
sympathetics become strongly stimulated within a few seconds, and the
ing the sympathetic nervous system. But whatever the reflexes might be, the
reflexes that originate in the damaged heart
central nervous system ischemic response
, the
chemoreceptor reflex
, which is activated by diminished arterial pressure. It is probable
in Chapter 18 are immediately activated. The best known of these is the
cardiac output falls precariously low, many of the circulatory reflexes discussed
When the
Compensation for Acute Cardiac Failure by Sympathetic Nervous Reflexes.
heart, as follows.
reflexes occur immediately and compensate, to a great extent, for the damaged
perhaps a few hours, but it is likely to be associated with fainting. Fortunately,
the right atrium. This low cardiac output is still sufficient to sustain life for
4 mm Hg
two-fifths normal, whereas the right atrial pressure has risen to
than point A, illustrating that the cardiac output has fallen to 2 L/min, about
Within a few seconds, a new circulatory state is established at point B rather
becomes greatly lowered, falling to the lowest curve at the bottom of the graph.
Immediately after the heart becomes damaged, the cardiac output curve
resting conditions of 5 L/min and a right atrial pressure of 0 mm Hg.
curve is the normal operating point, showing a normal cardiac output under
top curve of this figure shows a normal cardiac output curve. Point A on this
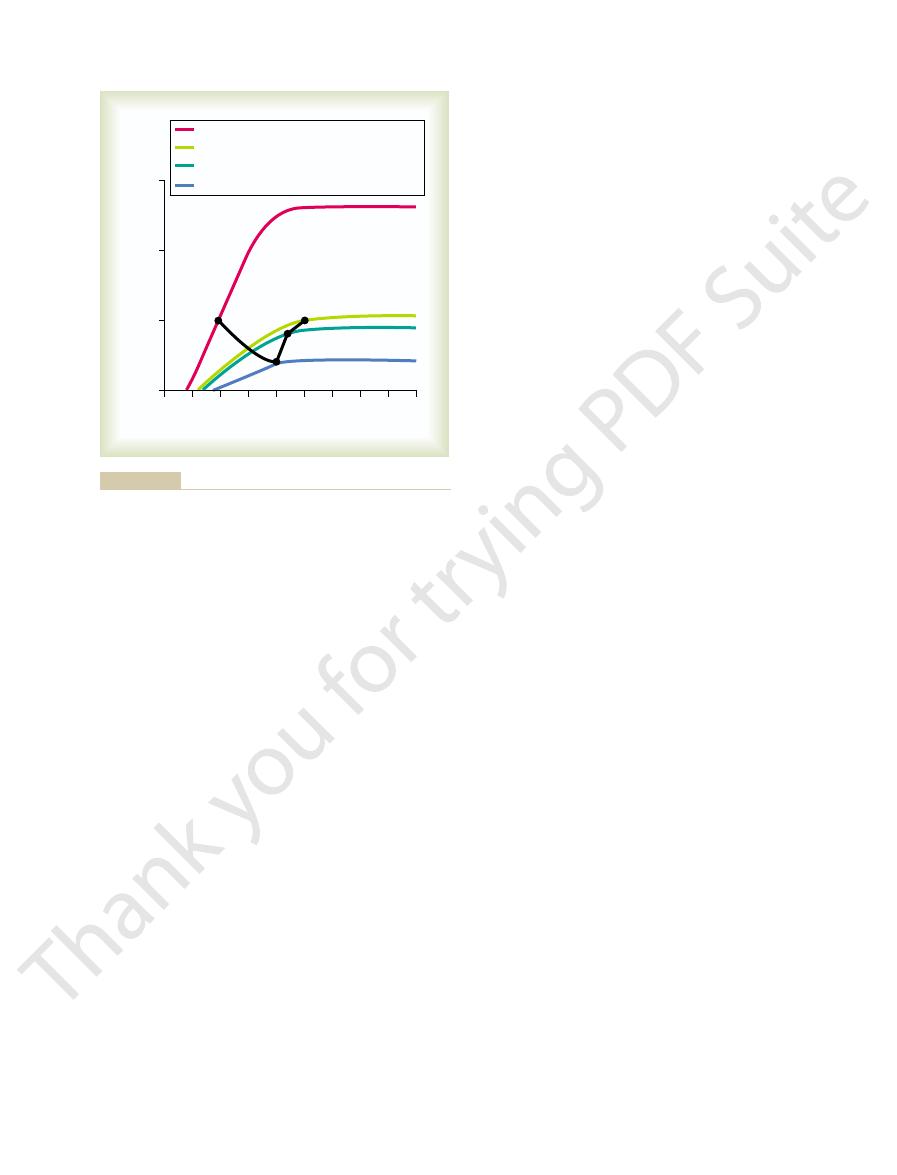
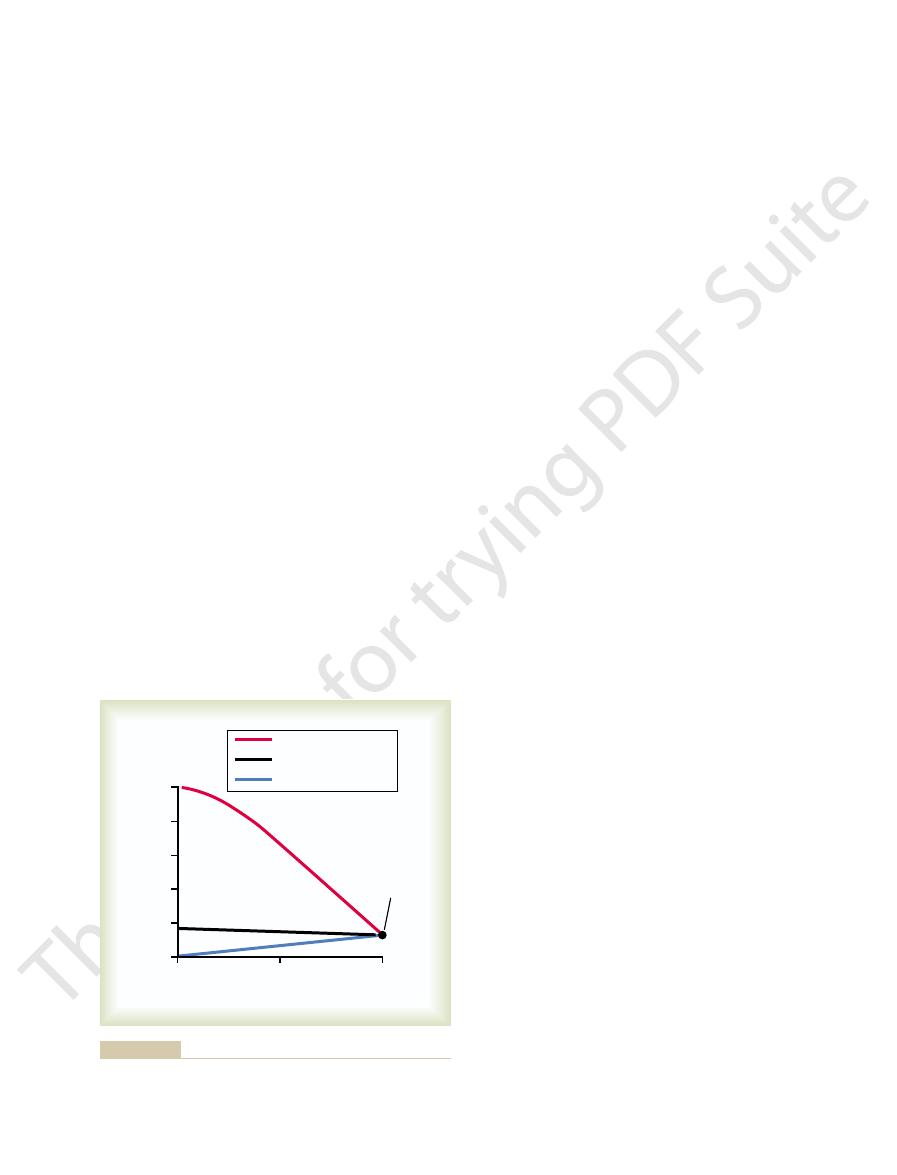
after an acute myocardial infarction are shown graphically in Figure 22–1. The
The progressive changes in heart pumping effectiveness at different times
veins, resulting in increased venous pressure.
main effects occur: (1) reduced cardiac output and (2) damming of blood in the
tion, the pumping ability of the heart is immediately depressed. As a result, two
If a heart suddenly becomes severely damaged, such as by myocardial infarc-
Acute Effects of Moderate Cardiac Failure
Dynamics of the Circulation in Cardiac Failure
the heart to pump enough blood to satisfy the needs of the body.
