In hemodynamic studies, it usually is much more important to know the
Vascular Compliance (or Vascular Capacitance)
tensibility of systemic arteries.
and their distensibilities are correspondingly greater, about six times the dis-
to those of the systemic circulation. But, the pulmonary arteries normally
In the pulmonary circulation, the pulmonary vein distensibilities are similar
in a vein as in an artery of comparable size.
ies, on average, are about eight times less distensible than the veins. That is, a
of the arteries are far stronger than those of the veins. Consequently, the arter-
Anatomically, the walls
Difference in Distensibility of the Arteries and the Veins.
mm Hg, or 10 per cent per mm Hg.
blood to increase its volume by 1 milliliter, the distensibility would be 0.1 per
That is, if 1 mm Hg causes a vessel that originally contained 10 millimeters of
fractional increase in volume for each millimeter of mercury rise in pressure, in
Vascular distensibility normally is expressed as the
Units of Vascular Distensibility.
blood. Therefore, the veins provide a
The most distensible by far of all the vessels are the veins. Even slight
of the tissues.
provides smooth, continuous flow of blood through the very small blood vessels
the pulsatile output of the heart and to average out the pressure pulsations. This
For example, the distensible nature of the arteries allows them to accommodate
Vascular distensibility also plays other important roles in circulatory function.
because of increased pressure but also because of decreased resistance, usually
ance. The result is increased blood flow not only
sure in blood vessels is increased, this dilates the
one example of this in Chapter 14: When the pres-
. We have seen
Vascular Distensibility
Venous Systems
Functions of the Arterial and
Vascular Distensibility and
C
H
A
P
T
E
R
1
5
171
A valuable characteristic of the vascular system is
that all blood vessels are distensible
blood vessels and therefore decreases their resist-
giving at least twice as much flow increase for each increase in pressure as one
might expect.
increases in venous pressure cause the veins to store 0.5 to 1.0 liter of extra
reservoir function for storing large quan-
tities of extra blood that can be called into use whenever required elsewhere in
the circulation.
accordance with the following formula:
given increase in pressure causes about eight times as much increase in blood
operate under pressures about one sixth of those in the systemic arterial system,
total
quantity of blood that can be stored in a given portion of the circulation for
each millimeter of mercury pressure rise than to know the distensibilities of the
Increase in pressure
Original volume
Vascular distensibility
Increase in volume
=
¥
liters of blood, the pressure falls to zero.
100 mm Hg, but when it is
milliliters of blood, the mean arterial pressure is
small arteries, and arterioles) is
average adult person (including all the large arteries,
system, showing that when the arterial system of the
represent, respectively, the volume-pressure curves
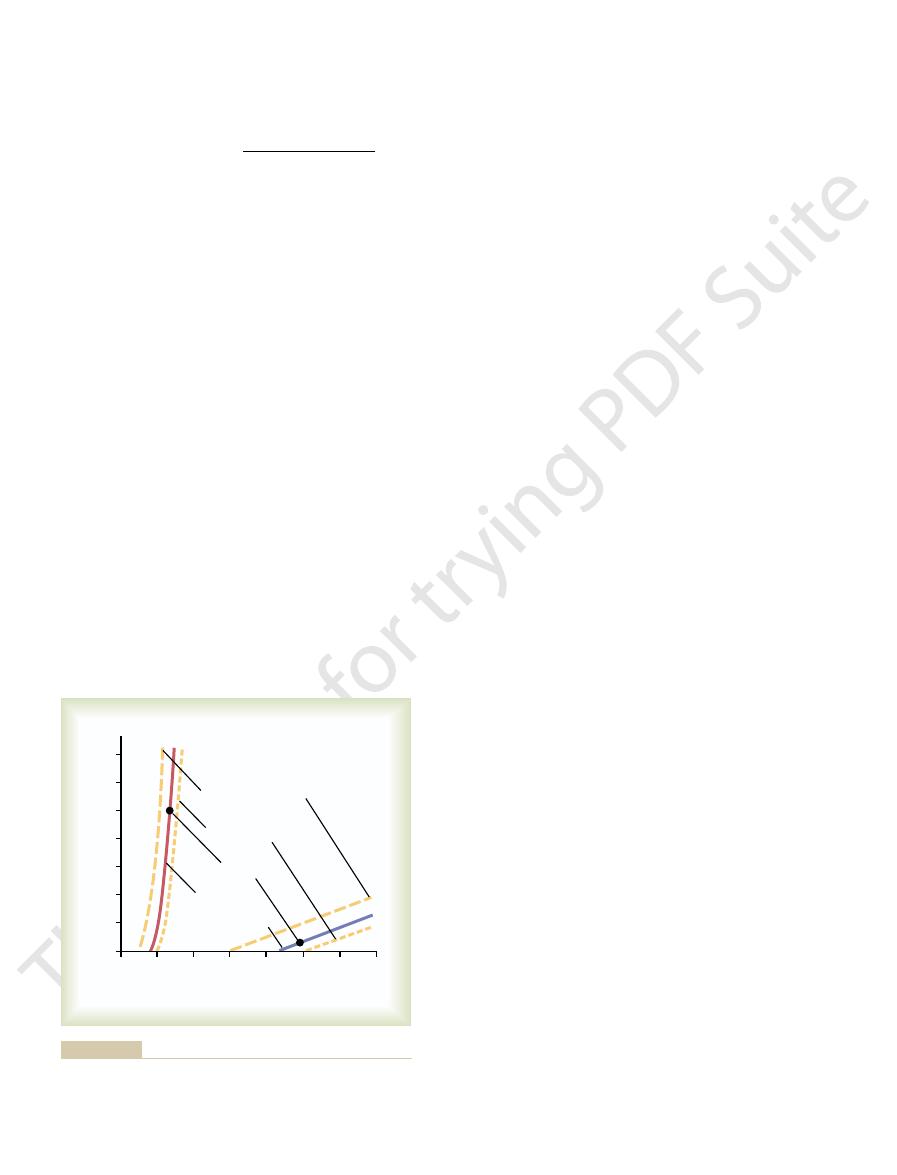
The red and blue solid curves in Figure 15
curve.
Arterial and Venous Circulations
Volume-Pressure Curves of the
The compliance of a systemic vein is about 24 times
equal to distensibility times volume.
Compliance and distensibility are quite different. A
of the respective vascular bed; that is,
individual vessels. This value is called the
172
Unit IV
The Circulation
compliance
or capacitance
highly distensible vessel that has a slight volume may
have far less compliance than a much less distensible
vessel that has a large volume because compliance is
that of its corresponding artery because it is about 8
times as distensible and it has a volume about 3 times
as great (8
¥ 3 = 24).
A convenient method for expressing the relation of
pressure to volume in a vessel or in any portion of the
circulation is to use the so-called volume-pressure
–1
of the normal systemic arterial system and venous
filled with about 700
filled with only 400 milli-
Vascular compliance
Increase in volume
Increase in pressure
=
ished blood volume after serious hemorrhage.
