
especially in muscles and connective tissue. Note that the wall is composed of
typical endothelial cells in the capillary wall as found in most organs of the body,
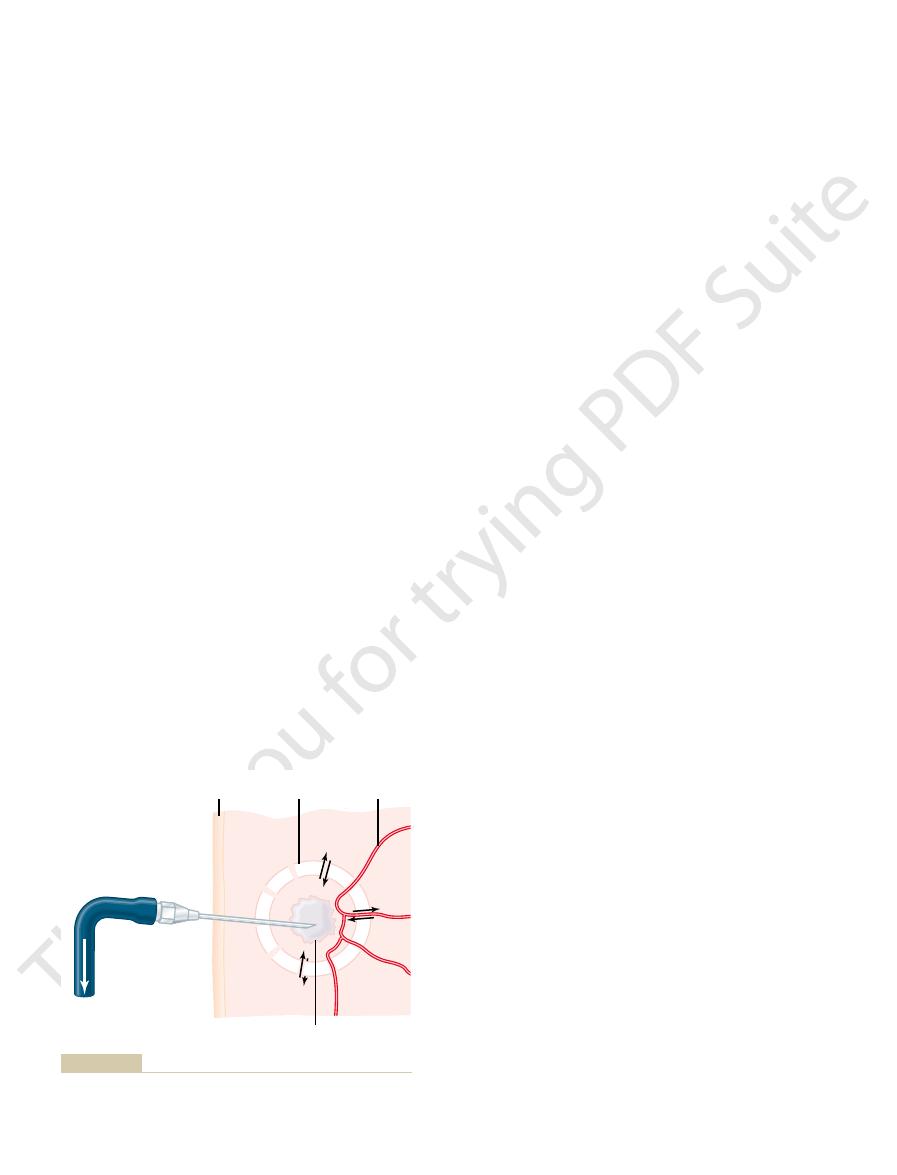
Figure 16–2 shows the ultramicroscopic structure of
Structure of the Capillary Wall.
nutrients, end products of metabolism, hydrogen ions, and so forth—can cause direct
they serve. Therefore, the local conditions of the tissues—the concentrations of
however, some similar arrangement serves the same purposes. Most important, the
This typical arrangement of the capillary bed is not found in all parts of the body;
muscle.
in the arterioles, so that the venules still can contract considerably despite the weak
Yet it must be remembered that the pressure in the venules is much less than that
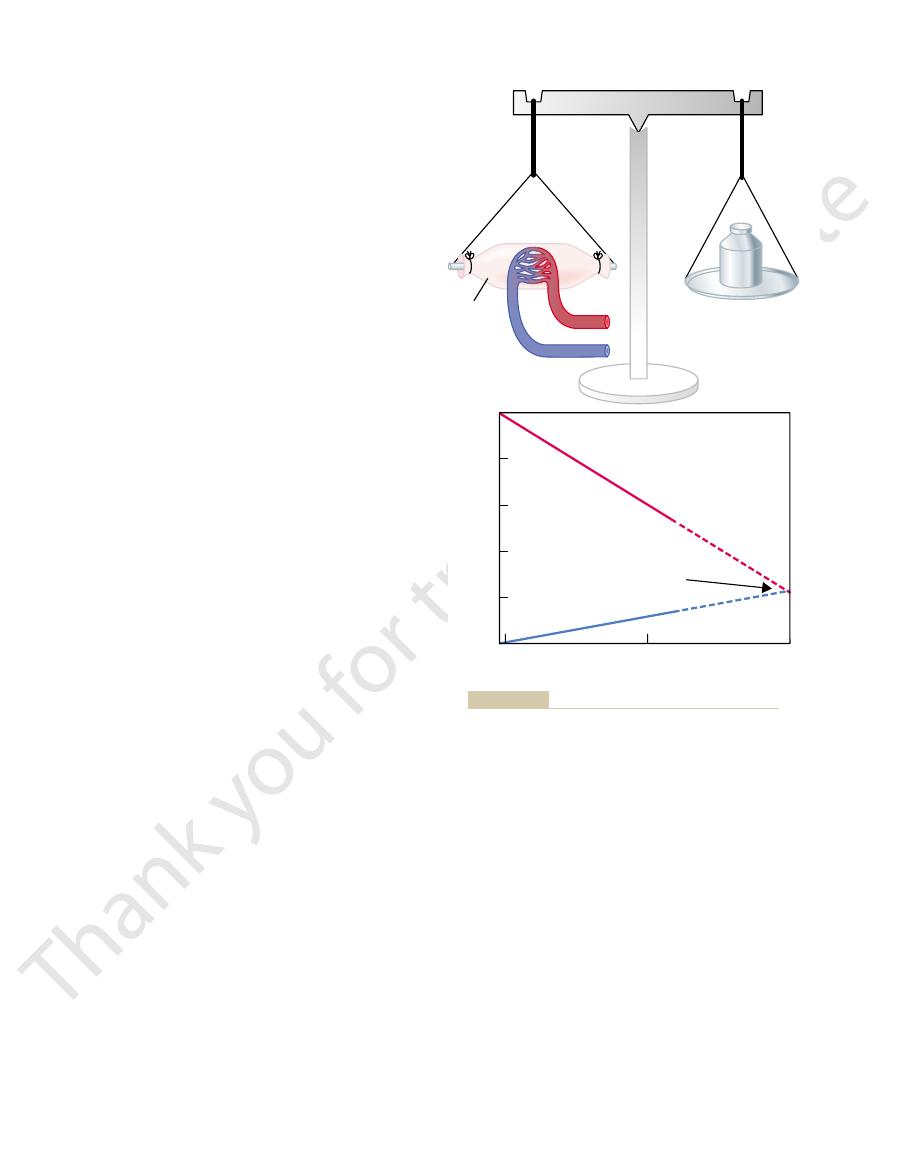
The venules are larger than the arterioles and have a much weaker muscular coat.
This sphincter can open and close the entrance to the capillary.
precapillary sphincter.
muscle fiber usually encircles the capillary. This is called the
At the point where each true capillary originates from a metarteriole, a smooth
16–1 by the black dots on the sides of the metarteriole.
smooth muscle fibers encircle the vessel at intermittent points, as shown in Figure
metarterioles (the terminal arterioles) do not have a continuous muscular coat, but
The arterioles are highly muscular, and their diameters can change manyfold. The
where they supply blood to the capillaries.
branch two to five times, reaching diameters of 5 to 9 micrometers at their ends
have internal diameters of only 10 to 15 micrometers. Then the arterioles themselves
arterioles,
needs. In general, each nutrient artery entering an organ branches six to eight times
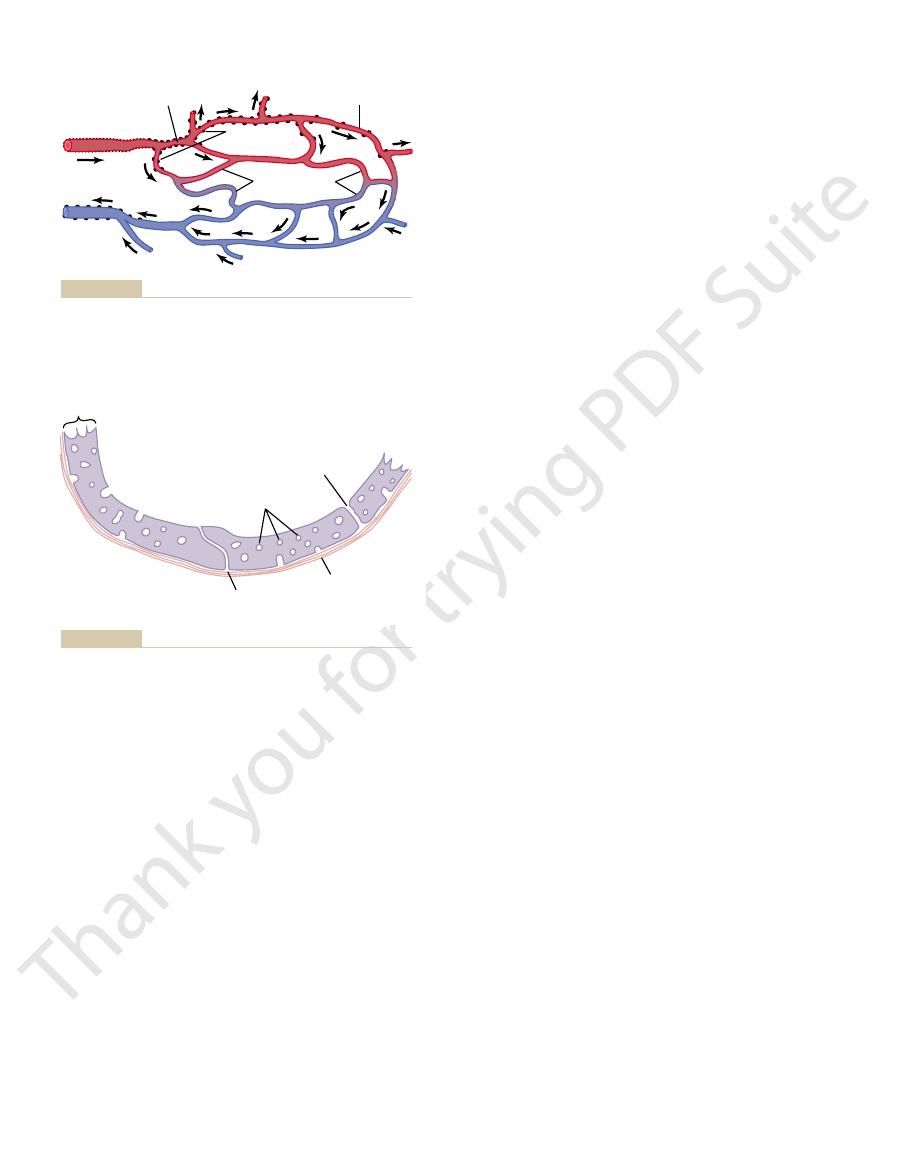
The microcirculation of each organ is organized specifically to serve that organ’s
Capillary System
Structure of the Microcirculation and
tional cell of the body is more than 20 to 30 micrometers away from a capillary.
eighth the surface area of a football field). Indeed, it is rare that any single func-
The peripheral circulation of the whole body has about 10 billion capillaries
highly permeable endothelial cells. Therefore, water, cell nutrients, and cell
The walls of the capillaries are extremely thin, constructed of single-layer,
in relation to its individual needs, a subject that is
tissue, in most instances, controls its own blood flow
control the diameters of the arterioles. Thus, each
tissue area, and local conditions in the tissues in turn
The small arterioles control blood flow to each
nutrients to the tissues and removal of cell excreta
occurs in the microcirculation: this is
The most purposeful function of the circulation
and Lymph Flow
Fluid Exchange, Interstitial Fluid,
Lymphatic System: Capillary
The Microcirculation and the
C
H
A
P
T
E
R
1
6
181
transport of
.
discussed in detail in Chapter 17.
excreta can all interchange quickly and easily between the tissues and the cir-
culating blood.
with a total surface area estimated to be 500 to 700 square meters (about one-
before the arteries become small enough to be called
which generally
metarterioles and the precapillary sphincters are in close contact with the tissues
effects on the vessels in controlling local blood flow in each small tissue area.
in the tissues. When
oxygen
The most important factor
Regulation of Vasomotion.
intermittency is the phenomenon called
and off every few seconds or minutes. The cause of this
capillaries. Instead, it flows intermittently, turning on
Capillaries—Vasomotion
clefts between the endothelial cells.
cells, so that tremendous amounts of very small
, numerous
4. In the
muscles and those of the liver.