The term “cardiac failure” means simply failure of
congenital heart disease.
blockage of the coronary blood vessels. In Chapter 23, we discuss valvular and
mality that makes the heart a hypoeffective pump. In this chapter, we discuss
heart, vitamin B deficiency, primary cardiac muscle disease, or any other abnor-
damaged heart valves, external pressure around the
blood flow. However, failure can also be caused by
The cause usually is decreased contractility of the
failure”). This can result from any heart condition
Cardiac Failure
C
H
A
P
T
E
R
2
2
258
One of the most important ailments that must be
treated by the physician is cardiac failure (“heart
that reduces the ability of the heart to pump blood.
myocardium resulting from diminished coronary
mainly cardiac failure caused by ischemic heart disease resulting from partial
Definition of Cardiac Failure.
+
because venous blood returning to the heart from the body is dammed up in
this acute stage usually lasts for only a few seconds because sympathetic nerve
barore-
ceptor reflex
that the
,
and even
also contribute to activat-
water to equal salt and water intake. Therefore, fluid
still more, blood flow to the kidneys finally becomes
When the heart’s pumping capability is reduced
in a quiet resting state.
reduced to as low as 40 to 50 per cent of normal, the
fact that even when the heart’s pumping ability is
for the heart’s diminished pumping ability—enough in
If the heart is not too greatly damaged, this
it distends the veins, which
. Second,
causing venous flow of blood toward the heart
pressure, which
in two ways: First, it increases the mean systemic filling
The increased blood volume increases venous return
always to have a detrimental effect in cardiac failure.
sure remain significantly less than normal, and urine
general, the urine output remains reduced below
output falls to one-half to two-thirds normal. In
function, sometimes causing anuria when the cardiac
Volume Occur for Hours to Days
Renal Retention of Fluid and Increase in Blood
trated by the light green curve in Figure 22–1; this was
heart itself over a period of weeks to months, as illus-
kidneys and (2) varying degrees of recovery of the
mainly by two events: (1) retention of fluid by the
prolonged semi-chronic state begins, characterized
After the first few minutes of an acute heart attack, a
Retention Helps to Compensate
Chronic Stage of Failure—Fluid
or she remains quiet, although the pain might persist.
thetic reflex compensations, the cardiac output may
fainting. Shortly thereafter, with the aid of the sympa-
a sudden, moderate heart attack might experience
oped in about 30 seconds. Therefore, a person who has
The sympathetic reflexes become maximally devel-
4.2 L/min and a right atrial pressure of 5 mm Hg.
is depicted by point C, showing a cardiac output of
blood. Thus, in Figure 22–1, the new circulatory state
usual, and the right atrial pressure rises still further,
the veins back into the heart. Therefore, the damaged
greatly increases the tendency for blood to flow from
cussed in Chapter 20, this increased filling pressure
mm Hg, almost 100 per cent above normal. As dis-
blood vessels of the circulation, especially the veins,
cardiac output curve.
strated in Figure 22–1, showing after sympathetic com-
. This effect is also demon-
one way or another
functional muscle. Thus,
tion, in this way partially compensating for the non-
functional and part of it is still normal, the normal
this damaged musculature. If part of the muscle is non-
still functional, sympathetic stimulation strengthens
and second on the peripheral vasculature. If all the
effects on the circulation: first on the heart itself,
reciprocally inhibited at the same time.
Cardiac Failure
Chapter 22
259
parasympathetic nervous signals to the heart become
Strong sympathetic stimulation has two major
ventricular musculature is diffusely damaged but is
muscle is strongly stimulated by sympathetic stimula-
the heart,
,
becomes a stronger pump
pensation about twofold elevation of the very low
Sympathetic stimulation also increases venous
return because it increases the tone of most of the
raising the mean systemic filling pressure to 12 to 14
heart becomes primed with more inflowing blood than
which helps the heart to pump still larger quantities of
nothing more than cardiac pain and a few seconds of
return to a level adequate to sustain the person if he
Cardiac Output
also discussed in Chapter 21.
A low cardiac output has a profound effect on renal
normal as long as the cardiac output and arterial pres-
output usually does not return all the way to normal
after an acute heart attack until the cardiac output and
arterial pressure rise either all the way back to normal
or almost to normal.
Moderate Fluid Retention in Cardiac Failure Can Be Beneficial.
Many cardiologists formerly considered fluid retention
But it is now known that a moderate increase in body
fluid and blood volume is an important factor in
helping to compensate for the diminished pumping
ability of the heart by increasing the venous return.
increases the pressure gradient for
reduces the venous resist-
ance and allows even more ease of flow of blood to the
heart.
increased venous return can often fully compensate
increased venous return can often cause an entirely
normal cardiac output as long as the person remains
too low for the kidneys to excrete enough salt and
2
0
+2
+4
+6
+8 +10 +12 +14
Cardiac output (L
/min)
0
5
10
15
–4
–
Right atrial pressure (mm Hg)
Normal heart
Partially recovered heart
Damaged heart + sympathetic stimulation
Acutely damaged heart
A
B
C
D
sure change progressively from point A to point D (illustrated by
myocardial infarction. Both the cardiac output and right atrial pres-
Progressive changes in the cardiac output curve after acute
Figure 22–1
the black line) over a period of seconds, minutes, days, and
weeks.
compensation, either by sympathetic nervous reflexes
If the heart becomes severely damaged, no amount of
reserve is discussed more fully later in the chapter.
compensated heart failure. This concept of cardiac
cardiac reserve
fore, it is said that the
capacity to the levels required for the exercise. There-
When a person is in compensated heart failure, any
progressive stages of damage.
the damage often has occurred a little at a time, and
degrees of “compensated heart failure.” These persons
Thus many people, especially older people, have
normal. This demonstrates that an increase in right
light green curve, is still depressed to less than one-half
recovered heart, as depicted by the plateau level of the
Note especially in Figure
ery and fluid retention (point D). This final state is
by sympathetic stimulation (point C), and final return
B), the rise in cardiac output toward normal caused
(point A), the state a few seconds after the heart attack
by the black curve in Figure 22–1. The progression of
tion of fluid. All these changes are shown graphically
seconds to 1 minute; and (3) chronic compensations
nervous system, which occurs mainly within the first 30
cardiac damage; (2) compensation by the sympathetic
after an acute, moderate heart attack, we can divide
To summarize the events discussed in the past few sec-
After Acute Cardiac Failure
the acute stage of cardiac failure gradually disappear.
recovers even slightly, the fast pulse rate, cold skin,
sympathetic stimulation can. Therefore, as the heart
the following reasons: The partial recovery of the
adequate fluid volume has been retained, the sympa-
this figure, the person now has essentially normal car-
. Therefore, except for the
further fluid retention occurs, except that
renal output of fluid also returns to normal, and no
atrial pressure increased to 6 mm Hg.
culation is now changed from point C to point D, which
has risen even more. As a result, the state of the cir-
markedly as well; therefore, the right atrial pressure
the tendency for venous return has increased
or so after acute myocardial infarction. By this time,
Figure 22–1
The Cardiac Output Curve After Partial Recovery.
months.
final state of recovery within 5 to 7 weeks, although
infarction, the heart ordinarily recovers rapidly during
almost complete recovery. After acute myocardial
cardiac damage, and it varies from no recovery to
The degree of recovery depends on the type of
way offsetting much of the cardiac damage.
portion of the heart musculature hypertrophies, in this
to become functional again. Also, the undamaged
eral portions of the infarcted area of the heart, often
restore normal cardiac function. For instance, a new
of myocardial infarction, the natural reparative
Myocardial Infarction
Recovery of the Myocardium After
are discussed in later sections of this chapter.
of the body.These detrimental effects of excessive fluid
filtration of fluid into the lungs, causing pulmonary
the heart, thus weakening the heart still more; (2)
cal consequences. They include (1) overstretching of
ate fluid retention in cardiac failure, in severe failure
severe edema develops throughout the body, which
on the circulation. Instead,
, this excess fluid no
Furthermore, because the heart is already pumping at
major therapeutic procedures are used to prevent this.
retention begins and continues indefinitely, unless
260
Unit IV
The Circulation
its maximum pumping capacity
longer has a beneficial effect
can be very detrimental in itself and can lead to death.