sion. Delayed compliance in the reverse direction is one
blood when necessary, such as after too large a transfu-
spondingly decrease. This effect is a characteristic of all
to longer lengths, and their tensions corre-
vein, but then the smooth muscle
after several minutes. In other words, the volume of
decrease immediately and approaches about 9 mm Hg
removed after it is injected, the pressure begins to
5 to 12 mm Hg. Even though none of the blood is
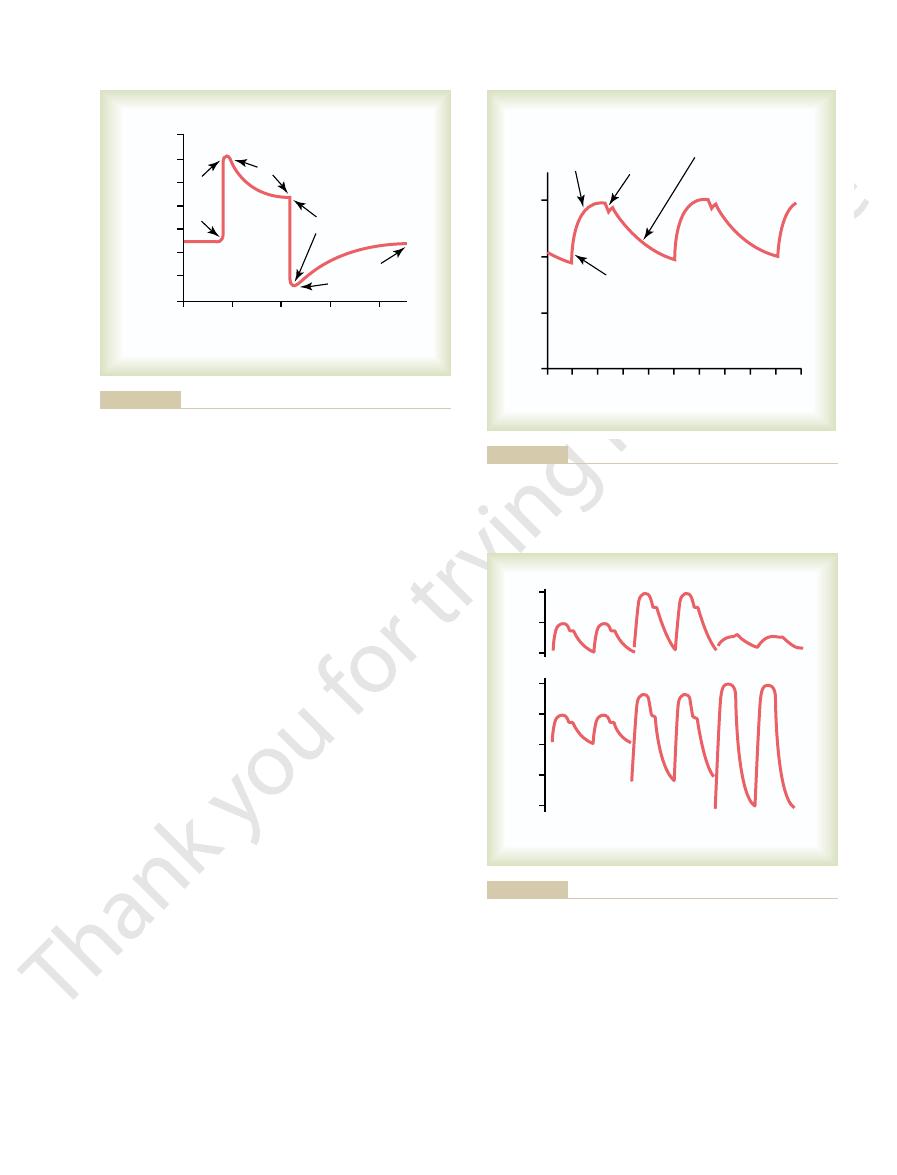
vein that is occluded at both ends. An extra volume of
gure, the pressure is recorded in a small segment of a
2. In this
to hours. This effect is shown in Figure 15
increase in pressure, but progressive delayed stretching
The term
(Stress-Relaxation) of Vessels
sympathetic tone, especially to the veins, reduces the
highly important during hemorrhage. Enhancement of
that the body uses to increase heart pumping.
into the heart, which is one of the principal methods
transferring blood to other segments. For instance, an
dimensions of one segment of the circulation, thus
inhibition decreases the pressure at each volume.
volume of the arteries or veins, whereas sympathetic
has on the volume-pressure curves. It is evident that
Also shown in Figure 15
the Volume-Pressure Relations of the Arterial and Venous
5 mm Hg. This mainly explains why as much as one
normally ranges from 2000 to 3500 milliliters, and a
In the entire systemic venous system, the volume
change of several hundred millimeters in this volume
is required to change the venous pressure only 3 to
half liter of blood can be transfused into a healthy
person in only a few minutes without greatly altering
function of the circulation.
Effect of Sympathetic Stimulation or Sympathetic Inhibition on
Systems.
–1 are the effects that
exciting or inhibiting the vascular sympathetic nerves
increase in vascular smooth muscle tone caused by
sympathetic stimulation increases the pressure at each
Control of the vessels in this manner by the sympa-
thetics is a valuable means for diminishing the
increase in vascular tone throughout the systemic cir-
culation often causes large volumes of blood to shift
Sympathetic control of vascular capacitance is also
vessel sizes enough that the circulation continues to
operate almost normally even when as much as 25 per
cent of the total blood volume has been lost.
Delayed Compliance
“delayed compliance” means that a vessel
exposed to increased volume at first exhibits a large
of smooth muscle in the vessel wall allows the pressure
to return back toward normal over a period of minutes
–
fi
blood is suddenly injected until the pressure rises from
blood injected causes immediate elastic distention of the
fibers of the vein begin
to “creep”
smooth muscle tissue and is called stress-relaxation,
which was explained in Chapter 8.
Delayed compliance is a valuable mechanism by
which the circulation can accommodate much extra
of the ways in which the circulation automatically
adjusts itself over a period of minutes or hours to dimin-
500
1000 1500 2000 2500 3000 3500
Pressure (mm Hg)
0
0
20
40
60
80
100
120
140
Volume (ml)
Sympathetic stimulation
Sympathetic inhibition
Arterial system
Venous system
Normal volume
pathetic nerves to the circulatory system.
systems, showing the effects of stimulation or inhibition of the sym-
Volume-pressure curves” of the systemic arterial and venous
Figure 15–1
“
affects the pulse pressure.
. Any condition of the cir-
In effect, then, pulse pressure is determined ap-
rises to as much as twice normal, because the arteries
4, the pulse pressure in old age sometimes
Figure 15
instance, as demonstrated by the middle top curves in
stroke volume of blood pumped into the arteries. For
rial system, the greater the rise in pressure for a given
sure. Conversely, the less the compliance of the arte-
systole and diastole, thus causing a greater pulse pres-
therefore, the greater the pressure rise and fall during
dated in the arterial tree with each heartbeat, and,
In general, the greater the stroke volume output, the
the heart during systole.
of the arterial tree. A third,
Two major factors affect the pulse pressure: (1) the
pulse pressure.
these two pressures, about 40 mm Hg, is called the
it is about 80 mm Hg. The difference between
pressure,
At the lowest point of each pulse, called the
is about 120 mm Hg.
systolic pressure,
pulse, called the
healthy young adult, the pressure at the top of each
3. In the
root of the aorta is shown in Figure 15
reaches the capillaries; therefore, tissue blood
occur during diastole. However, normally the compli-
neously, only during cardiac systole, and no
rial system, all of this new blood would have to
the arteries. Were it not for distensibility of the arte-
With each beat of the heart a new surge of blood
Arterial Pressure Pulsations
Vascular Distensibility and Functions of the Arterial and Venous Systems
Chapter 15
173
fills
flow
through the peripheral blood vessels almost instanta-
flow would
ance of the arterial tree reduces the pressure pulsa-
tions to almost no pulsations by the time the blood
flow is
mainly continuous with very little pulsation.
A typical record of the pressure pulsations at the
–
diastolic
stroke volume output of the heart and (2) the compli-
ance (total distensibility)
less important factor is the character of ejection from
greater the amount of blood that must be accommo-
–
have become hardened with arteriosclerosis and there-
fore are relatively noncompliant.
proximately by the ratio of stroke volume output to
compliance of the arterial tree
culation that affects either of these two factors also
20
80
Pressure (mm Hg)
0
0
12
10
8
6
4
2
14
60
40
Minutes
Increased
volume
Decreased
volume
Delayed
compliance
Delayed
compliance
into a venous segment and later removing the excess blood,
Effect on the intravascular pressure of injecting a volume of blood
Figure 15–2
demonstrating the principle of delayed compliance.
– 80
– 80
– 80
+20
0
0.2 0.4 0.6 0.8 1.0 1.2 1.4 1.6 1.8 2.0
Pressure (mm Hg)
Seconds
Slow rise
to peak
Sharp
incisura
Exponential diastolic decline
(may be distorted by
reflected wave)
Sharp
upstroke
(Redrawn from Opdyke DF: Fed Proc 11:734, 1952.)
