the abdominal contents and after the
upper end and should be considered as part of the abdomi
the anterior abdominal wall. The false pelvis flares out at its
and the iliacus muscles, and in front by the lower part of
behind by the lumbar vertebrae, laterally by the iliac fossae
The false pelvis is of little clinical importance. It is bounded
sacrum is directed forward and downward.
faces upward and backward and the anterior surface of the
This means that the pelvic surface of the symphysis pubis
superior iliac spines should lie in the same vertical plane.
tion. The front of the symphysis pubis and the anterior
trunk, with the individual standing in the anatomic posi
the correct orientation of the bony pelvis relative to the
It is important for the student, at the outset, to understand
true pelvis
which forms part of the abdominal cavity. Below the brim
false pelvis,
is the
.
Orientation of the Pelvis
-
False Pelvis
-
-
C H A P T E R O B J E C T I V E S
■
■
The pelvis is a bowl-shaped bony structure that protects the ter-
minal parts of the gastrointestinal tract and the urinary system
and the male and female internal organs of reproduction.
■
■
It also contains important nerves, blood vessels, and lymphatic
tissues.
■
■
The purpose of this chapter is to review the significant anatomy
of the pelvic walls relative to clinical problems. Particular atten-
tion is paid to age and sexual differences and to the anatomic
features associated with pelvic examinations.
C H A P T E R O U T L I N E
(continued)
Radiographic Anatomy 259
Surface Anatomy 259
Surface Landmarks 259
Iliac Crest 259
Anterior Superior Iliac Spine 260
Posterior Superior Iliac Spine 260
Pubic Tubercle 260
Pubic Crest 260
Symphysis Pubis 260
Spinous Processes of Sacrum 260
Sacral Hiatus 260
Coccyx 260
Viscera 260
Urinary Bladder 260
Uterus 260
Rectal and Vaginal Examinations as
a Means of Palpating the Pelvic
Viscera 261
natomy
asic
B
a
The pelvis
(joint between bodies of pubic
symphysis pubis
ward around the inner surface of the ileum) laterally,
(a line that runs downward and for
iliopectineal lines
upper margin of the first sacral vertebra) behind, the
(anterior and
sacral promontory
which is formed by the
pelvic brim
The pelvis is divided into two parts by the
organs of reproduction.
parts of the intestinal and urinary tracts and the internal
basin-shaped structure that contains and protects the lower
. The bony pelvis thus forms a strong
sacroiliac joints
and posteriorly with the sacrum at
symphysis pubis
The two hip bones articulate with each other anteriorly
umn and form the back wall (Fig. 6.1).
, which are part of the vertebral col
coccyx
sacrum
, which form the lateral and anterior walls, and the
bones
The bony pelvis is composed of four bones: the two
and provides attachment for trunk and lower limb muscles.
tion, it contains, supports, and protects the pelvic viscera
the body from the vertebral column to the femurs. In addi
The bony pelvis’s main function is to transmit the weight of
continuous, the two regions are described separately.
abdomen. Although the abdominal and pelvic cavities are
is the region of the trunk that lies below the
*
The Pelvis
-
hip
and the
-
at the
the
,
-
and the
applied to the skeleton of the region—that is, the pelvic girdle or bony pelvis.
lower limbs meet. The word pelvis means “a basin” and is more correctly
*The term pelvis is loosely used to describe the region where the trunk and

242
CHAPTER 6
inflexible, they should be considered to form part of
the sacrotuberous ligaments are strong and relatively
(see page 246). From an obstetric standpoint, because
lesser sciatic foramina
and
greater
and 6.2) into the
(Figs. 6.1
sacrospinous ligaments
sacrotuberous
sciatic notches. The sciatic notches are divided by the
is between the ischiopubic rami, and laterally are the
outlet has three wide notches. Anteriorly, the pubic arch
(Figs. 6.2 and 6.3). The pelvic
pubic arch
riorly by the
the coccyx, laterally by the ischial tuberosities, and ante
(Fig. 6.2) is bounded posteriorly by
pelvic outlet
The
(Fig. 6.1).
opectineal lines, and anteriorly by the symphysis pubis
posteriorly by the sacral promontory, laterally by the ili
(Fig. 6.2), is bounded
pelvic brim
, or
pelvic inlet
The
lateral walls and an inferior wall or floor (Fig. 6.6).
parietal peritoneum. The pelvis has anterior, posterior, and
that are partly lined with muscles covered with fascia and
The walls of the pelvis are formed by bones and ligaments
Structure of the Pelvic Walls
a much deeper posterior wall (Fig. 6.2).
is a short, curved canal, with a shallow anterior wall and
lies between the inlet and the outlet. It
pelvic cavity
The
boundaries behind.
the sacrotuberous ligaments and the coccyx forming the
symphysis pubis forming the boundaries in front and
diamond shaped, with the ischiopubic rami and the
the perimeter of the pelvic outlet. Thus, the outlet is
The Pelvis: Part I—The Pelvic Walls
■
■
■
■
-
■
■
-
and
promontory of sacrum
first sacral spine
sacral canal
sacroiliac joint
lateral mass of sacrum
ischial spine
iliopectineal line
acetabulum
obturator foramen
ramus of ischium
pubic crest
pubic tubercle
body of pubis
superior ramus of pubis
sacrospinous ligament
sacrotuberous
ligament
tubercle of iliac crest
iliac fossa
iliopectineal line
pubic crest
pubic tubercle
symphysis pubis
tip of coccyx
greater trochanter of femur
A
B
promontory of sacrum
FIGURE 6.1
Anterior view of the male pelvis and female pelvis
(A)
(B).
