that would be lethal without immunity. This is the reason the treatment process
tetanus, can be protected against in doses as high as 100,000 times the amount
certain toxins, such as the paralytic botulinum toxin or the tetanizing toxin of
Acquired immunity can often bestow extreme protection. For instance,
phocytes that attack and destroy the specific invading organism or toxin. It is
. Acquired immunity is
animals. This is called
agents such as lethal bacteria, viruses, toxins, and even foreign tissues from other
In addition to its generalized innate immunity, the human body has the ability
Acquired (Adaptive) Immunity
and syphilis, which are very damaging or even lethal to human beings.
to many human diseases, such as poliomyelitis, mumps, human cholera, measles,
afflicted with it. Conversely, many lower animals are resistant or even immune
some paralytic viral infections of animals, hog cholera, cattle plague, and dis-
This innate immunity makes the human body resistant to such diseases as
even some infected cells.
that can recognize and destroy foreign cells, tumor cells, and
activated in various ways to destroy bacteria; and (4)
that is described later, a system of about 20 proteins that can be
inactivate certain types of gram-positive bacteria; (3) the
, which react with and
causes them to dissolute; (2)
, a mucolytic polysaccharide that attacks bacteria and
foreign organisms or toxins and destroy them. Some of these compounds
4. Presence in the blood of certain chemical compounds that attach to
3. Resistance of the skin to invasion by organisms.
and the digestive enzymes.
2. Destruction of swallowed organisms by the acid secretions of the stomach
of the tissue macrophage system, as described in Chapter 33.
1. Phagocytosis of bacteria and other invaders by white blood cells and cells
innate immunity.
at specific disease organisms. This is called
immunity results from general processes, rather than from processes directed
requiring weeks or months to develop the immunity. An additional portion of
attacked by a bacterium, virus, or toxin, often
nity.
tissues and organs. This capability is called
The human body has the ability to resist almost all
Infection: II. Immunity and Allergy
C
H
A
P
T
E
R
3
4
439
Resistance of the Body to
Innate Immunity
types of organisms or toxins that tend to damage the
immu-
Much of immunity is acquired immunity that
does not develop until after the body is first
It includes the
following:
are (1) lysozyme
basic polypeptides
complement
complex
natural killer
lymphocytes
temper—a viral disease that kills a large percentage of dogs that become
to develop extremely powerful specific immunity against individual invading
acquired or adaptive immunity
caused by a special immune system that forms antibodies and/or activated lym-
with this acquired immunity mechanism and some of its associated reactions—
especially the allergies—that this chapter is concerned.
known as immunization is so important in protecting human beings against
of the embryo, these
lymphocyte-committed stem cells
Although all lymphocytes in the body originate from
Lymphocytes
Preprocessing of the T and B
cytes and (2) the antibodies.
mation, respectively, of (1) the activated T lympho-
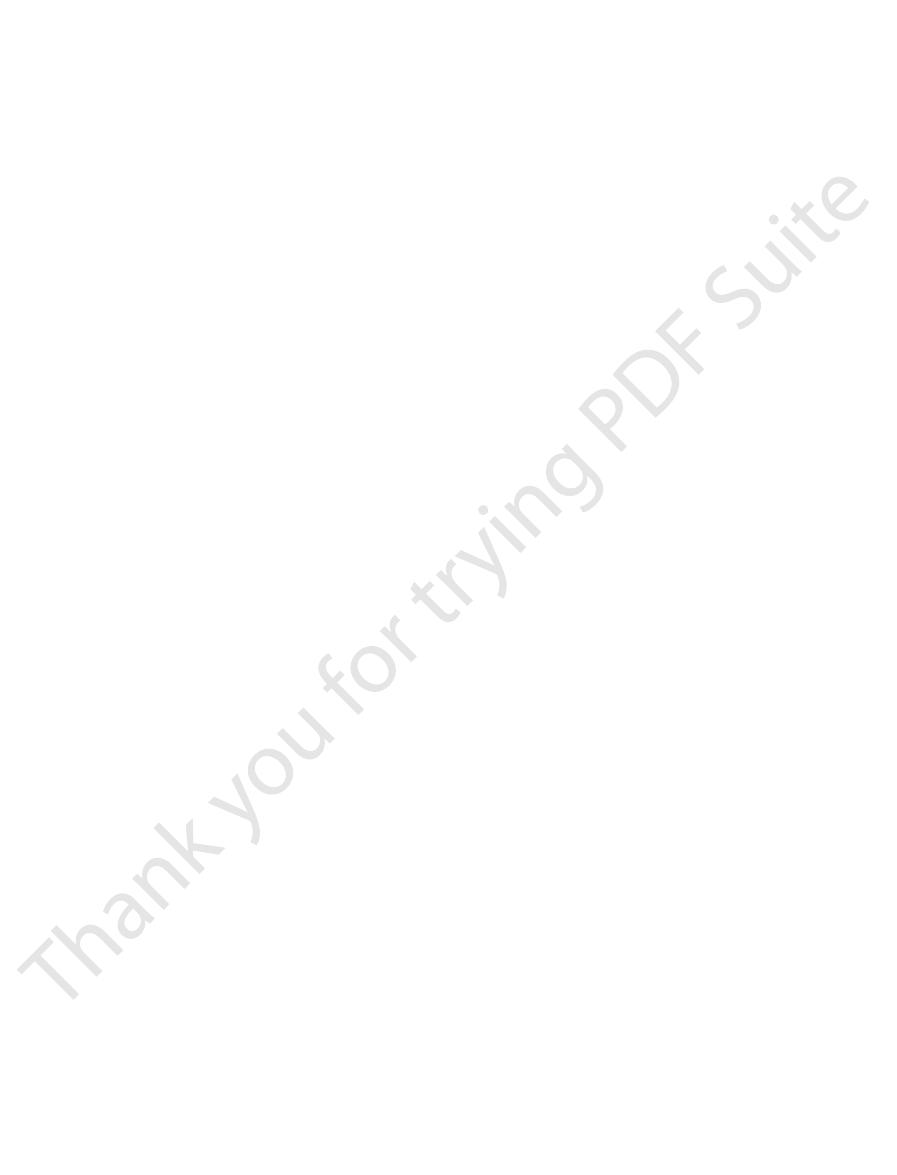
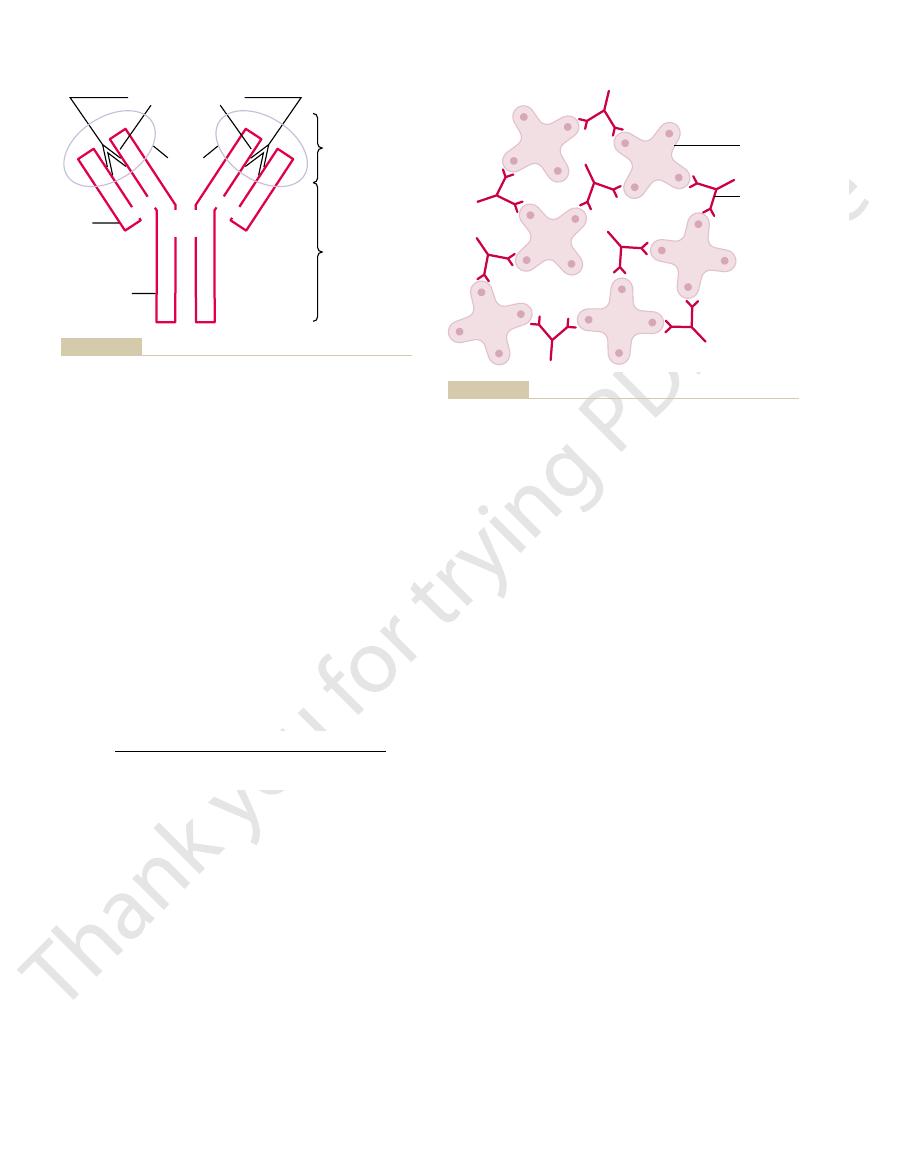
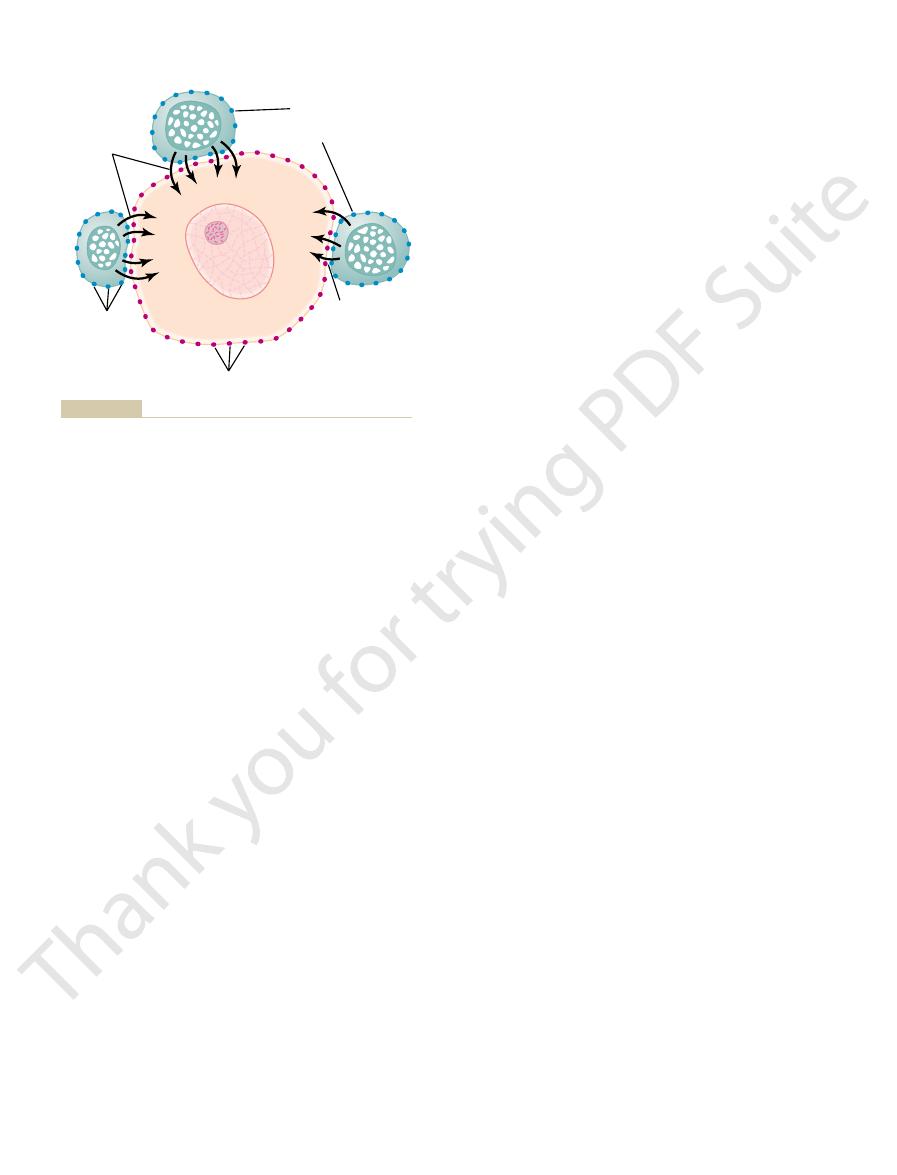
34–1 shows the two lymphocyte systems for the for-
they are responsible for humoral immunity. Figure
to designate the role of the bursa, and
. For this reason, these lymphocytes are called
bursa of Fabri-
ulation of cells was first discovered in birds, which have
bone marrow in late fetal life and after birth. This pop-
phocytes that are destined to form antibodies—are
The other population of lymphocytes—the B lym-
immunity.
the thymus. They are responsible for cell-mediated
“T” lymphocytes
gland, and thus they are
form activated T lymphocytes first migrate to and are
The lymphocytes that are destined to eventually
differentiated or “preprocessed” in the following ways.
lymphoid tissue, but before doing so, they are further
phocytes that are formed eventually end up in the
offspring as they differentiate. Almost all of the lym-
that form lymphocytes as one of their most important
pluripotent hematopoietic stem cells
Both types of lymphocytes are derived originally in
immunity.
for forming antibodies that provide “humoral”
other population, the B lymphocytes, is responsible
cytes that provide “cell-mediated” immunity, and the
cytes, is responsible for forming the activated lympho-
populations. One of the populations, the T lympho-
tissue look alike when studied under the microscope,
Although most lymphocytes in normal lymphoid
or “Humoral” Immunity—the T and the B Lymphocytes.
Two Types of Lymphocytes Promote “Cell-Mediated” Immunity
the spleen, thymus, and bone marrow plays the specific
tissues of the body. And, finally, the lymphoid tissue of
piratory tract. The lymphoid tissue in the lymph nodes
from the gut. The lymphoid tissue of the throat and
instance, the lymphoid tissue of the gastrointestinal
to the lymph node or other lymphoid tissue. For
In most instances, the invading agent first enters the
before they can spread too widely.
The lymphoid tissue is distributed advantageously in
bone marrow
, and
, but they are also found in special lym-
The lymphocytes are located most extensively in the
phocytes are essential to survival of the human being.
by heroic measures. Therefore, it is clear that the lym-
develop. And within days after birth, such a person
by radiation or chemicals, no acquired immunity can
phocytes or whose lymphocytes have been destroyed
phocytes. In people who have a genetic lack of lym-
Acquired immunity is the product of the body’s lym-
Lymphocytes Are Responsible for
eochemical characteristic.
always antigenic, because both of these have this ster-
the surface of the large molecule. This also explains
epitopes,