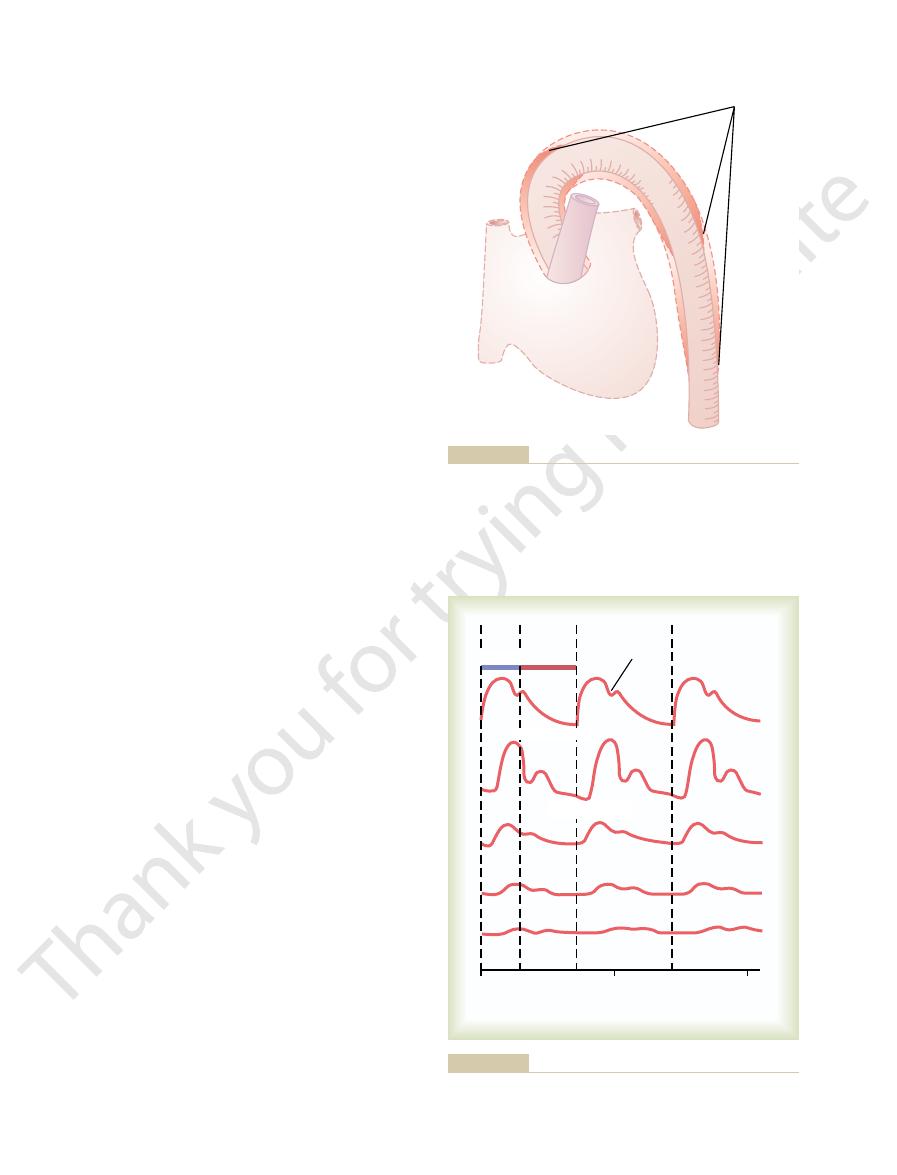
Pressure pulse contour recorded from the ascending aorta.
Figure 15–3
Arteriosclerosis Aortic stenosis
160
120
80
160
120
80
40
0
Normal
Normal
Patent ductus
arteriosus
Aortic
regurgitation
patent ductus arteriosus, and aortic regurgitation.
Aortic pressure pulse contours in arteriosclerosis, aortic stenosis,
Figure 15–4
observed in the capillaries.
the arterioles, and, especially, the capillaries. In fact,
becomes progressively less in the smaller arteries,
travels into the peripheral vessels. Note especially in
Figure 15
Damping of the Pressure Pulses in the Smaller Arteries, Arteri-
forward total movement of blood volume.
small distal arteries. In the aorta, the velocity of trans-
each vascular segment, the slower the velocity, which
35 m/sec. In general, the greater the compliance of
branches, 7 to 10 m/sec; and in the small arteries, 15 to
normal aorta is 3 to 5 m/sec; in the large arterial
The velocity of pressure pulse transmission in the
in the arteries.
5. This is called
the aorta, as shown in Figure 15
mal aorta rapidly overcomes this inertia, and the wave
periphery. However, the rising pressure in the proxi-
systole, at
When the heart ejects blood into the aorta during
to the Peripheral Arteries
Transmission of Pressure Pulses
valve to close.
to zero between heartbeats. Also, there is no incisura
cle. As a result, the aortic pressure can fall all the way
beat, the blood that has just been pumped into the
will not close completely. Therefore, after each heart-
, the aortic valve is absent or
into the pulmonary artery and lung blood vessels, thus
, one half or more of the
ow outward through the stenotic valve.
cantly, and the aortic pres-
, the diameter of the aortic valve
Figure 15
sus, and aortic regurgitation, each of which is shown in
among these are aortic stenosis, patent ductus arterio-
to altering the pulse pressure. Especially distinctive
Abnormal Pressure Pulse Contours
174
Unit IV
The Circulation
Some conditions of the circulation also cause abnor-
mal contours of the pressure pulse wave in addition
–4.
In aortic stenosis
opening is reduced signifi
sure pulse is decreased significantly because of dimin-
ished blood fl
In patent ductus arteriosus
blood pumped into the aorta by the left ventricle flows
immediately backward through the wide-open ductus
allowing the diastolic pressure to fall very low before
the next heartbeat.
In aortic regurgitation
aorta flows immediately backward into the left ventri-
in the aortic pulse contour because there is no aortic
first only the proximal portion of the aorta
becomes distended because the inertia of the blood
prevents sudden blood movement all the way to the
front of distention spreads farther and farther along
–
trans-
mission of the pressure pulse
explains the slow transmission in the aorta and the
much faster transmission in the much less compliant
mission of the pressure pulse is 15 or more times the
velocity of blood flow because the pressure pulse is
simply a moving wave of pressure that involves little
oles, and Capillaries.
–6 shows typical changes
in the contours of the pressure pulse as the pulse
the three lower curves that the intensity of pulsation
only when the aortic pulsations are extremely large or
the arterioles are greatly dilated can pulsations be
Wave fronts
aorta.
Progressive stages in transmission of the pressure pulse along the
Figure 15–5
0
1
2
Time (seconds)
Incisura
Radial artery
Arteriole
Capillary
Diastole
Proximal aorta
Femoral artery
Systole
toward the smaller vessels.
Changes in the pulse pressure contour as the pulse wave travels
Figure 15–6
The mean arterial pressure is the
pressure, as previously explained.
. The
hardening of the arteries, which itself is an end-stage
occurs beyond the age of 60 years. This results from
age, especially after the age of 50 years.
term regulation of arterial pressure; and it is well
control mechanisms. We shall see in Chapter 19 that
ages. The progressive increase in pressure with age
Figure 15
Normal Arterial Pressures as Measured by the Auscultatory
inside the arteries.
systolic and diastolic pressures is not entirely accurate,
pressure. The auscultatory method for determining
quality; this pressure is about equal to the diastolic
when the Korotkoff sounds change to the muf
in cuff pressure. One notes the manometer pressure
ed quality, then dis-
squeezed artery) is no longer present. Therefore, the
during diastole, which means that the basic factor
to equal diastolic pressure, the artery no longer closes
nally, when the pressure in the cuff falls
quality. Then,
Korotkoff sounds change in quality, having less of the
As the pressure in the cuff is lowered still more, the
about equal to the systolic pressure.
as these sounds begin to be heard, the pressure level
cubital artery in synchrony with the heartbeat. As soon
beneath the cuff during the peak of systolic pressure,
tolic pressure, blood begins to slip through the artery
Just as soon as the pressure in the cuff falls below sys-
artery. But then the cuff pressure gradually is reduced.
Therefore, no Korotkoff sounds are heard in the lower
lower artery during any part of the pressure cycle.
pressure is higher than systolic pressure, the brachial
above arterial systolic pressure. As long as this cuff
method, the pressure in the cuff is
stethoscope.