Basic Anatomy
243
C L I N I C A L N O T E S
Clinical Concept: The Pelvis is a Basin with
, which is normally about 5 in. (13 cm).
diagonal conjugate
der of the symphysis. The fingers are then withdrawn and the
examining hand where it makes contact with the lower bor
the perineum sufficiently, an attempt is made to palpate the
amine its shape. Is it broad or angular? The examiner’s four
is an imaginary line joining the central
is the space between the inlet and the out
pelvic cavity
and posteriorly by the coccyx. The sacrotuberous ligaments
Four terms relating to areas of the pelvis are commonly used
importance in obstetrics. The female pelvis is well adapted for
pudendal nerve and internal pudendal vessels are the wires and
[lesser sciatic foramen]. In the case of the human body, the
get outside the building and then return through a second hole
floor, they have to pierce the wall [greater sciatic foramen] to
gain entrance to the apartment below, without going through the
vessels. (One can make a further analogy here: For the wires to
gluteal region for the pudendal nerve and the internal pudendal
sciatic foramen provides an entrance into the perineum from the
pudendal nerve, and the gluteal nerves and vessels; the lesser
the true pelvis into the gluteal region for the sciatic nerve, the
. The greater sciatic foramen provides an exit from
lesser sciatic
convert the greater
the passage of the anterior rami of the sacral spinal nerves. The
, for
The basin has many holes: The posterior wall has holes on the
inferior wall or floor formed by the important levator ani and coc
are partly lined with muscles (obturator internus and piriformis)
The walls of the pelvis are formed by bones and ligaments; these
Holes in its Walls
covered with fascia and parietal peritoneum. On the outside of
the pelvis are the attachments of the gluteal muscles and the
obturator externus muscle. The greater part of the bony pelvis is
thus sandwiched between inner and outer muscles.
The basin has anterior, posterior, and lateral walls and an
-
cygeus muscles and their covering fascia.
anterior surface of the sacrum, the anterior sacral foramina
sacrotuberous and sacrospinous ligaments
and lesser sciatic notches into the greater and
foramina
the levator ani and the coccygeus muscles are the floor.)
The lateral pelvic wall has a large hole, the obturator fora-
men, which is closed by the obturator membrane, except for a
small opening that permits the obturator nerve to leave the pelvis
and enter the thigh.
Pelvic Measurements in Obstetrics
The capacity and shape of the female pelvis are of fundamental
the process of childbirth. The pelvis is shallower and the bones
are smoother than in the male. The size of the pelvic inlet is simi-
lar in the two sexes, but in the female, the cavity is larger and
cylindrical and the pelvic outlet is wider in both the anteroposte-
rior and the transverse diameters.
in clinical practice:
■
■
The pelvic inlet or brim of the true pelvis (Fig. 6.4) is bounded
anteriorly by the symphysis pubis, laterally by the iliopectin-
eal lines, and posteriorly by the sacral promontory.
■
■
The pelvic outlet of the true pelvis (Fig. 6.4) is bounded in
front by the pubic arch, laterally by the ischial tuberosities,
also form part of the margin of the outlet.
■
■
The
-
let (Fig. 6.4).
■
■
The axis of the pelvis
points of the anteroposterior diameters from the inlet to the out-
let and is the curved course taken by the baby’s head as it de-
scends through the pelvis during childbirth (Figs. 6.4 and 6.5A).
Internal Pelvic Assessments
Internal pelvic assessments are made by vaginal examination
during the later weeks of pregnancy, when the pelvic tissues are
softer and more yielding than in the newly pregnant condition.
■
■
Pubic arch: Spread the fingers under the pubic arch and ex-
fingers should be able to rest comfortably in the angle below
the symphysis.
■
■
Lateral walls: Palpate the lateral walls and determine
whether they are concave, straight, or converging. The prom-
inence of the ischial spines and the position of the sacrospi-
nous ligaments are noted.
■
■
Posterior wall: The sacrum is palpated to determine whether
it is straight or well curved. Finally, if the patient has relaxed
promontory of the sacrum. The second finger of the examin-
ing hand is placed on the promontory, and the index finger of
the free hand, outside the vagina, is placed at the point on the
-
distance measured (Fig. 6.5B), providing the measurement of
the
The anteroposterior diameter from the sacrococcygeal joint
to the lower border of the symphysis is then estimated.
conditions such as malpresentation or malposition of the fetus,
the fetus. It may be indirectly responsible for dystocia by causing
labor). A contracted pelvis may obstruct the normal passage of
(difficult
The distance between the ischial tuber
Ischial tuberosities:
■
■
-
osities may be estimated by using the closed fist (Fig. 6.5D).
It measures about 4 in. (10 cm), but it is difficult to measure
exactly.
Needless to say, considerable clinical experience is required
to be able to assess the shape and size of the pelvis by vaginal
examination.
The Female Pelvis
Deformities of the pelvis may be responsible for dystocia
premature rupture of the fetal membranes, and uterine inertia.
The cause of pelvic deformities may be congenital (rare) or
acquired from disease, poor posture, or fractures caused by
injury. Pelvic deformities are more common in women who have
grown up in a poor environment and are undernourished. It is
probable that these women suffered in their youth from minor
degrees of rickets.