Detrimental Effects of Excess Fluid Retention in Severe Cardiac
Failure.
In contrast to the beneficial effects of moder-
extreme excesses of fluid can have serious physiologi-
edema and consequent deoxygenation of the blood;
and (3) development of extensive edema in most parts
After a heart becomes suddenly damaged as a result
processes of the body begin immediately to help
collateral blood supply begins to penetrate the periph-
causing much of the heart muscle in the fringe areas
the first few days and weeks and achieves most of its
mild degrees of additional recovery can continue for
shows function of the partially recovered heart a week
considerable fluid has been retained in the body and
shows a normal cardiac output of 5 L/min but right
Because the cardiac output has returned to normal,
the retention
of fluid that has already occurred continues to maintain
moderate excesses of fluid
high right atrial pressure represented by point D in
diovascular dynamics as long as he or she remains at
rest.
If the heart recovers to a significant extent and if
thetic stimulation gradually abates toward normal for
heart can elevate the cardiac output curve the same as
and pallor resulting from sympathetic stimulation in
Summary of the Changes That Occur
—
“Compensated Heart Failure”
tions describing the dynamics of circulatory changes
the stages into (1) the instantaneous effect of the
resulting from partial heart recovery and renal reten-
this curve shows the normal state of the circulation
but before sympathetic reflexes have occurred (point
of the cardiac output almost exactly to normal after
several days to several weeks of partial cardiac recov-
called compensated heart failure.
Compensated Heart Failure.
22–1 that the maximum pumping ability of the partly
atrial pressure can maintain the cardiac output at a
normal level despite continued weakness of the heart.
normal resting cardiac outputs but mildly to moder-
ately elevated right atrial pressures because of various
may not know that they have cardiac damage because
the compensation has occurred concurrently with the
attempt to perform heavy exercise usually causes
immediate return of the symptoms of acute failure
because the heart is not able to increase its pumping
is reduced in
Dynamics of Severe Cardiac Failure—
Decompensated Heart Failure
reducing water and salt intake, which brings about a
tion normally again, or (2)
, so that
istration of a cardiotonic drug, such as
in any one of several ways, especially by admin-
The decompensation
Treatment of Decompensation.
hunger). All clinicians know that lack of appropriate
edema, especially edema of the lungs, which leads
completely. Clinically, one detects this serious condi-
even moderate quantities of blood and, therefore, fails
systemic filling pressure, and (3) progressive elevation
Thus, one can see from this analysis that failure of
the patient dies. This state of heart failure in which the
approached or reached incompatibility with life, and
the right atrial pressure 16 mm Hg. This state has
of the circulation has reached point F on the curve,
occurs). Consequently, within a few days, the state
normal renal function, so that fluid retention not
detrimental than beneficial to the circulation. Yet the
diminish the heart’s pumping performance. It is
edema of the heart muscle, and other factors that
level. This decline is caused by overstretch of the heart,
atrial pressure has risen still further, but by now,
After another few days of fluid retention, the right
balance.
becomes that depicted by point D. Still, the cardiac
pressure rises to 9 mm Hg, and the circulatory state
to be retained. After another day or so, the right atrial
normal renal output of fluid; therefore, fluid continues
and the cardiac output to 4.2 L/min. Note again that
the circulation changes in Figure 22–2 from point B to
the right atrial pressure. After 1 day or so, the state of
peripheral veins into the right atrium, thus increasing
increasing quantities of blood from the person’s
circulation continues to rise; this forces progressively
volume, the mean systemic filling pressure of the
and the body fluid volume increases progressively.
output below this level, all the fluid-retaining mecha-
to be as great as the intake of these. At any cardiac
fluid balance—that is, for the output of salt and water
output level of 5 L/min. This is approximately the crit-
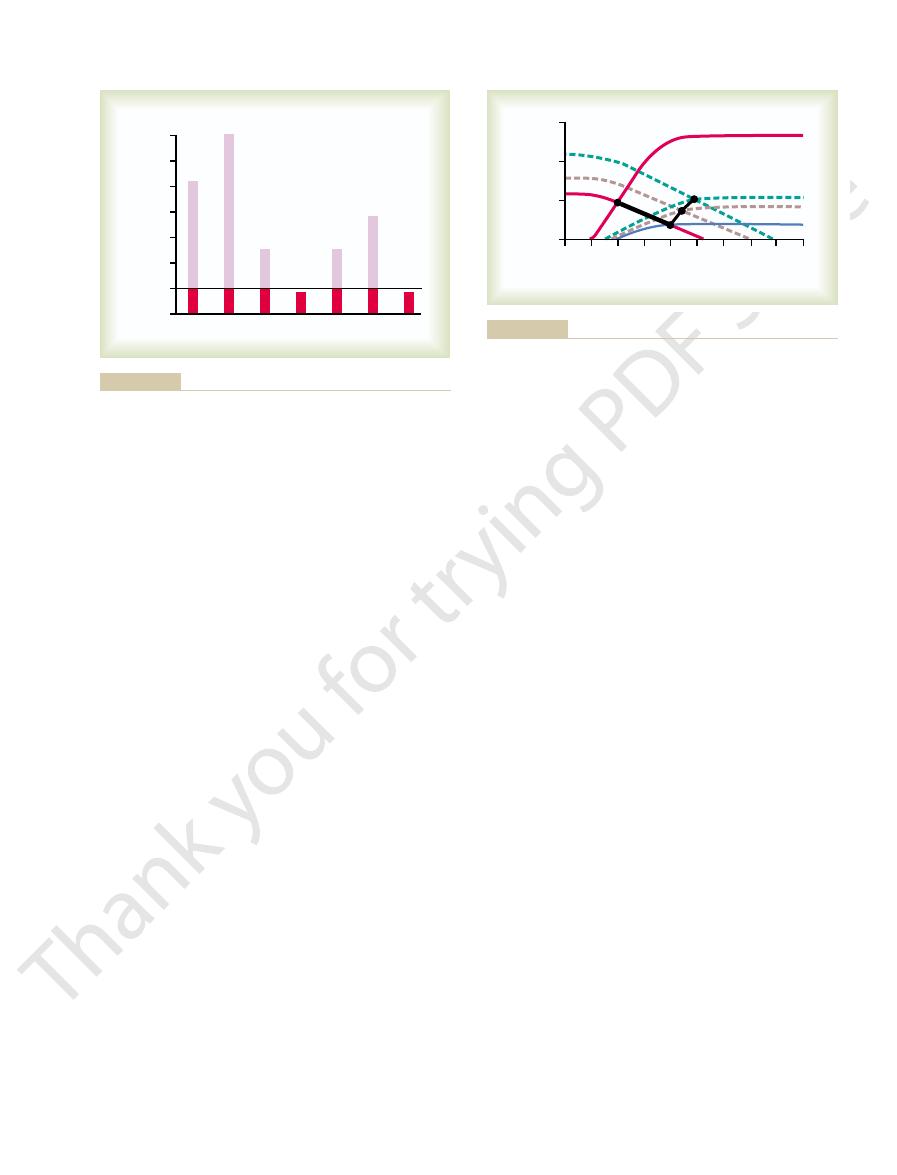
Note the straight line in Figure 22–2, at a cardiac
tatively in the following way.
cause of death. These events can be explained quanti-
to cause adequate kidney excretion of fluid; therefore,
good condition, but this state will not remain stable
to 5 mm Hg. The person appears to be in reasonably
tion has begun. At this time, the cardiac output has
compensation has occurred, and point B, the state a
severely weakened. Point A on this curve represents
ent times (points A to F) after the heart has become
Figure
Thus, the main cause of decom-
pensated heart failure.
events eventually leads to death. This is called
develops more and more edema, and this state of
Therefore, fluid continues to be retained, the person
sequence, the cardiac output cannot rise high enough
ened heart pump a normal cardiac output. As a con-
or by fluid retention, can make the excessively weak-
Cardiac Failure
Chapter 22
261
to make the kidneys excrete normal quantities of fluid.
decom-
pensated heart failure is failure of the heart to pump
sufficient blood to make the kidneys excrete daily the
necessary amounts of fluid.
Graphical Analysis of Decompensated Heart Failure.