The jet causes turbulence in the vessel beyond the cuff,
debated, but they are believed to be caused mainly
The exact cause of Korotkoff sounds is still
Korotkoff sounds
pulsation. These sounds are called
arterial pressure cycle, a sound then is heard with each
with the stethoscope. However, when the cuff pressure
artery, no sounds are heard from the antecubital artery
upper arm. As long as the cuff continues to compress
pressures. A stethoscope is placed over the antecubital
Figure 15
Auscultatory Method.
systolic and diastolic pressures by indirect means,
studies are necessary. Instead, the clinician determines
routine pressure measurements in human patients,
Clinical Methods for Measuring
increase in pressure. Therefore, in effect,
the more compliant a vessel, the greater the quantity
occur. The compliance damps the pulsations because
greater the resistance, the more dif
front to distend the next segment of the vessel; the
The resistance damps the pulsations because a small
ment in the vessels and (2) compliance of the vessels.
cause of this is twofold: (1) resistance to blood move-
of the pressure pulses. The
This progressive diminution of the pulsations in the
Vascular Distensibility and Functions of the Arterial and Venous Systems
Chapter 15
175
periphery is called damping
amount of blood must flow forward at the pulse wave
ficult it is for this to
of blood required at the pulse wave front to cause an
the degree of
damping is almost directly proportional to the product
of resistance times compliance.
Systolic and Diastolic Pressures
It is not reasonable to use pressure recorders that
require needle insertion into an artery for making
although these are used on occasion when special
usually by the auscultatory method.
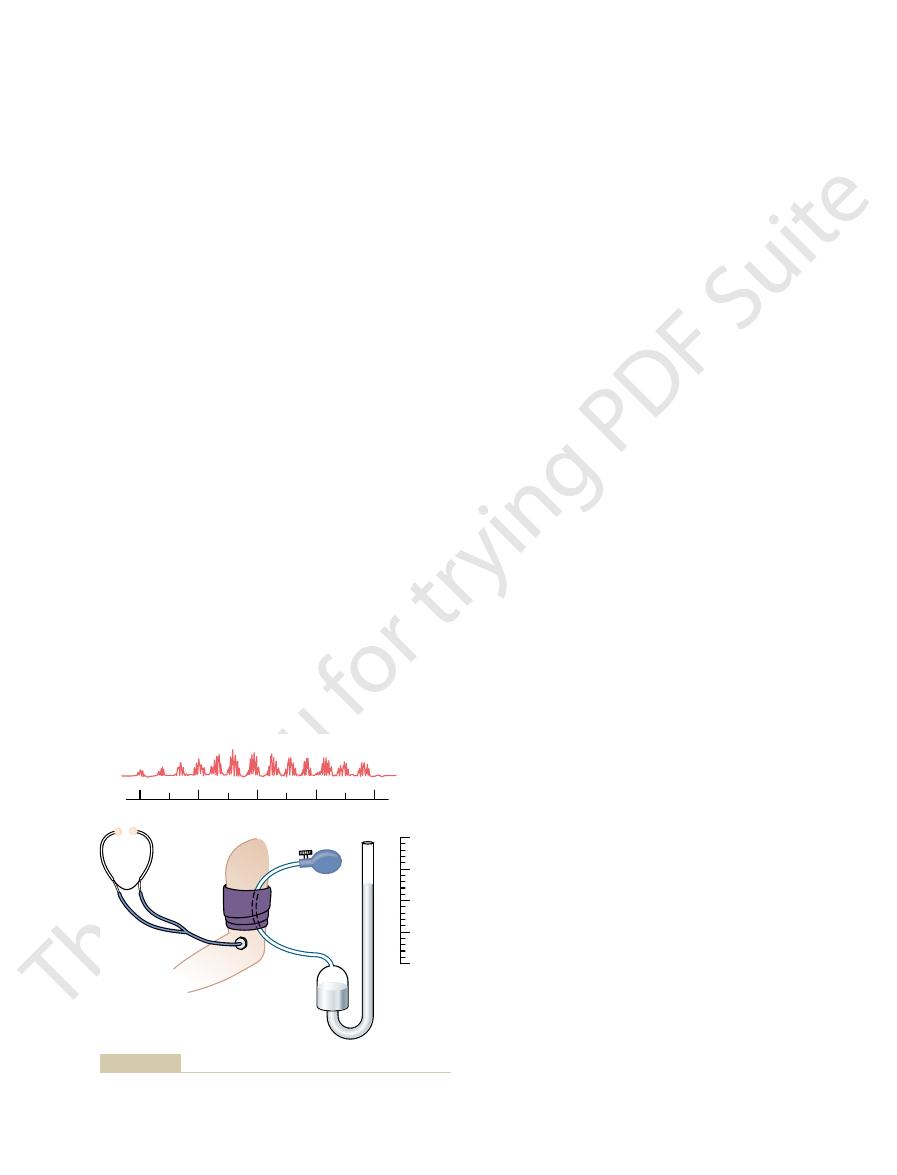
–7 shows the auscultatory
method for determining systolic and diastolic arterial
artery and a blood pressure cuff is inflated around the
the arm with too little pressure to close the brachial
is great enough to close the artery during part of the
.
by blood jetting through the partly occluded vessel.
and this sets up the vibrations heard through the
In determining blood pressure by the auscultatory
first elevated well
artery remains collapsed so that no blood jets into the
and one begins to hear tapping sounds from the ante-
indicated by the manometer connected to the cuff is
tapping quality and more of a rhythmical and harsher
fi
causing the sounds (the jetting of blood through a
sounds suddenly change to a muffl
appear entirely after another 5- to 10-millimeter drop
fled
but it usually gives values within 10 per cent of those
determined by direct catheter measurement from
Method.
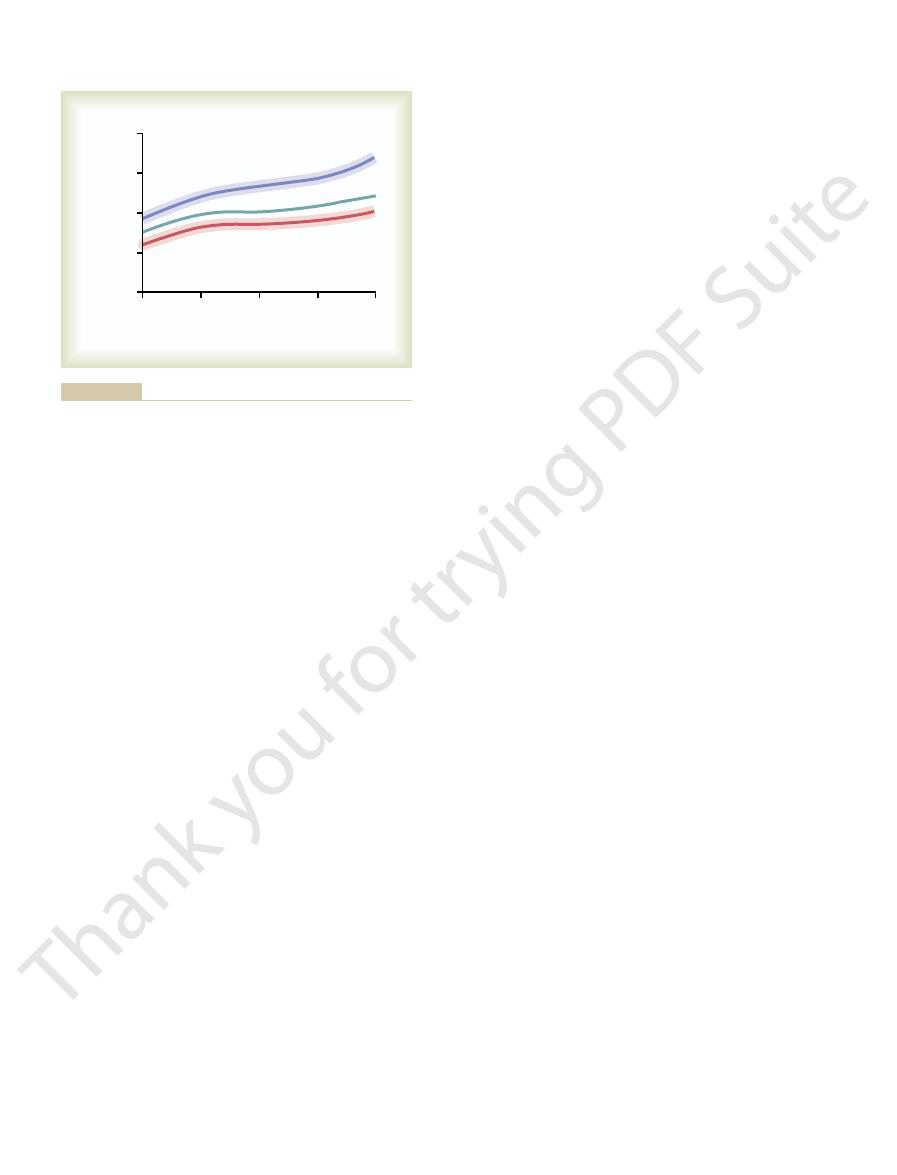
–8 shows the approximate normal
systolic and diastolic arterial pressures at different
results from the effects of aging on the blood pressure
the kidneys are primarily responsible for this long-
known that the kidneys exhibit definitive changes with
A slight extra increase in systolic pressure usually
result of atherosclerosis
final effect is a bounding
systolic pressure with considerable increase in pulse
Mean Arterial Pressure.
average of the arterial pressures measured millisecond
120
100
Sounds
150
mm Hg
100
50
0
80
pressures.