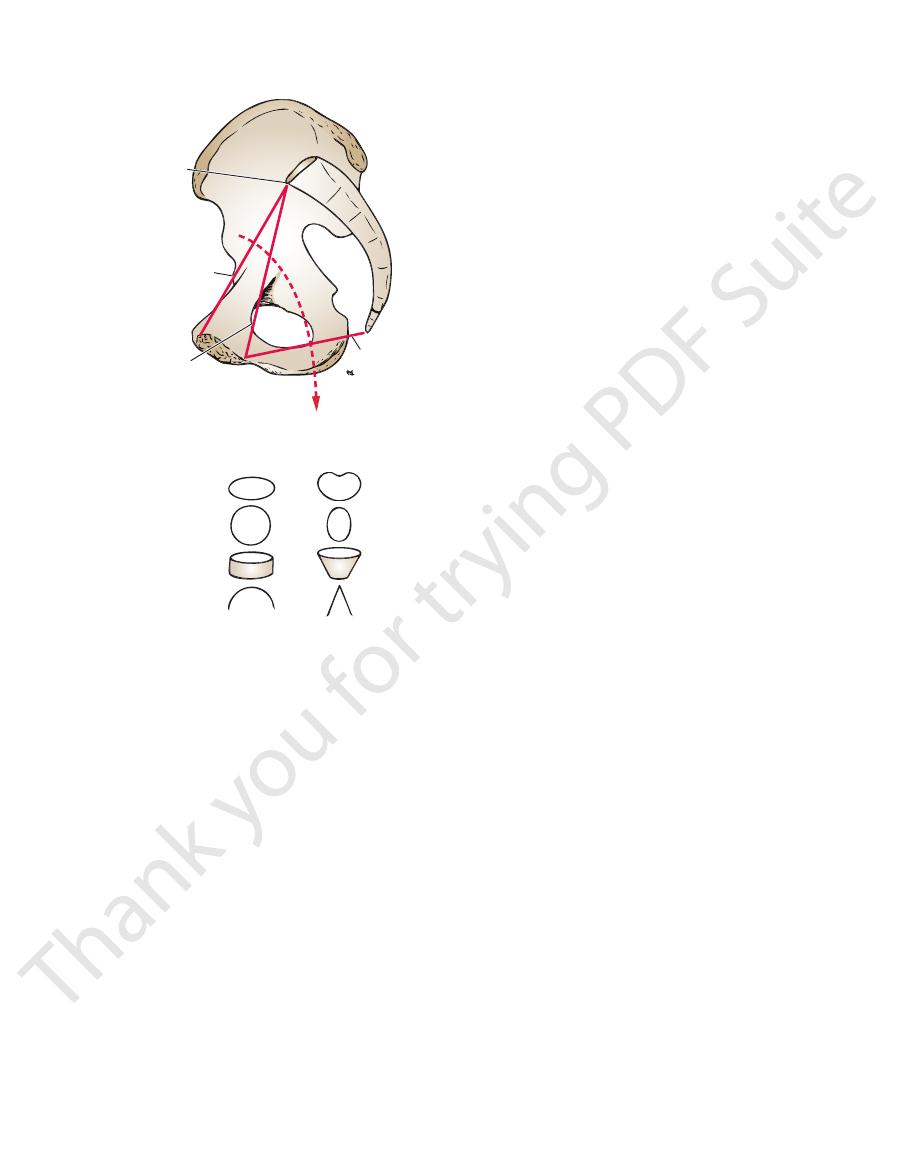
In 1933, Caldwell and Moloy classified pelves into four groups:
gynecoid, android, anthropoid, and platypelloid (Fig. 6.5C). The
type, present in about 24% of white females
gynecoid type, present in about 41% of women, is the typical
female pelvis, which was previously described.
The android type, present in about 33% of white females and
16% of black females, is the male or funnel-shaped pelvis with a
contracted outlet.
The anthropoid
and 41% of black females, is long, narrow, and oval shaped.
The platypelloid type, present in only about 2% of women,
is a wide pelvis flattened at the brim, with the promontory of the
sacrum pushed forward.

244
CHAPTER 6
symphysis pubis (Fig. 6.7).
by the bodies of the pubic bones, the pubic rami, and the
The anterior pelvic wall is the shallowest wall and is formed
Anterior Pelvic Wall
(Fig. 6.8).
rior and posterior rami of the upper four sacral nerves
sess on each side four foramina for the passage of the ante
The anterior and posterior surfaces of the sacrum pos
(Fig. 6.10).
down as far as the lower border of the 2nd sacral vertebra
It also contains the lower part of the subarachnoid space
spinal nerves; the filum terminale; and fibrofatty material.
rior and posterior roots of the lumbar, sacral, and coccygeal
sacral hiatus (Fig. 6.8). The sacral canal contains the ante
those of the 4th, fail to meet in the midline, forming the
The laminae of the 5th sacral vertebra, and sometimes
sacral canal
The vertebral foramina together form the
mark used when measuring the size of the pelvis.
(Fig. 6.2)—which is an important obstetric land
ontory
sacral prom
the posterior margin of the pelvic inlet—the
upper margins of the first sacral vertebra bulge forward as
(Fig. 6.1). The anterior and
sacroiliac joints
to form the
Laterally, the sacrum articulates with the two iliac bones
The narrow inferior border articulates with the coccyx.
base of the bone articulates with the fifth lumbar vertebra.