22–2 shows greatly depressed cardiac output at differ-
the approximate state of the circulation before any
few minutes later after sympathetic stimulation has
compensated as much as it can but before fluid reten-
risen to 4 L/min and the right atrial pressure has risen
because the cardiac output has not risen high enough
fluid retention continues and can eventually be the
ical cardiac output level that is required in the normal
adult person to make the kidneys re-establish normal
nisms discussed in the earlier section remain in play
And because of this progressive increase in fluid
point C—the right atrial pressure rising to 7 mm Hg
the cardiac output is still not high enough to cause
output is not enough to establish normal fluid
cardiac function is beginning to decline toward a lower
now clear that further retention of fluid will be more
cardiac output still is not high enough to bring about
only continues but accelerates because of the falling
cardiac output (and falling arterial pressure that also
with the cardiac output now less than 2.5 L/min and
failure continues to worsen is called decompensated
heart failure.
the cardiac output (and arterial pressure) to rise to the
critical level required for normal renal function results
in (1) progressive retention of more and more fluid,
which causes (2) progressive elevation of the mean
of the right atrial pressure until finally the heart is so
overstretched or so edematous that it cannot pump
tion of decompensation principally by the progressing
to bubbling rales in the lungs and to dyspnea (air
therapy when this state of events occurs leads to rapid
death.
process can often be stopped by (1) strengthening the
heart
digitalis
the heart becomes strong enough to pump adequate
quantities of blood required to make the kidneys func-
administering diuretic drugs
to increase kidney excretion while at the same time
balance between fluid intake and output despite low
cardiac output.
4
0
+4
+8
+12
+16
(L
/min)
0
2.5
5.0
Cardiac output
–
Right atrial pressure (mm Hg)
A
F
B
C
D
E
Critical cardiac output level
for normal fluid balance
from point A to point F, until death occurs.
pressure over a period of days, and the cardiac output progresses
. Progressive fluid retention raises the right atrial
heart disease
Greatly depressed cardiac output that indicates
Figure 22–2
decompensated
can be elevated high enough, the coronary blood flow
to sustain the arterial pressure. If the arterial pressure
blood, plasma, or a blood pressure–raising drug is used
shows signs of deterioration. Also, infusion of whole
problems in the management of acute heart attacks.
pressure) to a life-sustaining level. Therefore, treat-
Physiology of Treatment.
this reason, in treating myocardial infarction, it is
set off a vicious circle of cardiac deterioration. For
even a small decrease in arterial pressure can now
pressure falls below 80 to 90 mm Hg. In other words,
vessel, deterioration sets in when the coronary arterial
before cardiac deterioration sets in. However, in a
For instance, in a healthy heart, the arterial pres-
pounded by already existing coronary vessel blockage.
by myocardial infarction, this problem is greatly com-
of cardiac deterioration. In cardiogenic shock caused
worse, the process eventually becoming a vicious circle
pressure fall still more, which makes the shock still
makes the heart still weaker, which makes the arterial
reduces the coronary blood supply even more. This
is, the low arterial pressure that occurs during shock
supply is reduced during the course of the shock. That
emphasizes the tendency for the heart to become pro-
The discussion of circulatory shock in Chapter 24
ops cardiogenic shock, the survival rate is often less
. Once a person devel-
cardiac shock
shock
cardiogenic
tening death. This circulatory shock syndrome caused
with the remainder of the body), deteriorates, thus has-
system suffers from lack of nutrition, and it, too (along
explained in Chapter 24. Even the cardiovascular
The picture then is one of circulatory shock, as
often leading to death within a few hours to a few days.
body tissues begin to suffer and even to deteriorate,
required to keep the body alive. Consequently, all the
cardiac deterioration, the heart becomes incapable of
Cardiogenic Shock
Low-Output Cardiac Failure—
which we discuss more fully later in the chapter.
it can cause death by suffocation in 20 to 30 minutes,
. In severe, acute left heart failure,
Thus, among the most important problems of left
stitial spaces and alveoli, resulting in pulmonary
osmotic pressure of the plasma, about 28 mm Hg, fluid
pulmonary capillary pressure increases, and if this rises
As the volume of blood in the lungs increases, the
a result, the
by the left heart into the systemic circulation. As
be pumped into the lungs with usual right heart vigor,
comitant failure of the right side, blood continues to
When the left side of the heart fails without con-
unilateral heart failure.
without significant failure of the left side. Therefore,
sided failure, and in rare instances, the right side fails
failure, left-sided failure predominates over right-
number of patients, especially those with early acute
sidered failure of the heart as a whole. Yet, in a large
In the discussions thus far in this chapter, we have con-
Unilateral Left Heart Failure
slightly.
mechanism a moderate amount using digitalis, allow-
increase the muscle contractile force. Therefore, it is
case of a failing heart, extra calcium is needed to
pumps calcium ions out of the muscle. However, in the
brane of the cardiac muscle fibers. This pump normally
cause full contraction of the muscle. One effect of dig-
therefore, cannot release enough calcium ions into
failing heart muscle, the sarcoplasmic reticulum fails
the quantity of calcium ions in muscle fibers. In the
heart failure.
myocardium as much as 50 to 100 per cent. Therefore,
person with a chronically failing heart, the same drugs
the cardiac muscle. However, when administered to a
administered to a person with a healthy heart, have
Cardiotonic drugs, such as digitalis, when
Mechanism of Action of the Cardiotonic Drugs Such as
re-establishing normal fluid balance, so that at least as
262
Unit IV
The Circulation
Both methods stop the decompensation process by
much fluid leaves the body as enters it.
Digitalis.
little effect on increasing the contractile strength of
can sometimes increase the strength of the failing
they are one of the mainstays of therapy in chronic
Digitalis and other cardiotonic glycosides are
believed to strengthen heart contraction by increasing
to accumulate normal quantities of calcium and,
the free-fluid compartment of the muscle fibers to
italis is to depress the calcium pump of the cell mem-
usually beneficial to depress the calcium pumping
ing the muscle fiber intracellular calcium level to rise
we need especially to discuss the special features of
whereas it is not pumped adequately out of the lungs
mean pulmonary filling pressure rises
because of shift of large volumes of blood from the sys-
temic circulation into the pulmonary circulation.
above a value approximately equal to the colloid
begins to filter out of the capillaries into the lung inter-
edema.
heart failure are pulmonary vascular congestion and
pulmonary edema
pulmonary edema occasionally occurs so rapidly that
In many instances after acute heart attacks and
often after prolonged periods of slow progressive
pumping even the minimal amount of blood flow
by inadequate cardiac pumping is called
or simply
than 15 per cent.
Vicious Circle of Cardiac Deterioration in Cardiogenic Shock.
gressively more damaged when its coronary blood
sure usually must be reduced below about 45 mm Hg
heart that already has a blocked major coronary
extremely important to prevent even short periods of
hypotension.
Often a patient dies of cardio-
genic shock before the various compensatory
processes can return the cardiac output (and arterial
ment of this condition is one of the most important
Immediate administration of digitalis is often used
for strengthening the heart if the ventricular muscle
cortex. But some of the increase in aldosterone
This results mainly from the effect of angiotensin
stage of heart failure, large quantities of
3. Increased aldosterone secretion.
body.
into the urine decreases greatly, and large
from the tubules. Therefore, loss of water and salt
surrounding the renal tubules, promoting greatly
the blood flow through the kidneys, which
19. The angiotensin in turn has a direct effect on
, as described in Chapter
by the kidneys, and this in turn causes the
The reduced blood flow to the
renal tubules.
increased reabsorption of water and salt by the
2. Activation of the renin-angiotensin system and
about one-half normal, this can result in almost
When the cardiac output falls to
filtration rate becomes less than normal. It is
mildest degrees of heart failure, the glomerular
. As a consequence, except in the
cardiac output has a tendency to reduce the
1. Decreased glomerular filtration.
equally important but in different ways.
output of urine during cardiac failure, all of which are
There are three known causes of the reduced renal
, thus causing loss of fluid into the tissues and
the capillary pressure now also rises
Therefore,
dency for blood to return to the heart. This elevates
systemic filling pressure, resulting in increased ten-
. The retention of fluid increases the mean
because of fluid retention by
right-ventricular heart failure, peripheral edema does
Heart Failure
Long-Term Fluid Retention by the Kidneys—
pheral edema.
