
Basic Anatomy
without interruption from one organ to the other. The
the neck of the bladder, the smooth muscle passing
The base of the prostate is continuous with
Superiorly:
Relations
margins of the prostatic utricle (see Fig. 7.16).
the prostate to open into the prostatic urethra at the lateral
tory ducts pierce the upper part of the posterior surface of
against the urogenital diaphragm below. The two ejacula
which lies
apex,
lies against the bladder neck above, and an
which
Fig. 7.16). The somewhat conical prostate has a
The prostate is surrounded by a fibrous capsule (see
above and the urogenital diaphragm below (see Fig. 7.16).
1.25 in. (3 cm) long and lies between the neck of the bladder
rounds the prostatic urethra (see Figs. 7.4 and 7.16). It is about
The prostate is a fibromuscular glandular organ that sur
Location and Description
the prostatic urethra.
tatic utricle; their function is to drain the seminal fluid into
static part of the urethra, close to the margins of the pros
the posterior surface of the prostate and open into the pro
the seminal vesicle (Fig. 7.16). The ejaculatory ducts pierce
are formed by the union of the vas deferens and the duct of
The two ejaculatory ducts are each <1 in. (2.5 cm) long and
thus washing the spermatozoa out of the urethra.
contract and expel their contents into the ejaculatory ducts,
the spermatozoa. During ejaculation, the seminal vesicles
that is added to the seminal fluid. The secretions nourish
The function of the seminal vesicles is to produce a secretion
Function
The internal iliac nodes.
Lymph Drainage
The veins drain into the internal iliac veins.
Veins
The inferior vesicle and middle rectal arteries.
Arteries
embedded in connective tissue.
Each seminal vesicle consists of a much-coiled tube
ejaculatory duct.
the same side to form the
each seminal vesicle narrows and joins the vas deferens of
vesicles are related to the rectum (see Fig. 7.4). Inferiorly,
terminal part of the vas deferens. Posteriorly, the seminal
(see Fig. 7.13). On the medial side of each vesicle lies the
(5 cm) long lying on the posterior surface of the bladder
The seminal vesicles are two lobulated organs about 2 in.
Seminal Vesicles
ejaculatory duct.
the duct of the seminal vesicle to form the
The inferior end of the ampulla narrows down and joins
ampulla of the vas deferens.
deferens is dilated to form the
of the bladder (see Fig. 7.11). The terminal part of the vas
275
Blood Supply
Ejaculatory Ducts
-
-
Prostate
-
base,
-
■
■
bladder wall
sphincter vesicae
prostate
sphincter urethrae
spinal cord
A
B
FIGURE 7.15
then runs medially and downward on the posterior surface
the ureter in the region of the ischial spine. The vas deferens
and backward on the lateral wall of the pelvis and crosses
epigastric artery (see Fig. 7.11). It then passes downward
nal ring and passes around the lateral margin of the inferior
through the inguinal canal. It emerges from the deep ingui
from the lower end or tail of the epididymis and passes
epididymis to the ejaculatory duct and the urethra. It arises
(45 cm) long that conveys mature sperm from the
The vas deferens is a thick-walled tube about 18 in.
Vas Deferens
are described on page 131.
epididymides
testes
The
during the second or third year of life.
Voluntary control of micturition is normally developed
which compresses the bladder neck.
closes the urethra; this is assisted by the sphincter vesicae,
accomplished by contracting the sphincter urethrae, which
segments of the cord. Voluntary control of micturition is
with the corticospinal tracts to the 2nd, 3rd, and 4th sacral
rition are favorable. The inhibitory fibers pass downward
of the cerebral cortex until the time and place for mictu
omitted for clarity.
to the bladder are shown; the sympathetic fibers have been
ous system and the parasympathetic efferent fibers passing
sensory fibers from the bladder entering the central nerv
The afferent
of the spinal cord in the upper thoracic region. Destruction
Nervous control of the bladder after section
A.
of the sacral segments of the spinal cord. B.