larly recurring molecular groups, called
a high molecular weight, 8000 or greater. Furthermore,
For a substance to be antigenic, it usually must have
ate the acquired immunity. These substances are called
teins or large polysaccharides, and it is they that initi-
from all other compounds. In general, these are pro-
nizing this invasion. Each toxin or each type of organ-
after invasion by a foreign organism or toxin, it is clear
Initiated by Antigens
Both Types of Acquired Immunity Are
antigens.
phoid tissues of the body. Let us discuss the initiation
and the activated lymphocytes are formed in the lym-
cytes). We shall see shortly that both the antibodies
(because the activated lymphocytes are T lympho-
T-cell immunity
cell-mediated immunity
destroy the foreign agent. This type of immunity is
activated T lymphocytes
B lymphocytes produce the antibodies). The second
attacking the invading agent. This type of immunity is
antibodies,
nity occur in the body. In one of these the body
Two basic but closely allied types of acquired immu-
Basic Types of Acquired Immunity
of this chapter.
disease and against toxins, as explained in the course
Blood Cells, Immunity, and Blood Clotting
440
Unit VI
develops circulating
which are globulin
molecules in the blood plasma that are capable of
called humoral immunity or B-cell immunity (because
type of acquired immunity is achieved through the
formation of large numbers of
that are specifically crafted in the lymph nodes to
called
or
of the immune process by
Because acquired immunity does not develop until
that the body must have some mechanism for recog-
ism almost always contains one or more specific
chemical compounds in its makeup that are different
antigens (antibody generations).
the process of antigenicity usually depends on regu-
on
why proteins and large polysaccharides are almost
Acquired Immunity
dies of fulminating bacterial infection unless treated
lymph nodes
phoid tissues such as the spleen, submucosal areas of
the gastrointestinal tract, thymus
.
the body to intercept invading organisms or toxins
tissue fluids and then is carried by way of lymph vessels
walls is exposed immediately to antigens invading
pharynx (the tonsils and adenoids) is well located to
intercept antigens that enter by way of the upper res-
is exposed to antigens that invade the peripheral
role of intercepting antigenic agents that have suc-
ceeded in reaching the circulating blood.
these cells are distinctly divided into two major
the embryo from
preprocessed in the thymus
called
to designate the role of
preprocessed in the liver during midfetal life and in the
a special preprocessing organ called the
cius
“B”
lymphocytes
areas.
near but slightly removed from the T-lymphocyte
phoid tissue throughout the body, where they lodge
lymphocytes, like the T lymphocytes, migrate to lym-
ferent specific reactivities. After preprocessing, the B
millions of types of B-lymphocyte antibodies with dif-
diversity than the T lymphocytes, thus forming many
33. Second, the B lymphocytes have even greater
and destroying the antigenic substance, which is
that are the reactive agents. These agents are large
phocytes, the B lymphocytes actively secrete
reactivity against the antigen, as occurs for the T lym-
two ways: First, instead of the whole cell developing
B lymphocytes are different from T lymphocytes in
the human being, B lymphocytes are known to be pre-
lymphocytes than for preprocessing T lymphocytes. In
Liver and Bone Marrow Preprocess the B Lymphocytes.
kidneys, one can transplant organs with much less like-
rejection of transplanted organs, such as hearts and
development of all cell-mediated immunity. Because
the T-lymphocytic immune system. However, removal
few months after birth. Beyond this period, removal of
Most of the preprocessing of T lymphocytes in the
a toxin, or even transplanted tissue from another
gens from an outside source, such as from a bacterium,
the body’s own antigens—they react only against anti-
90 per cent of the cells. Thus, the only cells that are
instead of being released. This happens to as many as
lymphocyte reacts, it is destroyed and phagocytized
cific “self-antigens” from the body’s own tissues. If a T
The thymus selects which T lymphocytes will be
lethal to the person’s own body in only a few days.
own tissues; otherwise, the T lymphocytes would be
or other antigens that are present in the body’s
cytes leaving the thymus will not react against proteins
The thymus also makes certain that any T lympho-
to lodge in lymphoid tissue everywhere.
preprocessed T lymphocytes now leave the thymus
sands of different antigens. These different types of
phocytes with specific reactivities against many thou-
ficity against another antigen. This continues until
one antigen. Then the next lymphocyte develops speci-
thymic lymphocyte develops specific reactivity against
reacting against different specific antigens. That is, one
migrate to the thymus gland. Here they divide rapidly
phocytes, after origination in the bone marrow, first
The T lym-
Thymus Gland Preprocesses the T Lymphocytes.
appropriate processing areas as follows.
they can do so, they must be further differentiated in
either activated T lymphocytes or antibodies. Before
Resistance of the Body to Infection: II. Immunity and Allergy
Chapter 34
441
stem cells themselves are incapable of forming directly
and at the same time develop extreme diversity for
there are thousands of different types of thymic lym-
and spread by way of the blood throughout the body
released by first mixing them with virtually all the spe-
finally released are those that are nonreactive against
person.
thymus occurs shortly before birth of a baby and for a
the thymus gland diminishes (but does not eliminate)
of the thymus several months before birth can prevent
this cellular type of immunity is mainly responsible for
lihood of rejection if the thymus is removed from an
animal a reasonable time before its birth.
