volume output per beat even during periods of rest. When the athlete is at rest,
that of a normal person, which allows the athlete’s heart to pump a large stroke
The athlete’s heart is larger and considerably stronger than
beats per minute. Bradycardia is shown by the electrocardiogram in Figure 13–2.
The term “bradycardia” means a slow heart rate, usually defined as fewer than 60
and this elicits sympathetic reflexes to increase the heart rate.
often increases the heart rate to 150 to 180 beats per minute.
passes into a state of shock or semishock, sympathetic reflex stimulation of the heart
discuss at multiple points in this text. For instance, when a patient loses blood and
Many factors can cause the sympathetic nervous system to excite the heart, as we
node, which in turn directly increases its excitability and rate of rhythm.
progressive debility of the heart muscle as a result of the fever. Fever causes tachy-
ture of about 105°F (40.5°C); beyond this, the heart rate may decrease because of
(18 beats per degree Celsius) increase in body temperature, up to a body tempera-
The heart rate increases about 10 beats per minute for each degree Fahrenheit
of the heart by the sympathetic nerves, or toxic conditions of the heart
increased body temperature, stimulation
The general causes of tachycardia include
is about 150 per minute instead of the normal 72 per minute.
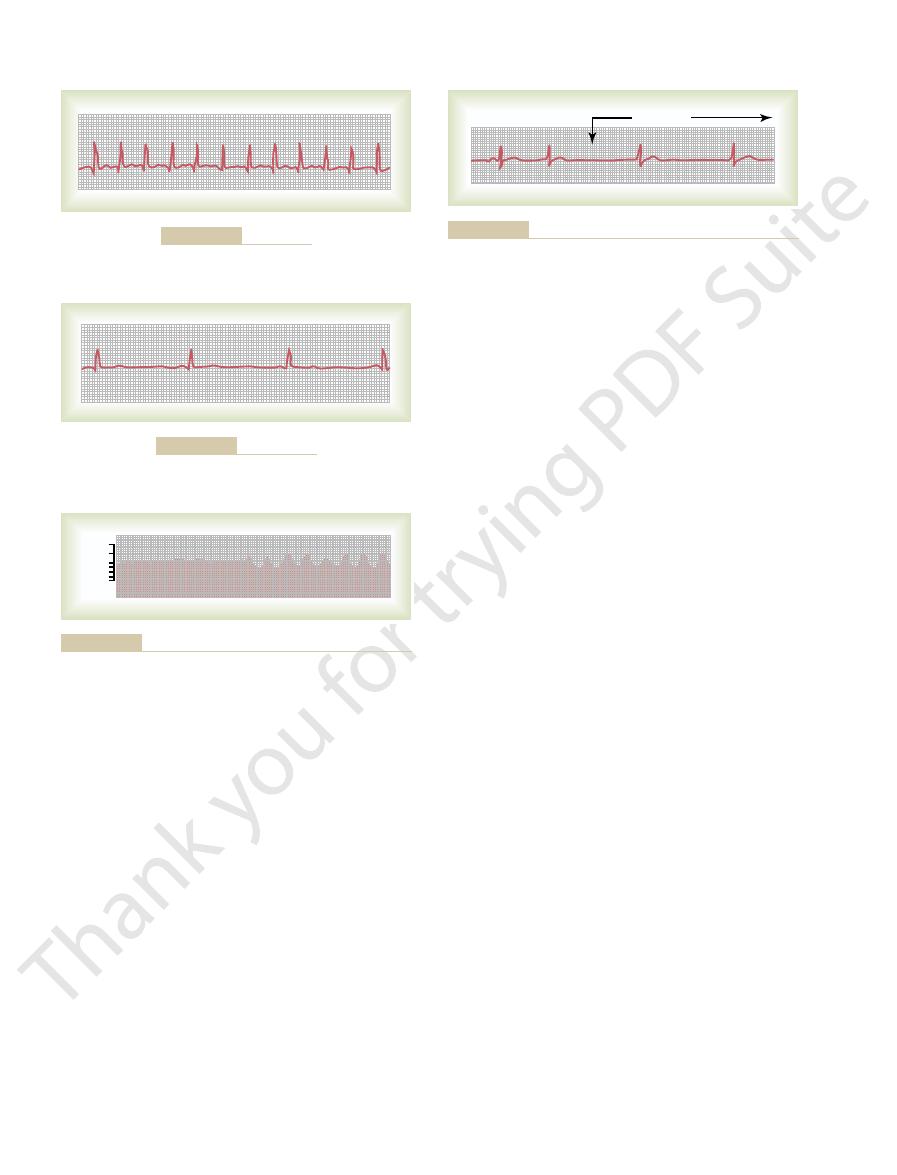
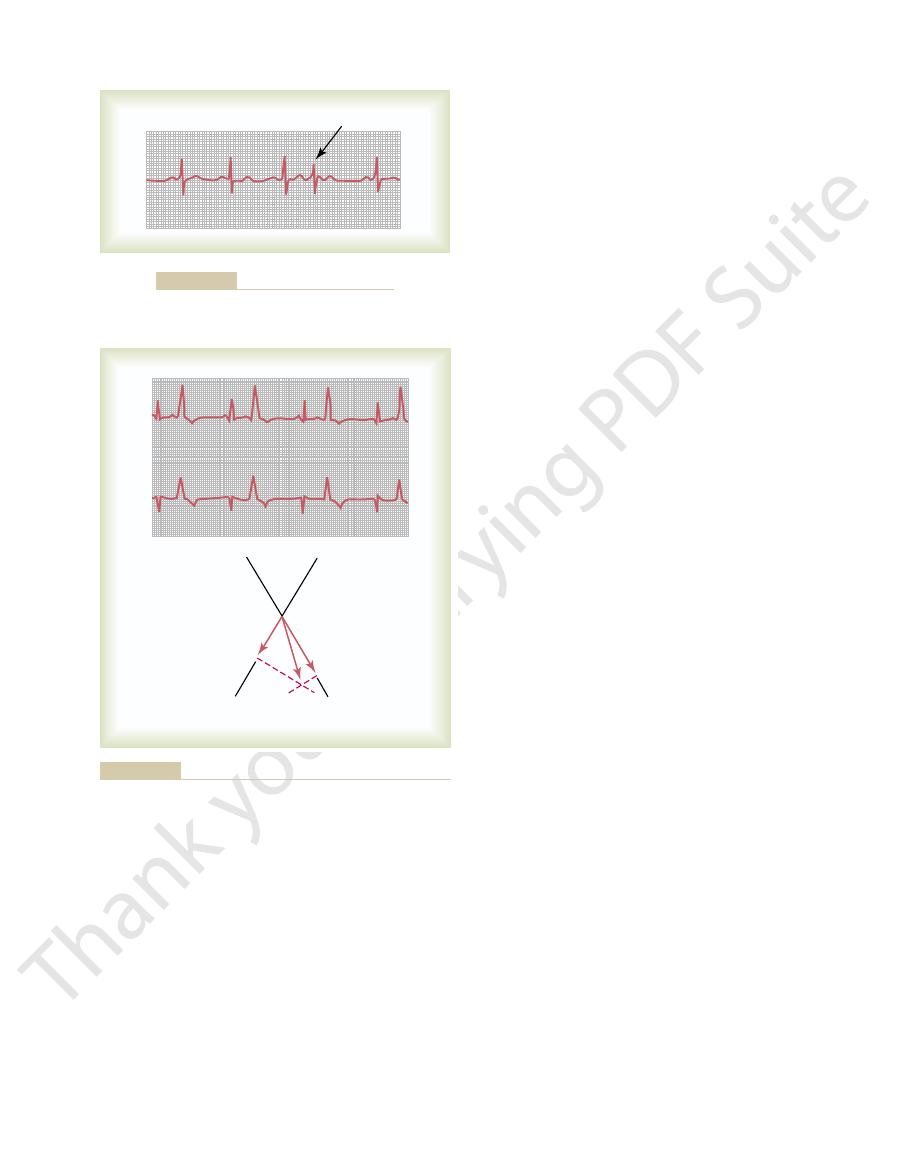
that the heart rate, as determined from the time intervals between QRS complexes,
with tachycardia is shown in Figure 13–1. This electrocardiogram is normal except
faster than 100 beats per minute. An electrocardiogram recorded from a patient
fast heart rate,
The term “tachycardia” means
Tachycardia
Abnormal Sinus Rhythms
5. Spontaneous generation of spurious impulses in almost any part of the heart
4. Abnormal pathways of impulse transmission through the heart
3. Blocks at different points in the spread of the impulse through the heart
2. Shift of the pacemaker from the sinus node to another place in the heart
1. Abnormal rhythmicity of the pacemaker
electrocardiography. The causes of the cardiac arrhythmias are usually one or a com-
effects on heart pumping, as well as their diagnosis by
The purpose of this chapter is to discuss the
function as primer pumps for the ventricles.