3. The pores of the
blood into the liver tissues.
including the plasma proteins, can pass from the
the capillary endothelial cells are wide open, so
, the opposite is true. The clefts between
2. In the
out of the brain tissues.
water, oxygen, and carbon dioxide to pass into or
endothelial cells are mainly “tight” junctions that
, the junctions between the capillary
1. In the
of the organs. Some of these characteristics are as
The “pores” in the capillaries of some organs
Special Types of “Pores” Occur in the Capillaries of Certain
transport are quantitatively of little importance.
However, careful measurements in laboratory animals
cell, which is demonstrated to the right in Figure 16–2.
vesicular channels
through the endothelial cell. It also has been postu-
or extracellular fluid. They can then move slowly
These form at one
plasmalemmal vesicles.
intercellular clefts.
rior of the capillaries through these “slit-pores,” the
motion of water molecules as well as most water-
the capillary wall. Nevertheless, the rate of thermal
the edges of the endothelial cells, they usually repre-
protein molecule.
cleft. The cleft normally has a uniform spacing with a
that hold the endothelial cells together, but between
adjacent endothelial cells. Each cleft is interrupted
which is the thin-slit, curving
interior of the capillary with the exterior. One of these
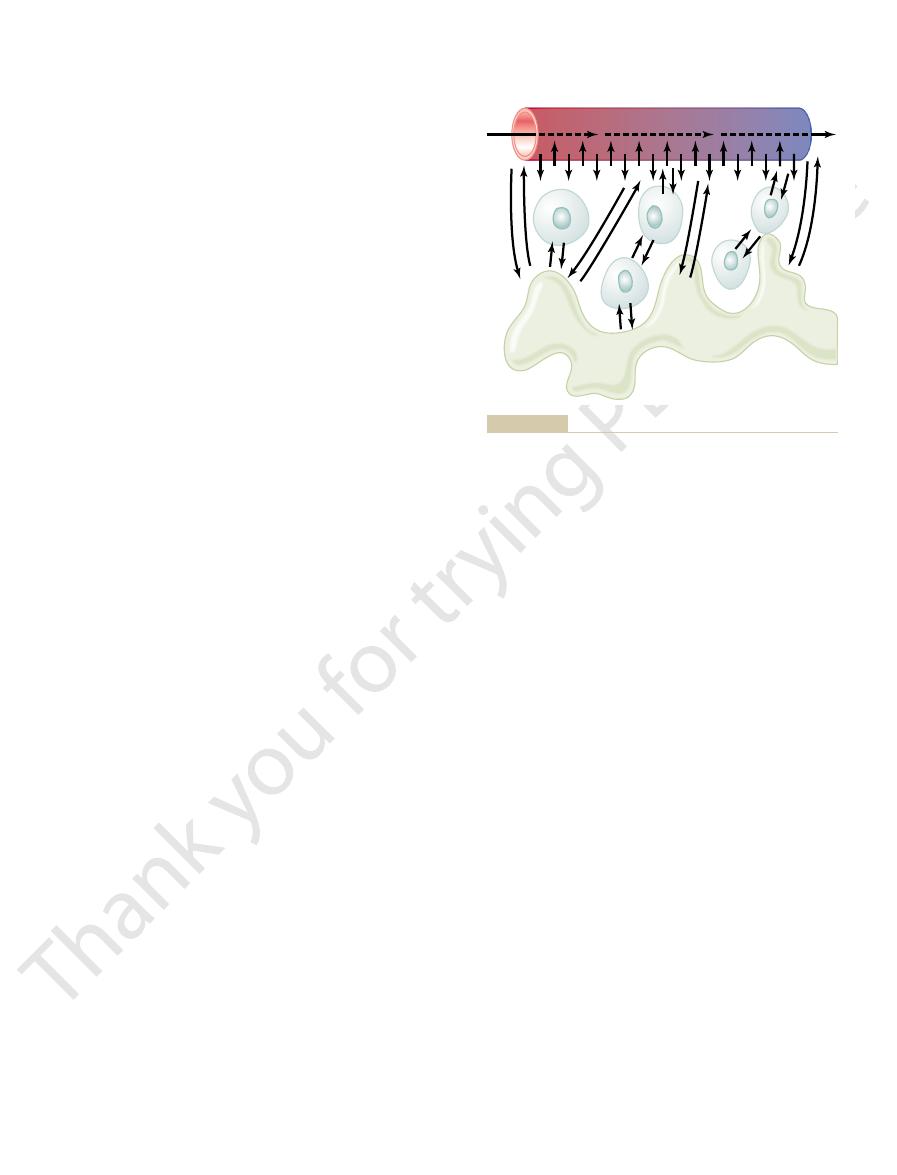
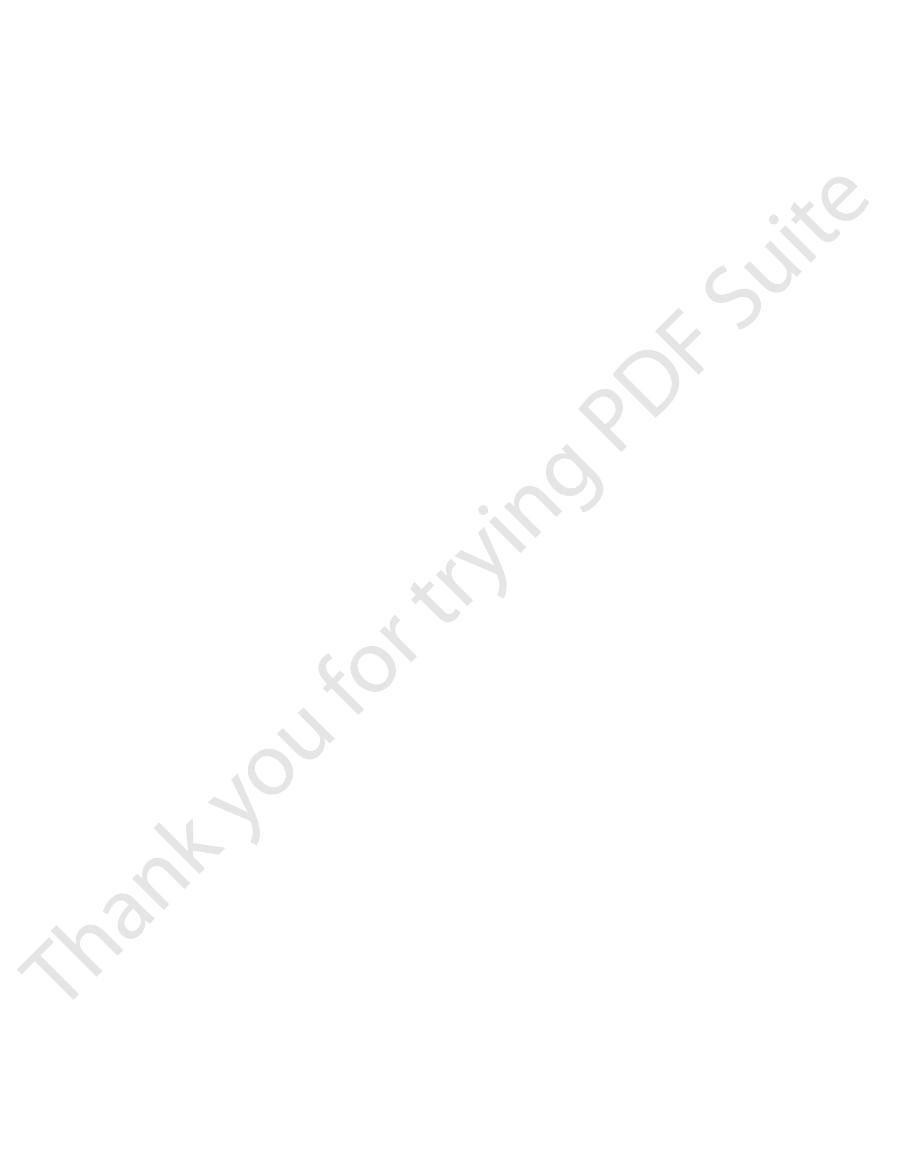
Studying Figure 16–2,
“Pores” in the Capillary Membrane.
diameter of the capillary is 4 to 9 micrometers, barely
illary wall is only about 0.5 micrometer. The internal
outside of the capillary. The total thickness of the cap-
182
Unit IV
The Circulation
a unicellular layer of endothelial cells and is sur-
rounded by a very thin basement membrane on the
large enough for red blood cells and other blood cells
to squeeze through.
one sees two very small passageways connecting the
is an intercellular cleft,
channel that lies at the bottom of the figure between
periodically by short ridges of protein attachments
these ridges fluid can percolate freely through the
width of about 6 to 7 nanometers (60 to 70 angstroms),
slightly smaller than the diameter of an albumin
Because the intercellular clefts are located only at
sent no more than 1/1000 of the total surface area of
soluble ions and small solutes is so rapid that all of
these diffuse with ease between the interior and exte-
Also present in the endothelial cells are many
minute
surface of the cell by imbibing small packets of plasma
lated that some of these vesicles coalesce to form
all the way through the endothelial
probably have proved that these vesicular forms of
Organs.
have special characteristics to meet the peculiar needs
follows:
brain
allow only extremely small molecules such as
liver
that almost all dissolved substances of the plasma,
gastrointestinal capillary
membranes are midway between those of the
glomerular tufts of the kidney
small oval windows called fenestrae penetrate all
the way through the middle of the endothelial
molecular and ionic substances (but not the large
molecules of the plasma proteins) can filter through
the glomeruli without having to pass through the
Flow of Blood in the
Blood usually does not flow continuously through the
vasomotion,
which means intermittent contraction of the metarte-
rioles and precapillary sphincters (and sometimes
even the very small arterioles as well).
found thus far to affect the degree of opening and
closing of the metarterioles and precapillary sphinc-
ters is the concentration of
Preferential channel
Metarteriole
Arteriole
Venule
Precapillary
sphincter
True capillaries
Jr., Foundation, 1950.)