ward concavity (Figs. 6.2 and 6.8). The upper border or
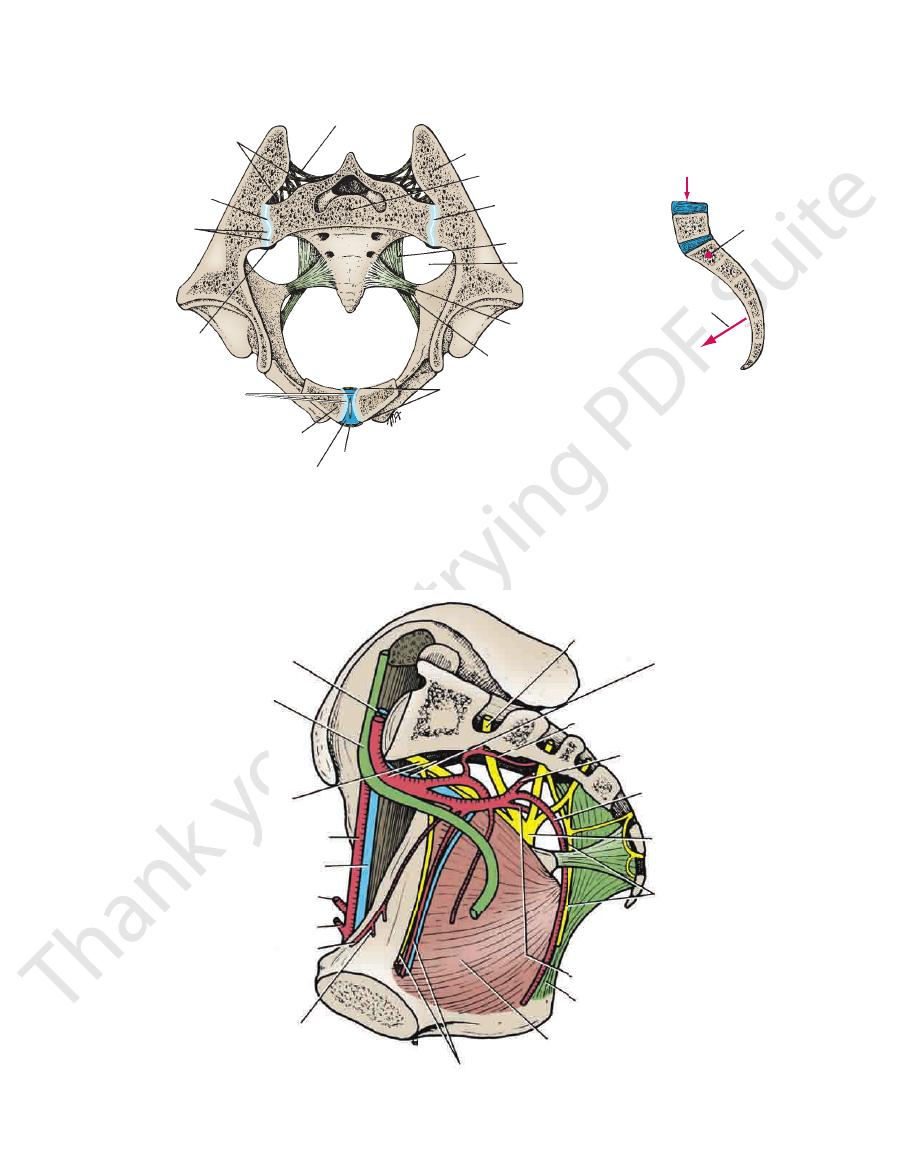
together to form a single wedge-shaped bone with a for
The sacrum consists of five rudimentary vertebrae fused
Sacrum
(Fig. 6.9) and their covering of parietal pelvic fascia.
sacrum and coccyx (Fig. 6.8) and by the piriformis muscles
The posterior pelvic wall is extensive and is formed by the
Posterior Pelvic Wall
The Pelvis: Part I—The Pelvic Walls
-
-
-
.
-
-
-
iliac crest
rough surface for attachment of
interosseous ligament
posterior superior iliac spine
auricular surface
posterior inferior iliac spine
greater sciatic notch
ischial spine
lesser sciatic notch
obturator membrane
ischial tuberosity
ischial ramus
inferior ramus of pubis
obturator canal
pubic crest
pubic tubercle
body of pubis
iliopectineal line
anterior inferior
iliac spine
anterior superior
iliac spine
iliac fossa
ilium
tubercle
of ilium
acetabulum
obturator
foramen
pubis
ischium
line of fusion
of bones
A
B
superior ramus
of pubis
FIGURE 6.3
Right hip bone.
ilium, the ischium, and the pubis.
Lateral surface. Note the lines of fusion between the three bones—the
Medial surface.
A.
B.
promontory
of sacrum
pelvic inlet
body of pubis
pubic arch
pelvic outlet
ischial tuberosity
tip of coccyx
sacrospinous
ligament
sacrotuberous
ligament
FIGURE 6.2
Right half of the pelvis showing the pelvic inlet,
pelvic outlet, and sacrotuberous and sacrospinous ligaments.
Basic Anatomy
pubis. The obturator foramen is filled in by the obturator
, which is bounded by the parts of the ischium and
men
obturator fora
of the hip bone is a large opening, the
(Fig. 6.1). In the lower part
symphysis pubis
side at the
and articulates with the pubic bone of the opposite
cle
pubic tuber
pubic crest
of the pubis bears the
. The body
inferior pubic rami
superior
body
is the anterior part of the hip bone and has
The
(Fig. 6.3).
ity
ischial tuberos
ischial spine
bone and possesses an
is the inferior and posterior part of the hip
ischium
The
divide the false from the true pelvis.
ward around the inner surface of the ilium and serves to
runs downward and for
iliopectineal line
the sacrum. The
for articulation with
auricular surface
ilium is the large
posterior inferior iliac spines. On the inner surface of the
Below these spines are the corresponding anterior and
posterior superior iliac spines
anterior
between the
(Fig. 6.3). The iliac crest runs
iliac crest
bone, possesses the
, which is the upper flattened part of the hip
ilium
The
(Fig. 6.2).
sacrospinous ligaments
sacrotuberous
ence of the
by the pres
lesser sciatic foramina
greater
into the
. The sciatic notches are converted
spine of the ischium
by the
lesser sciatic notch
which is separated from the
greater sciatic notch
the acetabulum is a large notch, the
spherical head of the femur (Figs. 6.1 and 6.3). Behind
, which articulates with the hemi
acetabulum
sion, the
On the outer surface of the hip bone is a deep depres
symphysis pubis.
they also articulate with one another anteriorly at the
iliac joints and form the anterolateral walls of the pelvis;
The hip bones articulate with the sacrum at the sacro
bones fuse together to form one large, irregular bone.
