the capillaries open. This opening of dormant capillaries diminishes the dis-
capillaries have little or no flowing blood. But during strenuous exercise, all
During rest, some muscle
blood flow can be almost stopped, but this also causes rapid weakening of the
contraction, which causes sustained compression of the blood vessels, the
is compression of the blood vessels by the contracted muscle. During strong
The cause of the lower flow during the muscle contraction phase of exercise
seconds but then fades toward normal during the next few minutes.
At the end of the contractions, the blood flow remains very high for a few
cise. Note that the flow increases and decreases with each muscle contraction.
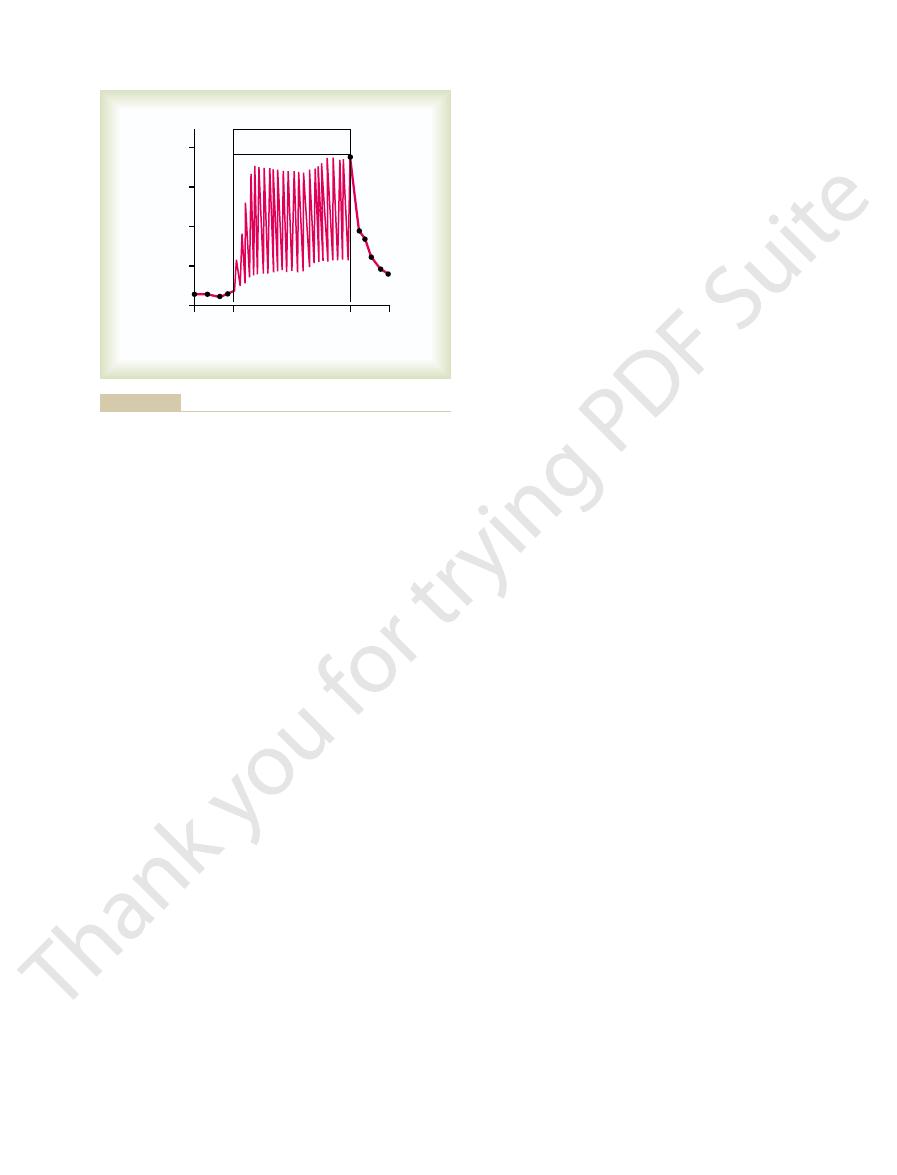
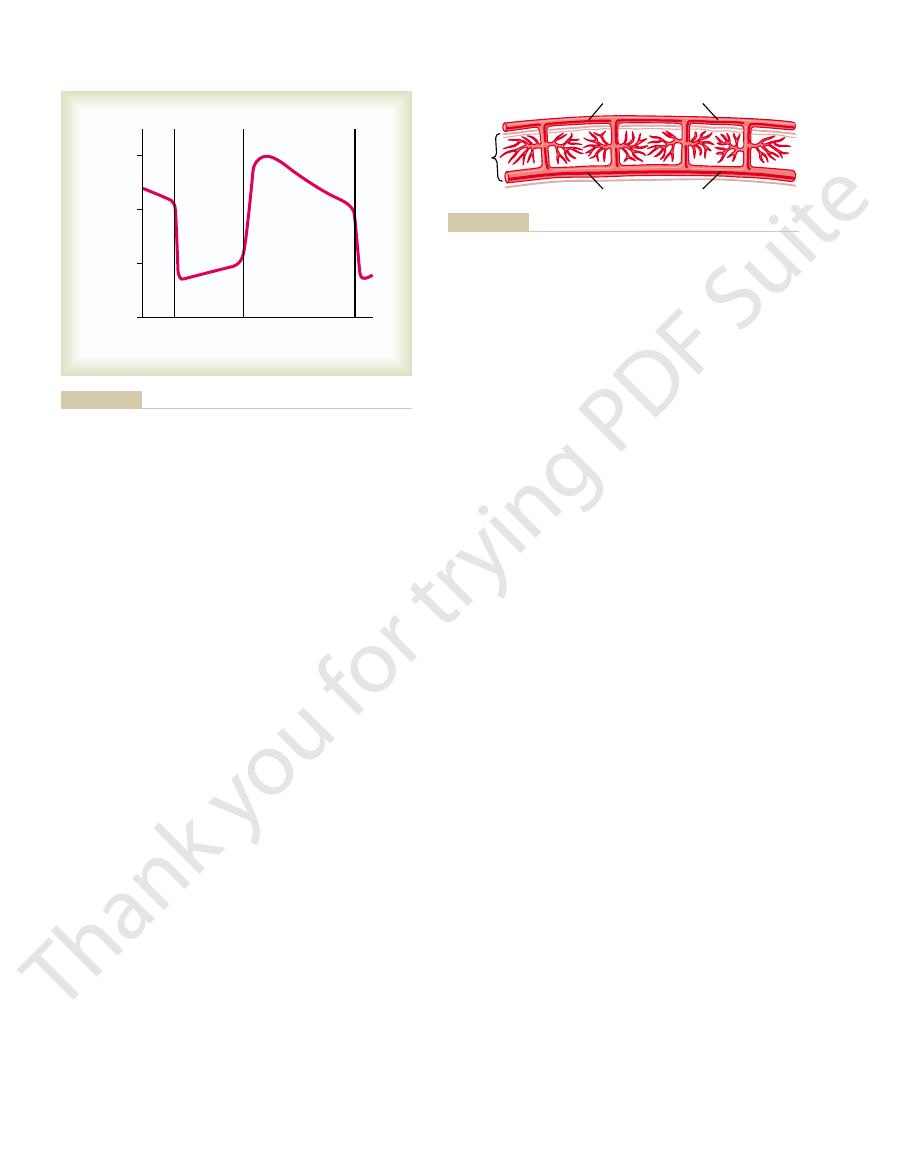
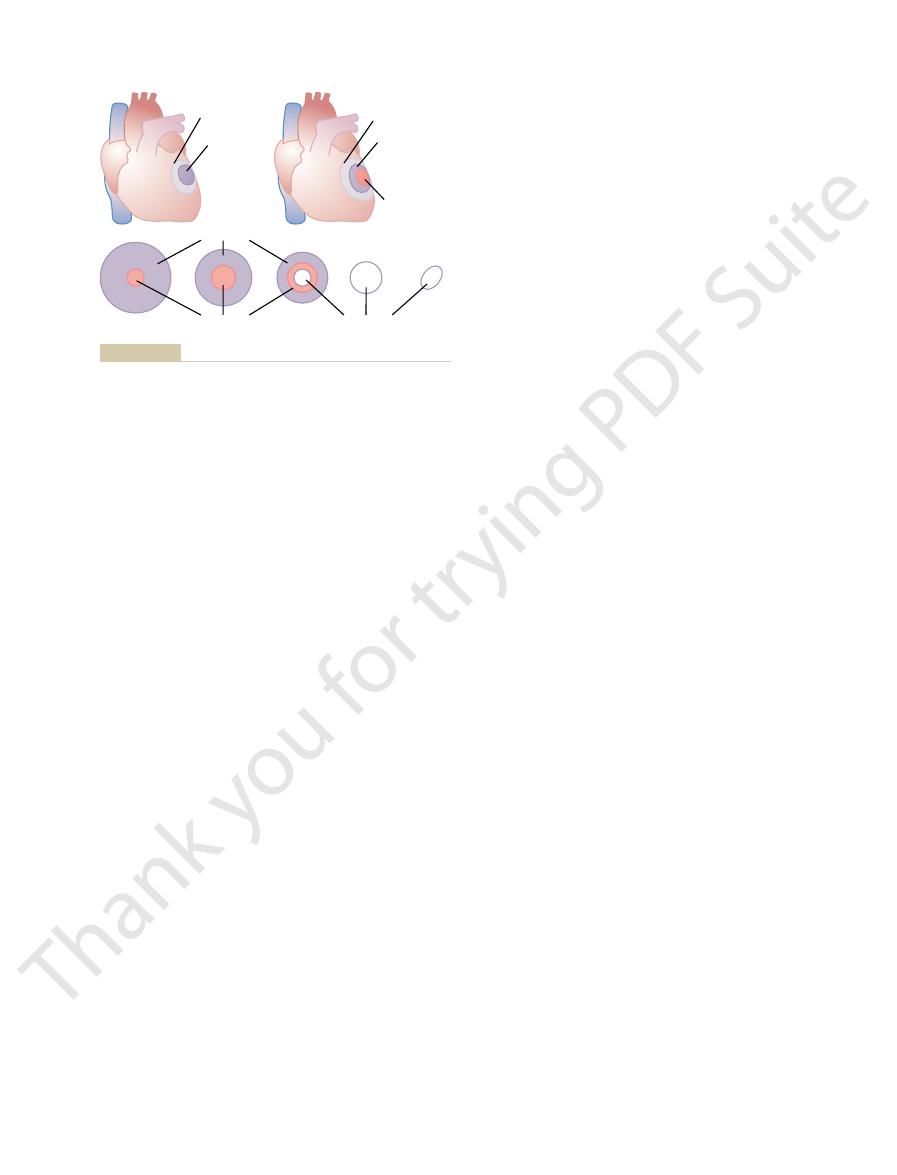
Figure 21–1 shows a record of blood flow
15- to 25-fold, rising to 50 to 80 ml/min/100 g of muscle.
