Basic Anatomy
303
natomy
asic
B
a
Definition of Perineum
their covering fasciae (see Fig. 8.1). It is incomplete
tores ani muscles and the small coccygeus muscles and
The pelvic diaphragm is formed by the important leva
and laterally by the ischial tuberosities (Fig. 8.2).
by the symphysis pubis, posteriorly by the tip of the coccyx,
the perineum is diamond shaped and is bounded anteriorly
(Fig. 8.1). When seen from below with the thighs abducted,
into the main pelvic cavity above and the perineum below
The cavity of the pelvis is divided by the pelvic diaphragm
Pelvic Diaphragm
-
anteriorly to allow passage of the urethra in males and
inguinal nodes.
of the skin drain into the medial group of the superficial
the inferior rectal (hemorrhoidal) nerve. The lymph vessels
ischiorectal fossa. The skin around the anus is supplied by
the anal canal, lies in the midline, and on each side is the
or lower opening of
anus,
maximus muscle (Fig. 8.3). The
tuberous ligament, overlapped by the border of the gluteus
cyx and on each side by the ischial tuberosity and the sacro
The anal triangle is bounded behind by the tip of the coc
Contents of Anal Triangle
page 247).
the urethra and the vagina in females (for details see
-
-
C H A P T E R O B J E C T I V E S
■
■
Infections, injuries, and prolapses involving the anal canal, the
urethra, and the female external genitalia are common problems
facing the physician.
■
■
Urethral obstruction, traumatic rupture of the penile urethra,
and infections of the epididymis and testis are frequently seen
in the male.
■
■
The purpose of this chapter is to cover the significant anatomy
relative to these clinical problems. Because the descent of the
testes and the structure of the scrotum are intimately related
to the development of the inguinal canal, they are dealt with in
detail in Chapter 4.
region of
main pelvic
cavity
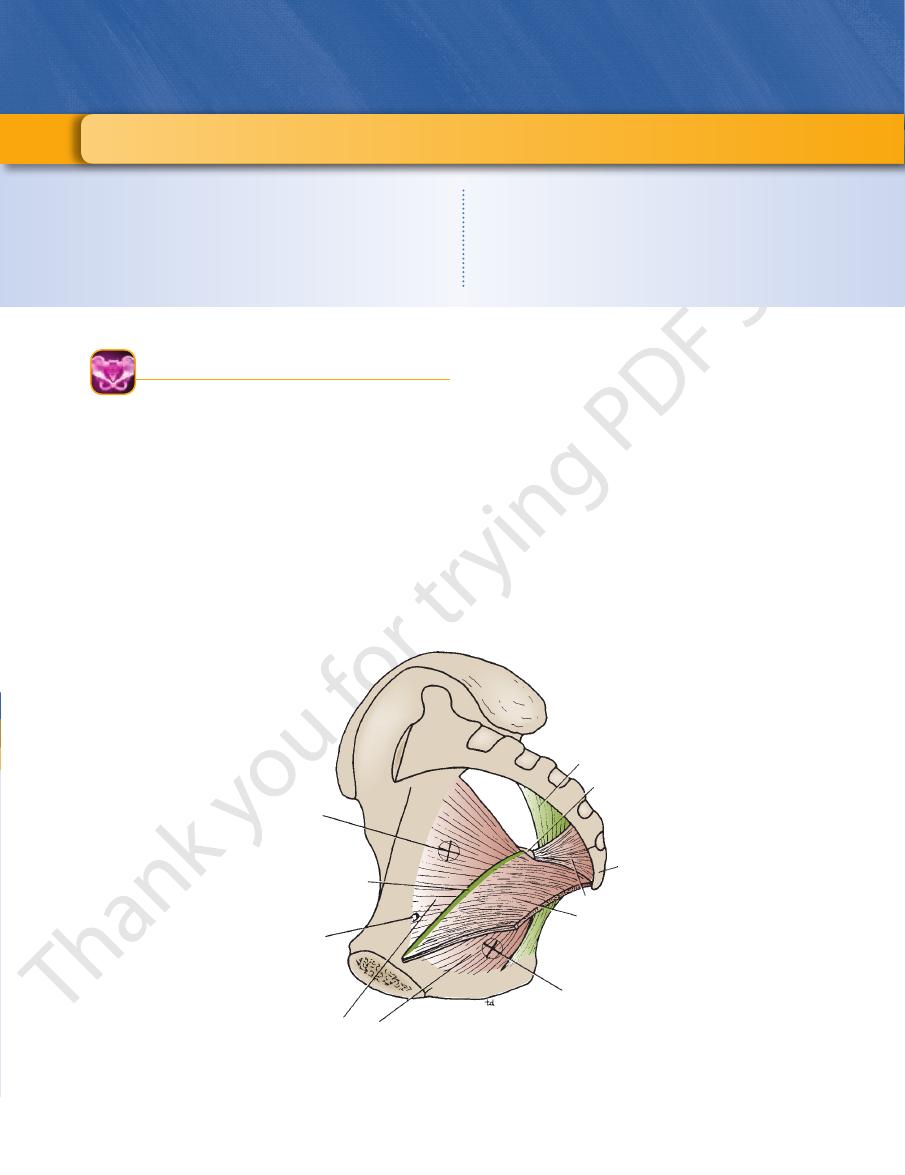
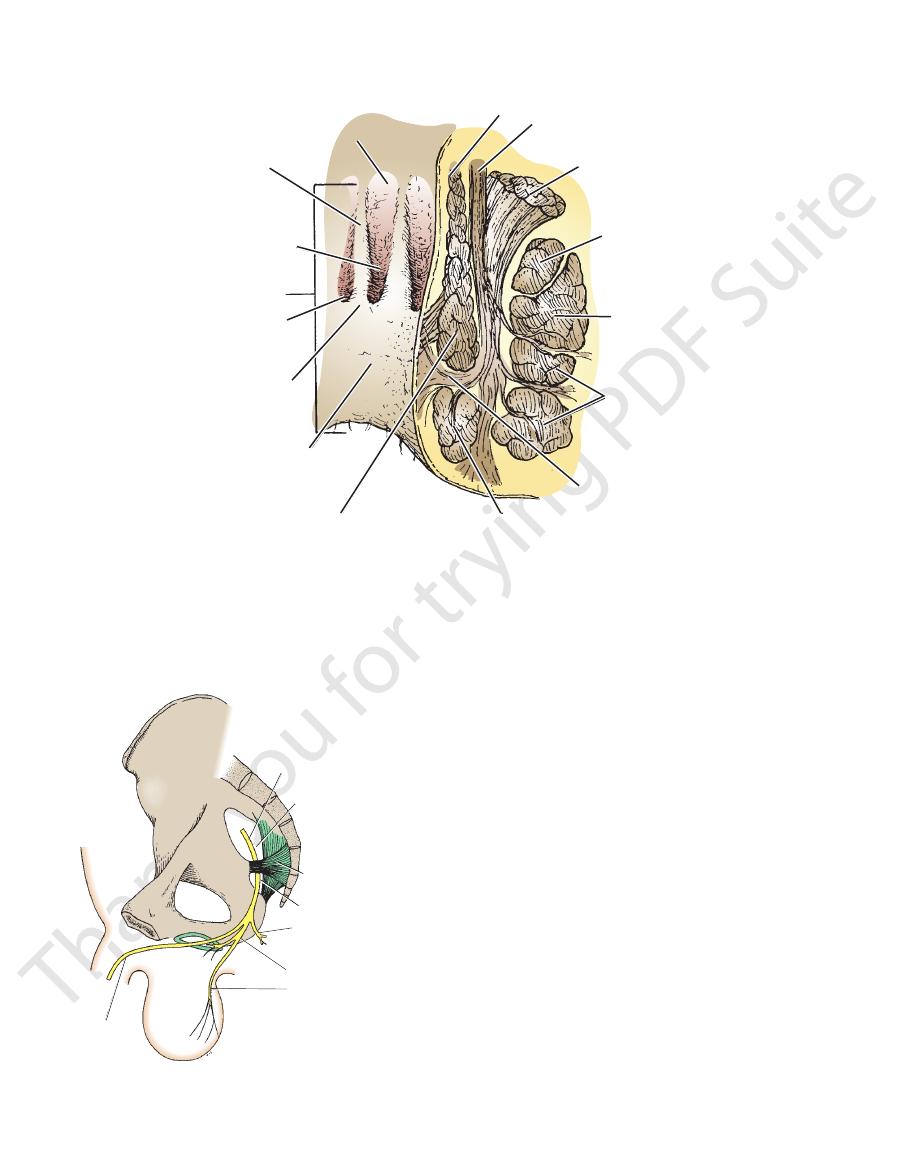
linear thickening
of fascia covering
obturator internus
muscle
obturator canal
for obturator
nerve and
vessels
obturator
internus muscle
region of
perineum
levator ani
muscle
coccyx
coccygeus muscle
ischial spine
sacrotuberous
ligament
FIGURE 8.1
vator ani and the coccygeus
Right half of the pelvis showing the muscles forming the pelvic floor. Note that the le
the pelvic diaphragm and the region of the perineum lies below the diaphragm.