Much
less is known about the details for preprocessing B
processed in the liver during midfetal life and in the
bone marrow during late fetal life and after birth.
antibod-
ies
protein molecules that are capable of combining with
explained elsewhere in this chapter and in Chapter
T lymphocytes
Thymus
Cell-Mediated Immunity
Humoral Immunity
Antigen
Activated T
lymphocytes
Antigen
Antibodies
Plasma
cells
B lymphocytes
Fetal liver,
bone marrow
Stem cell
Lymph node
and humoral immune processes.
responsible for the cell-mediated
phocytes that respectively are
This figure also shows the origin
node in response to antigens.
Formation of antibodies and sen-
Figure 34–1
sitized lymphocytes by a lymph
of thymic (T) and bursal (B) lym-
immunity.
to describe the mechanisms of the T-cell system of
this cooperative relationship between helper T cells
by the B lymphocytes is usually slight. We will discuss
these helper T cells, the quantity of antibodies formed
specific B lymphocytes. Indeed, without the aid of
, secrete specific substances
formed, called
cytes at the same time. Some of the T cells that are
antigens activate both T lymphocytes and B lympho-
Role of the T Cells in Activation of the B Lymphocytes.
reproduction of the specific lymphocytes. This sub-
macrophages, in addition, secrete a special activating
activation of the specified lymphocytic clones. The
contact directly to the lymphocytes, thus leading to
ucts are liberated into the macrophage cytosol. The
digested by the macrophages, and the antigenic prod-
ing organisms are first phagocytized and partially
to many of the lymph node lymphocytes. Most invad-
and other lymphoid tissue, and they lie in apposition
These line the sinusoids of the lymph nodes, spleen,
of macrophages are also present in the same tissue.
the lymphocytes in lymphoid tissue, literally millions
the surface of the T-cell membrane, and these, too,
), are on
T-cell markers
lymphocytes, molecules similar to antibodies, called
in more detail subsequently. In the case of the T
this leads to the activation process, which we describe
the appropriate antigen comes along, it immediately
only one specific type of antigen. Therefore, when
the case of the B lymphocytes, each of these has on the
characteristics). The reason for this is the following: In
Each clone of lymphocytes is responsive to only a
of Lymphocytes
spread to and populate the lymphoid tissue.
then become the highly specific T and B cells that
for only a single antigen specificity. These mature cells
phocyte that is finally formed, the gene structure codes
types that can occur. For each functional T or B lym-
in which the segments can be arranged in single cells,
segments, as well as millions of different combinations
Because there are several hundred types of gene
whole genes.
in random combinations, in this way finally forming
cessing of the respective T- and B-cell lymphocytes,
such segments—but not whole genes. During prepro-
there are only “gene segments”—actually, hundreds of
which the functional immune cells are formed. Instead,
The whole gene for forming each type of T cell or B
protein. This mystery has now been solved.
can be produced by the lymphoid tissue, especially
ferent specificities of antibody molecules or T cells that
lymphocytes. At first, it was a mystery how it was pos-
for the millions of different types of antibodies and T
of Lymphocytes
Origin of the Many Clones
one or a few early lymphocytes of its specific type.
. That is, the lymphocytes in
forming one specificity of antibody or T cell are called
All the different lymphocytes that are capable of
around in this circuit for months or years.
into the lymph, sometimes circulating around and
its progeny are specific sensitized T cells that are
circulates throughout the body. If it is a T lymphocyte,
cytes. If it is a B lymphocyte, its progeny will eventu-
phocyte is activated by its antigen, it reproduces wildly,
which it can react can activate it. Once the specific lym-
specificity. And only the specific type of antigen with
antibody or one type of T cell with a single type of
lymphocytes is capable of forming only one type of
tissue, as explained earlier. Each of these preformed
antibodies or T cells have been stored in the lymph
formed B lymphocytes and preformed T lymphocytes
Lymphoid Tissue.
Millions of Specific Types of Lymphocytes Are Stored in the
following.
opment. The mechanism of this specificity is the
vated to form antibodies. The activated T cells and
cells, and certain of the B lymphocytes become acti-
lymphocytes become activated to form activated T
lymphocytes in the lymphoid tissue, certain of the T
When specific antigens come in contact with T and B
Lymphocyte Clones
Against Specific Antigens—Role of
T Lymphocytes and B-Lymphocyte
Blood Cells, Immunity, and Blood Clotting
442
Unit VI
Antibodies React Highly Specifically
antibodies in turn react highly specifically against the
particular types of antigens that initiated their devel-
Millions of different types of pre-
that are capable of forming highly specific types of
forming tremendous numbers of duplicate lympho-
ally secrete the specific type of antibody that then
released into the lymph and then carried to the blood
and circulated through all the tissue fluids and back
a clone of lymphocytes
each clone are alike and are derived originally from
Only several hundred to a few thousand genes code
sible for so few genes to code for the millions of dif-
when one considers that a single gene is usually nec-
essary for the formation of each different type of
cell is never present in the original stem cells from
these gene segments become mixed with one another
one can understand the millions of different cell gene
Mechanism for Activating a Clone
single type of antigen (or to several similar antigens
that have almost exactly the same stereochemical
surface of its cell membrane about 100,000 antibody
molecules that will react highly specifically with
attaches to the antibody in the cell membrane;
surface receptor proteins (or
are highly specific for one specified activating
antigen.
Role of Macrophages in the Activation Process.
Aside from
macrophages then pass these antigens by cell-to-cell
substance that promotes still further growth and
stance is called interleukin-1.
Most
helper cells
(collectively called lymphokines) that activate the
and B cells again after we have an opportunity
other biological properties of the antibody.
which the antibodies pass through membranes, and
, the ease with
the antibody to specific structures within the tissues,
diffusivity of the antibody in the tissues, adherence of
properties of the antibody, establishing such factors as
attaches specifically to a particular type of antigen. The
specificity of antibody, and it is this portion that
. The variable portion is different for each
; the remainder of each chain is called the
end of each light and heavy chain, called the
Figure 34–3 shows by the circled area a designated
such pairs in each immunoglobulin molecule.
pair, and there are always at least 2 and as many as 10
light chain at one of its ends, thus forming a heavy-light
immunoglobulins, each heavy chain is paralleled by a
high-molecular-weight immunoglobulins. Yet, in all
10 heavy and 10 light chains, which gives rise to
as shown in Figure 34–3. However, some of the
a combination of two light and two heavy chains,
. Most are
heavy polypeptide chains
constitute about 20 per cent of all the plasma proteins.
lar weights between 160,000 and 970,000. They usually
), and they have molecu-
The antibodies are gamma globulins called
Nature of the Antibodies
injections.