in the well-conditioned athlete, this can increase
During extreme exercise
muscle.
, blood flow through skeletal muscle averages 3 to 4 ml/min/100 g of
Rate of Blood Flow Through the Muscles
normal, or in the well-trained athlete to six to seven times normal.
tal muscle in the body, all of it requiring large amounts of blood flow. Also, the
circulatory system faces. This is true because there is such a large mass of skele-
Very strenuous exercise is one of the most stressful conditions that the normal
Regulation During Exercise
acteristics of heart attacks, and (3) the pain of angina pectoris.
(1) cardiac output control during exercise, (2) char-
In addition, related subjects are discussed, such as
needs.
to the heart. Regulation of each of these is
Output During Exercise; the
C
H
A
P
T
E
R
2
1
246
Muscle Blood Flow and Cardiac
Coronary Circulation and Ischemic
Heart Disease
In this chapter we consider (1) blood flow to the
skeletal muscles and (2) coronary blood flow
achieved mainly by local control of vascular
resistance in response to muscle tissue metabolic
Blood Flow in Skeletal Muscle and Blood Flow
cardiac output often must increase in the non-athlete to four to five times
During rest
Blood Flow During Muscle Contractions.
changes in a calf muscle of a human leg during strong rhythmical muscular exer-
tetanic
contraction.
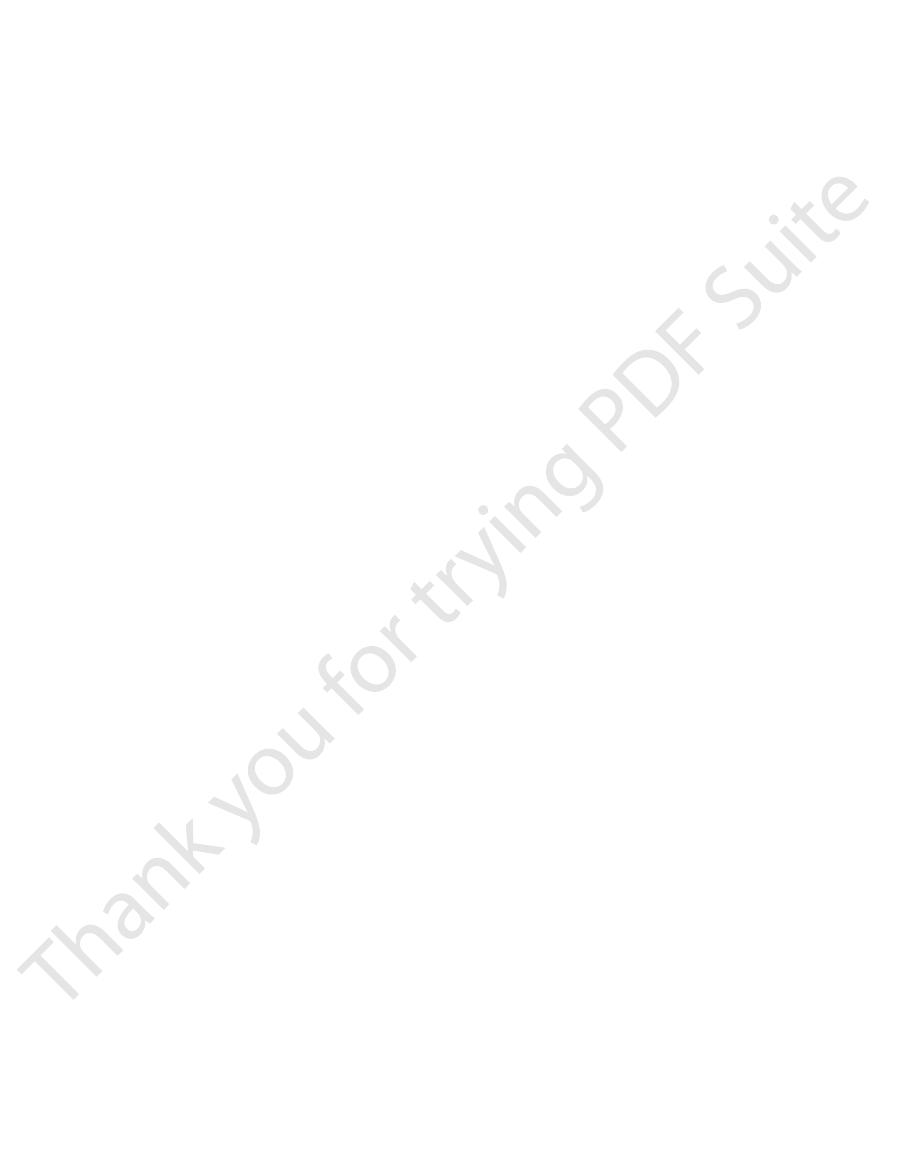
Increased Blood Flow in Muscle Capillaries During Exercise.
tance that oxygen and other nutrients must diffuse from the capillaries to the
contracting muscle fibers and sometimes contributes a twofold to threefold
increased capillary surface area through which oxygen and nutrients can diffuse
from the blood.
2 L/min of extra blood flow to the muscles, which is
supply to the muscles. This accounts for as much as
reduced, thereby temporarily “lending” their blood
muscles, while at the same time blood flow through
muscles as noted above. Thus, the heart is stimulated
arterioles in the active muscles, which are strongly
, except for the
heart are attenuated. Therefore, three major circula-
Simultaneously, the parasympathetic signals to the
tiate mass sympathetic discharge throughout the body.
At the onset of exercise, signals are transmitted not
Effects of Mass Sympathetic Discharge
arterial pressure, and (3) increase in cardiac output.
tory effects on the entire circulation, (2) increase in
tremendous blood flow required by the muscles. They
Three major effects occur during exercise that are
Total Body Circulatory Readjustments
receptors excited especially by norepinephrine. These
tor receptors, in contrast to the alpha vasoconstrictor
adrenergic receptors of the vessels, which are vasodila-
epinephrine, however, often has a slight vasodilator
caused by direct sympathetic nerve stimulation. The
cise. The circulating norepinephrine acts on the muscle
sympathetic vasoconstrictor nerve endings, the medul-
pressure.
to as little as one half to one third normal. This vaso-
at their nerve endings. When maximally activated,
The sympa-
Sympathetic Vasoconstrictor Nerves.
nerves as well.
tissue vasodilator mechanisms, skeletal muscles are
Nervous Control of Muscle Blood Flow.
and (4) carbon dioxide. We still do not know quanti-
ions, (2) adenosine triphosphate (ATP), (3) lactic acid,
exercise continues. These factors include (1) potassium
adenosine, still other vasodilator factors continue to
Fortunately, even after the muscle blood vessels
for more than about 2 hours.
sine, but experiments have shown that even large
causes release of vasodilator substances. The most
absence of oxygen and because oxygen deficiency
oxygen concentration in the tissue fluids. This in turn
the muscle uses oxygen rapidly, thereby decreasing the
in the muscle tissues. That is, during muscle activity,
on the muscle arterioles to cause dilation. One of the
The tremendous increase in muscle
Enhances Flow.
Control of Blood Flow Through the
Muscle Blood Flow and Cardiac Output During Exercise
Chapter 21
247
Skeletal Muscles
Local Regulation—Decreased Oxygen in Muscle Greatly
blood flow that occurs during skeletal muscle activity
is caused primarily by chemical effects acting directly
most important chemical effects is reduction of oxygen
causes local arteriolar vasodilation both because the
arteriolar walls cannot maintain contraction in the
important vasodilator substance is probably adeno-
amounts of adenosine infused directly into a muscle
artery cannot sustain vasodilation in skeletal muscle
have become insensitive to the vasodilator effects of
maintain increased capillary blood flow as long as the
tatively how great a role each of these plays in in-
creasing muscle blood flow during muscle activity;
this subject was discussed in additional detail in
Chapter 17.