the beat of the ventricles, so that the atria no longer
because of abnormal rhythm of the heart. For instance,
Their Electrocardiographic
Cardiac Arrhythmias and
C
H
A
P
T
E
R
1
3
147
Interpretation
Some of the most distressing types of heart malfunction
occur not as a result of abnormal heart muscle but
sometimes the beat of the atria is not coordinated with
physiology of common cardiac arrhythmias and their
bination of the following abnormalities in the rhythmicity-conduction system of the
heart:
usually defined in an adult person as
.
cardia because increased temperature increases the rate of metabolism of the sinus
Simple weakening of the myocardium usually increases the heart rate because
the weakened heart does not pump blood into the arterial tree to a normal extent,
Bradycardia
Bradycardia in Athletes.
excessive quantities of blood pumped into the arterial tree with each beat initiate
feedback circulatory reflexes or other effects to cause bradycardia.
ventricles. Inflammation results frequently from
Inflammation of the A-V node or A-V bundle
conduction from the atria to the ventricles.
Compression of the A-V bundle
ischemia of the A-V node and bundle in the same
the ventricles. Coronary insufficiency can cause
Ischemia of the A-V node or A-V bundle fibers
bundle of His.
bundle,
The only means by which impulses ordinarily can pass
atrioventricular (A-V) node, so that the rate of the ven-
the atria. However, the ventricles pick up a new rhythm,
sudden cessation of P waves, with resultant standstill of
nomenon is demonstrated in Figure 13–4, which shows
blocked before it enters the atrial muscle. This phe-
In rare instances, the impulse from the sinus node is
Intracardiac Conduction
Result from Block of Heart
Abnormal Rhythms That
ratory and expiratory cycles of respiration. The spillover
“spillover” of signals from the medullary respiratory
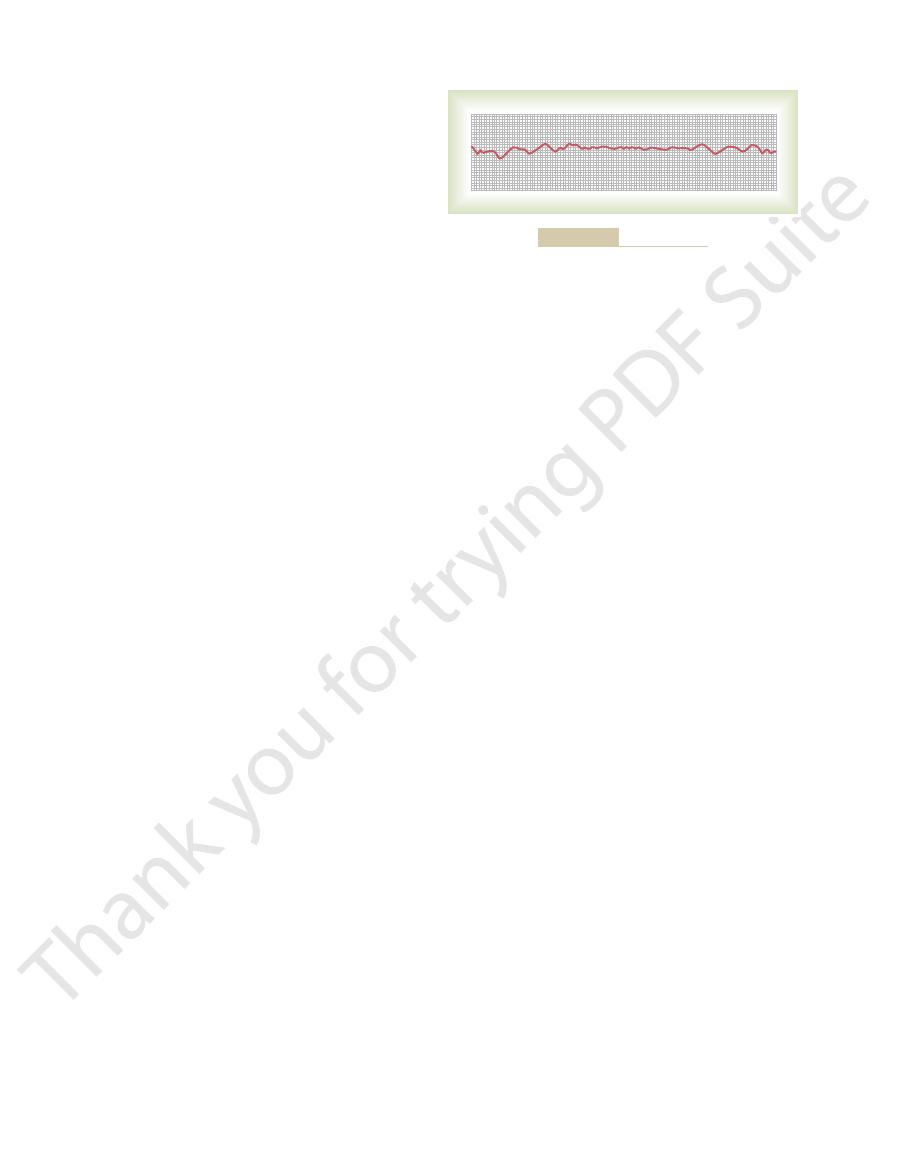
mia, as shown in Figure 13–3, this results mainly from
sinus node. In the “respiratory” type of sinus arrhyth-
with each respiratory cycle by as much as 30 per cent.
, the heart rate increased and decreased
quiet respiration (left half of the record). Then,
diogram. Note from this record that the heart rate
by the height of
half of the record) during deep respiration. A cardiota-
heart rate, at first during normal and then (in the second
cardiotachometer
Figure 13–3 shows a
ally stops the heart for 5 to 10 seconds.
Indeed, sometimes this reflex is so powerful that it actu-
effects on the heart, including extreme bradycardia.
baroreceptor reflex, causing intense vagal-acetylcholine
artery walls are excessively sensitive. Therefore, even
In these patients, the pressure receptors
syndrome.
giving a parasympathetic effect. Perhaps the most strik-
acetylcholine at the vagal endings in the heart, thus
Vagal Stimulation as a Cause of Bradycardia.
148
Unit III
The Heart
Any circulatory
reflex that stimulates the vagus nerves causes release of
ing example of this occurs in patients with carotid sinus
(baroreceptors) in the carotid sinus region of the carotid
mild external pressure on the neck elicits a strong
Sinus Arrhythmia
recording of the
chometer is an instrument that records
successive spikes the duration of the interval between
the successive QRS complexes in the electrocar-
increased and decreased no more than 5 per cent during
during
deep respiration
Sinus arrhythmia can result from any one of many cir-
culatory conditions that alter the strengths of the sym-
pathetic and parasympathetic nerve signals to the heart
center into the adjacent vasomotor center during inspi-
signals cause alternate increase and decrease in the
number of impulses transmitted through the sympa-
thetic and vagus nerves to the heart.
Signals Within the
Pathways
Sinoatrial Block
the impulse usually originating spontaneously in the
tricular QRS-T complex is slowed but not otherwise
altered.
Atrioventricular Block
from the atria into the ventricles is through the A-V
also known as the
Conditions that
can either decrease the rate of impulse conduction in
this bundle or block the impulse entirely are as follows:
1.
often delays or blocks conduction from the atria to
way that it can cause ischemia of the myocardium.
2.
by scar tissue or by
calcified portions of the heart can depress or block
3.
can depress conductivity from the atria to the
Sinus tachycardia (lead I).
Figure 13–1
Sinus bradycardia (lead III).
Figure 13–2
60
70
80
100
120
Heart rate
when breathing deeply.
the record when the subject was breathing normally; to the right,
Sinus arrhythmia as recorded by a cardiotachometer. To the left is
Figure 13–3
SA block
Figure 13–4
Sinoatrial nodal block, with A-V nodal rhythm during the block
period (lead III).
ventricular escape.
ventricles. This is called
the blocked point in the node, or in the A-V bundle,
block, usually in the distal part of the A-V node beyond
seconds, some part of the Purkinje system beyond the
than their natural rate of rhythm. However, after a few
This means that ventricular
overdrive suppression.
