1
Lec.1 Pediatric
6
th
stage
session notes
د
.
ندى
Edema:
Is it truly edema or not?
It may be due to steroid, allergy, or other causes.
Is this edema localized or generalized
If it’s generalized the most common cause →nephritic syndrome especially if there
is peri-orbital edema.
Then→ protein losing enteropathy → cardiac → liver
Pathophysiology :
↑ hydrostatic pressure
o Acute nephritic syndrome.
o Congestive cardiac failure (CHF)
↓ plasma oncotic pressure
o Protein energy malnutrition (PEN), Nephrotic syndrome and protein
loosing enteropathy.
↑ capillary leakage
o Allergy, sepsis, angioedema.
Impaired venous flow
o Venacaval obstruction, hepatic vein obstruction.
Impaired lymphatic flow
o Congenital lymphedema, Wuchereria bancrofti infection (elphantaiasis)
The most common cause of
nephrotic syndrome in children
is →Minimal change nephropathy

2
Clinical approach to edema :
renal :
Periorbital edema, history of collagen vascular disesase (SLE, RA, rash, joint
pain frothy urine due to protein)
Cardiac: Ask about:
-Palpitation: if the child is > 3 year
- Fainting, bluish episode (TOF).
Hepatic:
Jaundice, umbilical infection (omphalitis) → neonatal sepsis.
_________________________________
Sign of adequacy of breast milk intake:
1. Urine output: a well-hydrated infant voids six to eight times a day. Each
voiding should soak, not merely moisten, a diaper, and urine should be
colorless.
2. Stool: By 5 to 7 days, loose yellow stools should be passed at least four
times a day.
3. Growth: Rate of weight gain provides the most objective
4. indicator of adequate milk intake in mother: let down reflex
The way of sterilization:
First wash the bottle with cold water + detergent (to remove protein - albumin)
→ Brush it
Wash it by hot water (to remove lipids - carbohydrate)
Take off the tit and put the bottle in boiling water for 10-15min.
Put the tit for 3-5 min in the boiling water.
Then put the bottle in the refrigerator till you will use it.
Types of sterilization: by Boiling or Steaming Sterilizer or using chemicals
(specialized for sterilizing baby feeding equipments)
Number of bottles = number of feeds + 1 .
3
Assessment of degree of dehydration:
(3-6 %) of body weight mild
(6-10 %) moderate
(> 10 %) severe
>14 %) incompatible with life
)
Indication for hospital admission in diarrhea:
1. Moderate – severe dehydration.
2. Persistent vomiting.
3. Social background.
4. Diagnose in doubt (e.g meningitis, parentaral diarrhea)
5. Food poisoning.
Treatment:
ORS: oral rehydration should be given to infants and children slowly, especially if
they have emesis. It can be given initially by a dropper, teaspoon, or syringe,
beginning with as little as 5mL at a time .The volume is increased as the pt.
tolerates the ORS.
_____________________________
Assessment of Developmental age:
If there is discrepancy between chronological age and developmental age→ think
about:
1. UMNL due to any cause: trauma for example.
2. Cerebral palsy.
3. Degenrative brain disorder.
4. Kernicterus
_________________________________
Anti-motility drugs: should be avoided in children as it may cause respiratory
depression:
- <1 year (Absolutely contraindicated)
- >1 year (relatively contraindicated)
When to give antibiotics in pt. diarrhea:
1. Less than 3 month.
2. Marsmus to avoid septicemia.
3. Malnutrition. 4. Food poisoning.
Chronological age: age of the pt.
Developmental age: degree of maturation of
function
If you need to ↓ diarrhea →give
adsorbent of water (Pectin, caulin).
Note: Normal increment in
weight below 3 months
600-900 g or
20-30 g daily
4
Session notes
د
.
رؤى
Pediatrics
6
th
stage
Important steps should not be forgotten in exam:
1. Greeting the parent.
2. Introduce yourself.
3. Take permission.
4. Thank them finally.
GIT examination:
General exam(related to GIT) + abdominal exam :
Abdominal examination:
1. Inspection: Scar of previous surgery, hernia, dilated veins, abdominal
distension, shape of umbilicus
2. Palpation: first of all ask about any pain and try to avoid paiful area
A. Superficial: for tenderness, rigidity, mass.
B. Deep: for any mass, tenderness, and organomegally.
Infant spleen palpation begins from left iliac fossa
Spleen if palpable it is enlarged
Liver: start from RIF upward till you feel the live →if palpable: comment on:
Surface: smooth or nodular.
Consistency: Soft, firm or hard.
Border: sharp or blunted.
Tender or not (tender in RV heart failure, hepatitis, liver abscess)
Then→ measure how many cm below costal margin.
Then → measure liver span (differ according to age of child).
->3cm BCM is significant.
-Liver is always palpable in neonate
The liver may be palpable but not enlarged as in hyperinflated lungs
Spleen: palpate for spleen from RIF and ascend diagonally till you reach the left costal margin
→ if you couldn’t feel the spleen→ turn the baby to the Rt. Then palpate.
→ If you felt the spleen→ comment on (as in case of live).
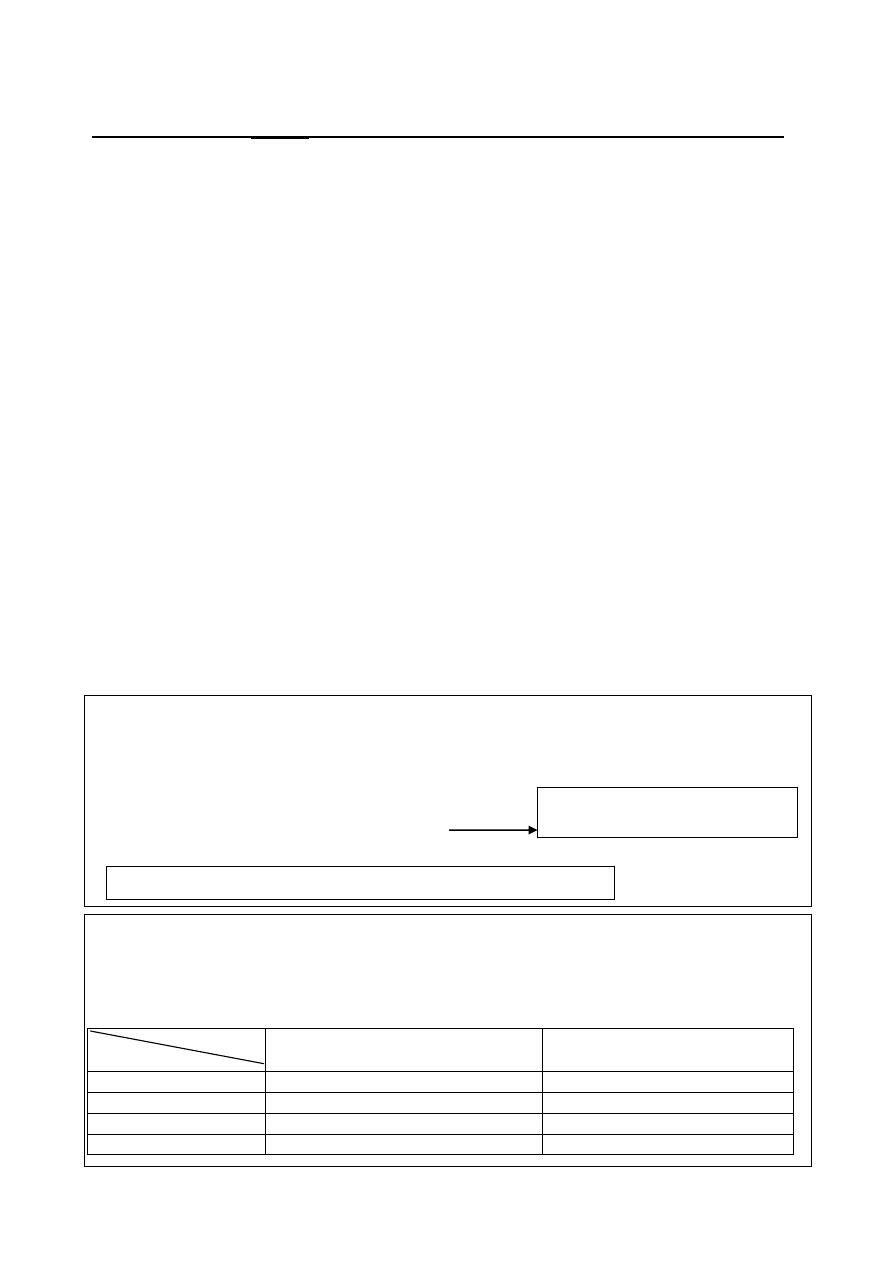
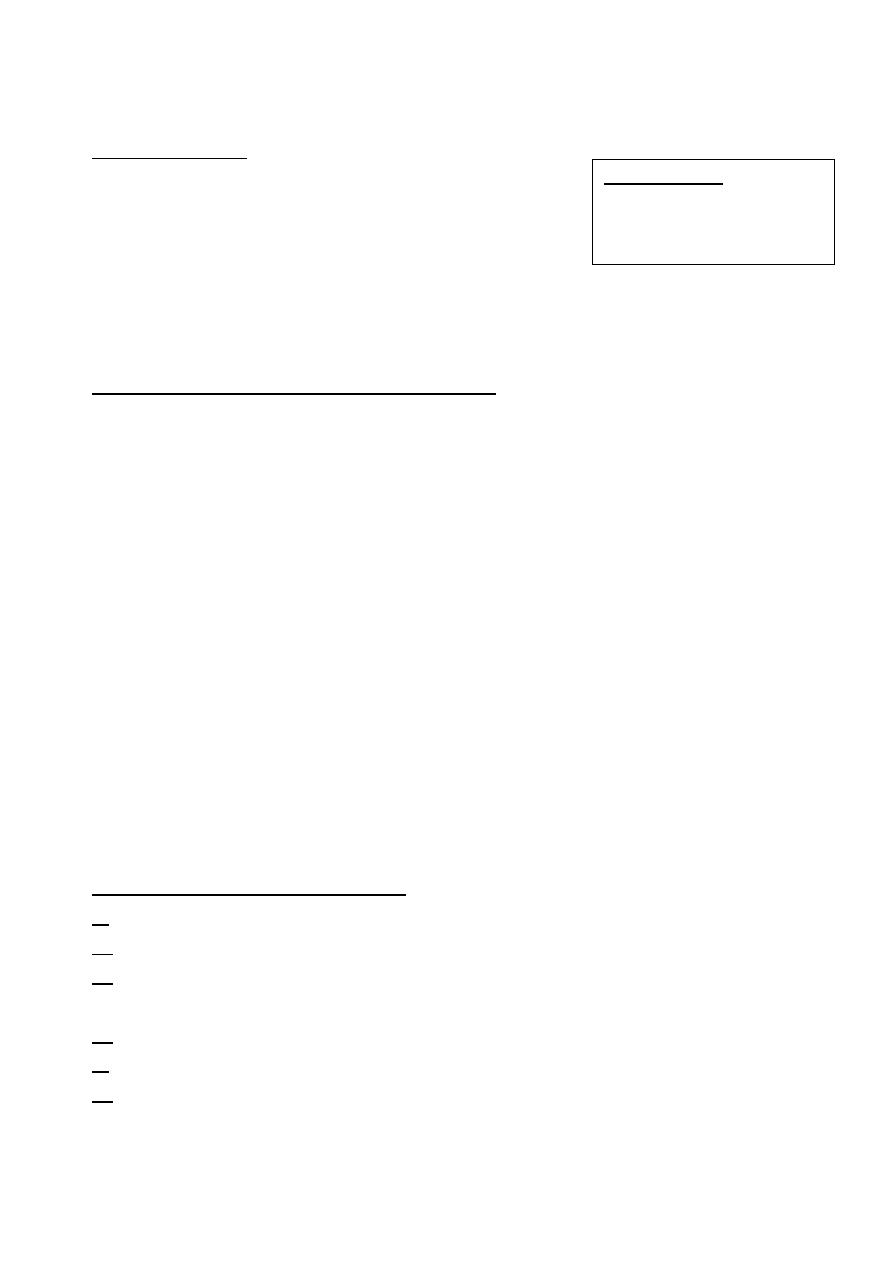
Q/ How to differentiate between palpable spleen and the left kidney?
Organ
Features
Spleen
Lt. kidney
Movement with respiration
yes
No
Direction of enlargement
Diagonally toward RIF
Vertically toward LIF
Can get above it?
No
yes
Presence of notches?
yes
No
left kidney
1.moves with respiration 1. Not movable
5
Febrile convulsion: Age 6-60 months (6m-5years)
Types:
a. Simple (generalized, < 15 min, occurs 1 time in 24 hours and does not recur)
b. complex ( focal, > 15 min, > 1 time in 24 hours, recurrent)
c. status epilepticus: seizure that is lasting >20-30 min or recurrent convulsive
attacks without retaining consciousness in between.
Risk factor of recurrence (in febrile convulsion):
1. Age <1 year.
2. Duration between fever and seizure <24 hours.
3. Temperature >39 C.
4. Family Hx of epilepsy.
5. Male gender.
6. Hypernatremia (young age).
Causes of status epilepticus:
1. Missed dose of anti-epileptic drug.
2. Febrile convulsion “most common”.
3. Meningitis.
4. Hypoglycemia
5. Electrolyte disturbance: (↓Na
+
, ↓Ca
++
, ↓Mg
++
).
6. Subarachnoid hemorrhage.
7. Intracranial hemorrhage.
8. Drugs " naldixic acid = nigram " and aminophyllin.
Convulsion (status epilipticus): emergency management:
1. ABC (airway, breathing, circulation)
2. Recovery position (lateral)
3. Don’t put any thing in the mouth
4.Suctioning.
5. Diazepam IV: 0.1-0.3 mg\kg. slowly
+
O2
→
#If no response after 15 min→ repeat dose up to 3 times.
#If no response →give phenytoin or fosphenytoin
(20 mg\kg at rate not >50mg/min + Normal saline)
#If no response after 20 min→ give additional 10mg/kg phenytoin.
#If no response →Give Phenobarbital “luminal" (20 mg\kg slowly).
Note: staring of the eye:
# upward → generalized
#laterally → focal
#Diazepam should be given slowly (5-10
min) as it may cause respiratory
depression.
#Rout: IV or rectally using insulin syringe.
#Fosphyitoin→rapid rate of administration+↓ irritation
#never use 5% dextrose as it causes crystal
precipitation
Used with caution when co-
adminstered with benzo-
diazipines as it may cause
ventilator failure
6
#If no response→ Admit the pt. to ICU and call anesthetist in order to give
general anesthesia (propofol or halothane or ketamine).
Investigation:
1.Blood sugar
2.Serum electrolyte
3.CBC
4.Blood culture
5.CRP
6.lumbar puncture : before you do it, do fundoscopy
looking for papilledma:
-If present → do CT scan to exclude brain mass.
-If absent → do LP safely.
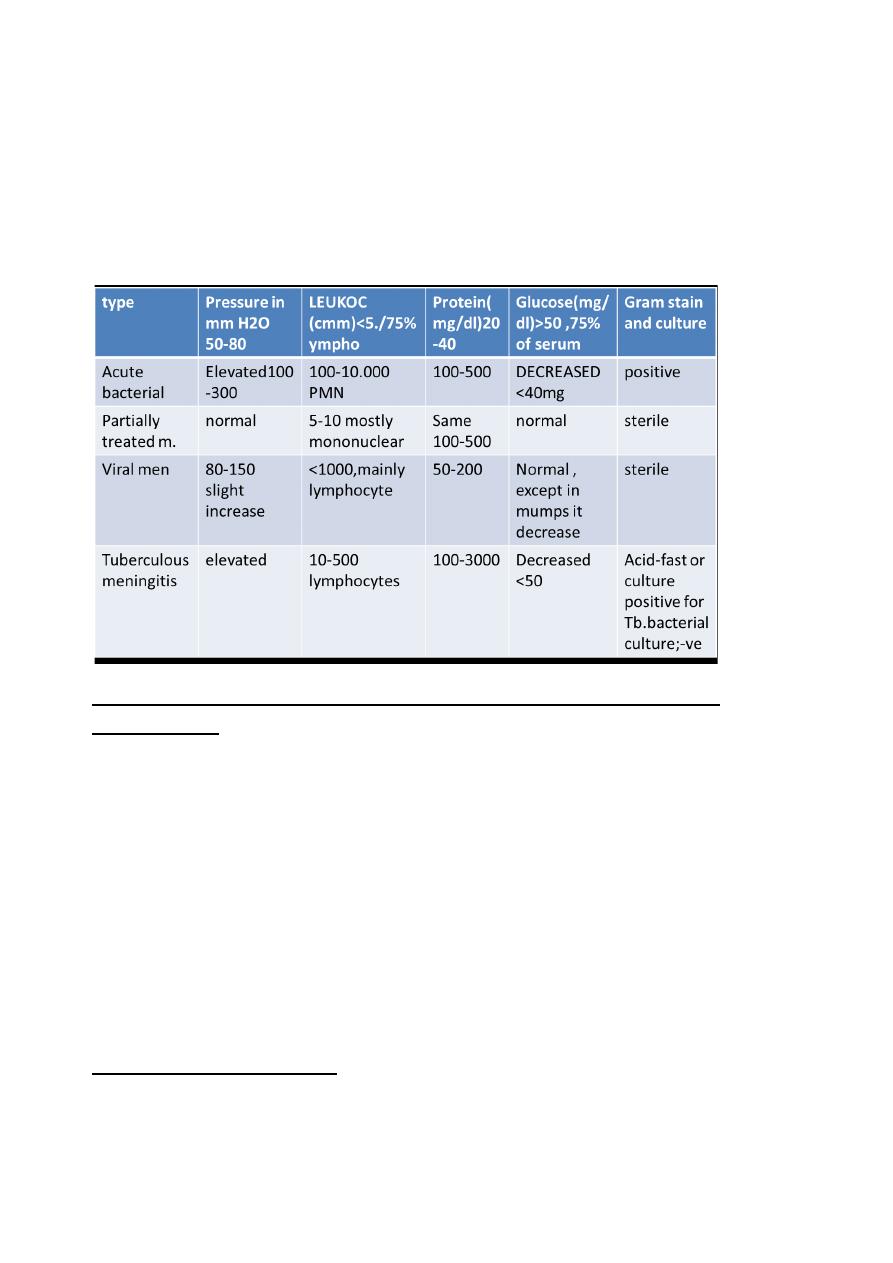
Q/ If we give antibiotics before doing lumbar
puncture what changes seen in CSF?
CSF analysis will not change significantly
but the culture always changes.
Procedure of LP:
1. Patient sitting position or leaning forward or laterally directed.
2. Sterilization of the area in circular pattern
3. Draw an imaginary line between the 2 iliac crests→ insert the needle just above it
between L4-L5.
4. Collect CSF (15 drops are enough) and check the pressure.
What to do after collection of CSF sample?
1. Inspection: clear crystal or turbid (infected).
2. Send for biochemistry: glucose, protein.
3. Send for Gram stain and microscopy.
4. Send for Culture and sensitivity test.
Drugs induced fever:
1. Pencillin.
2. Cephalosporin.
3. Quinidine.
4. Alfa-Methyldopa.
5. Nitrofurntin and INH.
NOTES:
#Turbid CSF contains: > 350 cell
#In acute bacterial infection , at early phase
(1
st
to 12 hours) lymphocyte predominant,
while later on, neutrophils predominant.
#CSF glucose should=
½ - ⅔
of blood glucose
#↓ CSF glucose is called hypoglycoratia.
NOTES: In any convulsion do not forget to ask about
:
#fever, trauma, and symptoms of meningitis.
#Dysentery (shigellosis may cause counvulsion).
#Cough and SOB→ pneumonia may cause convulsion by (Cerebral
anoxia and SIADH→ cerebral edema as a result of hyponatremia)
#Skin rash →measles & roseola infantum can cause convulsion .
# Family Hx. (Febrile convulsion and epilepsy)
7
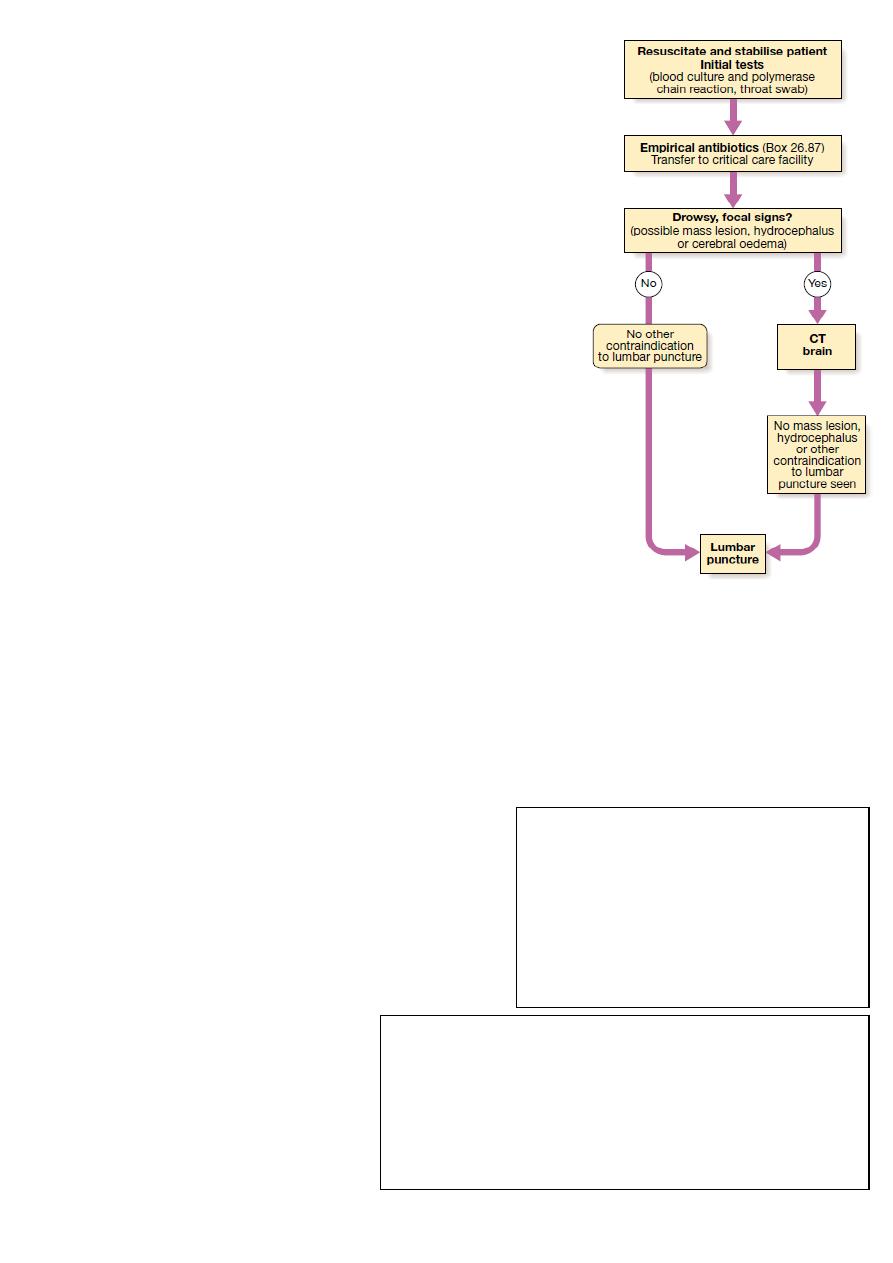
Meningitis:
Symptoms: pyrexia, headache, vomiting photophobia photophobia or even
convulsion develops over few days.
Signs: meningism (brudizinski sign, neck stiffness, kerning sign).
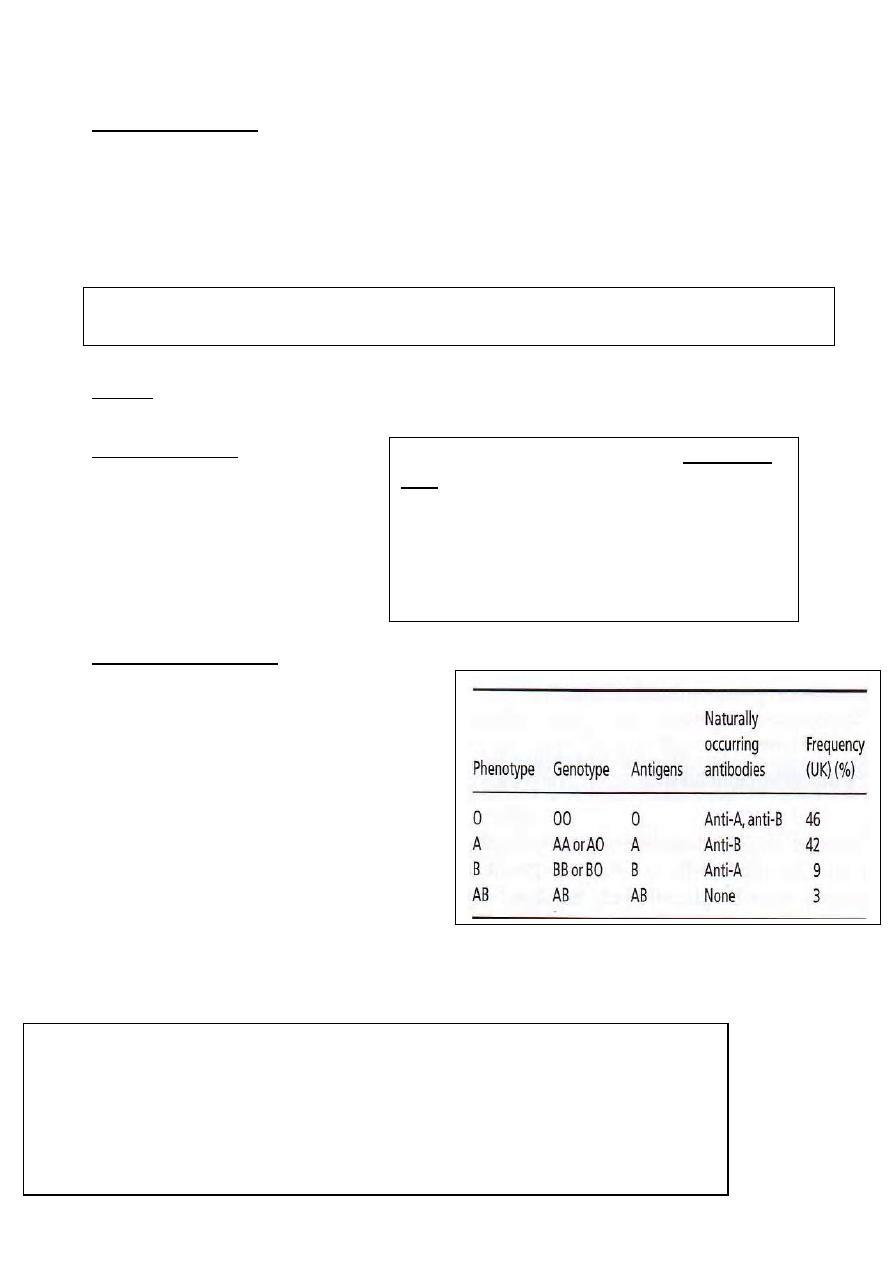
CSF: Findings:
____________________________________________________________
Galactossemia:
Decrease in G-1-PH UT enzyme which essential in glucose metabolism.
Presentation:
1.jaundice
2.hepatomegaly
3.feeding poorly
4.hepatic failure
5.vomiting
Q/Patient with galactosemia can’t lie for long time?
A/Because they are susceptible for sepsis with E.coli
Indirect hyperbilirubenimia:
1. Gilbert syndrome
2.Crigglar syndrome (type I or II)
8
Gilbert syndrome: Benign condition→ causes indirect hyperbilirubinemia at time of
stress such as fasting \ infection because of deficient of hepatic conjugate enzyme.
Direct hyperbilirubinemia :
1. Biliary atresia (diagnosed by US ).
-surgical treatment: (Kasai porto-enterostomy)
-Should be done once biliary atresia is suspected.
2. Neonatal sepsis
3.Hepatitis
4.Cystic fibrosis
5.Galactosemia
Investigation:
1.TSB ( total serum bilirubin ) + differenation ( direct or indirect ).
2. Blood culture
3. WBCs.
4. Reticulocyte count.
5. US of abdomen
6.PT + PTT
6. TFT (T3, T4 and TSH)
Neonatal jaundice: DDx
1. Biliary atresia
2.Cystic fibrosis
3.metabolic disease (+ve family history, +ve consangity )
4. TORCH infection (most important→ CMV)
Stigmata of chronic liver disease:
1. Jaundice
2. Spider naevi
3.Ascites
4.Palmar erythemia
5.Internal bleeding (intra abdominal, in joint) because of clotting factor deficiency
9
Causes of acute liver injury:
1. Viral hepatitis (A > B & others)
2. Actominophen poisoning > 200 mg\kg (dose in pediatric) while in adult is (7 gm)
3.Wlison disease.
4. Alpha anti-trypsin deficiency.
5. Glycogen storage disease: type 1 & 2 cause hetaptomegaly only.
Rx of chronic liver disease:
-Albumin 5 cc\kg
-vit.K, blood transfusion
-If there is infection → antibiotics.
____________________________________________________________
Respiratory distress syndrome: lack of surfactant due to prematrity.
-Surfactant formation starts at 28 wks and complete at 37 wks.
-For maturation of lung: give betamethasone before delivery 1 injection \ 24 hours
To differentiate RDS of respiratory source from CVS sourc:
→Respiratory: respond to O
2
→CVS : doesn’t respond to O
2
Side effect of ↑O
2
administration→ bronchpulmonary dysplasia (long term complication)
DDx of RDS:
-Pneumonia, bronchiolitis , asthma , PE , ARF , DKA , anemia .
DDx of hyperinflated chest
1. Asthma.
2. Bronchiolitis.
3. Emphysema.
_____________________________________________________________
Infective Endocarditis :
Symptoms:
Prolonged fever, malaise, anorexia, weight loss
dyspnea, cough, SOB, myalgias, nightsweets
and joint pain.
NOTES: about Auscultation of heart:
#S1 beast heard at mitral area.
#S2 beast heard at pulmonary area.
#loud S1 →ASD
#Loud S2 → Pul. HT, ASD and VSD
#S3→ (after S2) normal or anemia
#S4→(before S1) always abnormal
#Murmur of aortic coarctation→ interscapular
#HF →base of the lung.
10
Signs:
-Petechiae: not specific
- Splinter hemorrhage
- Jane way lesion: Non-tender macules on the palms and soles.
-Osler nodes: tender subcut. Nodules usually found on distal pads of the digits.
-Roth spots: Retinal hemorrhage (found in 5% of Pt.)
-Heart murmurs (85%): change in characteristics of previously heard murmur (10%).
-Signs of embolic stroke
-Signs of systemic septic emboli.
-Splenomegaly
Investigations:
1.Blood culture.
2. ECHO →vegetations.
3. US.
4. Radiology.
Pathogen: S.viridians, fungal infection , s.epidermis (in catheterized pt.)
Indication for prophylaxis:
1. Prosthetic heart valve.
2. CHD.
3. Coronary heart stent.
4. Dental and genitourinary procedures.
5. Procedure on infected skin or musculoskeletal tissue.
6. Procedures involving incision in respiratory mucosa
7. History of IE
Developmental hx: من المحاظرة
11
Pediatrics
6th stage
Session notes
د
.
أوس
-In rota virus vomiting is before the diarrhea but not always.
-Diarrhea due to small intestinal cause →low amount stool.
-In colitis →Large amount stool
-one of the features of mal-absorption is→ large bowel diarrhea
-Shiglla , sallmonilla , E.coli , campylobacter , pesdomembranous colitis ,
associated listeria.
-Clostiridium toxin for rapid assessment, skip AB
-Antibiotics cause (watery diarrhea) eg: ampicillin
Q/How can you differentiate bloody diarrhea due to bact. or parasite?
A/ by chronicity: short period →bacterial, long period →parasitic
Cow’s milk allergy:
cause colitis and bloody diarrhea.
Diarrhea is of two type:
1.non-infectious
2.infectious (viral, bacterial, parasitic, non-viral)
*Bed dysentery (bacterial).
*Walking dysentery (E. histolytica), IBD.
Cow's milks allergy findings:
-Cough, skin rash, GIT problem, wheezes
-Bloody diarrhea Caused by → bovine, protein (casein)
-Can be replaced by: Hydrolyzed formula
-Side effect of this formula is→ the taste (Not sweet)
-If not benefit → give amino acid Formula (elemental formula)
-From the mother transmitted by the breast when she ingested the
cow's milk then to the baby by breast feeding.
12
-Soy formula →isomil →Should not give it below 6 monthes,
because it contain estrogen
-We can administer hypo-allergic diet
Lactose intoleranc
e: (2ndry)
occur secondary to acute gastro-enteritis → chronic diarrhea with
peri-anal excoriation, flatulence and distended abdomen.
#this is occurred due to mucosal damage of GIT by disturbance in
lactase enzyme function. (The enzyme is located in the brush
border of epithelial cells)
Investigation:
1.culture for bacteria
2.ELISA for viral mainly rota virus
3.microscopic for parasitic showing trophozoite
4.clostridia difficile.
Investigation for Lactose
1.ph stool: acidic
2.reducing substance in stool: +ve
in urine >>> -ve mean galactosemia
Convulsion associated with diarrhea:
-(UTI, meningitis, Febrile convulsion, parental diarrhea)
-Electrolyte disturbance (hyponatremia).
-Hypoglyemia
-Shigllosis (convulsion + bloody diarrhea)
How to prove?
- Urine, stool and blood culture
-CSF.
-Serum electrolyte.
-RBS (random blood sugar)