In addition to local
provided with sympathetic vasoconstrictor nerves and
(in some species of animals) sympathetic vasodilator
thetic vasoconstrictor nerve fibers secrete norepineph-
rine
this can decrease blood flow through resting muscles
constriction is of physiologic importance in circulatory
shock and during other periods of stress when it is
necessary to maintain a normal or even high arterial
In addition to the norepinephrine secreted at the
lae of the two adrenal glands also secrete large
amounts of norepinephrine plus even more epineph-
rine into the circulating blood during strenuous exer-
vessels to cause a vasoconstrictor effect similar to that
effect because epinephrine excites more of the beta
receptors are discussed in Chapter 60.
During Exercise
essential for the circulatory system to supply the
are (1) mass discharge of the sympathetic nervous
system throughout the body with consequent stimula-
only from the brain to the muscles to cause muscle
contraction but also into the vasomotor center to ini-
tory effects result.
First, the heart is stimulated to greatly increased
heart rate and increased pumping strength as a result
of the sympathetic drive to the heart plus release of
the heart from normal parasympathetic inhibition.
Second, most of the arterioles of the peripheral
circulation are strongly contracted
vasodilated by the local vasodilator effects in the
to supply the increased blood flow required by the
most nonmuscular areas of the body is temporarily
0
10
16
18
Blood flow (100 ml
/min)
0
20
40
Minutes
Rhythmic exercise
Calf
flow
Barcroft and Dornhorst: J Physiol 109:402, 1949.)
during contractions than between contractions. (Adapted from
strong rhythmical contraction. The blood flow was much less
Effects of muscle exercise on blood flow in the calf of a leg during
Figure 21–1
easy to understand. It results almost entirely from
The increased level of the cardiac output curve is
as follow.
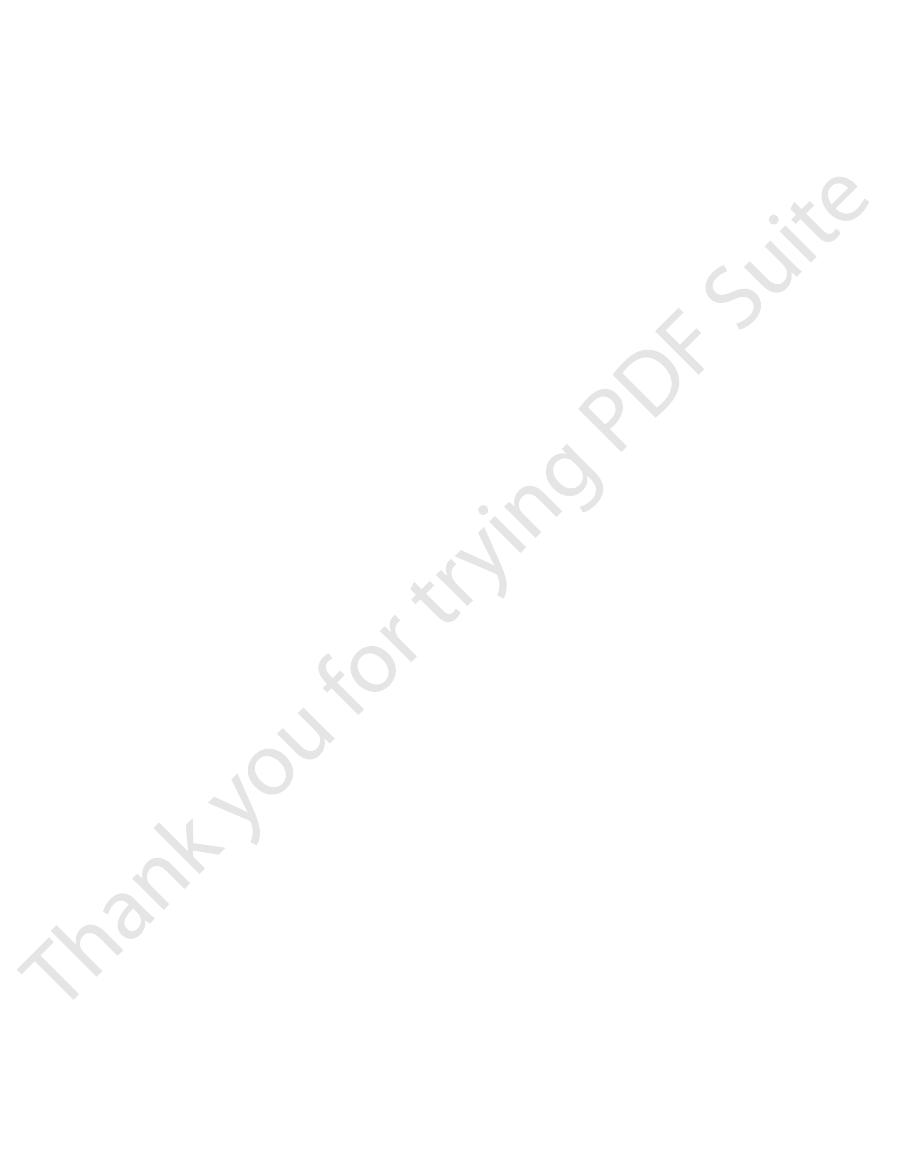
the cardiac output curve and the venous return curve,
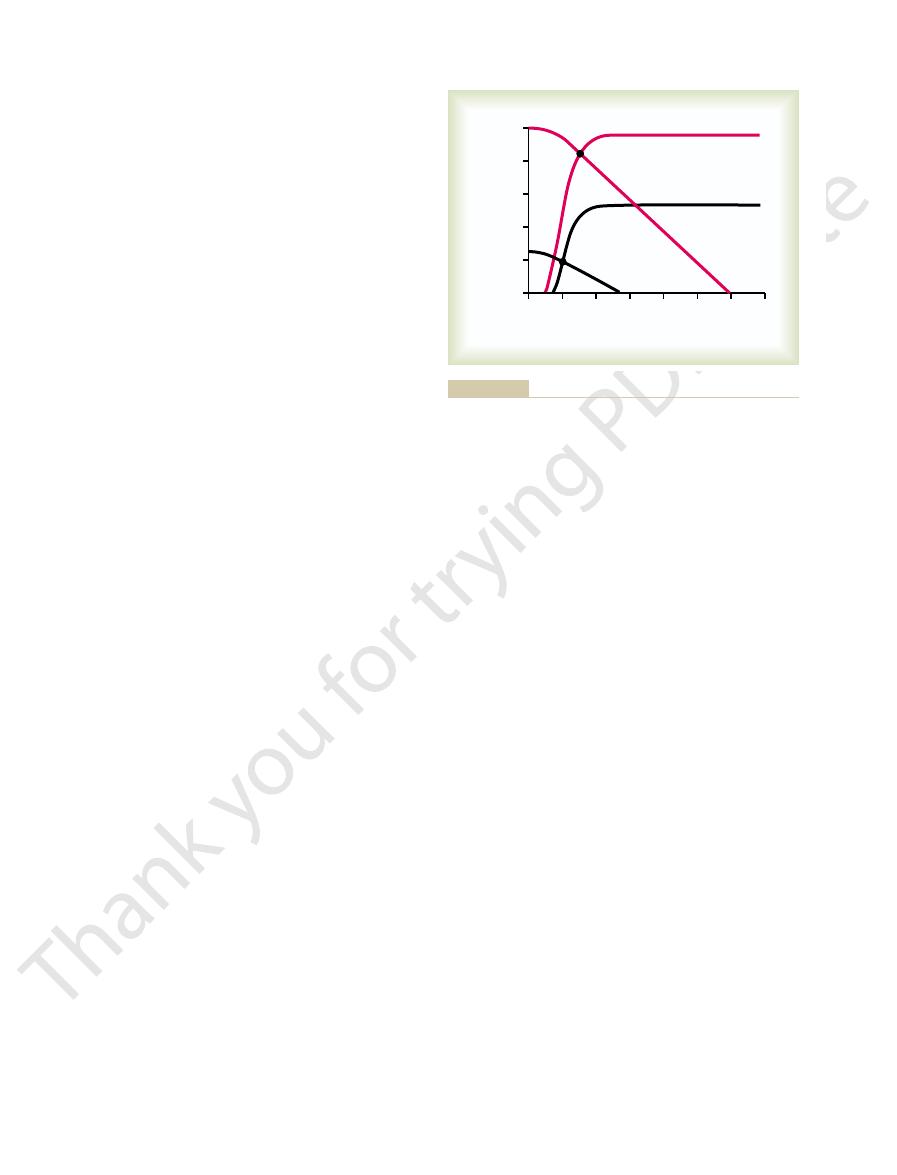
B analyze heavy exercise. Note that the great increase
the normal circulation; and the curves crossing at point
return curves crossing at point A give the analysis for
during heavy exercise. The cardiac output and venous
Figure 21–2 shows a graphical analysis
times.
work. For instance, marathon runners who can
In fact, the ability of the circulatory system to provide
approximately in proportion to the degree of exercise.
During Exercise
Importance of the Increase in Cardiac Output
this is not the only important effect; the extra pressure
to push blood through the muscle tissue vessels. But
This 30 per cent increase causes 30 per cent more force
30 per cent, a common increase during heavy exercise.
assume, for instance, that the arterial pressure rises
. Let us
arterial pressure rises during normal exercise
ratory experiment. What is the difference? Mainly,
to at least 20 L/min during maximal activity. Therefore,
than about eightfold. Yet, we know from studies of
pressure to rise, muscle blood flow seldom rises more
When muscles are stimulated maximally in a lab-
simultaneously in large masses of active muscle.