BW: Factors Regulating Blood Pressure. New York: Josiah Macy,
Structure of the mesenteric capillary bed. (Redrawn from Zweifach
Figure 16–1
Endothelial
cell
Plasmalemmal
vesicles
Vesicular
channel??
Basement
membrane
Intercellular
cleft
that most water-soluble substances diffuse through the capillary
intercellular cleft
Structure of the capillary wall. Note especially the
Figure 16–2
at the junction between adjacent endothelial cells; it is believed
membrane along the clefts.
Therefore, the permeability of the capillary pores for
ions, glucose, and urea, have intermediate diameters.
pores. Other substances, such as sodium ions, chloride
pores. Conversely, the diameters of plasma protein
ter of the water molecule, which is the smallest
pores, 6 to 7 nanometers, is about 20 times the diame-
The width of the capillary intercellular cleft-
capillary.
That is, the water of the plasma is exchanged with
which plasma itself flows linearly along the capillary
rate at which water molecules diffuse through the cap-
of the rapidity with which these substances diffuse,
stances through these cleft-pores. To give one an idea
tremendous diffusion of water and water-soluble sub-
intercellular clefts between the endothelial cells, the
. Despite the fact that not more than 1/1000 of
, and
chloride ions
themselves,
the endothelial cells; such substances include
Through Intercellular “Pores” in the Capillary Membrane.
Water-Soluble, Non-Lipid-Soluble Substances Diffuse Only
go only through the pores.
substances, such as sodium ions and glucose that can
meate all areas of the capillary membrane, their rates
. Because these substances can per-
carbon dioxide
oxygen
through the pores. Such substances include
lipid soluble, it can diffuse directly through the cell
Membranes of the Capillary Endothelium.
tion and then another, bouncing randomly in every
, the
forth through the capillary wall, providing continual
lumen of the capillary, tremendous numbers of water
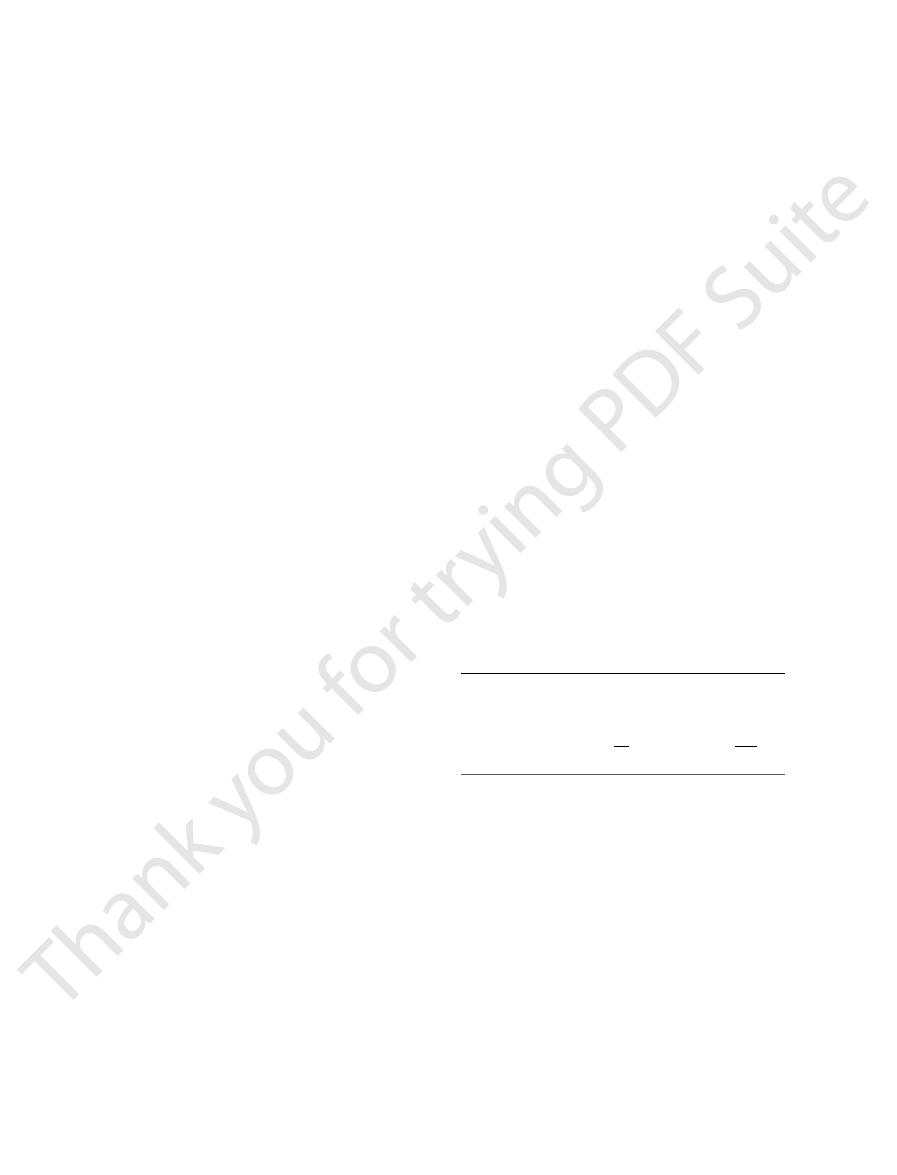
process, showing that as the blood flows along the
. Figure 16–3 demonstrates this
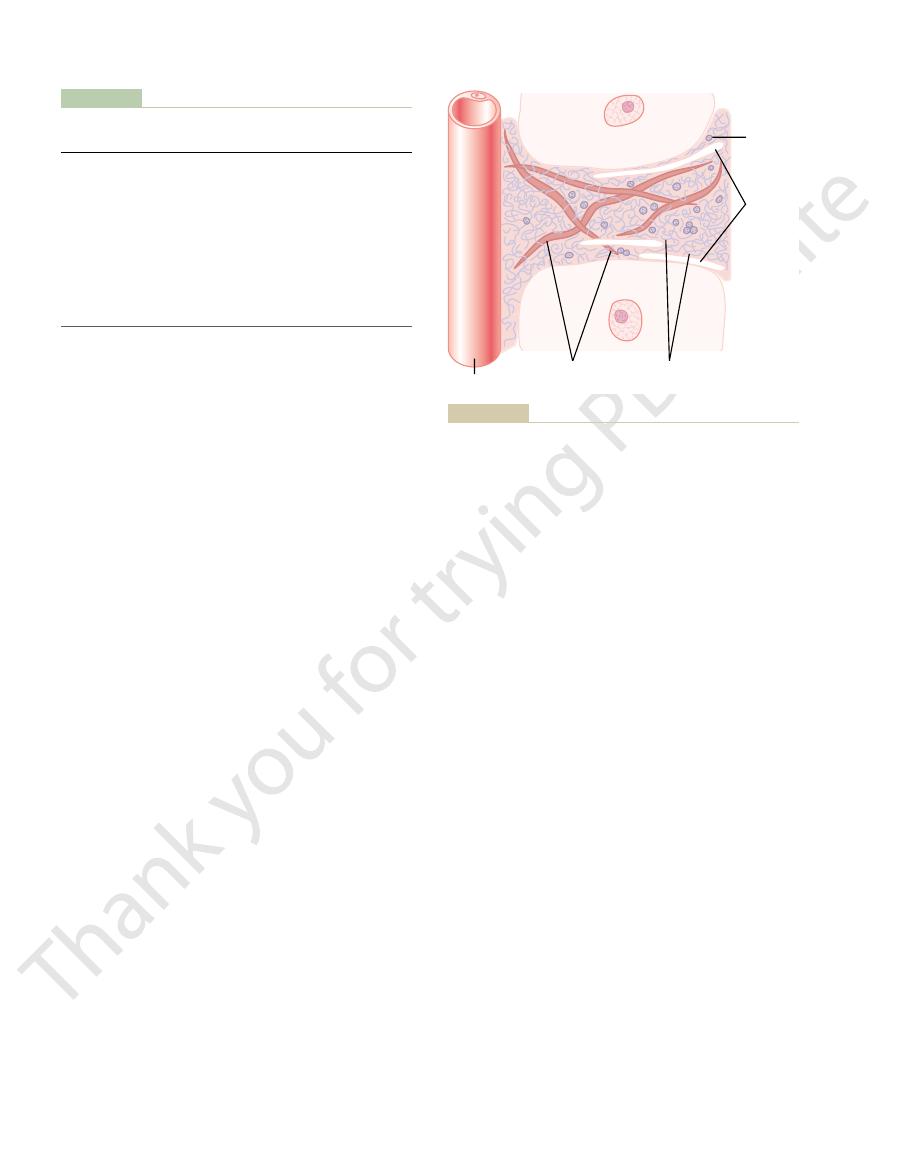
Exchange of Water, Nutrients,
response to local conditions in the tissues.
individual capillaries, each operating intermittently in
tions are, in reality, the functions of literally billions of
chapter, we will be concerned with these averages,
surrounding interstitial fluid. In the remainder of this
within the capillaries, and an
each tissue capillary bed, an
average rate of blood flow
That is, there is an
is intermittent, so many capillaries are present in the
Average Function of the
ple other factors that control local tissue blood flow, is
nutrients) to the tissues. This effect, along with multi-
lasts longer, thereby allowing the capillary blood to
more often, and the duration of each period of flow
The Microcirculation and the Lymphatic System
Chapter 16
183
the rate of oxygen usage by the tissue is great so that
tissue oxygen concentration decreases below normal,
the intermittent periods of capillary blood flow occur
carry increased quantities of oxygen (as well as other
discussed in Chapter 17.
Capillary System
Despite the fact that blood flow through each capillary
tissues that their overall function becomes averaged.
through
average capillary pressure
average rate of transfer of
substances between the blood of the capillaries and the
although one must remember that the average func-
and Other Substances
Between the Blood and
Interstitial Fluid
Diffusion Through the
Capillary Membrane
By far the most important means by which substances
are transferred between the plasma and the interstitial
fluid is diffusion
molecules and dissolved particles diffuse back and
mixing between the interstitial fluid and the plasma.
Diffusion results from thermal motion of the water
molecules and dissolved substances in the fluid
different molecules and ions moving first in one direc-
direction.
Lipid-Soluble Substances Can Diffuse Directly Through the Cell
If a substance is
membranes of the capillary without having to go
and
of transport through the capillary membrane are
many times faster than the rates for lipid-insoluble
Many substances needed by the tissues are soluble in
water but cannot pass through the lipid membranes of
water
molecules
sodium ions,
glucose
the surface area of the capillaries is represented by the
velocity of thermal molecular motion in the clefts is so
great that even this small area is sufficient to allow
the
illary membrane is about 80 times as great as the rate at
.
the water of the interstitial fluid 80 times before the
plasma can flow the entire distance through the
Effect of Molecular Size on Passage Through the
Pores.
molecule that normally passes through the capillary
molecules are slightly greater than the width of the
Arterial end
Venous end
Blood capillary
Lymphatic
capillary
the capillary and interstitial fluid spaces.
Diffusion of fluid molecules and dissolved substances between
Figure 16–3
protein. These molecules are so thin that they can
of the tissues. The proteoglycan filaments, however, are
tances in the interstitium. They are extremely strong
The collagen fiber bundles extend long dis-
ments.