30 seconds. This results from the phenomenon called
Each time A-V conduction ceases, the ventricles often
weeks or longer before conduction returns. This condi-
be a few seconds, a few minutes, a few hours, or even
impulses are not conducted. The duration of block may
that is, impulses are conducted from the atria into the
patients with A-V block, the total block comes and goes;
Stokes-Adams Syndrome—Ventricular Escape.
or A-V bundle.
often by rhythmical signals generated in the A-V node
are beating at their own natural rate, controlled most
cles have “escaped” from control by the atria, and they
is less than 40 per minute. Furthermore,
is about 100 beats per minute, whereas the
QRS-T complexes, as shown in Figure 13–7. Note that
Therefore, the P waves become dissociated from the
usually originating in the A-V node or A-V bundle.
from the atria into the ventricles occurs. In this instance,
bundle becomes severe, complete block of the impulse
tion causing poor conduction in the A-V node or A-V
When the condi-
other times, rhythms of 3:2 or 3:1 also develop.
beating twice for every single beat of the ventricles. At
dropped, so that a “2:1 rhythm” develops, with the atria
At times, every other beat of the ventricles is
failure of conduction from the atria to the ventricles.
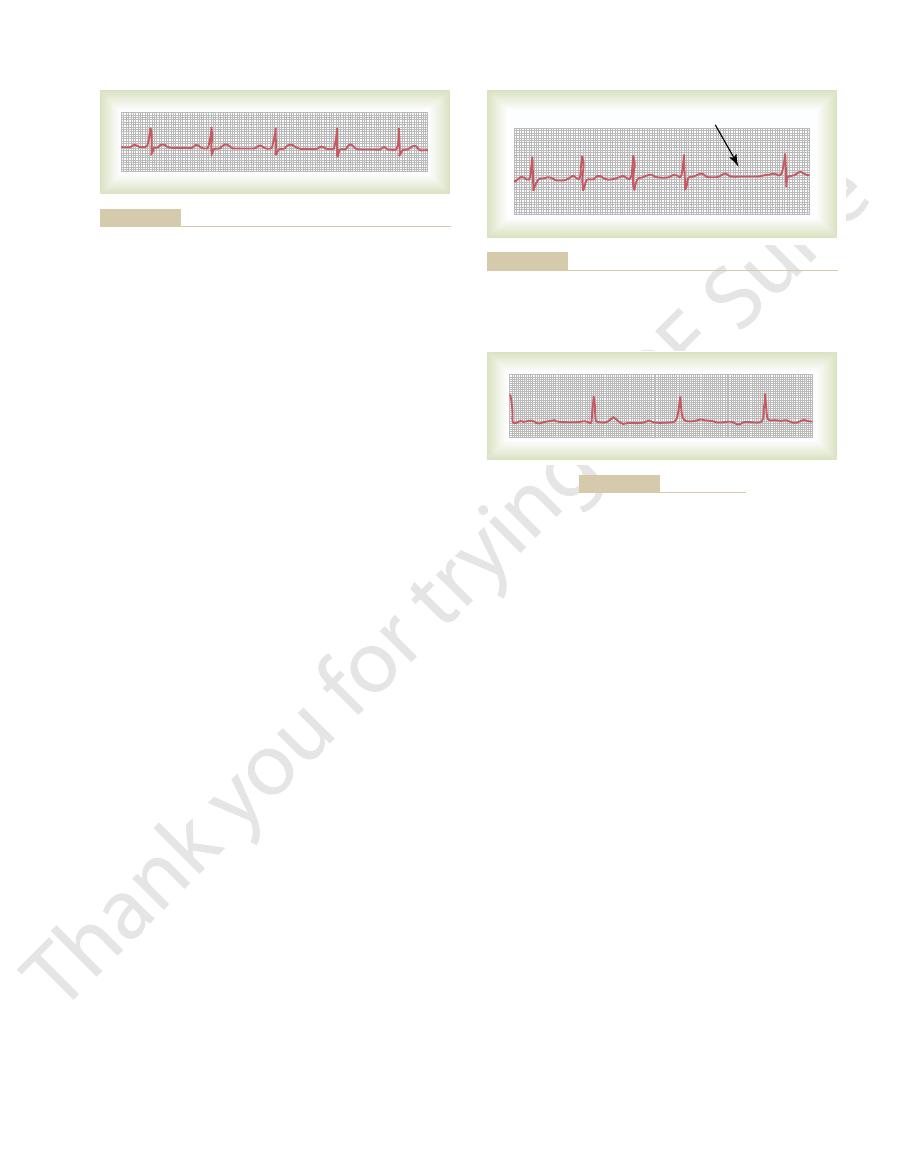
Figure 13–6 shows P-R intervals of 0.30 second, as
block.
ventricles. This condition is called
wave, and it is said that there are “dropped beats” of the
instance, there will be an atrial P wave but no QRS-T
tricles and sometimes is not strong enough. In this
0.25 to 0.45 second, the action potential sometimes is
When conduction through the A-V
stops entirely. One means for determining the severity
the A-V bundle is depressed so much that conduction
to 0.45 second because, by that time, conduction through
duction. The P-R interval seldom increases above 0.35
delay
0.30 second instead of the normal 0.20 or less. Thus, first
longed P-R interval; the interval in this instance is about
Figure 13–5 shows an electrocardiogram with pro-
block.
0.20 second, the P-R interval is said to be prolonged, and
general, when the P-R interval increases to greater than
faster heartbeat and increases with slower heartbeat. In
when the heart is beating at a normal rate. This so-
The usual
Prolonged P-R (or P-Q) Interval—First Degree Block.
syndrome,
through the A-V node. Such vagal excitation
Extreme stimulation of the heart by the vagus nerves
by diphtheria or rheumatic fever.
different types of myocarditis, caused, for example,
Cardiac Arrhythmias and Their Electrocardiographic Interpretation
Chapter 13
149
4.
in rare instances blocks impulse conduction
occasionally results from strong stimulation of the
baroreceptors in people with carotid sinus
discussed earlier in relation to
bradycardia.
Incomplete Atrioventricular
Heart Block
lapse of time between beginning of the P wave and
beginning of the QRS complex is about 0.16 second
called P-R interval usually decreases in length with
the patient is said to have first degree incomplete heart
degree block is defined as a
of conduction from
the atria to the ventricles but not actual blockage of con-
of some heart diseases—acute rheumatic heart disease,
for instance—is to measure the P-R interval.
Second Degree Block.
bundle is slowed enough to increase the P-R interval to
strong enough to pass through the bundle into the ven-
second degree heart
well as one dropped ventricular beat as a result of
Complete A-V Block (Third Degree Block).
the ventricles spontaneously establish their own signal,
the rate of rhythm of the atria in this electrocardiogram
rate of ven-
tricular beat
there is no relation between the rhythm of the P waves
and that of the QRS-T complexes because the ventri-
In some
ventricles for a period of time and then suddenly
tion occurs in hearts with borderline ischemia of the
conductive system.
do not start their own beating until after a delay of 5 to
excitability is at first in a suppressed state because the
ventricles have been driven by the atria at a rate greater
begins discharging rhythmically at a rate of 15 to 40
times per minute and acting as the pacemaker of the
P
P
P
P
P
Prolonged P-R interval caused by first degree A-V heart block
Figure 13–5
(lead II).
P
P
P
P
P
P
Dropped beat
tricles to receive the excitatory signals (lead V
Second degree A-V block, showing occasional failure of the ven-
Figure 13–6
3
).