muscles and their covering fascia form the pelvic diaphragm. Note also that the region of the main pelvic cavity lies above

304
CHAPTER 8
The Perineum
urogenital
triangle
anal
triangle
FIGURE 8.2
Diamond-shaped perineum divided by a broken
line into the urogenital triangle and the anal triangle.
symphysis pubis
perineal body
ischial tuberosity
inferior rectal artery
anococcygeal body
tip of coccyx
gluteus maximus muscle
subpubic ligament
urethra
inferior ramus of pubis
urogenital diaphragm
external anal sphincter
levator ani
inferior rectal nerve
sacrotuberous ligament
FIGURE 8.3
Anal triangle and urogenital triangle in the male as seen from below.
downward and backward from the rectal ampulla to the
The anal canal is about 1.5 in. (4 cm) long and passes
Location and Description
teric artery (see Fig. 8.6). The venous drainage is mainly
superior rectal artery, a branch of the inferior mesen
The arterial supply is that of the hindgut—namely, the
It is sensitive only to stretch (see Fig. 8.6).
and is derived from the autonomic hypogastric plexuses.
The nerve supply is the same as that for the rectal mucosa
deal membrane) (Figs. 8.5 and 8.7).
(remains of procto
anal valves
semilunar folds called
which are joined together at their lower ends by small
anal columns,
It is thrown into vertical folds called
It is lined by columnar epithelium.
lowing important anatomic features:
is derived from hindgut entoderm (Fig. 8.6). It has the fol
mucous membrane of the upper half of the anal canal
The
Structure
part of the vagina (see Fig. 8.4).
perineal body, the urogenital diaphragm, and the lower
the bulb of the penis (see Fig. 8.4). In the female, the
tal diaphragm, the membranous part of the urethra, and
In the male, the perineal body, the urogeni
Anteriorly:
The fat-filled ischiorectal fossae (Fig. 8.5).
Laterally:
cyx (see Fig. 8.4).
fibrous tissue lying between the anal canal and the coc
which is a mass of
anococcygeal body,
Posteriorly: The
anal sphincters.
are kept in apposition by the levatores ani muscles and the
