32
Lec. 7 Metabolism of iodine
1. Iodine is one of the most important essential trace elements.
2. Involved in the synthesis of thyroid hormones.
3. Total body contact of iodine is 10-20 mg.
4. Daily requirement are about 0.2 mg/day.
Absorption and metabolism
1) Iodine in the diet is mainly inorganic iodide.
2) Absorbed in stomach & small intestine and transported in the plasma by plasma
proteins.
3) Then removed from circulation by the thyroid gland and kidneys.
4) The thyroid gland contains about 90% of the iodine in the body.
5) Iodide is used by the thyroid gland for the synthesis of thyroxin (T4) and a small
amount of tri-iodothronin (T3).
6) Thyroid hormones affect absorption.
Sources of iodine
1) Sea foods. 2) Milk & dairy products. 3) Iodized salt.
The thyroid gland
90% of total body iodine is in the thyroid gland
The thyroid gland is composed of two lobes. Connected by a thin band of tissue
(the isthmus). Which gives the gland the appearance of a butterfly. It is closely
attached to the trachea in the anterior aspect of the neck.
Each lobe measures 2-2.5 cm thickness and about 4 cm length.
The secretary units of the thyroid gland are called follicles, that consist of a layer
of epithelial cells, these cells rest on a basement membrane and enclose an
amorphous material called: colloid.
(Which is composed of a thyroglobulin) (Iodide glycoprotein).
The functional unit of the thyroid gland is called the follicle
Follicular cells are able to concentrate iodide to: 30 or 40 times that of the normal
plasma levels.
By means of energy dependent mechanism, and even reaches 850 times that of the
plasma after stimulation of the gland by the: Thyroid stimulating hormones (TSH)
thyrotropine.
The synthesis of thyroid hormones
There are 4 stages in the synthesis of T4 and T3 and their release from the
thyroid gland:
1) The first is: the trapping of the iodide from the plasma by the thyroid follicles.
2) The second is: The oxidation of iodide to iodine.
3) Incorporation of iodine into thyroglobulin to form: mono and di-iodotyrosines.
33
4) Formation of tri-iodothyronine (T3). By the combination of mono & di- iodotyrosine.
5) Formation of tetra-iodothyronine (T4). By the combination of two di-iodotyrosines.
6) Splitting of T3, and T4 from thyroglobulin and release in the circulation.
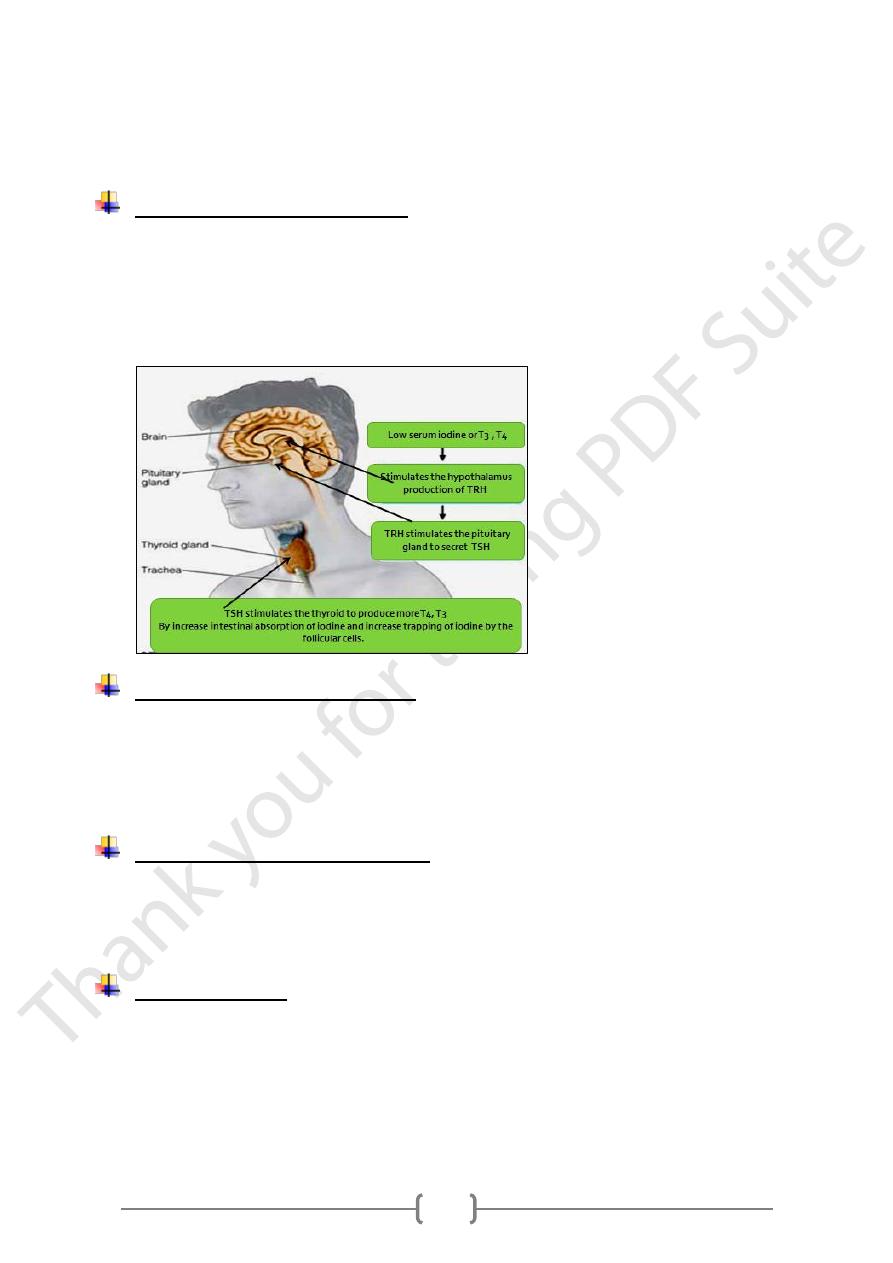
Secretion of thyroid hormones
The secretion of thyroid hormones is under the control of coordinated feedback
mechanism exists among the thyroid, pituitary gland and the hypothalamus.
Serum conc. of T3, T4 stimulate: The hypothalamus: to produces thyrotropine
releasing hormone TRH.
TRH stimulates the pituitary to secrete TSH.
The thyroid gland secrets T4 and T3.
Transport of thyroid hormones
Thyroid hormones transported in plasma, entirely bound to plasma proteins.
About 99.95% of T4 and 99.50% of T3: are protein-bound in plasma. Thyroxin
binding globulin (TBG): is the most important of these proteins: It binds 70% of
T4 and 80% of T3 in the blood. Only the free hormones can cross cell membranes
and affect intracellular metabolism.
Metabolism of thyroid hormones
1) Is by deiodination and oxidative deamination.
2) Iodine released into the circulation, is mostly taken up again by thyroid and re- used.
3) Other metabolites are conjugated in the liver and excreted in bile.
4) Some amounts of un metabolized T4, T3 are excreted unchanged in urine.
Iodine deficiency
A. Goiter (less severe): Enlarged thyroid gland due iodine deficiency in attempt to
increase thyroid hormone production.
B. Cretinism (more severe): Severe iodine deficiency during Pregnancy leads to serious
problems in baby: Stunted growth, deaf, mentally retarded.
C. Hypothyroidism in adults.
Simple goiter