Auscultatory method for measuring systolic and diastolic arterial
Figure 15–7
and because of this, the pressure in the more
flow,
to an ovoid or slitlike state. For these reasons, the
sure, so that they usually are at least partially collapsed
neck causes these veins to collapse. Finally, veins
Also, the pressure in the neck veins often falls so low
rst rib.
points. For instance, the veins from the arms are com-
rounding tissues, so that blood
9, most of the large veins that enter
shown in Figure 15
zero and is of almost no importance. However, as
Venous Pressure
Venous Resistance and Peripheral
severe hemorrhage.
peripheral vessels is greatly depressed, such as after
rounds the heart. The right atrial pressure approaches
This is also the pressure in the chest cavity that sur-
5 mm Hg below atmospheric pressure.
The lower limit to the right atrial pressure is usually
from the peripheral vessels.
or (2) after massive transfusion of blood, which greatly
abnormal conditions, such as (1) serious heart failure
body. It can increase to 20 to 30 mm Hg under very
is about 0 mm Hg,
The
peripheral vessels. Therefore, we will discuss regula-
the tendency for blood to
The same factors that regulate right atrial pressure
ow of blood from the arteries into the veins.
venous pressures, and (3) dilatation of the arterioles,
blood volume, (2) increased large vessel tone through-
elevates the right atrial pressure. Some of the factors
pressure. Also, any effect that causes rapid in
versely, weakness of the heart elevates the right atrial
strongly, the right atrial pressure decreases. Con-
the tendency for blood to flow from the peripheral veins
between (1) the ability of the heart to pump blood out
Right atrial pressure is regulated by a balance
central venous pressure.
atrium of the heart; therefore, the pressure in the right
the veins and what determines the pressure.
To understand the various functions of the veins, it is
and Peripheral Venous Pressures
Pressure (Central Venous Pressure)
Venous Pressures—Right Atrial
, and they even help to regulate cardiac output,
der of the circulation. The peripheral veins can also
the circulation. Especially important, they are capable
For years, the veins were considered to be nothing
Veins and Their Functions
to the systolic pressure.
in Figure 15
pressure and 40 per cent by the systolic pressure. Note
of the cardiac cycle. Therefore, the mean arterial pres-
by millisecond over a period of time. It is not equal to
176
Unit IV
The Circulation
the average of systolic and diastolic pressure because
the arterial pressure remains nearer to diastolic pres-
sure than to systolic pressure during the greater part
sure is determined about 60 per cent by the diastolic
–8 that the mean pressure (solid green
line) at all ages is nearer to the diastolic pressure than
more than passageways for flow of blood to the heart,
but it has become apparent that they perform other
special functions that are necessary for operation of
of constricting and enlarging and thereby storing
either small or large quantities of blood and making
this blood available when it is required by the remain-
propel blood forward by means of a so-called venous
pump
an exceedingly important function that is described in
detail in Chapter 20.
first necessary to know something about pressure in
Blood from all the systemic veins flows into the right
atrium is called the
of the right atrium and ventricle into the lungs and (2)
into the right atrium. If the right heart is pumping
flow of
blood into the right atrium from the peripheral veins
that can increase this venous return (and thereby
increase the right atrial pressure) are (1) increased
out the body with resultant increased peripheral
which decreases the peripheral resistance and allows
rapid fl
also enter into the regulation of cardiac output
because the amount of blood pumped by the heart
depends on both the ability of the heart to pump and
flow into the heart from the
tion of right atrial pressure in much more depth in
Chapter 20 in connection with regulation of cardiac
output.
normal right atrial pressure
which is equal to the atmospheric pressure around the
increases the total blood volume and causes excessive
quantities of blood to attempt to flow into the heart
about
-3 to -
these low values when the heart pumps with excep-
tional vigor or when blood flow into the heart from the
Large veins have so little resistance to blood flow when
they are distended that the resistance then is almost
–
the thorax are compressed at many points by the sur-
flow is impeded at these
pressed by their sharp angulations over the fi
that the atmospheric pressure on the outside of the
coursing through the abdomen are often compressed
by different organs and by the intra-abdominal pres-
large veins do usually offer some resistance to blood
20
80
Pressure (mm Hg)
0
0
150
100
200
60
40
Age (years)
50
Systolic
Mean
Diastolic
age. The shaded areas show the approximate normal ranges.
Changes in systolic, diastolic, and mean arterial pressures with
Figure 15–8
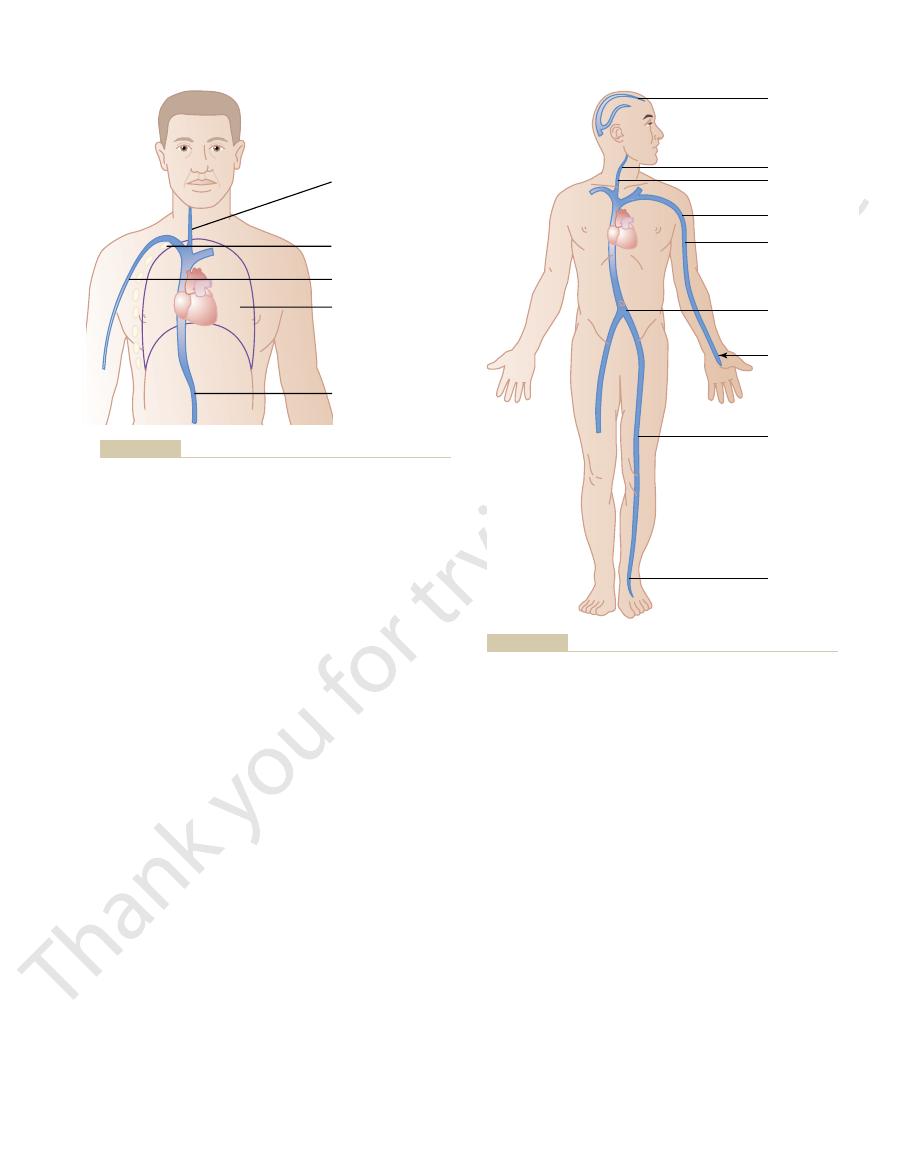
rib. Thus, if the gravitational difference between the
of the subclavian vein as it passes over this rib. The
6 mm Hg because of compression
In the arm veins, the pressure at the level of the top
90 mm Hg.