anus (Fig. 8.4). Except during defecation, its lateral walls
Relations
■
■
-
■
■
■
■
-
-
■
■
■
■
-
■
■
■
■
-
Anal Canal
Basic Anatomy
305
penile urethra
fossa terminalis
external urethral orifice
urogenital diaphragm
bulb of penis
lves
bladder
prostate
puborectalis
anococcygeal body
anal canal
anal va
perineal body
prepuce
body of penis
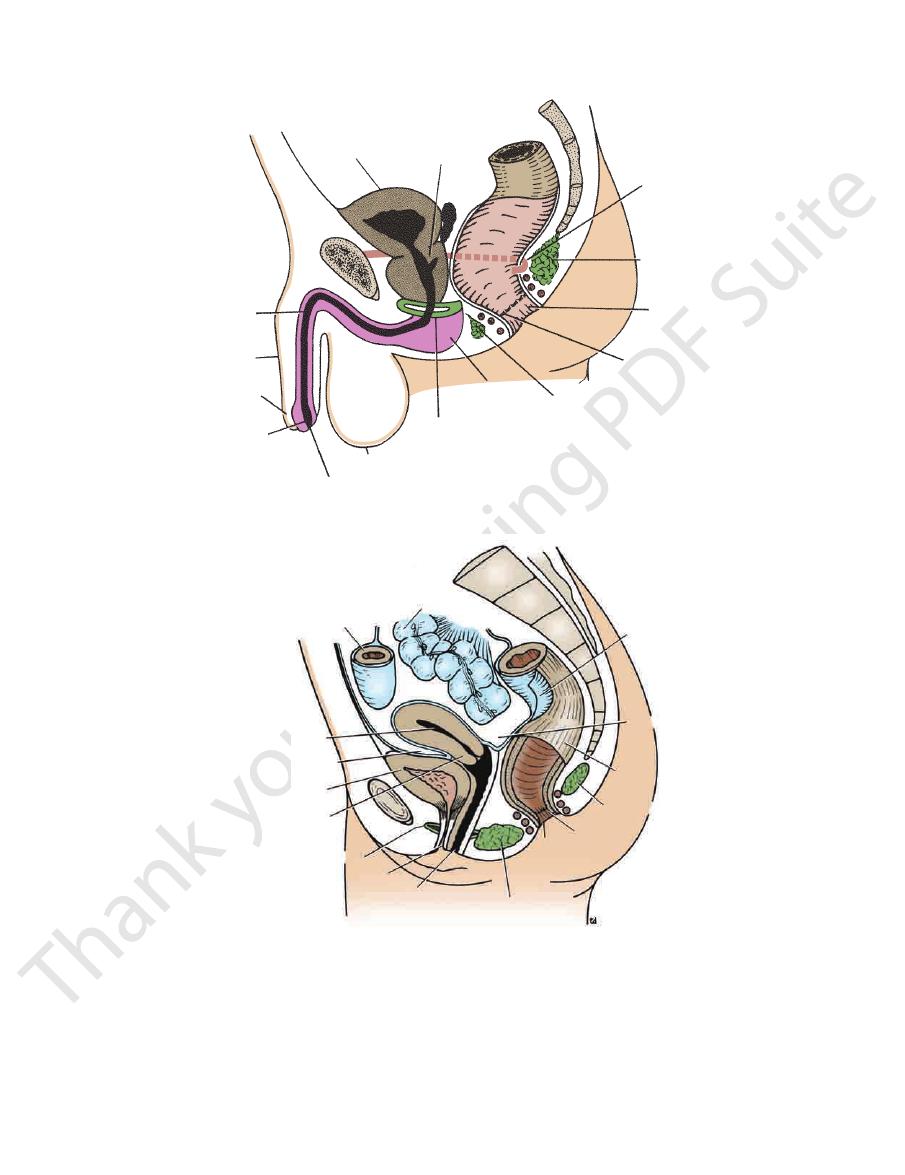
rectouterine pouch
perineal body
vagina
urethra
cervix
bladder
cavity of uterus
A
sigmoid colon
coil of ileum
uterovesical pouch
urogenital diaphragm
anus
anal canal
anococcygeal body
rectum
peritoneum
S3
B
FIGURE 8.4
Sagittal sections of the male (
mis (see Fig. 8.6).
gradually merges at the anus with the perianal epider
It is lined by stratified squamous epithelium, which
lowing important features:
is derived from ectoderm of the proctodeum. It has the fol
mucous membrane of the lower half of the anal canal
The
Fig. 8.6).
then eventually to the inferior mesenteric nodes (see
superior rectal artery to the pararectal nodes and
The lymphatic drainage is mainly upward along the
mesenteric vein, and the portal vein (see Fig. 8.5).
by the superior rectal vein, a tributary of the inferior
) pelvis. Sagittal sections of the female (
A
B) pelvis.
■
■
-
■
■
-
306
CHAPTER 8
The Perineum
superficial
inferior rectal vein
superior rectal vein
lower transverse fold of rectum
middle rectal vein
obturator internus
levator ani
pudendal canal
puborectalis
deep
external
sphincter
subcutaneous
internal sphincter
anus
anal valve
anal column
fat in ischiorectal fossa
internal
pudendal
vessels
pudendal nerve
rectum
longitudinal muscle
ischium
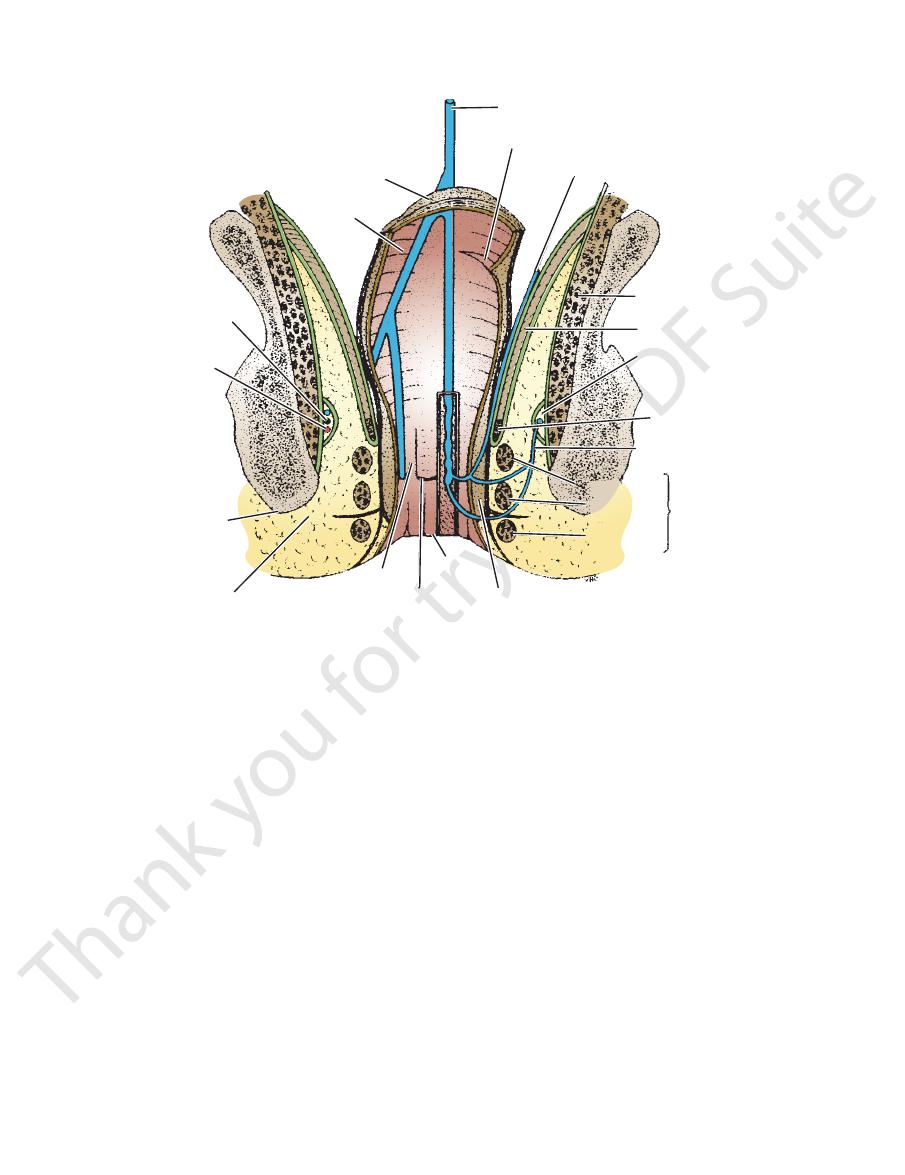
FIGURE 8.5
Coronal section of the pelvis and the perineum showing venous drainage of the anal canal.
At the junction of the rectum and anal canal
skin (see Fig. 8.5).
into the ischiorectal fossa or are attached to the perianal
membrane of the anal canal, whereas others pass laterally
Some of the longitudinal fibers are attached to the mucous
interval between the internal and external anal sphincters.