P
P
P
P
P
P
P
P
P
P
Figure 13–7
Complete A-V block (lead II).
originated in the A-V node or in the A-V bundle. The
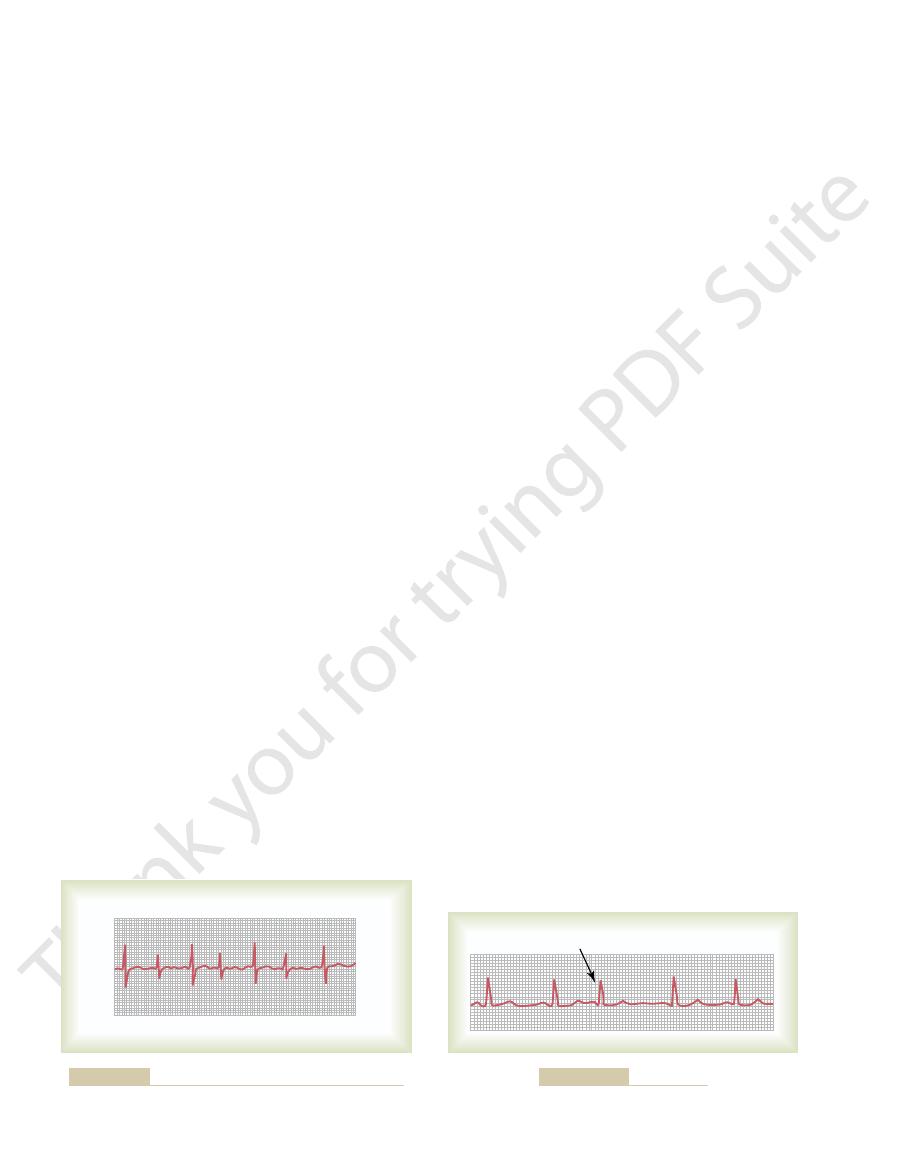
Figure 13–10 shows a premature contraction that
A-V Nodal or A-V Bundle Premature
felt in the radial artery. Thus, a deficit in the number of
contraction is depressed or almost absent. Therefore,
mally, and the stroke volume output during that
ule, the ventricles will not have filled with blood nor-
When the heart contracts ahead of sched-
such contractions.
alcoholism, and use of various drugs can also initiate
smoking, lack of sleep, ingestion of too much coffee,
otherwise healthy people. Indeed, they often occur in
sinus node discharge also late in appearing.
in the premature cycle, and this made the succeeding
sinus node. Consequently, the sinus node discharged late
node, and the impulse had to travel through a consid-
compensatory pause.
prolonged, which is called a
node. Also, the interval between the premature con-
ectopic origin of the beat is in the atria near the A-V
cycle; the P-R interval is shortened, indicating that the
The P wave of this beat occurred too soon in the heart
Figure 13–9 shows a single premature atrial contraction.
Premature Atrial Contractions
is also frequent during cardiac catheterization; large
feine. Mechanical initiation of premature contractions
system, or myocardium caused by drugs, nicotine, or caf-
and (3) toxic irritation of the A-V node, Purkinje
ent points in the heart, which press against the adjacent
areas of ischemia; (2) small calcified plaques at differ-
rhythm. Possible causes of ectopic foci are (1) local
in the heart, which emit
extrasystole,
been expected. This condition is also called
Premature Contractions
electrical alternans.
cause incomplete intraventricular block, resulting in
such as ischemia, myocarditis, or digitalis toxicity, can
heartbeat. Also, many conditions that depress the heart,
occurred, because when the rate of the heart is rapid, it
heart rate), which is probably the reason the block has
tachycardia
This electrocardiogram also shows
electrical alternans,
tricular Purkinje system. Figure 13–8 shows the condi-
Most of the same factors that can cause A-V block can
that take control of the ventricles.
electrodes usually connected to the right ventricle. The
electrical stimulator planted beneath the skin, with
artificial pacemaker,
Consequently, most of these patients are provided
detrimental to the patient’s health or even causes death.
Stokes-Adams syndrome.
the person. These periodic fainting spells are known as
until the ventricles “escape.” After escape, however, the
heart does not pump any blood for 5 to 30 seconds,
4 to 7 seconds without blood supply, most patients faint
150
Unit III
The Heart
Because the brain cannot remain active for more than
a few seconds after complete block occurs because the
slowly beating ventricles usually pump enough blood to
allow rapid recovery from the faint and then to sustain
the
Occasionally the interval of ventricular standstill at
the onset of complete block is so long that it becomes
with an
a small battery-operated
pacemaker provides continued rhythmical impulses
Incomplete Intraventricular Block—
Electrical Alternans
also block impulse conduction in the peripheral ven-
tion known as
which results from
partial intraventricular block every other heartbeat.
(rapid
may be impossible for some portions of the Purkinje
system to recover from the previous refractory period
quickly enough to respond during every succeeding
A premature contraction is a contraction of the heart
before the time that normal contraction would have
premature beat, or ectopic beat.
Causes of Premature Contractions.
Most premature con-
tractions result from ectopic foci
abnormal impulses at odd times during the cardiac
cardiac muscle so that some of the fibers are irritated;
numbers of premature contractions often occur when
the catheter enters the right ventricle and presses
against the endocardium.
traction and the next succeeding contraction is slightly
One
of the reasons for this is that the premature contraction
originated in the atrium some distance from the sinus
erable amount of atrial muscle before it discharged the
Premature atrial contractions occur frequently in
athletes whose hearts are in very healthy condition.
Mild toxic conditions resulting from such factors as
Pulse Deficit.
the pulse wave passing to the peripheral arteries after a
premature contraction may be so weak that it cannot be
radial pulses occurs when compared with the actual
number of contractions of the heart.
Contractions
P wave is missing from the electrocardiographic record
Partial intraventricular block—“electrical alternans” (lead III).
Figure 13–8
Premature beat
Atrial premature beat (lead I).
Figure 13–9
heart. This is believed to be caused most frequently by
cles, can occasionally cause rapid rhythmical discharge
including the atria, the Purkinje system, or the ventri-
Paroxysmal Tachycardia
therefore is the locus of the ectopic focus.
ture contraction is near the base of the ventricles, which
its positive end toward the apex. Thus, the first portion
leads II and III are both strongly positive. Plotting these
13–11 the point of origin of the PVC as follows: Note
can determine from the electrocardiogram in Figure
analysis are explained. Applying these principles, one
In Chapter 12, the principles of vectorial
Vector Analysis of the Origin of an Ectopic Premature Ventricular
explained later in the chapter.
the ventricles are coming out of refractoriness, as
causing fibrillation, just at the end of the T wave when
ated by one of the PVCs. This is especially true when
neous lethal ventricular fibrillation, presumably initi-
of such PVCs is not to be taken lightly. Statistics show
infarcted or ischemic areas of the heart. The presence
toxic states, and even emotional irritability. Conversely,
factors as cigarettes, coffee, lack of sleep, various mild
overall pumping by the heart; they can result from such
slow conduction of the
QRS complex, because the
3. After almost all PVCs, the T wave has an electrical
Figure 13–11.
electrical potentials, as shown for the PVCs in
depolarized ahead of the other; this causes large
electrocardiogram. When a PVC occurs, the
heart, the depolarization waves of the two sides
nearly simultaneously; consequently, in the normal
through the heart, it passes through both ventricles
following reasons: when the normal impulse passes
2. The QRS complex has a high voltage for the
prolonged. The reason is that the impulse is
1. The QRS complex is usually considerably
effects in the electrocardiogram, as follows:
ing with normal contractions. PVCs cause specific
The electrocardiogram of Figure 13–11 shows a series
Premature Ventricular Contractions
contractions.
general, A-V nodal premature contractions have
but the P wave itself cannot be discerned as such. In
cles; this P wave slightly distorts the QRS-T complex,
of the premature contraction. Instead, the P wave is
Cardiac Arrhythmias and Their Electrocardiographic Interpretation
Chapter 13
151
superimposed onto the QRS-T complex because the
cardiac impulse traveled backward into the atria at
the same time that it traveled forward into the ventri-
the same significance and causes as atrial premature
of premature ventricular contractions (PVCs) alternat-
conducted mainly through slowly conducting
muscle of the ventricles rather than through the
Purkinje system.
of the heart—mainly of opposite polarity to each
other—partially neutralize each other in the
impulse almost always travels in only one direction,
so that there is no such neutralization effect,
and one entire side or end of the ventricles is
potential polarity exactly opposite to that of the
impulse through the cardiac muscle causes the
muscle fibers that depolarize first also to repolarize
first.