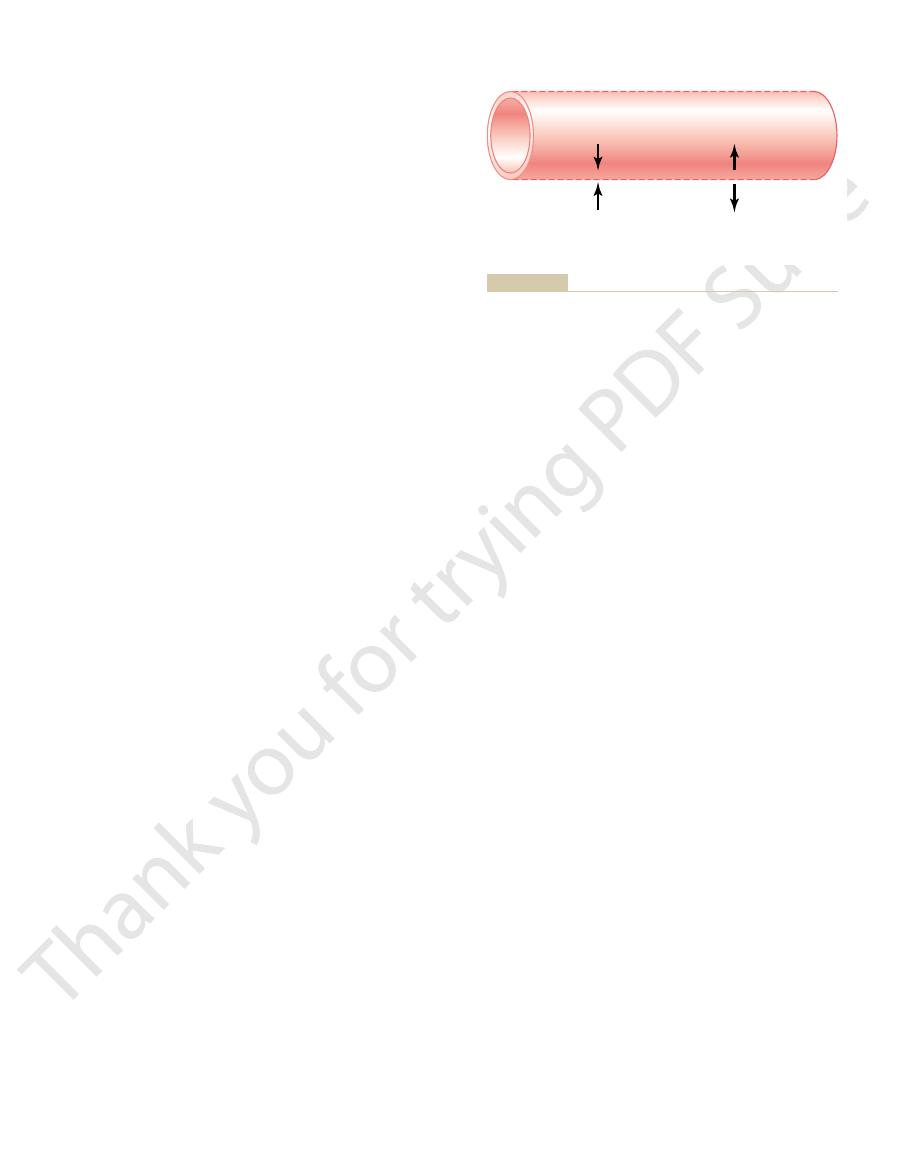
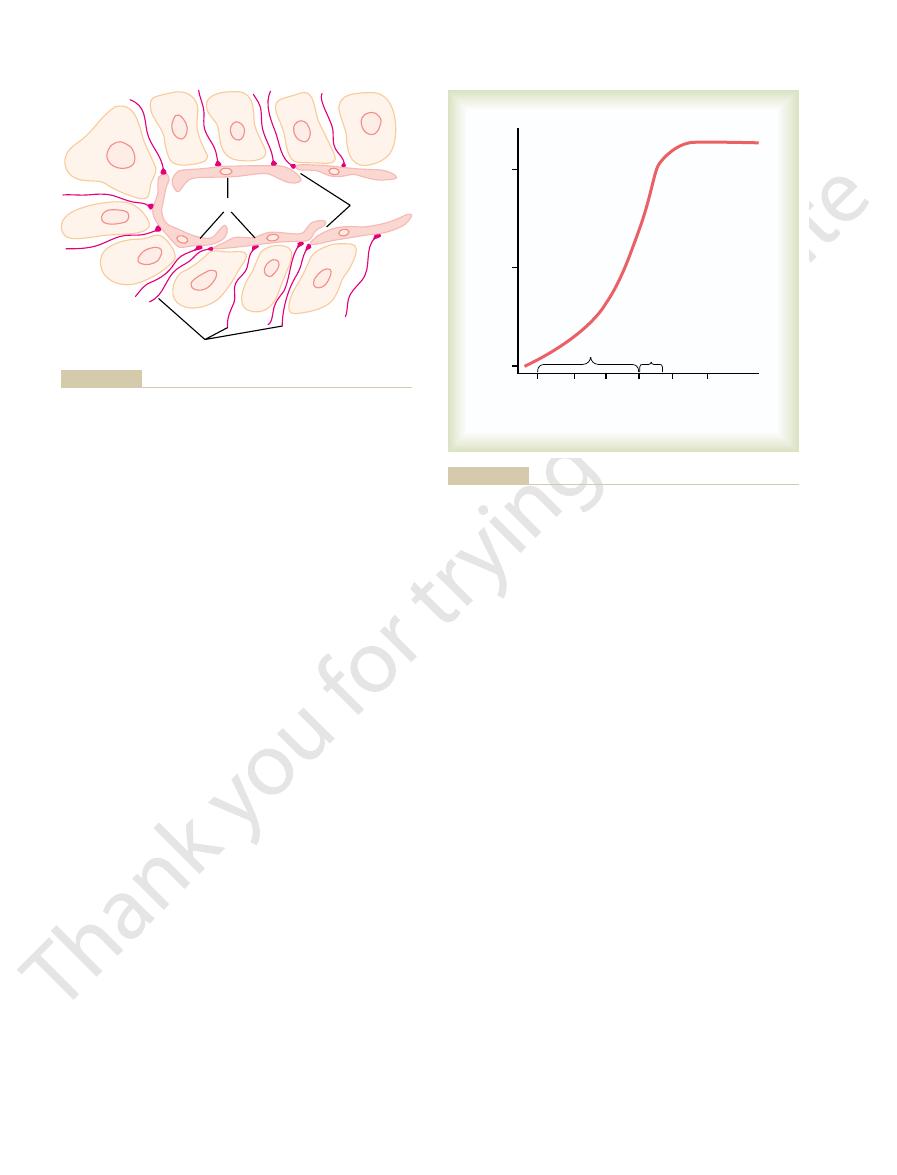
16–4. It contains two major types of solid structures:
The structure of the interstitium is shown in Figure
The fluid in these spaces is the
sists of spaces between cells, which collectively are
during very active states of the body.
blood, yet this slight difference causes enough oxygen
the plasma and interstitial fluid. For instance, the con-
The rates of diffusion through the capillary mem-
the tissues.
than in the blood, which causes excess carbon dioxide
from the blood toward the tissues. Conversely, the con-
Therefore, large quantities of oxygen normally move
instance, the concentration of oxygen in capillary
stance in one direction through the membrane. For
membrane, the greater the net movement of the sub-
between the two sides of the membrane. That is, the
The “net” rate of diffu-
Through the Capillary Membrane.
of large quantities of fluid for formation of urine.
parenchymal cells, and the kidneys to allow filtration
liver, for instance—require greater degrees of capillary
this text, it should become clear why some tissues—the
organs. When we study these different organs later in
permeabilities are very slight, as in other tissues and
true for the plasma proteins; for these, the capillary
permeability of the muscle capillaries, but this is not
Also, the permeability of the renal glomerular mem-
walls, almost as easily as water and other substances.
ferences in their permeabilities. For instance, the mem-
The capillaries in different tissues have extreme dif-
for water molecules.
albumin molecules is very, very slight, only 1/1000 that
for water molecules, whereas the permeability for
monly encountered, demonstrating, for instance, that
Table 16–1 gives the relative permeabilities of the
lar diameters.
184
Unit IV
The Circulation
different substances varies according to their molecu-
capillary pores in skeletal muscle for substances com-
the permeability for glucose molecules is 0.6 times that
A word of caution must be issued at this point.
brane of the liver capillary sinusoids is so permeable
that even plasma proteins pass freely through these
brane for water and electrolytes is about 500 times the
permeability than others to transfer tremendous
amounts of nutrients between the blood and liver
Effect of Concentration Difference on Net Rate of Diffusion
sion of a substance through any membrane is propor-
tional to the concentration difference of the substance
greater the difference between the concentrations of
any given substance on the two sides of the capillary
blood is normally greater than in the interstitial fluid.
centration of carbon dioxide is greater in the tissues
to move into the blood and to be carried away from
branes of most nutritionally important substances are
so great that only slight concentration differences
suffice to cause more than adequate transport between
centration of oxygen in the interstitial fluid immedi-
ately outside the capillary is no more than a few per
cent less than its concentration in the plasma of the
to move from the blood into the interstitial spaces to
provide all the oxygen required for tissue metabolism,
often as much as several liters of oxygen per minute
The Interstitium and
Interstitial Fluid
About one sixth of the total volume of the body con-
called the interstitium.
interstitial fluid.
(1) collagen fiber bundles and (2) proteoglycan fila-
and therefore provide most of the tensional strength
extremely thin coiled or twisted molecules composed
of about 98 per cent hyaluronic acid and 2 per cent
never be seen with a light microscope and are difficult
Relative Permeability of Skeletal Muscle Capillary Pores to
Table 16–1
Albumin
69,000
0.001
Hemoglobin
68,000
0.01
Myoglobin
17,600
0.03
Inulin
5,000
0.2
Sucrose
342
0.4
Glucose
180
0.6
Urea
60
0.8
NaCl
58.5
0.96
Water
18
1.00
Substance
Molecular Weight
Permeability
Different-Sized Molecules
Physiol Rev 33:387, 1953.
Data from Pappenheimer JR: Passage of molecules through capillary walls.
Free fluid
vesicles
Rivulets
of free
fluid
Proteoglycan
filaments
Collagen fiber
bundles
Capillary
occasionally also occur.
vesicles and small amounts of free fluid in the form of rivulets
where in the spaces between the collagen fiber bundles. Free fluid
Structure of the interstitium. Proteoglycan filaments are every-
Figure 16–4
organs. The rate of fluid filtration in a tissue is also
normal conditions, resulting in a net filtration of fluid
As discussed later, the NFP is slightly positive under
tial spaces into the capillaries. The net filtration pres-
from the intersti-
capillaries. If the sum of the Starling forces is negative,
is positive, there will be a net
If the sum of these forces, the
through the capillary membrane.
outward
4. The
through the capillary membrane.
inward
p), which tends to cause osmosis of fluid
3. The capillary
Pif is negative.
inward
(Pif), which tends
2. The
through the capillary membrane.
outward
(Pc), which tends to force
1. The
who first demonstrated their importance, are:
called “Starling forces” in honor of the physiologist
stitial fluid or in the opposite direction. These forces,
Figure
Fluid Movement Through the Capillary Membrane.
Four Primary Hydrostatic and Colloid Osmotic Forces Determine
interstitial spaces. In the remainder of this chapter, we
, which
spaces.
into the blood. This osmotic pressure exerted by
colloid osmotic pressure
capillary pores into the interstitial spaces. Conversely,
The hydrostatic pressure in the capillaries tends to
Capillary Filtration Coefficient
Osmotic Pressures, and
by Hydrostatic and Colloid
Capillaries Is Determined
Fluid Filtration Across
fluid independent of the proteoglycan filaments.
edema, these small pockets
is slight, usually much less than 1 per cent. Conversely,
The amount of “free” fluid present in
faces of cells.
through the interstitium in the small rivulets, usually
into the circulating blood, it often can be seen to flow
and therefore can flow freely. When a dye is injected
are also present, which
rivulets of “free” fluid
the tissue gel, occasionally small
excreta, oxygen, carbon dioxide, and so forth.
electrolytes, small molecular weight nutrients, cellular
cells, this diffusion allows rapid transport through the
cent as rapidly as it does through free fluid. For the
large numbers of molecules moving together.
to another by kinetic, thermal motion rather than by
that is, it moves molecule by molecule from one place
it mainly diffuses
tissue gel. Instead,
difficult for fluid to flow
ments, it is
proteoglycan filaments. This combination of proteo-
pores of the capillaries with ease. The interstitial fluid
derived by filtration and diffusion from the capillaries.