tinuous coat around the anal canal and descends in the
continuous above with that of the rectum. It forms a con
The longitudinal smooth muscle of the anal canal is
canal, pulling the two forward at an acute angle (see Fig. 8.6).
and passes around the junction of the rectum and the anal
form a sling, which is attached in front to the pubic bones
8.5, 8.6, and 8.7). The puborectalis fibers of the two sides
blend with the deep part of the external sphincter (see Figs.
fibers of the two levatores ani muscles
puborectalis
The
canal and has no bony attachments
which encircles the upper end of the anal
deep part,
behind and the perineal body in front
which is attached to the coccyx
superficial part,
the anal canal and has no bony attachments
which encircles the lower end of
subcutaneous part,
can be divided into three parts:
external sphincter
The
sphincter (see Figs. 8.5, 8.6, and 8.7).
sheath of striped muscle that forms the voluntary external
of the anal canal. The internal sphincter is enclosed by a
the smooth muscle of the circular coat at the upper end
is formed from a thickening of
internal sphincter
The
voluntary external sphincter.
The anal canal has an involuntary internal sphincter and a
Anal Sphincters
muscle (see Fig. 8.5).
an outer longitudinal and an inner circular layer of smooth
As in the upper parts of the intestinal tract, it is divided into
of the anal canal joins the lower half (see Fig. 8.7).
indicates the level where the upper half
pectinate line
The
superficial inguinal nodes (see Fig. 8.6).
The lymph drainage is downward to the medial group of
iliac vein (see Figs. 8.5 and 8.6).
internal pudendal vein, which drains into the internal
drainage is by the inferior rectal vein, a tributary of the
of the internal pudendal artery (see Fig. 8.3). The venous
The arterial supply is the inferior rectal artery, a branch
and pressure (see Figs. 8.3 and 8.6).
nerve; it is thus sensitive to pain, temperature, touch,
The nerve supply is from the somatic inferior rectal
anal columns (see Fig. 8.7).