13
General exam:
First of all ask about permission
Try not to disturb the child
a. General appearance:
1.general look (looks comfortable, ill, distress, dyspneaic, irritable,
semiconscious, drowsy, unconscious).
2. Dysmorphism (looks normal, any dysmorphic features).
3. Body built (looks thin, emaciated, good body built, thriven, I have
to plot his parameters on growth chart)
4. Neurodevelopmental: abnormal posture, not moving limb, No
special posture.
Hand:
-Looks for clubbing but at least 6 months, peripheral cyanosis
-Nail →koilonychia (iron deficiency anemia), Leukonychia
(hypoalbuminemia), splinter hemorrhage, capillary refill (2 sec),
pale or not.
Face:
Eye: looks for conjunctiva for pallor, sclera for jaundice.
Mouth: (hygiene, color of tongue, dental caries (source of IE),
ulceration, aphthous, pigmentation (addison disease) talk about any
striking abnormality.
Legs:
Scar, color, edema.
#General examination is introduction for every systemic exam:
#Edema could be due to respiratory problem caused by right-sided
heart failure (cor pulmonale).
14
GIT exam:
General exam:
Hand looks for clubbing (Look for angle between nail and nail bed→ do
shamroth’s test), palmor erythema, nail changes, pallor of creases
→Causes of clubbing:
liver cirrhosis, cyanotic heart disease, lung (bronchiactasis, cystic fibrosis,
empyema, pulmonary fibrosis (fibrosing alveolitis), familial, hereditary.
Abdominal exam:
Inspection, palpation, percussion and auscultation. (like adults)
-----------------------------------------------------
Case: Cerebral palsy → findings:
-Head → microcephalus.
-CP posture spastic→ scissoring of legs.
General exam:
-looks ill, thin and emaciated,
dysmorphic face, abnormal posture
CNS exam: Upper and lower limbs:
Inspection: abnormal posture, wasting, joint swelling, fixed deformity.
Palpation: tone of each limb, reflex, power and sensation.
Hyper-reflexia and hypertonia → due to upper motor neuron lesion.
Babniski sign → +ve
Cranial nerve examination:
Abnormal C.N 9 +10 (psudobulbar palsy) → inability to swallow,
uveola deviated to side, loss of gags reflex,
and loss of taste is post. ⅓ of
the tongue.
Hx of pt. with CP: important pointes:
1.Current illness.
2. Per-natal→ Rash, fever during pregnancy (cong. inf.)
3. Natal hx →prematurity, mode of delivery and birth
asphyxia.
4. Post-natal: Birth wt., crying, NICU, jaundice, hx of head
trauma and CNS infection.
5. Family Hx: consanguinity, same condition.
Diaplegia means:
affection of both upper and lower
limbs with lower limb predominance.
Lower limbs > upper.
#Psudobulbar palsy→ UMN lesion of cranial nerves 9+10
→ paralysis of pharyngeal, laryngeal and soft palate
muscles →dysphgia (as in patient with CP).
#bulbar palsy → same as psuedobulbar palsy but it’s due
to LMN lesion of cranial nerves 9+10.
15
Why pt. with CP is liable for recurrent chest infection?
- Because of recurrent aspiration, which is due to:
1. Psudobulbar palsy.
2. GERD (many pt
s
. with CP have concurrent GERD) →
Cerebellar exam:
1. Speech (scanning or dysarthric speech).
2. Eyes (Nystagmus).
3. Gait: heel-toe test→ (ataxic gait).
4. Rapid alternating movement (dysdiadochokinesia).
5. Finger –nose test → dysmetria (dysmetria).
6. Heel-shin test.
______________________________________________________________
Lec.2
Pediatrics
6
th
stage
Session notes
د
.
اوس حازم
Meningism:
consists of headache, photophobia
and neck stiffness, often accompanied by other
signs of meningeal irritation including:
Kernig’s sign (extension at the knee with the
hip joint flexed causes spasm in the hamstring
muscles) and Brudzinski’s sign (passive flexion
of the neck causes flexion of the hips and knees).
• Examination steps:
o Position the patient supine with no pillow
o Expose and fully extend both the legs.
Neck stiffness:
-Put one hand under the occiput of the baby and support the body with the other hand→
try to flex the head forward aiming to make the chin touches the front of the chest.
-If there is neck stiffness→ there will be resistance to flexion movement.
-If the pt. is old enough → ask him to touch the front of his chest by his chin.
Rx: -Medical→ PPI, H
2
blockers and
domperidon.
-Surgical (Niesson fundiplication)
Important causes of CP:
Prenatal: cerebral malformation,
congenital infection.
Natal: prematurity and birth asphyxia
Post – natal: Kernicterus, non specific
head trauma and CNS infection.
#Meningism is not specific for meningitis.
#Causes of meningism:
1.meningitis.
2. Subarachnoid hemorrhages.
#Conditions that may mimic meningism:
1.cervical spondylosis.
2.Tetanus.
3. ↑ICP
16
Brudzinski sign: While you are examining for the neck stiffness, if the flexion of the head
was accompanied by flexion of the knees→ +ve Brudziniski sign.
Kernig’s sign:
-Flex the hip and knee of one side to 90⁰.
-Put your left hand over the hamstring muscles (posterior thigh) → extend the flexed
knee → if the there is any resistance to extension or the hamstring muscle spasm
→ +ve Kerning’s sign.
______________________________________________
↑ICP: can cause meningism: Symp. and Signs →
Note:
6
th
C.N palsy→ Convergent squint (can’t abduct
the eye of the affected.
3
rd
C.N palsy→ -Divergent squint (can’t adduct
the eye of the affected side) with ptosis and dilated pupil
(No parasympathetic).
Squint caused by nerve affection is called → paralytic squint.
How to differentiate between paralytic and non-paralytic squint?
-By cover test: Cover the normal eye:
→ if the squint eye is corrected → non-paralytic squint.
→ if the squint is NOT corrected→ Paralytic squint.
______________________________________________
Facial palsy (VII): due to UMNL or LMNL.
-In UMNL:
1.Deviation of angle of mouth (toward normal side).
2.Flattening of the nasolabial fold.
3. Inability to blow cheeks.
4. Preservation of the upper face
(check it by asking the pt. to elevate his eyebrows and see the wrinkles in the forehead).
-In LMNL:
1.Deviation of angle of mouth toward normal side
2.Flattening of the nasolabial fold.
3. Inability to blow cheeks.
4. Dropped eyebrow (of the affected side).
Symptoms of ↑ICP:
1.Vomiting.
2. Headache.
3. Diplopia.
4. Disturbed level
of consciousness.(DLC)
Signs of ↑ICP:
1. DLC
2.Bradycardia.
3. Hypertesion.
4. Respiratory depression
5.Bulging fontanelle.
6. Paralytic sequint
(6
th
C.N palsy).
17
5. Loss of forehead wrinkles.
6.inability to close the eye and +ve Bell’s phenomenon: when you ask the pt. to close
his eyes→ the eye of the affected side will not be closed, so the pt. elevate his eye
upward in order to seem like he is closing his eye.
#Examination of the cranial nerves
Start by general exam for example: the baby is conscious alert (small child) or oriented
(older child), normal posture or lying supine or in the lab of his/her mother, no squint,
no nystagmus, no facial asymmetry, no any dysmorphic features. .
Olfactory nerve (I):
1-Exam each nostril separately
2-You should confirm that the nostril is patent (Rhinitis (increased secretion), foreign
body obstructing the nostril interfere with smell)
3-Bring familial odors as apple or tea or others in tubes specific for smell examination
4-Never use irritant smell because its sensed by the ophthalmic division of the V cranial
nerve not olfactory nerve.
#Most common cause of VII C.N palsy is Bell’s palsy.
# Bell’s palsy: is LMNL of facial nerve which is mostly idiopathic.
# Other causes of facial n. palsy include:
1. Ramsuy-Hunt syndrome (RHS): Herpetic viral infection of facial n.
2. Complicated otitis media.
LMNL
3. Gullian-Barre syndrome (GBS)
4. Hypertension: also can cause facial palsy.
5. Trauma.
So, when you face a case of facial palsy (LMNL)→ the next step will be:
→Examination of ear looking for herpetic vesicles (In RHS) and signs of otitis media.
→Examination of the lower limbs for→ hypotonia and hyporeflexia (ascending paralysis in GBS).
→Examination of blood pressure.
→Examine for any sign of trauma.

18
Optic nerve (II):
Examination: It has five components to be examined:
1-Visual acuity: Above 4 months you can use Fixation and follow test, this done by
holding an interesting toy about one meter in front of the baby, once baby fixes his
vision to it, you start to move it in an arc, if the baby follow it, consider that this baby
has normal vision.
Below 4 months, the baby can follow faces and light only. Above 7 years (cooperative
child), we can use Snellen chart Sometimes Allen’s chart (pics of animals with different
sizes) can be used below 7 years.
2-Visual field (in cooperative child): One meter distance between doctor and baby then
the doctor closes one eye by his hand and the child asked to close the eye opposite to
the doctor eye, then the doctor start to test upper, lower and right and left fields of
each eye separately by comparing with his eye considering that the doctor has normal
visual fields.
3-Color vision: (in cooperative and old child): This can be tested by using Ishihara test,
which consist of book containing different figures with different colors, and the child is
asked about these figures (considering that the child knowing these figures e.g.
numbers, pictures etc.)
4-Pupillary reflex: Optic nerve form the sensory (afferent) part of this reflex, while the
motor (efferent) part is oculomotor (will be discussed next)
Oculomotor, trochlear and abducent (III, IV, and VI):
Examination: These nerves should be examined simultaneously, their examination
consist of three components:
1-Eyeball movement: One meter between the child and examiner:
-In small child move an interesting toy in H shape pattern and look at the child if he
follows the toy by his eyes, in the same time you should look for sequent and nystagmus
with each movement.

19
-In older cooperative child you can move your finger or any object in H shape pattern
and asking him/her to follow, in every movement you should look for sequent and
nystagmus and ask about diplopia.
2-Accommodation:
-In small child, move an interesting toy toward the nose, normally there will be ptosis,
conversion and meiosis of both eyes. 2-In older child, you can move your finger or any
other object same as above. 3-Pupillary reflex: Afferent: optic nerve Efferent:
Oculomotor nerve This test has two parts:
1-Direct: By using light torch, come out of the visual field and direct the light toward the
pupil, normally the pupil size will decrease
2-Indirect (consensual): the same maneuver but this time you put a barrier between the
two eyes, then direct the torch toward one eye and look at the other eye for pupil
constriction (normal consensual reflex).
Notes: Types of squint: divergent squint and convergent squint. Diplopia: as patient
looks downward like step down a ladder. Dilated pupil
3
rd
cranial nerve lesion lead to:Downward divergent squint (inferolaterally) + ptosis +
lack of accommodation (mydriasis) + lacrimation also affected.
Trigeminal nerve (V): Function: motor, sensory, reflexes.
1-Motor: supply the muscles of mastication by the motor fibers of the mandibular
division which includes:
a-Masseter muscle, temporalis muscle: closing the mouth (clenching the mouth)
b-Lateral ptrygoid muscles: open the mouth and moving the lower jaw from side to side
(lesion in the nerve causes deviation of the jaw toward it).
2-Sensory: Supply the skin of the face by the three division as follow:
a-Ophthalmic; supply the skin above the imaginary line that runs from the middle of
cranium downward to the lateral angle of the eye.
b-Maxillary; supply the skin below the imaginary line as described above and above an
imaginary line from anterior third of the lateral part of the cranium to the angle of the
mouth.
c-Mandibular: supply the skin below the imaginary line as described in b.

20
3-Reflexes:
a-Corneal reflex: Afferent: Ophthalmic division of trigeminal. Efferent: Branch from
fascial nerve causes blinking of the eye.
Two ways of examination:
1-Blowing on the child eye (usually not done due to risk of transmit infection to child as
respiratory infection) its positive when the child blink his eyes.
2-By using cotton, bring it out of the field of the child and touch rapidly the
corneoscleral junction, positive when the child blink his eye(also not done due to risk of
corneal ulceration)
b- Jaw jerk:
Afferent: 5th CN mandibular division.
Efferent; 5th CN mandibular division.
Ask the child to slightly open his mouth, put your index finger on the the chin
and by taping it by the hummer, you will notice slight or no upward
movement of the jaw normally, while brisk upward movement seen in upper
motor neuron lesion. .
Facial nerve (VII):
Function: motor supply for facial muscles and sensation of taste of the anterior two
thirds of the tongue.
Anatomy: nucleus in the pons.
Examination: In facial nerve you should examine 3 components:
1-Motor: facial muscles (4 muscles which are; frontalis, orbicularis oculi, cheek muscles
and orbicularis oris) and this done as follow:
a-Ask the child to look upward while fixing his neck in normal anatomical position, check
for forehead wrinkles bilaterally
b-Ask the child to close his eyes as much as he can till the eyebrow is buried, then try to
open his eyes by your hands to check for resistance .
c-Ask the child to blow against closed mouth, also check the resistance by pushing his
cheeks with your fingers
d-Ask the child to smile, look for the angle of the mouth if they are normal or there is
mouth deviation. If there is a lesion in the right fascial nerve, the mouth will be deviated
toward the normal side. All muscles affected in upper motor neuron lesion, while only
cheek muscles and orbicularis oris muscles are affected in lower motor neuron lesion,
21
because the upper two muscles supplied by nerve fibers that come from the upper half of
fascial nucleus, and the lower two muscles supplied by nerve fibers that originate from
the lower half of fascial nucleus, the upper half has innervation from both cerebral
hemispheres therefore when the fibers come from one hemisphere affected, the
branched from the other side will take its place, while lower half of the nucleus take
innervation only from the ipsilateral hemisphere, therefore when its fibers damaged
nothing take its place!
2-Sensory: it takes taste sensation of the anterior two thirds of the tongue by its sensory
branch, chorda tympani. To examine this typically the tongue should be pulled by forceps
out of the mouth, and then put drops of specific taste on its specific are of sensation
(sweet on the anterior part of the tongue, salty and sour on the lateral side and biter on
the posterior part of the tongue)
#Note: Ramsay-Hunt syndrome, its herpes zoster of the sensory part of the facial nerve
of part of the external auditory canal. .
o Facial nerve palsy: Upper motor neuron lesion: only lower part affected (toward
lesion). Lower motor neuron lesion: Bell's palsy, all sites of face, no wrinkling, deviation
of mouth toward same side .
Vestibulcohlear nerve (VIII):
1-Hearing:
a-Audiometery; it’s a device that needs cooperative child > 5 years
b-Tunic fork; used in children > 5 years, also needs cooperative child.
c-Distraction test; could be used in babies > 4 months, this can be done by two
examiners one stand infront of the child having an interesting toy in his hand and the
other examiner stand behind the baby, when the child fixes his vision to the toy infront
of him/her, the examiners behind will produce a sound, if the child turn his head
toward him, means his hearing is ok.
2-Balance:
a-Nystagmus: there are 3 types, transverse, vertical and arc movement. You can examine
for it by two methods:
1-Water caloric test: a-warm water (44C and above) introduced in the external auditory
canal, head will turn to the ipsilateral side, both eyes will turn toward contralateral side
with horizontal nystagmus toward the ipsilateral ear. b-Cold water (30 C or below)
introduced in the external auditory canal, head will turn to the contralateral side, both
eyes will turn toward the ipsilateral side with horizontal nystagmus toward the

22
contralateral ear.
2-Hallpike test; Check Macleods for further information b-Ataxia: Incoordination of body
movement .
Glossopharyngeal and vagus nerves (IX and X):
Examination: You should examine these nerves together and start as follow:
1-The Uvula, should be central, if there is lesion in one side the uvula should deviated to
the normal side. Ask the baby to say Ahh to demonstrate the uvula clearly.
2-Gag reflex; by touching the posterior wall of the pharynx by tongue depressor (afferent
by glossopharyngeal), this will cause contration of the pharyngeal muscles (efferent by
vagus nerve), this reflex induces sense of vomiting .
Accessory nerve (IX):
1-Ask the baby to elevate or shrug his shoulder, and push against his shoulders by your
hands.
2-If the child is small, move an interesting toy in front of him from side to side to check
for sternocleidomastoid muscles 3-If the child is old and cooperative ask him to look to
the side, the push his jaw by your hand and ask him to push against your hand .
Hypoglossal nerve (XII):
Examination: (you need cooperative child):
1-Examine the tongue in resting and look for:
a-Wasting
b-Fasciculation (fibrillation when seen on EMG, but in tongue examination we can use
both words)
2-Exmine the tongue after asking the baby to protrude his tongue out of the mouth and
look for a-Weakness b-Deviation (deviation is toward the abnormal side)
3-Then ask the baby to close his mouth and push his cheeks by his tongue .
#Baby during feeding uses 9 cranial nerves:
-Eye to eye contact with mother by optic nerve (indirectly related).
-Eye movement by 3rd, 4th and 6th cranial nerves (indirectly related).
-Muscles of mastication by V CN (directly related).
-Facial muscles (sucking muscles) by VII CN (directly related).
-Muscles of deglutition by IX and X CNs (directly related).
Swallowing (tongue) by XII CN (directly related).
23
If more than 7 years: You can proceed in examination as follow:
#Olfactory
#Optic:
-Visual acuity : snellen chart
-Visual field : con frontation test or perimetry
-Papillary reflex
#3 , 4 , 6 ( H-shape )
#5 cranial nerve ( trigeminal ):
-Sensory
-Motor ---> mastication
-Jaw jerk reflex ( +ve UMNL )
-Corneal reflex
#Facial deviation to normal side, flattening of nasolabial fold to the affected.
#8 cranial ( vetibulocochlear ) :
-Whisper in child ear
#9 , 10 cranial nerve : swallowing , say ahh there is uveal move
Bulbar palsy ( UMNL ) , psedoubulbar ( LMNL )
-Pseudobulbar ( supra-nuclear ) , bulbar ( infra – nuclear )
-NG tube or gasrostomy
-Post 1/3 of 9 GN taste
#Acessory n.
#12 cranial nerve : tongue affected deviation , fasiculation , wasting
-vagus : uveal pulled to normal side
1 min. Is enough for test
In infant:
#Sucking 9 , 10 ( swallowing ) look to his mother
#Move a toy in front if him for 3 , 4 , 6
#Crying for facial palsy deviation
#Jaw jerk

24
Exam limb:
Appeareance: Scissoring of leg: CP, wasting of muscle.
Feel :
-Tone ( ankle , knee , hip )
-power
-reflex
#How to examine properioception?
-Explain to patient →close the eye → ask the pt. to tell you to which direction his joint is
moving (upward and downward)
-Romberg sign: pt. is doing well when eyes are opened → ask him to close eyes→ if the
pt. start to deviate and lost his balance → Romberg sign +ve → defect in proprioception
(dorsal column of spinal cord) and not cerebellum as pt. with cerebellar ataxia has
unbalance even when his eyes are opened.
-plantar reflex (Babinski sign) : Normally +ve in children <2years.
one of the reflexes occur in infants, responses when body receives certain stimulus, after
sole of foot firmly stroked , big toe upward and others fan out
- normal in children up to 2 years and disappear as child gets older, may disappear as
early as 12 months.
25
Lec.1
Pediatric 6
th
stage
Session
+ Tutorial Notes
د
.
رياض
The degree at which the pt. is considered febrile =38.3centigrade.
*The tool for measuring temperature is "thermometer"
*Sites of measuring the body temperature:-
1- oral.
2- Axillary: the most commonly used in children.
3-Rectal:-the most accurate route
4-From tympanic membrane: otometry
*Axillary temperature = 0.5 C⁰ less than that of oral & 1 C⁰ less than that is of rectal
*be careful drug fever? But which drugs?
-Injections like ampicillin or ceftriaxone even Intravenous fluid could elevate our body
temperature,
*Investigations you may send in feverish pt.:
CBC
ESR
CRP
CXR (if cough is present or any sign of RD)
US
Even B.M exam
*PUO:-pyrexia of unknown origin: 8days of elevated body temperature (fever) with
basic physical examinations & investigations (as inpatient or outpatient) but there is
no clear cause.
*always in fever ask about travelling to other areas.
26
*Some of researchers put priority for certain diseases as causative agents of PUO:
1-UTI
2-Kawasaki disease
3-EBV infection
*rash types also can give you clues about the underlying disease.
*is there any rigor? "Rigor in brucellosis is common"
*is there any sweating “as in T.B"
*2 spikes of increased body temperature: Falciparum malaria
*fever at morning & evening: typical of Kala – azar.
**Kawasaki disease: fever for 5 days, injected eyes, redness of mouth with fissuring
of lips, ↑ESR, ↑CRP and thrombocytosis.
*most PUO remit with time ""pyrexia of unknown source""
NOTES: important points in Hx that shouldn't be forgotten:-
1-where does the pt. lives?
2-Who diagnose the fever, mothe or doctor? And how?
*In convulsion Hx taking:-
Ask about vaccination recently? DPT can lead to convulsion.
Vomiting and diarrhea? because this can result in electrolyte disturbance→ convulsion
Look for signs of rickets→ hypocalcemia → tetany.
باقي النق اط مذكورة في سشن
-
2
-
د
-
ررؤ
Sometimes tonsillitis or otitis media + feverconvulsion, so don't miss the
examination of tonsils and ear.
*Causes of big head:
1- Congenital hydrocephalus.
2- Storage disease.
3- Arnold-Chiari malformation herniation of cerebellar tonsils through the foramen
magnum Non-communicating hydrocephalus.
#Q/when you face a child with big head, what is the next step in examination?
A/-Fontannelles .
-Sutures
-Back for spina bifida (meningocele or meningomyelocele). Most important.
#Dandy-walker syndrome: complete absence of cerebellar vermis with enlarment of
the 4
th
ventricle leads to enlargement of skull posteriorly (bulging at back of head)
unlike hydrocephalus which enlargement of entire head.
27
-In pt. sudden cessation of urination: try to concentrate on these points in the history:
could be → anuria or retention of urine.
1-is the child constipated? → Hard stool can press on the urethra→ cessation of urine
(especially in females).
2-Vomiting and/or diarrhea present? Dehydration pre-renal failure.
3- Evidences of UTI.
4- Menstural Hx and puberty in young girls→ if you suspect hematocolpus
(imperforated hymen), and examine the breast for Tanner staging.
Menstrual cycle usually start at 3
rd
or 4
th
Tanner stage.
Other causes of sudden cessation of urination:
1-acute renal shutdown
2-drugs
3-GN the pt. is edematous + tired + acidotic.
4-renal tubular necrosis
5-HUS
Investigations you may send in such a pt. : according to the condition you suspect:
-CBC\Blood culture
-RFT
-US
-CT scan.
Important
Question
#Oliguria <1ml /kg/ hr
#Anuria <180ml/24 hrs.
28
Lec.1
Pediatrics
6
th
stage
Session notes
د
.
ربيع الدبوني
Questions from previous years:
A neonate 1month age , with persistent jaundice , hard stool , posterior fontanlle open
The result of investigations:
TSB( total serum bilirubin ) =? , Hb=14g/dl , T3=low , T4=low , TSH= high
Dx:-Cretinism (1ry or congemital hypothyroidism).
A child 2years old ,presented with fever for 2 weeks ,
on exam:-
his temperature = 38.9 degree centigrades , spleen ,L.N all are NOT palpable ,liver
1finger palpable.
1. mention two possible differential diagnose?
2. mention most important investigation ?
Hint:
Platlets count=60
Hb=6g/dl
Bilirubin=normal
WBCs =5000 (5 x 10
9
/L)
DDx:
1-leukemia
2-Aplastic anemia
Others (rarely parvovirus infection, infectious mononuclosis)
Investigation:-Bone Marrow exam.
Note: always consider B.M exam in pancytopenia .(very imp)
When two line of cell affected in bone marrow then we need BM biopsy
29
Neonatal jaundice:
65% of infants are having jaundice in 1
st
wk of life.
In most cases it is benign condition & resolved spontaneously.
Others are pathological and can end with persistent damage and kernictrus.
Pathophysiology of physiologiacal jaundice:
-the liver is incapable of dealing with the excess bilirubin, this excess bilirubin resulted
from the normal polycythemic state of the infant in the intrauterine life,when baby is
delivered there will be no need for the polycythemic state (lazy circulation is being
established),and hyperviscosity syndrome so the excess RBCs will be degraded &
bilirubin level will start to raise .
-This bilirubin needs mature hepatocytes to be dealt with & sufficient amount & activity
of transferase enzymes.
-Prematurity predisposes neonates to more severe jaundice.
Notes:
Dusky color of a neonate masks the yellow tint of jaundice and that is explaining the late
presentation of jaundice baby.
Hb in neonate= 18 ± 2.
There is physiological anemia in 2 months infant
[Hb] =9g/dl (full term baby) and 7.5g/dl (preterm baby).
Bilirubin is one of the most potent anti-oxidant, when it is raised in the early days of life
this will help in getting rid of the free radicals.
1g/dl of Hb will give 34mg/dl of bilirubin.
Papkin's reflex: palmomental reflex, if persisted beyond 4-6mo, this is mostly due to
frontal lobe damage "CP".
Glanzmann disease: platelets dysfunction.
In first days of neonate life Hb < 18 mg/dl considered anemic
If [Hb] is <9 g/dl (in full term) or <7.5 g/dl (in premature)Consider the baby as anemic .
30
Hx of baby with jaundice:-
1- Cause
2- Effect of this jaundice
3- Duration (in hours not days)
4- LMP/EDD
5- Birth weight, Rh, ABO of father and mother
6- Prenatal (mother's disease, chemical exposure, drugs, Hx of maternal hepatitis.
7- Natal (mode of delivery)
8- Postnatal Hx
-Did he cry immediately after birth? Needed resuscitation?
- Time of start of feeding? Type?
- Child now receives adequate nutrition?
9-ask about signs & symptoms of kernicterus?
-Poor sucking
-Poor reflexes (by examination absent Moro reflex)
-Lethargy
10- Family History:
- Any of siblings have the same condition?
- Needed phototherapy? Exchange transfusion?
- Hx of hemolytic diseases (G6PD" & hereditary spherocytosis ) or early cholecystectomy.
At last you can say: the health of the baby is severely disturbed.
Example:
A baby who was delivered by NVD at (39) wks was presented to hospital with jaundice
started at 2
nd
day as it was observed by the family.
Physical exam:
Is it jaundice really??
By gentle pressure on the nose or forehead or sternum.
What is the cause?
What is the effect?
#β-thalassemias and sickle cell disease can’t present as neonatal jaundice as
there is minimal HbA in the first 3-6 months of life an the majority of Hb is HbF.
# α- thalassemia can present as neonatal jaundice.
31
Eye exam: if the eyes are closed by holding the baby from axillae, bending him
forward & backward, he will open the eye & we can see the sclera.
Don’t try to open eye forcefully because this can lead to orbicularis oculi muscle
damage.
Measure the wt?
Mature or premature?
Dysmorphic features?
Anterior & posterior fontannelles? "wide posterior fontannelle in hypothyroidism"
Birth markers? (bruises & cephalohematoma).
Hepatosplenomegaly?
Rash? "TORCHS infection & severe Rh incompatibility"
Anemia "pallor"
Activity "primitive reflexes"
Important definitions:
Small for gestational age: birth weight <10
th
centile mostly due to IUGR as a result of
placental insufficiency "fetal hypoxia" → 2ry polycythemia increase Hb breakdown
increase bilirubin → jaundice
Large for date: birth weight >90
th
centile infant of diabetic mother.
Poorly controlled maternal diabetes intermittent periods of hyperglycemia
Hyperglycemia in the fetus stimulation of insulin, insulin like growth factors,
growth hormone, and other growth factorsstimulate fetal growth and deposition of
fat and glycogen Macrosomia
LBW: Birth weight <2500kg.
Premature: baby NOT completed 37wks gestational age calculated from 1
st
day of LMP.
Full term: 37-42 wks
Rash + jaundice = TORCH infection
Criteria of physiological jaundice?
Important من محاظرة النظري
10
th
- 90
th
centile he is appropriate for age
32
Rh incompatibility:
-No naturally occurring Anti-D, it should be given once there is suspicion of feto-maternal
bleeding: abortion, birth trauma, previous still birth.
-Anti-D must be given at 28-32 wks of gestation within 72 hrs after delivery to prevent
sensitization of maternal blood.
-Once sensitization occurs ( anti-D titer in maternal blood) Anti-D injection is useless.
History : yellowish discoloration started from the 1
st
day ,his mother Rh-ve.
His brother has the same condition, or one of his brothers has kernicterus.
4 investigations:-
1- TSB: direct and indirect
2- CBC and retic count.
3- hematocrit (PCV)
3- Rh & ABO testing
4- coomb's test: strongly +ve.
ABO incompatibility: >common than Rh incompatibility.
Mother =O
Infant=A/B/AB.
Investigations:
Coomb’s test= weakly –ve or weakly +ve.
Retic count:
Hb: ↓
In the film of ABO incompatibility :
Brisk spherocytosis, this condition is
also encountered in:
1- Autoimmune Hemolytic anemia.
2- Burns.
Note: we give anti-D to the mother to get rid of the RBC
s
that is escaped from baby’s blood to maternal blood
TO PREVENT MATERNAL IMMUNE SYSTEM FROM BEING SENSITIZED AND PRODUCTION OF IT’S OWN Ab
s
#
When there is sign of hemolysis with -ve coomb’s
test you should think about:
-ABO incompatibility.
-non immune cause of hemolysis as:
1. Enzyme deficiency ( G6PD,PK deficiency ).
2. Cell membrane disease spherocytosis
3.alpha Thalasaemia.
#Mother A (or B) have baby with B(or A) is there any sensitization?
-Although Anti- A & Anti - B Ab are naturally present without previous immunization that
is usually in the form of IgM that can not cross the placenta, but when the mother exposes
to A or B Ag (during first ABO incompatibility pregnancy or abortion ) leading to maternal
sensitization & formation of IgG which can cross the placenta leading to fetal hemolysis
during 2
nd
or next ABO incompatibility pregnancy .
33
G-6-PD deficiency
Characteristics:
-↓Hb
-↑ Retic. count.
- Family Hx: +ve X- linked recessive (Brother, mother,
aunt)
- Coomb's test -ve .
The mother is carrier in 40-60% of cases.
Management of jaundice in the 1
st
week of life:
-25 mg/dl Bilirubin is considered the limit border
Either there is no need for Tx especially if there is no hemolysis, full term baby, healthy
active and the jaundice is not deep with criteria of physiologic jaundice.
-For safe management start at 20 mg/dl to prepare for blood transfusion
Double volume exchange
Technique: a double volume exchange removes approximately twice the infant
circulating blood volume 170 ml/kg of the (infant is approximately 80-90 ml/kg body
wt.) replacing it with cross matched whole blood. The procedure involves placement of
central catheter and removing and placing blood in a volume that is approximately 10%
or less of the infant blood volume.
Most of bilirubin is extravascular, as a result exchange transfusion remove
approximately 25% of the total body bilirubin, after the procedure serum bilirubin falls
to approximately ½ of pre exchange value then increases to ⅔ of that levels as
extravascular and vascular bilirubin re-equilibrate .
Side effects of exchange transfusion
1.Hyperkalemia (if old blood is being used > 72 hours).
2. Hypocalcemia ( if Ca
++
hadn't given)
3. Hypoglycemia (Glucose must be monitored especially in Rh incompatibility because of
hyperinsulinemia or pancreatic islet hypertrophy).
4. Volume overload (if your transfusion wasn't accurate).
5. Shock (if large amount had been drawn at first).
6. Anemia (if you didn’t shake well the contents, RBCs precipitate downward)
Lyon hypothesis: Randomly one x
will be inactivated, other one
remains active
(dose effective).
34
-you should monitor the heart
-Should be in a controlled environment to avoid hypothermia
-Acid glucose-phosphate added
-Phosphate chelate the calcium can lead to convulsion because of hypocalcemia.
-Bicarbonate added to resolve acidosis.
-MR (mortality rate) is 1-2%
-Advice mother to prevent feeding before 1 hour of procedure.
-Check blood glucose.
-Q/Pt. with Rh incompatibility glucose + hypothermia, why?
A/ patient Rh incompatibility has
Nesidioblastosis which means hyperinsuliemic
hypoglycemia
(due to hyperplasia of pancreatic islet cell this lead to surge secretion of
insulin which cause hypoglycemia).
Phototherapy
-visible spectrum of light (it is NOT ultraviolet light).
-The most appropriate spectrum is blue light with 450nm wave length.
Mechanism: bilirubin in the skin absorbs the light energy which by photoisomerization
converts the toxic unconjucated bilirubin to a product which can be excreted in bile
without the need for conjucation,also phototherapy converts unconjucated bilirubin to
lumirubin which is excreted in the kidney.
Side effects of phototherapy: ( very important).
i
Hypo/hyperthermia
ii
Dehydration
iii
Diarrhea
iv
Rash
v
Bronze baby syndrome (if the pt. has direct hyperbilirubinemia).
vi
Eye injury & nasal obstruction.
Note:
TSB at first 7hrs, begin to rise, then it goes down as the phototherapy continued.
As you perform phototherapy, you should increase the maintainance fluid by 10%-30%.
35
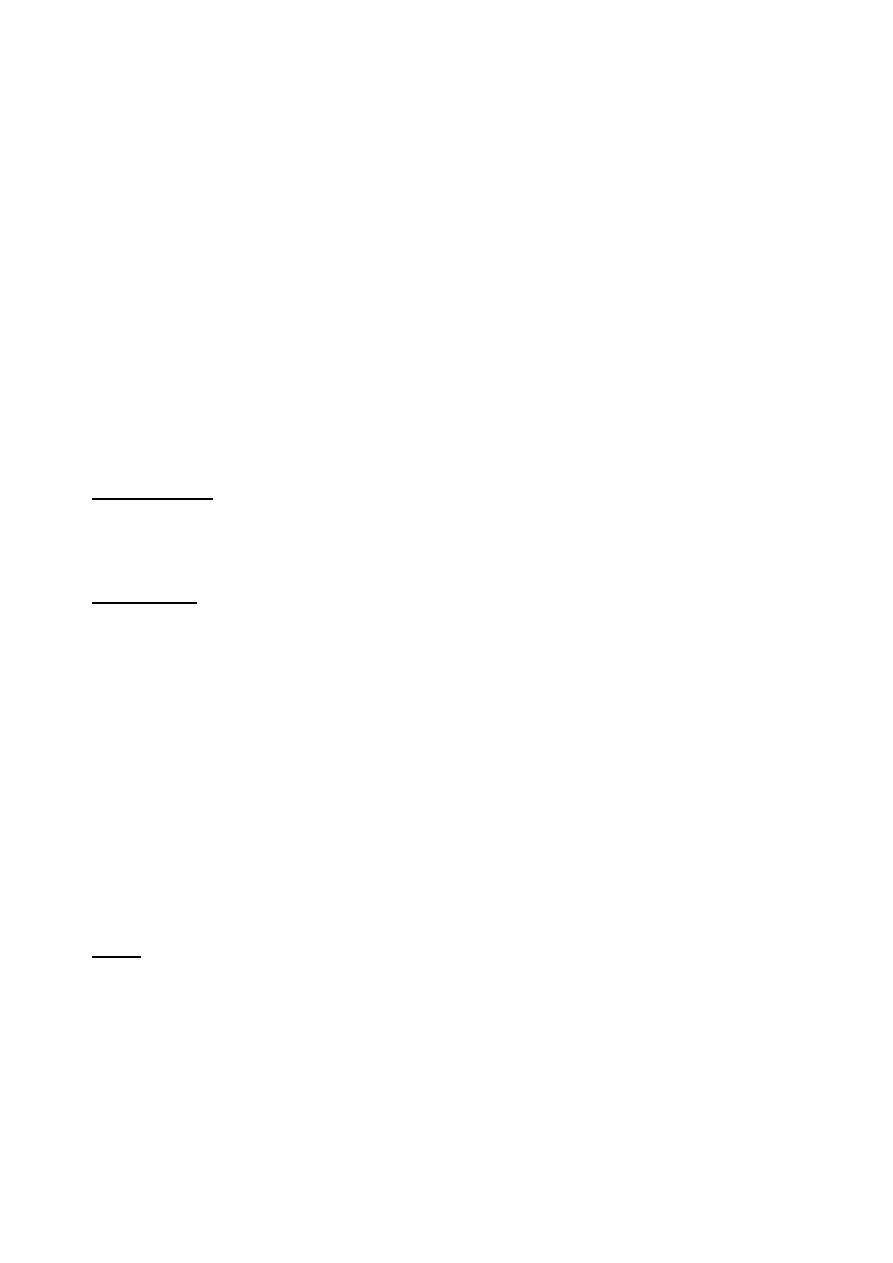
Jaundice (prolonged neonatal jaundice): >10days
Divided into two divisions:
Indirect hyperbilirubinemia
Cholestatic jaundice
Conjugated (direct) bilirubin <20%
of total Serum bilirubin.
Conjugated (direct) bilirubin >20%
of total serum bilirubin
**4 causes prolonged jaundice:
1-Hemolysis
2-crigler-Najjar syndrome
3-Breast milk jaundice
4- Hypothyroidism.
Prolonged jaundice + indirect hyperbilirubinemia screening for hemolysis is
indicated.
Direct hyperbilirubinemia
1-Extrahepatic biliary atresia: clay color stool, portal hypertension.
# Surgery is the only treatment: kasai-portojejunostomy. (Alkaline phosphatase raised
as there is biliary obstruction)
#Mal-rotation of mid gut diagnosed by: Ba enema.
#Choledochal cyst diagnosed by Ultrasound.
2-idiopathic neonatal hepatitis mostly male, normal color stool & consistency for
some time before the condition deteriorates//ALT & AST will be raised.
How to differentiate between the two?
By HIDA test: Radio-isotope in vein:
if the uptake is Normal but the excretion is slow
biliary atresia.
idopathic neonatal hepatitis عكس هذا يحدث في
Rx:-
1- Medium chain triglycerides.
2- Vitamins injection (A, K, E, D).
3- Cholestramine
4- Supportive care.
5- Liver transplant.
36
Others:
o TORCH serology
o HBV/HCV serology
o Sepsis (Blood, CSF & urine cultures)
o UTIurine culture.
o Cystic fibrosissweat chloride test
o Alpha -1- anti-trypsin deficiency (immunoassay).
o Galactosemia (deficiency in Glucose -1-PUT): this enzyme is estimated in RBCs &
fibroblasts//if there is +ve reducing substance in urine other than glucose means
galactosemia (Isomil is prescribed for them)
Notes:-
Glucose deposition in the eyescataract.
In brainconvulsion
In kidneyRTA
In liverjaundice
37
Lec.1
Pediatrics
6
th
stage
2016/8/14
Session notes
د
.
بسام
Shortness of breath:
NOTES :
Duration acute or chronic
If patient presented with recurrent pneumonia and received antibiotics With
no improving think about Foreign body aspiration
Asthma a common cause for recurrent admission
Using accessory muscle of respiration mainly sternocleidomastoid muscle in
respiratory distress causes head nodding.
Frontal bossing is one of the features of rickets.
Infant with breast feeding more liable to rickets.
Vit. D deficiency patient more risky for asthma.
Bowing of the leg during the period (8 – 24) months is physiological.
Delayed tooth eruption can be due to Rickets
Ask also about: Bluish discoloration, whooping cough.
Whooping cough: rare in the 1
st
year of life.
#Post – tussive emesis is not characteristic (but not pathognomonic).
#Ask about feeding, sleeping if there is disturbance,
indicate severity of disease.
#Ask about convulsion, whooping cough can lead to convulsion
by inducing cerebral hypoxia.
IN reveiw :
Renal :
-Ask about: urine output Very important.
- UOP in pt. with SOBis a sign of dehydration.
- Dehydration may cause pre-renal failure.
__________________________________
Characteristic: one of the
disease features.
Pathognomonic: specific
only for this dis.
Causes of post-tussive emesis:
Asthma, Bronchiolitis and
whooping cough.
Pneumonia can cause convulsion by:
1. Cerebral hypoxia or anoxia.
2. SIADHHyponatremia cerebral edema
Causes of dehydration in pt. with SOB:
1.↓ food and water intake.
2.↑ insensible loss by sweating (due to fever)
and rapid breathing
38
Prei-natal Hx: ask about:
-Maternal fever, rashes and any illness, leaking liquor, gestational age, prematurity? ,
cry immediately and NICU admission RDS
-Meconium aspiration, usage of mechanical ventilationmay cause bronco-pulmonary
dysplasia.
-
Oligohydramnios hypovoluemia heart failure
-
Polyhydramnios chest compression affects growth of lung hyopoplastic lung.
-Hypoplastic kidney in intrautrine life oligohydramnios renal failure and metabolic
acidosis at birth.
Feeding Hx:
-Is there any aspiration during feeding?
Past medical Hx:
Recurrent problems, asthma, heart failure, pneumonias.
Family Hx:
Child contact with TB patients, asthma, cystic fibrosis, kartagener syndrome.
Social Hx:
Domestic animals, overcrowding, sewage, air conditioning.
ON EXAM:
-Face of the child looks ill or will.
-Color: cyanosis? , pink color or pale
- Posture: patient can’t lie in asthma, tripod position in Severe SOB (acute epiglotitis).
- Sign of respiratory distress (flaring of ala nasi, subcostal, suprasternal resscion and use
of extra muscles of respiration), deviated trachea.
- Hydration state, level of consciousness.
Investigations:
-CXR
-Blood gas analysis (PO
2
→
normal (60-90 mmHg) if < 60 mmHg, OR PCO
2
(normal 35-45
mmHg) if > 45 mmHg Mechanical ventilator.
Causes of aspiration:
-Direct causes: Cleft palate, Tracheo-
esophageal fistula (H type), bulbar or
(psudobulbar palsy as in CP).
-Indirect causes: Over feeding, GERD,
esophageal dysmotility (transient).