rience in humans, show that acute cardiac failure
. Therefore, animal experiments, as well as expe-
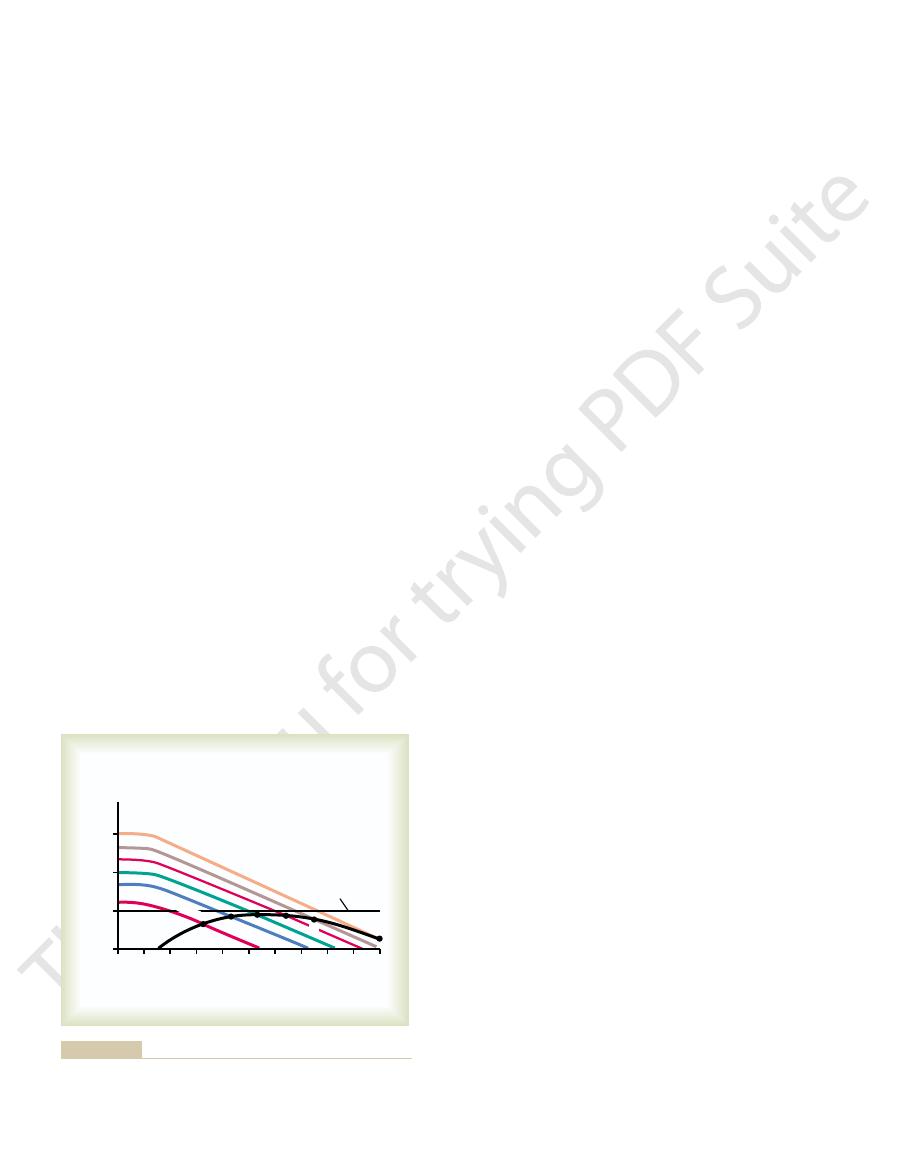
severe acute cardiac failure often
of 13 mm Hg. Thus,
13 mm Hg. Capillary pressure also falls from its normal
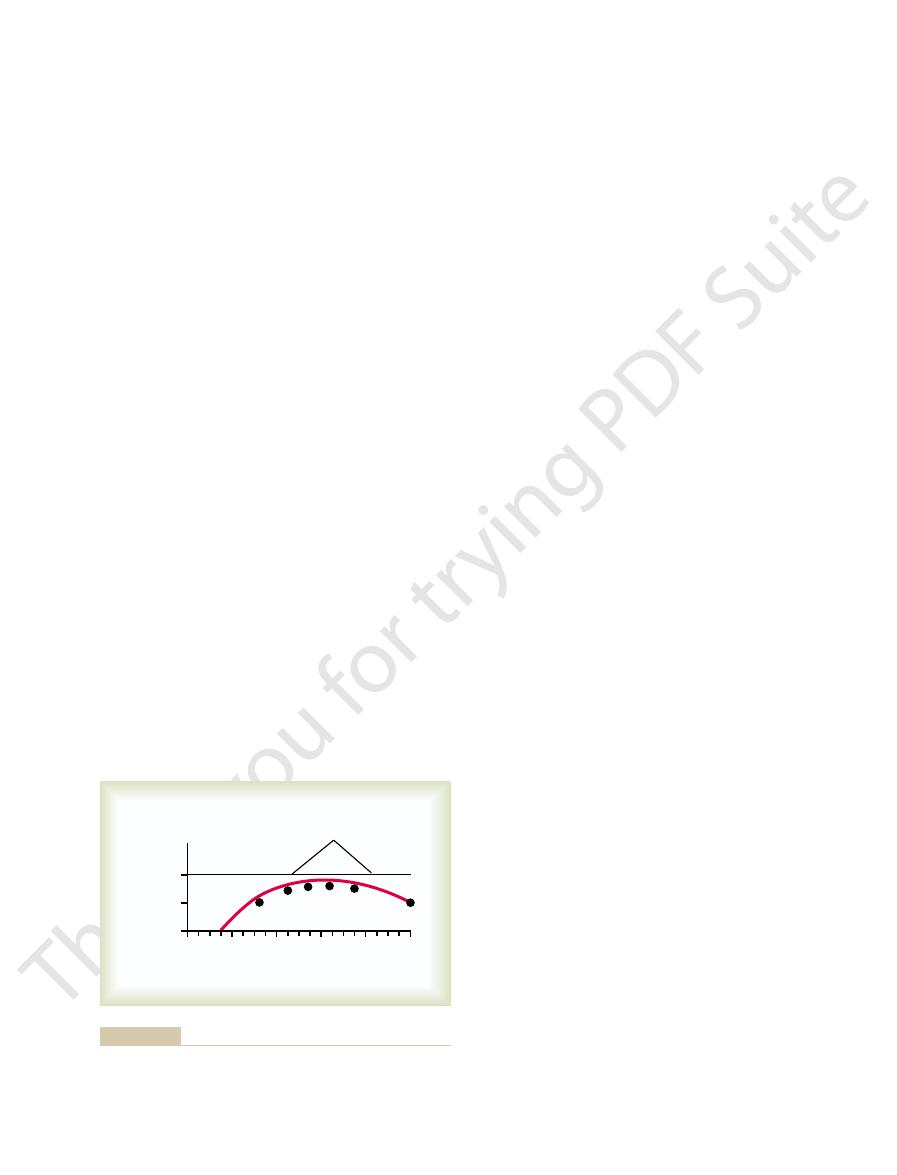
cardiac output approaches zero, these two pressures
pressure falls and the right atrial pressure rises. As the
ously healthy heart acutely fails as a pump, the aortic
explained by referring to Figure 22–3. When a previ-
. This can best be
However, either left or right heart failure is very
hours.
congestion of the lungs, with development of
Cardiac Failure
if any, benefit after 3 hours.
within the first hour of cardiogenic shock but of little,
dissolution of the clot. The results occasionally are
coronary bypass graft, or (2) catheterizing the blocked
clot in the coronary artery, often in combination with
the following procedures: (1) surgically removing the
of deterioration. And this allows enough time for
Cardiac Failure
Chapter 22
263
often will increase enough to prevent the vicious circle
appropriate compensatory mechanisms in circulatory
system to correct the shock.
Some success has also been achieved in saving the
lives of patients in cardiogenic shock by using one of
coronary artery and infusing either streptokinase or
tissue-type plasminogen activator enzymes that cause
astounding when one of these procedures is instituted
Edema in Patients with
Inability of Acute Cardiac Failure to Cause Peripheral Edema.
Acute left heart failure can cause terrific and rapid
pul-
monary edema and even death within minutes to
slow to cause peripheral edema
approach each other at an equilibrium value of about
value of 17 mm Hg to the new equilibrium pressure
causes a fall in peripheral capillary pressure rather than
a rise
almost never causes immediate development of peri-
The Cause of Peripheral Edema in Persisting
After the first day or so of overall heart failure or of
begin to occur principally
the kidneys
the right atrial pressure to a still higher value and
returns the arterial pressure back toward normal.
markedly
development of severe edema.