There are
■
■
no
■
■
■
■
■
■
Muscle Coat
■
■
A
■
■
A
■
■
A
-
(see Fig.
rnal sphincter, the deep part of the
8.6), the inte
on rectal examination.
which can be felt
anorectal ring,
distinct ring, called the
external sphincter, and the puborectalis muscles form a
Basic Anatomy
307
columnar epithelium
sensitive to stretch
entoderm
sensitive to pain,
touch, and temperature
stratified squamous epithelium
superior rectal artery
inferior rectal artery
superior rectal vein
inferior rectal vein
pararectal lymph nodes
along superior
rectal artery
superficial inguinal
lymph nodes
rectum
deep
coccyx
anococcygeal body
superficial
subcutaneous
anal canal
perineal body
puborectalis
A
B
C
D
E
ectoderm
anus
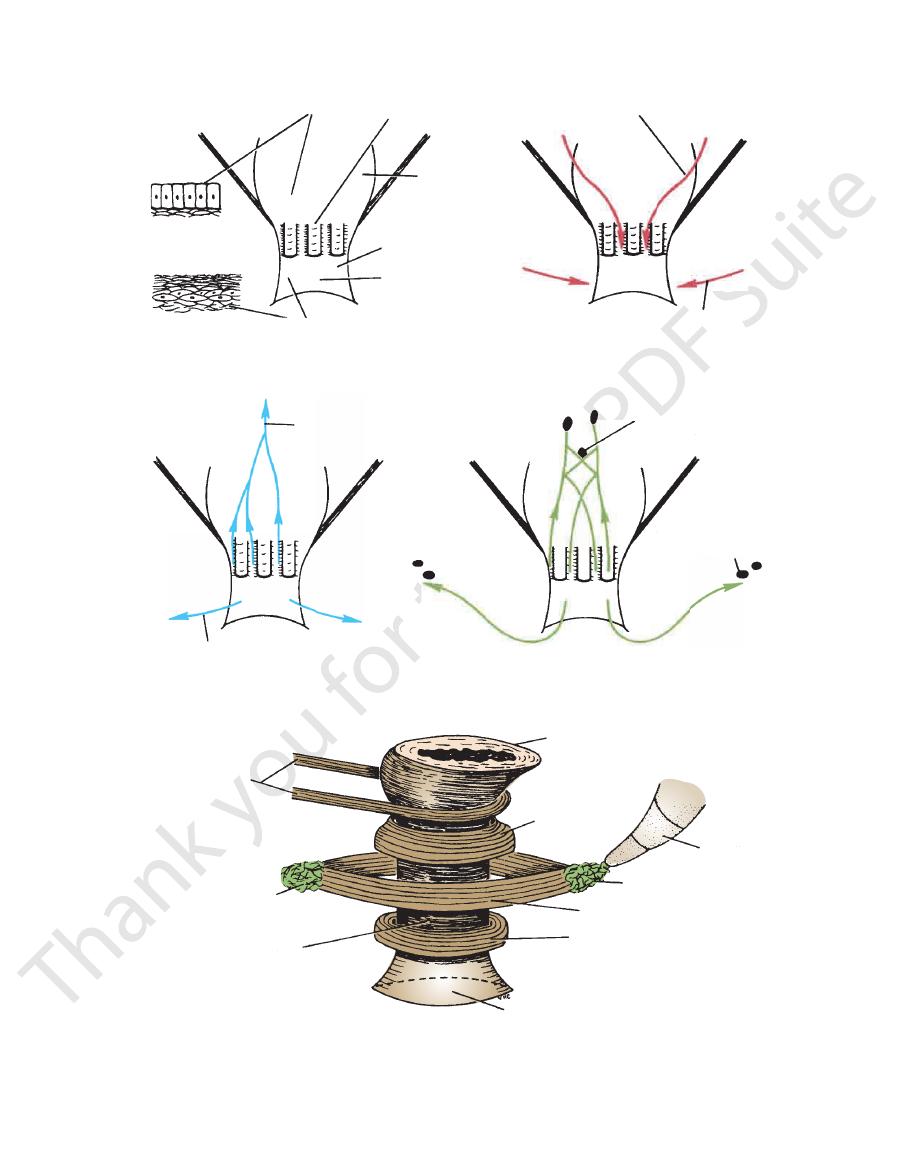
FIGURE 8.6
wing their embryologic origin and lining epithelium (
Upper and lower halves of the anal canal sho
muscle and different parts of the external anal sphincter (
). Arrangement of the muscle fibers of the puborectalis
), their venous drainage (
A), their arterial
supply (B
C), and their lymph drainage (D
E).