39
Neonatal Emergencies
:
Birth asphaxia
First of all the asphyxiated newborn baby should be put on a resuscitation trolley where
the baby put under a radiant heater to avoid hypothermia then drying up of the baby,
the head is positioned down & slightly extended, the airway is cleared by suctioning,
and also gentle tactile stimulation provided (slapping the foot or rubbing of the back).
If spontaneous respiration started and the cardiac output improved where the color of
the baby becoming pink, then there is no need now to go onto further steps of
resuscitation, but if these measures fails to improve the condition of the baby and the
heart rate is < 100 /min so we need:-
2- Positive pressure ventilation with a 100% oxygen is given through a tightly fitted mask
& bag for 15-30 sec, subsequent breaths are given at a rate of 40-60 /min with pressure
of 15- 20 cm water. Successful ventilation is determined by good chest rise symmetric
breath sounds, improved pink color, heart rate of >100 /min, spontaneous respiration
and improved tone. If no response within 15-30 sec.
the next step is:- Ambu bag Traditionally, the inspired gas for neonatal resuscitation has
been 100% oxygen. Resuscitationwith room air (or 30%) is equally effective and may
reduce the risk of hyperoxia, which is associated with decreased cerebral blood flow and
generation of oxygen free radicals. Currently 100% O2 is recommended. Room air (or
30%) may become the preferred initial gas for neonatal resuscitation in the future.
3- Insert an endotracheal tube and start to push an oxygen through the tube by an
ambu bag, if after 15-30 sec of doing that & the baby does not improve: (no
spontaneous respiration, heart rateis < 100/min, no improvement in the color of the
baby, so the next step is:-
4- Starting chest compression (cardiac compression to improve circulation) the
compression is exerted to the lower third of the sternum at a rate of 120 per min. the
ratio of compression to ventilation is 3:1 simultaneously the color, the heart rate the
respiration and muscle tone should be assessed, if the baby did not respond after 15- 30
sec of chest compression & oxygen supply through an endotracheal tube then:-

40
5- An intravenous drugs are used after an insertion of an intravenous (usually umbilical)
catheter and as follows:-
1. Epinephrine 1/10000 (0.1-0.3) ml/kg IV or intratracheal is given for asystole or for
failure to respond to 30 sec of combined resuscitation and the heart rate is < 60/min,
this can be repeated every 5 min .
2. Volume expanders 10 - 20 ml/kg of (normal saline, blood, 5% albumine, or ringers
solution) should be given for hypovolemia,pallor,E.M dissociation (weak pulses with
norml heart rate), history of blood loss, suspicion of septic shock, hypotension or in
poor response to resuscitation.
3. Sodium bicarbonate (1-2meq/kg) should be given slowly in case of metabolic acidosis
and resuscitation is prolonged.
4. Calcium gluconate (2-4 ml/kg of 10% solution) if there is evidence of hypocalcemia.
5. Naloxone given in a dose of 0.1 mg/ kg repeated as needed when there is CNS
depression due to maternal narcotic analgesic administration during labor which will
results in respiratory depression & failure to initiate spontaneous respiration. 6.
Dopamine or dobutamine may be given in a dose of 5-20 microgram / kg/ min. this drug
may be used in severe asphyxia when there is depressed myocardial function
Kernictus
:
تفاصيل الموضوع موجودة في محاظرة د
.
بسام النظري
Sepsis and meningitis :
Check for hyperthermia or hypothermia (hypothermia > hyperthermia), lethargy ,
hardening of subcutaneous tissue.
Urgently start with empirical antibiotics:
-Either Ampicillin ( 300 mg/kg ) + Gentamicin for 2-3 weeks
-Or 3
rd
generation cephlaosporin ( Cefoxime ) + gentamicin
-Most common pathogen ( Group B steptococcus , E.coli , H.influanzae )
-Neonatal sepsis carries poor prognosis ( fatality rate).
41
Neonatal hypoglycemia
:
-It is dangerous because it may end with brain damage
-Risk factors are: hyperinsulenemia as in pt. with Rh incompatibility, premature baby,
IUGR, low birth weight, polycythemia.
-Can be presented with seizure, lethargic, apnea.
-Tx: dextrose 10% by IV infusion avoid > 10% dextrose as it is irritant to vein
(thrombophilibitis), if >10% dextrose is needed use central vein.
-Initially start wit bolus dose 200-400 mg/kg
-Maitenance 6 mg /kg .
Hemorrhagic disease :
-Check for petechea, melena, heamtemesis, Caused by clotting factor deficiency
(hepatic immaturity, vitamin K deficiency).
-Vit . K deficiency result from insufficient amount of normal intestinal flora
Patient with breast feeding more liable for Vit . K deficiency.
-Tx : Vit. K replacement 5-7 unit, 1 unit prophylaxis
If there is severe hemorrhage or no response vit. K give Fresh frozen plasma
Neonatal seizures
:
-Stop convulsion urgently to avoid cerebral anoxia
-usually occur 12–48hr after delivery.
-Can be generalized or focal, and tonic, clonic, tonic-
clonic or myoclonic.
-Startle or Moro reflexes, normal jittery movements
(fine, fast limb movements that are abated by holding affected limb), Sleep myoclonus
(REM movements).
Tx :
IV phenobarbital (10–20mg/kg bolus; give further 10–15mg if seizures persist after
30min maintenance dose 5mg/kg/day)
Non-accidental injury (child abuse):
Check for :
Delay in seeking medical attention.
The details of the mechanism of injury are implausible, different stories with different
informants, injury inconsistent with the story mentioned by family.
Avoid using bolus dose in an infant of diabetic mother
with hypoglycemic pancreatic overstimulation which
result in resistant hypoglycemia.
Subtle seizure patterns (lip-smacking,
limb-cycling, eye deviation, apnea, etc.)
can be difficult to identify or
differentiate from other benign
conditions that may mimic seizures.
42
Lack of concern by the person accompanying the child.
Abnormal behavior or demeanor by the child e.g. withdrawn, avoiding eye contact. This
should be observed in the context of the child's background – for example it is usual to
avoid eye contact in some Pacific cultures.
Direct disclosure by the child that the injury was deliberately inflicted.
Bruises, Thermal burns and multiple fractures shown by X-ray at different stages of
healing
Congenital malformation
:
Bilateral choanal atresia : presented with difficult feeding , cyclical apnea and cyanosis
that is relieved once the child cry (become pink and cyanosis disappear) as the
neonate is obligatory nasal breather.
Dx 1. Simply by inserting an NG tube through the anterior nostrils→ resistance to
flow through posterior choana.
2. CT-scan.
Esophageal atresia.
Neoanatal intestinal obstruction: Cause gangrene
sepsis
death
-Usually result from duodenal atresia , imperforated anus , volvulus and malrotation.
In upper intestinal obstruction vomiting preceding the constipation in lower intestinal
intestinal obstruction constipation preceding the vomiting
Necroting enterocolitis :
Cardiac malformation: TGA , critical coarctation of
arota, hypoplastic right ventricles , tricuspid atresia
-Presented with early birth cyanosis
Rx→ prostaglandin to maintain duct opening.
Renal :
-Hypoplastic or agensis of kidney treated by kidney transplantation
-If urine not pass check for bladder may be due to posterior urethral valve obstruction if
the cause in the kidney may be pelvic uretiric junction obstruction , mass (teratoma).
-Meningiomyocele
More risky if leaking→ closed by surgery
Life threatening birth injury :
By forceps during delivery cause depressed skull fractures or intra-cerebral hemorrhage,
Subglial hemorrhage may result in → hypovolumia
-Check blood to exclude if there is bleeding tendency
-Give the child BT or NS or any volume expander
Bilateral phrenic nerve palsy: Transient and patient need assisted ventilation
Duct dependent CHD:
1.Pulmonary atresia
2. Severe a stenosis
3. TOF with severe pulmonary stenosis
4. Coarctation of Aorta (severe)
5. Interrupted Aortic Arch
6. Hypoplastic Left Heart

43
Splenic , hepatic injury:
-Need urgent correction to stop bleeding
-Check for ecchymosis , hypovolumia
-Investigate by US
Bilaterla femoral fracture
Congenital adrenal hypoplasia
In children with the more severe form of the disorder, symptoms often develop within
2 or 3 weeks after birth.
Poor feeding or vomiting
Dehydration
Electrolyte changes (↓Na+ ,↑K
+
) → due to ↓aldosterone level.
Abnormal heart rhythm
Girls with the milder form will usually have normal female reproductive organs (ovaries,
uterus, and fallopian tubes). They may also have the following changes:
Abnormal menstrual periods or failure to menstruate
Early appearance of pubic or armpit hair
Failure to menstruate
Some enlargement of the clitoris
Exams and Tests
Your child's health care provider will order certain tests. Common blood tests include:
-
The goal of treatment is to return hormone levels to normal, or near normal. This is
done by taking a form of cortisol, most often hydrocortisone. People may need
additional doses of medicine during times of stress, such as severe illness or surgery.

44
Lec.1 Pediatrics
6
th
stage
Session notes
د
.
فارس الصواف
Respiratory emergencies
Notes:
Melena : Shiny black tarry stool
Viral hepatitis : presented with jaundice, hepatomegaly, abdominal pain and the most
important symptom is loss of appetite, so try to save the patient with good feeding,
well dehydration, encourage carbohydrate intake and avoid diet restriction
Respiratory ER:
Croup: is not an emergent condition, but need monitoring in the severe cases to
resuscitate the patient by endotracheal intubation, or tracheostomy if there is any total
upper air way obstruction that may be associated with disturbed level of consciousness
-Use steriod on demand (don’t let the patient die before giving him steriod)
-Steriod can be used until 2 weeks safely (1 week on textbooks) and stoppe without
tapering.
Acute epiglottitis:
It is life threatening condition (Total airway obstruction).
Severe bacterial infection of epiglottis and subepiglottic fold
Bacteria: Hemophilus infleunzae type b, Strep.pyogens
Features: sudden onset, high fever, toxic, sore throat, dysphagia, tripode position,
drooling of saliva, dyspnea, collapse, coma, death (in few hours).
Clinical diagnosis (not use tongue depressor
lead to respiratory obstruction)
Don’t take history, don't do x-ray.
Blood culture investigation is hazardous.
Do examination in theater room with available tools for intubation, tracheostomy and
anesthesia.
All children need intubation for 2-3 days.
Antibiotics: for H.infleunzae (amoxicillin or ceftriaxone) for 7-10 days 3
Then send child to home.
Give rifampicin to house hold members for 2 days to prevent meningitis due to
H.infleunzae.
Avoid ceftriaxone in children espicially with breast feeding
Procaine pencillin best drug for H.inf
Chloramphenicol also can be used ( S/E : aplastic anemia )
Some medical schools administer steriod for aryepiglottic fold inflammation
Foreign body inhalation (aspiration)
Common in infants and toddlers
45
(Infant can swallow F.B because they explore environment by their mouth).
Inhale things like: خرز، سمش بح ،قتسف
History: very important, healthy baby, sudden onset, parent denies something (social
circumstances).
Cause acute strider.
First stage: severe paroxysm of cough, cyanosis, chock, sneezing, gagging.
Second stage: Misleading (like a recovery state).
Third stage: symptoms of complications because F.B go to the right lung and lead to
atelectasis, pneumonia, tachypnea, cyanosis, retractions, fever, and other symptoms.
Diagnosis clinically
Investigations: CXR should be done in deep inhalation see localized hyperinflation,
most are radio-lucent.
Treatment: upside down, big thrust on baby back, laryngoscope or bronchoscope,
tracheostomy (trans-thoracic approach).
In presistent pnemonia think about FB inhalation
Or H-type TEF fistula in slowely resolving pneumonia
Penmonia : The commonest bacteria in pneumonia in all age groups are strepto
pnemoniae, H.influenzae.
o Neonate (less than 3 or 4 weeks) : group B strepto, E.coli, G+ bacillus. o Pneumonia in
neonate is like septicemia : give parenteral antibiotics for two weeks then admission.
o After neonate : viral infection.
o After 3 months : chlamydia, uroplasma, mycoplasma.
o After age of 5 years : most common is strepto pneDiagnosis by CXR opacity, patchy
infiltrate (viral), lobar infiltrate (viral).
Staph. pneumonia:
o High fever, toxic, dramatic and progressive course.
o CXR very characteristic : lung abscess, empyema, plural effusion, pneumatocele.
o Come with septicemia and coma.
o Blood culture (+ve in 10% only)
o Give anti-staph drugs. (vancomycin , gentamicin , fluxacilliin) with supportive
treatment , IV fluid , monitoring.
-bronchiactasis beast treated by physiotherapy and antibiotics
For mycoplasma pneumoniae azithromycin or clarithromycin.
For pneumococcus amoxicillin for 7-10 days (40-100 mg/kg in day)
Indication for hospital admission:
o Need O2. o Less than 6 months age.
o Need fluid and supplements.
o Immuno-deficient baby.
o Slowly resolving pneumonia.
o Multiple infections. umoniae then mycoplasma pneumonia.
46
Status asthmaticus
Chest X-ray (CXR):
o Is indicated in:
1- First attack to exclude other DDx (no need to repeat CXR in the other attack).
2- If we treating the patient with his good compliance but the patient condition still NOT
stable, perform CXR to diagnose complications or to exclude other Diseases
o Findings like pneumothorax, atelectasis, mediastinum widening
Peak expiratory flow (PEF):
o Very important but is indicated in children who are 6 years old age or
Short acting B agonist (SABA).
Inhaled Side effects less than oral one.
Side effects like tachycardia, hyperkalemia, tremor.
It is bronchodilator.
Like salbutamol, albuterol.
0.5 ml
for less than 5 years // 1 ml
for more than 5 years ((only ml, not ml/kg)
Very effective.
Give it with 2 ml of normal saline
use nebulizer.
Oral is as effective as parenteral.
Treatment:
Admission to ICU
Monitoring
Two rescue treatment
Inhaled and systemic corticosteroids
aminophylline infusion
Mg sulfate (IV 75 mg/kg)
ipratropium bromide
terbutaline
Adrenaline (0.01 mg/kg) SC or IM (very painful)
Ventilator
No need for
Oral beta 2 agonist / Ketotifen (anti-histamine) / Antibiotics /Oral
bronchodilators (side effects).
Aminophylline :
-Give it by infusion
-The bolus dose 5 mg/kg ( slowely )
-Maintenance 0.7-1 mg/kg by infusion pump
-Don’t give aminophylline in supine position , give it in lying postions
-S/E: seizure, arrythemia, vomiting, hypotension