-
-
Male Genital Organs
and
-
276
CHAPTER 7
The Pelvis: Part II—The Pelvic Cavity
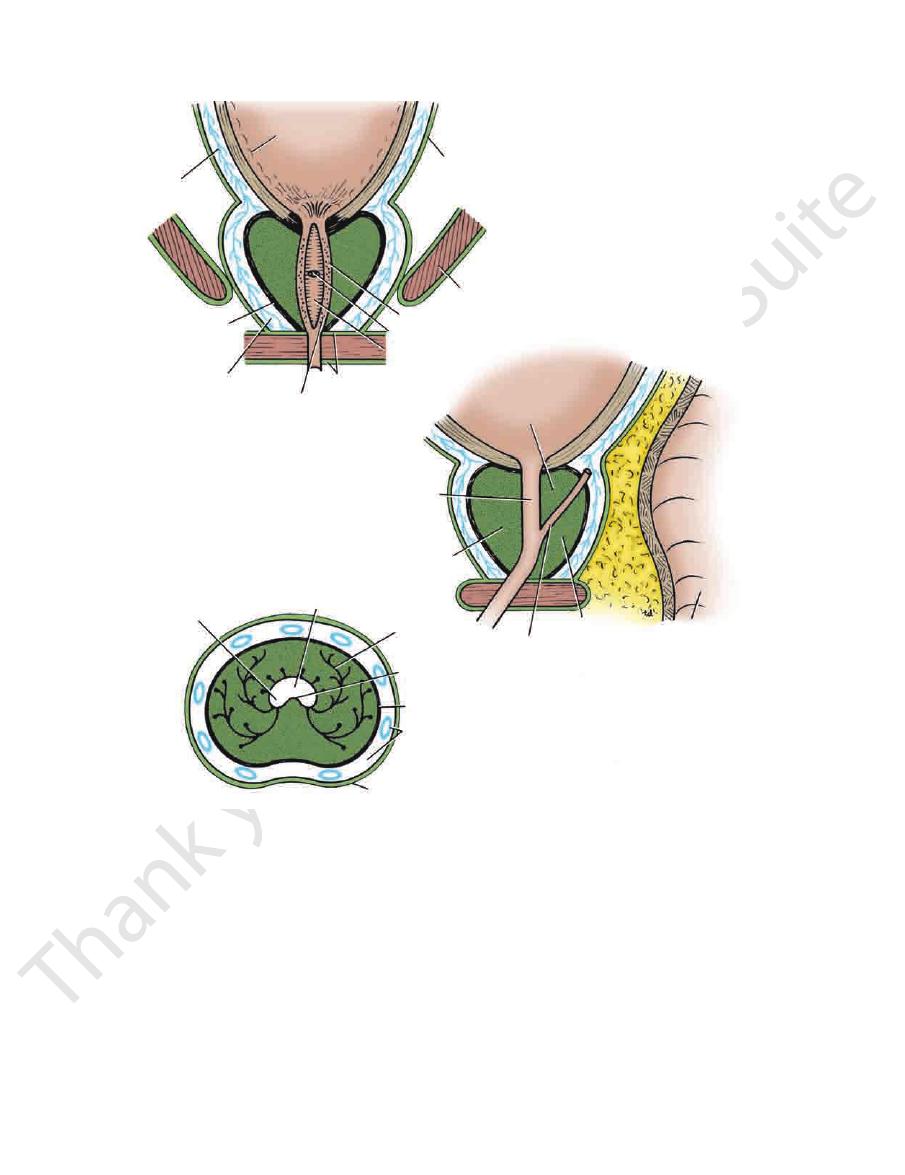
mucous membrane
bladder
vesicle veins
capsule
of prostate
prostatic venous plexus
openings of prostatic glands
urogenital diaphragm
urethral crest
prostatic utricle
prostatic sinus
levator ani
visceral pelvic fascia
bladder
median lobe
urethra
anterior lobe
ejaculatory duct
posterior lobe
anal
canal
prostatic sinus
prostatic urethra
glands of prostate
urethral crest
capsule of prostate
prostatic venous plexus
fascial sheath of prostate
A
B
C
FIGURE 7.16
Prostate in coronal section
lies in front of the urethra and
anterior lobe
Fig. 7.16). The
The prostate is incompletely divided into five lobes (see
ducts open into the prostatic urethra.