308
CHAPTER 8
The Perineum
anal column
anal sinus
anal canal
(1.5 in. long)
anal valve
pectinate line
pecten
or transitional
zone
internal
sphincter
of anal canal
intersphincteric
plane
superficial part
of external
sphincter of
anal canal
deep part of
external sphincter
of anal canal
puborectalis
levator ani
muscle
longitudinal muscle of
rectum
circular muscle of rectum
rectal ampulla
subcutaneous part
of external
sphincter of
anal canal
FIGURE 8.7
Coronal section of the anal canal showing the detailed anatomy of the mucous membrane and the arrangement
“pecten” (the transitional zone between the skin and the mucous membrane) are sometimes used by clinicians.
of the internal and external anal sphincters. Note that the terms “pectinate line” (the line at the level of the anal valves) and
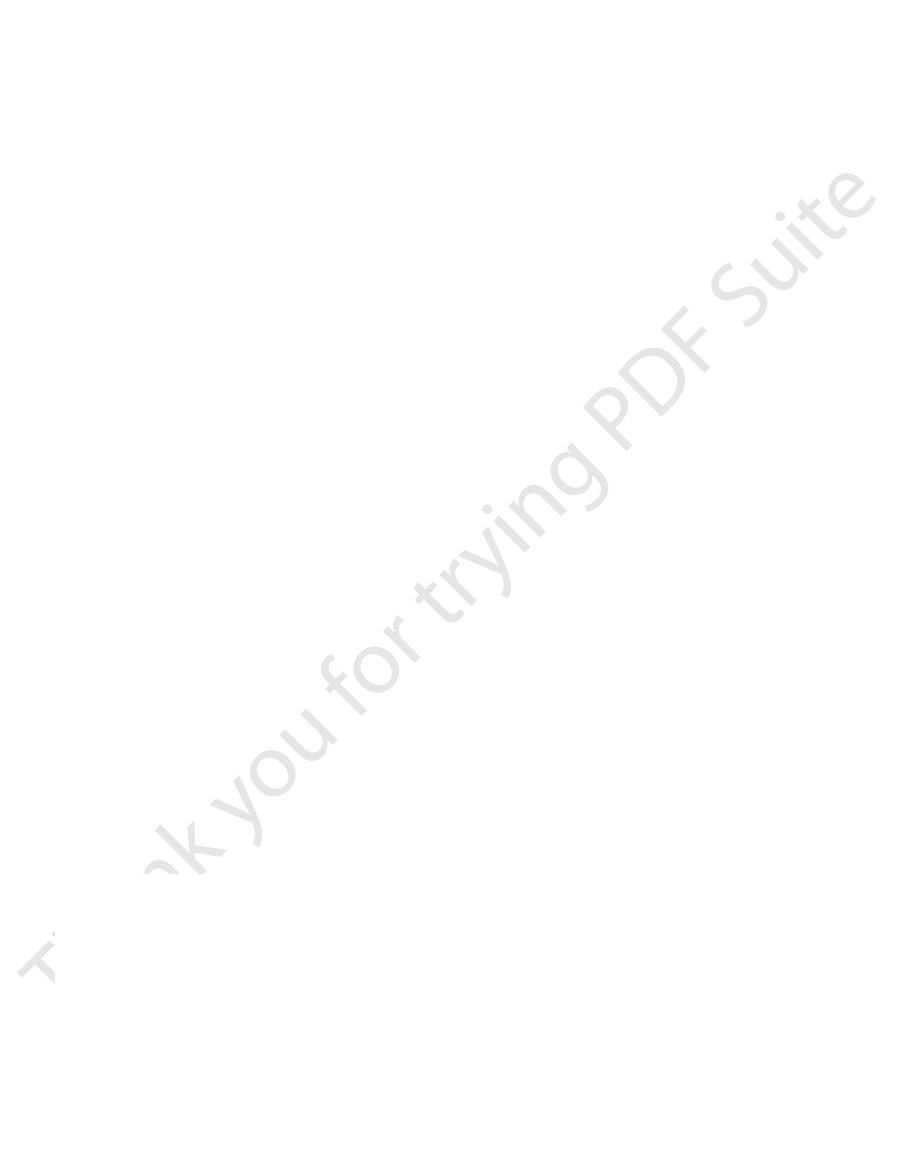
pudendal nerve
greater sciatic foramen
lesser sciatic foramen
inferior rectal nerve
dorsal nerve
of penis
perineal nerve
scrotal nerves
sacrospinous ligament
FIGURE 8.8
Course and branches of the pudendal nerve in
internal sphincter is supplied by sympathetic fibers from
innervated by the inferior rectal nerves. The involuntary
sitive to pain, temperature, touch, and pressure and is
through the hypogastric plexuses. The lower half is sen
stretch and is innervated by sensory fibers that ascend
The mucous membrane of the upper half is sensitive to
Nerve Supply
nodes (see Fig. 8.6).
half drains into the medial group of superficial inguinal
nodes and then the inferior mesenteric nodes. The lower
The upper half of the anal canal drains into the pararectal
Lymph Drainage
vein.
by the inferior rectal vein into the internal pudendal
the inferior mesenteric vein, and the lower half is drained
The upper half is drained by the superior rectal vein into
Veins
artery supplies the lower half (see Fig. 8.6).
