three types but only one type on each of the two chromosomes: type O, type A,
chromosomes, determine the O-A-B blood type. These genes can be any one of
Two genes, one on each of two paired
. When both A and B agglutinogens are present, the blood is
. When only type B agglutinogen is present, the blood
present, the blood is
. When only type A agglutinogen is
tinogen is present, the blood is
the two agglutinogens, the A and B agglutinogens. When neither A nor B agglu-
blood types, as shown in Table 35–1, depending on the presence or absence of
In transfusing blood from one person to another, the
Major O-A-B Blood Types.
may have both simultaneously.
ited, people may have neither of them on their cells, they may have one, or they
blood transfusion reactions. Because of the way these agglutinogens are inher-
in a large proportion of human beings. It is these antigens (also called
Two antigens—type A and type B—occur on the surfaces of the red blood cells
A and B Antigens—Agglutinogens
O-A-B Blood Types
cause blood transfusion reactions. They are the
Two particular types of antigens are much more likely than the others to
parentage.
faces of the cell membranes. Most of the antigens are weak and therefore are
antibody reactions, have been found in human blood cells, especially on the sur-
and hundreds of other rare antigens, each of which can at times cause antigen-
tions are taken, one can determine ahead of time whether the antibodies
gens on the surfaces of the red cells of another blood type. If proper precau-
properties, so that antibodies in the plasma of one blood will react with anti-
tions that frequently led to death. Soon it was dis-
often occurred, resulting in typical transfusion reac-
another were first attempted, immediate or delayed
When blood transfusions from one person to
and Organ Transplantation
Blood Types; Transfusion; Tissue
C
H
A
P
T
E
R
3
5
451
Antigenicity Causes Immune
Reactions of Blood
agglutination and hemolysis of the red blood cells
covered that the bloods of different people have different antigenic and immune
and antigens present in the donor and recipient bloods will cause a transfusion
reaction.
Multiplicity of Antigens in the Blood Cells.
At least 30 commonly occurring antigens
of importance principally for studying the inheritance of genes to establish
O-A-B system of antigens and
the Rh system.
agglu-
tinogens because they often cause blood cell agglutination) that cause most
bloods of donors and recipients are normally classified into four major O-A-B
type O
type A
is type B
type AB.
Genetic Determination of the Agglutinogens.
contain A or B agglutinogens, respectively, the red
When bloods are mismatched so that anti-A or anti-B
Agglutination Process In Transfusion