A decrease in
glomerular pressure in the kidneys because
of (1) reduced arterial pressure and (2) intense
sympathetic constriction of the afferent arterioles
of the kidney
clear from the discussion of kidney function in
Chapters 26 through 29 that even a slight decrease
in glomerular filtration often markedly decreases
urine output.
complete anuria.
kidneys causes marked increase in renin secretion
formation of angiotensin
the arterioles of the kidneys to decrease further
especially reduces the pressure in the capillaries
increased reabsorption of both water and salt
quantities of salt and water accumulate in the
blood and interstitial fluids everywhere in the
In the chronic
aldosterone are secreted by the adrenal cortex.
to stimulate aldosterone secretion by the adrenal
secretion often results from increased plasma
Normal
1/2 Normal
Zero
0
20
40
60
80
100
Pressure (mm Hg)
Cardiac output
Mean aortic pressure
Capillary pressure
Right atrial pressure
13 mm Hg
falls from normal to zero.
capillary pressure, and right atrial pressure as the cardiac output
Progressive changes in mean aortic pressure, peripheral tissue
Figure 22–3

uses up the small amount of reserve that is available,
cardiac output. The increased load on the heart rapidly
down steps, either of which requires greatly increased
disease. However, a diagnosis of low cardiac reserve
rest, they usually will not know that they have heart
Diagnosis of Low Cardiac Reserve—Exercise Test.
which are shown in Figure 22–4.
valvular heart disease, and many other factors, some of
cardiac muscle, physical damage to the myocardium,
myocardial disease, vitamin deficiency that affects
This can result from ischemic heart disease, primary
blood satisfactorily will decrease the cardiac reserve.
a cardiac reserve of 400 per cent
cent—that is,
normal; this is an increase above normal of 400 per
reserve, during severe exercise the cardiac output of a
there is no cardiac reserve. As an example of normal
is occasionally 500 to 600 per cent. But in heart failure,
300 to 400 per cent. In athletically trained persons, it
Thus, in the healthy young adult, the cardiac reserve is
cardiac reserve
The maximum percentage that the cardiac output can
Cardiac Reserve
cessful must be instituted immediately.
to 1 hour. Therefore, any procedure that is to be suc-
This vicious circle of acute pulmonary edema can
drug, such as digitalis, to strengthen the heart
5. Giving the patient a rapidly acting cardiotonic
deterioration, and the peripheral vasodilation
reverse the blood oxygen desaturation, the heart
4. Giving the patient pure oxygen to breathe to
furosemide, to cause rapid loss of fluid from the
3. Giving a rapidly acting diuretic, such as
2. Bleeding the patient
therefore, decrease the workload on the left side
1. Putting tourniquets on both arms and legs to
ures that can reverse the process and save the patient’s
within minutes. The types of heroic therapeutic meas-
certain critical point, it will continue until death of the
Thus, a vicious circle has been established.
desaturation, more venous return, and so forth.
more transudation of fluid, more arterial oxygen
damming of the blood in the lungs, leading to still
6. The increased venous return further increases the
still more.
5. The peripheral vasodilation increases venous
everywhere in the body, thus causing peripheral
4. The decreased oxygen in the blood further
3. The increased fluid in the lungs diminishes the
pulmonary capillary pressure, and a small amount
2. The increased blood in the lungs elevates the
begins to dam up in the lungs.
limited pumping capacity of the left heart, blood
left ventricle initiates the vicious circle. Because of
1. A temporarily increased load on the already weak
The acute pulmonary edema is believed to result from
cise, some emotional experience, or even a severe cold.
heart, such as might result from a bout of heavy exer-
occurs in a person without new cardiac damage, it
had chronic heart failure for a long time. When this
Failure—Another Lethal Vicious Circle
Acute Pulmonary Edema in Late-Stage Heart
toms during cardiac failure. The renal effects of ANF
excretion of salt and water. Therefore, ANF plays a
to tenfold in severe heart failure. The ANF in turn has
culating levels of ANF in the blood increase fivefold
left atrial pressures that stretch the atrial walls, the cir-
they become stretched. Because heart failure almost
tubular reabsorption of water.
(discussed in Chapter 29). The antidiuretic
fluid everywhere in the body. This elicits
with the sodium, mainly chloride ions, increase
Second, the absorbed sodium and anions that go
pressure in the renal interstitial fluids; these
sodium is reabsorbed, it reduces the osmotic
in water reabsorption for two reasons: First, as the
tubules. This in turn leads to a secondary increase
The elevated aldosterone level further increases
to reduced renal function in cardiac failure.
potassium. Excess potassium is one of the most
264
Unit IV
The Circulation
powerful stimuli known for aldosterone secretion,
and the potassium concentration rises in response
the reabsorption of sodium from the renal
pressure in the tubules but increases the osmotic
changes promote osmosis of water into the blood.
the osmotic concentration of the extracellular
antidiuretic hormone secretion by the
hypothalamic–posterior pituitary gland system
hormone in turn promotes still greater increase in
Role of Atrial Natriuretic Factor to Delay Onset of Cardiac
Decompensation.
Atrial natriuretic factor (ANF) is a
hormone released by the atrial walls of the heart when
always causes excessive increase in both the right and
a direct effect on the kidneys to increase greatly their
natural role to help prevent extreme congestive symp-
are discussed in Chapter 29.
A frequent cause of death in heart failure is acute pul-
monary edema occurring in patients who have already
usually is set off by some temporary overload of the
the following vicious circle:
of fluid begins to transude into the lung tissues
and alveoli.
degree of oxygenation of the blood.
weakens the heart and also weakens the arterioles
vasodilation.
return of blood from the peripheral circulation
Once this vicious circle has proceeded beyond a
patient unless heroic therapeutic measures are used
life include the following:
sequester much of the blood in the veins and,
of the heart
body
proceed so rapidly that death can occur in 20 minutes
increase above normal is called the
.
healthy young adult can rise to about five times
.
Any factor that prevents the heart from pumping
As long as
persons with low cardiac reserve remain in a state of
usually can be easily made by requiring the person to
exercise either on a treadmill or by walking up and
is, at a right atrial pressure of
venous return curves now equilibrate at point C, that
the right and upward. The new cardiac output and
Hg up to 10 mm Hg. This increase in mean systemic
mercury—in this figure, from a normal value of 7 mm
output curve as much as 30 to 100 per cent. It can also
return curves, raising both of them
They affect both the cardiac output and the venous
seconds, the sympathetic reflexes become very active.
Within the next 30
ately to 4 mm Hg, whereas the cardiac output falls to
curve. Thus, the right atrial pressure rises immedi-
circulation is depicted by point B, where the new
still operating normally. Therefore, the new state of the
few seconds, the venous return curve still has not
. During these
lowermost curve
after a moderately severe heart attack, the cardiac
0 mm Hg.