. At puberty, these three
acetabulum
by cartilage at the
riorly (Fig. 6.3). The three separate bones are joined
inferiorly; and the pubis, which lies anteriorly and infe
lies superiorly; the ischium, which lies posteriorly and
In children, each hip bone consists of the ilium, which
internus muscle and its covering fascia.
rotuberous and sacrospinous ligaments, and the obturator
below the pelvic inlet, the obturator membrane, the sac
The lateral pelvic wall is formed by part of the hip bone
Lateral Pelvic Wall
245
-
Hip Bone
-
-
-
-
,
and
-
and
and
.
-
and an
-
pubis
a
and
and
and the
-
-
membrane (Fig. 6.3).
plexus.
It receives branches from the sacral
Nerve supply:
It is a lateral rotator of the femur at the hip joint.
Action:
greater trochanter of the femur.
men (Fig. 6.9). It is inserted into the upper border of the
region by passing laterally through the greater sciatic fora
mass of the sacrum and leaves the pelvis to enter the gluteal
The piriformis muscle arises from the front of the lateral
Piriformis Muscle
late with the sacral cornua (Fig. 6.8).
superior articular processes and project upward to articu
. The cornua are the remains of the pedicles and
cornua
transverse process
first vertebra possesses a rudimentary
The coccygeal vertebrae consist of bodies only, but the
with the lower end of the sacrum (Fig. 6.8).
form a small triangular bone, which articulates at its base
The coccyx consists of four vertebrae fused together to
lumbosacral angle
called the
so that it forms an angle with the fifth lumbar vertebra,
in the female than in the male. The sacrum is tilted forward
The sacrum is usually wider in proportion to its length
rior inferior iliac spine to the ischial tuberosity (Figs. 6.2
the lateral part of the sacrum and coccyx and the poste
The sacrotuberous ligament is strong and extends from
Sacrotuberous Ligament
(Fig. 6.3).
nerve and vessels as they leave the pelvis to enter the thigh
, for the passage of the obturator
obturator canal
gap, the
completely closes the obturator foramen, leaving a small
The obturator membrane is a fibrous sheet that almost
Obturator Membrane
-
and 6.9).
.
Coccyx
and
-
-
■
■
■
■
promontory
pelvic inlet
diagonal conjugate
axis of pelvis
pelvic outlet
Female
Male
pelvic inlet
pelvic outlet
pelvic cavity
pubic arch
FIGURE 6.4
Pelvic inlet, pelvic outlet, diagonal conjugate,
between the female and the male pelvis are also shown.
and axis of the pelvis. Some of the main differences

246
CHAPTER 6
lesser sciatic foramina
greater
and lesser sciatic notches into foramina, the
body (Fig. 6.11). The two ligaments also convert the greater
rotated upward at the sacroiliac joint by the weight of the
the lower end of the sacrum and the coccyx from being
The sacrotuberous and sacrospinous ligaments prevent
coccyx and by its apex to the spine of the ischium (Figs. 6.2
is attached by its base to the lateral part of the sacrum and
The sacrospinous ligament is strong and triangle shaped. It
Sacrospinous Ligament
branch from the sacral plexus
The nerve to the obturator internus, a
Nerve supply:
It laterally rotates the femur at the hip joint.
Action:
femur.
foramen and is inserted into the greater trochanter of the
tendon, which leaves the pelvis through the lesser sciatic
the hip bone (Fig. 6.12). The muscle fibers converge to a
face of the obturator membrane and the adjoining part of
The obturator internus muscle arises from the pelvic sur
Obturator Internus Muscle
The Pelvis: Part I—The Pelvic Walls
-
■
■
■
■
and 6.9).
and
.
axis of birth canal
measuring the diagonal conjugate
gynecoid
android
anthropoid
platypelloid
measuring transverse diameter of pelvic outlet
A
B
C
D
FIGURE 6.5
Estimation of the width of the pelvic outlet by
Different types of pelvic inlets, according to Caldwell and Moloy.
Procedure used in measuring the diagonal con
Birth canal. Interrupted line indicates the axis of the canal.
A.
B.
-
jugate. C.
D.
means of a closed fist.