few, if any, agglutinins, showing that agglutinin forma-
of anti-A agglutinins than ever. Also, the neonate has
For instance, infusion of group A antigen into a
anti-B agglutinins.
food, in bacteria, and in other ways, and these sub-
amounts of type A and B antigens enter the body in
red blood cells? The answer to this is that small
molecules.
gens. Most of them are IgM and IgG immunoglobulin
gamma globulins, as are almost all antibodies, and they
The agglutinins are
remaining years of life.
of age, and this gradually declines throughout the
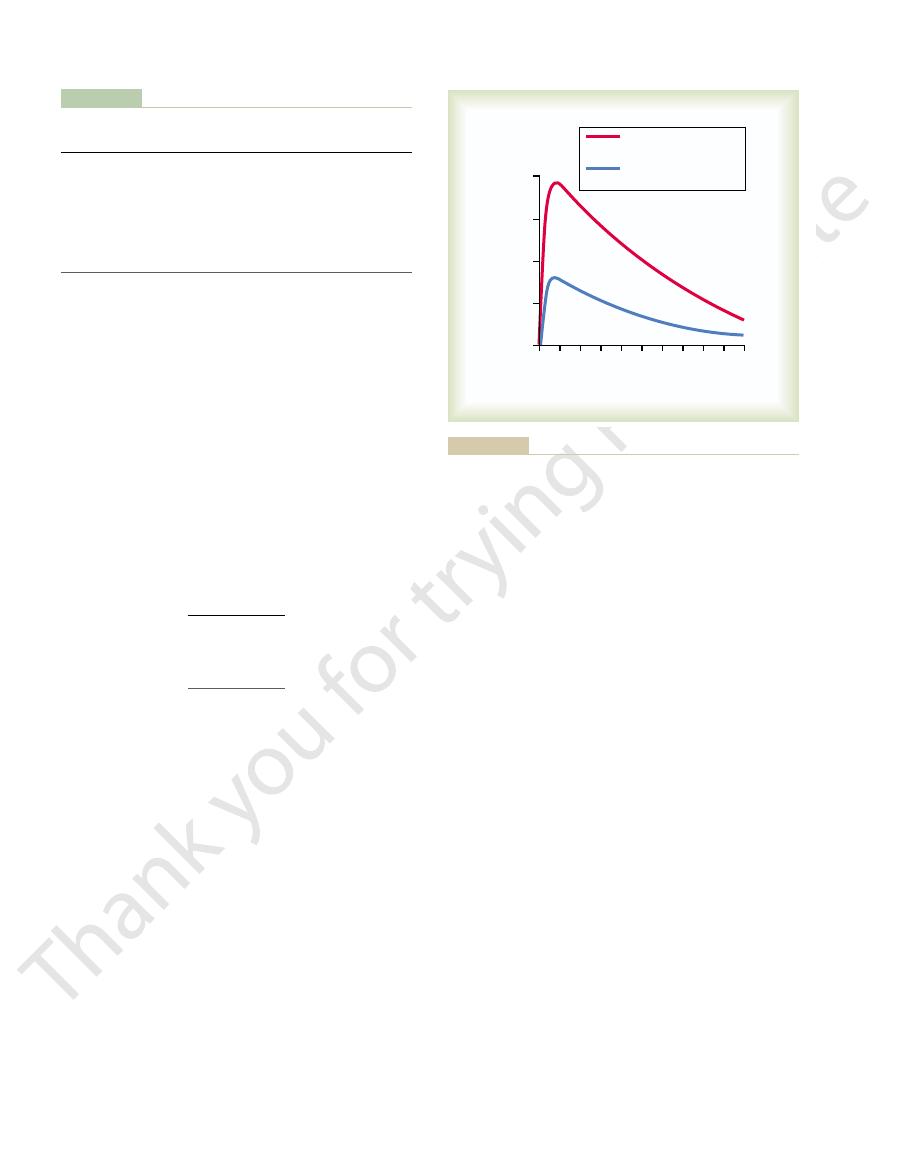
of the anti-A and anti-B agglutinins at different ages.
not in the cells. Figure 35–1 shows the changing titers
when type A agglutinogens are not present in the cells,
The prevalence of the different blood types among one
Relative Frequencies of the Different Blood Types.
type B blood, and genotype AB gives type AB blood.
fore has blood type A. Genotypes OB and BB give
OA or AA produces type A agglutinogens and there-
therefore the blood type is O. A person with genotype
with genotype OO produces no agglutinogens, and
One can also observe from Table 35–1 that a person
and each person is one of the six genotypes.
genotypes,
Table 35–1, are OO, OA, OB, AA, BB, and AB. These
The six possible combinations of genes, as shown in
cells.
O agglutinogen on the cells. Conversely, the type A
almost functionless, so that it causes no significant type
or type B. The type O gene is either functionless or
Blood Cells, Immunity, and Blood Clotting
452
Unit VI
and type B genes do cause strong agglutinogens on the
combinations of genes are known as the
group of persons studied was approximately:
and anti-B agglutinins when type B agglutinogens are
A maximum titer is usually reached at 8 to 10 years
Origin of Agglutinins in the Plasma.
are produced by the same bone marrow and lymph
gland cells that produce antibodies to any other anti-
But why are these agglutinins produced in people
who do not have the respective agglutinogens in their
stances initiate the development of the anti-A and
recipient having a non-A blood type causes a typical
immune response with formation of greater quantities
tion occurs almost entirely after birth.
Reactions
plasma agglutinins are mixed with red blood cells that
Blood Types with Their Genotypes and Their Constituent
Table 35–1
OB or BB
B
B
Anti-A
OA or AA
A
A
Anti-B
OO
O
—
Anti-A and
Genotypes
Blood Types
Agglutinogens
Agglutinins
Agglutinogens and Agglutinins
Anti-B
AB
AB
A and B
—
0 10 20 30 40 50 60 70 80 90 100
0
100
200
300
400
Average titer of agglutinins
Age of person (years)
Anti-A agglutinins in
groups B and O blood
Anti-B agglutinins in
groups A and O blood
people with different blood types.