is where the two curves cross at point A. Therefore, the
at which the circulatory system can operate. This point
20, there is only one point on each of these two curves
. As pointed out in Chapter
normal cardiac output curve
circulation. The two curves passing through Point A
cardiac output
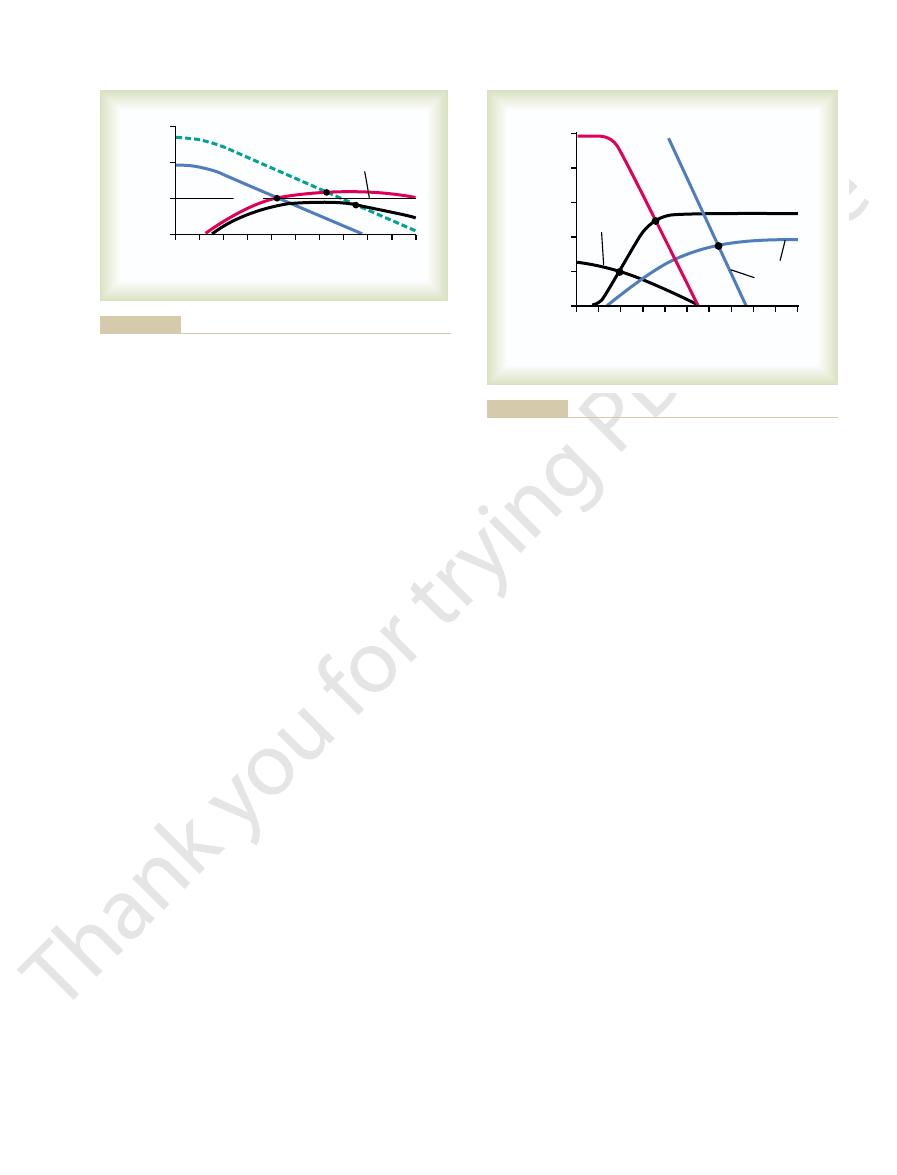
Figure 22–5 shows
Chronic Compensation
Graphical Analysis of Acute Heart Failure and
using this graphical technique.
chapter, we analyze several aspects of cardiac failure,
duced in Chapter 20. In the remaining sections of this
tive approaches. One such approach is the graphical
logic, as we have done thus far in this chapter, one can
Quantitative Graphical Method for
in most clinical settings.
cardiologist. These tests take the place of cardiac
3. Excessive increase in heart rate because the
ischemia, thus limiting the person’s ability to
2. Extreme muscle fatigue resulting from muscle
heart to pump sufficient blood to the tissues,
1. Immediate and sometimes extreme shortness of
to sustain the body’s new level of activity. The acute
Cardiac Failure
Chapter 22
265
and the cardiac output soon fails to rise high enough
effects are as follows:
breath (dyspnea) resulting from failure of the
thereby causing tissue ischemia and creating a
sensation of air hunger
continue with the exercise
nervous reflexes to the heart overreact in an
attempt to overcome the inadequate cardiac
output
Exercise tests are part of the armamentarium of the
output measurements that cannot be made with ease
Analysis of Cardiac Failure
Although it is possible to understand most general
principles of cardiac failure using mainly qualitative
grasp the importance of the different factors in cardiac
failure with far greater depth by using more quantita-
method for analysis of cardiac output regulation intro-
and venous return
curves for different states of the heart and peripheral
are (1) the
and (2) the
normal venous return curve
normal state of the circulation is a cardiac output and
venous return of 5 L/min and a right atrial pressure of
Effect of Acute Heart Attack.
During the first few seconds
output curve falls to the
changed because the peripheral circulatory system is
cardiac output curve crosses the normal venous return
2 L/min.
Effect of Sympathetic Reflexes.
. Sympathetic stim-
ulation can increase the plateau level of the cardiac
increase the mean systemic filling pressure (depicted
by the point where the venous return curve crosses the
zero venous return axis) by several millimeters of
filling pressure shifts the entire venous return curve to
+5 mm Hg and a cardiac
output of 4 L/min.
0
100
200
300
400
500
600
Cardiac reserve (%)
Moderate
coronary
disease
Diphtheria
Severe
coronary
thrombosis
Mild
valvular
disease
Severe
valvular
disease
Athlete
Normal
Normal
operation
reserve for two of the conditions.
Cardiac reserve in different conditions, showing less than zero
Figure 22–4
venous return (L
/min)
2
0
2
4
6
8
10
12
14
0
5
10
15
–4
–
Cardiac output and
Right atrial pressure (mm Hg)
A
B
C
D
Normal
during different stages of cardiac failure.
Progressive changes in cardiac output and right atrial pressure
Figure 22–5
and a right atrial pressure of 4.6 mm Hg. This cardiac
digitalized heart at point H, at an output of 5 L/min
becomes the curve labeled “Several days later.” This
down to 11.5 mm Hg, and the new venous return curve
The progressive loss of fluid over a period of several
effect of digitalis.
, a well-known therapeutic
normally, causing
Therefore, the kidneys eliminate much more fluid than
make the kidneys excrete normal amounts of urine.
point G. The cardiac output is now 5.7 L/min, a value
the venous return curve. Therefore, the new cardiac
Figure 22–7, but there is not an immediate change in
time, digitalis is given to strengthen the heart. This
proceed to the same point E in Figure 22–7. At this
already reached point E in Figure 22–6, and let us
Treatment of Decompensated Heart Disease with Digitalis.
Thus, “decompensation” results from the fact that
erates downhill until death occurs.
mental effect on cardiac output. The condition accel-
cardiac output curve, so that further retention of fluid
to point D, to point E, and, finally, to point F. The equi-
venous return curve continues to shift to the right, and
mean systemic filling pressure continues to rise, the
renal function. Fluid continues to be retained, the
During the succeeding days, the cardiac output
atrial pressure to 7 mm Hg.
C. The cardiac output rises to 4.2 L/min and the right
venous return curve becomes that labeled “2nd day”
pressure rises from 10.5 to almost 13 mm Hg. Now the
tinues to be retained, and the mean systemic filling
the kidneys to function normally. Therefore, fluid con-
The cardiac output of 4 L/min is still too low to cause
pressure to 5 mm Hg.
equates with the cardiac output curve at point B. The
compensation.” Thus, the new venous return curve
the right to produce the curve labeled “autonomic
Hg. This shifts the venous return curve upward and to
this low cardiac output, increases the mean systemic
ulation of the sympathetic nervous system, caused by
give a cardiac output of about 3 L/min. However, stim-
curve to this low level. At point A, the curve at time
great as this heart can achieve. In this figure, we have
curve that has already reached a degree of recovery as
same as the curve shown in Figure 22–2, a very low
The black cardiac output curve in Figure 22–6 is the
Cardiac Failure
manner.
Figure 22–5, they are presented in a more quantitative
the same as those presented in Figure 22–1, but in
Note that the events described in Figure 22–5 are
degrees of heart failure.
culation in mild to moderate heart failure. And one
Using this technique for analysis, one can see espe-
curve.
pressure, until some additional extrinsic factor changes
continue to function at point D and remain stable, with
balance has been achieved. The circulatory system will
normal, so that a new state of equilibrated fluid
the cardiac output is now normal, renal output is also
6 mm Hg. Because
however, has risen still further to
now returned to normal. The right atrial pressure,
equilibrate at point D. Thus, the cardiac output has
12 mm Hg. The two new curves now
heart and (2) renal retention of salt and water, which
ensuing week, the cardiac output and venous return
266
Unit IV
The Circulation
Compensation During the Next Few Days.
During the
curves rise further because of (1) some recovery of the
raises the mean systemic filling pressure still further—
this time up to
+
+
a normal cardiac output and an elevated right atrial
either the cardiac output curve or the venous return
cially the importance of moderate fluid retention and
how it eventually leads to a new stable state of the cir-
can also see the interrelation between mean systemic
filling pressure and cardiac pumping at various
Graphical Analysis of “Decompensated”
added venous return curves that occur during succes-
sive days after the acute fall of the cardiac output
zero equates with the normal venous return curve to
filling pressure within 30 seconds from 7 to 10.5 mm
cardiac output has been improved to a level of 4 L/min
but at the expense of an additional rise in right atrial
and equilibrates with the cardiac output curve at point
never rises quite high enough to re-establish normal
the equilibrium point between the venous return curve
and the cardiac output curve also shifts progressively
libration process is now on the down slope of the
causes only more severe cardiac edema and a detri-
the cardiac output curve never rises to the critical level
of 5 L/min needed to re-establish normal kidney excre-
tion of fluid that would be required to cause balance
between fluid input and output.