The fluid in the interstitium is
aments aptly described as a “brush pile.”
Nevertheless, they form a mat of very fine reticular fil-
to demonstrate even with the electron microscope.
The Microcirculation and the Lymphatic System
Chapter 16
185
“Gel” in the Interstitium.
It contains almost the same constituents as plasma
except for much lower concentrations of proteins
because proteins do not pass outward through the
is entrapped mainly in the minute spaces among the
glycan filaments and fluid entrapped within them has
the characteristics of a gel and therefore is called tissue
gel.
Because of the large number of proteoglycan fila-
easily through the
through the gel;
Diffusion through the gel occurs about 95 to 99 per
short distances between the capillaries and the tissue
interstitium not only of water molecules but also of
“Free” Fluid in the Interstitium.
Although almost all the
fluid in the interstitium normally is entrapped within
and small free fluid vesicles
means fluid that is free of the proteoglycan molecules
coursing along the surfaces of collagen fibers or sur-
normal tissues
when the tissues develop
and rivulets of free fluid expand tremendously until one
half or more of the edema fluid becomes freely flowing
force fluid and its dissolved substances through the
osmotic pressure caused by the plasma proteins
(called
) tends to cause fluid
movement by osmosis from the interstitial spaces
the plasma proteins normally prevents significant loss
of fluid volume from the blood into the interstitial
Also important is the lymphatic system
returns to the circulation the small amounts of excess
protein and fluid that leak from the blood into the
discuss the mechanisms that control capillary filtration
and lymph flow function together to regulate the
respective volumes of the plasma and the interstitial
fluid.
16–5 shows the four primary forces that determine
whether fluid will move out of the blood into the inter-
capillary pressure
fluid
interstitial fluid pressure
to force fluid
through the capillary
membrane when Pif is positive but outward when
plasma colloid osmotic pressure
(
P
interstitial fluid colloid osmotic pressure (
Pif),
which tends to cause osmosis of fluid
net filtration pressure,
fluid filtration across the
there will be a net fluid absorption
sure (NFP) is calculated as:
across the capillaries into the interstitial space in most
determined by the number and size of the pores in
each capillary as well as the number of capillaries in
N
=
-
-
+
FP
Pc
Pif
p
if
P
P
Capillary
pressure
(Pc)
Plasma colloid
osmotic pressure
(
P
p)
Interstitial
fluid pressure
(Pif)
Interstitial fluid
colloid osmotic pressure
(
P
if)
inward through the membrane pores.
capillary membrane, tending to move fluid either outward or
Fluid pressure and colloid osmotic pressure forces operate at the
Figure 16–5
maneuvers; otherwise, either
at this same level of 17 mm Hg throughout these
Therefore, the capillary pressure must have remained
venous lines meet each other at a value of 17 mm Hg.
nullify all weight changes are shown. The arterial and
gure, the
and (2) increasing the venous pressure.
words, the capillary pressure is kept constant while
effect of decreasing the arterial pressure. In other
To prevent this weight decrease, the venous pressure
gut wall and makes the weight of the gut decrease. This
arterial pressure is decreased, the resulting decrease in
through the blood vessels of the gut wall. When the
one arm of a gravimetric balance. Blood is perfused
pressure. This
Figure 16
Capillary Pressure.
Hg in the middle.
10 to 15 mm Hg in the venous ends, and about 25 mm
30 to 40 mm Hg in the arterial ends of the capillaries,
humans. These measurements have given pressures of
micromanometer system. Using this method, capillary
illary, and the pressure is measured by an appropriate
measure pressure in a capillary by cannulation, a
Micropipette Method for Measuring Capillary Pressure.
averaging about 17 mm Hg.
, which has given a capillary pressure
mm Hg, and (2)
, which has
mate the capillary hydrostatic pressure: (1)
Two experimental methods have been used to esti-
The rate of capillary
ltration pressure.
NFP and is usually expressed as ml/min per mm Hg
). The K
owing. These factors are usually
186
Unit IV
The Circulation
which blood is fl
expressed together as the capillary filtration coefficient
(K
f
f
is therefore a measure of the capacity of
the capillary membranes to filter water for a given
net fi
fluid filtration is therefore
determined as:
In the following sections we discuss in detail each
of the forces that determine the rate of capillary fluid
filtration.
Capillary Hydrostatic Pressure
direct
micropipette cannulation of the capillaries
given an average mean capillary pressure of about 25
indirect functional measurement of the
capillary pressure
To
microscopic glass pipette is thrust directly into the cap-
pressures have been measured in capillaries of
exposed tissues of animals and in large capillary loops
of the eponychium at the base of the fingernail in
Isogravimetric Method for Indirectly Measuring “Functional”
–6 demonstrates an iso-
gravimetric method for indirectly estimating capillary
figure shows a section of gut held up by
capillary pressure allows the osmotic pressure of the
plasma proteins to cause absorption of fluid out of the
immediately causes displacement of the balance arm.
is increased an amount sufficient to overcome the
simultaneously (1) decreasing the arterial pressure
In the graph in the lower part of the fi
changes in arterial and venous pressures that exactly
filtration or absorption of
Filtration
K
NFP
f
=
¥
give higher pressure values. The most important
averages about 17 mm Hg.
the isogravimetric method. Therefore, one is justi
is the normal state, the average functional capillary
out of the capillaries. Because such a balance of forces
same capillary pressure. However, the isogravimetric
Why Is the Functional Capillary Pressure Lower than Capillary
pressure is measured to be about 17 mm Hg.
Thus, in a roundabout way, the
fluid through the capillary walls would have occurred.
“functional” capillary
Pressure Measured by the Micropipette Method?
It is clear
that the aforementioned two methods do not give the
method determines the capillary pressure that exactly
balances all the forces tending to move fluid into or
pressure must be close to the pressure measured by
fied
in believing that the true functional capillary pressure
It is easy to explain why the cannulation methods
reason is that these measurements usually are made
in capillaries whose arterial ends are open and when
100
50
Arterial pressure
Gut
100
80
60
Pressure 40
20
0
Capillary pressure
= 17 mm Hg
Arterial
Venous
Arterial pressure – venous pressure
0
Venous pressure
Isogravimetric method for measuring capillary pressure.
Figure 16–6
pressure. The importance of these observations is
cause no more than about 2 mm Hg of positive
interstitial space, when injected into these areas,
scrotum. Amounts of
the lower eyelid, in the axillary space, and in the
into loose subcutaneous tissues, such as beneath
2. Less than 1 mm Hg of positive pressure is
the skin back into the concavity.
pull it away from the concavity. Nevertheless,
attempts to shorten, with the result that it tends to
collect underneath the graft. Also, the skin
removal of the eye, before the skin becomes
of the body, such as in an eye socket after
1. When a skin graft is placed on a concave surface
uid pressure was always positive. Some of the per-
The concept that the interstitial
Is the True Interstitial Fluid Pressure in Loose
tissue.
which is considered to be zero pressure, one might for-
pressure exerted on the skin is atmospheric pressure,
6 mm Hg. Thus, if one remembers that the
13 mm Hg, whereas the
Hg. In the kidneys, the capsular pressure surrounding
6 mm
10 mm Hg, whereas the
their encasements. For instance, the cerebrospinal
pressures are usually positive. However, these intersti-
method used for measurement, the interstitial
around the eye. In most of these, regardless of the
brous sheaths around the muscles, and the sclera
brous capsule around the kidney, the
brain, the strong
encasements, such as the cranial vault around the
Interstitial Fluid Pressures in Tightly
3 mm Hg.
negative, usually measuring
usual manometric means. Pressures measured by this
uid pressure into the Te
protruding from its end. The cotton
tissue a small Te
Measurement of Interstitial Free Fluid Pressure by Means of a
measured by the micropipette in Figure 16-7.
2 mm Hg
6 mm Hg, but with smaller capsules,
slightly less than atmospheric pressure.
tissues, such as skin, that are
2 mm Hg, giving average
ment for making such measurements, more recent pres-
slightly positive. With experience and improved equip-
2 mm Hg but were usually
The
interstitium. Therefore, the pressure that is measured is
of the micropipette is about 1 micrometer in diameter,
uid pressure. The tip
The same type of micropipette used for
cotton wick inserted into the tissue.
capsules, and (3) measurement of the pressure from a
nulation of the tissues with a micropipette, (2) meas-
. The
ters of mercury less than atmospheric pressure, that is,
uid pressure, and each of these gives slightly differ-
As is true for the measurement of capillary pressure,
the functional capillary pressure to a lower value.
rial capillaries. Both of these effects further decrease
the venules than to the arterioles. Second, the venous
nulation. First, there are far more capillaries nearer to
There are two other reasons why the functional cap-
pressure in the arterial ends.
over a period of time, one would expect the
laries, about 10 mm Hg. Therefore, when averaged
of the vasomotion cycle. When closed, the pressure in
owing into the capillary. However, it
The Microcirculation and the Lymphatic System
Chapter 16
187
blood is actively fl
should be recalled from the earlier discussion of cap-
illary vasomotion that the metarterioles and precapil-
lary sphincters normally are closed during a large part
the capillaries beyond the closures should be almost
equal to the pressure at the venous ends of the capil-
functional
mean capillary pressure to be much nearer to the pres-
sure in the venous ends of the capillaries than to the
illary pressure is less than the values measured by can-
capillaries are several times as permeable as the arte-
Interstitial Fluid Hydrostatic Pressure
there are several methods for measuring interstitial
fl
ent values but usually values that are a few millime-
values called negative interstitial fluid pressure
methods most widely used have been (1) direct can-
urement of the pressure from implanted perforated
Measurement of Interstitial Fluid Pressure Using the
Micropipette.
measuring capillary pressure can also be used in some
tissues for measuring interstitial fl
but even this is 20 or more times larger than the sizes
of the spaces between the proteoglycan filaments of the
probably the pressure in a free fluid pocket.
first pressures measured using the micropipette
method ranged from
-1 to +
sures have averaged about
-
pressure values in loose
Measurement of Interstitial Free Fluid Pressure in Implanted Per-
forated Hollow Capsules.
Interstitial free fluid pressure
measured by this method when using 2-centimeter
diameter capsules in normal loose subcutaneous tissue
averages about
-
the values are not greatly different from the
-
Cotton Wick.