mixture of smooth muscle and connective tissue, and their
The numerous glands of the prostate are embedded in a
Structure of the Prostate
pubis (see Fig. 7.16).
ers of the levator ani as they run posteriorly from the
The prostate is embraced by the anterior fib
Laterally:
extended down to the perineal body.
the rectovesical pouch of peritoneum, which originally
in fetal life by the fusion of the walls of the lower end of
This septum is formed
tum (fascia of Denonvilliers).
rectovesical sep
ampulla and is separated from it by the
closely related to the anterior surface of the rectal
The prostate (see Figs. 7.4 and 7.16) is
Posteriorly:
(see Fig. 7.4).
puboprostatic ligaments
nected to the posterior aspect of the pubic bones by the
The prostate is con
(cave of Retzius).
retropubic space
extraperitoneal fat
pubis, separated from it by the
The prostate is related to the symphysis
Anteriorly:
(see Fig. 7.16).
the prostate just above the apex on the anterior surface
surface of the urogenital diaphragm. The urethra leaves
The apex of the prostate lies on the upper
Inferiorly:
Fig. 7.4).
urethra enters the center of the base of the prostate (see
openings of the ejaculatory ducts on the margin of the prostatic utricle.
and horizontal section
sagittal section
(A),
(B),
(C). In the coronal section, note the
■
■
■
■
in the
-
fascial
■
■
-
■
■
-
Basic Anatomy
ous vesical veins and drains into the internal iliac veins.
plexus receives the deep dorsal vein of the penis and numer
side the capsule of the prostate (see Fig. 7.16). The prostatic
which lies out
prostatic venous plexus,
The veins form the
Veins
Branches of the inferior vesical and middle rectal arteries.
Arteries
tralize the acidity in the vagina.
urethra. The prostatic secretion is alkaline and helps neu
rounds the glands, squeezes the secretion into the prostatic
at the time of ejaculation. The smooth muscle, which sur
acid and acid phosphatase that is added to the seminal fluid
The prostate produces a thin, milky fluid containing citric
Function of the Prostate
of the prostate. The lateral lobes contain many glands.
another by a shallow vertical groove on the posterior surface
lie on either side of the urethra and are separated from one
left lateral lobes
right
contains glandular tissue. The
behind the urethra and below the ejaculatory ducts and also
is situated
posterior lobe
the bladder; it is rich in glands. The
ejaculatory ducts. Its upper surface is related to the trigone of
is the wedge of gland situated between the urethra and the
middle, lobe
or
median,
is devoid of glandular tissue. The
ulate the smooth muscle of the prostate during ejaculation.
Inferior hypogastric plexuses. The sympathetic nerves stim
Nerve Supply
Internal iliac nodes.
Lymph Drainage
277
-
and
-
-
Blood Supply
-
-
Prostate Examination
prostate. Cancer cells enter the skull via this route by floating up
vertebral veins exist. During coughing and sneezing or abdomi
Many connections between the prostatic venous plexus and the
are valveless, and are drained by several large trunks directly
adds to the patient’s
(Fig. 7.17). The stagnant urine frequently becomes infected,
stagnant urine behind the urethral orifice within the bladder
enlarged median lobe) results in the formation of a pouch of
plication. The enlargement of the uvula vesicae (owing to the
culty in passing urine and the stream is weak. Back-pressure
the gland produces elongation and lateral compression and
micturate. The enlargement of the median and lateral lobes of
into the prostatic urethra causes an intense reflex desire to
cae, located at the neck of the bladder. The leakage of urine
hormonal control of the gland. The median lobe of the gland
than 50 years. The cause is possibly an imbalance in the
Benign enlargement of the prostate is common in men older
tate, this protein appears in the blood in increased amounts. The
It has been shown that trace amounts of proteins produced
producing this enzyme cannot discharge their secretion into the
The prostate can be examined clinically by palpation by perform-
ing a rectal examination (see page 311). The examiner’s gloved
finger can feel the posterior surface of the prostate through the
anterior rectal wall.