47
-Social management with action plan (how they use the spacer, allergen avoiding, sign
of severity)
-Spiromety not used in children < 7 years not – cooperative
Bronchiolitis:
Common wheezy infection
Occur in few months up to 2 years
Above 5 years rare.
Viral infection (RSV)
Rarely mycoplasma pneumoniae.
More in boys
Breast feeding is protective.
Neonate (1 month) rarely have bronchiolitis and rarely have viral infection
Diagnosis clinically
Features: rhinorrhea, cough, sneezing, common cold, low grade fever, respiratory
distress, cyanosis, tachypnea (120/min), wheezing, flaring ala nasi, recession, tired,
hyperinflated chest, air trapping, auscultation (wheezing, fine bilateral crackles), may
feel liver and spleen (due to hyperinflation), poor appetite, refuse eating.
Not diagnose H.F with radiological evidence of cardiomegaly.
CXR: Flat diaphragm, narrow mediastinum.
Clinical cases notes:
-In convulsion exclude meningitis
-1
st
attack of convulsion + fever , < 18 months
-Lumbar puncture is mandatory because of meningitis suspicion in this age and its signs
not specific.
-If CSF in lumbar puncture is turbid by eye and exit under high pressure give him
intensive antibiotics
-Don’t say febrile convulsion if the baby is < 6 months, check for electrolyte disturbance,
hypoglycemia or idiopathic convulsion.
Case of nephrotic syndrome: التناذر الكلوي
-Edema, scrotal edema, eye puffiness
-Check for BP always in Cardiac, CNS, Renal
-Rx: steriod dependent or resistent , free sloute albumin , diuretics , K replacement
48
Diarrhea: increase frequency, consistency and liquidity of stool that is
observed by the mother.
Diarrhea (WHO): > 3 bowel motions/day (except for babies who are
exclusively abreast fed.
Approach to acute diarrhea: <14 days.
History: Same history but should include (thirst and UOP) to estimate the
severity of dehydration.
Feeding Hx: should include:
Type of feeding: breast, Bottle or mixed.
If Bottle feeding:
-sterilization method (boiling for 10 min.)
-preparation of milk.
-No. o bottles (should be= No. of feds +1)
-Type of milk.
Examination: we have to look for signs of dehydration:
1. Ant. Fontanelles → should be: At sitting position + baby not crying ( .)مهم
2. Sunken eyes.
3. Mucus membrane.
4. Skin Turgor → should be <2 seconds, if >2 seconds → dehydration.
5. UOP.
Investigations:
1. Serum electrolytes:
2. RBS (random blood sugar).
3. Blood urea and serum creatinine.
4. CBC: -RBC and HB: Normal or ↓
-shift to left {e.g: neutrophia +band cells (bandemia)}
→ suggest shigellosis.
-PCV {normal or ↑(hemoconsitration)}
-platelet: normal or ↓ (in case of HUS)
-Na
+
(N.R 135-145 mEq/l)
-Ca
++
a(N.R 8.5-11 mg/dl)
- K
+
(N.R 3.5-4.5 mEq/l)
-HCO
3
-
-PH
HUS: is a triad of:
1.Microangiopathic anemia (helmet and
fragamented RBC in blood film).
2. Thrombocytopenia.
3. Uremia.
Note: presence of 2 out 3 + predisposing
factors can make the Dx .
6th stage Pediatrics Lec.2
د
.
ربيع
Session notes 2016/8/21
49
5. General stool exam: Mcroscopic, chemical and microscopic exam:
Macroscopic: volume, consistency, color …etc
Chemical: -PH→
-Reducing agents: if +ve
→ (e.g lactose intolerance)
-Occult blood.
Microscopic:
1. RBC
2. Pus cells
3. Fatty cells
4. Cysts or trophozoits.
_________________________________________________________________
Approach to a pt. with chronic diarrhea: >14 days
We can classify chronic diarrhea into 3 types:
1) Chronic diarrhea without FTT.
2) Chronic diarrhea with FTT.
3) Chronic diarrhea with blood.
________________________
1)DDx of Chronic diarrhea without FTT:
Lactose intolerance.
Giardiasis.
Toddler’s diarrhea.
Color of stool:
-red →blood
-Non-bilious→ Cholera,
obst. Jaundice.
-Green → rapid transient
time (benign)
-Normal PH is alkaline (because of HCO
3
)
→Whenever it’s acidic→ considered abnormal (e.g
lactose intolerance) except in breast fed baby.
DDx:
1.Infection: Bacterial (shigella, salmonella,
yersenia,capelobacter…etc) or protozoal.
2. Cow’s milk allergy.
3. IBD.
4. Post antibiotic psuedomembranous colitis.
FFT: definitions:
Child with weight persistently <5
th
centile.
Child who had crossed 2 major percentiles
in a period of 2 months.
Child’s weight < 80% of the median
weight for the height
of the child.
NOTES: مهم باألمتحان
CASE1: Pt. with diarrhea get improving →develops
abdominal distention → what is the Dx? And how to prove
it?
A/-Dx: paralytic ileus from hypokalemia .
-Proof: by
##Auscultation →sluggish bowel sounds
##serum K
+
(If there’s no facility to do serum K
+
) then we
can do:
##ECG (flattening of T wave, prolonged QT interval)
CASE2: Pt with chronic diarrhea →develops bloody diarrhea
→ what is the Dx?
A/ Vit. K deficiency, because of antibiotic use →Kills bact.
Flora which can produce Vit. K
50
Lactose intolerance:
Types:
1.Primary.
2. Developmental (very rare) → temporary →eg. Prematurity.
3.Secondary to (very common): celiac dis., Rota virus inf.,cow’s milk allergy…etc
How to Dx:
-Clinical: diarrhea, abd. pain & distension, exaggerated bowel sounds and
perianal excoriation.
-PH of stool: ↓
-Reducing substances: +ve
-Jejunal biopsy →Histochemical study→reduced lacose in brush border.
-lactose tolerance test: flat (no ↑ in glucose after CHO meal).
-H
+
breath test: ↑ (as aresult of bacterial fermentation of undigested
lactose)
Rx: Lactose free formula (LF) → Isomil
Soy milk(isomil)→ for 2-4 wks then re-introduce
into ordinary formula.
_______________
Giardiasis:
How to Dx:
1. Finding trophozoites (not cyst) in FRESH stool: (25% +ve).
2. Dudenal aspirate: (75% +ve).
3. Metronidazol trial.
Rx: 20-30 mg/kg metronidazole for 10 days.
_______________
Toddler’s diarrhea:
How to Dx: by exclusion of other causes of
chronic diarrhea. (Correlate to IBS in adults).
Isomil used only in:
1.Galactossemia.
2. Lactose intolerance.
3. Cow’s milk allergy
Q/What is the difference in metronidazol use in
amebiasis and Giardiasis?
A/ in amebiasis:
50 mg/kg metronidazole for 2 wks in divided
dose to be followed by diloxanide furoateor
paromomycin to get rid of cysts in order to
prevent relapses
51
2)DDx of Chronic diarrhea with FTT:
Lactose intolerance.
Giardiasis.
Celiac Dis.
Cystic fibrosis.
Bact. Overgrowth.
UTI.
Endocrinpaties→ thyrotoxicosis, Addison’s dis., VIPomas
Cow’s milk allergy.
___________________
Celiac Dis.:
Presentation: Abd. pain & distension, chronic diarrhea (large, greasy, offensive)
poor weight gain, anorexia, vomiting …etc .
How to Dx:
1.Serology: anti-tissue transglutaminase IgA ab
and total IgA.
If anti-tissue transglutaminase Ab is ↑
and total IgA is normal then we have to do:
2. Dudenal or jejuna biopsy: Histopathological findings:
-Total or subtotal villous atrophy.
-Deepening of the crypts of langerhans (cryptitis)
-Intraepithelial and submucosal infiltration of lymphocytes and plasma cells.
## If the above findings was found + serology ↑ titer → definitive Dx.
Rx: Gluten-free diet for life long.
___________________
Can cause chronic diarrhea
WITH or WITHOUT FTT
NOTE: celiac dis. Is never diagnosed
<9 months age.
Celiac syndrome: diseases similar to
celiac dis. But it’s not celiac dis.:
-Tropical sprue.
- Giardiasis
-Malnutrition.
-Eosinophilic enteritis.
Note: Malignancy (lymphoma and
pancreatic CA) is a possible
complication of celiac dis.
Note: Gluten-free diet dose not
eliminate the risk of malignancy.
52
Cystic fibrosis:
How to Dx:
1. It can be diagnosed 1 hr. after birth because it can cause meconium ileus.
2. Sweet chloride test →>60 mmol/L
3. DNA diagnosis.
Can cause bronchiectasis as result of recurrent chest infection→ can cause death.
Rx: Antibiotics + physiotherapy.
__________________
UTI: Very important → DDx of many complaints.
How to Dx:
1. GUE → >5 pus cells/HPF
2.Urine culture (main diagnostic method) : specimen:
- Mid-steam urine :
## >100,000 colony/ml of the same M.O →UTI
##10,000 colony/ml→ NOT UTI.
##10,000 - 100,000 → Suspicious → Repeat the test or do more accurate
method
-Suprapubic aspiration→ if single colony is recovered→ definitive Dx of UTI.
Or- Urine obtained by foly’s catheter→If single colony is recovered→UTI.
3. U/S
4. MCUG
If the above mentioned investigations are:
- Norml → No need for IVU.
-Abnormal → we have to do IVU to estimate the remaining functioning part of the
kidney →If the kidney is still functioning →it’s worth to do surgery for VUR dis.
→If the kidney is scarred → No need to do the corrective surgery.
To Diagnosis Vesicouretric reflux dis. In pt. with recurrent UTI.
53
Rx: cystitis →symptmatic Rx + Antibiotic (amoxicillin or 3
rd
generation
cephalosporin as cefixime) orally for 7-10 days.
Pyelonephritis→ Hospitalization +symptomatic Rx + Antibiotic (combination of
3
rd
generation cephalosporin + amynoglycoside) parenterally for 10-14 days to be
switched into oral therapy once the pt. is able to.
Cow’s milk protein allergy: (Casein protein):
Presentation: bloody diarrhea, abdominal pain, urticaria, runny nose and even
FTT.
How to Dx:
1. Challenge test.
2. Specific Ab
Rx: Extensively hydrolyzed formula.
____________________
3)DDx of Chronic diarrhea with Blood:
Post-antibiotic pseudomembranous colitis.
Lec.3 Pediatrics
6
th
stage
2016/8/23 Session notes
د
.
ربيع الدبوني
General notes:
Palpitation: never mention in the history of child (<3 years) who are not old
enough to express such a feeling. →"palpitation " because it is subjective
( it is feeling by the patient him/herself )
Feeding Hx :
Ask about any new introduction of unmodified cow's milk?
Convlusion is pyrmidal tract in origin, while occulogyric crisis is extra-pyramidal origin.
Child with no symptoms, no murmurs upon auscultation and normal ECG and CXR
(no cardiomegaly)→ unlikely to have cardiac problem (CHD) →NO matter to do ECHO.
Note:
30-50 % of pt. with cow’s milk
allergy have soy protein allergy
54
Chyne-stoke breathing: special breathing pattern characterized by tachypnea
that is slowly come down followed by a period of apnea then tachypnea
progress again.
-This is normal condition in premature babies in first few weeks of life and
even in healthy full term babies, usually after sleeping deeply.
-This is abnormal is adults → indicating severe brain damage, renal failure.
Home care: supine position, avoid soft pillows and smoking, never shake
baby to breath as it may cause brain injury.
CVS notes
Apex beat:
o Apex beat outermost, lowermost visible or palpable to the left or right
o If you don’t find the pulsation; look at the axilla (left side), if you still don’t
find the pulsation; see the right side (dextrocardia)
Regions in auscultation:
o Mitral (Apex) area : 4th left ICS at mid-clavicular line or 5th
ICS in older child.
o Aortic area : 2nd ICS right to the sternum
o Pulmonary area : 2nd ICS left to the sternum
o Tricuspid area : left sternal border in 4th ICS or 5th ICS in older child
Coarctation of aorta is characterised by the following features
Usually seen in male patient and they presents with headache, claudication,
palpitation, anginal pain or cold extremities.
The upper extremity and thorax may be more developed compared to lower
extremities.
Radiofemoral delay is present.
All the peripheral pulses should be examined carefully
Prominent suprasternal and carotid pulsations are present
Dilated pulsating collaterals especially intercostal arteries which can be seen
in the inter-scapular region posteriorly (Suzman sign).and is best elicited with
patient bending forward with arms hanging by the side of the body.
Systemic hypertension.
Bruit over the collaterals.
Left ventricular type of cardiac enlargement and heaving apex is seen.
A systolic murmur may be heard over the anterior chest and back.
Continuous murmur is heard over the collaterals.
Causes of absent apex beat:
1.obesity.
2 .Thick chest wall
3. pericardial effusion
4. Dextrocardia
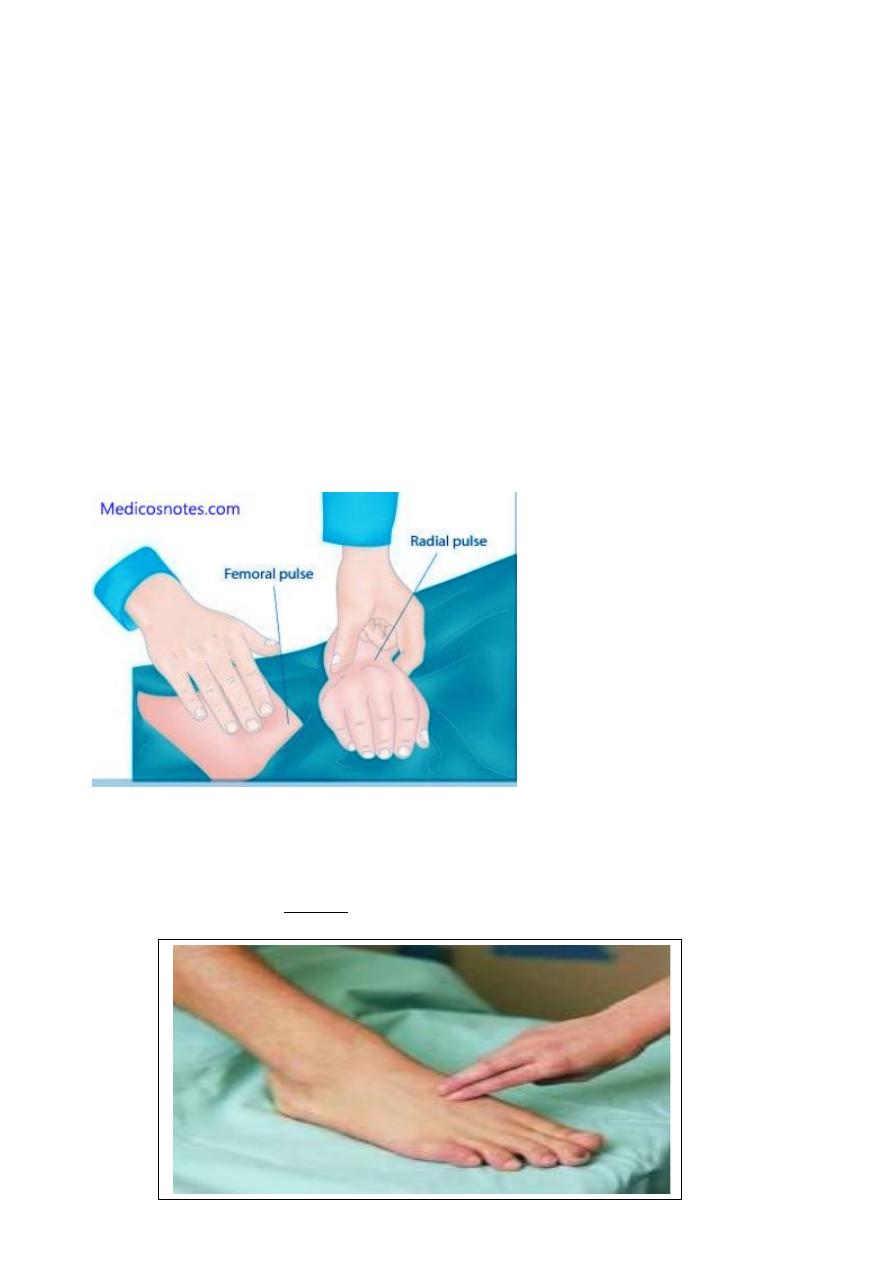
55
Clinical association of coarctation:
Bicuspid aortic valve
Turner’s syndrome
Berry aneurysm
Polycystic kidney
Radio radial delay:
To detect the radioradial delay you should simultaneously palpate both the
radial arteries by both your hands, using your left hand for patient’s right
radial artery and vice versa
Normal situation radial and femoral pulsations are felt equally and
synchronously. The inequality between two radial pulses is known as Radio
radial delay. The delay between the radial pulse and femoral pulse is called
as Radiofemoral delay.
Dorsalis pedis exam :
The pulse of the dorsalis pedis artery, palpable at the prominent arch of the t
op of the foot between the first and secondmetatarsal bones. It can be felt in
approximately 90% of people.
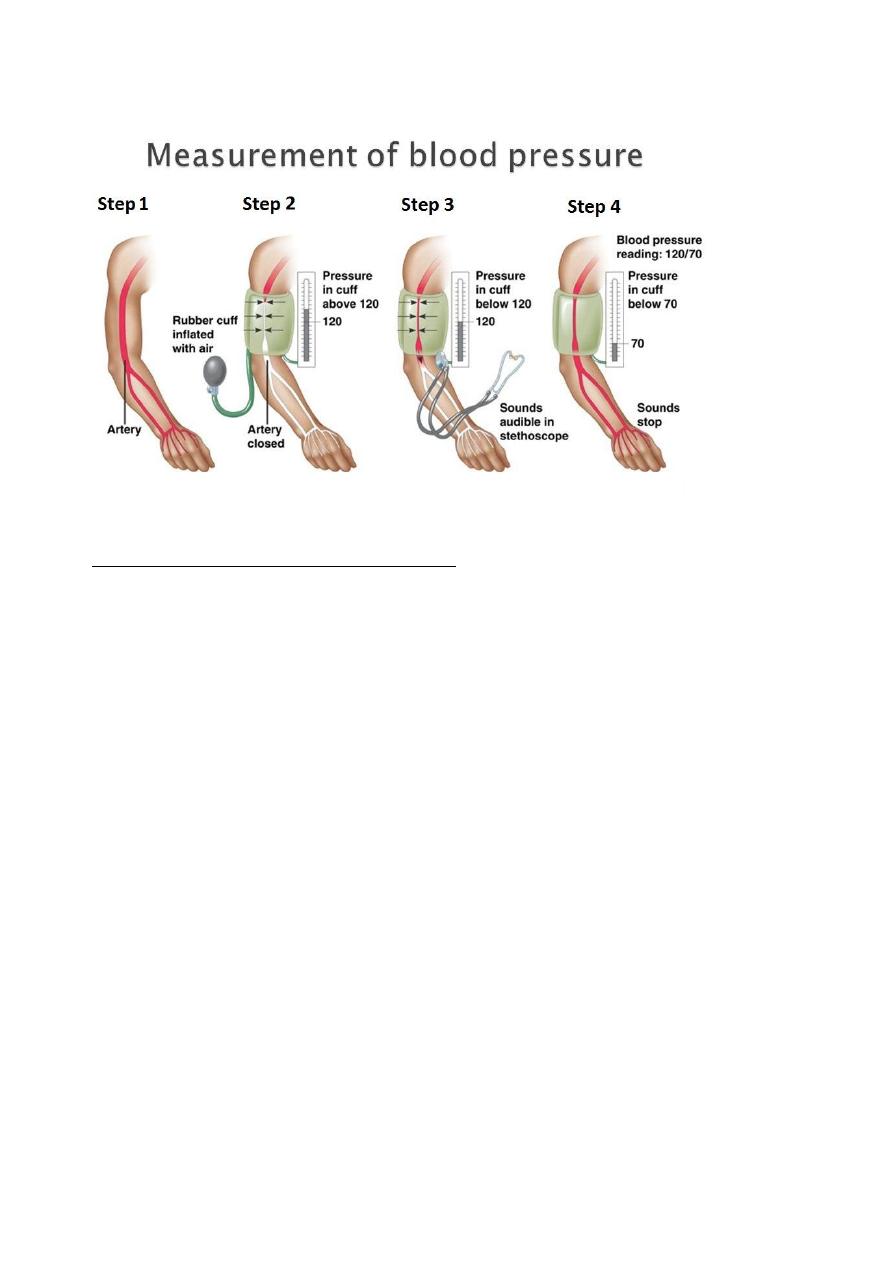
56
Blood pressure measurement:
Flush method:
Flush technique for obtaining pediatric BP:
Used in infants or very young children where lack of cooperation precludes
use of auscultation and palpation to determine BP
The flush technique allows for a value lying between the systolic and diastolic
to be determined
With the cuff in place, an elastic bandage is wrapped around the elevated
arm
Proceeding from the fingers to the anticubital space emptying of the
capillaries and venous network occurs
The cuff is now inflated to a pressure above the expected systolic reading
The bandage is removed
The now pallid arm is placed at the patient’s side
The pressure is allowed to fall slowly until the sudden flush of normal colour
returns to forearm, hand and fingers.
The endpoint is strikingly clear
This method may also be used on the thigh
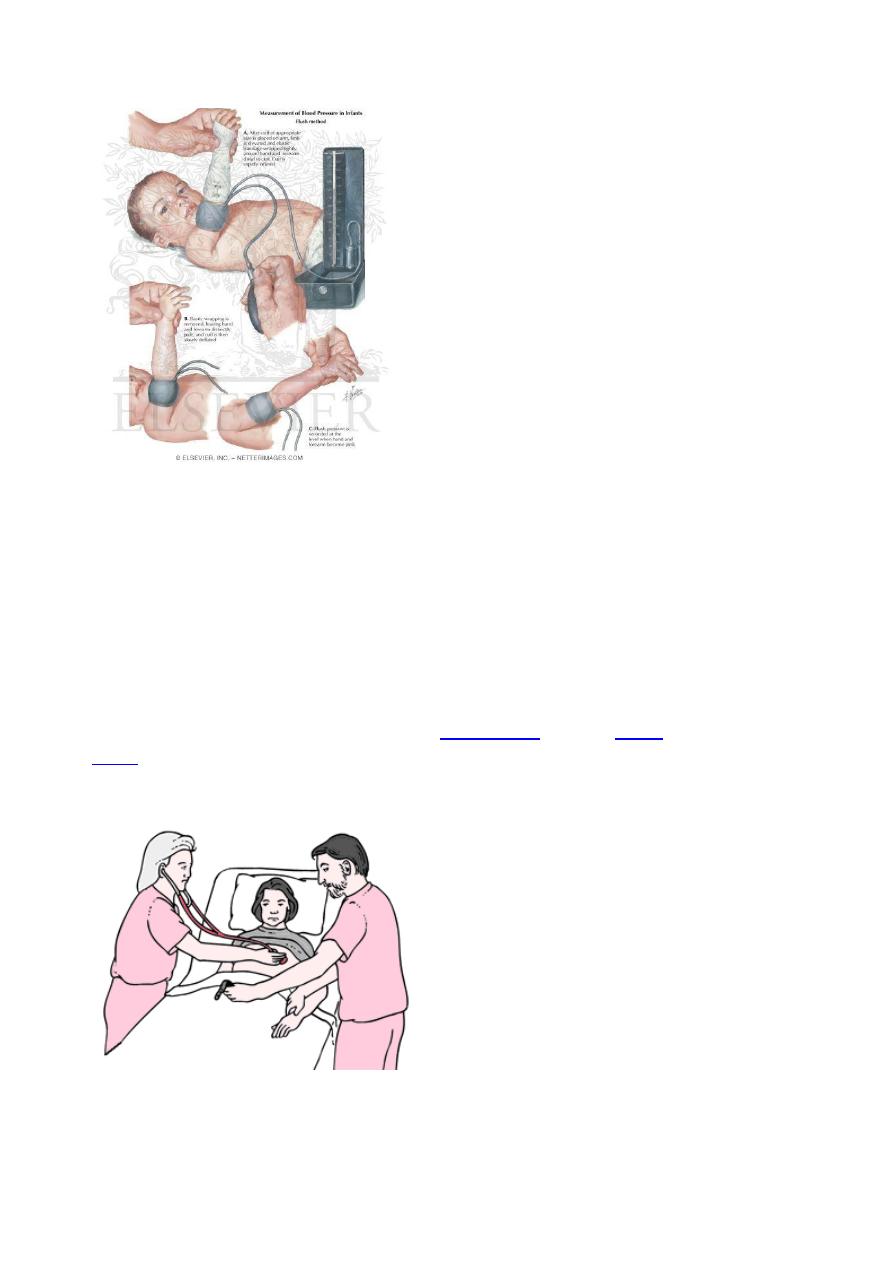
57
First check for brachial blood pressure it is audible or not by the stethoscope
then checks for the radial pulse it is palpable or not if neither brachial or
radial pulse felt now you can change to the Flush meyod
Pulsus deficit :
a condition in which a peripheral pulse rate is less than the ventricular contra
ction rate as auscultated at the apex of theheart or seen on the electrocardio
gram, indicating a lack of peripheral perfusion.
pulse deficit the difference between the
, obtained by having one person count theapical pulse as heard through
a stethoscope over the heart and a second person count the radial pulse at th
e same time.
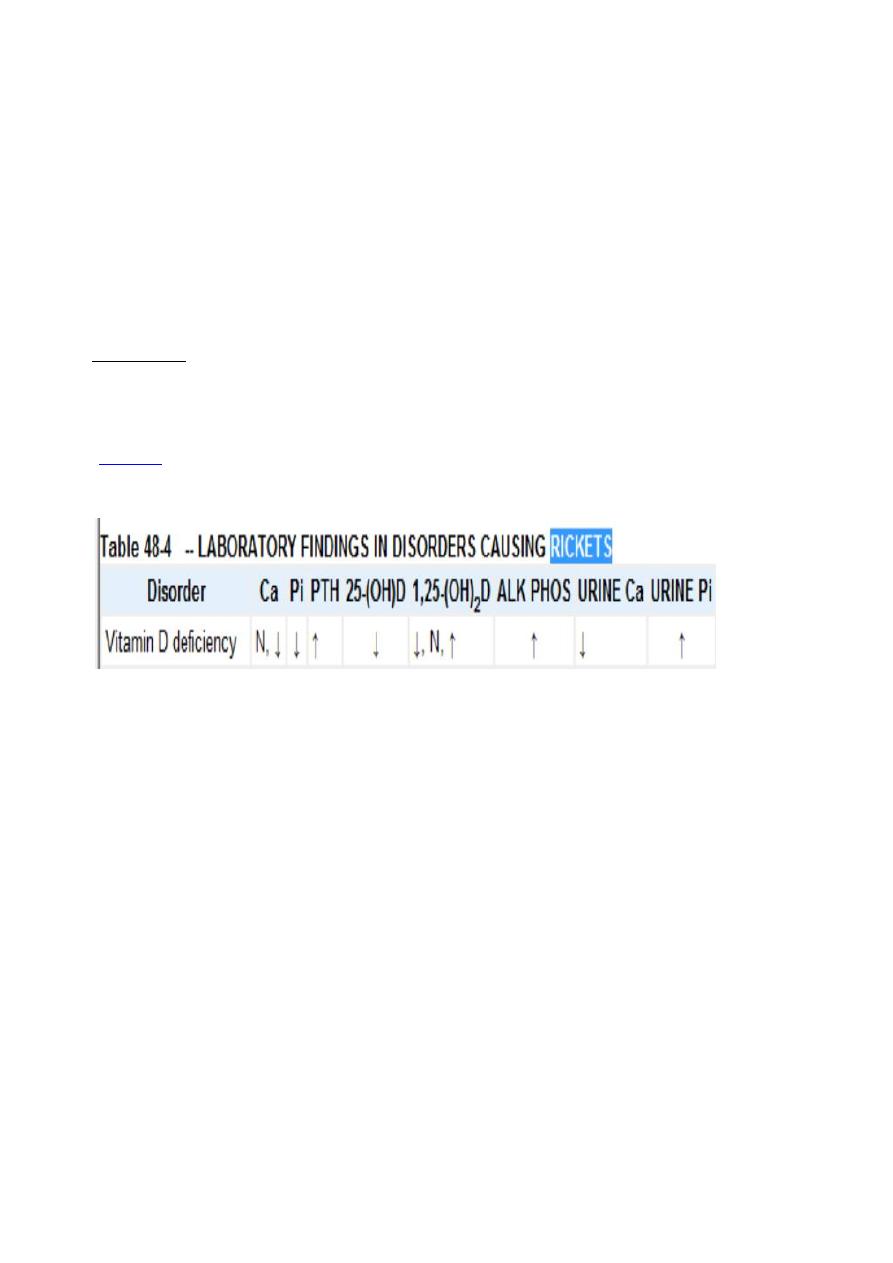
58
Exam the gentalia:
Check for any ambigious gentalia (congenital adrenal hyperplasia → ↓Na
+
),
imperforated anus
Exam the back
Exam the skin: for any neurocutaneous disease; eg: neurofibromatosis
Tuberus sclerosis
Rickets: Vitamin D deficiency rickets.
How to Dx: by X-ray and laboratory tests
X-ray:
-Widening and cupping of the metaphysis→ best seen at wrist or ankle.
-Fraying of metaphysis.
-
-Development of knock-knees, or genu valgum.
LAB findings:
Early on in the course of rickets, the calcium (ionized fraction) is low.
However, this level is often within the reference range at the time of
diagnosis, as a consequence of increased parathyroid hormone secretion.
Although calcidiol (25-hydroxy vitamin D) is low and parathyroid hormone is
elevated, determining calcidiol and parathyroid hormone levels is typically
not necessary in order to establish a diagnosis.
Calcitriol levels maybe normal or elevated because of increased parathyroid
activity.
The phosphorus level is invariably low for age, unless recent partial treatment
or recent exposure to sunlight has occurred. Alkaline phosphatase levels are
uniformly elevated.
A generalized aminoaciduria occurs from the parathyroid activity. However,
aminoaciduria does not occur in familial hypophosphatemia rickets (FHR).
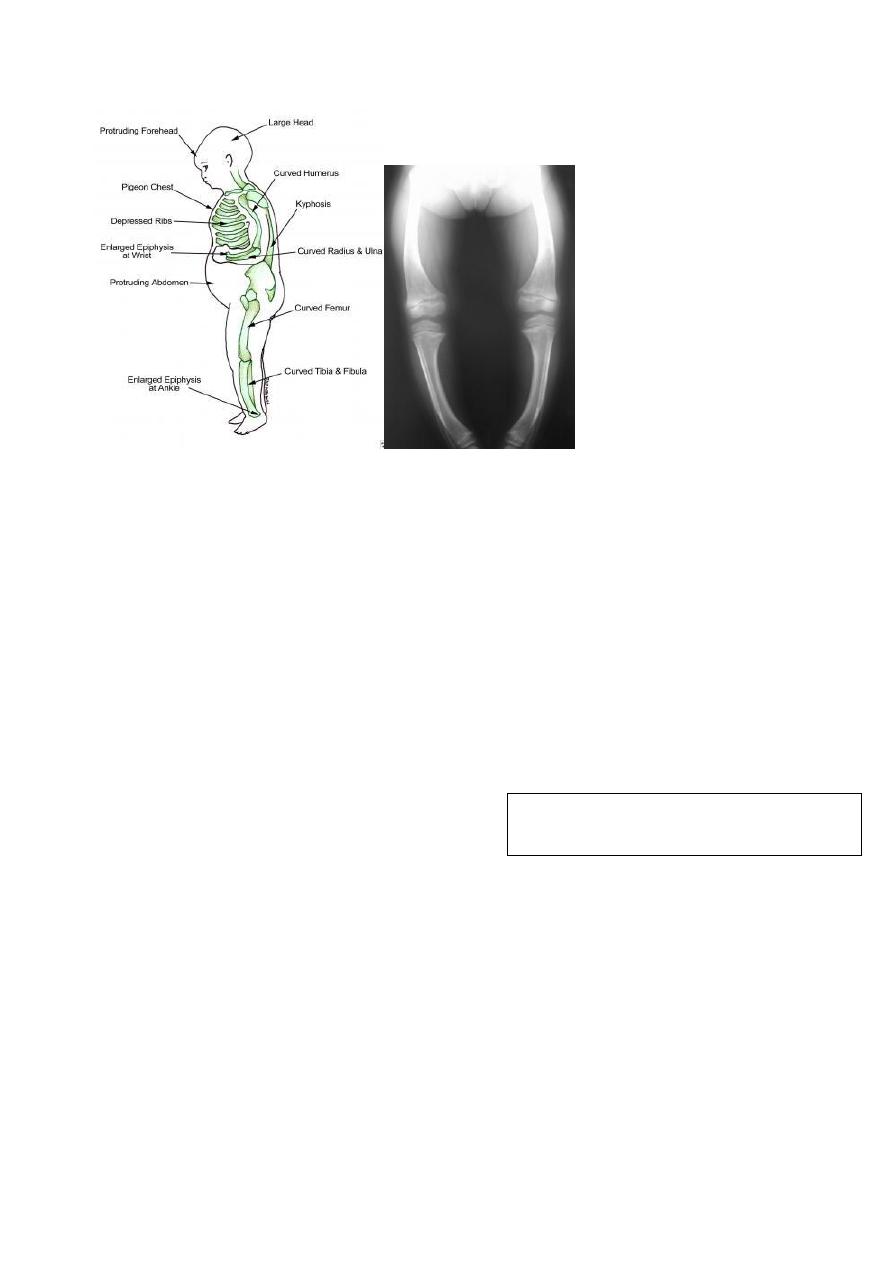
59
Treatment
Children with nutritional vitamin D deficiency should receive vitamin D and
adequate nutritional intake of calcium and phosphorus. There are 2 strategies
for administration of vitamin D. With stoss therapy, 300,000-600,000 IU of
vitamin D are administered orally or intramuscularly as 2-4 doses over 1 day.
Because the doses are observed, stoss therapy is ideal in situations where
adherence to therapy is questionable. The alternative is daily, high-dose
vitamin D, with doses ranging from 2,000-5,000 IU/day over 4-6 wk. Either
strategy should be followed by daily vitamin D intake of 400 IU/day if 1 yr,
typically given as a multivitamin
Most sensitive alkaline phosphatse enzemye the first one is affeted
And the last improved if it is become normal after treatment
So rickets due to vit.d deficiency if not return to normal
Rickets may be due to :
1-vit.D resistant
2-congenital hypophosphatemia
3-renal tubular acidosis
SHORT STATURE:
#Constitutional growth delay: This condition describes children who are
small for their ages but who are growing at a normal rate. They usually have a
delayed "bone age," which means that their skeletal maturation (bone age) is
younger than their age(chronological)in years. (Bone age is measured by
taking an X-ray of the hand and wrist and comparing it with standard X-ray
findings seen in kids the same age).
The marker of response to Rx is the reduction in
the level of Alkaline phosphatase enzyme.
60
These children don't have any signs or symptoms of diseases that affect
growth. They tend to reach puberty later than their peers do, with delay in
the onset of sexual development and the pubertal growth spurt. But because
they continue to grow until an older age, they tend to catch up to their peers
when they reach adult height. One or both parents or other close relatives
often had a similar "late-bloomer" growth pattern.
#Familial (or genetic) short stature: This is a condition in which shorter
parents tend to have shorter children. This term applies to short children who
don't have any symptoms of diseases that affect their growth. Kids with
familial short stature still have growth spurts and enter puberty at normal
ages, but they usually will only reach a height similar to that of their parents.
With both constitutional growth delay and familial short stature, kids and
families need to be reassured that the child does not have a disease or
medical condition that poses a threat to health or that requires treatment.
However, because they may be short or may not enter puberty when their
classmates do, some may need extra help coping with teasing or reassurance
that they will go through full sexual development eventually. In a few children
who are very short or very late entering puberty, hormone treatment may be
helpful.
Diseases of the kidneys, heart, gastrointestinal tract, lungs, bones, or other
body systems might affect growth. Other symptoms or physical signs in kids
with these illnesses usually give clues as to the disease causing the growth
delay. However, poor growth can be the first sign of a problem in some.
Growth disorders include:
: which isn't a specific growth disorder itself, but can be a
sign of an underlying condition causing growth problems. Although it's
common for newborns to lose a little weight in the first few days, failure to
thrive is a condition in which some infants continue to show slower-than-
expected weight gain and growth. Usually caused by inadequate nutrition or
a feeding problem, it's most common in kids younger than age 3. It may also
be a symptom of another problem, such as an
, a digestive problem,
diseases : (diseases involving hormones, the chemical messengers
of the body) involve a deficiency or excess of hormones and can be
responsible for growth failure during childhood and adolescence.
Growth hormone deficiency is a disorder that involves the pituitary gland
(the small gland at the base of the brain that secretes several hormones,
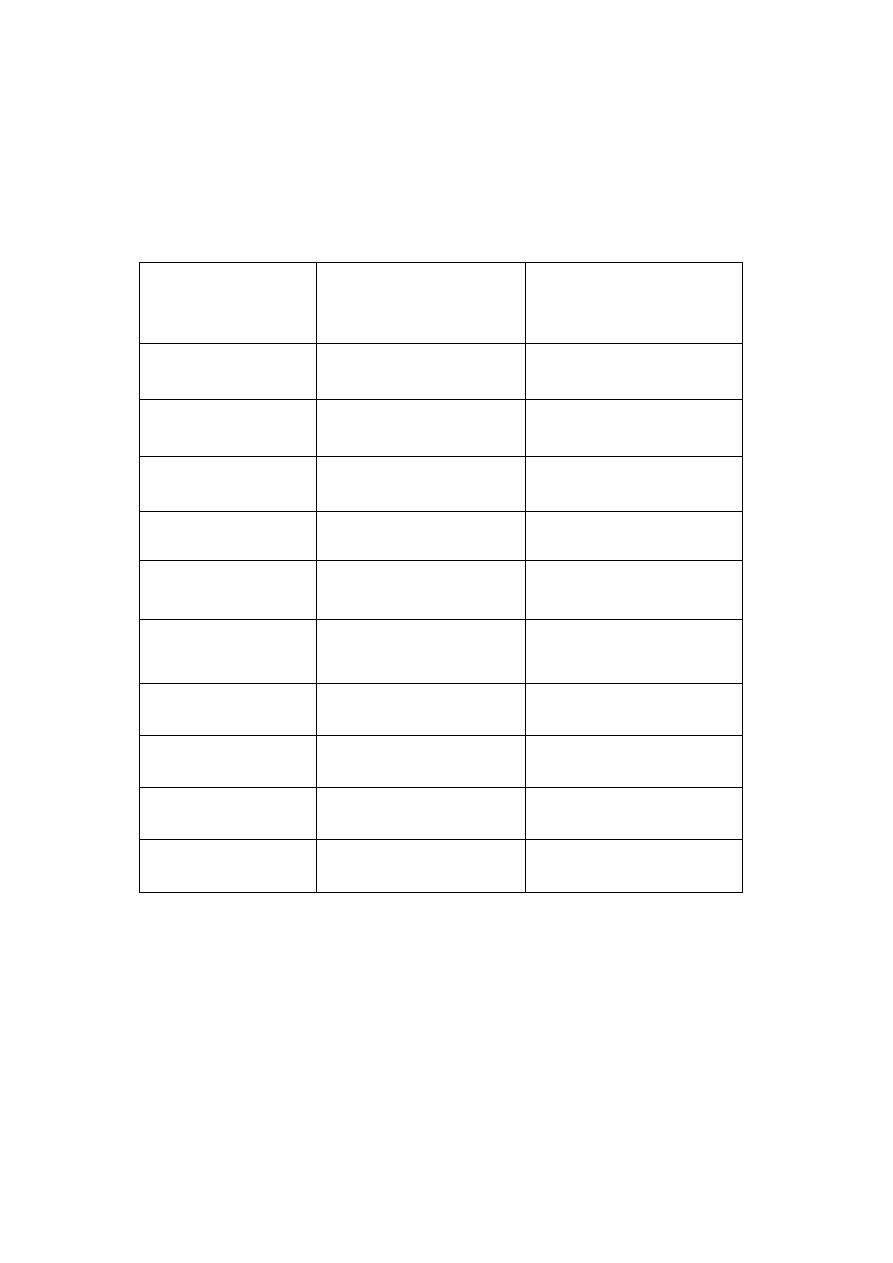
61
including growth hormone). A damaged or malfunctioning pituitary gland
may not produce enough hormones for normal growth.
Hypothyroidism is a condition in which the thyroid gland fails to make
enough thyroid hormone, which is essential for normal bone growth.
Occipitofrontal circumferance of the head:
OFC OFC()in Cm
Rate of ↑ of OFC in
Cm
Age
35
At birth
39
4
2 months
42
3
4 months
44
2
6 months
45
1
8 months
46
1
10 months
47
1
12 months
49.5
2.5
(whole 2nd year)
2 year
1/2
(each year)
3-7 year
1/3
(each year)
8-12 year
62
Hypocalcemia cauesd by SOB:
Hyperventilation syndrome often occurs under stressful conditions which cause
hypocapnia and consequently results in respiratory alkalosis and a wide range of
somatic symptoms. Respiratory alkalosis can induce secondary hypocalcaemia (shift
of ionized Ca
++
into bound Ca
++
) that may cause cardiac arrhythmias, conduction
abnormalities and various somatic symptoms such as paraesthesia, hyperreflexia,
convulsive disorders, muscle spasm and tetany. Acute hypocalcaemia is an
emergency that requires prompt attention and management.
Difference between modified and unmodified cow's milk ?
Unmodified cow’s milk:
o Contain protein 4% (human milk 1%) so it exhaust the liver and kidney
during metabolism and excretion.
↑↑ Na
+
than breast milk
hypernatremic dehydration.
↑phosphorus
chelate calcium
lead to convulsion.
Modified but modified cow’s milk suitable from birth.
Water, solids, calories, fat
same level in human and cow milk.
Modified cow’s milk is cow milk with less protein and sodium and
phosphorus but contains ↑ fat and CHO.
Modified and fortified milk is modified milk with vitamins and minerals.
#NOTE:
Acidosis causes the reverse of alkalosis (i.e causing shift of protein bound calcium into ionized ca
++
),
that is why the pt. with renal failure (acisdotic) does not develop tetany despite the hypocacemia that
he has (as result of failure of renal activation of vit. D into active vit. D3) .
Unmodified cow’s milk should
not be given to baby less than
one year age
#NOTE:
Modified cow’s milk contains proteins (energy) < cow’s milk but CHO and oils are higher, so the
calorie content is equal to cow’s milk and breast milk which 20 Kcal/oz.