40 mm Hg. This lack of a large increase in pressure
whole-body exercise, such as running or swimming,
Conversely, when a person performs massive
above. The tenseness of the situation is obvious.
the mean arterial pressure to as high as 170 mm Hg.
the effect is mainly vasoconstriction, often increasing
vasodilation occurs, but everywhere else in the body
everywhere in the body. In the few active muscles,
muscles, the sympathetic nervous response still occurs
the exercise is performed. When a person performs
80 mm Hg, depending on the conditions under which
increase the arterial pressure during exercise. This
These effects, working together, virtually always
by the heart, and (3) a great increase in mean systemic
the active muscles, (2) increased pumping activity
effects, including (1) vasoconstriction of the arterioles
rial pressure. This results from multiple stimulatory
An Important Result of Increased
Increase in Arterial Pressure During Exercise—
venous return of blood to the heart and, therefore, in
. As we learned in Chapter 20, this is one of
, which greatly
itative areas of the circulation are contracted power-
, the muscle walls of the
Third
to exercise as are the skeletal muscles.
coronary and cerebral systems
and death. Two of the peripheral circulatory systems,
248
Unit IV
The Circulation
exceedingly important when one thinks of a person
running for his life—even a fractional increase in
running speed may make the difference between life
the
, are spared this vaso-
constrictor effect because both these circulatory areas
have poor vasoconstrictor innervation—fortunately so
because both the heart and the brain are as essential
veins and other capac-
fully
increases the mean systemic filling
pressure
the most important factors in promoting increase in
increasing the cardiac output.
Sympathetic Stimulation
One of the most important effects of increased sym-
pathetic stimulation in exercise is to increase the arte-
and small arteries in most tissues of the body except
filling pressure caused mainly by venous contraction.
increase can be as little as 20 mm Hg or as great as
exercise under tense conditions but uses only a few
Such a condition might occur in a person standing
on a ladder and nailing with a hammer on the ceiling
the increase in arterial pressure is often only 20 to
results from the extreme vasodilation that occurs
Why Is the Arterial Pressure Increase During Exercise Impor-
tant?
oratory experiment but without allowing the arterial
marathon runners that muscle blood flow can increase
from as little as 1 L/min for the whole body during rest
it is clear that muscle blood flow can increase much
more than occurs in the aforementioned simple labo-
the
also stretches the walls of the vessels so much that
muscle total flow often rises to more than 20 times
normal.
Many different physiologic effects occur at the same
time during exercise to increase cardiac output
increased cardiac output for delivery of oxygen and
other nutrients to the muscles during exercise is
equally as important as the strength of the muscles
themselves in setting the limit for continued muscle
increase their cardiac outputs the most are generally
the same persons who have record-breaking running
Graphical Analysis of the Changes in Cardiac Output During
Heavy Exercise.
of the large increase in cardiac output that occurs
in cardiac output requires significant changes in both
sympathetic stimulation of the heart that causes (1)
4
0
+4
+8
+12
+16
+20
+24
venous return (L
/min)
0
Cardiac output and
–
5
10
15
20
25
Right atrial pressure (mm Hg)
B
A
, heavy exercise.
circulation.
, normal
pressure with onset of strenuous exercise.
Graphical analysis of change in cardiac output and right atrial
Figure 21–2
Black curves
Red curves
normal arterial pressure. Consequently, the
fold, and it pumps this blood against a higher than
During strenuous exercise, the heart in the young
averages about 225 ml/min, which is about 4 to 5 per
The resting coronary blood flow in the human being
veins, which empty directly into
the coronary sinus. A very small amount of coronary
that flow directly into the right atrium, not by way of
anterior cardiac veins
75 per cent of the total coronary blood flow. And most
tricle in 80 to 90 per cent of people.
and left lateral portions of the left ventricle, whereas
The
tion is minuscule.
cardiac chambers, so that this source of muscle nutri-
receives its nutritive blood supply. Only the inner 1/10
trate from the surface into the cardiac muscle mass. It
supply. Note that the main coronary arteries lie on the
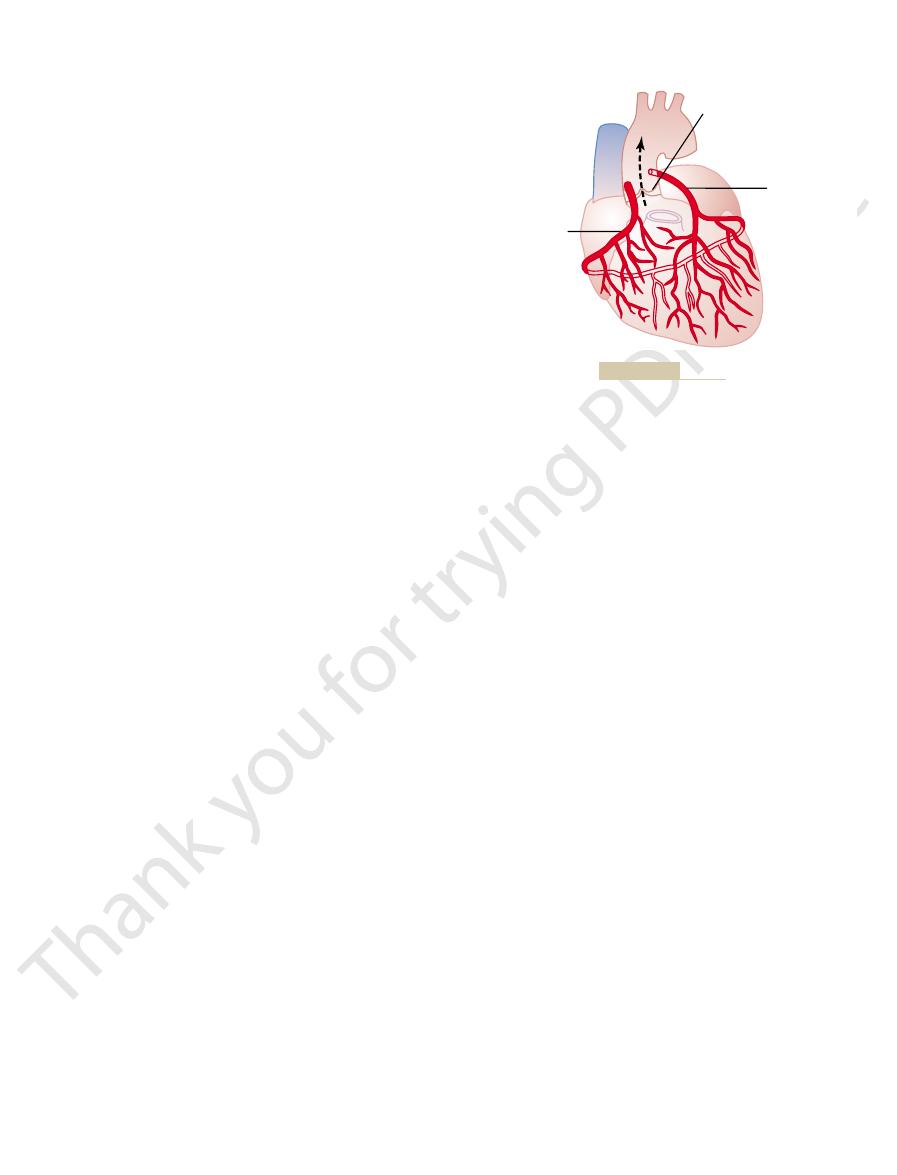
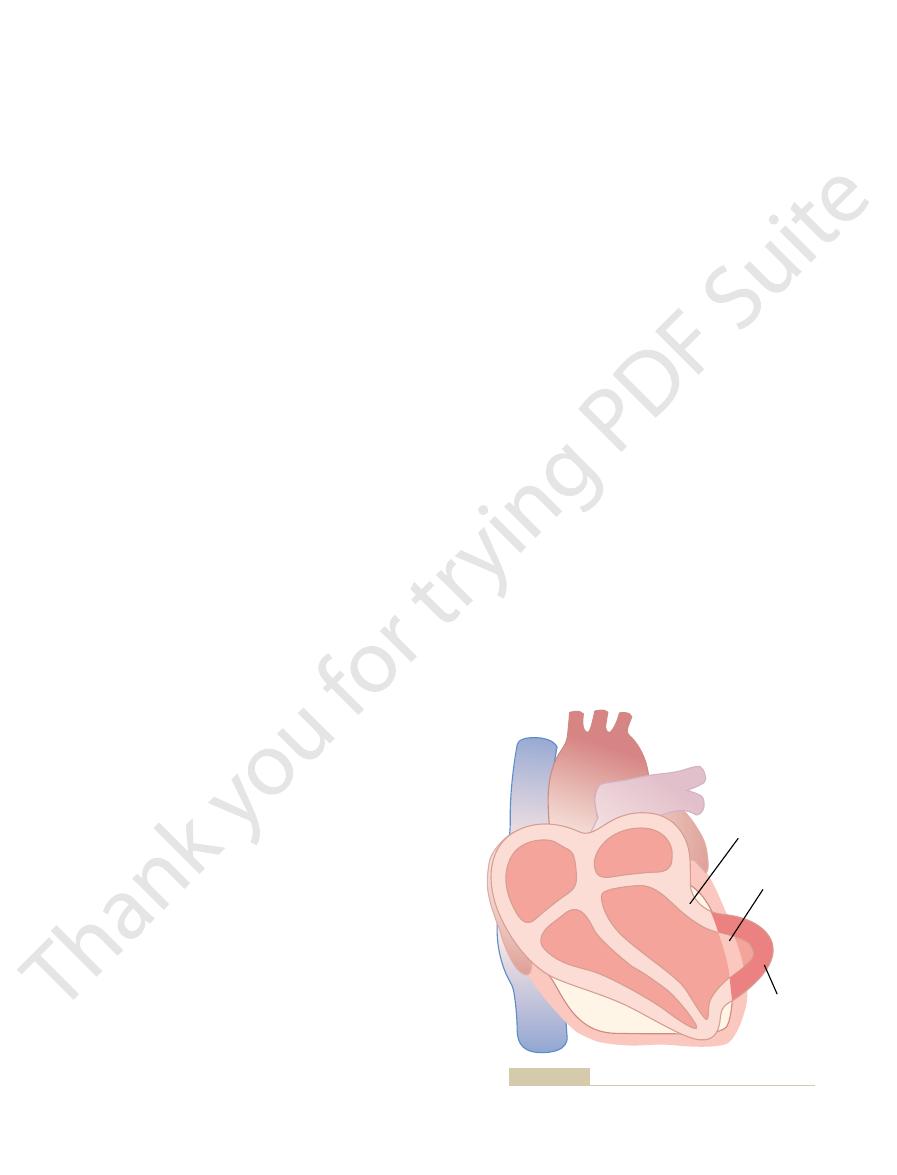
Figure 21–3 shows the heart and its coronary blood
Physiologic Anatomy of the Coronary
important subjects in medicine.