Some PVCs are relatively benign in their effects on
many other PVCs result from stray impulses or re-
entrant signals that originate around the borders of
that people with significant numbers of PVCs have a
much higher than normal chance of developing sponta-
the PVCs occur during the vulnerable period for
Contraction.
that the potentials of the premature contractions in
potentials on the axes of leads II and III and solving by
vectorial analysis for the mean QRS vector in the heart,
one finds that the vector of this premature contraction
has its negative end (origin) at the base of the heart and
of the heart to become depolarized during this prema-
Some abnormalities in different portions of the heart,
of impulses that spread in all directions throughout the
P
P
P
Premature beat
P
P
T
T
T
T
T
A-V nodal premature contraction (lead III).
Figure 13–10
III
II
–
+
+
–
II
II
III
III
premature contractions is plotted in accordance with the princi-
large abnormal QRS-T complexes (leads II and III). Axis of the
Premature ventricular contractions (PVCs) demonstrated by the
Figure 13–11
ples of vectorial analysis explained in Chapter 12; this shows the
origin of the PVC to be near the base of the ventricles.

the heart muscle, of its specialized conducting system,
sudden electrical shock of the heart, or (2) ischemia of
rillation. Especially likely to initiate fibrillation are (1)
one moment, but 1 second later, the ventricles are in fib-
minutes.
flow to the brain, and irretrievable death of tissues
ble amounts. Therefore, after fibrillation begins, uncon-
partial contraction, pumping either no blood or negligi-
the ventricles, the ventricular chambers neither enlarge
required for a pumping cycle of the heart. Despite
tion of all the ventricular muscle at once, which is
be relaxing. Thus, there is never a coordinate contrac-
the same time, while equally as many other portions will
over—never stopping. When this happens, many small
portion, then another, and eventually feeding back onto
first one portion of the ventricular muscle, then another
berserk within the ventricular muscle mass, stimulating
minutes, is almost invariably fatal. Ventricular fibrilla-
which, if not stopped within 1 to 3
The most serious of all cardiac arrhythmias is
Ventricular Fibrillation
cardiac muscle, may be used to block irritable foci
, which increases
lar tachycardia. Conversely,
repeated stimulation of the ventricular muscle, as we
ischemic damage is present in the ventricles. Second,
serious condition for two reasons. First, this type of
Ventricular paroxysmal tachycardia is usually a
tricular tachycardia. The electrocardiogram of ventricu-
Figure 13–13 shows a typical short paroxysm of ven-
Ventricular Paroxysmal Tachycardia
weakness during the paroxysm, but only seldom does
after adolescence. In general, supraventricular tachy-
occurs in young, otherwise healthy people, and they gen-
supraventricular tachycardias,
Atrial or A-V nodal paroxysmal tachycardia, both of
complexes but totally missing or obscured P waves.
A-V node. This usually causes almost normal QRS-T
A-V Nodal Paroxysmal Tachycardia.
not near the sinus node.
because the P wave is abnormal in shape, the origin is
of this paroxysmal tachycardia is in the atrium, but
of the preceding beat. This indicates that the origin
wave is partially superimposed onto the normal T wave
wave is seen before each QRS-T complex, and this P
trocardiogram during the rapid heartbeat, an inverted P
about 150 beats per minute. On close study of the elec-
Figure 13–12 demonstrates in the middle of the record
Atrial Paroxysmal Tachycardia
dine and lidocaine, either of which depresses the normal
may also be used. Two drugs frequently used are quini-
of a vagal reflex to stop the paroxysm. Various drugs
regions of the carotid sinuses, which may cause enough
iting a vagal reflex. A type of vagal reflex sometimes
the sinus node.
paroxysm usually ends as suddenly as it began, with
few minutes, a few hours, or much longer. Then the
beginning suddenly and lasting for a few seconds, a
becomes rapid in paroxysms, with the paroxysm
The term “paroxysmal” means that the heart rate
rapid rhythm in the irritable focus, this focus becomes
up local repeated self–re-excitation. Because of the
152
Unit III
The Heart
re-entrant circus movement feedback pathways that set
the pacemaker of the heart.
the pacemaker of the heart instantly shifting back to
Paroxysmal tachycardia often can be stopped by elic-
elicited for this purpose is to press on the neck in the
increase in sodium permeability of the cardiac muscle
membrane during generation of the action potential,
thereby often blocking the rhythmical discharge of the
focal point that is causing the paroxysmal attack.
a sudden increase in the heart rate from about 95 to
Paroxysmal tachycardia
often results from an aberrant rhythm that involves the
which are called
usually
erally grow out of the predisposition to tachycardia
cardia frightens a person tremendously and may cause
permanent harm come from the attack.
lar paroxysmal tachycardia has the appearance of a
series of ventricular premature beats occurring one
after another without any normal beats interspersed.
tachycardia usually does not occur unless considerable
ventricular tachycardia frequently initiates the lethal
condition of ventricular fibrillation because of rapid
discuss in the next section.
Sometimes intoxication from the heart treatment
drug digitalis causes irritable foci that lead to ventricu-
quinidine
the refractory period and threshold for excitation of
causing ventricular tachycardia.
ventricu-
lar fibrillation,
tion results from cardiac impulses that have gone
itself to re-excite the same ventricular muscle over and
portions of the ventricular muscle will be contracting at
massive movement of stimulatory signals throughout
nor contract but remain in an indeterminate stage of
sciousness occurs within 4 to 5 seconds for lack of blood
begins to occur throughout the body within a few
Multiple factors can spark the beginning of ventricu-
lar fibrillation—a person may have a normal heartbeat
or both.
Atrial paroxysmal tachycardia—onset in middle of record (lead I).
Figure 13–12
Ventricular paroxysmal tachycardia (lead III).