63
Lec.1 Pediatrics 6
th
stage
Wednesday 17-8-2016 Session notes
د
.
رنا
Approach to examine a pt with neurological problem?
Start from the head:
1-hair texture: shiny brittle hair easily broken in FTT, sparse with coarse facies in
hypothyroidism.
2-fontanelles:-examine the pt in semi-sitting position (45 degrees) ,avoid
supine position as this will depress the fontanelle
While sitting position will bulge the fontanelle so also avoid it.
DDx of delayed closure of fontanelle?
1)ricket
2)hydrocphalus
3)osteogenesis imperfect
4)metabolic disease
5)hypothyroidism.
*******************************
3-eye :-nystagmus,squint,upright slanting (as in Down syndrome).
4-nose :-shape of nose ,saddle nose in syphilis/ Hypertelorism.
5- Chin: Micrognathia
6-mouth:-dental carie , state of hydration, tongue size .
**protruded but not macroglossic tongue in Down syndrome
7-Neck swelling in midline for goiter.
8-Hand:-fingers & hand creases.
9-foot ,legs for peripheral edema ,sandle gap in down syndrome.
10-peripheral pulses
11-LAP
12-vital signs
13-growth parameters.

64
Growth parameters :-
Head circumference :-
-3times attempts & take the highest.
-Normal ranges:-
-At 1
st
(3)moincreased by 2cm
-At 2
nd
(3)moincreased by 1cm.
-At (6)mo &later on1/2cm
-After 1yr 1cm/yr.
The increment stops when we stop growth.
LENGTH
-Till 2yrs we use the term (length) →Then after use the term(height).
BP : Start to be measured at(3)yrs & later but with indications:
-Cvs
-Renal problem
-Umbilical problem
**Use WHO chart for BP
In child with convulsion CNS exam :-
1) general look fornutrition,well or sick?conscious ?alert?oriented? , posture, any
deformity, any abnormal movement, tremor, any scar over legs, wasting ,hypertrophy,
irritability.
2) Tone exam
3) Power exam
4) reflexes
5) Coordination (Heel shin test, finger nose test)
**speech(dysarthria), nystagmus, dysdiadichokinesia, ataxic gait→ cerebellar problem.
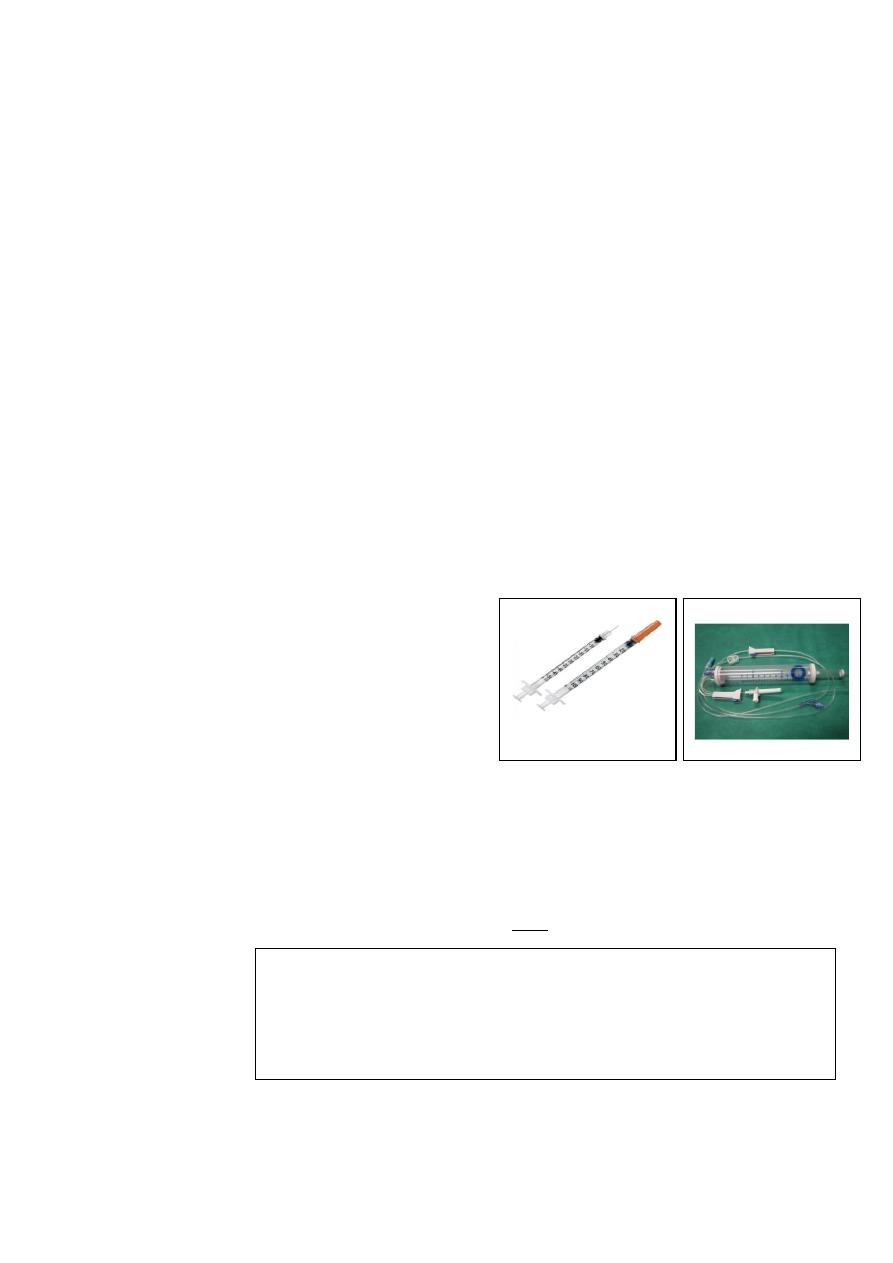
65
In ER, how do you treat pt with convulsion?
ABC-put pt in recovery position (lateral position) /airway in mouth for
avoiding tongue biting/suctioning of mouth.
Diazepam IV/rectally very slowly with O2.
--(ampoule contain 10mg/2cc),we give (1) mg for each (3)kg or (4)kg.
--Every ( 1)cc =(5)mg.
--We use insulin syringe
--It is graduated into (100) ,, divide 100 by (5) =(20)units in insulin syringe
=(1)mg.
Fill the syringe fully with D.W.تخفيف--
--Give it over(7)min to (10) min (very slowly).
--Wait for (20) min for response
--the microdrip is used for dilution & to control the speed of infusion)in
pediatric age group to avoid overload.
--In microdrip, each (1)ml gives(15)drops.
If NO RESPONSE
Give 20mg/kg luminal (luminal in ampoul is "200"mg/kg) then wait ( 20)min,
NO RESPONSE increase the dose by 5 ,then 10 min afterincrease by 5 ,till
you reach to 40 no response give both diazepam + Phenobarbital.
If you prescribe AED allow pt to take them for 2yrs if no response then
change.
مالحظة
:
-
لكن دكتورة رنا ذكزته حسة توفز، باتكلا هزكذي امك سيل روكذملا ةيودلأا لسلست
االدوية في الطوارئ
.
-
التسلسل كما يشزح في الكتة موجود في سشن دكتورة رؤى ص
5
66
Case of Epilepsy
C.C :-abnormal involuntary body movement for 10 days duration.
H.P.I:-
(9mo) old baby ,known case of epilepsy on treatment, his condition started as
continuous fever , for (2)days duration not associated with sweating or rigor
,then suddenly abnormal involuntary body movement for (10)min duration
occured with generalized ,spastic posturing
It was Associated with salivation & bluish discoloration of mouth ,not passed
motion or urine,aggravated by fever with no Hx of trauma ,the pt
immediately was brought to hospital after admission &receiving Rx ,he had
developed vomiting & FBM ,(6)times/day,watery in nature ,no blood or
muscus in stool ,convulsion attacks continued at hospital although Rx is
continuous
Electrolytes & blood sugar with GUE were performed ,MRI has been given as
appointment but has NOT been done till now,
Diazepam was given on admission,the pt was on Phenobarbital then
converted to sodium valproate before (2)mo.
Review of system:-nothing significant.
Prenatal Hx
Prenatal:-No vaccination,no smoking , mother age 39yrs,not anemic,bad
ANC.
Natal :-primigravida,no fever,No APH,No G.D,No Hypertension, no
preclampsia,NVD,No PPH,slight leaking liquor,no abortion .
Postnatal:-cyanosed,2days in NICU, wt:3.5kg,No jaundice,no crying at birth.
Developmental Hx:-
Gross motor:-no sitting,no crawling, no rolling over,he controlled his head at
4
th
month.
Fine motor:-palmar grasp,not able to reach the object to mouth,not able to
transfer objects from one hand to another.
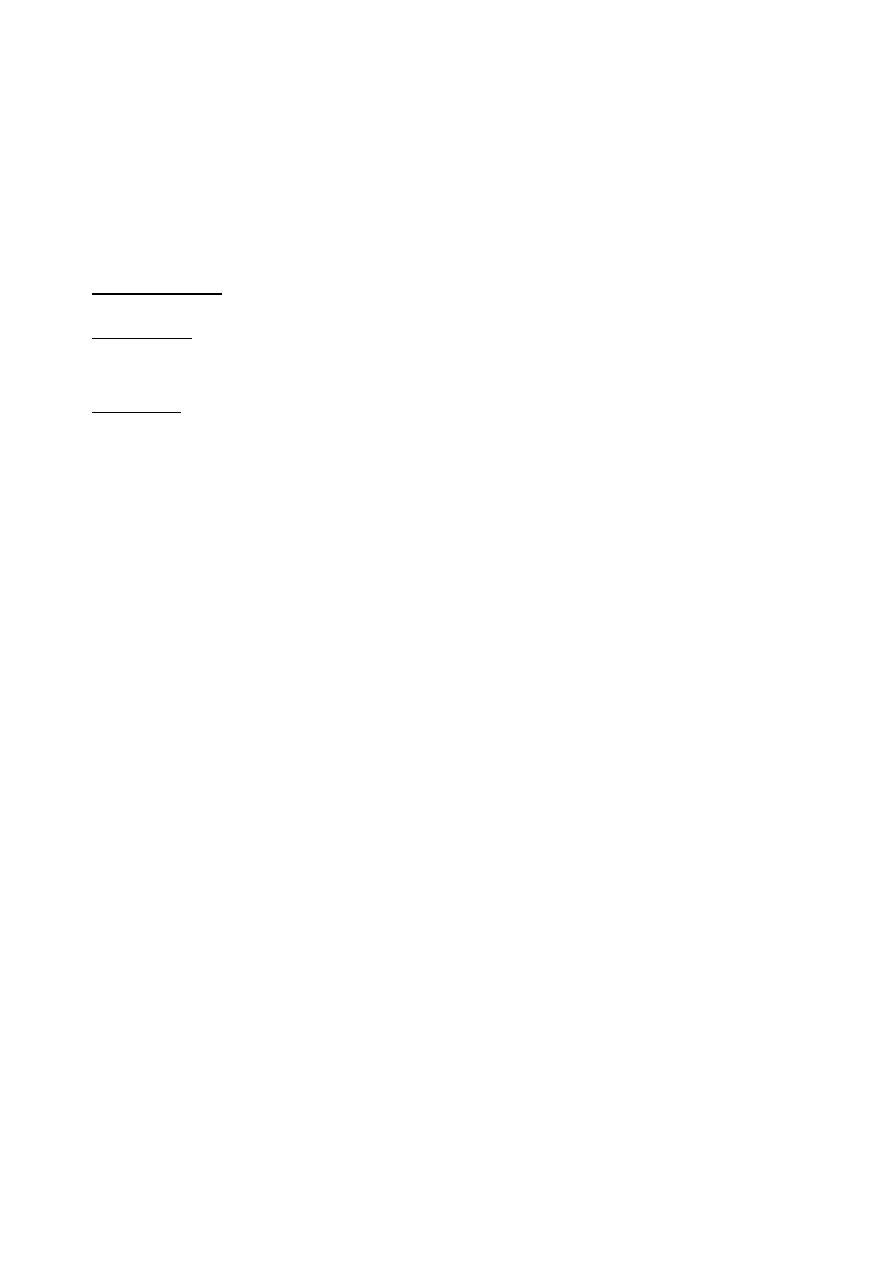
67
Social :-smile to his mother at 2
nd
month.
Language & speech:- only prounounce some incomprehensible sounds,not
able to say mamma ,baba.
Hearing&vision:-no response to his name.
Immunization:- upto date.
Family Hx:- no member in the family with febrile convulsion or epilepsy/no
Hx of chronic illnesses
Social Hx:-using tap water, no travel to other areas or countries, no animals in
the house ,average outcome.
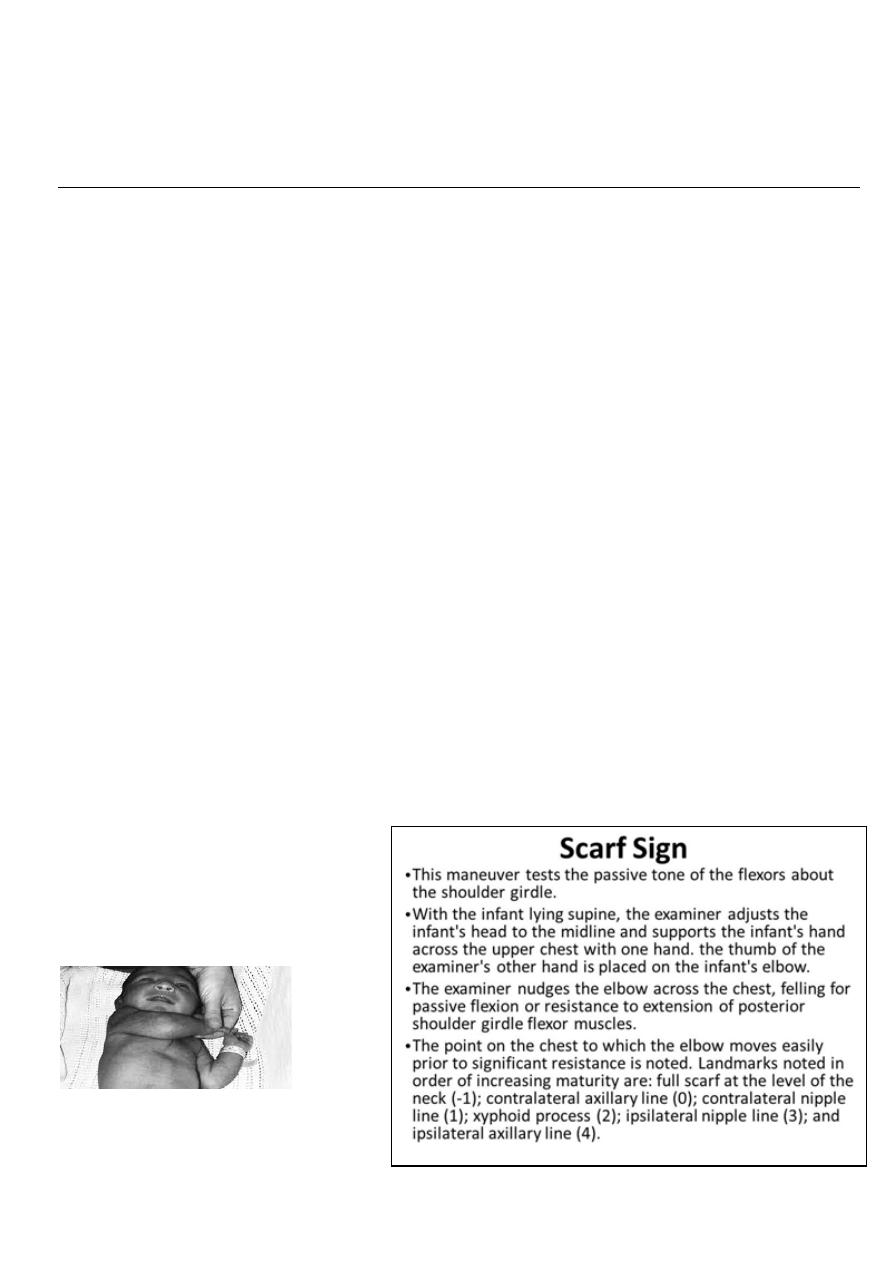
68
6
th
stage
Pediatrics
lec.4
د
.
ربيع الدبوني
Session notes
Werdnig-hoffmann disease(SMD):
Progressive degeneration of AHC (anterior motor horn cell) .
3 types(early type WHD) , (late type Kugelberg-Welander syndrome) , intermediate type).
Autosomal recessive.
WHD: start as progressive proximal weakness , ↓spontaneous movement , floppiness ,
atrophy of muscles , loss of head control , drooling , ↓ facial expression ,loss of reflex , eyes
remain bright open , engaging , tongue fasciculation(sleep) normal mentality , language ,
sensation
Cause of death: respiratory infection , respiratory failure.
Diagnosis: CPK↑, EMG.
TREATMENT: CONSERVATIVE
Hypotonia occur in:
1-Surgical cut of nerve
2-Diabetes mellitus
3- B complex deficiency
4- myaesthania gravis
In the first week hypotonia is unusual
In case of cerebral palsy hypotonia can occur at first early life and then changed to either
spastic paralysis or still in hyopotonic pattern
The death is due to respiratory failure infantile death All lesion result
in hypotonia + hyporelfexia .
In case of UMNL it result in hypotonia + hyporeflexia
On Exam:
-hypotonia: can be found by:
1.ventral suspension
2.Scarf Sign
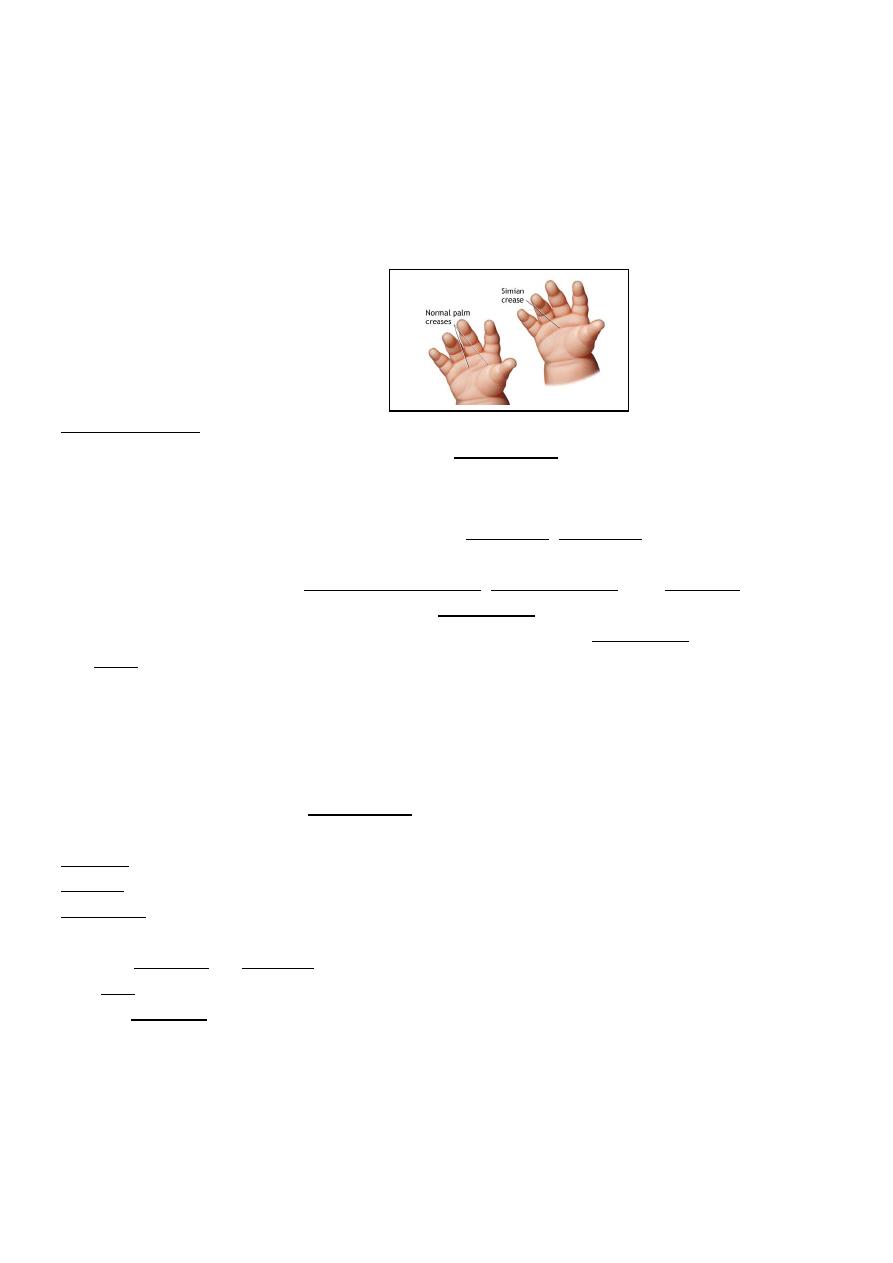
69
3. Both Elbow meet on the back
4.heel reach and touch the ear lobule ( Heel – Ear test )
5. Sun set sign during hands rising up
Prognosis: it is lethal disease
25% of siblings are affected, 50% carrier, 25 % normal
Advice family to avoid consanguineous marriage
Notes:
Simian creases is a normal finding
# Heat exhaustion
Heat exhaustion is a heat-related illness that can occur after you've been exposed to high
temperatures, and it often is accompanied by dehydration.
There are two types of heat exhaustion:
Water depletion. Signs include excessive thirst, weakness, headache, and loss of
consciousness.
Salt depletion. Signs include nausea and vomiting, muscle cramps, and dizziness.
Although heat exhaustion isn't as serious as heat stroke, it isn't something to be taken lightly.
Without proper intervention, heat exhaustion can progress to heat stroke, which can damage
the brain and other vital organs, and even cause death.
Symptoms of Heat Exhaustion
The most common signs and symptoms of heat exhaustion include:
Confusion
Dark-colored urine (a sign of dehydration)
Dizziness
Muscle or abdominal cramps
Nausea, vomiting, or diarrhea
Pale skin
Profuse sweating
Rapid heartbeat
Treatment for Heat Exhaustion
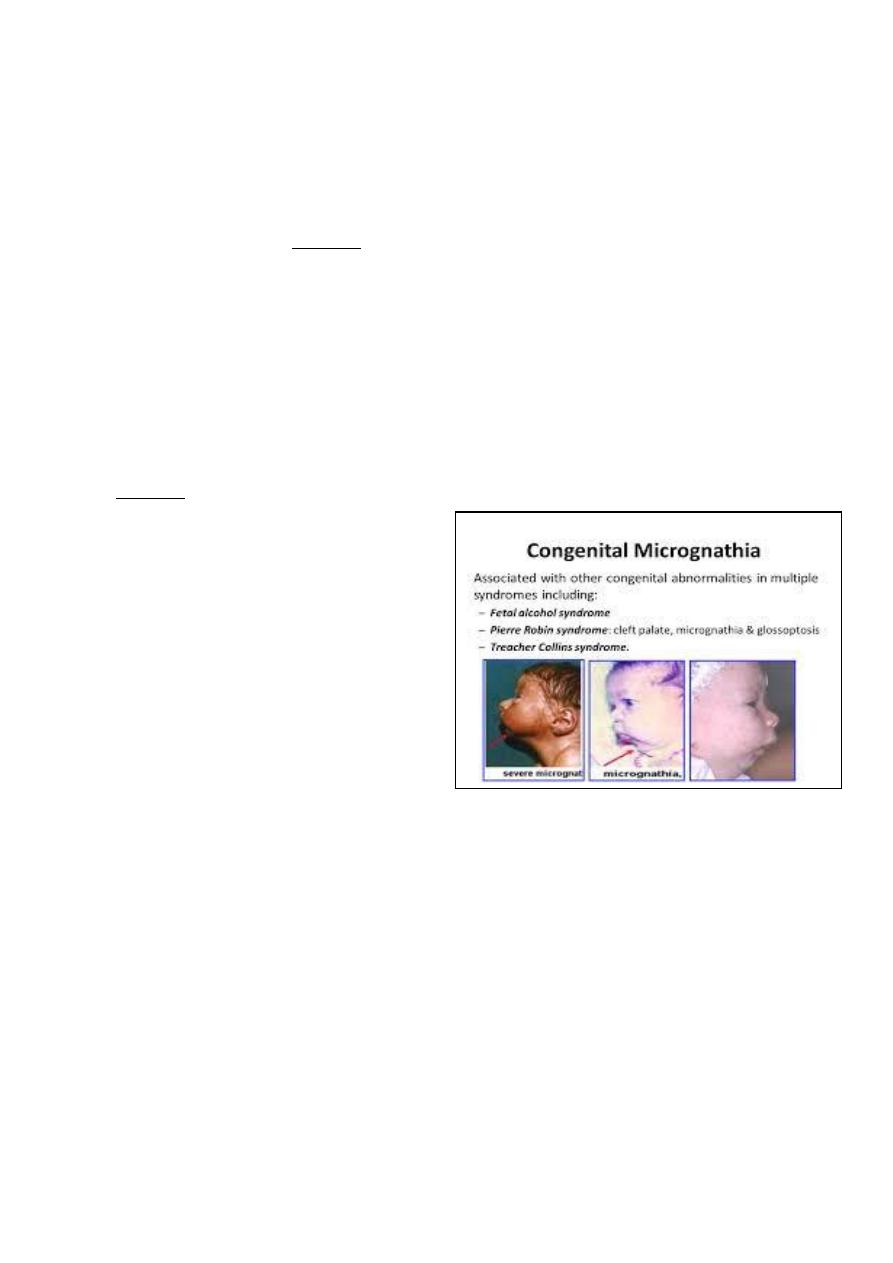
70
If you, or anyone else, has symptoms of heat exhaustion, it's essential to immediately get out
of the heat and rest, preferably in an air-conditioned room. If you can't get inside, try to find
the nearest cool and shady place.
Other recommended strategies include:
Drink plenty of fluid (avoid caffeine and alcohol).
Remove any tight or unnecessary clothing.
Take a cool shower, bath, or sponge bath.
Apply other cooling measures such as fans or ice towels.
If such measures fail to provide relief within 15 minutes, seek emergency medical help,
because untreated heat exhaustion can progress to heat stroke.
After you've recovered from heat exhaustion, you'll probably be more sensitive to high
temperatures during the following week. So it's best to avoid hot weather and
heavy exercise until your doctor tells you that it's safe to resume your normal activities.
Notes on general exam:
Check for :
-Position
-consiounesss
-respiratory condition
-color :
1-pale : check the eye and palm
2-cyanosis : central and peripheral , clubbing , heart
3-rash : distrunution , nature of ras
4-jaundice
-Reaction to examiner
-state of hydration
- state of nutrition
- vital sign
Cervical and inguinal LN is recurrently enlarged in the infancy
Due to infection
Axillary LN is impt. During exam if there is any LAP , sometimes is enlarged due to BCG
vaccine
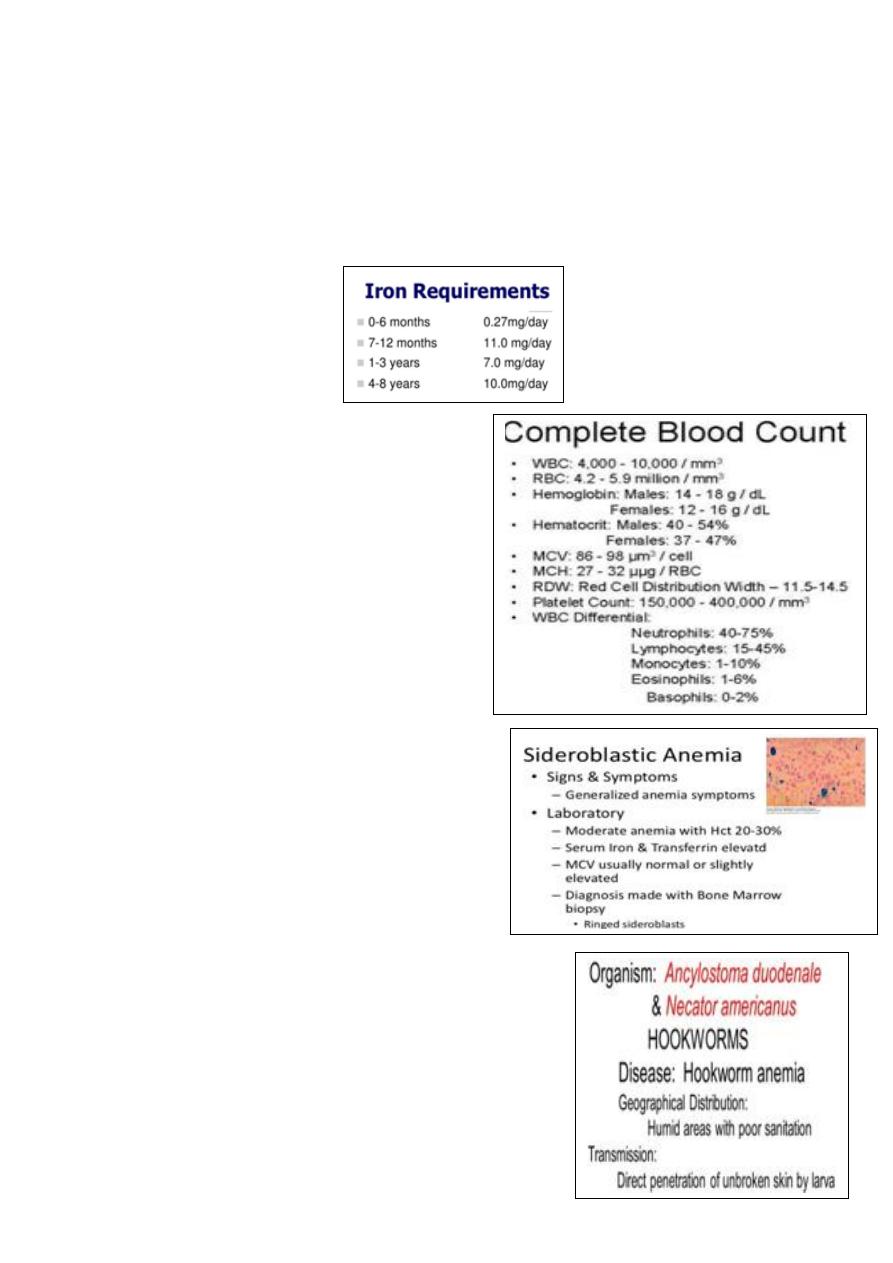
71
Notes :
Don’t mix egg with iron it will be non-absorbable in the intestine
Milk + iron = non-absorbable complex
Green leafy vegetable contain iron but is non-absorbable because it is ferric
Physiological needs of iron:
On Exam check for nutritional status by:
Fat and carbohydrate check for wasting
Protein check for edema
Mineral and vitamins check for rickets
Water check for dehydration
Anemia: Normal retic count is 0.2-2%
when increase indicates BM compensation
Differential diagnosis of Anemia:
1-iron def. Anemia (serum ferritin test)
2-Thalassemias Hemoglobin electrophoresis
with quantitative hemoglobin A2 and hemoglobin F
3-sidroblastic anemia
4-lead poisoning porphyrin in urine test
5-anemia of chronic disease
6-Hodgkin dis take biobsy
7-Atransferrin anemia (congenital loss
of iron binding protein)
Ancylostoma Duodenale :
If patient has iron def anemia and not respond to Tx check
Dx: stool microscopy looking for D-shape ova
Rx : Albendazol
72
6
th
stage
Pediatrics
lec.2
د
.
بسام
Session notes
Notes:
In SOB ask about:
-fever
-previous attack of SOB
-Cough at day or at night (nocturnal)?
-Cough with on-off nature?
In systematic review ask about:
1-GIT : vomiting , diarreheoa
2-UT : check for urine output
Indication of admission in SOB:
Less than 6 months age.
Severe respiratory distress.
Need O2.
Baby with high risk factors
CHD, chronic lung diseases (broncho-pulmonnary
dysplasia), immune deficiency, and neuromuscular weakness.