Still another method is to insert into a
flon tube with about eight cotton fibers
fibers form a “wick”
that makes excellent contact with the tissue fluids and
transmits interstitial fl
flon tube:
the pressure can then be measured from the tube by
technique in loose subcutaneous tissue also have been
-1 to -
Encased Tissues
Some tissues of the body are surrounded by tight
fi
fi
fluid
tial fluid pressures almost invariably are still less than
the pressures exerted on the outsides of the tissues by
fluid
pressure surrounding the brain of an animal lying on
its side averages about
+
brain
interstitial fluid pressure averages about
+4 to +
the kidney averages about
+
reported renal interstitial fluid pressures have averaged
about
+
mulate a general rule that the normal interstitial fluid
pressure is usually several millimeters of mercury neg-
ative with respect to the pressure that surrounds each
Subcutaneous Tissue Subatmospheric?
fluid pressure is sub-
atmospheric in many if not most tissues of the body
began with clinical observations that could not be
explained by the previously held concept that intersti-
tial fl
tinent observations are the following:
attached to the sublying socket, fluid tends to
some negative force underneath the skin causes
absorption of the fluid and usually literally pulls
required to inject tremendous volumes of fluid
fluid calculated to be more
than 100 times the amount of fluid normally in the
that they show that such tissues do not have
mass, the following chart gives both the relative mass
rather than by the mass of these molecules. Therefore,
as 1 gram of albumin, and 1 gram of
brinogen, 400,000. Thus,
69,000; globulins, 140,000; and
tains albumin, with an average molecular weight of
The plasma proteins are a mixture that con-
caused by sodium, potassium, and the other cations
that is, extra osmotic pressure
molecular effects of the dissolved protein and 9 mm by
averages about 28 mm Hg; 19 mm of this is caused by
The
Normal Values for Plasma Colloid Osmotic Pressure.
The
oncotic pressure.
that which occurs at the cell membrane, it is called
membrane. To distinguish this osmotic pressure from
through the capillary pores, it is the proteins of the
able membrane exert osmotic pressure. Because the
basic discussion of osmotic pressure in Chapter 4, it
spaces.
This overall process creates the slight negative pres-
uid enters the terminal lymphatic capillaries,
and other matter from the tissue spaces. Normally,
uid, excess protein molecules, debris,
The lymphatic system is a
uid pressure.
The lymphatic system is discussed later in the chapter,
Fluid Pressure
Pumping by the Lymphatic System Is the
3 mm Hg.
tissue is slightly less subatmospheric, averaging about
uid pressure, there currently
Pressure in Loose Subcutaneous Tissue.
Summary—An Average Value for Negative Interstitial Fluid
pressure.
uid from the tissue spaces. It
surrounding tissue space, or (3) when a highly
or decreased, (2) when
dynamic changes in this pressure. The changes are
4. The implanted capsule for measuring the
6 mm Hg
6 mm Hg
Joint synovial spaces:
8 mm Hg
have been measured have been negative. Some of
uids, the pressures that
3. In most natural cavities of the body where there
uid pressure system, must be available
uid. Therefore, some other mechanism, such as a
188
Unit IV
The Circulation
strong fibers that can prevent the accumulation of
fl
negative fl
to prevent such fluid accumulation.
is free fluid in dynamic equilibrium with the
surrounding interstitial fl
these are the following:
Intrapleural space:
-
-
4 to
-
Epidural space:
-
4 to
-
interstitial fluid pressure can be used to record
approximately those that one would calculate to
occur (1) when the arterial pressure is increased
fluid is injected into the
concentrated colloid osmotic agent is injected into
the blood to absorb fl
is not likely that these dynamic changes could be
recorded this accurately unless the capsule
pressure closely approximated the true interstitial
Although the
aforementioned different methods give slightly differ-
ent values for interstitial fl
is a general belief among most physiologists that the
true interstitial fluid pressure in loose subcutaneous
-
Basic Cause of the Negative Interstitial
but we need to understand here the basic role that this
system plays in determining interstitial fl
“scavenger” system that
removes excess fl
when fl
the lymph vessel walls automatically contract for a few
seconds and pump the fluid into the blood circulation.
sure that has been measured for fluid in the interstitial
Plasma Colloid Osmotic Pressure
Proteins in the Plasma Cause Colloid Osmotic Pressure.
In the
was pointed out that only those molecules or ions that
fail to pass through the pores of a semiperme-
proteins are the only dissolved constituents in the
plasma and interstitial fluids that do not readily pass
plasma and interstitial fluids that are responsible for
the osmotic pressures on the two sides of the capillary
either colloid osmotic pressure or
term “colloid” osmotic pressure is derived from the
fact that a protein solution resembles a colloidal solu-
tion despite the fact that it is actually a true molecu-
lar solution.
colloid osmotic pressure of normal human plasma
the Donnan effect—
held in the plasma by the proteins.
Effect of the Different Plasma Proteins on Colloid Osmotic
Pressure.
fi
1 gram of globulin contains only half as many molecules
fibrinogen contains
only one sixth as many molecules as 1 gram of albumin.
It should be recalled from the discussion of osmotic
pressure in Chapter 4 that osmotic pressure is deter-
mined by the number of molecules dissolved in a fluid
when corrected for number of molecules rather than
concentrations (g/dl) of the different types of proteins
in normal plasma and their respective contributions to
the total plasma colloid osmotic pressure (
Pp).
Globulins
2.5
6.0
Albumin
4.5
21.8
p (mm Hg)
g/dl
P
Fibrinogen
0.3
0.2
the total quantity of protein in the plasma itself, but
The total quantity of protein in the entire 12 liters
interstitial spaces.
not true of all the pores. Therefore, small amounts of
than the molecular sizes of the plasma proteins, this is
uid dynamics, it is mainly
brinogen. Therefore, from the point of view
tion, 20 per cent from the globulins, and almost none
Thus, about 80 per cent of the total colloid osmotic
Total
7.3
28.0
pressure of the plasma results from the albumin frac-
from the fi
of capillary and tissue fl
albumin that is important.
Interstitial Fluid Colloid
Osmotic Pressure
Although the size of the usual capillary pore is smaller
plasma proteins do leak through the pores into the
of interstitial fluid of the body is slightly greater than
of the capillary. This calculates to be 17.3 mm Hg.
rial and venous capillaries are averaged to calculate
ling equilibrium. For this chart, the pressures in the arte-
The following chart shows the principles of the Star-
that is eventually returned by way of the lymphatics.
circulation by absorption. The slight disequilibrium
exists at the capillary membrane. That is, the amount
under normal conditions, a state of near-equilibrium
E. H. Starling pointed out over a century ago that
The remaining one tenth
the capillaries to be reabsorbed at the venous ends.
The reabsorption pressure causes about nine tenths
capillaries, so that less reabsorption pressure is
ends, but remember that the venous capillaries are
capillaries. This reabsorption pressure is considerably
reabsorption, 21 mm Hg. The difference, 7 mm Hg, is
capillary, 28 mm Hg, is greater than that opposing
Thus, the force that causes
The low blood pressure at the venous end of the cap-
Analysis of Reabsorption at the Venous End of the Capillary.
through the capillaries.
average, about 1/200 of the plasma in the
ltration pressure causes, on the
This 13 mm Hg
lary pores.
Hg, tending to move
of 13 mm
Thus, the summation of forces at the arterial end of
The approximate average forces operative
the Capillary.
are as follows.
illaries to the venous ends. The dynamics of this
ies. Thus, a small amount of
out of the capillaries at their arterial ends, but at their
venous ends. Because of this difference,
of the capillaries is 15 to 25 mm Hg greater than at the
The average capillary pressure at the arterial ends
discussed, it is possible to put all these together to
Exchange of Fluid Volume Through
this concentration of proteins is about 8 mm Hg.
or about 3 g/dl. Quantitatively, one
plasma, the average protein
The Microcirculation and the Lymphatic System
Chapter 16
189
because this volume is four times the volume of
concentration of the inter-
stitial fluid is usually only 40 per cent of that in plasma,
finds that the
average interstitial fluid colloid osmotic pressure for
the Capillary Membrane
Now that the different factors affecting fluid move-
ment through the capillary membrane have been
see how the capillary system maintains normal fluid
volume distribution between the plasma and the inter-
stitial fluid.
fluid “filters”
venous ends fluid is reabsorbed back into the capillar-
fluid actually “flows”
through the tissues from the arterial ends of the cap-
flow
Analysis of the Forces Causing Filtration at the Arterial End of
at the arterial end of the capillary that cause movement
through the capillary membrane are shown as follows:
the capillary shows a net filtration pressure
fluid outward through the capil-
fi
flowing blood
to filter out of the arterial ends of the capillaries into
the interstitial spaces each time the blood passes
illary changes the balance of forces in favor of absorp-
tion as follows:
fluid to move into the
the net reabsorption pressure at the venous ends of the
less than the filtration pressure at the capillary arterial
more numerous and more permeable than the arterial
required to cause inward movement of fluid.
of the fluid that has filtered out of the arterial ends of
flows into the lymph vessels
and returns to the circulating blood.
Starling Equilibrium for
Capillary Exchange
of fluid filtering outward from the arterial ends of cap-
illaries equals almost exactly the fluid returned to the
that does occur accounts for the small amount of fluid
mean functional capillary pressure for the entire length
uid pressure
3
Capillary pressure (arterial end of capillary)
30
mm Hg
Forces tending to move fluid outward:
Negative interstitial free fl
total outward force
uid colloid osmotic pressure
8
Interstitial fl
41
Forces tending to move fluid inward:
Outward
41
total inward force
Plasma colloid osmotic pressure
28
28
Summation of forces:
Inward
28
)
13
at arterial end
net outward force (
Forces tending to move fluid inward:
mm Hg
uid pressure
3
Capillary pressure (venous end of capillary)
10
Forces tending to move fluid outward:
total inward force
Plasma colloid osmotic pressure
28
28
Negative interstitial free fl
Inward
28
total outward force
uid colloid osmotic pressure
8
Interstitial fl
21
Summation of forces:
Outward
21
net inward force
7
uid pressure
3.0
Mean capillary pressure
17.3
mm Hg
Mean forces tending to move fluid outward:
Negative interstitial free fl
Mean force tending to move fluid inward:
total outward force
uid colloid osmotic pressure
8.0
Interstitial fl
28.3
Outward
28.3
total inward force
Plasma colloid osmotic pressure
28.0
28.0
Summation of mean forces:
Inward
28.0
net outward force
0.3
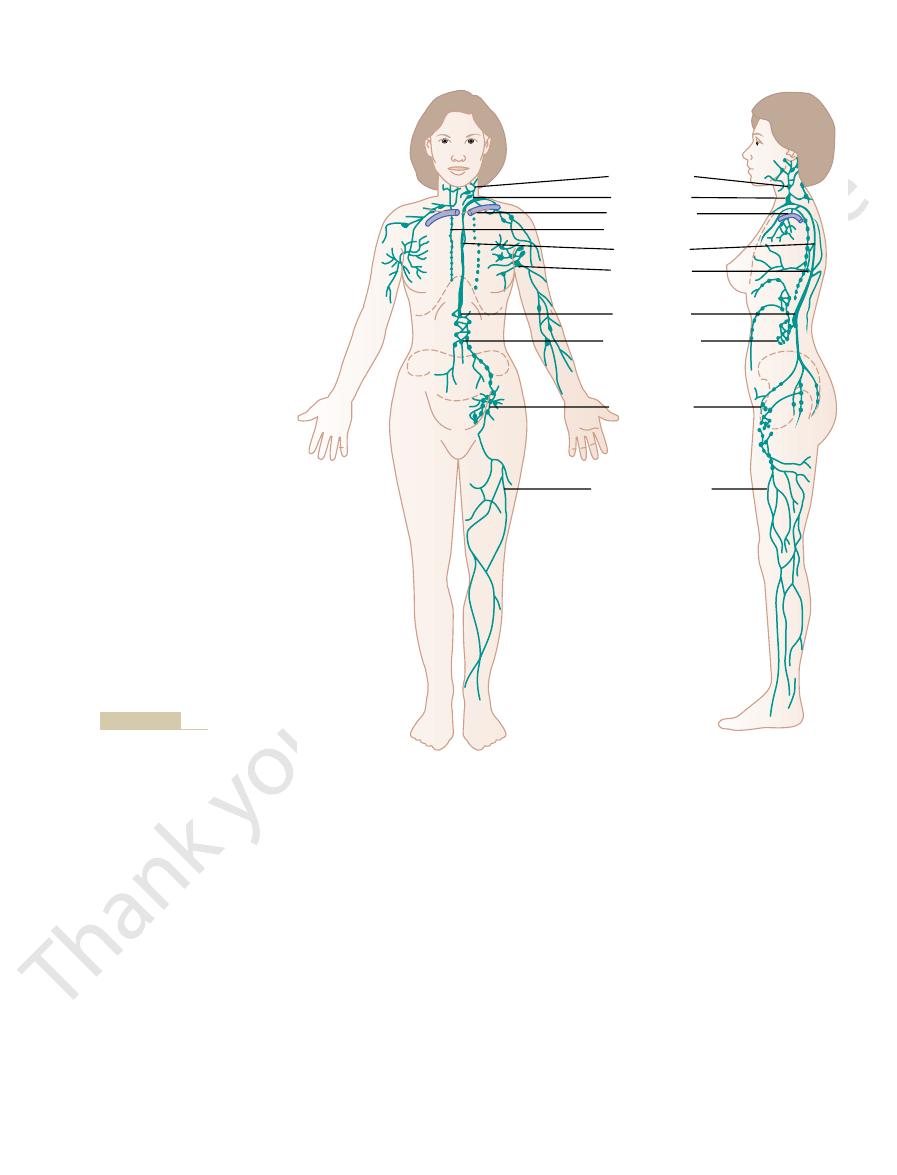
Terminal Lymphatic Capillaries and Their Permeability.