Prostate Activity and Disease
It is now generally believed that the normal glandular activity of
the prostate is controlled by the androgens and estrogens cir-
culating in the bloodstream. The secretions of the prostate are
poured into the urethra during ejaculation and are added to the
seminal fluid. Acid phosphatase is an important enzyme pres-
ent in the secretion in large amounts. When the glandular cells
ducts, as in carcinoma of the prostate, the serum acid phospha-
tase level of the blood rises.
specifically by prostatic epithelial cells are found in peripheral
blood. In certain prostatic diseases, notably cancer of the pros-
specific protein level can be measured by a simple laboratory
test called the PSA test.
Benign Enlargement of the Prostate
enlarges upward and encroaches within the sphincter vesi-
distortion of the urethra so that the patient experiences diffi-
effects on the ureters and both kidneys are a common com-
and the inflamed bladder (cystitis)
symptoms.
In all operations on the prostate, the surgeon regards the
prostatic venous plexus with respect. The veins have thin walls,
into the internal iliac veins. Damage to these veins can result in
a severe hemorrhage.
Prostate Cancer and the Prostatic Venous Plexus
-
nal straining, it is possible for prostatic venous blood to flow in a
reverse direction and enter the vertebral veins. This explains the
frequent occurrence of skeletal metastases in the lower verte-
bral column and pelvic bones of patients with carcinoma of the
the valveless prostatic and vertebral veins.
C L I N I C A L N O T E S
enlarged median lobe of prostate
bladder wall
ejaculatory duct
posterior lobe
urethra
sphincter
vesicae
pouch of
stagnant urine
FIGURE 7.17
Sagittal section of a prostate that had under
der pouch filled with stagnant urine behind the prostate.
-
gone benign enlargement of the median lobe. Note the blad-
278
CHAPTER 7
lateral to the lateral fornix of the vagina, to enter the bladder.
artery (Figs. 7.18 and 7.19). The ureter then runs forward,
of the broad ligament, where it is crossed by the uterine
spine. It then turns forward and medially beneath the base
behind the ovary until it reaches the region of the ischial
ward and backward in front of the internal iliac artery and
cation of the common iliac artery (Fig. 7.18). It runs down
The ureter crosses over the pelvic inlet in front of the bifur
sections.
the pelvic cavity in the female are described in the following
as described previously. The contents of the anterior part of
occupy the posterior part of the pelvic cavity (see Fig. 7.5),
The rectum, sigmoid colon, and terminal coils of ileum
Pelvic Viscera in the Female
directly in contact with the abdominal wall.
the anterior abdominal wall so that the bladder becomes
up into the abdomen and peels off the peritoneum from
to remember that as the bladder fills, the superior wall rises
not cover the lateral surfaces of the bladder. It is important
bladder passes laterally to the lateral pelvic walls and does
The peritoneum covering the superior surface of the
the erect position, is the rectovesical pouch (see Fig. 7.4).
abdominopelvic peritoneal cavity, when the patient is in
abdominal wall. It is thus seen that the lowest part of the
continuous with the parietal peritoneum on the posterior
surfaces of the upper third of the rectum. It then becomes
the middle third of the rectum and the front and lateral
The peritoneum then passes up on the front of
pouch.
rectovesical
aspect of the rectum, forming the shallow
nal vesicles. Here, it sweeps backward to reach the anterior
a short distance until it reaches the upper ends of the semi
then runs down on the posterior surface of the bladder for
nal wall onto the upper surface of the urinary bladder. It
The peritoneum passes down from the anterior abdomi
pelvis in a sagittal plane (see Fig. 7.4).
The peritoneum is best understood by tracing it around the
covers and supports the pelvic viscera (see Fig.7.16).
The visceral pelvic fascia is a layer of connective tissue that
Visceral Pelvic Fascia
openings of the two ejaculatory ducts (see Fig. 7.16).
in females. On the edge of the mouth of the utricle are the
which is an analog of the uterus and vagina
static utricle,
pro
the summit of the urethral crest is a depression, the
the prostatic glands open into these grooves. On
sinus;
prostatic
On each side of this ridge is a groove called the
(see Fig. 7.16).
urethral crest
longitudinal ridge called the
On the posterior wall is a
portion of the entire urethra.
prostatic urethra is the widest and most dilatable
The
with the membranous part of the urethra (see Fig. 7.16).