Let
us assume that the stage of decompensation has
raises the cardiac output curve to the level shown in
output curve equates with the venous return curve at
greater than the critical level of 5 liters required to
diuresis
days reduces the mean systemic filling pressure back
curve equates with the cardiac output curve of the
Cardiac output and venous return (L
/min)
2
0
2
4
6
8
10
12
14
16
0
5
10
15
–4
–
Right atrial pressure (mm Hg)
8th day
6th day
4th day
2nd day
Critical cardiac
output level
for normal
fluid balance
A
u
t
onomic
com
pens
ation
A
B
C
D
F
Normal ven
ous
return
E
of continued fluid retention.
progressive shift of the venous return curve to the right as a result
Graphical analysis of decompensated heart disease showing
Figure 22–6
level of the cardiac output curve.
weak heart, as demonstrated by the depressed plateau
normal; this high cardiac output occurs despite the
beriberi, with a right atrial pressure in this instance of
point C, which describes the circulatory condition in
The two blue curves (cardiac output curve and
explained in Chapter 17.
minosis has dilated the peripheral blood vessels, as
the right. Finally, the venous return curve has rotated
11 mm Hg. This has shifted the venous return curve to
fluid, which in turn has increased the mean systemic
decreased the blood flow to the kidneys. Therefore, the
the beriberi syndrome. The weakening of the heart has
. The decreased level of the cardiac output
Figure 22–8 shows the approximate changes
and is called “high-output failure,” but in reality, the
fistula. This condition resembles a failure condition
eral congestion. If the person attempts to exercise, he
is slightly elevated, and there are mild signs of periph-
has become greatly elevated, the right atrial pressure
atrial pressure of 3 mm Hg. Thus, the cardiac output
point B, with a cardiac output of 12.5 L/min and a right
the curve labeled “AV fistula.” This venous return
vein). The venous return curve rotates upward to give
min and a normal right atrial pressure of 0 mm Hg.
venous return curves. These equate with each other at
The “normal” curves of Figure
cular resistance, but at the same time, the pumping
, in which the venous return is
capability of the heart is not depressed. The other is
of excessive venous return, even though the pumping
arteriovenous fistula
output cardiac failure. One of these is caused by an
Figure 22–8 gives an analysis of two types of high-
Cardiac Failure
for normal fluid balance. The compensatory mecha-
curve, the venous return curve, and the critical level
the crossing point of three curves: the cardiac output
pensated.” And to state this another way, the final
decompensation of the heart failure has been “com-
system has now stabilized, or in other words, the
none will be gained. Consequently, the circulatory
balance. Therefore, no additional fluid will be lost and
Cardiac Failure
Chapter 22
267
output is precisely that required for normal fluid
steady-state condition of the circulation is defined by
nisms automatically stabilize the circulation when all
three curves cross at the same point.
Graphical Analysis of High-Output
that overloads the heart because
caused by beriberi
greatly increased because of diminished systemic vas-
capability of the heart is depressed.
Arteriovenous Fistula.
22–8 depict the normal cardiac output and normal
point A, which depicts a normal cardiac output of 5 L/
Now let us assume that the systemic resistance (the
total peripheral resistance) becomes greatly decreased
because of opening a large arteriovenous fistula (a
direct opening between a large artery and a large
curve equates with the normal cardiac output curve at
or she will have little cardiac reserve because the heart
is already being used almost to maximum capacity to
pump the extra blood through the arteriovenous
heart is overloaded by excess venous return.
Beriberi.
in the cardiac output and venous return curves caused
by beriberi
curve is caused by weakening of the heart because of
the avitaminosis (mainly lack of thiamine) that causes
kidneys have retained a large amount of extra body
filling pressure (represented by the point where the
venous return curve now intersects the zero cardiac
output level) from the normal value of 7 mm Hg up to
upward from the normal curve because the avita-
venous return curve) intersect with each other at
9 mm Hg and a cardiac output about 65 per cent above
venous return (L
/min)
2
0
2
4
6
8
10 12 14 16
0
5
10
15
–4 –
Cardiac output and
Right atrial pressure (mm Hg)
Critical cardiac output
level for normal
fluid balance
G
E
H
S
e
veral d
ays
later
Se
ver
ely
failing
hea
rt
Di
git
ali
ze
d h
ear
t
First da
y
increased urine output and progressive shift of the venous return
digitalis in elevating the cardiac output curve, this in turn causing
Treatment of decompensated heart disease showing the effect of
Figure 22–7
curve to the left.
venous return (L
/min)
2
0
2
4
6
8
10 12 14 16
0
5
10
15
20
25
–4 –
Cardiac output and
Right atrial pressure (mm Hg)
B
A
C
AV fistula
Normal cardiac
output curve
Beriberi
heart
disease
Normal
venous
return
curve
beriberi heart disease.
output cardiac failure: (1) arteriovenous (AV) fistula and (2)
Figure 22–8
Graphical analysis of two types of conditions that can cause high-
and treatment. Circulation 105:1503, 2002.
tion and diastolic heart failure: Part II: causal mechanisms
Zile MR, Brutsaert DL: New concepts in diastolic dysfunc-
105:1387, 2002.
sis, and measurements of diastolic function. Circulation
tion and diastolic heart failure: Part I: diagnosis, progno-
Zile MR, Brutsaert DL: New concepts in diastolic dysfunc-
349:684, 2003.
Spodick DH: Acute cardiac tamponade. N Engl J Med
contraction coupling. J Physiol 546:33, 2003.
Sjaastad I, Wasserstrom JA, Sejersted OM: Heart failure—
with renal insufficiency. Ann Intern Med 138:917, 2003.
Shlipak MG: Pharmacotherapy for heart failure in patients
failure. Endocr Rev 24:341, 2003.
Ruskoaho H: Cardiac hormones as diagnostic tools in heart
infarction and cardiogenic shock. Lancet 362:392, 2003.
Pfisterer M: Right ventricular involvement in myocardial
gestive heart failure: Part II. Circulation 105:2223, 2002
McMurray J, Pfeffer MA: New therapeutic options in con-
gestive heart failure: Part I. Circulation 105:2099, 2002.
McMurray J, Pfeffer MA: New therapeutic options in con-
Curr Cardiol Rep 6:96, 2004.
tion in chronic heart failure: more questions than answers?
Mehra MR, Gheorghiade M, Bonow RO: Mitral regurgita-
Integr Comp Physiol 283:R810, 2002.
in hemorrhage and heart failure. Am J Physiol Regul
Lohmeier TE: Neurohumoral regulation of arterial pressure
2998, 2003.
dial infarction: expanding the paradigm. Circulation 107:
Hochman JS: Cardiogenic shock complicating acute myocar-
Saunders Co, 1973.
Cardiac Output and Its Regulation. Philadelphia: WB
Guyton AC, Jones CE, Coleman TG: Circulatory Physiology:
left heart failure. Chest 125:669, 2004.
Gehlbach BK, Geppert E: The pulmonary manifestations of
failure. Hypertension 37:342, 2001.
tion in hypertension, ischemic heart disease, and heart
Gavras H, Brunner HR: Role of angiotensin and its inhibi-
Physiol Scand 177:391, 2003.
diverse mechanisms, therapeutic opportunities. Acta
Floras JS: Sympathetic activation in human heart failure:
Coll Cardiol 41(4 Suppl S):70S, 2003.
thrombin inhibitors in acute coronary syndromes. J Am
Eikelboom J, White H, Yusuf S: The evolving role of direct
326:1450, 2003.
cutaneous coronary intervention: cardiogenic shock. BMJ
Ducas J, Grech ED: ABC of interventional cardiology. Per-
lation 109:150, 2004.
tractility in heart failure: data from mice and men. Circu-
Dorn GW 2nd, Molkentin JD: Manipulating cardiac con-
cular Medicine. 6th Ed. Philadelphia: WB Saunders Co,
Braunwald E, Zipes DP, Liby P: A Textbook for Cardiovas-
Andrew P: Diastolic heart failure demystified. Chest 124:744,
268
Unit IV
The Circulation
References
2003.
2001.
a challenge to our current concepts of excitation-