The superior artery supplies the upper half and the inferior
Arteries
the male.
Blood Supply
-
Basic Anatomy
309
the inferior hypogastric plexuses. The voluntary external
arch and laterally by the ischial tuberosities (see Fig. 8.3).
The urogenital triangle is bounded in front by the pubic
Urogenital Triangle
spond to the branches of the internal pudendal artery.
The internal pudendal vein receives tributaries that corre
Internal Pudendal Vein
in the female.
clitoris
to the labia and
Branches to the penis
anal canal (see Fig. 8.3).
This supplies the lower half of the
Inferior rectal artery:
Branches
sciatic foramen.
sciatic foramen and enters the perineum through the lesser
iliac artery and passes from the pelvis through the greater
The internal pudendal artery is a branch of the internal
Internal Pudendal Artery
surface of the scrotum (or labia majora).
ital triangle (see Fig. 8.8) and the skin on the posterior
This supplies the muscles in the urogen
Perineal nerve:
uted to the penis (or clitoris) (see Fig. 8.8).
This is distrib
Dorsal nerve of the penis (or clitoris):
canal, and the perianal skin (see Fig. 8.3).
ter, the mucous membrane of the lower half of the anal
ischiorectal fossa and supplies the external anal sphinc
This runs medially across the
Inferior rectal nerve:
Branches
anal sphincter and the muscles and skin of the perineum.
canal and, by means of its branches, supplies the external
atic foramen. The nerve then passes forward in the pudendal
the lower limb, it enters the perineum through the lesser sci
men (see Fig. 8.8). After a brief course in the gluteal region of
leaves the main pelvic cavity through the greater sciatic fora
The pudendal nerve is a branch of the sacral plexus and
Pudendal Nerve
vessels and nerve cross the fossa to reach the anal canal.
the ischial tuberosity (Figs. 8.5 and 8.8). The inferior rectal
lateral wall of the ischiorectal fossa, on the medial side of
on the
pudendal canal,
embedded in a fascial canal, the
tion. The pudendal nerve and internal pudendal vessels are
ports the anal canal and allows it to distend during defeca
The ischiorectal fossa is filled with dense fat, which sup
Contents of Fossa
muscle, covered with pelvic fascia.
wall is formed by the lower part of the obturator internus
sloping levator ani muscle and the anal canal. The lateral
medial and lateral walls. The medial wall is formed by the
The edge of the wedge is formed by the junction of the
The base of the wedge is superficial and formed by the skin.
space located on each side of the anal canal (see Fig. 8.5).
The ischiorectal fossa (ischioanal fossa) is a wedge-shaped
now closed by the tonic contraction of the anal sphincters.
puborectalis muscle. The empty lumen of the anal canal is
the anal walls and the contraction and upward pull of the
to the anal canal by the tone of the longitudinal fibers of
fecal mass. At the end of the act, the mucosa is returned
of the anal canal is extruded through the anus ahead of the
submucous coat, the mucous membrane of the lower part
ated through the anal canal. Depending on the laxity of the
cles, is now voluntarily inhibited, and the feces are evacu
external anal sphincters, including the puborectalis mus
abdominal wall. The tonic contraction of the internal and
about by contraction of the muscles of the anterior
It is assisted by a rise in intra-abdominal pressure brought
descending colon, sigmoid colon, rectum, and anal canal.
a coordinated reflex that results in the emptying of the
ence of feces in the lumen. The act of defecation involves
stretch receptors in the wall of the rectum by the pres
The desire to defecate is initiated by stimulation of the
once in several days.
eral times a day, and some perfectly normal people defecate
habit. Some adults defecate once a day, some defecate sev
The time, place, and frequency of defecation are a matter of
of the fourth sacral nerve.
of the pudendal nerve (see Fig. 8.3), and the perineal branch
sphincter is supplied by the inferior rectal nerve, a branch
Defecation
-
-
-
-
Ischiorectal Fossa
-
-
-
-
■
■
-
■
■
-
■
■
-
■
■
■
■
in the male and
-
Portal–Systemic Anastomosis
anal columns at the 3-, 7-, and 11-o’clock positions when the
membrane (Fig. 8.9). The tributaries of the vein, which lie in the
superior rectal (hemorrhoidal) vein and are covered by mucous
Internal hemorrhoids are varicosities of the tributaries of the
The rectal veins form an important portal–systemic anastomo-
sis because the superior rectal vein drains ultimately into the
portal vein and the inferior rectal vein drains into the systemic
system.
Internal Hemorrhoids (Piles)
C L I N I C A L N O T E S
(continued)