increased potency and duration of the secondary
many months rather than for only a few weeks. The
hours), is far more potent, and forms antibodies for
life. The secondary response, by contrast, begins
the primary response, its weak potency, and its short
antigen. Note the 1-week delay in the appearance of
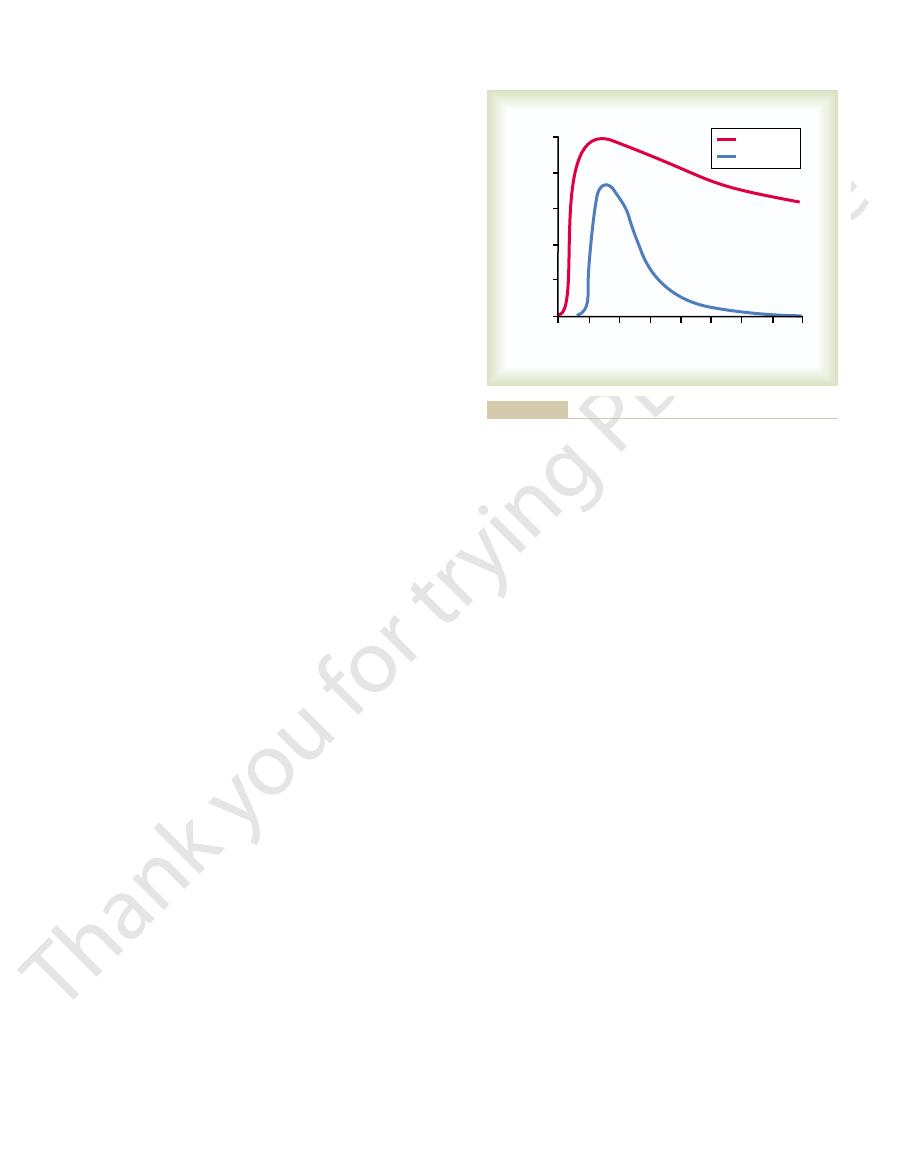
Figure 34–2 shows the differences between the
of the specific clone.
memory cells than there were original B lymphocytes
second time around, because there are many more
. Subsequent
lymphocytes are called
again by a new quantity of the same antigen. These
however, they remain dormant until activated once
populate all the lymphoid tissue; immunologically,
same clone. They also circulate throughout the body to
cytes are added to the original lymphocytes of the
becomes greatly enhanced, and the new B lympho-
to those of the original clone. In other words, the B-
form moderate numbers of new B lymphocytes similar
phocytes do not go on to form plasma cells but instead
Response and Secondary Response.
Formation of “Memory” Cells—Difference Between Primary
occur.
blood.This process continues for several days or weeks
second for each plasma cell. In turn, the antibodies are
cells for each original plasmablast. The mature plasma
sions, giving in 4 days a total population of about 500
proliferates. The plasmablasts then begin to divide at
. In the plasmablasts, the cytoplasm
, which are precursors
. Some of the lymphoblasts further dif-
Those B lymphocytes specific for the antigen imme-
more fully later.
extreme activation of the B lymphocytes, as we discuss
are formed. These helper cells also contribute to
T cells at the same time, and activated helper T cells
B lymphocytes. In addition, the antigen is presented to
phagocytize the antigen and then present it to adjacent
foreign antigen, macrophages in the lymphoid tissue
remain dormant in the lymphoid tissue. On entry of a
to a specific antigen, the clones of B lymphocytes
Immunity and the Antibodies
B-Lymphocyte System—Humoral
Specific Attributes of the
Resistance of the Body to Infection: II. Immunity and Allergy
Chapter 34
443
Formation of Antibodies by Plasma Cells.
Before exposure
diately enlarge and take on the appearance of
lymphoblasts
ferentiate to form plasmablasts
of plasma cells
expands and the rough endoplasmic reticulum vastly
a rate of about once every 10 hours for about nine divi-
cell then produces gamma globulin antibodies at an
extremely rapid rate—about 2000 molecules per
secreted into the lymph and carried to the circulating
until finally exhaustion and death of the plasma cells
A few of the lym-
phoblasts formed by activation of a clone of B lym-
cell population of the specifically activated clone
memory cells
exposure to the same antigen will cause a much more
rapid and much more potent antibody response this
primary response for forming antibodies that occurs on
first exposure to a specific antigen and the secondary
response that occurs after second exposure to the same
rapidly after exposure to the antigen (often within
response explain why immunization is usually accom-
plished by injecting antigen in multiple doses with
periods of several weeks or several months between
immuno-
globulins (abbreviated as Ig
All the immunoglobulins are composed of combi-
nations of light and
immunoglobulins have combinations of as many as
variable
portion
con-
stant portion
constant portion of the antibody determines other
attachment to the complement complex
0
2
4
8
6
Weeks
Concentration of antibody
0
64
32
16
8
128
Secondary
Primary
months later.
secondary
primary
Time course of the antibody response in the circulating blood to
Figure 34–2
a
injection of antigen and to a
injection several
normal person, and IgE, which constitutes only a small
importance: IgG, which is a bivalent antibody and con-
For the purpose of our present limited discussion,
five respective letters designate the respective classes.
. Ig stands for immunoglobulin, and the other
IgM, IgG, IgA, IgD,
antibodies, respectively named
There are five general classes of
sites.
chains, have as many as 10
. A small proportion of the antibodies, which
ment of antigens, making this type of antibody
Note, especially, in Figure 34–3 that there are two
law.
forces. It also obeys the thermodynamic mass action
bonding, (3) ionic attractions, and (4) van der Waals
together by (1) hydrophobic bonding, (2) hydrogen
antibody-antigen coupling is exceedingly strong, held
highly specific, there are so many bonding sites that the
the antibody and the antigen. When the antibody is
body, thus allowing rapid and tight bonding between
antigen fit as a mirror image with those of the anti-
contact with it, multiple prosthetic groups of the
antigen specificity, so that when an antigen comes in
tions of both the light and heavy chains. The amino
particular antigen; this is caused by its unique struc-
Blood Cells, Immunity, and Blood Clotting
444
Unit VI
Specificity of Antibodies.
Each antibody is specific for a
tural organization of amino acids in the variable por-
acid organization has a different steric shape for each
K
a
is called the affinity constant and is a measure of
how tightly the antibody binds with the antigen.
variable sites on the illustrated antibody for attach-
biva-
lent
consist of combinations of up to 10 light and 10 heavy
binding
Classes of Antibodies.
and IgE
two of these classes of antibodies are of particular
stitutes about 75 per cent of the antibodies of the
percentage of the antibodies but is especially involved
Concentration of bound antibody-antigen
K
Concentration of antibody
Concentration of antigen
a
=
¥
major role in protecting the body against the invader.
These direct actions of antibodies attacking the anti-
, in which some potent antibodies are
Lysis
, in which the antibodies cover the
, in which the molecular complex of
red cells, are bound together into a clump
with antigens on their surfaces, such as bacteria or
, in which multiple large particles
agent in one of several ways, as follows:
ing agents, the antibodies can inactivate the invading
objects). Because of the bivalent nature of the anti-
shows antibodies (designated by the red Y-shaped
Figure 34
destroying the invader.
against invading agents: (1) by direct attack on the
though there are not many IgM antibodies.
effective in protecting the body against invaders, even
primary response are of this type. These antibodies
in allergy. The IgM class is also interesting because
a large share of the antibodies formed during the
have 10 binding sites that make them exceedingly
Mechanisms of Action of Antibodies
Antibodies act mainly in two ways to protect the body
invader and (2) by activation of the “complement
system” that then has multiple means of its own for
Direct Action of Antibodies on Invading Agents.
–4
bars) reacting with antigens (designated by the shaded
bodies and the multiple antigen sites on most invad-
1. Agglutination
2. Precipitation
soluble antigen (such as tetanus toxin) and
antibody becomes so large that it is rendered
insoluble and precipitates
3. Neutralization
toxic sites of the antigenic agent
4.
occasionally capable of directly attacking
membranes of cellular agents and thereby cause
rupture of the agent
genic invaders often are not strong enough to play a
Most of the protection comes through the amplifying
effects of the complement system described next.
Antigen-binding sites
Antigen
Light
chain
Heavy
chain
Constant portion
Variable portion
S • S
S • S
S • S
S • S
The antigen binds at two different sites on the variable portions of
Structure of the typical IgG antibody, showing it to be composed
Figure 34–3
of two heavy polypeptide chains and two light polypeptide chains.
the chains.
Antigen
Antibodies
Figure 34–4
Binding of antigen molecules to one another by bivalent
antibodies.
immobilize the antigenic agent. The same factors
uid and plasma protein into the tissue, and other
ow, increased leakage of
uids. These substances in turn cause
heparin, and several other substances into the
basophils, causing them to release histamine,
C3a, C4a, and C5a activate mast cells and
Fragments
Activation of mast cells and basophils.
numbers of these phagocytes to migrate into the
neutrophils and macrophages, thus causing large
Fragment C5a initiates chemotaxis of
Chemotaxis.
The complement
Neutralization of viruses.
causing them to adhere to one another, thus
change the surfaces of the invading organisms,
The complement products also
organisms.
This has a direct effect of rupturing the cell
, which is a combination of multiple
Lysis.