Basic Anatomy
covering the obturator internus, and the spine of the
tendinous arch formed by a thickening of the fascia
linear origin from the back of the body of the pubis, a
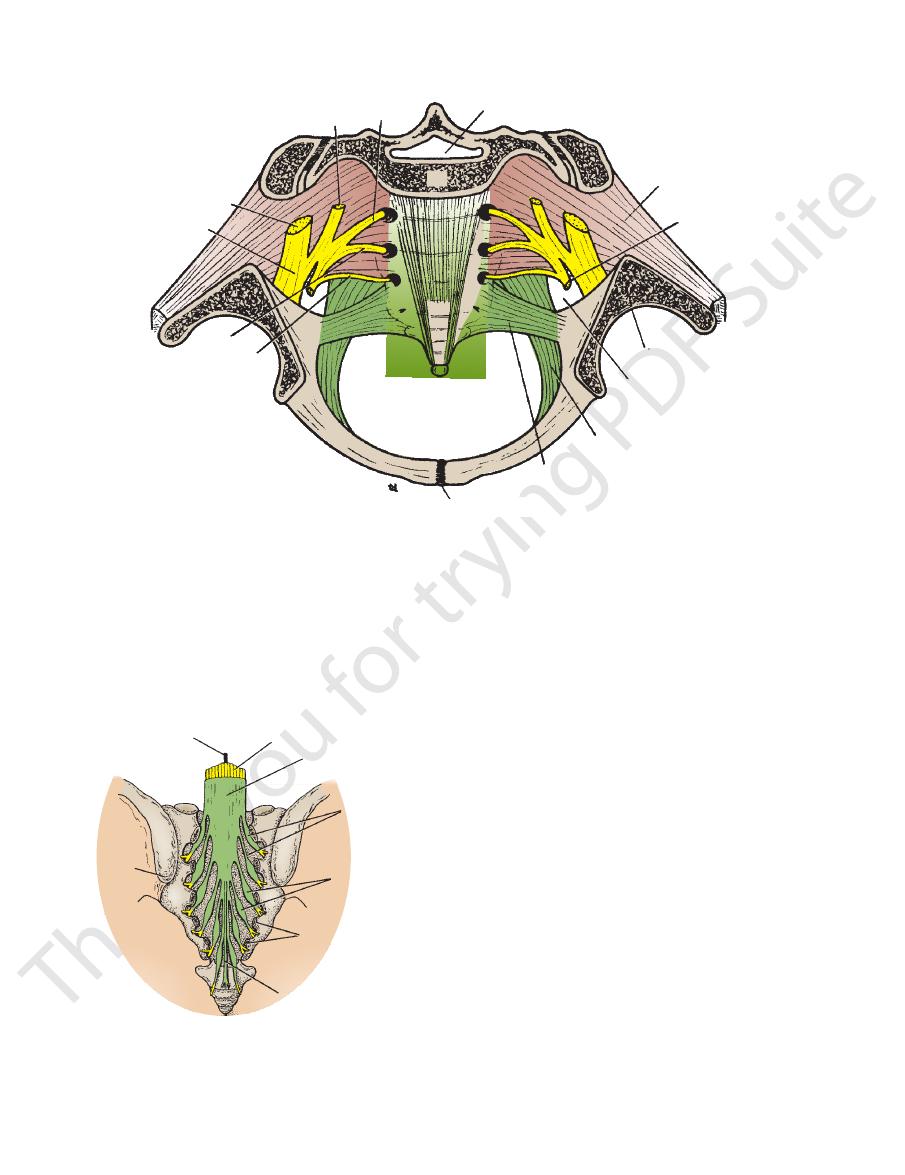
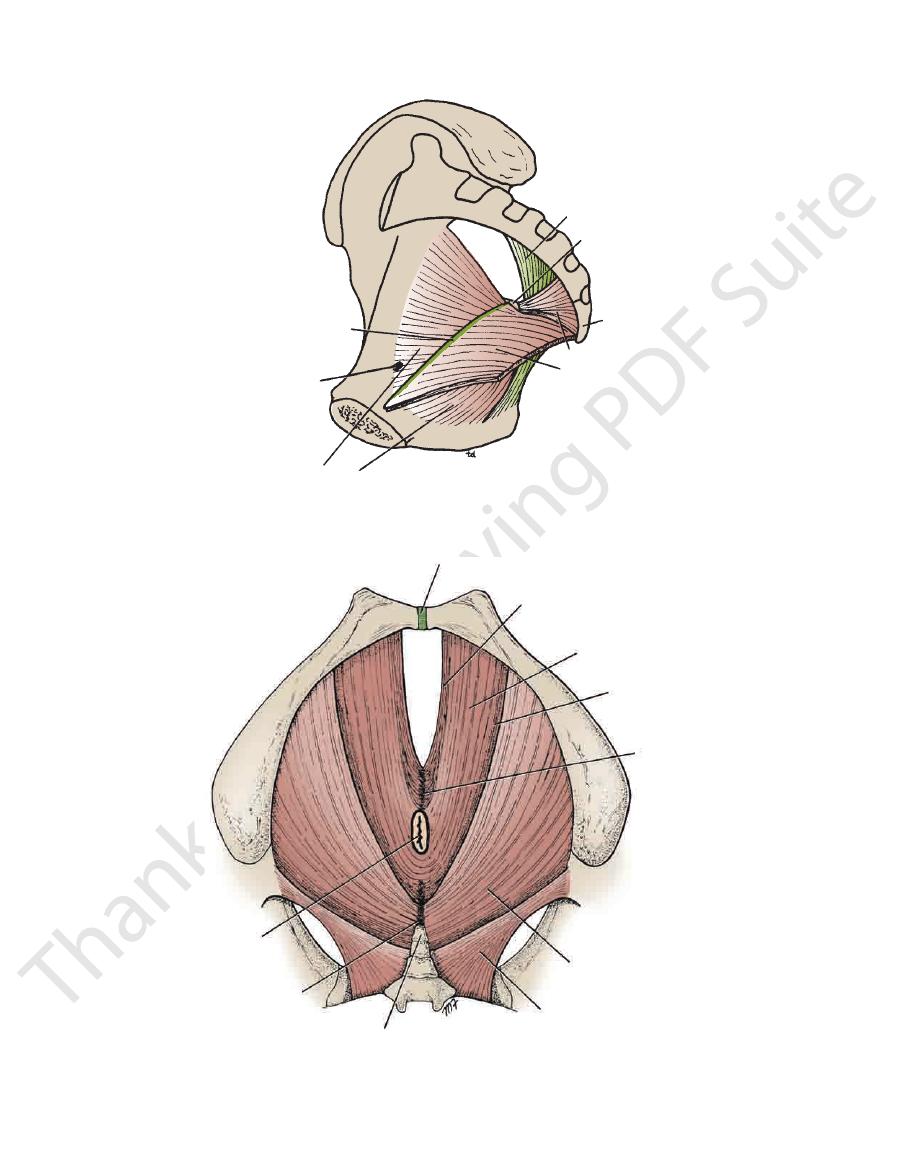
The levator ani muscle is a wide thin sheet that has a
Levator Ani Muscle
247
ischium (Fig.