Average titers of anti-A and anti-B agglutinins in the plasmas of
Figure 35–1
B
9%
A
41%
O
47%
almost zero. Two to 8 months after birth, an infant
birth, the quantity of agglutinins in the plasma is
Titer of the Agglutinins at Different Ages.
agglutinins.
contains both A and B agglutinogens but no
gens and anti-A agglutinins. Finally, type AB blood
A blood contains type A agglutinogens and
type O blood, although containing no agglutinogens,
Thus, referring once again to Table 35–1, note that
in the red blood cells, antibodies
develop in the plasma. Also, when type B agglutino-
red blood cells, antibodies known as
in a person’s
When type A agglutinogen
A genes occur frequently, whereas the B gene is
AB
3%
It is obvious from these percentages that the O and
infrequent.
Agglutinins
is not present
anti-A agglutinins
gen is not present
known as anti-B agglutinins develop in the plasma.
does contain both anti-A and anti-B agglutinins; type
anti-B
agglutinins; type B blood contains type B agglutino-
Immediately after
begins to produce agglutinins—anti-A agglutinins

“sensitized” to Rh factor.
in others. With multiple exposures to the Rh factor,
tinins about 2 to 4 months later. This immune response
slowly, reaching maximum concentration of agglu-
blood does not contain the Rh factor—that is, into
When red blood cells
African blacks, it is virtually 100 per cent.
the percentage of Rh-positives is about 95, whereas in
tive and 15 per cent, Rh negative. In American blacks,
usually much milder.
transfusion reactions, although the reactions are
people, some of the other Rh antigens can still cause
However, it must be noted that even in Rh-negative
, whereas a person who
the other Rh antigens. Anyone who has this type of
The type D antigen is widely prevalent in the
one of each of the three pairs of antigens.
manner of inheritance of these factors, each person has
for the D-d and E-e antigens. Also, because of the
C antigen always has the c antigen. The same is true
does not have the c antigen, but the person missing the
nated C, D, E, c, d, and e. A person who has a C antigen
. These types are desig-
There are six common types of Rh antigens, each of
reaction will develop.
fusion of blood containing the Rh antigen, before
massively exposed to an Rh antigen, such as by trans-
almost never occur. Instead, the person must first be
whereas in the Rh system, spontaneous agglutinins
causing transfusion reactions develop spontaneously,
O-A-B system, the plasma agglutinins responsible for
system and the Rh system is the following: In the
blood. The major difference between the O-A-B
Along with the O-A-B blood type system, the Rh
Rh Blood Types
agglutinins.
anti-B agglutinins. Type AB blood has both A and B
fore agglutinates with anti-A agglutinins. Type B
tinins. Type A blood has A agglutinogens and there-
agglutination of the four types of red blood cells. Type
Table 35–2 lists the presence (
that is, “agglutinated”—one knows that an antibody-
scope. If the red blood cells have become clumped—
minutes, the mixtures are observed under a micro-
another portion with anti-B agglutinin. After several
first separated from the plasma and diluted with saline.
formed in the following way: The red blood cells are
blood matching,
bloods can be appropriately matched. This is called
to determine the blood type of the recipient’s blood
Before giving a transfusion to a person, it is necessary
Blood Typing
be required, mainly the IgM antibodies; these anti-
occur, but also a different type of antibody seems to
hemolysis, because not only does
delayed
) that rupture the cell membranes, as
ment system, which releases proteolytic enzymes (the
the circulating blood. In this case, the antibodies cause
matched, immediate hemolysis of red cells occurs in
Sometimes, when recipient and donor bloods are mis-
Acute Hemolysis Occurs in Some Transfusion Reactions.
“hemolysis” of the red blood cells.
releasing hemoglobin into the plasma, which is called
cells destroys the membranes of the agglutinated cells,
tion of the cells or attack by phagocytic white blood
During ensuing hours to days, either physical distor-
process of “agglutination.” Then these clumps plug
agglutinin. This causes the cells to clump, which is the
to two or more red blood cells at the same time,
binding sites (IgM type), a single agglutinin can attach
ing themselves to the red blood cells. Because the
Blood Types; Transfusion; Tissue and Organ Transplantation
Chapter 35
453
cells agglutinate as a result of the agglutinins’ attach-
agglutinins have two binding sites (IgG type) or 10
thereby causing the cells to be bound together by the
small blood vessels throughout the circulatory system.
lysis of the red blood cells by activating the comple-
lytic complex
described in Chapter 34. Immediate intravascular
hemolysis is far less common than agglutination fol-
lowed by
there have to be a high titer of antibodies for lysis to
bodies are called hemolysins.
and the blood type of the donor blood so that the
blood typing and
and these are per-
One portion is then mixed with anti-A agglutinin and
antigen reaction has resulted.