. It often enhances the number
antibody complexes are attached. This process is
neutrophils and macrophages, causing these cells
strongly activates phagocytosis by both
products of the complement cascade, C3b,
Opsonization and phagocytosis.
toxin. Among the more important effects are the
gure, and several of these cause
occurs. Multiple end products are formed, as shown to
beginning, an extremely large
the later stages of the system, so that from a small
zyme C1 itself. The C1 enzymes that are formed then
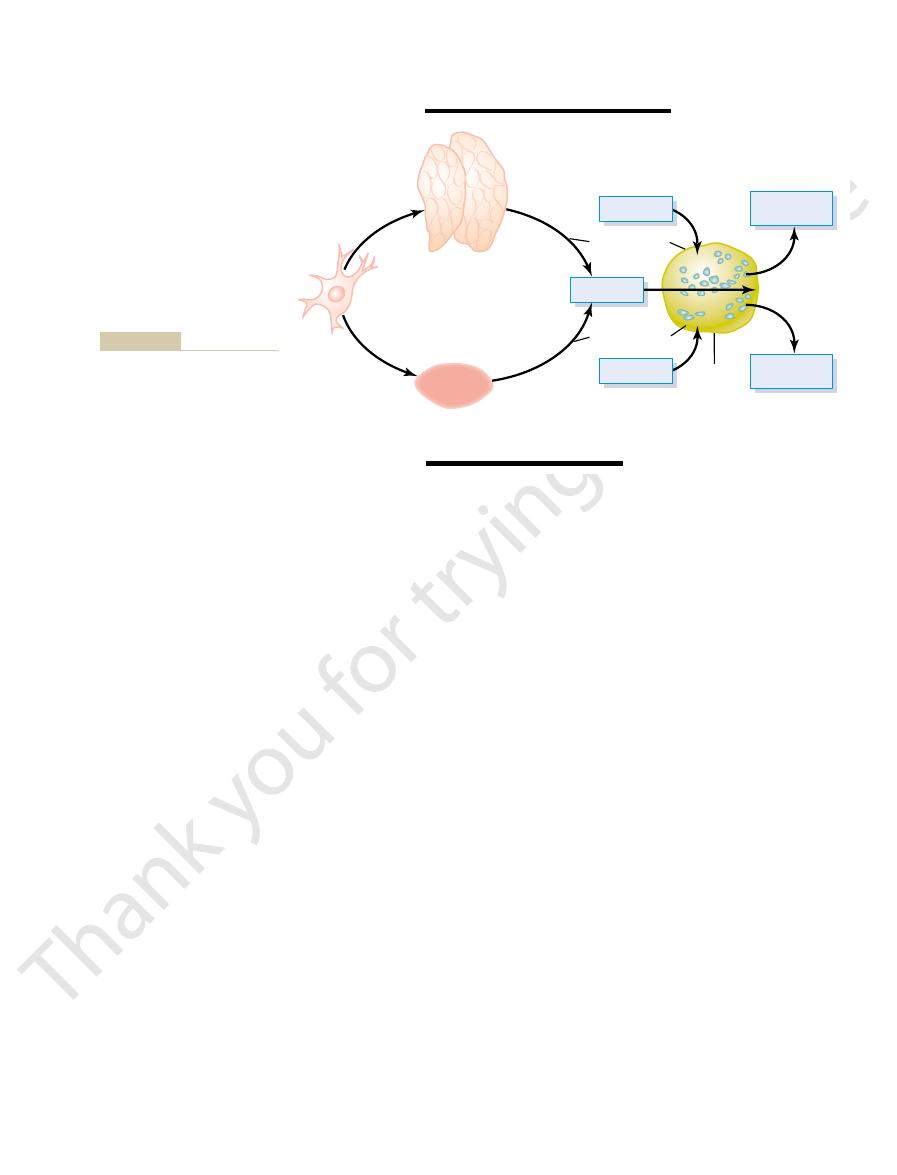
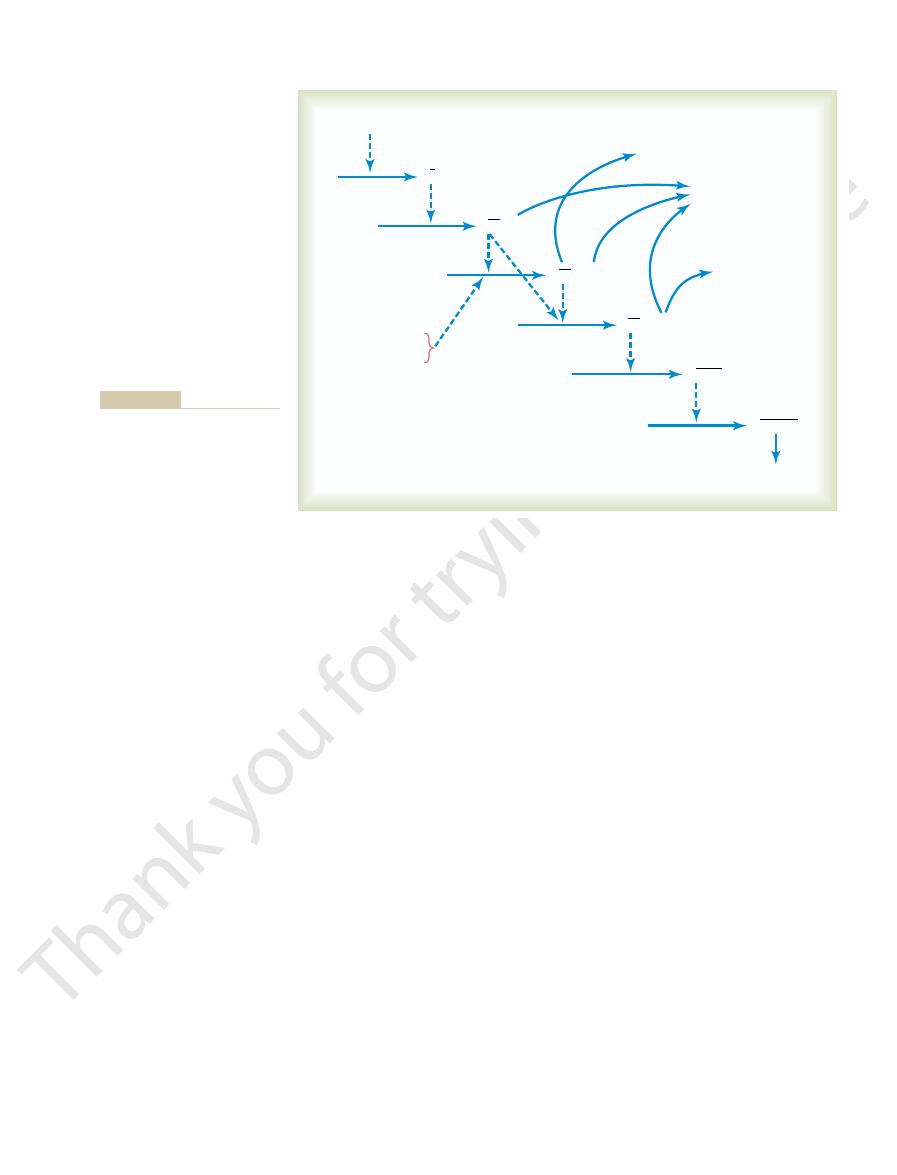
5, beginning with activation of the proen-
in Figure 34
of sequential reactions, shown
the C1 molecule of the complement system, setting
ered, or
binds with an antigen, a speci
antigen-antibody reaction. That is, when an antibody
The classic pathway is initiated by an
Classic Pathway.
classic pathway.
spaces. The enzyme precursors are normally inactive,
5. All these are present normally among
in Figure 34
proteins designated C1 through C9, B, and D, shown
precursors. The principal actors in this system are 11
system of about 20 proteins, many of which are enzyme
Resistance of the Body to Infection: II. Immunity and Allergy
Chapter 34
445
Complement System for Antibody Action
“Complement” is a collective term that describes a
–
the plasma proteins in the blood as well as among the
proteins that leak out of the capillaries into the tissue
but they can be activated mainly by the so-called
fic reactive site on the
“constant” portion of the antibody becomes uncov-
“activated,” and this in turn binds directly with
into motion a “cascade”
–
activate successively increasing quantities of enzymes in
“amplified” reaction
the right in the fi
important effects that help to prevent damage to the
body’s tissues caused by the invading organism or
following:
1.
One of the
to engulf the bacteria to which the antigen-
called opsonization
of bacteria that can be destroyed by many
hundredfold.
2.
One of the most important of all the
products of the complement cascade is the lytic
complex
complement factors and designated C5b6789.
membranes of bacteria or other invading
3. Agglutination.
promoting agglutination.
4.
enzymes and other complement products can
attack the structures of some viruses and thereby
render them nonvirulent.
5.
tissue area adjacent to the antigenic agent.
6.
local fl
increased local blood fl
fl
local tissue reactions that help inactivate or
play a major role in inflammation (which was
C6 + C7
C5b67
C4 + C2
C42 + C4a
Antigen–antibody complex
Micro-organism +
B and D
Opsonization of bacteria
Activate mast
cells and basophils
Chemotaxis of
white blood cells
C1
C3
C5
C1
C3b + C3a
C8 + C9
C5b + C5a
C5b6789
Lysis of cells
mentals of Clinical Immunology.
Alexander JW, Good RA: Funda-
of complement. (Modified from
Cascade of reactions during
Figure 34–5
activation of the classic pathway
Philadelphia: WB Saunders,
1977.)

T cells, usually constituting more than three quarters
The helper T cells are by far the most numerous of the
. The functions of each of these are distinct.