om this extensive origin, groups of
6.13). Fr
fibers sweep downward and medially to their insertion
(Fig.
ws:
6.14) as follo
1.
the perineal body.
The sphincter vaginae constrict the vagina and stabilize
tae support the prostate and stabilize the perineal body.
, in front of the anal canal. The levator prosta
ineal body
per
are inserted into a mass of fibrous tissue, called the
form a sling around the prostate or vagina and
vaginae
sphincter
or
levator prostatae
The
Anterior fibers:
-
-
2.
vagina in females.
passage of the urethra in males and the urethra and the
ering fasciae (Fig. 6.13). It is incomplete anteriorly to allow
ani muscles and the small coccygeus muscles and their cov
The pelvic diaphragm is formed by the important levatores
ered in detail in Chapter 8.
viscera, and the perineum below. The perineum is consid
into the main pelvic cavity above, which contains the pelvic
The pelvic floor stretches across the pelvis and divides it
formed by the pelvic diaphragm.
The floor of the pelvis supports the pelvic viscera and is
Inferior Pelvic Wall or Pelvic Floor
, between the tip of the coccyx and the anal
cygeal body
anococ
inserted into a small fibrous mass, called the
passes posteriorly to be
pubococcygeus
canal. The
sling around the junction of the rectum and anal
forms a
puborectalis
The
Intermediate fibers:
-
canal.
-
Pelvic Diaphragm
-
pelvic inlet
anterior wall
pelvic outlet
inferior wall or floor
posterior wall
FIGURE 6.6
Right half of the pelvis showing the pelvic walls.
body of pubis
superior ramus of pubis
obturator
membrane
inferior ramus of pubis
symphysis pubis
FIGURE 6.7
Anterior wall of the pelvis (posterior view).
superior articular
process
promontory
lateral mass
anterior sacral
foramina
transverse process
of coccyx
sacral canal
superior articular
process
first sacral spine
auricular surface
posterior sacral
foramina
sacral hiatus
tip of coccyx
coccygeal cornu
median crest
A
B
sacral cornu
FIGURE 6.8
Sacrum.
Posterior view.
Anterior view.
A.
B.
248
CHAPTER 6
visceral layers.
neum. The pelvic fascia can be divided into parietal and
Below, the fascia is continuous with the fascia of the peri
tinuous above with the fascia lining the abdominal walls.
The pelvic fascia is formed of connective tissue and is con
in Table 6.1.
walls and floor, their nerve supply, and their action is given
A summary of the attachments of the muscles of the pelvic
A branch of the 4th and 5th sacral nerves
Nerve supply:
porting the pelvic viscera.
The two muscles assist the levatores ani in sup
Action:
and into the coccyx (Figs. 6.13 and 6.14).
ischium and is inserted into the lower end of the sacrum
This small triangular muscle arises from the spine of the
Coccygeus Muscle
pudendal nerve
sacral nerve and from the perineal branch of the
The perineal branch of the fourth
Nerve supply:
vagina.
in the female they serve also as a sphincter of the
sphincter action on the anorectal junction, and
occurs in coughing). They also have an important
and expulsive efforts of the abdominal muscles (as
the rise in intrapelvic pressure during the straining
The Pelvis: Part I—The Pelvic Walls
■
■
■
■
-
■
■
Pelvic Fascia
-
-
3.
maintains the pelvic viscera in position. They resist
form an efficient muscular sling that supports and
The levatores ani muscles of the two sides
Action:
anococcygeal body and the coccyx.
is inserted into the
iliococcygeus
The
Posterior fibers:
■
■
sacral canal
S1
S2
lumbosacral trunk
sciatic nerve
S4
symphysis pubis
sacrospinous ligament
sacrotuberous ligament
greater sciatic foramen
acetabulum
pudendal nerve
piriformis muscle
S3
S2
FIGURE 6.9
Posterior wall of the pelvis.
sacral canal
S1
S2
lumbosacral trunk
sciatic nerve
S4
symphysis pubis
sacrospinous ligament
sacrotuberous ligament
greater sciatic foramen
acetabulum
pudendal nerve
piriformis muscle
S3
S2
FIGURE 6.9
Posterior wall of the pelvis.
filum terminale
cauda equina
dura mater
nerve roots of
sacral nerves
posterior
root ganglia
cut laminae
of sacrum
filum terminale
posterior
superior
iliac spine
FIGURE 6.10
Sacrum from behind. Laminae have been
vertebra.