Figure 13–13

muscle begins to come out of the refractory state. Some
in a refractory state. After about 0.25 second, part of this
directions, leaving all the muscle beneath the electrode
stimulating electrode. The first cycle of the electrical
a 60-cycle electrical stimulus is applied through a
central point in the ventricles of heart A in Figure 13–15,
electric shock caused by 60-cycle alternating electric
tion.” One of the best ways to explain this process in
wave fronts that have the appearance of a “chain reac-
Instead, they have degenerated into a series of multiple
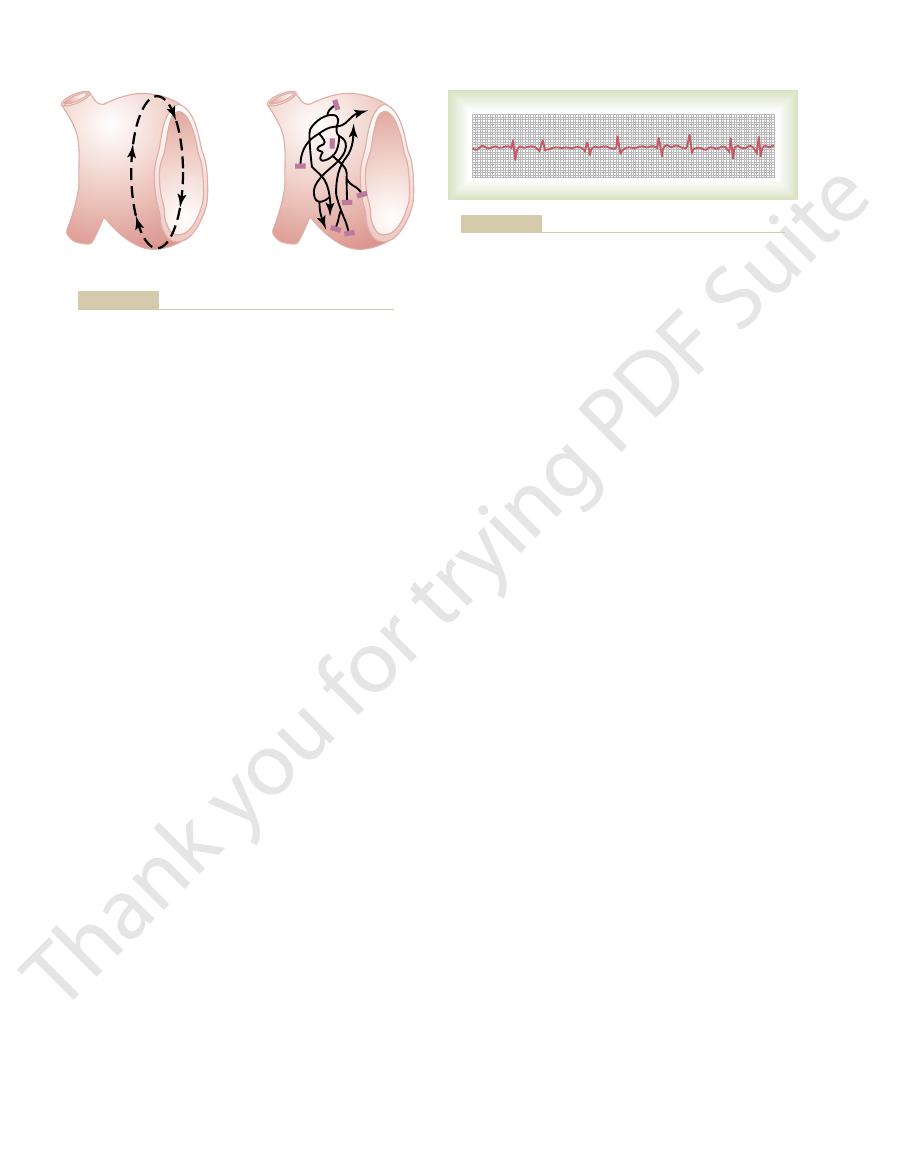
impulse moving in a circle, as shown in Figure 13–14.
different directions over the cardiac muscle. The re-
In ventricular fibrillation, one sees many separate and
ignore the pace-setting effects of the sinus node.
disturbances, re-entry can cause abnormal patterns of
repetitive electrical stimulation. Thus, in many cardiac
response to various drugs, such as epinephrine, or after
blood potassium levels, or (d) many other factors. (3)
Purkinje system, (b) ischemia of the muscle, (c) high
typically occurs in dilated hearts. (2) Decreased rate of
states of the human heart, as follows: (1) A long pathway
also continue around and around the circle.
In this case, the impulse could
Third,
the refractory state, and the impulse can continue
time, the originally stimulated muscle might be out of
the impulse returns to the 12 o’clock position. By this
enough, an increased interval of time will elapse before
Second, if the length of the pathway remains constant
pathway around the circle is too long,
First, if the
movement.”
has already been excited. This is called a “circus
to cause “re-entry” of the impulse into muscle that
impulse to continue to travel around the circle, that is,
refractory muscle cannot transmit a second impulse. But
a refractory state, the impulse then dies out because
tion. If the originally stimulated muscle fibers are still in
strips cut in the form of circles. If such a strip is stimu-
Figure 13–14 shows several small cardiac muscle
initiate re-entry and lead to “circus movements,” which
sequence of events does not occur. Therefore, let us
Under some circumstances, however, this normal
action potential to begin in the atrial sinus node.
Therefore, that impulse dies, and the heart awaits a new
refractory and cannot conduct the impulse farther.
has traveled through the extent of the ventricles, it has
When the
Ventricular Fibrillation
Cardiac Arrhythmias and Their Electrocardiographic Interpretation
Chapter 13
153
Phenomenon of Re-entry—“Circus
Movements” as the Basis for
normal cardiac impulse in the normal heart
no place to go because all the ventricular muscle is
explain more fully the background conditions that can
in turn cause ventricular fibrillation.
lated at the 12 o’clock position so that the impulse travels
in only one direction, the impulse spreads progressively
around the circle until it returns to the 12 o’clock posi-
there are three different conditions that can cause this
by
the time the impulse returns to the 12 o’clock position,
the originally stimulated muscle will no longer be
refractory and the impulse will continue around the
circle again and again.
but the velocity of conduction becomes decreased
around the circle again and again.
the refractory period of the muscle might
become greatly shortened.
All these conditions occur in different pathological
conduction frequently results from (a) blockage of the
A shortened refractory period commonly occurs in
cardiac contraction or abnormal cardiac rhythms that
Chain Reaction Mechanism
of Fibrillation
small contractile waves spreading at the same time in
entrant impulses in fibrillation are not simply a single
fibrillation is to describe the initiation of fibrillation by
current.
Fibrillation Caused by 60-Cycle Alternating Current.
At a
stimulus causes a depolarization wave to spread in all
portions come out of refractoriness before other
Absolutely
refractory
Absolutely
refractory
Relatively
refractory
LONG PATHWAY
NORMAL PATHWAY
pathway.
pathway and continued propagation of the impulse in the long
Circus movement, showing annihilation of the impulse in the short
Figure 13–14
Stimulus
point
Dividing
impulses
Blocked
impulse
A
B
fibrillatory
Continued propagation of
culature are present.
Initiation of fibrillation in a heart when patches of refractory mus-
Figure 13–15
A,
B,
impulses in the fibrillating ventricle.
volts of 60-cycle alternating current applied for 0.1
of the heart, fibrillation can usually be stopped using 110
When electrodes are applied directly to the two sides
may begin again immediately.
rillation often is still present, in which case fibrillation
becoming the pacemaker. However, the same re-entrant
5 seconds, after which it begins to beat again, usually
potentials stop, and the heart remains quiescent for 3 to
and causing them all to become refractory. All action
fibers of the ventricles at the same time, thus stimulat-
sides of the heart. The current penetrates most of the
ness simultaneously. This is accomplished by passing
throws the ventricles into fibrillation, a strong high-
of the Ventricles
electroshock through the heart, as explained in the next
stopped by some heroic therapy, such as immediate
during ventricular fibrillation, this state is lethal unless
pointed out, because no pumping of blood occurs
longer after ventricular fibrillation begins. As already
are usually only 0.2 to 0.3 millivolt. Minute voltages of
decay rapidly so that after 20 to 30 seconds, they
when ventricular fibrillation first begins, but they
The voltages of the waves in the electrocardiogram
any specific cycle.
small patches of muscle at a time, and electrocardio-
tern can be ascribed to ventricular fibrillation. Instead,
lar waves. Thus, no repetitive electrocardiographic pat-
changes into a new pattern of low-voltage, very irregu-
the ventricles disappear, and the electrocardiogram
After another few seconds, the coarse contractions of
causes coarse, irregular waves in the electrocardiogram.
large masses of muscle contract simultaneously, and this
first few seconds of ventricular fibrillation, relatively
dency toward a regular rhythm of any type. During the
bizarre (Figure 13–16) and ordinarily shows no ten-
In ventricular fibrillation, the electrocardiogram is
Electrocardiogram in Ventricular
ally around refractory areas of muscle, which will lead
blocked by refractory areas. In fact, a single electric
increasing the number of impulses, whereas others are
impulses traveling in all directions, some dividing and
that develops in fibrillation. Here one can see many
Heart B in Figure 13–15 demonstrates the final state
muscle comes out of refractoriness, an impulse is close
the impulses. Therefore, any time a single area of cardiac
cause more and more patches of refractory muscle, and
initiated: More and more impulses are formed; these
travel, greatly lengthening the conductive pathway, which
time. Furthermore, this irregular pattern of impulse
until, finally, there are many small depolariza-
chain
impulses. In this way, many new wave fronts are contin-
refractory area, it, too, divides to form two more
impulses. Then, when each of these reaches another
refractory area. Thus, a single impulse becomes two
area in the heart, it travels to both sides around the
A. When a depolarization wave reaches a refractory
division of impulses,
Third, one of the most important features of fibrilla-
than normally.
the heart. (2) The
tion through the heart muscle decreases,
dispose to circus movement: (1) The
changes in the cardiac muscle itself, both of which pre-
Second, the rapid stimulation of the heart causes two
but not other directions.
develop—that is,
First, block of the impulses in some directions but suc-
areas. Then, several events transpire in rapid succession,
then are blocked. But other impulses pass between the
tances, until they reach refractory areas of the heart, and
Thus, in heart A, certain impulses travel for short dis-
directions through the heart but not in all directions.
tory muscle. Now, continuing 60-cycle stimuli from the
muscle, and dark patches, which represent still refrac-
many lighter patches, which represent excitable cardiac
portions. This state of events is depicted in heart A by
154
Unit III
The Heart
electrode can cause impulses to travel only in certain
refractory areas and continue to travel in the excitable
all occurring simultaneously and eventuating in a state
of fibrillation.
cessful transmission in other directions creates one of
the necessary conditions for a re-entrant signal to
transmission of some of the depolar-
ization waves around the heart in only some directions
velocity of conduc-
which allows a
longer time interval for the impulses to travel around
refractory period of the muscle is
shortened, allowing re-entry of the impulse into previ-
ously excited heart muscle within a much shorter time
tion is the
as demonstrated in heart
ually being formed in the heart by progressive
reactions
tion waves traveling in many directions at the same
travel causes many circuitous routes for the impulses to
is one of the conditions that sustains the fibrillation. It
also results in a continual irregular pattern of patchy
refractory areas in the heart.