, and (3)
cytotoxic T cells
, (2)
helper T cells
ed into three major groups: (1)
cells. They are classi
It has become clear that there are multiple types of T
Several Types of T Cells and Their
There are as many as 100,000 receptor sites on a single
bound to the cell membrane of the T lymphocyte.
of the humoral antibody, but its stem section is
protein antibodies. These receptor molecules are com-
on the surfaces of T
The antigens on the surface of antigen-presenting
helper T cells are discussed later.
c functions of cytotoxic and
. The speci
, which present antigens
, and (2)
cytotoxic T
, which present antigens to
surface. There are two types of MHC proteins: (1)
. The MHC proteins bind peptide fragments
The MHC proteins are encoded by a large group of
is critical in permitting the T cells to bind
to present antigens to T cells. Interaction of
throughout the body, and their only known function is
potent of the antigen-presenting cells, are located
. The dendritic cells, the most
, and
6). The three major types of
tissues (Figure 34
T lymphocytes respond to antigens only when they are
Although B lymphocytes recognize intact antigens,
ally helping to eliminate invading pathogens.
begin the process, and T cells play a major role in actu-
responses usually require assistance from T cells to
fending against infection. In fact, acquired immune
c, like the antibody responses of B cells,
T-cell responses are extremely
tors on the T Lymphocytes.
rst exposure.
in the body, release of activated T cells occurs far more
out the lymphoid tissue of the entire body. Therefore,
clone; in fact, these memory cells even spread through-
become additional T lymphocytes of that speci
lymphocytes are preserved in the lymphoid tissue to
activated by an antigen, many of the newly formed
body system. That is, when a clone of T lymphocytes is
T-lymphocyte memory cells
Also,
body, sometimes lasting for months or even years.
again, and circulating again and again throughout the
the tissue spaces, back into the lymph and blood once
out the body, passing through the capillary walls into
are formed and released into the lymph. These then
instead of releasing antibodies, whole activated T cells
activated B cells. The principal difference is that
ing T cells in ways that parallel antibody release by
release large numbers of activated, speci
c lymphocyte clone proliferate and
cytes of a speci
as presented by adjacent macrophages, the T lympho-
tion of Memory Cells.
Release of Activated T Cells from Lymphoid Tissue and Forma-
T Cells and Cell-Mediated Immunity
T-Lymphocyte System
Special Attributes of the
organism through the tissues.
uid proteins to coagulate in the tissue spaces,
proteins to be increased, and (3) the interstitial
increase still further, (2) the capillary leakage of
ammation. These products
basophils, several other complement products
Inflammatory effects.
discuss later.
discussed in Chapter 33) and in allergy, as we
Blood Cells, Immunity, and Blood Clotting
446
Unit VI
7.
In addition to inflammatory
effects caused by activation of the mast cells and
contribute to local infl
cause (1) the already increased blood flow to
fl
thus preventing movement of the invading
–Activated
On exposure to the proper antigen,
fi
fically react-
pass into the circulation and are distributed through-
are formed in the
same way that B memory cells are formed in the anti-
fic
on subsequent exposure to the same antigen anywhere
rapidly and much more powerfully than had occurred
during fi
Antigen-Presenting Cells, MHC Proteins, and Antigen Recep-
antigen specifi
and are at least as important as antibodies in de-
bound to specific molecules called MHC proteins on
the surface of antigen-presenting cells in the lymphoid
–
antigen-presenting cells are macrophages, B lympho-
cytes
dendritic cells
cell adhe-
sion proteins
to antigen-presenting cells long enough to become
activated.
genes called the major histocompatibility complex
(MHC)
of antigen proteins that are degraded inside antigen-
presenting cells and then transport them to the cell
MHC I proteins
cells
MHC II proteins
to T helper cells
fi
cells bind with receptor molecules
cells in the same way that they bind with plasma
posed of a variable unit similar to the variable portion
firmly
T cell.
Different Functions
fi
suppressor
T cells
Helper T Cells—Their Role in Overall
Regulation of Immunity
Cell-cell
adhesion
proteins
T-cell receptor
Foreign protein
MHC protein
T cell
Antigen-
presenting
cell
to bind to the antigen-presenting cell long enough to become
(MHC) protein. Cell-to-cell adhesion proteins enable the T cell
antigen-presenting cell by a major histocompatibility complex
antigen (foreign protein) that is transported to the surface of the
Activation of T cells requires interaction of T-cell receptors with an
Figure 34–6
activated.
punched holes and delivered cytotoxic substances and
Especially important, these cytotoxic killer cells can
swollen, and it usually dissolves shortly thereafter.
Almost immediately, the attacked cell becomes greatly
cytotoxic substances directly into the attacked cell.
tial space. In addition, the cytotoxic T cell releases
Then
, that literally punch
, called
After binding, the cytotoxic T cell secretes
the attacked cell in the manner shown in Figure 34
c antigen. Then, they kill
surfaces of the cytotoxic cells cause them to bind
. The receptor proteins on the
s own cells. For this reason, these
capable of killing micro-organisms and, at times, even
The cytotoxic T cell is a direct-attack cell that is
This acts as an ampli
stimulating activation of the helper T cells themselves.
leukin-2, have a direct positive feedback effect in
Some of the lymphokines, especially inter-
bacteria or other tissue-destroying agents.
cient phagocytosis, allowing them
macrophages. Second, they activate the macrophages
tissue area, thus causing great accumulation of
phokines also affect the macrophages. First, they slow
The lym-
Activation of the Macrophage System.
B-cell growth factors
response, but especially interleukins 4, 5, and 6. In fact,
of the helper T cells.
mation of plasma cells, and secretion of antibodies are
of antigen to cause B-cell growth, proliferation, for-
The direct actions
Form Plasma Cells and Antibodies.
Stimulation of B-Cell Growth and Differentiation to
potent effects.
In addition, several of the other lymphokines have less
proliferation of both cytotoxic and suppressor T cells.
antigens. The lymphokine
suppressor T cells are activated only slightly by most
T cells, the clones for producing cytotoxic T cells and
Stimulation of Growth and Proliferation of Cytotoxic T
functions are the following.
lethal effects of AIDS. Some of the speci
totally unprotected against infectious disease, there-
, which leaves the body almost