Home condition is bad.
Carless parents.
During admission try to identify any life-threatening factors
If there is cyanosis give O
2
or even mechanical ventilation
If there is dehydration
IV fluid
Foreign body
bronchoscopy
Fever
try to decrease body temperature
Pneumothorax
chest tube
Notes on general exam:
Look for mouth or lips color if it is blue may be due to central cyanosis
or gentian violet pigments it is a very effective anti-fungal
using an accessory muscle eg; sternocleidomastoid muscle is called (head nodding) ,
using suprasternal muscle indicate upper respiratory tract obstruction.
On chest exam don’t forget to examine the back for ( pulmonary edema in the basal
zone ) , examine the liver if there is any hyperinflated lung
Causes of Nocturnal cough:
1-recurrent aspiration eg; GERD
2-Asthma
3-in adult or school age occurs in
sinusitis and mediastinal tumor.
#causes:
1-TB. 2-Foreign body aspiration 3-Bronchiactasis 4-TEF
5-Cleft palate
6-congenital lung emphysema (α1-antitrypsin deficency)
7-bronchopulmonary dysplasia
8-Heart failure with recurrent chest infection
9- Kartagenar syndrome (non-functioning pulmonary cilia)
10-cystic fibrosis
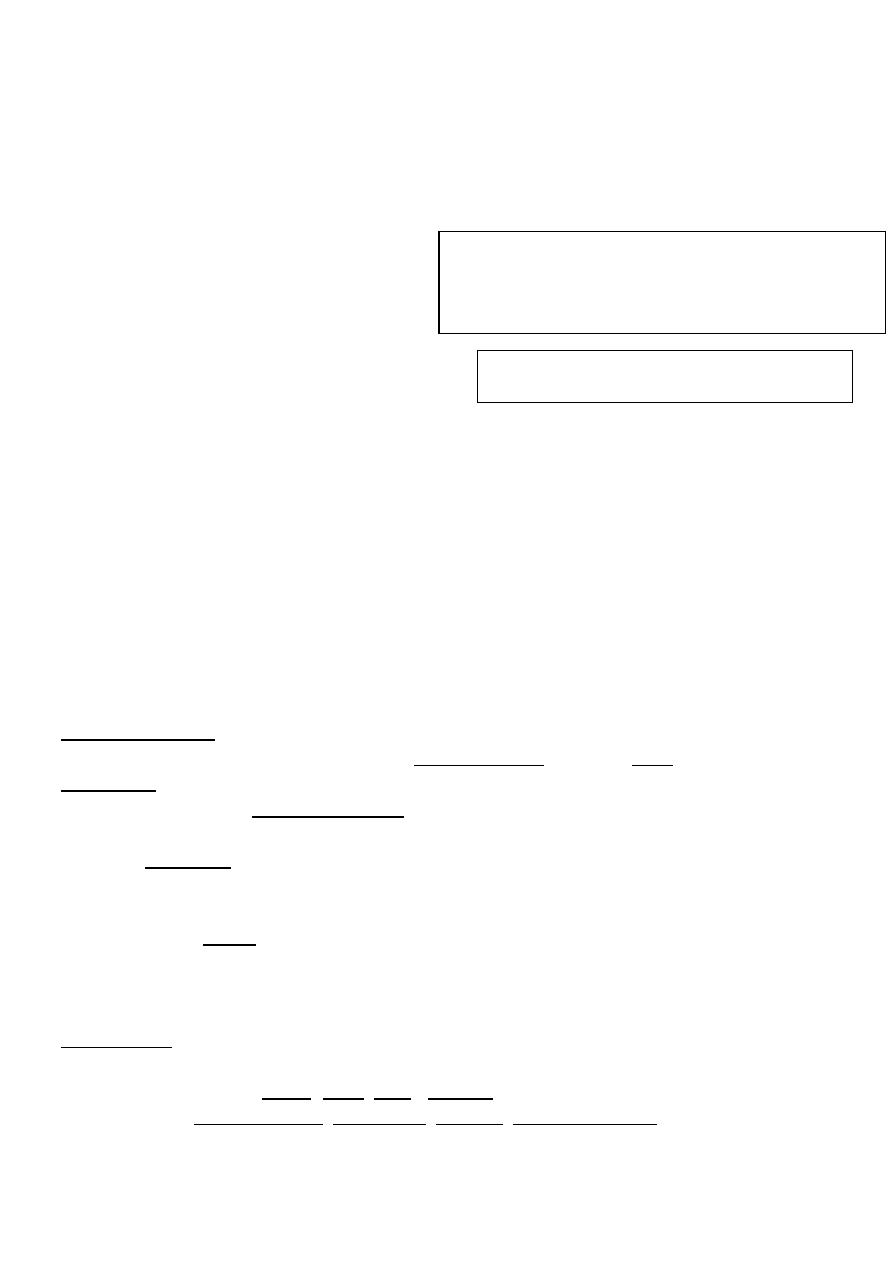
73
Signs of hyperinflated lung on CXR:
1-flat diaphragm.
2- Cylindrical heart shape.
3- Darkening of lung marking.
CXR finding in patient with bronchiolitis:
1-could be normal
2-hyperinflation
3-non-homogenous opacity
To assess whether it is good exposure or not
look to the vertebrae it must be just visible.
When to admit patient to the hospital if he
has diarrhea?
A. Severe Diarrhea with difficulty maintaining hydration
B. Very young
C. Severe co-morbid illness
D. Paralytic ileus
E. High fever
F. Intractable vomiting.
G. Coma
H. Complicated gastroenteritis eg; renal failure
Antibiotic usage in diarrhea:
A. Contraindications
1. Grossly bloody Diarrhea or other signs of Escherichia coli 0157:H7 (STEC: Shiga Toxin E coli)
B. Indications
1. Findings suggestive of Bacterial diarrhea
a. Guiaic positive stool (not grossly bloody stool)
b. Fecal Leukocyte positive
2. Diarrheal illness lasting longer than 10-14 days
3. Immunocompromised patients
4. Severe illness or Sepsis
5. Less than 3 months age.
6. Suspected meningitis
C. Empiric Antibiotics
1. Ciprofloxacin
a. Empiric dose: 500 to 1000 mg once or 500 mg twice daily for 3 days
b. Preferred agent for E. coli (ETEC, EIEC), Shigella
c. Also covers Campylobacter, Salmonella, Yersinia, Cryptosporidium
#NOTES:
-If the vertebrae are densely white low exposure to x-ray.
-If it’s nearly dark or transparent exposure to x-ray.
(the later may mimic hyperinflation of lungs)
Very important:
Recurrent CXR is needed in staph pneumonia
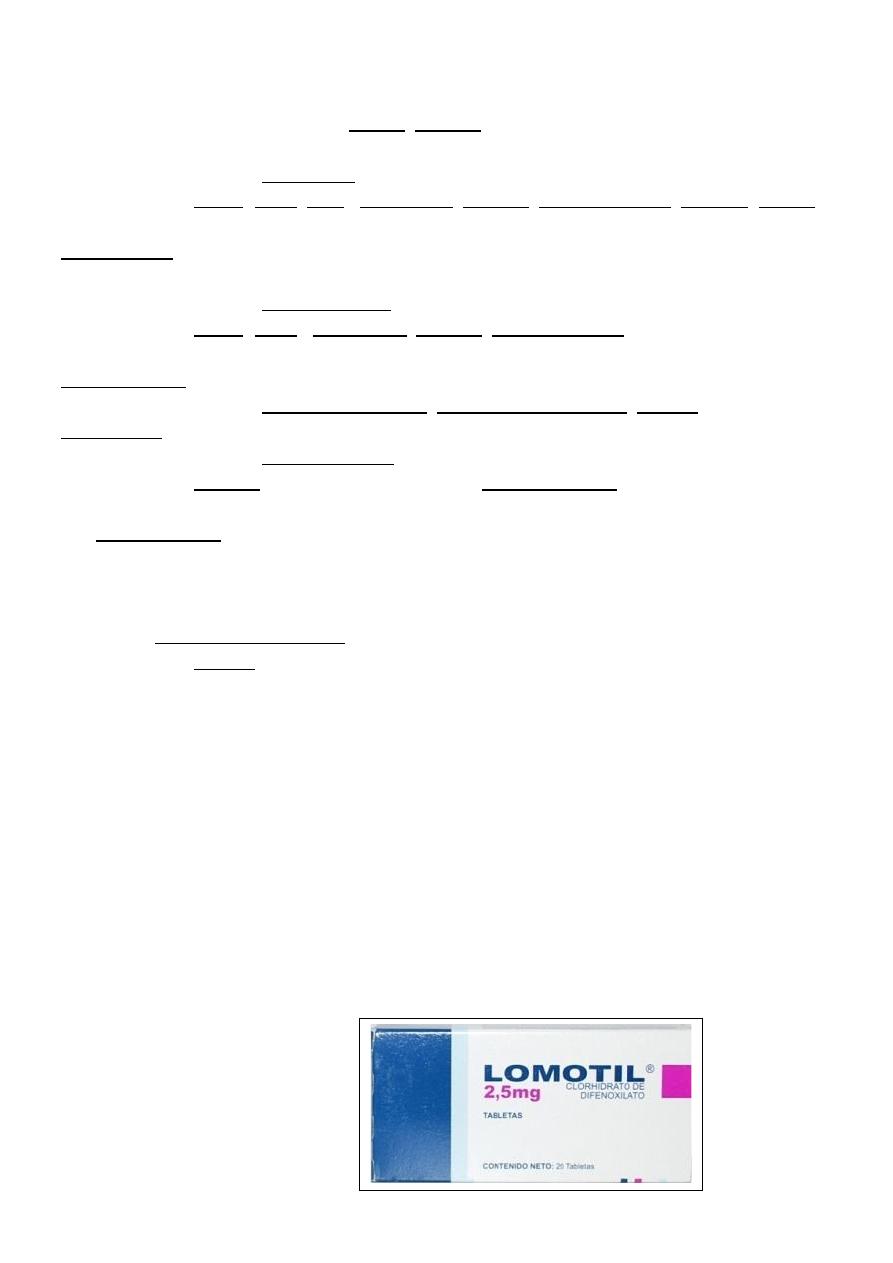
74
2. Trimethoprim-Sulfamethoxazole (Septra, Bactrim)
a. Empiric dose: One twice daily for 3-5 days
b. Preferred agent for Cyclospora or Isospora
c. Also covers E. coli (ETEC, EIEC), Salmonella, Shigella, Vibrio Cholerae, Yersinia (Septra has
higher resistance rates)
3. Azithromycin
a. Empiric dose: 500 mg daily for 3 days
b. Preferred agent for Campylobacter
c. Also covers E. coli (ETEC), Salmonella, Shigella, Vibrio Cholerae
D. Other antibiotics used for specific indications
a. Preferred agent for Clostridium difficile, Entamoeba histolytica, Giardia
2. Doxycycline
a. Preferred agent for Vibrio Cholerae
b. Also covers Yersinia (when combined with an Aminoglycoside)
E. Antiparasitic agents used for specific indications
1. See Metronidazole indications above
2. Albendazole (Albenza)
a. Preferred agent for Microsporida
3. Tindazole (Tindazole)
a. Covers Entamoeba histolytica (when treated in combination with Paromomycin)
b. Also covers Giardia
4. Naldixic acid (very effective)
SE: gastric upset, if less than 3 mo. It may lead to renal failure
By toxicity, increase intracrnial pressure, bulging fontanelle
Meningitis may presented as parentral diarrheoa
Cerebral edema presented in hypernatremia
In infancy when there is drowsiness think always in meningitis
Enterostop
Lomotil
It is anti-diarrheal agent (like entero-stop).
It is anti-chonergic agent.
Signs: respiratory depression, Hypotension, hypo-reflexia, coma, and death.
Don’t give lomotil until age of 4-5 years due to side effects.
If there is no cause of
diarrhea you can give lomotil.
Treatment
75
Sagwa poisoning:
It is lead acetate compounds.
Symptoms: Convulsion, coma, encephalopathy
death.
No surviving, it is acute positioning.
Motilium :
Phenothiazine group poisoning:
Anti-emetics (metochlopromide & domeperidone)
Treat the cause of vomiting and not give anti-emetic
to child side effects of antiemetics are hypotension,
ataxia, tachycardia, coma, occulogyric crisis, severe muscle rigidity.
Vomiting can be seen in any systemic diseases so treat the cause not the symptom.
Influenza, pneumonia, UTI, gastroenteritis, tonsillitis, infective hepatitis, meningitis…etc
all can lead to diarrhea.
The only indication for use of anti-emetics in children are GERD and before performing
jejunual biopsy in celiac disease
Treatment General Measures + Anti-dote (Benztropine) + anti-histamine
(chlorpheneramine) or diazepam (IV).
If you give diazepam only the case could be re-occur.
____________________________________________________________________________
6
th
stage
Pediatrics
lec.3
د
.
اوس حازم
Session notes
Notes :
Blood group taking in the history is important in hemolytic diseases such as : ABO
incompatibility & Rh incompatibility (mother: Rh-ve, baby:Rh+ve)
Cerebral palsy :
In general means disorder of posture & motion
Causes
1) Prenatal
o Prematurity
o LBW
o Intrauterine exposure to maternal infection
o Maternal medical problems
o Sever toxemia and eclampsia
o Bleeding in the 3rd trimester
o Drug abuse, drug therapy and toxic exposure
o Trauma
o Multiple pregnancies
o Placental insufficiency
o Congenital malformations
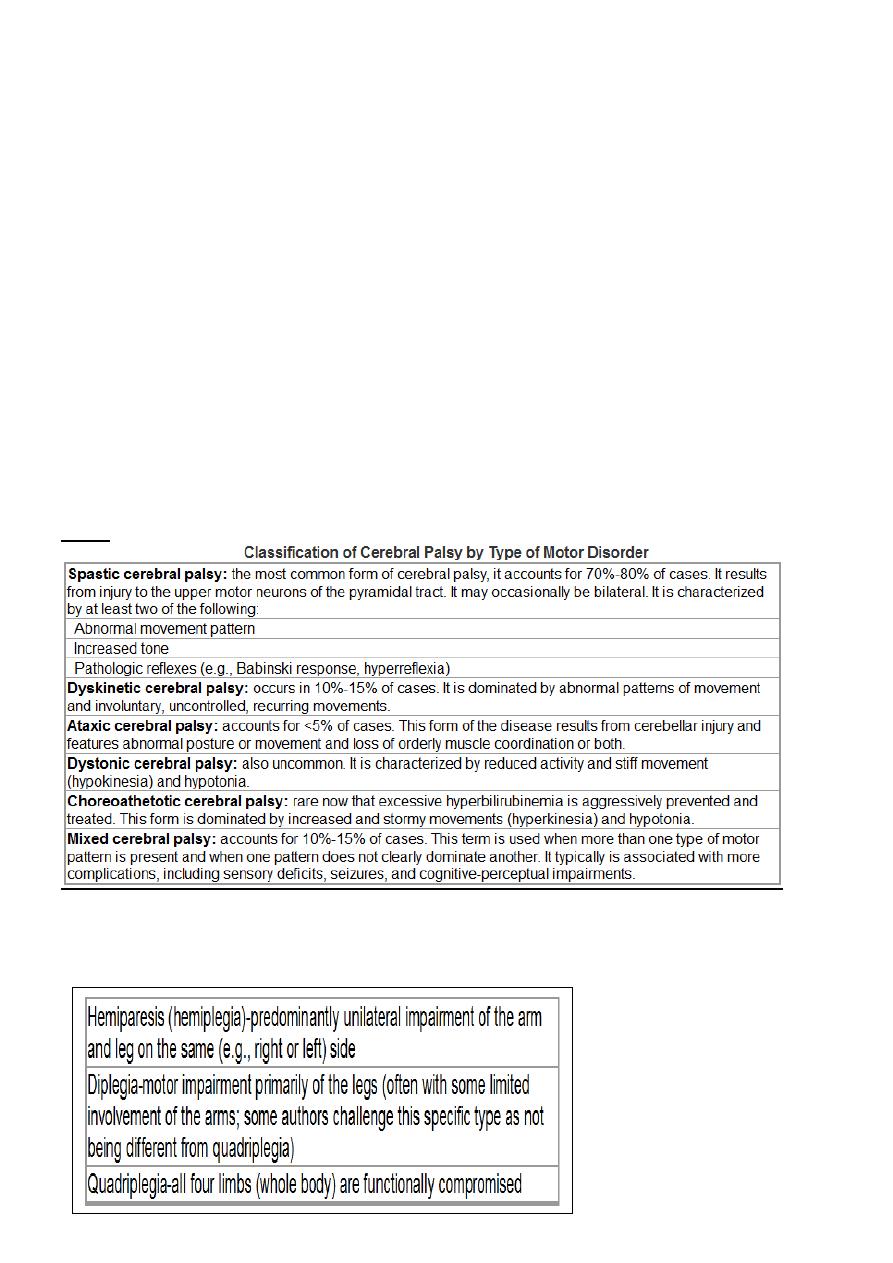
76
2) Natal
• Prolonged and difficult labor
• Premature rupture of membrane
• Presentation anomalies
• Vaginal bleeding at the time of admission for labor
• Bradycardia
• encephalopathy
3) Postnatal
o CNS infection: encephalitis and meningitis.
o Hypoxia.
o Seizure.
o Coagulopathies.
o Neonatal hyperbilirubinaemia (kernicterus):stormy event.
o Head trauma
ـــالنقاط السابقة كلها نسأل عنها لتحديد سبب ال
CP
Types
Topographic subclassification of spastic CP:
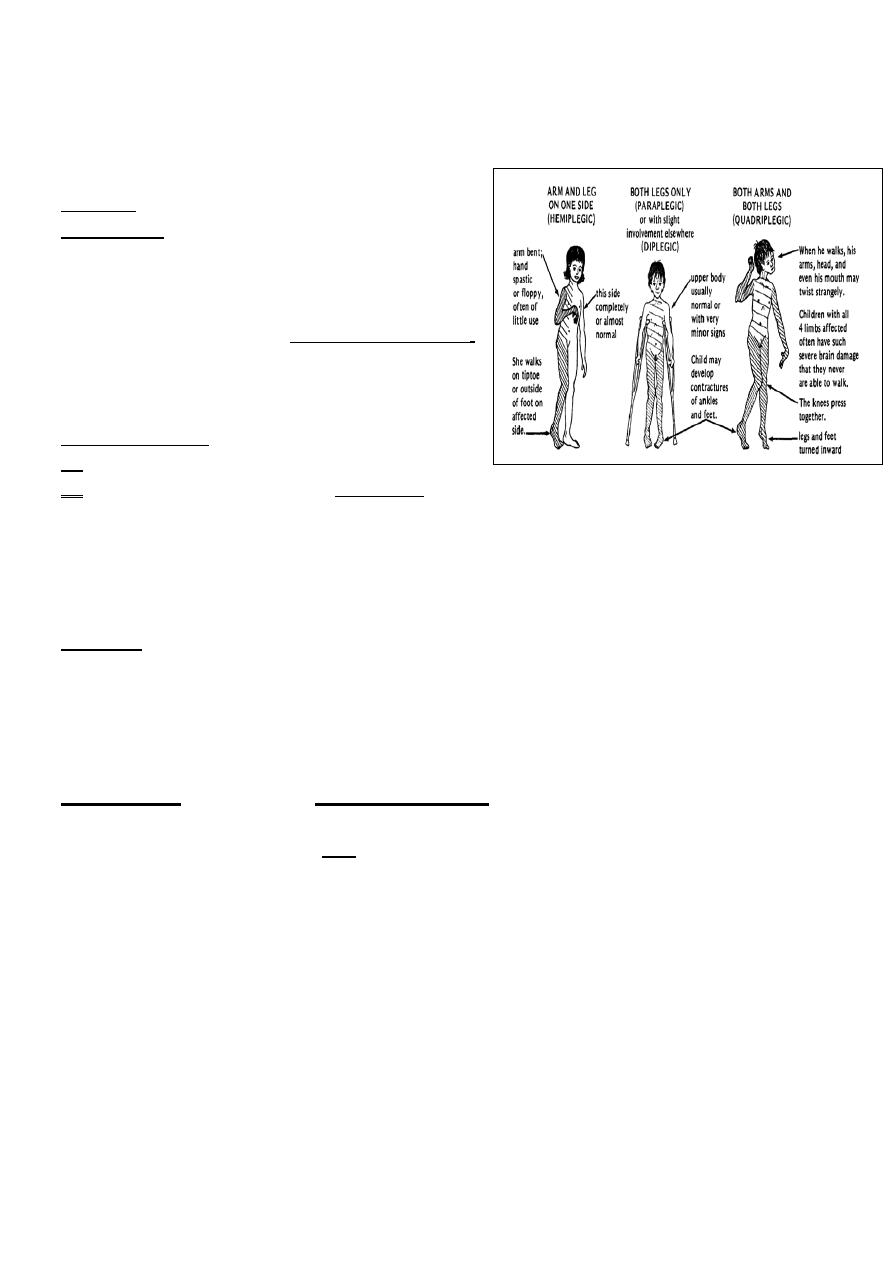
77
hemiplegic CP :the cause may be emboli or CVA in the intrauterine life.
in case of CP :concentrate on prenatal Hx,developmental Hx(Global or in certain parts),family
Hx is also important.
Grasping :- begins in (3)mo.
Grasp reflex :-hold the rattle.
(
خشخاشة
)
Don't forget hearing & vision,ask about them.
He developed well for some periods of time
then till (6) months he begin to regress,
this is typical Hx of pt with degenerative disease,
also called lysosomal storage disease.
Ex:-Gaucher's disease/Tay–Sachs disease.
Meningitis & CP:-
o CP : insult to brain during its development.
o CP is one of the complication of meningitis , they are :
1) Deafness/blindness.
2) Mental retardation
3) epilepsy
4) Hemiplegia/monoplegia
5) Hydrocephalus
Rx of CP:-multidisciplinary team ((very important))
1) Physiotherapist
2) Orthopedic surgeon
3) Pediatric surgeon
4) Ophthalmologist
5) Occupational therapist :-trying to make the child adapt.
Consanguinity is important in autosomal recessive disorders(galactosemia,Glycogen storage
disease, mucopolysacridosis
We share eighth of the genes (1/8 of the genes),especially if 1
st
degree relative.
General exam of the child with CP (**we saw in the ward**).
o are there any dysmorphic features?
o How is the body built?
o He looks ill or healthy?
o Dyspneic or NOT?
o Cyanosed ?
o Dehydrated ?
o Posture ?
o Instruments ?
o Abnormal body movement?(flexed spastic all joints are contracted for example).

78
Hands exam
Face exam
Legs exam
Malnutition:
Kwashiorkor
1. This disease is caused by the deficiency of protein in the diet of child.
2. Kwashiorkor occurs in children in the age group 1-5 years.
3. The disease is more common in villages where there is small gap period between
successive pregnancies.
4. In this disease, swelling of body is observed due to retention of fluids.
5. Wasting of muscles is not evident.
6. Skin changes color and become broken and scaly.
Marasmus
1. This disease is caused by deficiency of protein as well as energy nutrients (that is
carbohydrates and fats) in the diet.
2. Marasmus occurs in children below the age of 1 year.
3. This disease is more common in towns and cities where breast-feeding in discontinued
quite early.
4. No swelling of body takes place in Marasmus.
5. In Marasmus, wasting of muscles is quite evident. The child is reduced to skin and bones.
6. Skin does not change color and does not break.
Kwashiorkor
Oedema
Psychomotor changes
Growth retardation
Muscle wasting
Usually present signs:
Moon face
Hair changes
Skin depigmentation
Anaemia
Occasionally present signs :
Hepatomegaly
Flaky paint dermatitis
Cardiomyopathy & failure
Dehydration (diarrh. & vomiting)
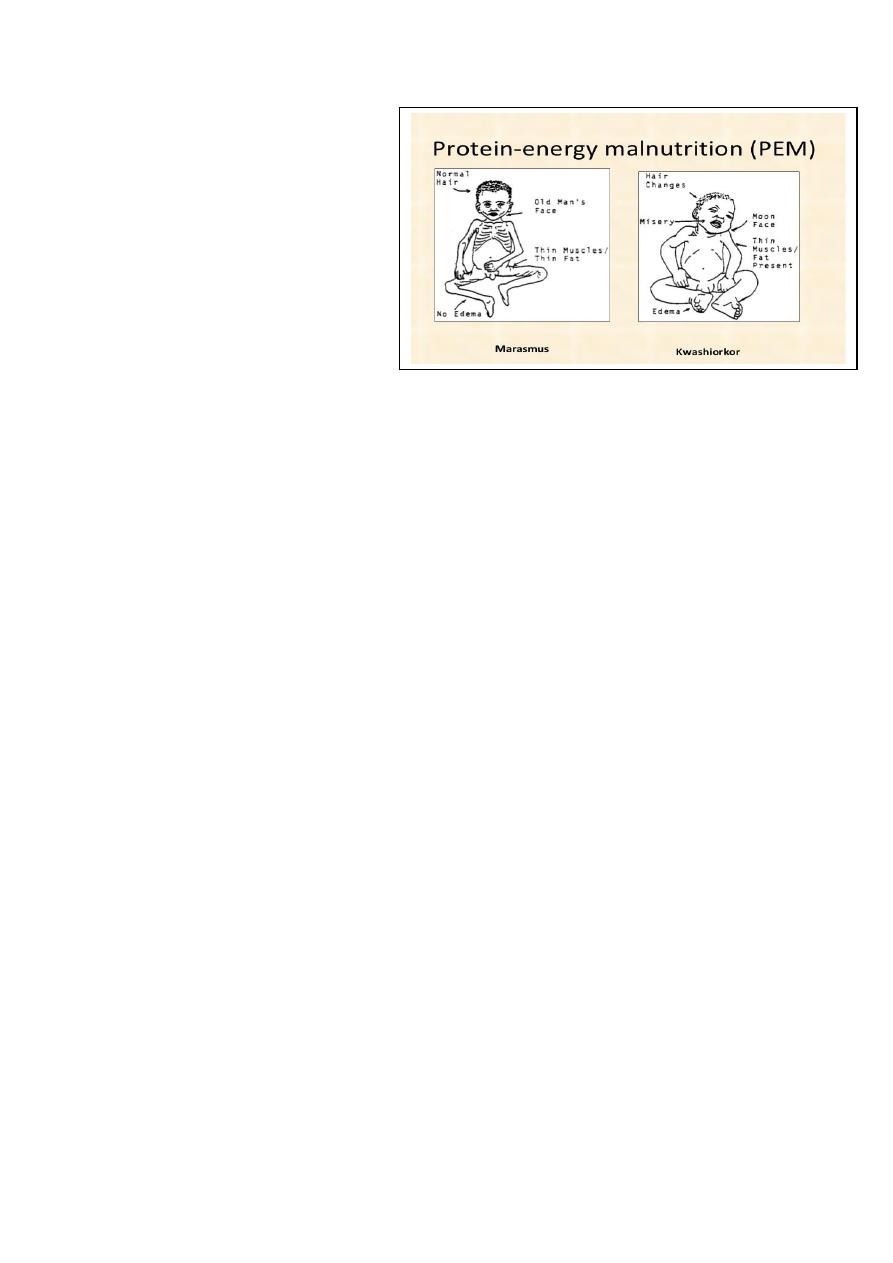
79
Signs of vitamin deficiencies
signs of infections
Clinical features of marasmus
Severe wasting of muscle & s/c fats
Severe growth retardation
Child looks older than his age
No edema or hair changes
Alert but miserable
Hungry
Diarrhoea & dehydration
Investigations are usually guided by history and examination. Routine tests may include:
FBC.
Urinalysis.
Urine culture.
U&E and creatinine.
LFTs, including total protein and albumin.
Celiac screen.
Prealbumin which may be used as a nutritional marker.
The following tests are not usually routine but may be indicated by history and examination:
Testing for HIV infection.
Sweat chloride test.
TFTs.
Stool studies for parasites or malabsorption.
Immunoglobulins.
Purified protein derivative (PPD) skin test (for tuberculosis).
Radiological studies (bone age may be helpful to distinguish genetic short stature from
constitutional delay of growth).
Special tests may be used for coeliac disease or to detect growth hormone deficiency
Treatment:
Normal formula contain 100 ml = 67 Kcl
In malnuritition this formula changed to F100 = 100 Kcl ( high calories )
Start at F75 milk to avoid vomiting and diarrhea
We can commence from 50% of the expected feeding at that age of child
Until reach 150 % of the expected
Developmental assessment:
-Gross motor.
-Fine motor.