One can readily see when a vicious circle has been
the refractory patches cause more and more division of
at hand to re-enter the area.
shock during this vulnerable period frequently can lead
to an odd pattern of impulses spreading multidirection-
to fibrillation.
Fibrillation
the ventricular muscle contracts at as many as 30 to 50
graphic potentials change constantly and spasmodically
because the electrical currents in the heart flow first in
one direction and then in another and seldom repeat
in ventricular fibrillation are usually about 0.5 millivolt
0.1 millivolt or less may be recorded for 10 minutes or
section.
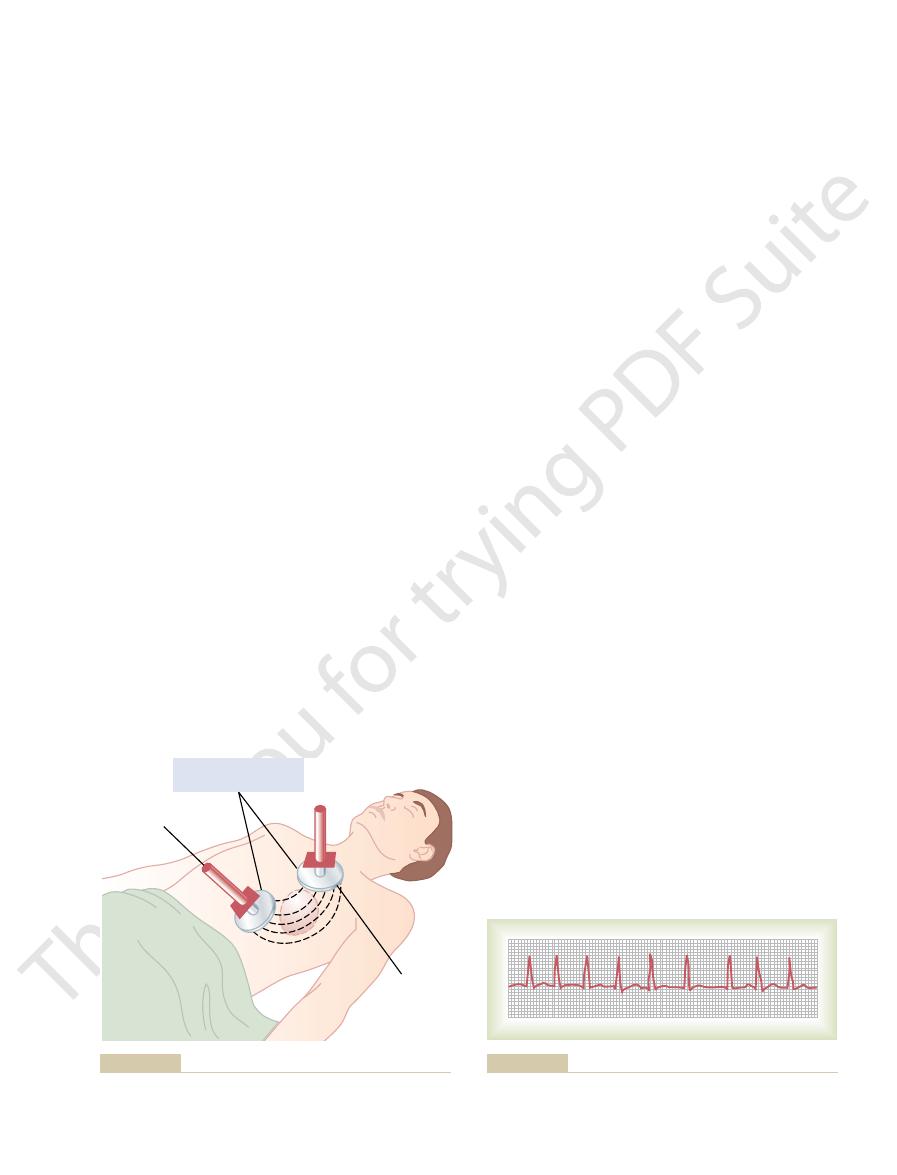
Electroshock Defibrillation
Although a moderate alternating-current voltage
applied directly to the ventricles almost invariably
voltage alternating electrical current passed through the
ventricles for a fraction of a second can stop fibrillation
by throwing all the ventricular muscle into refractori-
intense current through large electrodes placed on two
ing essentially all parts of the ventricles simultaneously
with the sinus node or some other part of the heart
focus that had originally thrown the ventricles into fib-
Ventricular fibrillation (lead II).
Figure 13–16
contraction and the next. Then an additional but
impulse for about 0.35 second after a previous one, at
larly. Because the A-V node will not pass a second
atrial muscle at the A-V node rapidly but also irregu-
When the atria are fibrillating, impulses arrive from the
Irregularity of Ventricular Rhythm During Atrial Fibrillation.
tricles, but their timing is irregular, as explained next.
voltage wavy record. Conversely, the QRS-T complexes
from the atria or only a fine, high-frequency, very low
the electrocardiogram, one can see either no P waves
pletely electrically neutralize one another. Therefore, in
polarity at any given time, they usually almost com-
through the atria during atrial fibrillation. Because the
the electrocardiogram during atrial fibrillation. Numer-
Figure 13–18 shows
although at reduced efficiency of overall heart pumping.
to the lethality of ventricular fibrillation, a person can
decreased only 20 to 30 per cent. Therefore, in contrast
ventricles, and the efficiency of ventricular pumping is
so, blood flows passively through the atria into the
become useless as primer pumps for the ventricles. Even
pump blood in atrial fibrillation. Therefore, the atria
blood during ventricular fibrillation, neither do the atria
For the same reasons that the ventricles will not pump
as well as slow conduction, both of which predispose to
damming of blood in the atria. The dilated atrial walls
ventricles, or from ventricular failure with excess
mass. A frequent cause of atrial fibrillation is atrial
of ventricular fibrillation, except that the process occurs
The mechanism of atrial fibrillation is identical to that
(shown to the right in Figure 13–19).
without atrial fibrillation. Likewise, fibrillation often
tissue. Therefore, ventricular fibrillation often occurs
through the A-V bundle, the atrial muscle mass is
heart is revived, the person may die from the effects of
ment or even destruction of brain tissue. Even if the
8 minutes usually causes permanent mental impair-
cardiopulmonary resuscitation,
defibrillation, is called
the chest wall along with artificial respiration. This, plus
ble. Indeed, fibrillating hearts have been pumped by
pumping, electrical defibrillation often becomes possi-
supply develops. Then, after a few minutes of hand
the heart later. In this way, small quantities of blood are
nary blood flow. However, it is still possible to revive the
begins, the heart is usually too weak to be revived by
an Aid to Defibrillation
Hand Pumping of the Heart
dog was defibrillated 130 times through the chest wall,
In our laboratory, the heart of a single anesthetized
electrodes on the chest wall, as shown in Figure 13–17,
thousandths of a second. When applied through two
Cardiac Arrhythmias and Their Electrocardiographic Interpretation
Chapter 13
155
second or 1000 volts of direct current applied for a few
the usual procedure is to charge a large electrical
capacitor up to several thousand volts and then to cause
the capacitor to discharge for a few thousandths of a
second through the electrodes and through the heart.
and the animal lived thereafter in perfectly normal
condition.