reason, understanding normal and pathological physi-
impairment of the coronary artery circulation. For this
the Western world result from coronary artery disease,
Coronary Circulation
sympathetic stimulation of the heart during exercise.
very heavy exercise because of the greatly increased
1.5 mm Hg. In fact, in a person with a strong heart,
atrial pressure has hardly changed, having risen only
normal level at point A. Note especially that the right
right atrial pressure is now point B, in contrast to the
rium point in Figure 21–2 for cardiac output and
curve and the cardiac output curve, the new equilib-
return curve.
Therefore, the combination of increased mean sys-
slope of the venous return curve.
return to decrease, thus increasing the upward
tissue, which also causes resistance to venous
. This is caused by decreased resistance in
upward
high as 30 mm Hg.
During maximal exercise, these two effects
increase in mean systemic filling pressure.
capacitative vascular system, causing a still greater
compresses many of the internal vessels, thus
. In addition, tensing of the
tremendously at the onset of heavy exercise. This
1. The mean systemic filling pressure rises
return curve is only 6 L/min. Yet two important
occurred from the normal venous return curve, the
Now study the venous return curves. If no change
can be achieved in some marathon runners.
plateau level of the normal heart, which would be a
Without this increased level of the output curve, the
tion of the heart, often to as much as twice normal.
190 beats/min, and (2) increased strength of contrac-
increased heart rate, often up to rates as high as 170 to
Muscle Blood Flow and Cardiac Output During Exercise
Chapter 21
249
increase in cardiac output would be limited to the
maximum increase of cardiac output of only about
2.5-fold rather than the 4-fold that can commonly be
achieved by the untrained runner and the 7-fold that
cardiac output could hardly rise at all in exercise
because the upper plateau level of the normal venous
changes do occur:
results partly from the sympathetic stimulation
that contracts the veins and other capacitative parts
of the circulation
abdominal and other skeletal muscles of the body
providing more compression of the entire
together can increase the mean systemic filling
pressure from a normal level of 7 mm Hg to as
2. The slope of the venous return curve rotates
virtually all the blood vessels in active muscle
temic filling pressure and decreased resistance to
venous return raises the entire level of the venous
In response to the changes in both the venous return
the right atrial pressure often falls below normal in
About one third of all deaths in the affluent society of
and almost all elderly people have at least some
ology of the coronary circulation is one of the most
Blood Supply
surface of the heart and smaller arteries then pene-
is almost entirely through these arteries that the heart
millimeter of the endocardial surface can obtain sig-
nificant nutrition directly from the blood inside the
left coronary artery supplies mainly the anterior
the right coronary artery supplies most of the right
ventricle as well as the posterior part of the left ven-
Most of the coronary venous blood flow from the
left ventricular muscle returns to the right atrium of
the heart by way of the coronary sinus—which is about
of the coronary venous blood from the right ventricu-
lar muscle returns through small
venous blood also flows back into the heart through
very minute thebesian
all chambers of the heart.
Normal Coronary Blood Flow
cent of the total cardiac output.
adult increases its cardiac output fourfold to seven-
work
Left coronary
artery
Aortic valve
Right coronary
artery
The coronary arteries.
Figure 21–3
research workers that a decrease in the oxygen
not been determined. It is speculated by many
However, the exact means by which increased
tunately, the coronary blood flow does increase almost
culature unless the coronary blood flow increases. For-
muscle. Because not much oxygen is left, very little
cardiac musculature for oxygen. Normally, about 70
Oxygen Demand as a Major Factor in Local Coronary Blood Flow
especially in the skeletal muscles all over the body.
to that occurring in many other tissues of the body,
accompanied by decreased coronary flow. This local
increases. Conversely, decreased heart activity is
less of cause, the rate of coronary blood flow also
the vigor of cardiac contraction is increased, regard-
cardiac muscle need for nutrition. That is, whenever
Controller of Coronary Flow
Local Muscle Metabolism Is the Primary
Control of Coronary Blood Flow
mally compensate for this. Later in the chapter, we will
by ventricular muscle contraction, tends to be reduced.
subendocardial plexus of the left ventricle, where the
. During systole, blood flow through the
supplying the needed nutrients. Lying immediately
from the epicardial arteries penetrate the muscle,
the muscle. Smaller,
epicardial coronary arteries
ferent depths in the heart muscle, showing on the outer
Figure 21–5 demonstrates
Epicardial Versus Subendocardial Coronary Blood Flow—Effect
ular muscle.
the left ventricular muscle, the inverse phasic changes
the cardiac cycle, but because the force of contraction
during all of diastole.
lar muscle capillaries, so that blood flows rapidly
, the cardiac muscle relaxes and no
body. The reason for this is strong compression of the
, which
experiments in lower animals. Note from this diagram
during systole and diastole, as extrapolated from
Figure
Phasic Changes in Coronary Blood Flow During Systole and
blood supply.
to make up for the relative deficiency of coronary
“efficiency” of cardiac utilization of energy increases
the heart to coronary blood flow increases. Thus, the
supply the extra nutrients needed by the heart. This
increase sixfold to ninefold. At the same time, the
250
Unit IV
The Circulation
output of the heart under severe conditions may
coronary blood flow increases threefold to fourfold to
increase is not as much as the increase in workload,
which means that the ratio of energy expenditure by
Diastole—Effect of Cardiac Muscle Compression.
21–4 shows the changes in blood flow through the
nutrient capillaries of the left ventricular coronary
system in milliliters per minute in the human heart
that the coronary capillary blood flow in the left ven-
tricle muscle falls to a low value during systole
is opposite to flow in vascular beds elsewhere in the
left ventricular muscle around the intramuscular
vessels during systolic contraction.
During diastole
longer obstructs blood flow through the left ventricu-
Blood flow through the coronary capillaries of the
right ventricle also undergoes phasic changes during
of the right ventricular muscle is far less than that of
are only partial in contrast to those in the left ventric-
of Intramyocardial Pressure.
the special arrangement of the coronary vessels at dif-
surface
that supply most of
intramuscular arteries derived
beneath the endocardium is a plexus of subendocar-
dial arteries
intramuscular coronary vessels are compressed greatly
But the extra vessels of the subendocardial plexus nor-
see that this peculiar difference between blood flow in
the epicardial and subendocardial arteries plays an
important role in certain types of coronary ischemia.
Blood flow through the coronary system is regulated
mostly by local arteriolar vasodilation in response to
regulation of coronary blood flow is almost identical
Regulation.
Blood flow in the coronaries usually is reg-
ulated almost exactly in proportion to the need of the
per cent of the oxygen in the coronary arterial blood
is removed as the blood flows through the heart
additional oxygen can be supplied to the heart mus-
in direct proportion to any additional metabolic con-
sumption of oxygen by the heart.
oxygen consumption causes coronary dilation has
Systole
Diastole
Coronary blood flow (ml/
min)
0
100
200
300
from measured flows in dogs).
left ventricle during cardiac systole and diastole (as extrapolated
Phasic flow of blood through the coronary capillaries of the human
Figure 21–4
Cardiac
muscle
Epicardial coronary arteries
Subendocardial arterial plexus
coronary vasculature.
Diagram of the epicardial, intramuscular, and subendocardial
Figure 21–5
oles during coronary hypoxia, as discussed earlier.