80
-Language
-Social.
Gross Motor:
A newborn has head lag on pulling to sitting position. In ventral suspension, the head and
the limbs are flexed.
By 3 months, the head lag is minimal when pulled to sitting position. The baby can raise the
chin in prone position. On ventral suspension, the head are in line with the body.
By 4 months, the baby has head control when held up. In prone position, the baby can raise
the head and shoulder.
By 5 months, the baby bears weight on the forearm in prone position and can bear weight
on standing, also rolling over can be seen at this age.
By 6 months, the baby bears weight on hands in prone position.
By 7 months, the baby can sit with support and lean forward and also bounce on standing.
By 8 months, the baby crawls on the abdomen, and can sits without support.
By 10 months, most of the babies pull to standing posture and walk holding on to a piece of
furniture. This is called “cruising”, they can crawl.
يمسك االثاث اثناء المشي
By 1 year, the baby can make a few steps with support.
By 15 months, the baby can walks alone.
By 18 months, the baby can runs.
By 24 months, the baby can climb stairs two feet per step and the baby can also kick a ball.
By 3 years, the baby can climb stairs 1 foot per step and can ride a tricycle.
By 4 years the baby can climb down stairs one foot per step.
By 5 years, the child can skip.
Fine Motor:
The newborn can focus on objects.
By 1 month, the baby can follow objects for up to 90º and for 180 degrees
by 2 months.
5 By 4 months the baby can hold objects with both hands and take them to the mouth.
By 5 months, the baby can take the feet to the mouth.
By 7 months, the baby can transfer objects from hand to hand and having a palmar grasp.
By 9 months, the baby can hit two cubes together, can drink by a cup
By 10 months, the baby has a “pincer grasp” by approximating the thumb and the index
finger and can uncover hidden things.
By 1 year, the baby can release objects on request and can make a tower of two cubes.
By 13 months, the baby can turn pages of a book, two to three pages at a time.
By 15 months, the baby can feed self with a spoon without much spilling.
By 18 months the baby can build a tower of 3 cubes.
By 2 years, the baby can turn page by page, and can build a tower of 6 cubes also he can
scribble lines ( horizantal line ) .

81
The baby can draw a circle by 3 years, a square by 4 years and a triangle by 6 years.
Baby can dress and undress alone by 4 years.
-suquare , traingle , cycle drawing is called coping if more than 6 mo.
If less than 6 mo. Is called Emitate
-seizuring حركة المقص
زرخلا دع وا كسم ةكرحbeating
- Language Development:
Baby makes cooing sounds by 3 months.
By 4 months, the baby can babble.
By 7 months the baby responds to his/her name. By 7-8 months, baby vocalizes
monosyllables.
By 10 months combines monosyllables, and understands spoken speech.
By 1 year, the baby speaks 2-3 words with meaning. By 18 months, one can speak 20 words.
By 2 years baby can speaks about 200 words and can make a 2 words sentence.
Personal Social Development:
The baby regards faces by 1 month, has social smile by 6 weeks and recognizes the mother
and caretakers by 3 months, can laugh loudly by 4 months.
The baby enjoys looking at the mirror by 6 months and imitates other by 1 year.
By 6 months, the baby shows sadness when mother leaves and has stranger anxiety by 8
months.
By 9 months, the baby can drink from a cup and by 15 months the baby can self feed with a
cup and a spoon with little spilling.
By 10 months baby can wave bye bye.
The baby starts toilet training by around 2 years, being dry during day by around 3 years.
Bowel control is before urine control, and girls can control before boys. By 2 years of age,
baby refers to self as “ I “ By 3 years, the baby also has gender identity.
#hearing :
At birth startle
Ask mother about hearing problem ?
Distraction test at 6 mo.
Hearing test at birth till 3mor 6 mo
9 mo. Listen to his / her name
PTA ( pure tone audiometry )
ABR ( auditory brain stem response )
Autoacustic machine
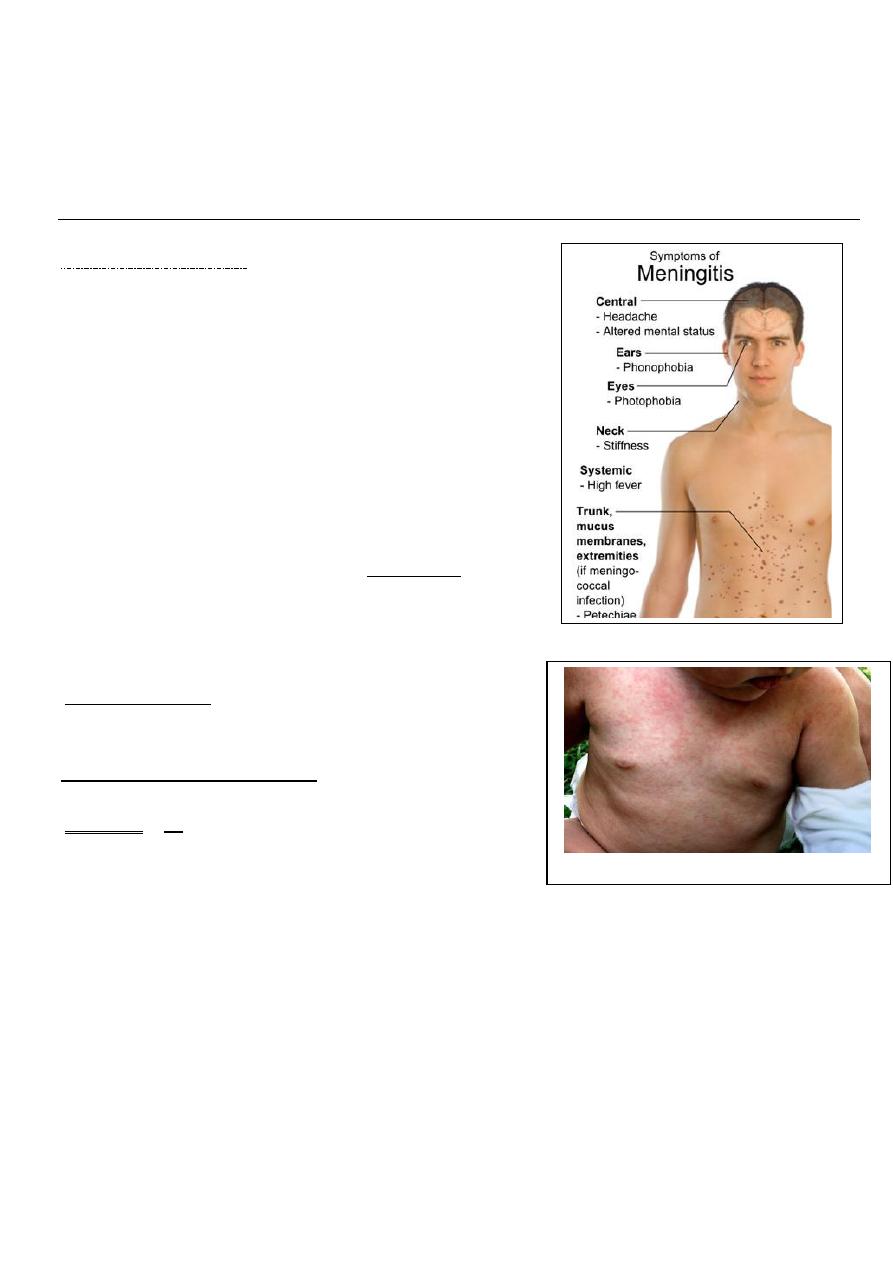
82
6
th
stage
Pediatrics
lec.2
د
.
فارس الصواف
Session notes
Febrile convulsion Hx
1.generalized or focal
2.duration
3.vomiting
4.fever
5.LOC
6.deep sleep *post ictal*
7.Hx of trauma
8.cyanosis
9.drooling saliva
10.staring of the eyes upward.
In physical exam ,try first to exclude meningitis:
then labile it "febrile convulsion",may be due to:
otitis media,tonsillitis,UTI,roseola infantum
(Human herpes virus-6:febrile convulsion,high grade fever &morbilliform rash),pneumonia.
Signs of meningeal irritation neck stiffness,kernig sign
,brudizinski sign. All are done & confirmatively
in >1yr old infant.
The most reliable sign in meningitis is:
deterioration of mental status(drowsiness).
Fever & convulsion in a child (<18mo)for the
1
st
attackLP is mandatory.
We exclude raised ICP by fundoscopy
(Atropine is given as dilator).
If parents refuse to do LP let them to sign on their responsibility.
Try to explain the procedure to parents before doing it.
(30%)recurrence of febrile convulsion
Educate the parents
o put the head in lateral position(to avoid URT obstruction).
o wait (1-2)min .
o try to reserve suppositories of anti-pyretics in the home always.
Morbiliform rash in pt with roseola infantum
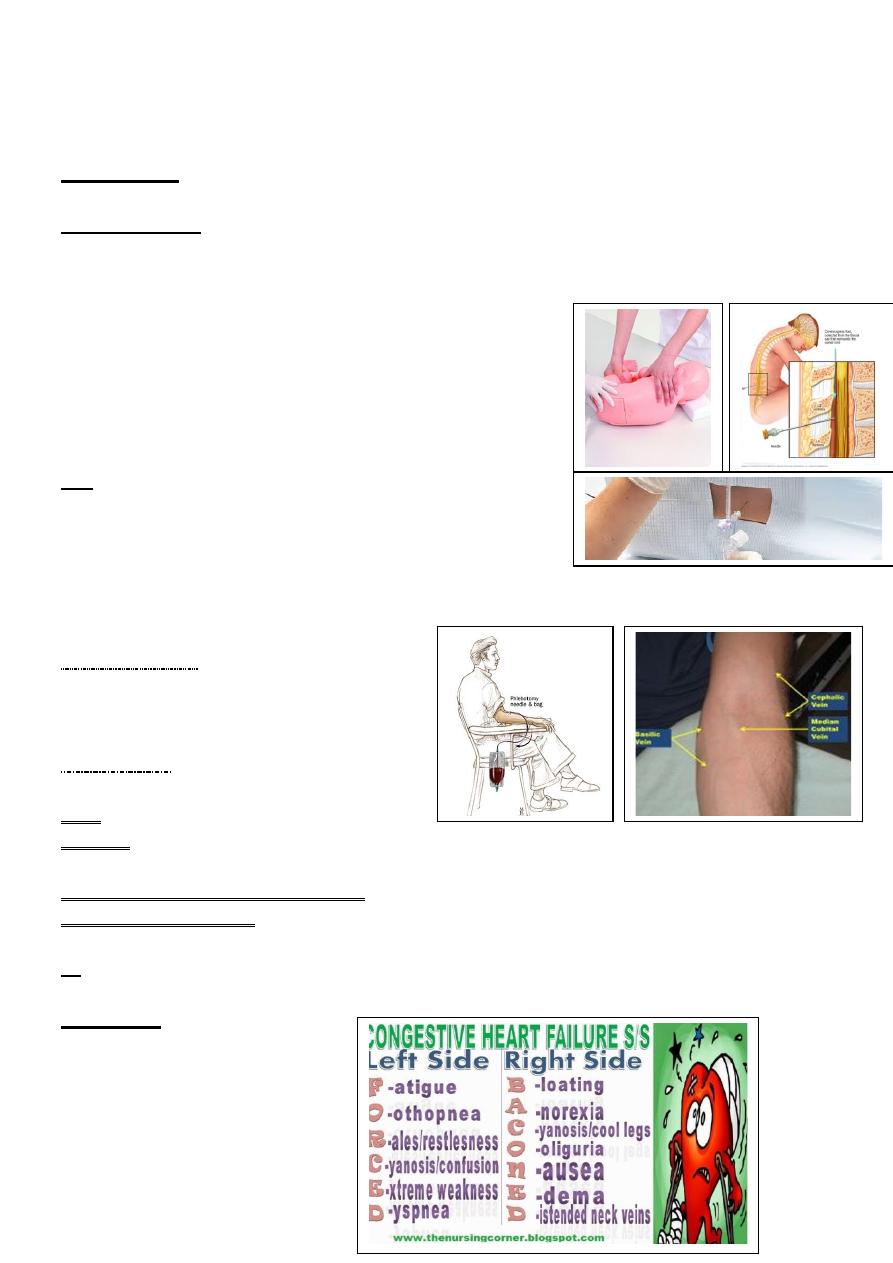
83
Investigations
RBS, serum electrolytes, CBC, blood culture, CRP, LP, CXR, GUE and neuroimaging (CT-scan).
Procedure of LP:
1)pt in sitting position & lean forward or laterally directed.
2)sterilization of the area in circular pattern ,beginning from centre &directed to periphery.
3.transverse line from iliac crest , space above,space below.
4.(2cc)is to be drawnif cloudy.
Most common organism is strep.pneumoniae
Try to calm the parents, say its benign problem.
If no meningitis ,put in your mind : viral infection :
no need for Rx only anti-pyretic.
Rx:-
Airway, O2, suctioning, IV cannula.
1/2 mg rectally diazepam.
0.25 mg/ kg IV diazepam.
*Next time if fever start: prophylactic diazepam is indicated.
**proper position of bottle feeding (to avoid air)
POLYCYTHEMIA
Emergency in diabetic mother infant.
Send for PCV,if >65venesection.
Heart failure
*admission to ICU
1.O2
2.IV line ((only give maintainence:150<6mo,125>6mo,after 1yr:100):chart input
/output/weighing the child every day is v.imp(to see if the edema resolved or NOT).
3.head up ,tube feeding "very imp".
4.diuretics.(1-2mg/kg).
5.digoxin
**don't diagnose H.F without cardiomegaly(is a must),tender
hepatomegaly,tachycardia/tachypnea,Galop rhythm.
Signs of H.F
1.dyspnea on exertion.
2.pulmonary rales.
3.tender hepatomegaly.
4.tachycardia.
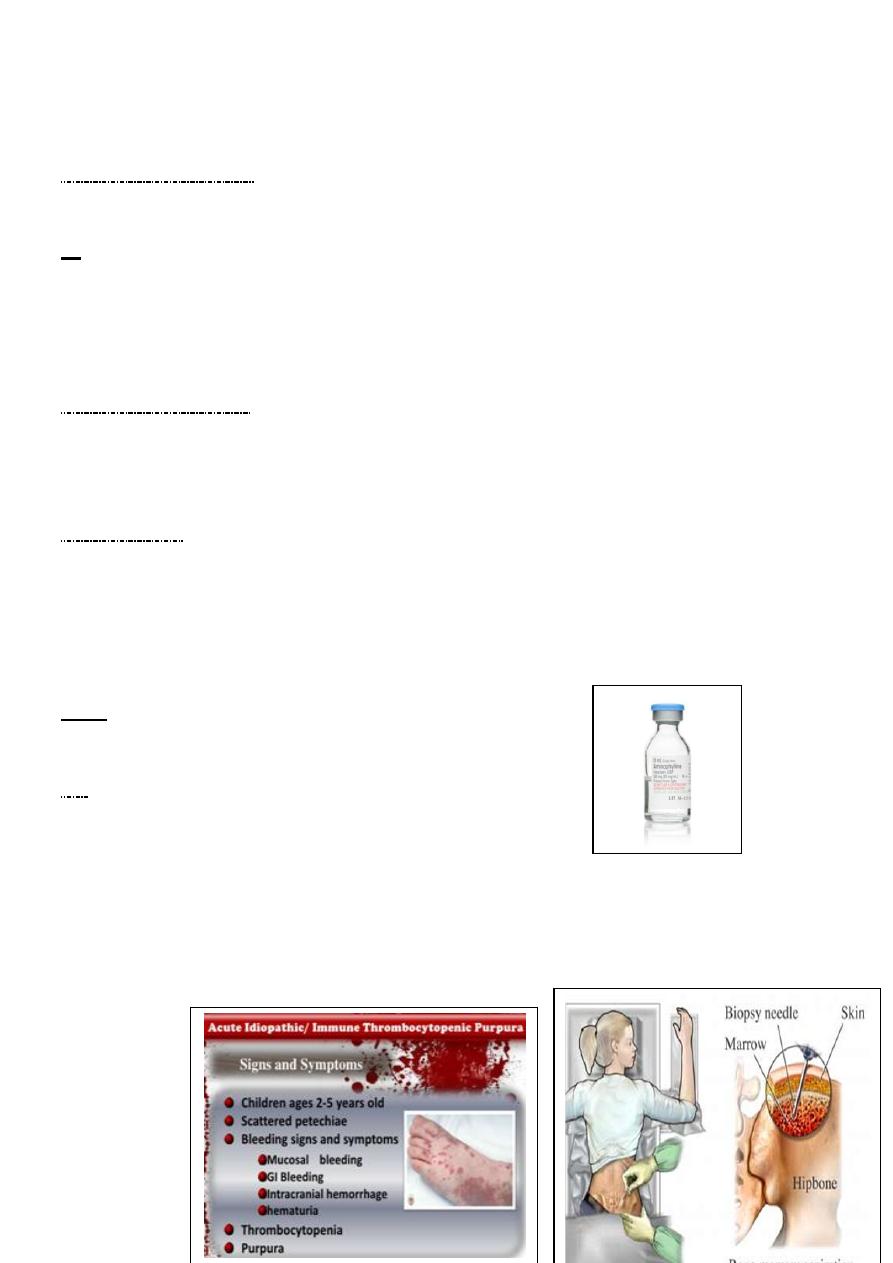
84
Acute chest syndrome
Severeand may be fatal due to vasooclusive crises leading to hypoxia and needs urgent
exchange blood transfusion and ventilation.
Rx
regular monthly blood transfusion to dilute the
sickling cells and prevent recurrence. Also give hydroxurea to increase HBF
Pneumococcal vaccine should be given and also routine vaccination for H.influenza .
Exclusive curative treatment is by BMT.
Renal failure "anuria"
Chart for input /output,Iv fluid/protein restriction/weighing every day/if hyperkalemia
correct/diuretics(1mg/kg/dose).
**then look for the cause.
Hypoglycemia
Presentation : Hypotonia, lethargy, apathy, poor feeding, jitteriness, and seizure are
common.
Congestive heart failure, tachycardia, cyanosis, pallor, diaphoresis, apnea, and hypothermia.
Rx: Requires IV fluid, hypertonic glucose as initial intravenous bolus infusion of 200mg/kg
[2ml/kg] 10%glucose, this should be followed immediately by continuous infusion of 6-
8mg/kg/min of glucose.
Note : aminophylline dose :250mg= 250cc/ 375 mg.
Don't use salbutamol in child (<15-12mo)age.
ITP
Hx of previous viral infection (2-3)wks.
Presentation:- in otherwise healthy infant in the absence
of Hepatosplenomegaly/bone pain/anemia/lymphadenopathy.
Investigations: CBC, blood filmreduction in
platelets count+absent of immature leucocytes.
Do n't do bleeding time test as this leads to severe
bleeding sometimes.
If leukemia is suspected Bone marrow exam is
mandatory.
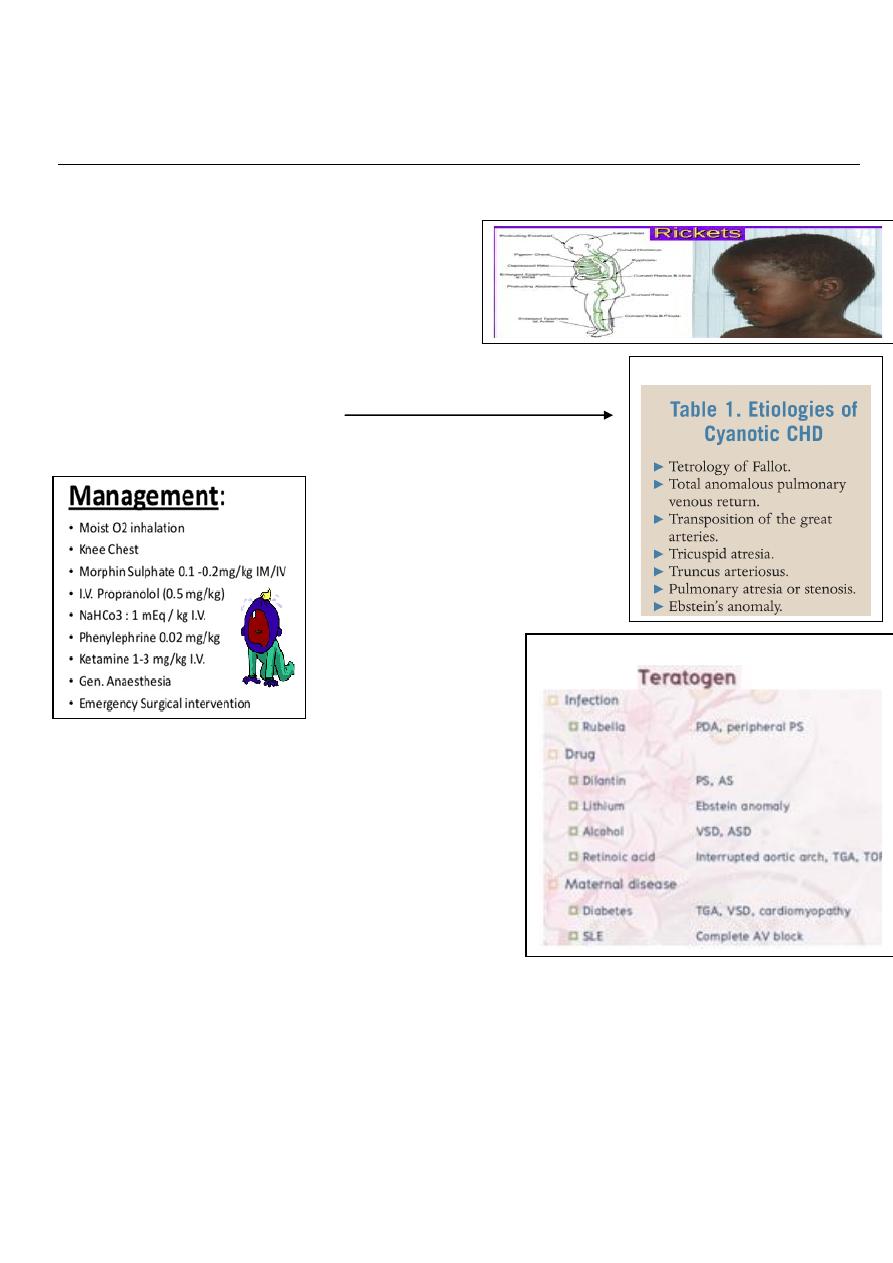
85
6
th
stage
Pediatrics
lec.5
د
.
ربيع الدبوني
Session notes
2016/9/3
General notes :
No rickets during marasmus due to calcium and minerals deficiency
-caput quadratum caused by rickets
-Clubbing most obvious site big toe
Cyanotic heart disease:
During history presentation try to avoid using definitive diagnose
try to give differential diagnose.
Hypercyanotic spell
-Recurrent chest infection occurs in right to left shunt
-Infection also reaches to brain brain abscess
-This infection can be rise from valve affected by
infective endocarditis.
-Circumsicion can result in bleeding due to
secondary polycythemia
-Child with snoring adenoid hypertrophy.
DDx of cyanotic heart disease:
Drugs cause congenital heart disease:
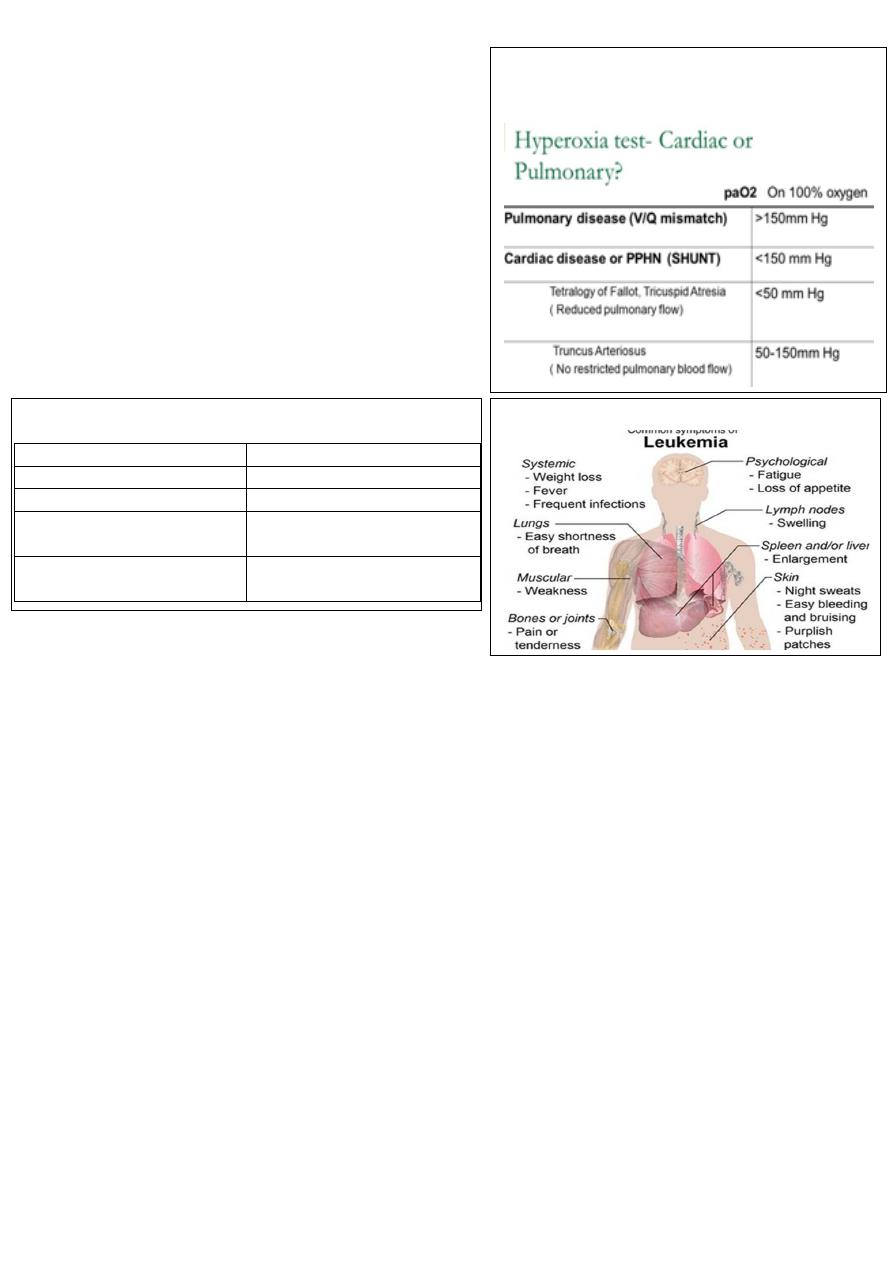
86
In a newborn which is centrally cyanosed at birth
what is your DDx?
1-CNS: convulsions, coma, abnormal breathing,
acidotic respiration gasping breathing, pupillary
dilatation, spastic.
2-haematological: rare may be due to
methaemglobinemia
3-respiratory
4- cardiac.
________________________________________
Bleeding tendency:
Check for
1-frequency
2- Local or general
3-any trauma, circumcision
4-history of affected liver or spleen
5-history of bleeding tendency , PUO , haematological dis.
6-family history
7- Ask about menorrhagia a,d metorrhagia in female
On Exam: look for:
1-anemia
2-purpura , petechia , ecchymosis
3-lymphadenopathy
4-hepatosplenpmegaly
5-uremia from acidotic breathing
6-exam the joint mainly in SLE ( bleeding + arthritis )
or recurrent haemarthrosis and leukemia
7-examine the skin , mucous membrane , conjunctiva
# How to differenciate between cardiac and
respiratory cause in cyanosed neoborn?
A/ by hyperoxia test.
Leukemia presentation:
#differences between CP and degenerative brain diseases:
Cerebral palsy
Degenerative brain disease
1. Acquired
1.
inherited
2.static
2-progressive
3-no inheritance
3-autosomal recessive
eg, WHD
4-associated with UTI
4-associated with PKU ,
glycogen storage diseases