(Cardiopulmonary Resuscitation) as
Unless defibrillated within 1 minute after fibrillation
defibrillation because of the lack of nutrition from coro-
heart by preliminarily pumping the heart by hand
(intermittent hand squeezing) and then defibrillating
delivered into the aorta and a renewed coronary blood
hand for as long as 90 minutes followed by successful
defibrillation.
A technique for pumping the heart without opening
the chest consists of intermittent thrusts of pressure on
or CPR.
Lack of blood flow to the brain for more than 5 to
brain damage or may live with permanent mental
impairment.
Atrial Fibrillation
Remember that except for the conducting pathway
separated from the ventricular muscle mass by fibrous
occurs in the atria without ventricular fibrillation
only in the atrial muscle mass instead of the ventricular
enlargement resulting from heart valve lesions that
prevent the atria from emptying adequately into the
provide ideal conditions of a long conductive pathway
atrial fibrillation.
Pumping Characteristics of the Atria During Atrial Fibrillation.
live for months or even years with atrial fibrillation,
Electrocardiogram in Atrial Fibrillation.
ous small depolarization waves spread in all directions
waves are weak and many of them are of opposite
are normal unless there is some pathology of the ven-
least 0.35 second must elapse between one ventricular
Several thousand volts
for a few milliseconds
Handle for
application
of pressure
Electrode
Application of electrical current to the chest to stop ventricular
Figure 13–17
fibrillation.
Atrial fibrillation (lead I). The waves that can be seen are ventric-
Figure 13–18
ular QRS and T waves.
349:465, 2003.
electrocardiographic exercise testing. N Engl J Med
Greenland P, Gaziano JM: Clinical practice: selecting asymp-
90:570, 2004.
in a patient with hypertrophic cardiomyopathy. Heart
Frenneaux MP: Assessing the risk of sudden cardiac death
Falk RH: Atrial fibrillation. N Engl J Med 344:1067, 2001.
Circulation 108:1263, 2003.
Cohn PF, Fox KM, Daly C: Silent myocardial ischemia.
J Am Soc Echocardiogr 16:1091, 2003.
lines for the Clinical Application of Echocardiography).
(ACC/AHA/ASE Committee to Update the 1997 Guide-
Heart Association Task Force on Practice Guidelines
report of the American College of Cardiology/American
application of echocardiography: summary article. A
ACC/AHA/ASE 2003 Guideline update for the clinical
Cheitlin MD, Armstrong WF, Aurigemma GP, et al:
modality? Clin Cardiol 8:390, 2003.
phy after acute coronary syndromes: still the first testing
Bigi R, Cortigiani L, Desideri A: Exercise electrocardiogra-
J Am Coll Cardiol 40:207, 2002.
logical basis and clinical application of T-wave alternans.
Armoundas AA, Tomaselli GF, Esperer HD: Pathophysio-
289:2120, 2003.
clinicians should know about the QT interval. JAMA
Al-Khatib SM, LaPointe NM, Kramer JM, Califf RM: What
to years.
implanted electronic cardiac pacemaker
To treat the condition, rhythmical electrical impulses
semipermanent cardiac arrest, which can cause death.
establishing a normal heart rhythm. In some patients,
affected that the automatic rhythmicity disappears.
across their membranes, and their excitability may be so
because of inadequate respiration. The hypoxia pre-
That is, no spontaneous rhythm remains.
This results from
cardiac arrest.
Cardiac Arrest
the atria, giving a 2:1 or 3:1 rhythm.
traction of semicoordinate masses of muscle. However,
atrial flutter. The P waves are strong because of con-
Figure 13–20 shows a typical electrocardiogram in
every single beat of the ventricles.
fore, there are usually two to three beats of the atria for
to pass more than a fraction of the atrial signals. There-
periods of the A-V node and A-V bundle are too long
passed into the ventricles, because the refractory
reach the A-V node too rapidly for all of them to be
pumped by the atria is slight. Furthermore, the signals
while the other side is relaxing, the amount of blood
However, because one side of the atria is contracting
the atria, usually between 200 and 350 beats per minute.
13–19. Atrial flutter causes a rapid rate of contraction of
the atrial muscle mass, as shown to the left in Figure
lation, in that the electrical signal travels as a single
movement in the atria. It is different from atrial fibril-
if the heart is capable of this.
into refractoriness for a few seconds; a normal rhythm
shock through the heart, which throws the entire heart
atrial fibrillation be converted by electroshock. The pro-
back to a normal rhythm by electroshock, so too can
Electroshock Treatment of Atrial Fibrillation.
minute.
heart rate, usually between 125 and 150 beats per
impulses in the atria, the ventricle is driven at a fast
tion. Also, because of the rapid rate of the fibrillatory
heartbeats in the electrocardiogram of Figure 13–18, is
irregularity, demonstrated by the variable spacing of the
second, causing a very irregular heartbeat. In fact, this
arrive at the A-V node. Thus, the interval between suc-
156
Unit III
The Heart
variable interval of 0 to 0.6 second occurs before one of
the irregular atrial fibrillatory impulses happens to
cessive ventricular contractions varies from a minimum
of about 0.35 second to a maximum of about 0.95
one of the clinical findings used to diagnose the condi-
In the same
manner that ventricular fibrillation can be converted
cedure is essentially the same as for ventricular fibrilla-
tion conversion—passage of a single strong electric
often follows
Atrial Flutter
Atrial flutter is another condition caused by a circus
large wave always in one direction around and around
note in the record that a QRS-T complex follows an
atrial P wave only once for every two to three beats of
A final serious abnormality of the cardiac rhythmicity-
conduction system is
cessation of all electrical control signals in the heart.
Cardiac arrest is especially likely to occur during deep
anesthesia, when many patients develop severe hypoxia
vents the muscle fibers and conductive fibers from main-
taining normal electrolyte concentration differentials
In most instances of cardiac arrest from anesthesia,
prolonged cardiopulmonary resuscitation (many
minutes or even hours) is quite successful in re-
severe myocardial disease can cause permanent or
from an
have
been used successfully to keep patients alive for months
References
tomatic patients for coronary computed tomography or
Atrial flutter
Atrial fibrillation
Figure 13–19
Pathways of impulses in atrial flutter and atrial fibrillation.
Figure 13–20
Atrial flutter—2:1 and 3:1 atrial to ventricle rhythm (lead I).
Philadelphia: WB Saunders, 1999.
Zipes DP, Jalife J: Cardiac Electrophysiology, 3rd ed.
in acute myocardial infarction. N Engl J Med 348:933,
Zimetbaum PJ, Josephson ME: Use of the electrocardiogram
basis and clinical significance. J Am Coll Cardiol 42:401,
ization components on the electrocardiogram: cellular
Yan GX, Lankipalli RS, Burke JF, et al: Ventricular repolar-
J Med 349:2128, 2003.
conditions other than acute myocardial infarction. N Engl
Wang K, Asinger RW, Marriott HJ: ST-segment elevation in
dromes. J Am Coll Cardiol 41(4 Suppl S):S123, 2003.
with non-ST-segment elevation acute coronary syn-
Topol EJ: A guide to therapeutic decision-making in patients
trophy. J Mol Med 81:336, 2003.
Swynghedauw B, Baillard C, Milliez P: The long QT interval
N Engl J Med 350:1013, 2004.
Roden DM: Drug-induced prolongation of the QT interval.
Nature 415:219, 2002.
Nattel S: New ideas about atrial fibrillation 50 years on.
349:1064, 2003.
Maron BJ: Sudden death in young athletes. N Engl J Med
channels in vasospastic angina. J Clin Invest 110:153,
Marban E: The surprising role of vascular K(ATP)
rent therapeutic strategies. Am Heart J 141(2 Suppl):S15,
Levy S: Pharmacologic management of atrial fibrillation: cur-
prognosis? Am J Med 115:732, 2003.
Lehmann MH, Morady F: QT interval: metric for cardiac
344:1840, 2001.
patients with stable coronary artery disease. N Engl J Med
Lee TH, Boucher CA: Clinical practice: noninvasive tests in
maintenance. Annu Rev Physiol 62:25, 2000.
Jalife J: Ventricular fibrillation: mechanisms of initiation and
process. Am J Cardiol 92:1072, 2003.
Hurst JW: Current status of clinical electrocardiography with
Cardiac Arrhythmias and Their Electrocardiographic Interpretation
Chapter 13
157
suggestions for the improvement of the interpretive
2001.
2002.
is not only inherited but is also linked to cardiac hyper-
2003.
2003.