(much smaller than the thoracic duct), which
right arm, and parts of the right thorax enters the
Lymph from the right side of the neck and head, the
before it empties into the veins.
Lymph from the left side of the head, the left arm, and
clavian vein, as shown in Figure 16
case of the brain, into the cerebrospinal
tually empties either into lymphatic vessels or, in the
ow; this
of muscles, and the bones. But, even these tissues have
of the skin, the central nervous system, the endomysium
spaces. The exceptions include the super
Lymph Channels of the Body
which we would die within about 24 hours.
laries. This return of proteins to the blood from the
from the tissue spaces, neither of which can be
spaces into the blood. Most important, the lymphatics
The lymphatic system represents an accessory route
Lymphatic System
These effects of imbalance at the capillary membrane
uid volume.
ltration, and the blood volume will
Conversely, if the capillary pressure falls very low,
to accumulate in the interstitial spaces, and edema will
lymphatics to carry away. As a result,
system, an amount that is 2 to 5 times too much for the
stitial spaces as normally occurs. To prevent accumu-
sure from 0.3 mm Hg to 20.3 mm Hg, which results in
tissue spaces rises. Thus, a 20 mm Hg rise in mean cap-
If the mean capillary pressure rises above 17 mm Hg,
at the Capillary Membrane
Effect of Abnormal Imbalance of Forces
6 g/dl.
taneous tissue, 2 g/dl; in intestine, 4 g/dl; and in liver,
uid of muscles is about 1.5 g/dl; in subcu-
greatly as well. The concentration of protein in the
or wide open. By the same token, the permeation
in the intestine, and extreme in the liver and glomeru-
muscle, moderately large in subcutaneous tissue, large
different tissues. It is very small in both brain and
abilities of the capillary systems in different tissues,
tissue. But, because of extreme differences in perme-
average tissue is about 0.01 ml/min/mm Hg/100 g of
of tissue. On this basis, the
The
mercury for the entire body. This is called the whole
of mercury imbalance, one
body of 2 ml/min. Expressing this for each millimeter
of 0.3 mm Hg causes net
In the above example, an average
about 2 milliliters per minute.
returned to the circulation through the lymphatics. The
, and it is the
spaces than reabsorption.This slight excess of
This slight imbalance of forces, 0.3 mm Hg, causes
28.3 mm Hg, and the total inward force, 28.0 mm Hg.
near-equilibrium between the total outward forces,
Thus, for the total capillary circulation, we
190
Unit IV
The Circulation
find a
slightly more filtration of fluid into the interstitial
filtration
is called net filtration
fluid that must be
normal rate of net filtration in the entire body is only
Filtration Coefficient.
net imbalance of forces at the capillary membranes
fluid filtration in the entire
finds a net filtration rate
of 6.67 milliliters of fluid per minute per millimeter of
body capillary filtration coefficient.
filtration coefficient can also be expressed for
separate parts of the body in terms of rate of filtration
per minute per millimeter of mercury per 100 grams
filtration coefficient of the
this coefficient varies more than 100-fold among the
lus of the kidney where the pores are either numerous
of proteins through the capillary membranes varies
interstitial fl
the net force tending to cause filtration of fluid into the
illary pressure causes an increase in net filtration pres-
68 times as much net filtration of fluid into the inter-
lation of excess fluid in these spaces would require 68
times the normal flow of fluid into the lymphatic
fluid will begin
result.
net reabsorption of fluid into the capillaries will occur
instead of net fi
increase at the expense of the interstitial fl
in relation to the development of different kinds of
edema are discussed in Chapter 25.
through which fluid can flow from the interstitial
can carry proteins and large particulate matter away
removed by absorption directly into the blood capil-
interstitial spaces is an essential function without
Almost all tissues of the body have special lymph chan-
nels that drain excess fluid directly from the interstitial
ficial portions
minute interstitial channels called prelymphatics
through which interstitial fluid can fl
fluid even-
fluid and then
directly back into the blood.
Essentially all the lymph vessels from the lower part
of the body eventually empty into the thoracic duct,
which in turn empties into the blood venous system at
the juncture of the left internal jugular vein and left sub-
–8.
parts of the chest region also enters the thoracic duct
right
lymph duct
empties into the blood venous system at the juncture of
the right subclavian vein and internal jugular vein.
Most
of the fluid filtering from the arterial ends of blood
Fluid filled cavity
To
measure
pressure
Skin
Implanted
capsule
Blood
vessels
pressure.
Perforated capsule method for measuring interstitial fluid
FIGURE 16–7
the lymphatics. Therefore, lymph as it
Lymph is derived from interstitial
Formation of Lymph
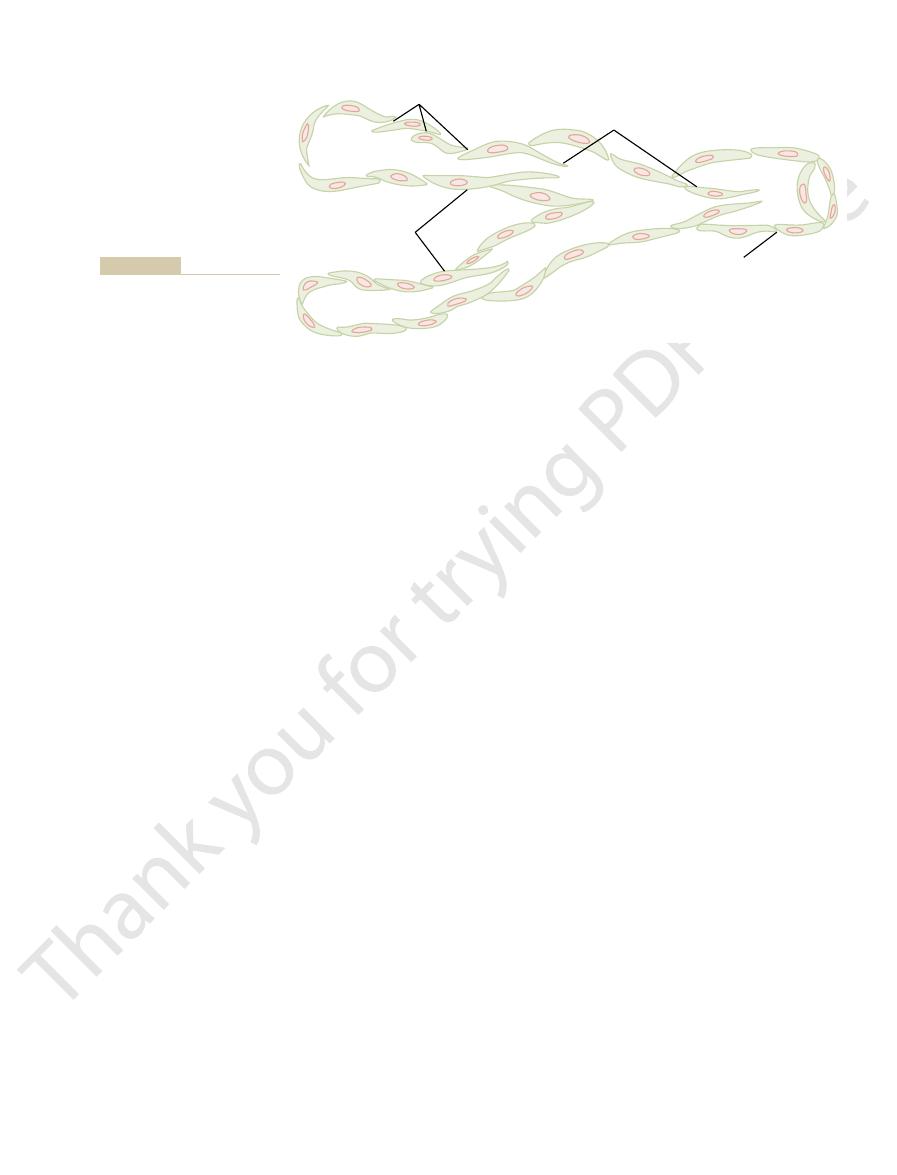
Thus, the lymphatics have valves at the very tips of the
ap valve.
ow directly into the lymphatic capillary. But
along with its suspended particles, can push the valve
interior of the lymphatic capillary. Interstitial
inward, thus forming a minute valve that opens to the
junctions of adjacent endothelial cells, the edge of one
to the surrounding connective tissue. At the
anchoring fila-
9. This
Figure 16
structure of the lymphatic capillaries, demonstrated in
almost unimpeded. The reason for this is a special
cannot be absorbed from the tissues in any other way,
stances of high molecular weight, such as proteins,
The
this lymph is normally only 2 to 3 liters each day.
through the venous capillaries. The total quantity of all
but on the average, about 1/10 of the
The Microcirculation and the Lymphatic System
Chapter 16
191
capillaries flows among the cells and finally is reab-
sorbed back into the venous ends of the blood capil-
laries;
fluid
instead enters the lymphatic capillaries and returns to
the blood through the lymphatic system rather than
fluid that returns to the circulation by way of
the lymphatics is extremely important because sub-
although they can enter the lymphatic capillaries
–
figure shows the endothelial cells of
the lymphatic capillary attached by
ments
endothelial cell overlaps the edge of the adjacent cell
in such a way that the overlapping edge is free to flap
fluid,
open and fl
this fluid has difficulty leaving the capillary once it has
entered because any backflow closes the fl
terminal lymphatic capillaries as well as valves along
their larger vessels up to the point where they empty
into the blood circulation.
fluid that flows into
first enters the
terminal lymphatics has almost the same composition
as the interstitial fluid.
Cervical nodes
Sentinel node
Subclavian vein
R. lymphatic duct
Thoracic duct
Axillary nodes
Cisterna chyli
Abdominal nodes
Inguinal nodes
Peripheral lymphatics
Lymphatic system.
FIGURE 16–8
lymph channels; typical valves are shown in Figure
Valves exist in all
Lymphatic Pump Increases Lymph Flow.
plateau in Figure 16
This is illustrated by the upper level
ow rate.
factors balance each other almost exactly, so that
ow. At the higher pressures, these two
outside surfaces of the larger lymphatics, thus imped-
sures. This results from the fact that the increasing
than atmospheric pressure (greater than 0 mm Hg),
However, note in Figure 16
at the same time.
uid pressure, and lymph
volume, interstitial
into the interstitium, thus increasing interstitial
vessels are functioning normally. Such factors include
20-fold. Therefore, any factor that increases interstitial
6 mm Hg. Then, as the pressure rises to 0 mm
ow as measured in dog legs.