lyzed. In fact, it is the helper T cells that are inactivated
absence of the lymphokines from the helper T cells,
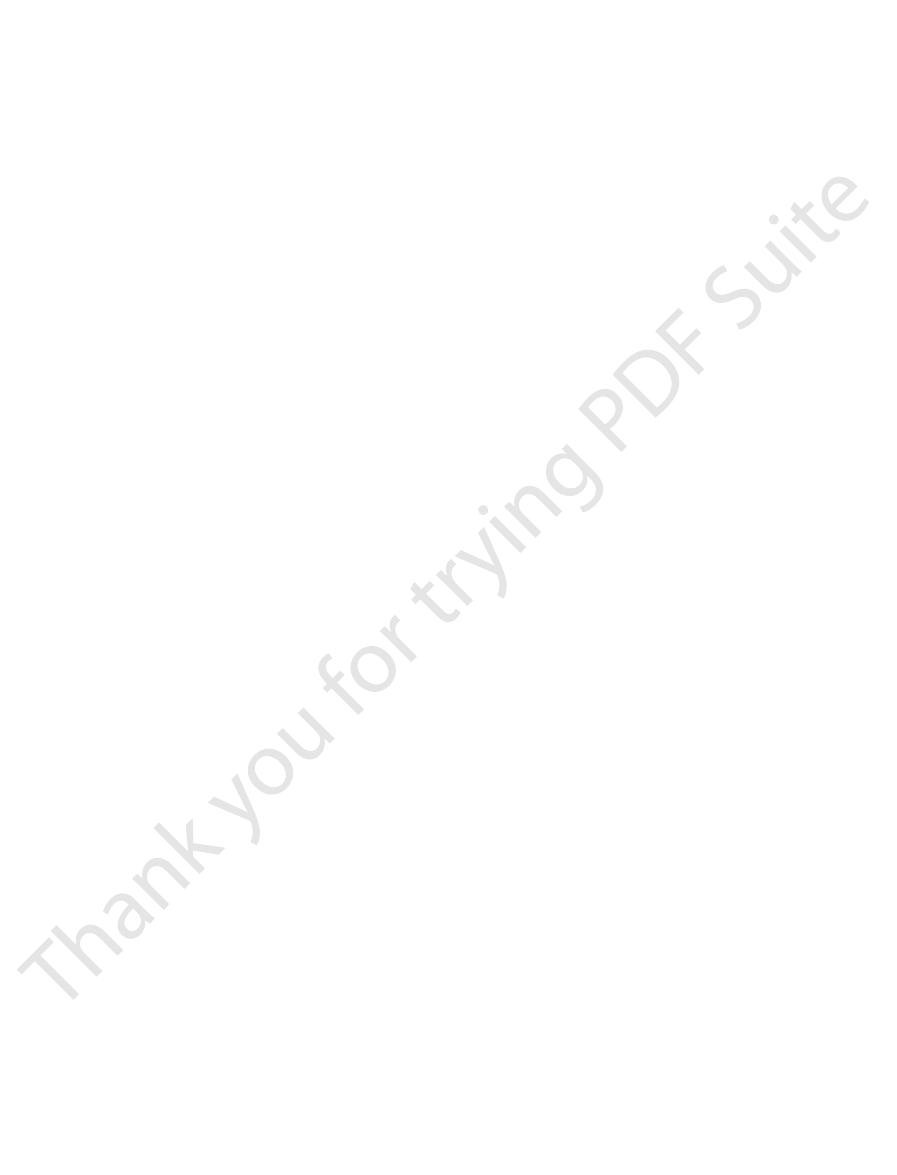
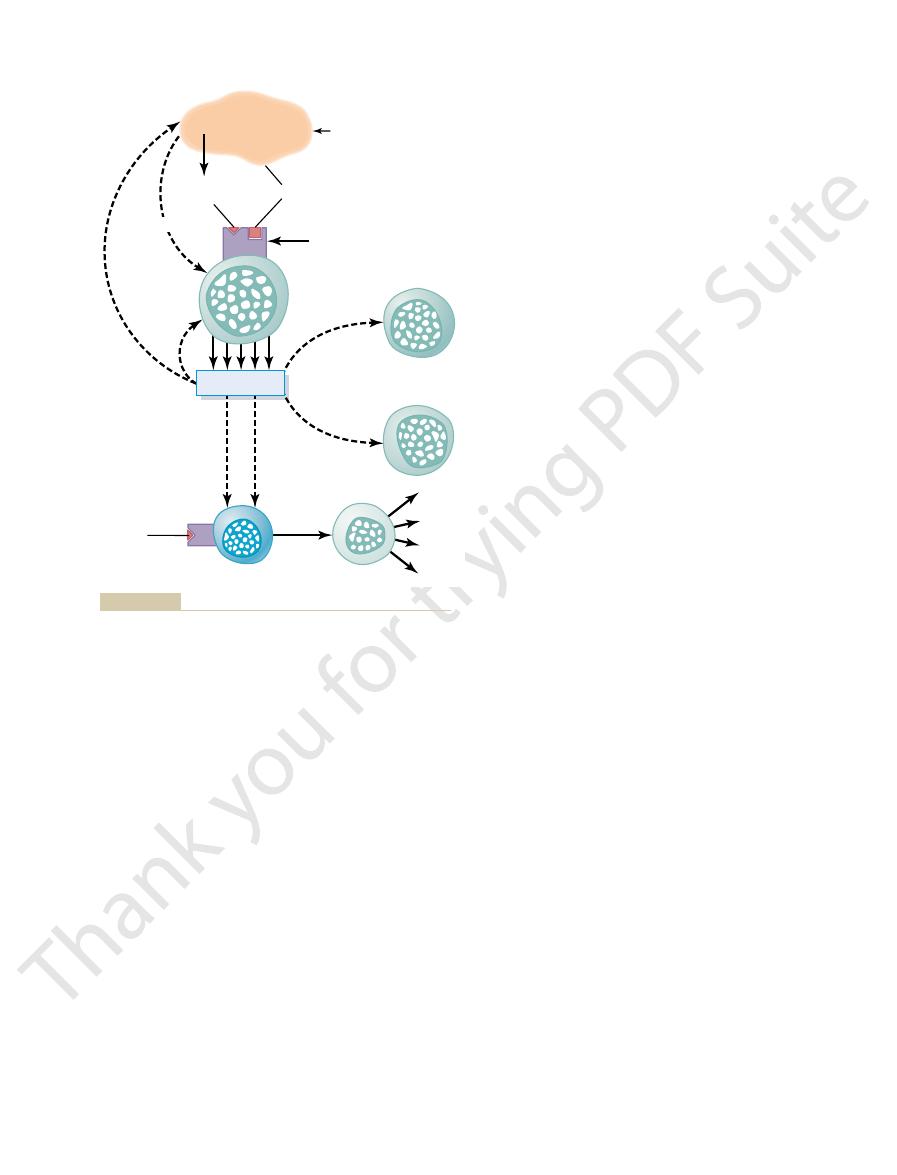
Specific Regulatory Functions of the Lymphokines.
Granulocyte-monocyte colony-stimulating factor
helper T cells are the following:
immune system as well as on bone marrow cells.
lymphokines,
ators, called
7. They do this by forming a series of protein medi-
of virtually all immune functions, as shown in Figure
many ways. In fact, they serve as the major regulator
functions of the immune system, and they do so in
of all of them. As their name implies, they
Resistance of the Body to Infection: II. Immunity and Allergy
Chapter 34
447
help in the
34–
that act on other cells of the
Among the important lymphokines secreted by the
Interleukin-2
Interleukin-3
Interleukin-4
Interleukin-5
Interleukin-6
Interferon-
g
In the
the remainder of the immune system is almost para-
or destroyed by the acquired immunodeficiency syn-
drome (AIDS) virus
fore leading to the now well-known debilitating and
fic regulatory
Cells and Suppressor T Cells.
In the absence of helper
interleukin-2 has an espe-
cially strong stimulatory effect in causing growth and
also slight without the “help”
Almost all the interleukins participate in the B-cell
these three interleukins have such potent effects on
the B cells that they have been called B-cell stimulat-
ing factors or
.
or stop the migration of the macrophages after they
have been chemotactically attracted into the inflamed
to cause far more effi
to attack and destroy increasing numbers of invading
Feedback Stimulatory Effect on the Helper Cells Them-
selves.
fier by further enhancing the
helper cell response as well as the entire immune
response to an invading antigen.
Cytotoxic T Cells
some of the body’
cells are called killer cells
tightly to those organisms or cells that contain the
appropriate binding-specifi
–8.
hole-
forming proteins
perforins
round holes in the membrane of the attacked cell.
fluid flows rapidly into the cell from the intersti-
pull away from the victim cells after they have
Preprocessor
areas
Lymphokines!!
Antigen
Antigen
Processed
antigen
MHC
B cell
Suppressor
T cells
Plasma
cells
Cytotoxic
T cells
Helper
T cells
Antigen-specific receptor
Differentiation
Proliferation
IgM
IgG
IgA
IgE
Preprocessor
areas
Interleukin-1
Regulation of the immune system, emphasizing a pivotal role of
Figure 34–7
the helper T cells. MHC, major histocompatibility complex.
immunization is used to protect against typhoid fever,
still have some of their chemical antigens. This type of
c diseases. A
Immunization by Injection of Antigens
same time, a disease that causes extensive damage and
, in which the person becomes
the neuromuscular junction, causing paralysis; and (4)
, in which immunity
glomeruli; (3)
, in which the person becomes
s own self-antigens; (2) one type of
heart, especially the heart valves, after exposure to a
, in which the body
antibodies.
immunity in the form of either activated T cells or
s own tissues, which releases
older a person becomes. It usually occurs after destruc-
of their own tissues. This occurs to a greater extent the
Failure of the Tolerance Mechanism Causes Autoimmune Dis-
antigens.
of those clones of lymphocytes that are speci
phocytes in the thymus and bone marrow, all or most
the total body lymphoid tissue.
proliferate considerably, and then combine with the
exposed to a strong antigen, become lymphoblastic,
c immature lymphocytes in the thymus, when
the injected antigen. Experiments have shown that
lymphocytes in the lymphoid tissue that are speci
fetus while the lymphocytes are being preprocessed in
and of B lymphocytes in the bone marrow. The reason
during preprocessing of T lymphocytes in the thymus
Most Tolerance Results from Clone Selection During Prepro-
activated T cells against his or her own antigens.
as being distinctive from bacteria or viruses, and the
s own body. The immune mech-
tissues, the process of acquired immunity would
s Own Tissues
System to One
Tolerance of the Acquired Immunity
, as we discuss in the
tissues, called
. It is probable that the suppressor T-cell
ulatory T cells
ed, along with the helper T cells, as
s own tissues. For this reason, the suppressor
purpose of preventing the cytotoxic cells from causing
the functions of both cytotoxic and helper T cells. It is
about the others, but they are capable of suppressing
Much less is known about the suppressor T cells than
Suppressor T Cells
s own body.
transplant cells, or other types of cells that are foreign
an important role in destroying cancer cells, heart
to the viral antigenicity. The cytotoxic cells also play
branes of the tissue cells and attract T cells in response
Some of the cytotoxic T cells are especially lethal to
cells persist for months in the tissues.
then move on to kill more cells. Indeed, some of these
Blood Cells, Immunity, and Blood Clotting
448
Unit VI
tissue cells that have been invaded by viruses because
many virus particles become entrapped in the mem-
to the person’
believed that these suppressor functions serve the
excessive immune reactions that might be damaging to
the body’
cells are classifi
reg-
system plays an important role in limiting the ability
of the immune system to attack a person’s own body
immune tolerance
next section.
’
—Role
of Preprocessing in the Thymus and
Bone Marrow
If a person should become immune to his or her own
destroy the individual’
anism normally “recognizes” a person’s own tissues
person’s immunity system forms few antibodies or
cessing.
It is believed that most tolerance develops
for this belief is that injecting a strong antigen into a
these two areas prevents development of clones of
fic for
specifi
stimulating antigen—an effect that is believed to cause
the cells themselves to be destroyed by the thymic
epithelial cells before they can migrate to and colonize
It is believed that during the preprocessing of lym-
fic to
damage the body’s own tissues are self-destroyed
because of their continual exposure to the body’s
eases.
Sometimes people lose their immune tolerance
tion of some of the body’
considerable quantities of “self-antigens” that cir-
culate in the body and presumably cause acquired
Several specific diseases that result from autoim-
munity include (1) rheumatic fever
becomes immunized against tissues in the joints and
specific type of streptococcal toxin that has an epitope
in its molecular structure similar to the structure of
some of the body’
glomerulonephritis
immunized against the basement membranes of
myasthenia gravis
develops against the acetylcholine receptor proteins of
lupus erythematosus
immunized against many different body tissues at the
often rapid death.