The released adenosine is believed to be one of the
is slightly permeable to adenosine, much of this
adenosine. Because the cardiac muscle cell membrane
diphosphate, then to adenosine monophosphate and
nary ischemia, the ATP degrades first to adenosine
traction and other cellular functions. In severe coro-
form ATP in the mitochondria. This ATP in turn acts
As is true in other tissues, more than 95 per cent of
in this chapter.
pain in cardiac ischemic conditions, as discussed later
tissue, which is probably one of the causes of cardiac
energy. Unfortunately, glycolysis consumes tremen-
anaerobic or ischemic conditions, cardiac metabolism
acids). However, as is also true of other tissues, under
tions, cardiac muscle normally consumes fatty acids to
tive differences. Most important, under resting condi-
same as for other tissues, but there are some quantita-
in Chapters 67 through 72, apply to cardiac muscle the
The basic principles of cellular metabolism, discussed
within seconds.
direction, the metabolic control of coronary flow
blood flow. Whenever the direct effects of nervous
drive, often with resultant anginal pain.
severe, and these people can have vasospastic myocar-
usually constriction. In some people, the alpha vaso-
slight overall coronary constriction or dilation, but
thetic stimulation can, at least theoretically, cause
preponderance of beta receptors. Therefore, sympa-
tors, whereas the intramuscular arteries may have a
coronary vessels have a preponderance of alpha recep-
exist in the coronary vessels. In general, the epicardial
. Both alpha and beta receptors
in the blood vessel walls. The constrictor receptors are
strictor or vascular dilator effects, depending on the
of the coronary vessels. In Chapter 60, we see that
There is much more extensive
acetylcholine released by parasym-
great. However, the
The distribution of parasympathetic (vagal) nerve
Direct Effects of Nervous Stimuli on the Coronary Vasculature.
coronary arteries.
consumption and, therefore, indirectly constrict the
tractility. These effects in turn decrease cardiac oxygen
ulation, with its release of acetylcholine, slows the
bolic needs of the heart muscle. In contrast, vagal stim-
for dilating the coronary vessels, and the blood flow
the heart. In turn, the increased metabolism of the
epinephrine, increases both heart rate and heart con-
thetic stimulation, which releases norepinephrine and
normal control of coronary blood flow. Thus, sympa-
the direct effects, play a far more important role in
The indirect effects, which are mostly opposite to
selves. The indirect effects result from secondary
The direct effects result from action of the nervous
affect coronary blood flow both directly and indirectly.
Nervous Control of Coronary Blood Flow
them. Therefore, the other vasodilator mechanisms
sine maintains vascular dilation for only 1 to 3 hours,
heart muscle activity. Second, studies in skeletal
First, pharmacologic agents that block or partially
Yet, difficulties with the vasodilator hypothesis exist.
prostaglandins and nitric oxide.
ions, carbon dioxide, bradykinin, and, possibly,
phosphate compounds, potassium ions, hydrogen
that has been identified. Others include adenosine
vasodilation, much of it is reabsorbed into the cardiac
local coronary blood flow. After the adenosine causes
fluids of the heart muscle, with resultant increase in
sine monophosphate; then small portions of this are
a large proportion of the cell’s ATP degrades to adeno-
very low concentrations of oxygen in the muscle cells,
. In the presence of
these dilate the arterioles. A substance with great
Muscle Blood Flow and Cardiac Output During Exercise
Chapter 21
251
concentration in the heart causes vasodilator sub-
stances to be released from the muscle cells and that
vasodilator propensity is adenosine
further degraded and release adenosine into the tissue
cells to be reused.
Adenosine is not the only vasodilator product
block the vasodilator effect of adenosine do not
prevent coronary vasodilation caused by increased
muscle have shown that continued infusion of adeno-
and yet muscle activity still dilates the local blood
vessels even when the adenosine can no longer dilate
listed above must be remembered.
Stimulation of the autonomic nerves to the heart can
transmitter substances acetylcholine from the vagus
nerves and norepinephrine and epinephrine from the
sympathetic nerves on the coronary vessels them-
changes in coronary blood flow caused by increased or
decreased activity of the heart.
tractility as well as increases the rate of metabolism of
heart sets off local blood flow regulatory mechanisms
increases approximately in proportion to the meta-
heart and has a slight depressive effect on heart con-
fibers to the ventricular coronary system is not very
pathetic stimulation has a direct effect to dilate the coro-
nary arteries.
sympathetic innerva-
tion
the sympathetic transmitter substances norepineph-
rine and epinephrine can have either vascular con-
presence or absence of constrictor or dilator receptors
called alpha receptors and the dilator receptors are
called beta receptors
constrictor effects seem to be disproportionately
dial ischemia during periods of excess sympathetic
Metabolic factors—especially myocardial oxygen
consumption—are the major controllers of myocardial
stimulation alter the coronary blood flow in the wrong
usually overrides the direct coronary nervous effects
Special Features of Cardiac
Muscle Metabolism
supply most of its energy instead of carbohydrates
(about 70 per cent of the energy is derived from fatty
must call on anaerobic glycolysis mechanisms for
dous quantities of the blood glucose and at the same
time forms large amounts of lactic acid in the cardiac
the metabolic energy liberated from foods is used to
as the conveyer of energy for cardiac muscular con-
can diffuse from the muscle cells into the circulating
blood.
substances that causes dilation of the coronary arteri-

coronary arteries, the small anastomoses begin to
When a sudden occlusion occurs in one of the larger
Figure 21–6.
sized 20 to 250 micrometers in diameter, as shown in
exist among the larger coronary arteries. But many
In a normal heart, almost no large communications
The
Lifesaving Value of Collateral Circulation in the Heart.
secondary thrombosis
vascular wall contraction. The spasm may then
arteriosclerotic plaque, or it might result from
of a coronary artery also can occur. The spasm
2. Many clinicians believe that local muscular spasm
where it blocks the artery at that point. A
peripheral branch of the coronary arterial tree,
it occludes the vessel. Or, occasionally, the
fibrin is deposited, and red blood cells become
unsmooth surface, blood platelets adhere to it,
the flowing blood. Because the plaque presents an
endothelium, thus coming in direct contact with
the artery. The thrombus usually occurs where the
thrombus,
1. The atherosclerotic plaque can cause a local blood
occlusion can result from any one of several effects,
in a person with a normal coronary circulation. Acute
Acute Coronary Occlusion
nary arteries.
lumens and either block or partially block blood flow.
calcified. The net result is the development of
are invaded by fibrous tissue and frequently become
throughout the body. Gradually, these areas of deposit
of cholesterol and have a sedentary lifestyle, large
erosclerosis, or in people who eat excessive quantities
Chapter 68. Briefly, this process is the following.
. The atherosclerotic process is
The
cardiac muscle.
, the most frequent cause of which is slowly
. In Chapter 22, we discuss
acute coronary occlusion and myocardial
coronary ischemia
In this chapter, we discuss acute
progressive weakening of the heart pumping process.
or fibrillation of the heart, whereas other deaths occur
in the United States die of this cause. Some deaths
cient coronary blood flow. About 35 per cent of people
is ischemic heart disease, which results from insuffi-
The most common cause of death in Western culture
the lives of the cardiac cells. This almost certainly is
minutes, relief of the ischemia may be too late to save
of only 2 per cent per hour. Therefore, once a serious
the affected cardiac muscle cells. Furthermore, this loss
coronary ischemia, as occurs after a myocardial infarct,
consequence. Within as little as 30 minutes of severe
However, loss of adenosine also has a serious cellular
252
Unit IV
The Circulation
about one half of the adenine base can be lost from
can be replaced by new synthesis of adenine at a rate
bout of coronary ischemia has persisted for 30 or more
one of the major causes of cardiac cellular death
during myocardial ischemia.
Ischemic Heart Disease
occur suddenly as a result of acute coronary occlusion
slowly over a period of weeks to years as a result of
caused by
infarction
congestive heart
failure
increasing coronary ischemia and weakening of the
Atherosclerosis as a Cause of Ischemic Heart Disease.
most frequent cause of diminished coronary blood
flow is atherosclerosis
discussed in connection with lipid metabolism in
In people who have genetic predisposition to ath-
quantities of cholesterol gradually become deposited
beneath the endothelium at many points in arteries
athero-
sclerotic plaques that actually protrude into the vessel
A common site for development of atherosclerotic
plaques is the first few centimeters of the major coro-
Acute occlusion of a coronary artery most frequently
occurs in a person who already has underlying ath-
erosclerotic coronary heart disease but almost never
two of which are the following:
clot called a
which in turn occludes
arteriosclerotic plaque has broken through the
entrapped to form a blood clot that grows until
clot breaks away from its attachment on the
atherosclerotic plaque and flows to a more
thrombus that flows along the artery in this way
and occludes the vessel more distally is called a
coronary embolus.
might result from direct irritation of the smooth
muscle of the arterial wall by the edges of an
local nervous reflexes that cause excess coronary
lead to
of the vessel.
degree of damage to the heart muscle caused either by
slowly developing atherosclerotic constriction of the
coronary arteries or by sudden coronary occlusion is
determined to a great extent by the degree of collat-
eral circulation that has already developed or that can
open within minutes after the occlusion.
anastomoses do exist among the smaller arteries
Artery
Vein
Artery
Vein
Minute anastomoses in the normal coronary arterial system.