87
Note: if there is any hemorrhagic bullae in the oral cavity or conjunctiva it is due to
thrombocttopenia
PT ( protrombin time to measure factors ( 2 , 5 , 7 , 10 ) abbreviated as (1927)
PTT ( prothromboplasin time ) : to measure any factor except 7
Case: a male baby with GIT bleeding, breast fed baby
Invx : PTT increased , PT increase , BT normal , what is the Dx ?
A: Hemorrhagic disease Vitamin K deficency
Invx : PTT , PT , BT
Tx :According to condition:
Life threatening bleeding blood transfusion, fresh frozen plasma
Mild Vit.K replacement
After 2 hours pt return normal
Case: male newborn his aunt son with bleeding tendency and heamarthrosis ?
A: Haemophilia
INVX: factor 8, 9
Tx : factor 8 replacement
Note: all thrombocytopenia associated with mucous membrane bleeding and GIT bleeding
more than deeper tissue bleeding
Haemophilia rarely associated with GIT bleeding
Case: a child with infuenza , recurrent nose bleeding , skin bleeding
After 2 weeks from starting of infection , on exam normal temp. Hb =12
No hepatosplenomegaly no LAP your Dx ?
A: Idiopathic thrombocytopenia (ITP)
Dx : BM biobsy , increase megakaryocytes
Case : a female child 3 years old with recurrent nose bleeding on exam well growth no
anemia no fever , Hb : 12 , platelets : 12 ,000
BT : increase , PTT : increase , her mother with heavy cycle ?
Dx : Von willbrand dis. VWB
Invx : PFT ( platelet function test )
Exam by : Antibiotics ( restocin ) , ADP
Treatment is to give DDAVP ,for mild bleeding, or give plasma-derived FVIII concentrate
,which cannot produced by recombinant way ,it should be with FVIII because it hold it in the
plasma. Also same advice to the pt, not to have intramuscular injection or aspirin or NSAID
Down's syndrome (trisomy 21)
This is the most common autosomal trisomy and the most common genetic cause of severe
learning difficulties. The incidence in live-born infants is about 1 in 650. Cytogenetics
The extra chromosome 21 may result from non-disjunction, translocation or Mosaicism
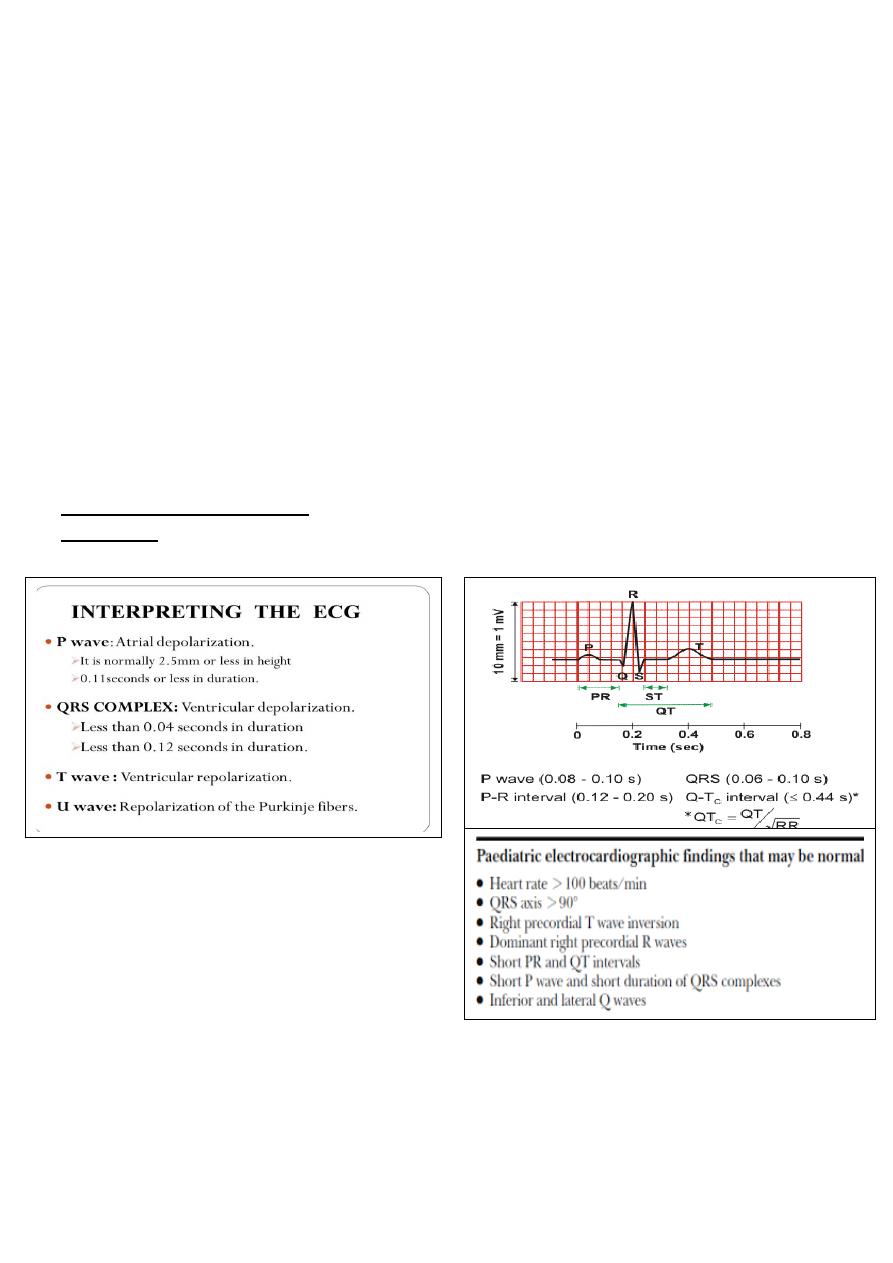
88
Non-disjunction (94%) most cases result from an error at meiosis the pair of chromosome
21s fails to separate, so that one gamete has two chromosome 21s and one has none
fertilisation of the gamete with two chromosome 21s gives rise to a zygote with trisomy 21
parental chromosomes do not need to be examined.
Translocation (5%) When the extra chromosome 21 is joined onto another chromosome
(usually chromosome 14, but occasionally chromosome 15, 22 or 21), this is known as an
unbalanced Robertsonian translocation. An affected child has 46 chromosomes, but three
copies of chromosome 21 material. In this situation, parental chromosomal analysis is
essential since one of the parents carries a balanced translocation in 25% of cases.
Translocation carriers have 45 chromosomes, one of which consists
the two joined chromosomes the risk of recurrence is 10-15% if the
mother is the translocation carrier and about 2.5% if the father is the carrier if a parent
carries the rare 21:21 translocation, all the offspring will have Down's syndrome if neither
parent carries a translocation (75% of cases).
Electrocardiography ( ECG ) :
Definition :
Recording the electrical activity of the heart
SPEED 25-50 mm/sec according to the activity
Prolonged PR interval BBB normal 3-5 small
sequares
Short PR interval WPW
QRS from beginning of Q till to the end of S
Prolonged in QRS BBB
QTc from end of QRS till to end of T-WAVE
QTc interval
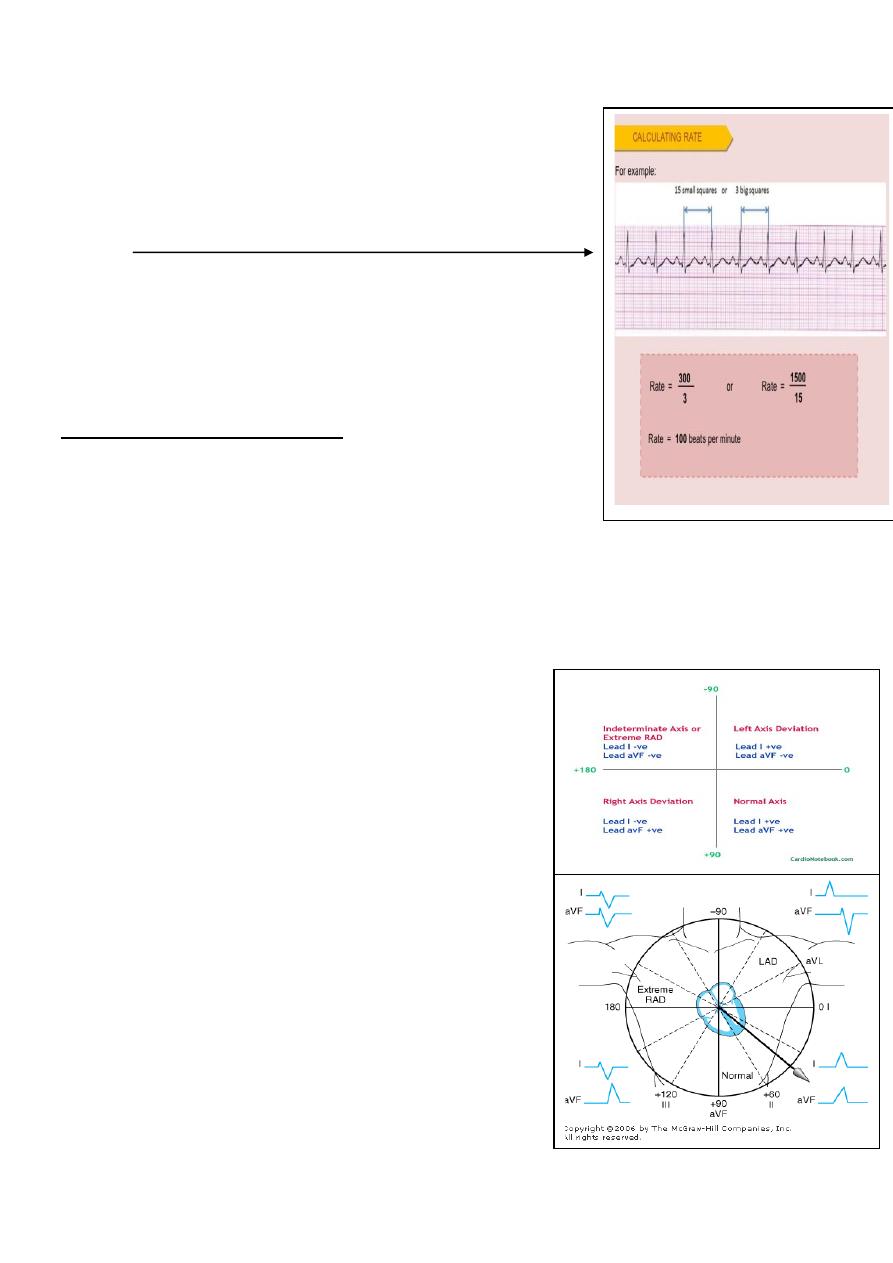
89
QT interval prolonged if > 0.45 sec
ECG reading :
When you ECG read should be done in a structured way:
1-rhythm: regular or irregular
Look for the interval between the R-R wave.
2-Rate:
3-The axis: it is right or left axis
How you going to assess the axis?
Before birth baby's right ventricle is the predominant and the
left ventricle is not-functioning as baby receives blood from
his circulation and mother and is it is oxygenated blood already
by SVC TO RA AND RIGHT VENTRICLE.
right ventricular predominance:
to decide the axis look for the:
lead I, III , avF = limb leads
Example: 1 day
-lead I shaking hand with lead II (lead I ↓ and AVf (or lead III) ↑ right axis deviation.
If lead I ↑and lead III (or AVf) ↓ left axis deviation
If the two leads looks toward the same side it is normal axis
If the both lead I and lead III are ↓ it is undetermined axis (extreme right or extreme left)
Axis:
0 90 normal
90 180 right axis
0 - 90 left axis
0 - 180 inderterminated axis or extreme
Right ventricular predominance
In normal Chest lead cover the right ventricle from V1-V5.
V6 receives the voltage from left ventricle as it is lies
posterior predominantly.
In patient with VSD can be present with right ventricular
hypertrophy and left to right shunt and pulmonary HT
If V6 is negative it is RVH
IF V6 is positive it is LVH
AFTER that look for the interval:
QRS, P-wave, QT interval, ST, PR
Right ventricular hypertrophy
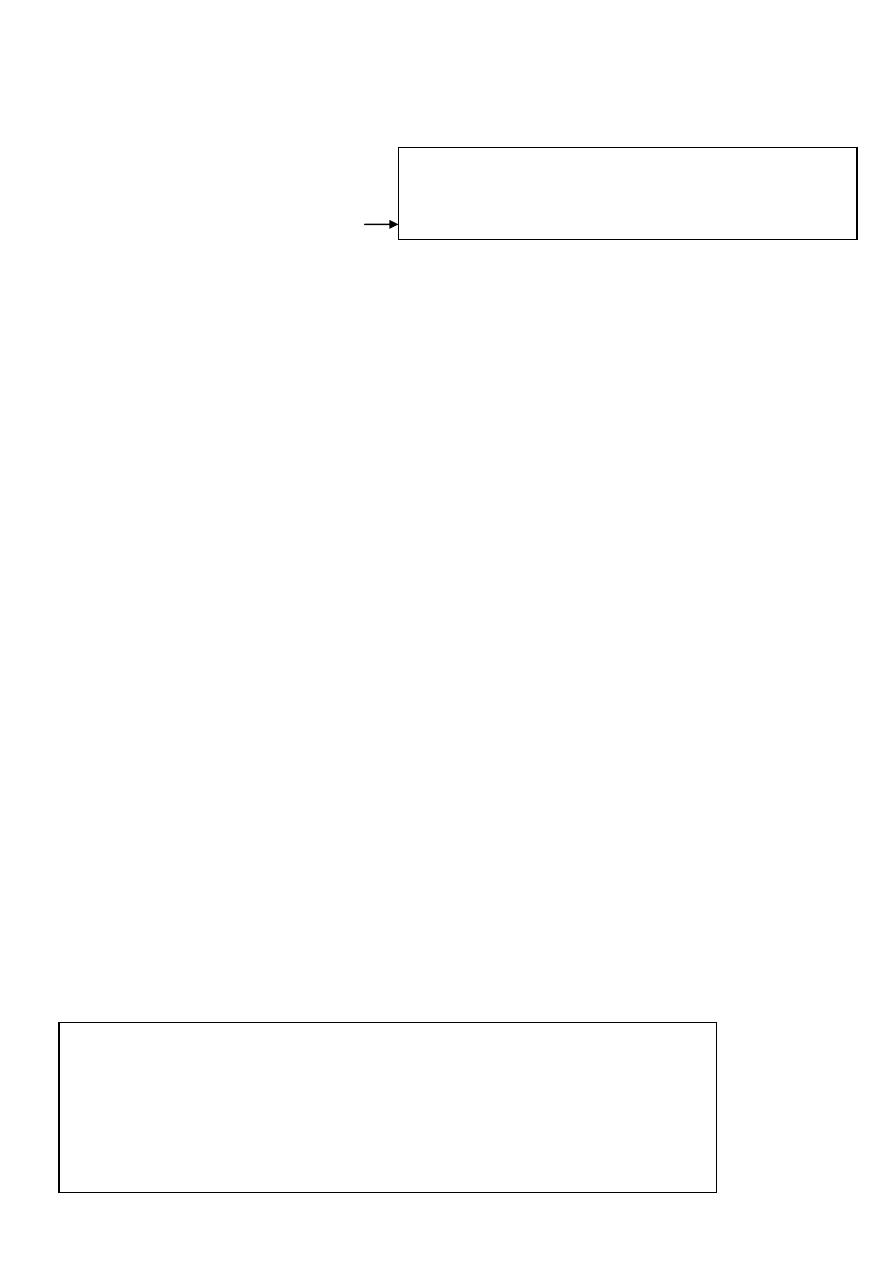
90
Criteria:
1. Prominent right axis deviation
2. Prominent R IN V1
3. Small S in V6
4. UP ward T-wave in (V 1, 2 and 3)
-When child grows right axis deviation changed from right toward the normal site
-During the first year of life right axis effects is resolved
-Normal RS progression proceeds during child growth and changed from right axis deviation
toward left axis until in become normal (0 - +90⁰).
-Prominent R in V1 decrease and increase in V6
-Prominent S1 increase in V1 and decrease in V6
Q/Can MI presented in pediatric age group?
1-Familial hyperlipidemia
2-anamolus origin from left coronary artery
3- Kawasaki dis. thrombosis of coronary a
4- Thrombophilia inheretd anti-thrombin deficiency.
-p- pulmonale right atrial hypertrophy
-p-mital left atrial hypertrophy
Best reading for ECG from lead II
And take a trace ECG to discover rhythm abnormality
Tented T-wave in in lead II indicate hyperkalemia
V4 R mains V4 on the right side and it is similar to V1
Sinus arrythemia Sinus arrythmia : occur during inspiration by increased heart beats
-Ectopic beat with pause temporary
ساليد
14
QRS distorted
Right ventricular hypertrophy: upward T-wave in V1 , V 4
Strain pattern in V6 IN left ventricular hypertrophy
Complete bundle branch block or RS-R pattern
ساليد
17
Look for V4 QRS M-shape
This condition presented in ostium primeum canal associated with Down's syndrome
ASD+VSD = AV CANAL
Regarding T wave in V1, 2 and 3:
- 6 days- 6years must be inverted (otherwise it is RVH)
- 6years- 12 years may or may not be inverted.
-
One of the main differences from adult ECG.
QT prolonged in
1- Congenital diseaase:
a- Autosomal recessive
b- Autosomal dominent
2- Acquired:
Hpypocalcemia most common and less in hypokalemia , hypomagnesimia
The danger when changed to arrythmia and it is bradycardia
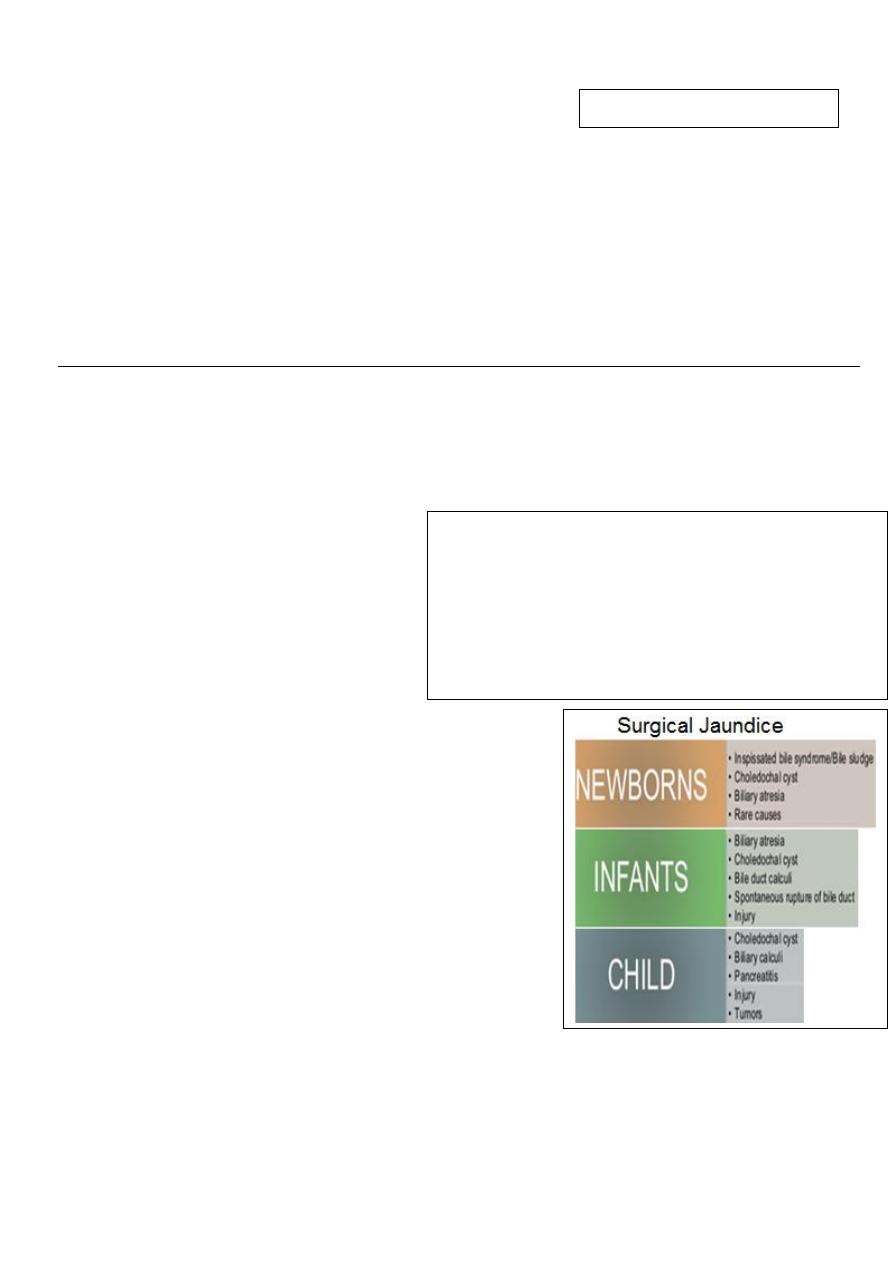
91
Tachycardia + absent p-wave = SVT
Tx :
Short PR , J-wave , wide QRS Wolf parkinsonian white syndrome
SVT + adenosine
اخر ساليد
ECG RBBB IN OSTIUM PRIMEIUM
LBBB IN CARDIAC SURGERY
____________________________________________________________________________
6
th
stage
Pediatrics
lec.3
د
.
رياض العبيدي
Session notes
Neonatal jaundice
Prolonged neonatal jaundice means more than the physiological pathological
Ask about family Hx, TORCH infection
Hemorrhagic disease of newborn indicate Vit.K deficeincy syndrome
DDx of Generalized bleeding tendency?
1-ITP (idiopathic thrombocytopenic
purpura)
2-Haemophilia
3-Factor 7, 5 deficeincy
Approach to patient with
hemorrhagic disease:
1-Bleeding profile
2-CBC
3-GUE: to search for bile pigment cholestasis
4-Urine reducing substance: to look for galactosemia
5-chromatography: to check for amino-acid
6-ASPG, ASPOT liver enzyme to see if there is hepatitis
7-Alkaline phosphatase enzyme.
8-Blood group: ABO, Rh to exclude inspissated bile
syndrome is defined as partial or complete obstruction
of the extra hepatic biliary system by impaction of thick
bile or sludge in the distal common bile duct during the
neonatal period.
9-congenital infection : TORCH ( Toxoplasmosis rubella , Cytomegallovirus , Herpes virus ) to
measure IgM or IgG
QRS MUST be followed by T
Hemorrhagic disease classified as :
1- Early type: 24 hours
2- Classical: 24 – 7 days
3- Late: > 7
eg ; liver disease (cholastasis), alpha1-antitrypsin deficeincy
, galactosemia, malabsorption
Invx : PTT , PT , CBC , BT ( Bleeding profile )
In Vit.K ↑PT, ↑APTT, BT normal
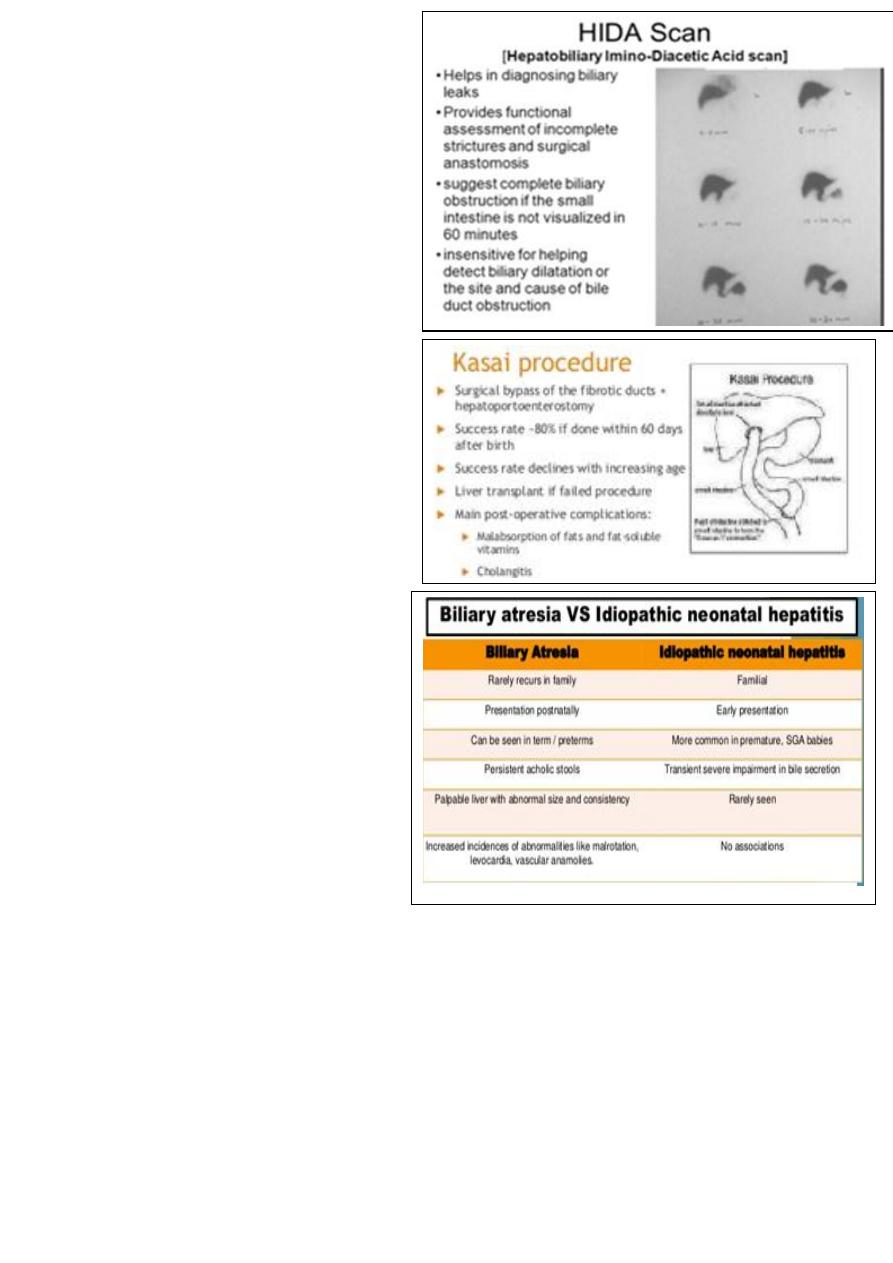
92
10-U/S: intrahepatic biliary diltation
11- Cholescitography using Hida scan.
On Exam :
1-cataract: associated with galactosemia
2-face: if ugly Argyll syndrome
3-Heart: look for coarctation of aorta,VSD
4-convlusion: seek for hypoglycemia
Treatment:
Vit. K replacement mainly fresh frozen
plasma, There is 3 types of vitamin K
(1, 2 and 3), given mainly IM and monitor
the patient to avoid anaphylactic shock
Surgical operation for biliary atresia is
called Kasai portoenterostomy.
________________________________
Diabetic ketoacidosis
Random blood sugar should be :
>11 mmol/l or 200 mg/l
In fasting > 7 mmol/l or 127 mg / l
Look for this sign in DKA :
1-Tachypnea
2-dehydration
3-Abdominal pain
4-vomiting
5- polyuria , polydepsia
Management
1-hospital admission
2-monitoring
3-IV canula
4-Draw bolld sample for : RBS , seum electrolyte
5-blood gas analysis ( BGA)
6- Serum BUN
Even pateint is severely dehydrated urin still present due to osmotic diuresis
7-HbA1c ( glycosalted hemoglobin )
For past 3 months if > 6.5 is diagnostic for DKA
There pseudohypernatremia in DKA
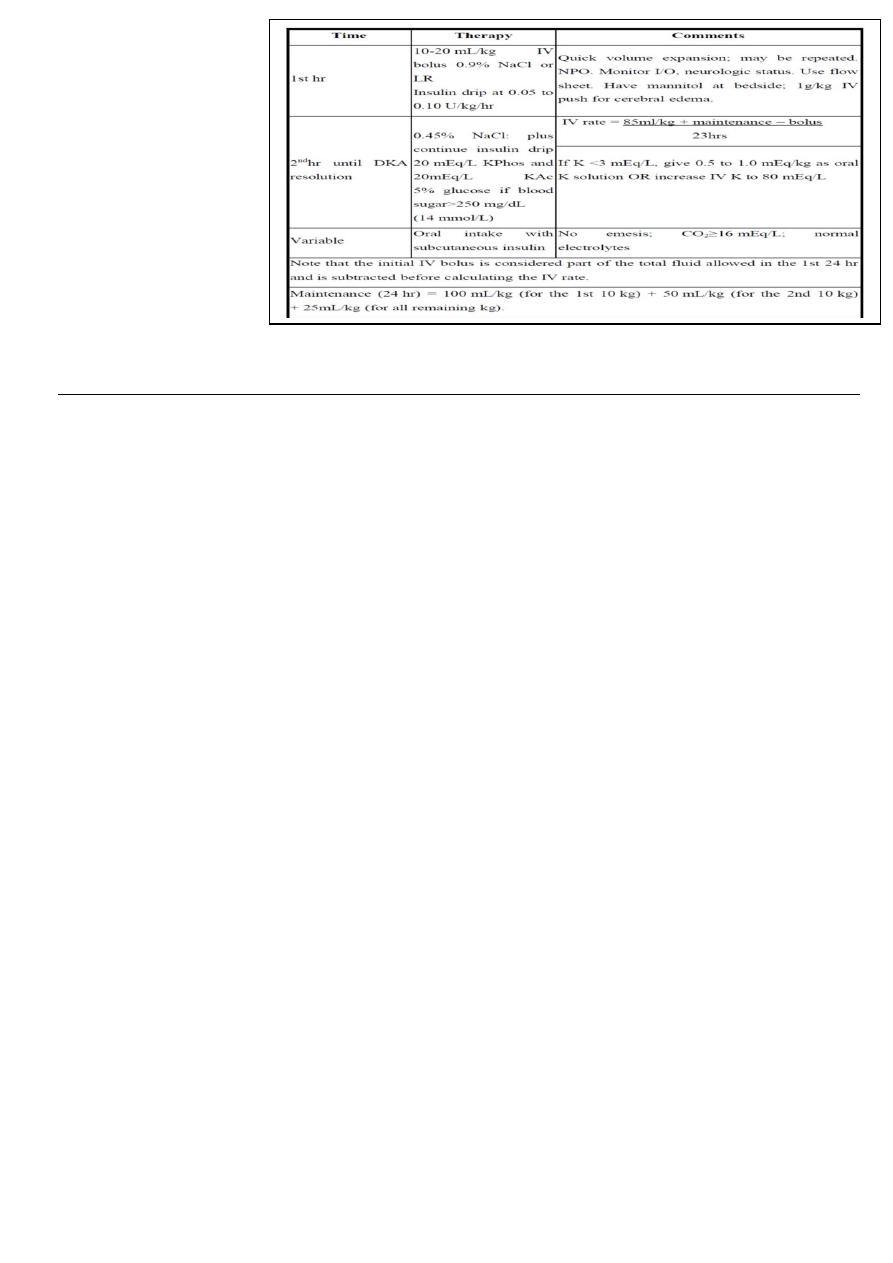
93
Treatment (important):
____________________________________________________________________________
6
th
satge
Pediatrics
lec.2
د
.
ندى العلي
Session notes
2016/9/8
Approach to pt with SOB
1-onset of SOB
2-duration of SOB
3-timing (at night or day time)
4- precipitating factors: exercise , perfume , dust.
5-Ass. symptoms : cyanosis or congestionيصير احمر مو ازرق, runny nose, noisy breathing,
chest pain , sore throat , sputum , hemoptysis
8- aggravating factors & relieving factors: certain position
9- frequency of the attacks
10- wt. gain , sleeping pattern , interfere with the activity
11- associated with eczema , allergy
12-management received ?response?
Pt with cough
1-Duration
2- Onset
3- Time of occurrence ( night , morning)
4- Frequency&severity
5- Short or Paroxysmal
6- Character : barking , whooping
7- Dry or productive : if there is sputum : color , amount , with blood , smell
8- Aggravating factors relieving factors
9- Associated symptoms( fever, dyspnea, vomiting , convulsion, cyanosis , noisy breathing,
hoarse voice, sore throat)
11- Effect on feeding , sleeping , activity
VSDacyanotic.
CHD inherited as multifactorial.

94
Accounts for 25% of CHD
harsh pansystolic murmur heard along the LSB, more prominent with small VSD
Complications:
1-FTT
2-CHF
3-pulmonary hypertension
4-infective endocarditis
5-CVA
6-arrythmia
Investigations:-
CXR
ECG
ECHO
Treatment
Small VSD - no surgical intervention, nophysical restrictions, just reassurance and periodic
follow-up and endocarditis prophylaxis.
Symptomatic VSD - Medical treatment initially with afterload reducers & diuretics± digoxin
Prophylaxis against infective endocarditis(after dental or GU procedures
Indications for Surgical Closure
Large VSD with medically uncontrolled symptomatology & continued FTT.
Ages 6-12 mo with large VSD & Pulmonary HTN.
Age > 24 mo w/ Qp:Qs ratio > 2:1.
Supracristal VSD of any size.
ASDRV heave, fixed widely split S2,systolic ejection murmer/on ECG —right-axis
deviation and RVH.
NOTERAD normal in infants & children till 4yrs of life.

95
H.F complications
1-FTT caused by chronic hypoxia+increased caloric needs by the tissue+feeding interruption
+drugs taken that leads to anorexia.
2-recurrent chest infection.
Signs of H.F
1) tachycardia
2 )tachypnea
3) pulmonary rales
4) cardiomegaly on XR.
**ask about consanguinity+ any family Hx for CHDfor recurrence of same problem in the
other siblings.
Rash +abdominal pain + fever+vomitingsuspect HSP+scarlet fever"pastia lines "
The definitive diagnostic method to enteric feverblood culture,widal test will be
positive 2 wks later on.
Connective tissue disease criteria(4 of which should be present):-
Constitutional (eg, fatigue, fever, arthralgia, weight changes)
Musculoskeletal (eg, arthralgia, arthropathy, myalgia, frank arthritis, avascular necrosis)
Dermatologic (eg, malar rash, photosensitivity, discoid lupus)
Renal (eg, acute or chronic renal failure, acute nephritic disease)
Neuropsychiatric (eg, seizure, psychosis)
Pulmonary (eg, pleurisy, pleural effusion, pneumonitis, pulmonary hypertension,
interstitial lung disease)
Gastrointestinal (eg, nausea, dyspepsia, abdominal pain)
Cardiac (eg, pericarditis, myocarditis)
Hematologic (eg, cytopenias such as leukopenia, lymphopenia, anemia, or
thrombocytopenia)