Immunization has been used for many years to
produce acquired immunity against specifi
person can be immunized by injecting dead organisms
that are no longer capable of causing disease but that
Cytotoxic
and
digestive
enzymes
Cytotoxic
T cells
(killer cells)
Antigen
receptors
Antigen
Attacked
cell
Specific
binding
Direct destruction of an invading cell by sensitized lymphocytes
Figure 34–8
(cytotoxic T cells).
directly into the circulation, the allergen can react with
When a speci
reactions caused in this manner are the following.
reaction occurs. Among the different types of allergic
several different tissue responses can occur, depend-
contraction of local smooth muscle cells. Therefore,
uid into the tissues; and
trophils to the reactive site; increased permeability of
local blood vessels; attraction of eosinophils and neu-
These substances cause such effects as dilation of the
, and
neutrophil chemo-
eosinophil chemotactic substance
slow-reacting substance of anaphy-
agents immediately or shortly thereafter, including
mast cells and basophils rupture; others release special
contort the cell membrane. At any rate, many of the
brane of the mast cell or basophil, perhaps resulting
basophil, this causes immediate change in the mem-
antibodies. Then, when an antigen (an allergen) that
and basophils. Indeed, a single mast cell or basophil
occurs.
reaction lakes place, and a subsequent allergic reaction
reagin antibody) enters the body, an allergen-reagin
ned as an antigen
bodies. When an
in the blood. These anti-
allergic tendency is genetically passed from parent to
by a nonordinary response of the immune system. The
tendency. Their aller-
Who Has Excess IgE Antibodies
Person,
attacks in the case of some airborne antigens.
is present, such as in the skin in the case of poison ivy,
can be serious tissue damage. The damage normally
their subsequent effects, one can well understand that
stances from the activated T cells as well as extensive
type of immune reaction. Remembering that this type
at the same time, these T cells elicit a cell-mediated
into the skin to respond to the poison ivy toxin. And,
ivy toxin, within a day or so, the activated T cells
T cells. Then, after subsequent exposure to the poison
cause the formation of activated helper and cytotoxic
to the tissues. However, on repeated exposure, it does
and not by antibodies. In the case of poison ivy, the
Delayed-reaction allergy is caused by activated T cells
Allergy Caused by Activated T Cells:
c allergic tendency.
several types of allergy and other hypersensitivities,
. There are
the development, under some conditions, of
immunity.
lymphocytes to confer immunity is called
from an animal. Such transfusion of antibodies or T
against the invading disease. Activated T cells last for
3 weeks, and during that time, the person is protected
infusing antibodies, activated T cells, or both obtained
person without injecting any antigen. This is done by
However, temporary immunity can be achieved in a
body develops either antibodies or activated T cells in
. That is, the person
Thus far, all the acquired immunity we have discussed
fever, measles, smallpox, and many other viral diseases.
dure is used to protect against poliomyelitis, yellow
c antigens required for immunization. This proce-
That is, these organisms either have been grown
nally, a person can be immunized by being
other similar toxic diseases.
used in immunizing against tetanus, botulism, and
causing immunity are still intact. This procedure is
bacterial diseases.
whooping cough, diphtheria, and many other types of
Resistance of the Body to Infection: II. Immunity and Allergy
Chapter 34
449
Immunity can be achieved against toxins that have
been treated with chemicals so that their toxic nature
has been destroyed even though their antigens for
And, fi
infected with live organisms that have been “attenu-
ated.”
in special culture media or have been passed through
a series of animals until they have mutated enough
that they will not cause disease but do still carry spe-
cifi
Passive Immunity
has been active immunity
’s own
response to invasion of the body by a foreign antigen.
from the blood of someone else or from some other
animal that has been actively immunized against the
antigen.
Antibodies last in the body of the recipient for 2 to
a few weeks if transfused from another person but
only for a few hours to a few days if transfused
passive
ALLERGY AND
HYPERSENSITIVITY
An important undesirable side effect of immunity is
allergy or
other types of immune hypersensitivity
some of which occur only in people who have a spe-
cifi
Delayed-Reaction Allergy
toxin of poison ivy in itself does not cause much harm
diffuse from the circulating blood in large numbers
of immunity can cause release of many toxic sub-
invasion of the tissues by macrophages along with
the eventual result of some delayed-reaction allergies
occurs in the tissue area where the instigating antigen
or in the lungs to cause lung edema or asthmatic
Allergies in the “Allergic”
Some people have an “allergic”
gies are called atopic allergies because they are caused
child and is characterized by the presence of large
quantities of IgE antibodies
bodies are called reagins or sensitizing antibodies to
distinguish them from the more common IgG anti-
allergen (defi
that reacts specifically with a specific type of IgE
A special characteristic of the IgE antibodies (the
reagins) is a strong propensity to attach to mast cells
can bind as many as half a million molecules of IgE
has multiple binding sites binds with several IgE anti-
bodies that are already attached to a mast cell or
from a physical effect of the antibody molecules to
his-
tamine, protease,
laxis (which is a mixture of toxic leukotrienes),
,
tactic substance, heparin
platelet activating factors.
the capillaries with loss of fl
ing on the type of tissue in which the allergen-reagin
Anaphylaxis.
fic allergen is injected
basophils of the blood and mast cells in the tissues
4:190, 2004.
witness of the past, actors of the future. Nat Rev Immunol
Vivier E, Anfossi N: Inhibitory NK-cell receptors on T cells:
roimmunol 146:1, 2004.
ammatory diseases and the effect of acute stress. J Neu-
Theoharides TC, Cochrane DE: Critical role of mast cells in
a few bugs in the system. J Membr Biol 193:137, 2003.
Scott CC, Botelho RJ, Grinstein S: Phagosome maturation:
lymphopoiesis in the thymus. Nat Rev Immunol 3:859,
Petrie HT: Cell migration and the control of post-natal T-cell
4:123, 2004 .
tant facets of T-cell repertoire diversity. Nat Rev Immunol
Nikolich-Zugich J, Slifka MK, Messaoudi I: The many impor-
113(4 Suppl):1107, 2004.
McGeady SJ: Immunocompetence and allergy. Pediatrics
Allergy Clin Immunol 112(4 Suppl):S53, 2003.
ammation. J
MacGlashan D Jr: Histamine: a mediator of in
development and function. Nat Immunol 5:133, 2004.
Linton PJ, Dorshkind K: Age-related changes in lymphocyte
Nat Rev Immunol 4:371, 2004.
La Cava A, Matarese G: The weight of leptin in immunity.
4:211, 2004.
mechanisms and clinical consequences. Nat Rev Immunol
Kupper TS, Fuhlbrigge RC: Immune surveillance in the skin:
Nat Rev Immunol 4:387, 2004.
comitant regulation of T-cell activation and homeostasis.
Grossman Z, Min B, Meier-Schellersheim M, Paul WE: Con-
J Leukoc Biol 75:579, 2004.
the microenvironment that directs the immune response.
Frossi B, De Carli M, Pucillo C: The mast cell: an antenna of
cell immunotherapy: mapping the way. Nat Med 10:475,
Figdor CG, de Vries IJ, Lesterhuis WJ, Melief CJ: Dendritic
syndromes. N Engl J Med. 350:2068, 2004.
Eisenbarth GS, Gottlieb PA: Autoimmune polyendocrine
of enteroinvasive pathogens. Science 304:242, 2004.
Cossart P, Sansonetti PJ: Bacterial invasion: the paradigms
ciencies. Am Fam Physician 68:2001, 2003.
Cooper MA, Pommering TL, Koranyi K: Primary immuno-
Rev Immunol 4:290, 2004.
memory T cells join forces at the mucosal front line. Nat
Cheroutre H, Madakamutil L: Acquired and natural
the Cell. New York: Garland Science, 2002.
Alberts B, Johnson A, Lewis J, et al: Molecular Biology of
Immunol 4:223, 2004.
Albert ML: Death-defying immunity: do apoptotic cells
Pediatr 144(4):421, 2004.
tors: clinical implications of basic science research. J
Abreu MT, Arditi M: Innate immunity and toll-like recep-
removed. Administration of antihistaminics has less
sequently, the person has dif
causes spasm of the bronchiolar smooth muscle. Con-
, which
slow-reacting substance of anaphylaxis
occurs in the bronchioles of the lungs. Here, an impor-
person. In such a person, the allergen-reagin reaction
eliciting the typical sneezing syndrome.
reagin reaction can still cause irritation of the nose,
swelling reaction. But other products of the allergen-
again, use of antihistamine drugs can prevent this
nasal linings become swollen and secretory. Here
into associated deeper tissues of the nose; and the
increased capillary permeability. Both these effects
occurs in the nose.
In hay fever, the allergen-reagin reaction
Hay Fever.
the hives.
hives.
skin within another few minutes. The swellings are
reactions.
ing an asthma-like attack, sometimes causing death by
spasm of the smooth muscle of the bronchioles, elicit-
. These leukotrienes can cause
slow-reacting
epinephrine to oppose the effects of the histamine.
loss of plasma from the circulation. An occasional
anaphylaxis. Histamine
system and closely associated tissues. This is called
by attachment of IgE reagins. Therefore, a widespread
Blood Cells, Immunity, and Blood Clotting
450
Unit VI
located immediately outside the small blood vessels
if the basophils and mast cells have been sensitized
allergic reaction occurs throughout the vascular
is released into the circulation
and causes body-wide vasodilation as well as increased
permeability of the capillaries with resultant marked
person who experiences this reaction dies of circula-
tory shock within a few minutes unless treated with
Also released from the activated basophils and mast
cells is a mixture of leukotrienes called
substance of anaphylaxis
suffocation.
Urticaria.
Urticaria results from antigen entering spe-
cific skin areas and causing localized anaphylactoid
Histamine released locally causes (1) vasodi-
lation that induces an immediate red flare and (2)
increased local permeability of the capillaries that
leads to local circumscribed areas of swelling of the
commonly called
Administration of antihista-
mine drugs to a person before exposure will prevent
Histamine released in response to
the reaction causes local intranasal vascular dilation,
with resultant increased capillary pressure as well as
cause rapid fluid leakage into the nasal cavities and
Asthma.
Asthma often occurs in the “allergic” type of
tant product released from the mast cells is believed
to be the
ficulty breathing until the
reactive products of the allergic reaction have been
effect on the course of asthma because histamine does
not appear to be the major factor eliciting the asth-
matic reaction.
References
influence antigen processing and presentation? Nat Rev
defi
2004.
fl
2003.
infl