Figure 21–6
sure that develops inside the ventricle. Therefore,
muscle, whether this be dead or simply nonfunctional,
ular muscle contract, the ischemic portion of the
21–7. That is, when the normal portions of the ventric-
, shown in Figure
systolic stretch
ventricle is proportionately depressed. Indeed, the
great force, the overall pumping ability of the affected
When some of the cardiac muscle fibers are not
Decreased Cardiac Output—Systolic Stretch and Cardiac
; and, occasionally, (4)
decreased cardiac output
The most common causes of death after acute
Causes of Death After Acute
cardial regions, and the damage then spreads outward
tion of the heart, as explained earlier. Therefore, any
the heart. The reason for this is that the subendocar-
The subendocardial muscle
does die.
there is almost no collateral blood flow, the muscle
central portion of a large infarct, however, where
coronary blood flow, the muscle will not die. In the
normal resting left ventricle each minute. Therefore, if
to remain alive. This is in comparison with about 8 mil-
no blood supply, the cardiac muscle cells die.
ished cellular metabolism. Within a few hours of almost
the local muscle tissue becomes edematous, and the
engorged despite lack of blood flow. In later stages, the
hue, and the blood vessels of the area appear to be
Therefore, the infarcted area takes on a bluish-brown
the last vestiges of the oxygen in the blood, causing
stagnant blood. Simultaneously the muscle fibers use
blood vessels, causes the area to become overfilled with
and this, combined with progressive dilation of local
Soon after the onset of the infarction, small amounts
myocardial infarction
. The overall
surrounding vessels. The area of muscle that has either
Immediately after an acute coronary occlusion, blood
Myocardial Infarction
older people.
of blood flow. This is one of the most common causes
limited in its work output, often so much so that the
When this occurs, the heart muscle becomes severely
blood vessels themselves develop atherosclerosis.
the needed blood flow, and sometimes the collateral
eventually, the sclerotic process develops beyond the
ence an acute episode of cardiac dysfunction. But,
more severe. Therefore, the person may never experi-
suddenly, collateral vessels can develop at the same
When atherosclerosis constricts the coronary arter-
nels, many patients recover almost completely from
1 month. Because of these developing collateral chan-
But then collateral flow does begin to increase, dou-
do not enlarge much more for the next 8 to 24 hours.
they now supply; the diameters of the collateral vessels
dilate within seconds. But the blood flow through these
Muscle Blood Flow and Cardiac Output During Exercise
Chapter 21
253
minute collaterals is usually less than one half that
needed to keep alive most of the cardiac muscle that
bling by the second or third day and often reaching
normal or almost normal coronary flow within about
various degrees of coronary occlusion when the area
of muscle involved is not too great.
ies slowly over a period of many years rather than
time while the atherosclerosis becomes more and
limits of even the collateral blood supply to provide
heart cannot pump even normally required amounts
of the cardiac failure that occurs in vast numbers of
flow ceases in the coronary vessels beyond the occlu-
sion except for small amounts of collateral flow from
zero flow or so little flow that it cannot sustain cardiac
muscle function is said to be infarcted
process is called a
.
of collateral blood begin to seep into the infarcted area,
the hemoglobin to become totally de-oxygenated.
vessel walls become highly permeable and leak fluid;
cardiac muscle cells begin to swell because of dimin-
Cardiac muscle requires about 1.3 milliliters of
oxygen per 100 grams of muscle tissue per minute just
liliters of oxygen per 100 grams delivered to the
there is even 15 to 30 per cent of normal resting
Subendocardial Infarction.
frequently becomes infarcted even when there is no
evidence of infarction in the outer surface portions of
dial muscle has extra difficulty obtaining adequate
blood flow because the blood vessels in the subendo-
cardium are intensely compressed by systolic contrac-
condition that compromises blood flow to any area of
the heart usually causes damage first in the subendo-
toward the epicardium.
Coronary Occlusion
myocardial infarction are (1)
;
(2) damming of blood in the pulmonary blood vessels
and then death resulting from pulmonary edema; (3)
fibrillation of the heart
rupture of
the heart.
Shock.
functioning and others are too weak to contract with
overall pumping strength of the infarcted heart is often
decreased more than one might expect because of a
phenomenon called
instead of contracting is forced outward by the pres-
Normal contraction
Non-functional
muscle
Systolic stretch
Systolic stretch in an area of ischemic cardiac muscle.
Figure 21–7
The upper left part of Figure 21–8 shows the effects of
Myocardial Infarction
Stages of Recovery from Acute
flow into the right atrium, and the patient dies of sud-
Because of this compression of the heart, blood cannot
outside by blood collecting in the pericardial cavity.
—that is, compression of the heart from the
cardiac
When a ventricle does rupture, loss of blood into the
systolic stretch is worsening.
by cardiac imaging (i.e., x-rays) whether the degree of
tures. In fact, one of the means used in assessing
systolic stretch
with each heart contraction, and this
happens, the dead muscle bulges outward severely
the heart wall becomes stretched very thin. When this
later, the dead muscle fibers begin to degenerate, and
of the ischemic portion of the heart, but a few days
after an acute infarct, there is little danger of rupture
movement” cycle of new excitation and causing
refractoriness, thereby initiating a “circus
Chapter 13, excess prolongation of conduction
of circus movements because, as discussed in
of the cardiac muscle.
abnormal conduction pathways all the way
increases the pathway length
. This
Cardiac muscle weakness
the arterial tree. The sympathetic stimulation also
massive infarction, principally because the heart
Powerful sympathetic reflexes
potential elsewhere in the heart. Therefore,
its membranes after a heart beat, so that the
myocardial infarction. That is, the ischemic
2. Ischemia of the muscle causes an “
fibrillating.
musculature and, therefore, its likelihood of
fluids surrounding the cardiac muscle fibers.
ischemic musculature. This also increases the
from the
1. Acute loss of blood supply to the cardiac muscle
At least four factors enter into the tendency for the
occur many days after the infarct but less likely so.
lasting for another few hours. Fibrillation can also
of relative safety, followed by a secondary period of
after the infarction occurs. Then there is a short period
likely to occur. The first is during the first 10 minutes
There are two especially dangerous periods after
with chronic coronary insufficiency die suddenly from
after small occlusions as well. Indeed, some patients
large infarction, but fibrillation can sometimes occur
dency to develop fibrillation is especially great after a
. The ten-
Fibrillation of the Ventricles After Myocardial Infarction.
initial pulmonary symptoms.
. Consequently,
therefore, leads to
This adds progressively to the total blood volume and,
Chapter 22. the kidneys fail to excrete enough urine.
kidneys. Then, for reasons that are discussed in
later for the following reason: The acutely diminished
dial infarction. Instead, symptoms develop a few days
This damming of blood in the veins often causes
lungs.
to increased capillary pressures, particularly in the
of the lungs or in the systemic circulation. This leads
heart is not pumping blood forward, it must be
When the
Damming of Blood in the Body’s Venous System.
40 per cent of the left ventricle is infarcted. And death
. It is discussed more fully in the next chapter.
low cardiac output
, or
cardiac shock
diogenic shock
coronary shock
. This condition is called
ischemia
peripheral arterial tree, cardiac failure and death of
When the heart becomes incapable of contracting
muscle.
254
Unit IV
The Circulation
much of the pumping force of the ventricle is dissi-
pated by bulging of the area of nonfunctional cardiac
with sufficient force to pump enough blood into the
peripheral tissues ensue as a result of peripheral
, car-
,
failure
Cardiac shock almost always occurs when more than
occurs in about 85 per cent of patients once they
develop cardiac shock.
damming blood in the atria and in the blood vessels
little difficulty during the first few hours after myocar-
cardiac output leads to diminished blood flow to the
congestive symptoms
many patients who seemingly are getting along well
during the first few days after onset of heart failure will
suddenly develop acute pulmonary edema and often
will die within a few hours after appearance of the
Many people who die of coronary occlusion die
because of sudden ventricular fibrillation
fibrillation without any acute infarction.
coronary infarction during which fibrillation is most
cardiac irritability beginning 1 hour or so later and
heart to fibrillate:
causes rapid depletion of potassium
potassium concentration in the extracellular
Experiments in which potassium has been injected
into the coronary system have demonstrated that
an elevated extracellular potassium concentration
increases the irritability of the cardiac
injury current,”
which is described in Chapter 12 in relation to
electrocardiograms in patients with acute
musculature often cannot completely repolarize
external surface of this muscle remains negative
with respect to normal cardiac muscle membrane
electric current flows from this ischemic area of
the heart to the normal area and can elicit
abnormal impulses that can cause fibrillation.
3.
often develop after
does not pump an adequate volume of blood into
increases irritability of the cardiac muscle and
thereby predisposes to fibrillation.
4.
caused by the
myocardial infarction often causes the ventricle to
dilate excessively
for impulse conduction in the heart and frequently
causes
around the infarcted area
Both of these effects predispose to development
pathways in the ventricles allows impulses to re-
enter muscle that is already recovering from
the process to continue on and on.
Rupture of the Infarcted Area.