the heart and the feet. The venous pressures at other
90 mm Hg simply because of the gravita-
, the pressure in the veins of the feet
mulate at this point. However, in an adult
remains about 0 mm Hg because the heart pumps into
a person is standing, the pressure in the right atrium
10. When
blood in the vessels, as shown in Figure 15
millimeters of distance below the surface. This pres-
pressure, but the pressure rises 1 mm Hg for each 13.6
In any body of water that is exposed to air, the pres-
Pressure
Effect of Gravitational Pressure on Venous
20 mm Hg.
20 mm Hg, the
ow from the legs to the heart. Thus,
above
abdominal pressure does rise, the pressure in the veins
) in the abdominal cavity. When the intra-
pregnancy, large tumors, or excessive
30 mm Hg as a result of
6 mm Hg,
The pressure in the abdominal cavity of a recum-
Effect of Intra-abdominal Pressure on Venous Pressures of the
of heart failure.
Hg, one often
6 mm
eral venous pressure in the limbs and elsewhere.
the right atrial pressure rises still further, the addi-
6 mm Hg. Then, as
the large veins. This enlarges the veins, and even the
normal value of 0 mm Hg, blood begins to back up in
When the right atrial pressure rises above its
Effect of High Right Atrial Pressure on Peripheral Venous Pres-
6 mm Hg greater than the right atrial pressure.
Vascular Distensibility and Functions of the Arterial and Venous Systems
Chapter 15
177
peripheral small veins in a person lying down is usually
+4 to +
sure.
collapse points in the veins open up when the right
atrial pressure rises above
+4 to +
tional increase causes a corresponding rise in periph-
Because the heart must be weakened greatly to cause
a rise in right atrial pressure as high as
+4 to +
finds that the peripheral venous pres-
sure is not noticeably elevated even in the early stages
Leg.
bent person normally averages about
+
but it can rise to
+15 to +
fluid (called
“ascites”
of the legs must rise
the abdominal pressure
before the abdominal veins will open and allow
the blood to fl
if the intra-abdominal pressure is
+
lowest possible pressure in the femoral veins is also
+
sure at the surface of the water is equal to atmospheric
sure results from the weight of the water and there-
fore is called gravitational pressure or hydrostatic
pressure.
Gravitational pressure also occurs in the vascular
system of the human being because of weight of the
–
the arteries any excess blood that attempts to accu-
who is stand-
ing absolutely still
is about
+
tional weight of the blood in the veins between
levels of the body are proportionately between 0 and
rib is usually about
+
gravitational pressure down the length of the arm then
is determined by the distance below the level of this
4 mm Hg
Atmospheric
pressure
collapse in neck
Axillary collapse
Abdominal
pressure
collapse
Intrathoracic
pressure =
-
Rib collapse
Compression points that tend to collapse the veins entering the
Figure 15–9
thorax.
9 0 mm
4 0 mm
3 5 mm
2 2 mm
8 mm
6 mm
0 mm
0 mm
1 0 mm
Sagittal sinus
-
+
+
+
+
+
+
Effect of gravitational pressure on the venous pressures through-
Figure 15–10
out the body in the standing person.

ulcerates. The best treatment for such a condition is
cells, so that the muscles become painful and weak,
illaries causes constant edema in the legs. The edema
become very high, and leakage of
than a few minutes, the venous and capillary pressures
Whenever people with varicose veins stand for more
the entire leg, particularly the lower leg.
which are characterized by large,
varicose veins,
function of the valves entirely. Thus, the person devel-
because of failure of the venous pump; this further
no longer close completely. When this develops, the
not increase in size. Therefore, the lea
cross-sectional areas, but the lea
most of the time. Stretching the veins increases their
months, as occurs in pregnancy or when one stands
is especially true when the veins have been over-
or sometimes even are destroyed. This
The
Venous Valve Incompetence Causes “Varicose” Veins.
minutes of standing absolutely still, as often occurs
Indeed, 10 to 20 per cent of the blood volume can be
the legs swell, and the blood volume diminishes.
circulatory system into the tissue spaces. As a result,
ies also increase greatly, causing
Hg in about 30 seconds. The pressures in the capillar-
legs increase to the full gravitational value of 90 mm
does not work, and the venous pressures in the lower
If a person stands perfectly still, the venous pump
20 mm Hg.
circumstances, the venous pressure in the feet of a
pump,
blood is propelled toward the heart. This pumping
tenses the leg muscles, a certain amount of venous
quently, every time a person moves the legs or even
ow can be only toward the heart. Conse-
11, are arranged so that the direction of venous
veins. But the valves in the veins, shown in Figure
the muscles, and this squeezes the blood out of the
However, every time one moves the legs, one tightens
90 mm Hg in a standing adult.
Were it not for valves in the veins, the gravitational
Their Effects on Venous Pressure
Venous Valves and the “Venous Pump”:
vessels.
rial pressure is 100 mm Hg, this generally means that
190 mm Hg. Therefore, when one states that the arte-
has a mean arterial pressure of 100 mm Hg at the level
effects in the veins. For instance, a standing person who
the peripheral arteries and capillaries, in addition to its
The gravitational factor also affects pressures in
death can ensue.
downward to cause air embolism in the heart, and
ately into the venous system; the air may even pass
is opened during surgery, air can be sucked immedi-
and the base of the skull. Therefore, if the sagittal sinus
10 mm Hg because of
ing position, the venous pressure in the sagittal sinus
they cannot collapse. Consequently,
The veins inside the skull, on the other hand, are in
sure back to zero.
zero collapses the veins still more, which further
any tendency for the neck vein pressure to fall below
ow of the blood. Conversely,
that any tendency for the pressure to rise above this
at zero along their entire extent. The reason for this is
atmospheric pressure on the outside of the neck. This
The neck veins of a person standing upright collapse
35 mm Hg pressure in the veins of
caused by compression of the vein as it crosses the rib,
6 mm Hg pressure
29 mm Hg, this grav-
178
Unit IV
The Circulation
level of the rib and the hand is
+
itational pressure is added to the
+
making a total of
+
the hand.
almost completely all the way to the skull because of
collapse causes the pressure in these veins to remain
level opens the veins and allows the pressure to fall
back to zero because of fl
increases their resistance and again returns the pres-
a noncollapsible chamber (the skull cavity) so that
negative pressure
can exist in the dural sinuses of the head; in the stand-
at the top of the brain is about
-
the hydrostatic “suction” between the top of the skull
Effect of the Gravitational Factor on Arterial and Other Pres-
sures.
of the heart has an arterial pressure in the feet of about
this is the pressure at the gravitational level of the
heart but not necessarily elsewhere in the arterial
pressure effect would cause the venous pressure in the
feet always to be about
+
the muscles and compresses the veins in or adjacent to
15–
blood fl
system is known as the “venous pump” or “muscle
” and it is efficient enough that under ordinary
walking adult remains less than
+
fluid to leak from the
lost from the circulatory system within the 15 to 30
when a soldier is made to stand at rigid attention.
valves of the venous system frequently become
“incompetent”
stretched by excess venous pressure lasting weeks or
flets of the valves do
flets of the valves
pressure in the veins of the legs increases greatly
increases the sizes of the veins and finally destroys the
ops “
”
bulbous protrusions of the veins beneath the skin of
fluid from the cap-
in turn prevents adequate diffusion of nutritional
materials from the capillaries to the muscle and skin
and the skin frequently becomes gangrenous and
Valve
Deep vein
Perforating
vein
Superficial
vein
Venous valves of the leg.