below, at the level of the lower border of the 1st lumbar
removed to show the sacral nerve roots lying within the
sacral canal. Note that in the adult the spinal cord ends
Basic Anatomy
249
posterior sacroiliac
ligament
ilium
sacrum
joint cavity
sacrotuberous
ligament
greater sciatic
foramen
sacrospinous
ligament
lesser sciatic foramen
anterior and posterior
symphyseal ligaments
symphysis pubis
disc of fibrocartilage
body of pubis
anterior sacroiliac
ligament
plates of hyaline
cartilage
sacroiliac joint
interosseous sacroiliac
ligament
weight of trunk
axis of rotation
sacrotuberous and
sacrospinous ligaments
plates of hyaline
cartilage
FIGURE 6.11
Horizontal section through the pelvis showing the sacroiliac joints and the symphysis pubis. The lower diagram
the weight of the trunk.
shows the function of the sacrotuberous and sacrospinous ligaments in resisting the rotation force exerted on the sacrum by
S1
internal iliac artery
and vein
lateral sacral artery
middle rectal artery
internal
pudendal artery
sciatic nerve
pudendal nerve
inferior gluteal artery
sacrotuberous ligament
obturator internus muscle
obturator nerve and vessels
common iliac artery and vein
ureter
lumbosacral trunk
external iliac artery
external iliac vein
deep circumflex iliac artery
inferior epigastric artery
obliterated umbilical artery
superior vesical artery
FIGURE 6.12
Lateral wall of the pelvis.
250
CHAPTER 6
The Pelvis: Part I—The Pelvic Walls
sacrotuberous ligament
ischial spine
coccyx
coccygeus muscle
levator ani muscle
obturator internus muscle
obturator canal
linear thickening of fascia
covering obturator internus muscle
FIGURE 6.13
Inferior wall or floor of the pelvis.
symphysis pubis
levator prostatae or
sphincter vaginae
puborectalis
iliococcygeus
perineal body
coccygeus
tip of coccyx
anococcygeal body
junction of rectum
and anal canal
pubococcygeus
FIGURE 6.14
Levator ani muscle and coccygeus muscle seen on their inferior aspects. Note that the levator ani is made up
muscular floor to the pelvis, known as the pelvic diaphragm.
of several different muscle groups. The levator ani and coccygeus muscles with their fascial coverings form a continuous
252
CHAPTER 6
see pages 278 and 296.
with the visceral peritoneum (Fig. 6.17). For further details,
reflected onto the pelvic viscera and becomes continuous
The parietal peritoneum lines the pelvic walls and is
sacrocervical ligaments.
to their attachments, for example, the pubovesical and the
vides support. These fascial ligaments are named according
and extends from the viscus to the pelvic walls and pro
the pelvic viscera. In certain locations, the fascia thickens
The visceral layer of pelvic fascia covers and supports all
Visceral Layer of Pelvic Fascia
superior fascial layer of the urogenital diaphragm.
and the perineal membrane (see page 314) and forms the
in the perineum. It covers the sphincter urethrae muscle
fascia covering the inferior surface of the pelvic diaphragm,
vic fascia becomes continuous through the opening with the
the pelvic diaphragm is deficient anteriorly, the parietal pel
named according to the muscle it overlies (Fig. 6.17). Where
The parietal pelvic fascia lines the walls of the pelvis and is
The Pelvis: Part I—The Pelvic Walls
Parietal Pelvic Fascia
-
-
Pelvic Peritoneum
Injury to the Pelvic Floor
may
. In the latter condition, the
and alteration in the position of the bladder neck and urethra,
, herniation of the bladder
vaginal prolapse
Injury to the pelvic floor during a difficult childbirth can result
in the loss of support for the pelvic viscera leading to uterine
and
(cystocele),
leading to stress incontinence
patient dribbles urine whenever the intra-abdominal pres-
sure is raised, as in coughing. Prolapse of the rectum
also occur.
Partial Fusion of the Sacral Vertebrae
The 1st sacral vertebra can be partly or completely separated
from the 2nd sacral vertebra. Occasionally, on radiographs of
the vertebral column, examples are seen in which the 5th lumbar
vertebra has fused with the 1st sacral vertebra.
Trauma to the True Pelvis
Trauma to the true pelvis can result in fracture of the lateral
mass of the sacrum (see previous column).
Name of Muscle
Origin
Insertion
Nerve Supply
Action
Piriformis
Front of sacrum
Greater trochanter of femur
Sacral plexus
Lateral rotator of femur
at hip joint
Obturator internus
Obturator membrane and
adjoining part of hip bone
Greater trochanter of femur
Nerve to obturator
internus from
sacral plexus
Lateral rotator of femur
at hip joint
Levator ani
Body of pubis, fascia of
obturator internus, spine
of ischium
Perineal body;
anococcygeal body;
walls of prostate, vagina,
rectum, and anal canal
Fourth sacral nerve,
pudendal nerve
Supports pelvic
viscera; sphincter to
anorectal junction
and vagina
Coccygeus
Spine of ischium
Lower end of sacrum;
coccyx
Fourth and fifth sacral
nerve
Assists levator ani
to support pelvic
viscera; flexes
coccyx
Muscles of the Pelvic Walls and Floor
T A B L E 6 . 1
anterior superior
iliac spine
ischial tuberosity
A
B
C
D
anterior
inferior
iliac
spine
FIGURE 6.15
hamstring muscles, for the avulsion of the ischial tuberosity.
for the avulsion of the anterior inferior iliac spine; and the
iliac spine; the straight head of the rectus femoris muscle,
cle is responsible for the avulsion of the anterior superior
Avulsion fractures of the pelvis. The sartorius mus
Different types of fractures of the pelvic
A–C.
basin. D.
-