During the first day or so
becomes greater and greater until finally the heart rup-
progress of severe myocardial infarction is to record
pericardial space causes rapid development of
tamponade
denly decreased cardiac output.
acute coronary occlusion in a patient with a small area
of their coronary arteries, cardiac pain, called
in the cardiac muscle, sending pain impulses through
coronary blood flow. The high concentrations of these
histamine, kinins, or cellular proteolytic enzymes, that
lactic acid, or other pain-promoting products, such as
causes the muscle to release acidic substances, such as
pain is not known, but it is believed that ischemia
tion—sometimes severe pain. Exactly what causes this
Normally, a person cannot “feel” his or her heart, but
normal activity of a quiet, restful type but not strenu-
as little as 100 per cent, the person can still perform
per cent. Even when the cardiac reserve is reduced to
a normal person has a “cardiac reserve” of 300 to 400
per minute than the body requires during rest—that is,
is depressed below normal, because the normal heart
heart. This does not mean that the person is necessar-
capability, but more frequently its pumping capability
Occasionally, a heart that has recovered from a large
from Myocardial Infarction
Function of the Heart After Recovery
the recovery process.
syndrome. Consequently, one of the most important
worsens. This condition is called the “coronary steal”
into the ischemic area, so that the ischemic condition
through the normal muscle tissue, thus leaving little
musculature become greatly dilated. This allows most
becomes excessively active, the vessels of the normal
the heart that they normally supply. When the heart
nutrients for sustaining its life. Furthermore, anasto-
fatigue, the heart needs increased oxygen and other
exercise, in severe emotional strain, or as a result of
When the workload is greatly increased, such as during
of ischemia and the workload on the heart muscle
The degree
Value of Rest in Treating Myocardial Infarction.
within a few months.
lost dead cardiac musculature. By these means, the
Finally, the normal areas of the heart gradually
to a year.
progressive contraction and dissolution, the fibrous
is gradually replaced by fibrous tissue. Then, because
ties of fibrous tissue. Therefore, the dead muscle tissue
dies—one or the other. In the meantime, fibrous tissue
recovers. After a few days to three weeks, most of
the infarcted area, much of the nonfunctional muscle
ischemia. At the same time, because of enlargement of
area of dead fibers becomes bigger because many of
ischemic area die. Then, during the ensuing days, this
the occlusion, the muscle fibers in the center of the
a large myocardial infarction are shown. Shortly after
part of Figure 21–8, the various stages of recovery after
Replacement of Dead Muscle by Scar Tissue.
tion and usually failure of impulse conduction. Then,
area is a nonfunctional area, with failure of contrac-
coronary blood supply. Immediately around the dead
muscle fibers in the center of the area die rapidly,
When the area of ischemia is large, some of the
small, little or no death of the muscle cells may occur,
a large area of ischemia. When the area of ischemia is
of muscle ischemia; to the right is shown a heart with
Muscle Blood Flow and Cardiac Output During Exercise
Chapter 21
255
but part of the muscle often does become temporarily
nonfunctional because of inadequate nutrition to
support muscle contraction.
within 1 to 3 hours where there is total cessation of
extending circumferentially around the nonfunctional
area is an area that is still contracting but weakly so
because of mild ischemia.
In the lower
the marginal fibers finally succumb to the prolonged
collateral arterial channels supplying the outer rim of
the nonfunctional muscle becomes functional again or
begins developing among the dead fibers because
ischemia can stimulate growth of fibroblasts and
promote development of greater than normal quanti-
it is a general property of fibrous tissue to undergo
scar may grow smaller over a period of several months
hypertrophy to compensate at least partially for the
heart recovers either partially or almost completely
of cardiac cellular death is determined by the degree
.
motic blood vessels that supply blood to ischemic
areas of the heart must also still supply the areas of
of the blood flowing into the coronary vessels to flow
blood to flow through the small anastomotic channels
factors in the treatment of a patient with myocardial
infarction is observance of absolute body rest during
myocardial infarction returns almost to full functional
is permanently decreased below that of a healthy
ily a cardiac invalid or that the resting cardiac output
is capable of pumping 300 to 400 per cent more blood
ous exercise that would overload the heart.
Pain in Coronary Heart Disease
ischemic cardiac muscle often does cause pain sensa-
are not removed rapidly enough by the slowly moving
abnormal products then stimulate pain nerve endings
sensory afferent nerve fibers into the central nervous
system.
Angina Pectoris
In most people who develop progressive constriction
angina
Dead fibers
Fibrous tissue
Mild
ischemia
Non-
functional
Mild
ischemia
Non-
functional
Dead fibers
Nonfunctional
of recovery from myocardial infarction.
, Small and large areas of coronary ischemia.
Top
Figure 21–8
Bottom, Stages
muscle. Acta Physiol Scand 177:329, 2003.
Joyner MJ, Dietz NM: Sympathetic vasodilation in human
2998, 2003.
dial infarction: expanding the paradigm. Circulation 107:
Hochman JS: Cardiogenic shock complicating acute myocar-
in the regulation of blood flow. Am J Physiol 282:R1280,
Hester RL, Hammer LW: Venular-arteriolar communication
Biol 23:1510, 2003.
and restenosis development. Arterioscler Thromb Vasc
muscle cell heterogeneity: implications for atherosclerosis
Hao H, Gabbiani J, Bochaton-Piallat M: Arterial smooth
Saunders Co, 1973.
Cardiac Output and Its Regulation. Philadelphia: WB
Guyton AC, Jones CE, Coleman TG: Circulatory Pathology:
left heart failure. Chest 125:669, 2004.
Gehlbach BK, Geppert E: The pulmonary manifestations of
nary artery disease. Ann Intern Med 136:54, 2002.
Freedman SB, Isner JM: Therapeutic angiogenesis for coro-
acute myocardial infarction. BMJ 328:693, 2004.
Dalal H, Evans PH, Campbell JL: Recent developments in
Circulation 108:1263, 2003.
Cohn PF, Fox KM, Daly C: Silent myocardial ischemia.
rotic plaque: a multifocal disease. Circulation 107:2072,
Casscells W, Nahai M, Willerson JT: Vulnerable atheroscle-
restenosis.
angioplasty to hold the artery open, thus preventing its
“sleeve” placed inside a coronary artery dilated by
atherosclerotic lesion. The laser literally dissolves the
development. One of these employs a laser beam from
still eventually require coronary bypass surgery.
for at least several years, although many of the patients
often increases threefold to fourfold, and more than
cedure is performed, the blood flow through the vessel
markedly stretches the diseased artery. After this pro-
the balloon is inflated with high pressure, which
catheter straddles the partially occluded point. Then
diameter, is passed under radiographic guidance into
A small balloon-tipped catheter, about 1 millimeter in
, is the following:
before they become totally occluded. This procedure,
Since the 1980s, a procedure has
Coronary Angioplasty.
to be of little value.
been severely damaged, the bypass procedure is likely
vival expectation. Conversely, if the heart has already
damaged before the operation, the coronary bypass
Anginal pain is relieved in most patients. Also, in
performed, each of which supplies a peripheral coro-
rotic blockage point. One to five such grafts are usually
, for removing a section of a
aortic-coronary bypass
gical procedure was developed in the 1960s, called
vessels elsewhere are normal or almost normal. A sur-
blocked by atherosclerotic disease, and the coronary
coronary ischemia, the constricted areas of the coro-
Aortic-Coronary Bypass Surgery.
Surgical Treatment of
severity.
stressful conditions. For obvious reasons, this can also
during exercise or emotional episodes. Therefore,
beta adrenergic receptors, which prevents sympathetic
such as propranolol. These drugs block sympathetic
beta blockers
often give immediate relief from the pain. Commonly
administered during an acute anginal attack, can
Several vasodilator drugs, when
Treatment with Drugs.
described as hot, pressing, and constricting; it is of such
pain is present all the time. The pain is frequently
usually lasts for only a few minutes. However, some
sympathetic vasoconstrictor nerve signals. The pain
from the same spinal cord segments.
do the arms. Therefore, both the heart and these
heart originates during embryonic life in the neck, as
. The reason for this distribution of pain is that the
neck
often referred to distant surface areas of the body,
the upper sternum over the heart, and in addition it is
coronary blood flow. This pain is usually felt beneath
, begins to appear whenever the load on the
256
Unit IV
The Circulation
pectoris
heart becomes too great in relation to the available
most commonly to the left arm and left shoulder but
also frequently to the
and even to the side of the
face
surface areas of the body receive pain nerve fibers
Most people who have chronic angina pectoris feel
pain when they exercise or when they experience
emotions that increase metabolism of the heart or
temporarily constrict the coronary vessels because of
patients have such severe and lasting ischemia that the
quality that it usually makes the patient stop all unnec-
essary body activity and come to a complete state of
rest.
used vasodilators are nitroglycerin and other nitrate
drugs.
A second class of drugs that are used for prolonged
treatment of angina pectoris is the
,
enhancement of heart rate and cardiac metabolism
therapy with a beta blocker decreases the need
of the heart for extra metabolic oxygen during
reduce the number of anginal attacks as well as their
Coronary Disease
In many patients with
nary arteries are located at only a few discrete points
subcutaneous vein from an arm or leg and then graft-
ing this vein from the root of the aorta to the side of
a peripheral coronary artery beyond the atheroscle-
nary artery beyond a block.
patients whose hearts have not become too severely
procedure may provide the patient with normal sur-
been used to open partially blocked coronary vessels
called coronary artery angioplasty
the coronary system and pushed through the partially
occluded artery until the balloon portion of the
three quarters of the patients who undergo the proce-
dure are relieved of the coronary ischemic symptoms
Still newer procedures for opening atherosclerotic
coronary arteries are constantly in experimental
the tip of a coronary artery catheter aimed at the
lesion without substantially damaging the rest of
the arterial wall.
Another development has been a minute metal
References
2003.
secondary prevention and cardiac rehabilitation after
2002.
83:1113, 2003.
from cellular physiology to clinical cardiology. Physiol Rev
Yellon DM, Downey JM: Preconditioning the myocardium:
microcirculation. Physiol Rev 83:933, 2003.
Tsai AG, Johnson PC, Intaglietta M: Oxygen gradients in the
tion 107:363, 2003.
cardiovascular disease detection and prevention. Circula-
Ridker PM: Clinical application of C-reactive protein for
gration of the muscle systems. Adv Physiol Educ 27:183,
Richardson RS: Oxygen transport and utilization: an inte-
Libby P: Inflammation in atherosclerosis. Nature 420:868,
aspect of coronary artery disease. Circulation 107:2507,
Coronary collaterals: an important and underexposed
Koerselman J, van der Graaf Y, de Jaegere PP, Grobbee DE:
Muscle Blood Flow and Cardiac Output During Exercise
Chapter 21
257
2003.
2002.
2003.