Figure 15–11
The sinuses can swell the same as any other part
pulp.
areas for storing blood: the
Figure 15
decrease to low values.
milliliters of blood; the lungs can contribute another
heart, for instance, shrinks during sympathetic stimu-
system, must also be considered blood reservoirs. The
lungs,
several hundred milliliters. The
tribute as much as 300 milliliters; and (4) the
large abdominal veins,
tion; (3) the
liver,
of blood into other areas of the circulation; (2) the
These
c blood reservoirs.
Specific Blood Reservoirs.
variable reservoir function of the veins.
total blood volume has been lost, the circulatory
blood. Indeed, even after as much as 20 per cent of the
veins, causing them to constrict. This takes up much of
These in turn elicit nerve signals from the brain and
areas of the circulation, as discussed in Chapter 18.
pressure begins to fall, nervous signals are elicited
When blood is lost from the body and the arterial
are so compliant, it is said that the venous system
the veins. For this reason and also because the veins
As pointed out in Chapter 14, more than 60 per cent
Blood Reservoir Function of the Veins
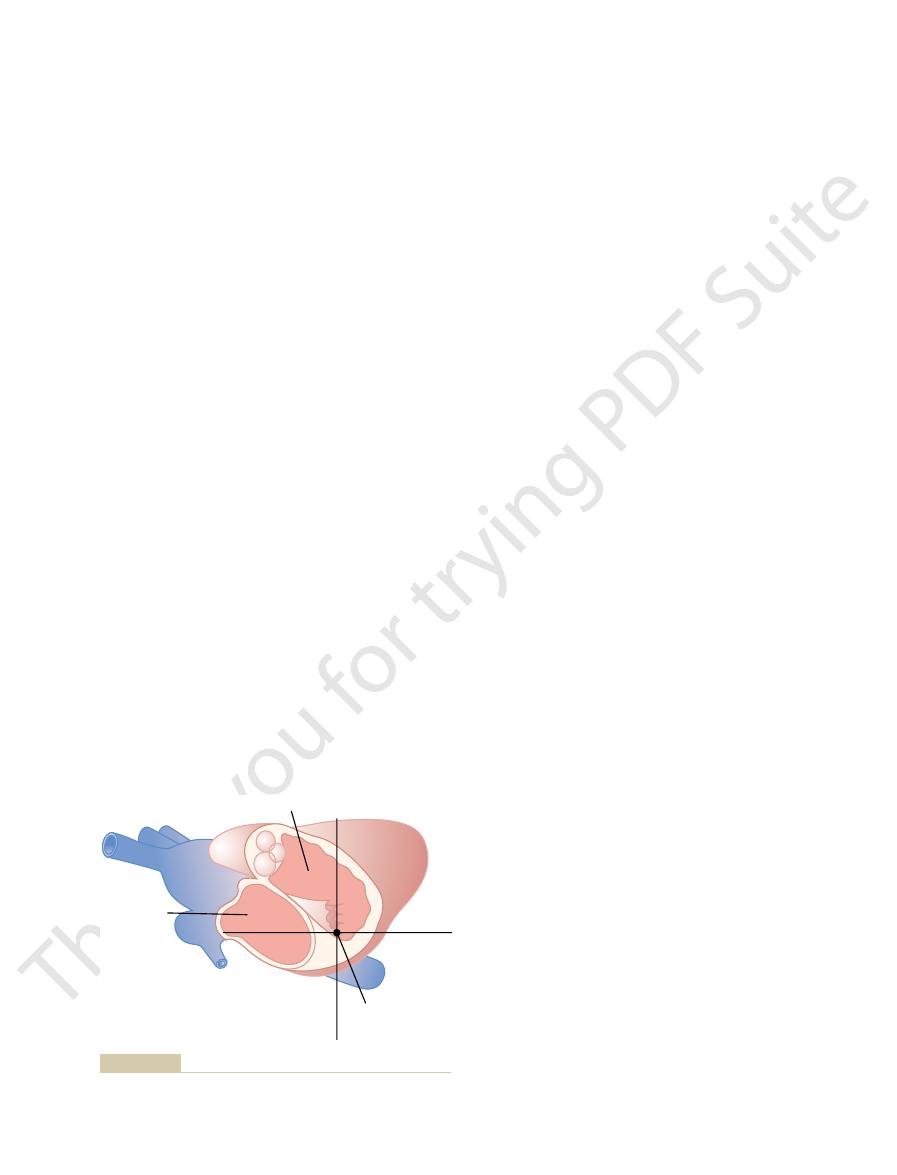
zero pres-
chest thickness in front of the back. This is the
When a person is lying on his or her back, the tricus-
tricuspid valve.
the heart acts as a feedback regulator of pressure
level again rises to the normal value. In other words,
adequately, its pumping decreases, and blood dams up
versely, if the pressure falls, the right ventricle fails to
cuspid valve back toward the normal mean value. Con-
than usual, causing the heart to pump blood more
above normal, the right ventricle
The reason for lack of gravitational effects at the
discussed in this text are referred to this level, which is
12. Therefore, all circulatory pressure measurements
cuspid valve, as shown by the crossed axes in Figure
than 1 to 2 mm Hg. This is at or near the level of the tri-
pressure is referred. There is one point in the circula-
sure as being 100 mm Hg, but we have not stated the
right atrial pressure as being 0 mm Hg and arterial pres-
In discussions up to this point, we often have spoken of
Circulatory Pressures
Pressure Reference Level for Measuring Venous and Other
assessment of heart pumping ability.
right atrium. Pressures measured through such
to a pressure recorder. The only means by which
Venous pressure can also be measured with ease by
Direct Measurement of Venous Pressure and
15 mm Hg
veins of the neck begin to protrude; and at
10 mm Hg, the lower
person. However, when the right atrial pressure be-
neck veins. For instance, in the sitting position, the neck
The venous pressure
Clinical Estimation of Venous Pressure.
its sequelae.
as the heart. Tight binders on the legs also can be of
Vascular Distensibility and Functions of the Arterial and Venous Systems
Chapter 15
179
continual elevation of the legs to a level at least as high
considerable assistance in preventing the edema and
often can be estimated by simply observing the degree
of distention of the peripheral veins—especially of the
veins are never distended in the normal quietly resting
comes increased to as much as
+
+
atrial pressure essentially all the veins in the neck
become distended.
Right Atrial Pressure
inserting a needle directly into a vein and connecting it
right
atrial pressure can be measured accurately is by insert-
ing a catheter through the peripheral veins and into the
central
venous catheters are used almost routinely in some types
of hospitalized cardiac patients to provide constant
gravitational level in the circulatory system to which this
tory system at which gravitational pressure factors
caused by changes in body position of a healthy person
usually do not affect the pressure measurement by more
15–
called the reference level for pressure measurement.
tricuspid valve is that the heart automatically prevents
significant gravitational changes in pressure at this point
in the following way:
If the pressure at the tricuspid valve rises slightly
fills to a greater extent
rapidly and therefore to decrease the pressure at the tri-
fill
in the venous system until the pressure at the tricuspid
at the
pid valve is located at almost exactly 60 per cent of the
sure reference level for a person lying down.
of all the blood in the circulatory system is usually in
serves as a blood reservoir for the circulation.
from the carotid sinuses and other pressure-sensitive
spinal cord mainly through sympathetic nerves to the
the slack in the circulatory system caused by the lost
system often functions almost normally because of this
Certain portions of the circu-
latory system are so extensive and/or so compliant that
they are called “specifi
”
include (1) the spleen, which sometimes can decrease
in size sufficiently to release as much as 100 milliliters
the sinuses of which can release several hundred
milliliters of blood into the remainder of the circula-
which can con-
venous
plexus beneath the skin, which also can contribute
heart and the
although not parts of the systemic venous reservoir
lation and in this way can contribute some 50 to 100
100 to 200 milliliters when the pulmonary pressures
The Spleen as a Reservoir for Storing Red Blood Cells.
–13 shows that the spleen has two separate
venous sinuses and the
of the venous system and store whole blood.
Right ventricle
Right atrium
Natural reference
point
Reference point for circulatory pressure measurement (located
Figure 15–12
near the tricuspid valve).