Figure
Effect of Interstitial Fluid Pressure on Lymph Flow.
per day.
each hour through other channels, making a total esti-
of a resting human, and approxi-
Rate of Lymph Flow
As the lymph passes through the lymph nodes, these
Finally, even large particles, such as bacteria, can
meal, thoracic duct lymph sometimes contains as much
food, as discussed in Chapter 65. Indeed, after a fatty
tract, especially for absorption of virtually all fats in
The lymphatic system is also one of the major routes
concentration of 3 to 5 g/dl.
lymph from all areas of the body, usually has a protein
tines, the thoracic duct lymph, which is a mixture of
high as 3 to 4 g/dl. Because about two thirds of all
protein concentration as high as 6 g/dl, and lymph
this value. Conversely, lymph formed in the liver has a
most tissues averages about 2 g/dl, and the protein con-
The protein concentration in the interstitial
192
Unit IV
The Circulation
fluid of
centration of lymph flowing from these tissues is near
formed in the intestines has a protein concentration as
lymph normally is derived from the liver and intes-
for absorption of nutrients from the gastrointestinal
as 1 to 2 per cent fat.
push their way between the endothelial cells of the
lymphatic capillaries and in this way enter the lymph.
particles are almost entirely removed and destroyed,
as discussed in Chapter 33.
About 100 milliliters per hour of lymph flows through
the thoracic duct
mately another 20 milliliters flows into the circulation
mated lymph flow of about 120 ml/hr or 2 to 3 liters
16–10 shows the effect of different levels of interstitial
fluid pressure on lymph fl
Note that normal lymph flow is very little at intersti-
tial fluid pressures more negative than the normal
value of
-
Hg (atmospheric pressure), flow increases more than
fluid pressure also increases lymph flow if the lymph
the following:
∑ Elevated capillary pressure
∑ Decreased plasma colloid osmotic pressure
∑ Increased interstitial fluid colloid osmotic pressure
∑ Increased permeability of the capillaries
All of these cause a balance of fluid exchange at the
blood capillary membrane to favor fluid movement
fluid
fl
flow all
–10 that when the inter-
stitial fluid pressure becomes 1 or 2 millimeters greater
lymph flow fails to rise any further at still higher pres-
tissue pressure not only increases entry of fluid into
the lymphatic capillaries but also compresses the
ing lymph fl
lymph flow reaches what is called the “maximum
lymph fl
”
–10.
Endothelial cells
Anchoring filaments
Valves
Special structure of the lymphatic capillaries that permits passage
FIGURE 16–9
of substances of high molecular weight into the lymph.
Relative lymph flow
0
2
4
2
0
–2
–4
–6
4
P
T
(mm Hg)
2 times/
mm Hg
7 times/
mm Hg
(0 mm Hg). (Courtesy Drs. Harry Gibson and Aubrey Taylor.)
, rises slightly above atmospheric pressure
interstitial pressure, P
leg of a dog. Note that lymph flow reaches a maximum when the
Relation between interstitial fluid pressure and lymph flow in the
FIGURE 16–10
T
First, remember that small amounts of proteins
uid pressure.
uid, and (3) the interstitial
uids, (2) the volume of
tissue spaces. Therefore, the lymphatic system also
Volume, and Interstitial Fluid Pressure
Concentration, Interstitial Fluid
Role of the Lymphatic System in
of lymph flow is determined by the product of intersti-
pump. Therefore, one can state that, roughly,
above discussion, one can see that the two primary
From the
Summary of Factors That Determine Lymph Flow.
lymphatics.
vessels also contract rhythmically. Therefore, it is
some animal tissues (e.g., the bat
laments. In
The lymphatic capillary endothelial cells also
the cell junctions.
Therefore, the pressure pushes the lymph forward into
ping edges of the endothelial cells to close like valves.
Then, when the tissue is compressed, the pressure
through the junctions between the endothelial cells.
laments pull on the wall of the lymphatic capillary,
the tissue and causes the tissue to swell, the anchoring
laments. Therefore, each time excess
As explained earlier in the chapter, the walls of the
the lymph pumping by the larger lymph vessels.
lary is also capable of pumping lymph, in addition to
The terminal lymphatic capil-
Lymphatic Capillary Pump.
almost zero.
versely, during periods of rest, lymph
ow 10- to 30-fold. Con-
cise, often increasing lymph
The lymphatic pump becomes very active during exer-
In order of their importance, such factors are:
compresses the lymph vessel also can cause pumping.
vessel walls, any external factor that intermittently
of the Lymphatics.
100 mm Hg.
large lymph vessel such as the thoracic duct, this lym-
nally emptied into the blood circulation. In a very
and a few seconds later it, too, contracts, the process
lymphatic segment. This
lling of a segment causes it to contract, and the
functions as a separate automatic pump. That is, even
the vessel automatically contracts. Furthermore, each
uid, the smooth muscle in the wall of
in animals and in human beings, show that when a
Motion pictures of exposed lymph vessels, both
phatic capillaries empty.
The Microcirculation and the Lymphatic System
Chapter 16
193
16–11 in collecting lymphatics into which the lym-
collecting lymphatic or larger lymph vessel becomes
stretched with fl
segment of the lymph vessel between successive valves
slight fi
fluid is pumped through the next valve into the next
fills the subsequent segment,
continuing all along the lymph vessel until the fluid is
fi
phatic pump can generate pressures as great as 50 to
Pumping Caused by External Intermittent Compression
In addition to the pumping caused
by intrinsic intermittent contraction of the lymph
∑ Contraction of surrounding skeletal muscles
∑ Movement of the parts of the body
∑ Pulsations of arteries adjacent to the lymphatics
∑ Compression of the tissues by objects outside the
body
fl
flow is sluggish,
lymphatic capillaries are tightly adherent to the sur-
rounding tissue cells by means of their anchoring
fi
fluid enters
fi
and fluid flows into the terminal lymphatic capillary
inside the capillary increases and causes the overlap-
the collecting lymphatic instead of backward through
contain a few contractile actomyosin fi
’s wing) these fila-
ments have been observed to cause rhythmical con-
traction of the lymphatic capillaries in the same way
that many of the small blood and larger lymphatic
probable that at least part of lymph pumping results
from lymph capillary endothelial cell contraction
in addition to contraction of the larger muscular
factors that determine lymph flow are (1) the intersti-
tial fluid pressure and (2) the activity of the lymphatic
the rate
tial fluid pressure times the activity of the lymphatic
pump.
Controlling Interstitial Fluid Protein
It is already clear that the lymphatic system functions
as an “overflow mechanism” to return to the circula-
tion excess proteins and excess fluid volume from the
plays a central role in controlling (1) the concentration
of proteins in the interstitial fl
interstitial fl
fl
Let us explain how these factors interact.
leak continuously out of the blood capillaries into the
Pores
Lymphatic
capillaries
Collecting
lymphatic
Valves
Structure of lymphatic capillaries
FIGURE 16–11
and a collecting lymphatic,
showing also the lymphatic
valves.
American Physiological Society, 1984, p 467.
(eds): Handbook of Physiology. Sec. 2, Vol. IV. Bethesda:
across the microcirculation. In: Renkin EM, Michel CC
Taylor AE, Granger DN: Exchange of macromolecules
Res 39:375, 2002.
Transendothelial transport: the vesicle controversy. J Vasc
Rippe B, Rosengren BI, Carlsson O, Venturoli D:
Immunol 4:35, 2004.
Oliver G: Lymphatic vasculature development. Nat Rev
Immunol 4:360, 2004.
endothelial venules: dogmas and enigmas. Nat Rev
Miyasaka M, Tanaka T: Lymphocyte traf
Rev 79:703, 1999.
Michel CC, Curry FE: Microvascular permeability. Physiol
phia: WB Saunders Co, 1975.
II. Dynamics and Control of the Body Fluids. Philadel-
Guyton AC, Taylor AE, Granger HJ: Circulatory Physiology
Circ Res 19:412, 1966.
uid mobility.
sure: III. Its effect on resistance to tissue
Guyton AC, Scheel K, Murphree D: Interstitial
capillary wall. Circ Res 19:1022, 1966.
pressure: IV. Its effect on
Guyton AC, Prather J, Scheel K, McGehee J: Interstitial
sure. Physiol Rev 51:527, 1971.
Guyton AC, Granger HJ, Taylor AE: Interstitial
curves of interstitial space. Circ Res 16:452, 1965.
uid pressure: II. Pressure-volume
Guyton AC: Interstitial
12:399, 1963.
on pressures in implanted perforated capsules. Circ Res
Guyton AC: Concept of negative interstitial pressure based
function: current perspectives. Ann N Y Acad Sci 979:178,
Gashev AA: Physiologic aspects of lymphatic contractile
Thromb Vasc Biol 23:1161, 2003.
caveolae, and endothelial cell function. Arterioscler
Frank PG, Woodman SE, Park DS, Lisanti MP: Caveolin,
Nat Rev Mol Cell Biol 5:261, 2004.
Dejana E: Endothelial cell-cell junctions: happy together.
Kidney Int 63:809, 2003.
Amico G, Bazzi C: Pathophysiology of proteinuria.
uid volume. Physiol Rev 73:1,
Aukland K, Reed RK: Interstitial-lymphatic mechanisms in
occurs, which is discussed
pressure,
partial vacuum. When the tissues lose their negative
uid pressure, which is actually a
at these places, the tissues are held together by the
over the back of the hand or over the face. Yet even
tissues slide over one another, such as the skin sliding
even absent. This occurs particularly at points where
the body, connective tissue
bers. However, at many places in
Traditionally, it has been assumed that the different
Body Tissues Together
Pressure as a Means for Holding the
uid from the blood capillaries.
state; they will remain balanced at these steady state
interstitium from the blood capillaries. Therefore, the
uid pressure, the return of protein and
Thus, once the interstitial
mulated in the spaces.
previously. This in turn carries away the excess inter-
ow, as explained
Third, the increasing interstitial
uid pressure.
lary wall by the proteins and into the interstitium, thus
into the interstitium. Therefore, in effect,
Second, the increasing colloid osmotic pressure in
uids.
uid, and this in
ends of the blood capillaries. Therefore, these proteins
interstitium. Only minute amounts, if any, of the leaked
194
Unit IV
The Circulation
proteins return to the circulation by way of the venous
tend to accumulate in the interstitial fl
turn increases the colloid osmotic pressure of the
interstitial fl
the interstitial fluid shifts the balance of forces at the
blood capillary membranes in favor of fluid filtration
fluid is
translocated osmotically outward through the capil-
increasing both interstitial fluid volume and interstitial
fl
fluid pressure
greatly increases the rate of lymph fl
stitial fluid volume and excess protein that has accu-
fluid protein concentra-
tion reaches a certain level and causes a comparable
increase in interstitial fluid volume and interstitial
fl
fluid by way
of the lymphatic system becomes great enough to
balance exactly the rate of leakage of these into the
quantitative values of all these factors reach a steady
levels until something changes the rate of leakage of
proteins and fl
Significance of Negative Interstitial Fluid
tissues of the body are held together entirely by
connective tissue fi
fibers are very weak or
negative interstitial fl
fluid accumulates in the spaces and the
condition known as edema
in Chapter 25.
References
the control of extracellular fl
1993.
D’
2002.
fl
fluid pres-
fluid
fluid movement through the
fluid pres-
fl
ficking across high