tate from the base to the apex, where it becomes continuous
begins at the neck of the bladder. It passes through the pros
The prostatic urethra is about 1.25 in. (3 cm) long and
The Pelvis: Part II—The Pelvic Cavity
Prostatic Urethra
-
-
Peritoneum
-
-
Ureters
-
-
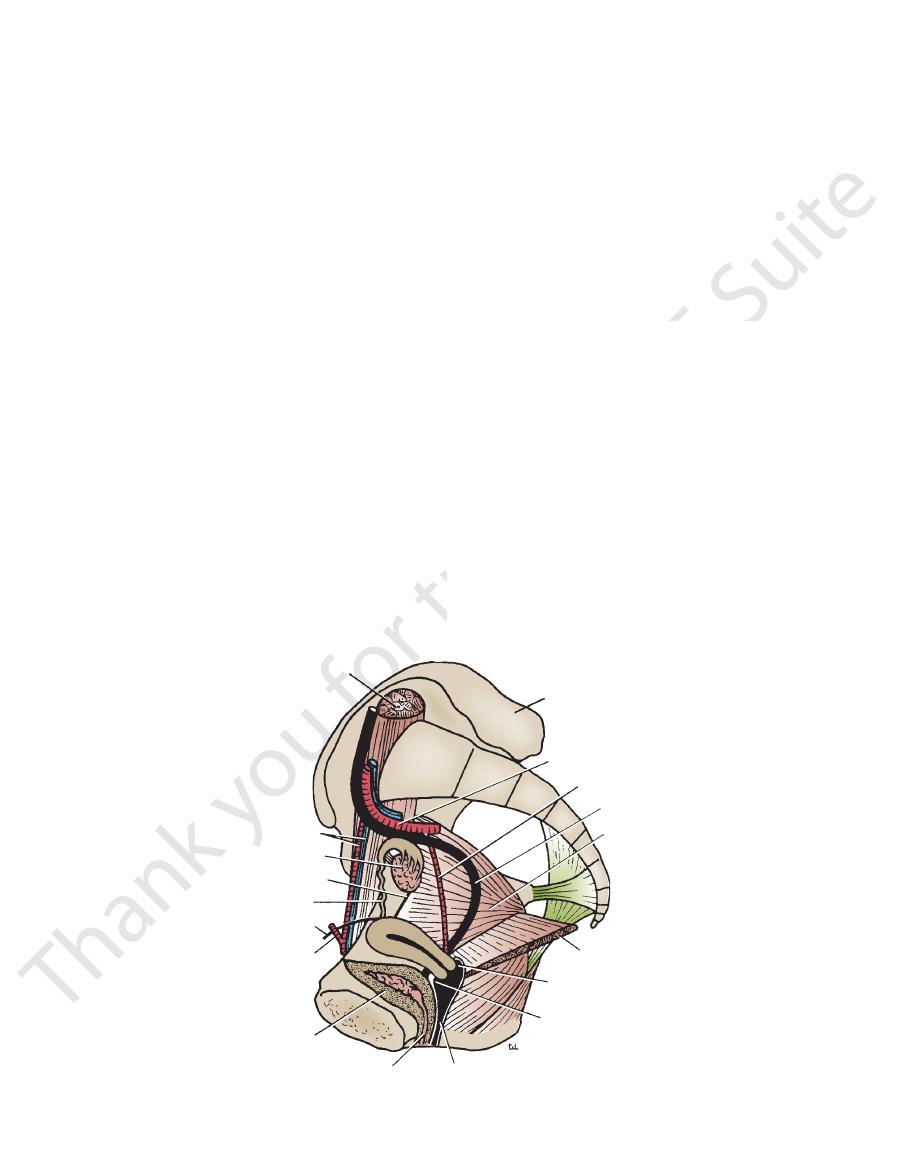
psoas
ilium
internal iliac artery
uterine artery
ureter
obturator internus
levator ani
posterior fornix
anterior fornix
vagina
bladder
inferior epigastric artery
round ligament of uterus
uterine tube
round ligament of ovary
ovary
external iliac vessels
urethra
FIGURE 7.18
y, the uterine tube, and the vagina.
Right half of the pelvis showing the ovar