15(Suppl 1):S30, 2004.
ambulatory blood pressure monitoring. J Am Soc Nephrol
Verdecchia P, Angeli F, Gattobigio R: Clinical usefulness of
sion and cardiovascular diseases. Circulation 107:2864,
Safar ME, Levy BI, Struijker-Boudier H: Current perspec-
(Adv Physiol Educ) 26:98, 2002.
interactive tutorial and mathematical model. Am J Physiol
Rothe CF, Gersting JM: Cardiovascular interactions: an
88:2460, 1993.
determination by sphygmomanometry.
Circulation
Perloff D, Grim C, Flack J, et al: Human blood pressure
Hypertens 21:821, 2003.
ambulatory and home blood pressure measurement. J
Brien E, Asmar R, Beilin L, et al: European Society
dence based review. BMJ 322:908, 2001.
hypertension. Measurement of blood pressure: an evi-
McAlister FA, Straus SE: Evidence based treatment of
107:139, 2003.
for vascular disease. Circulation
Aging arteries: a
shareholders in cardiovascular disease enterprises. Part I:
Lakatta EG, Levy D: Arterial and cardiac aging: major
289:1027, 2003.
sure accurately: New and persistent challenges. JAMA
Jones DW, Appel LJ, Sheps SG, et al: Measuring blood pres-
systems. Am J Physiol 262:R725-R732, 1992.
vs.
Hicks JW, Badeer HS: Gravity and the circulation:
Am J Physiol (Adv Physiol Educ) 22:s174, 1999.
Hall J: Integration and regulation of cardiovascular function.
Saunders Co, 1973.
Cardiac Output and Its Regulation. Philadelphia: WB
Guyton AC, Jones CE, Coleman TG: Circulatory Physiology:
431, 1973.
cance and clinical implications. Am Heart J 86:
Guyton AC, Jones CE: Central venous pressure: physiologi-
Philadelphia: WB Saunders Co, 1980.
Guyton AC:
Arterial Pressure and Hypertension.
N Y Acad Sci 902:230, 2000.
function, hemodynamic forces, and atherogenesis. Ann
Gimbrone MA Jr, Topper JN, Nagel T, et al: Endothelial dys-
15:1101, 2002.
arterial stiffness: clinical applications. Am J Hypertens
age, risk factors, and cardiovascular and renal disease on
Benetos A, Waeber B, Izzo J, Mitchell G, et al: In
Physiol (Adv Physiol Educ) 25:44, 2001.
Badeer HS: Hemodynamics for medical students. Am J
avidly.
Also, in many chronic infectious processes, the spleen
rapidly remove debris, bacteria, parasites, and so forth.
tious agents, the reticuloendothelial cells of the spleen
sinuses of the liver. When the blood is invaded by infec-
cleansing system for the blood, acting in concert with a
lined with similar cells. These cells function as part of a
reticuloendothelial cells, and the venous sinuses are
The pulp of the spleen contains many large phagocytic
nutrients, often for making new blood cells.
by the reticuloendothelial cells of the spleen, and the
nal demise in the spleen. After the cells rupture, the
would not withstand the trauma. For this reason, many
Therefore, it is to be expected that fragile red blood cells
entering the sinuses undergo thorough squeezing.
s immune system, described in Chapter 34.
manufactured in the lymph nodes. They are part of the
white pulp.
blood cells, which collectively are called the
to contract. As much as 50 milliliters of concentrated
These can then be expelled into the general
blood cells.
sequence, the red pulp of the spleen is a
sinuses and then into the general circulation. As a con-
trabeculae, while the plasma
The red cells are trapped by the
red pulp.
that whole blood, including the red blood cells, oozes
In the splenic pulp, the capillaries are so permeable
180
Unit IV
The Circulation
through the capillary walls into a trabecular mesh,
forming the
flows on into the venous
special reser-
voir that contains large quantities of concentrated red
circulation whenever the sympathetic nervous system
becomes excited and causes the spleen and its vessels
red blood cells can be released into the circulation,
raising the hematocrit 1 to 2 per cent.
In other areas of the splenic pulp are islands of white
Here lymphoid cells are manufactured similar to those
body’
Blood-Cleansing Function of the Spleen—Removal of Old Cells
Blood cells passing through the splenic pulp before
of the red blood cells destroyed in the body have their
fi
released hemoglobin and the cell stroma are digested
products of digestion are mainly reused by the body as
Reticuloendothelial Cells of the Spleen
similar system of reticuloendothelial cells in the venous
enlarges in the same manner that lymph nodes enlarge
and then performs its cleansing function even more
References
fluence of
cal signifi
“open”
“closed”
“set up”
O’
of Hypertension recommendations for conventional,
tives on arterial stiffness and pulse pressure in hyperten-
2003.
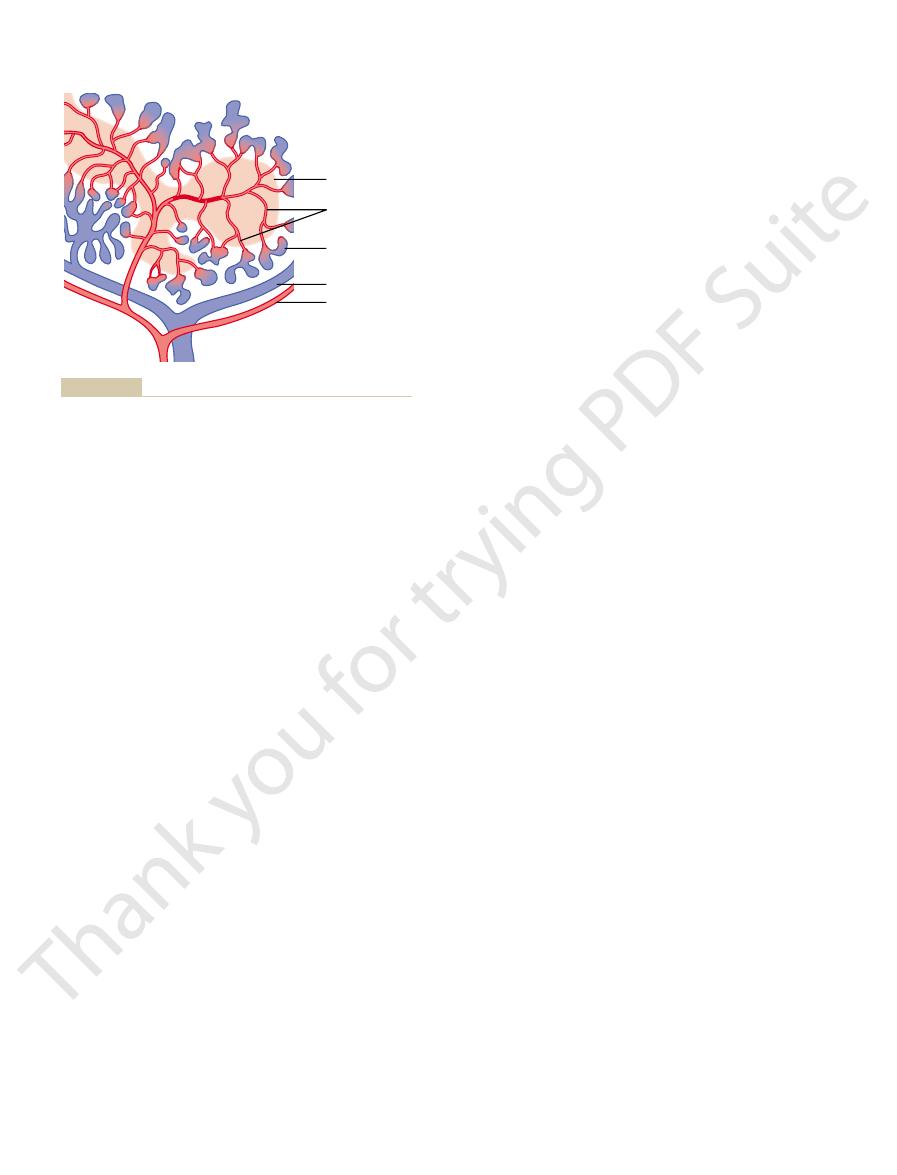
Pulp
Vein
Artery
Capillaries
Venous sinuses
Functional structures of the spleen. (Courtesy of Dr. Don W.
Figure 15–13
Fawcett, Montana.)