+) or absence (-) of
O red blood cells have no agglutinogens and therefore
do not react with either the anti-A or the anti-B agglu-
blood has B agglutinogens and agglutinates with
agglutinogens and agglutinates with both types of
blood type system is also important when transfusing
enough agglutinins to cause a significant transfusion
Rh Antigens—“Rh-Positive” and “Rh-Negative” People.
which is called an Rh factor
population and considerably more antigenic than
antigen is said to be Rh positive
does not have type D antigen is said to be Rh negative.
About 85 per cent of all white people are Rh posi-
Rh Immune Response
Formation of Anti-Rh Agglutinins.
containing Rh factor are injected into a person whose
an Rh-negative person—anti-Rh agglutinins develop
occurs to a much greater extent in some people than
an Rh-negative person eventually becomes strongly
Different Blood Types with Anti-A or Anti-B Agglutinins
Blood Typing, Showing Agglutination of Cells of the
Table 35–2
in the Sera
Anti-A
Anti-B
Red Blood Cell Types
Sera
O
-
-
A
+
-
B
-
+
AB
+
+
the plasma of the recipient, thereby decreasing the
, for the following reason: The plasma portion of
of the recipient’s
are agglutinated. It is rare that the
recipient who has another blood type, a transfusion
from Mismatched Blood Types
Transfusion Reactions Resulting
the expectant mother, thereby interfering with the
antibody production in the expectant mother. The
antibody is to inhibit antigen-induced B lymphocyte
completely understood, but one effect of the anti-D
The mechanism by which Rh immunoglobulin
amounts of D antibodies during the second pregnancy.
This greatly reduces the risk of developing large
gestation. The anti-D antibody is also administered to
lin globin, an anti-D antibody
an Rh-positive fetus. In the 1970’s, a dramatic reduc-
The D antigen of
Prevention of Erythroblastosis Fetalis.
cells, a process that requires 6 or more weeks, the anti-
cells are replaced with the infant’s own Rh-positive
kernicterus. By the time these transfused Rh-negative
several times during the first few weeks of life, mainly
is being removed. This procedure may be repeated
more hours while the neonate’s own Rh-positive blood
blood with Rh-negative blood. About 400 milliliters of
for erythroblastosis fetalis is to replace the neonate’s
Treatment of the Erythroblastotic Neonate.
cells, causing destruction of many, a condition called
fetalis is usually the cause of death, many children who
tory system, and it is because of the presence of these
passed from the baby’s bone marrow into the circula-
, are
cells, including many
production of red cells, many early forms of red blood
during the middle of gestation. Because of the rapid
replace the hemolyzed red blood cells. The liver and
The hematopoietic tissues of the infant attempt to
blood cells.
months after birth, destroying more and more red
circulate in the infant’s blood for another 1 to 2
The jaundiced, ery-
Clinical Picture of Erythroblastosis.
also attack and damage other cells of the body.
skin to become yellow (jaundiced). The antibodies can
hemoglobin into bilirubin, which causes the baby’s
blood. The fetus’s macrophages then convert the
quently hemolyze, releasing hemoglobin into the
fetus’s blood. The agglutinated red blood cells subse-
fetus’s blood. There they cause agglutination of the
Rh antibodies have formed in the mother, they diffuse
Effect of the Mother’s Antibodies on the Fetus.
pregnancies.
However, about 3 per cent of second Rh-positive
sure to the fetus’s Rh antigen. In turn, the mother’s
inherited the Rh-positive antigen from the father, and
negative and the father Rh positive. The baby has
instances of erythroblastosis fetalis, the mother is Rh
phagocytosis of the fetus’s red blood cells. In most
of the Newborn”)
Erythroblastosis Fetalis (“Hemolytic Disease
tion caused by mismatched type A or B blood.
factor, the transfusion reaction is greatly enhanced and
person, who is now already immunized against the Rh
reaction occurs, although it is usually mild. On subse-
delayed
tissue macrophage system. Thus, a
ing in the blood. These cells are then hemolyzed by the
However, anti-Rh antibodies can develop in sufficient
positive blood, transfusion of Rh-positive blood into
Characteristics of Rh Transfusion Reactions.
Blood Cells, Immunity, and Blood Clotting
454
Unit VI
If an Rh-
negative person has never before been exposed to Rh-
that person will likely cause no immediate reaction.
quantities during the next 2 to 4 weeks to cause agglu-
tination of those transfused cells that are still circulat-
transfusion
quent transfusion of Rh-positive blood into the same
can be immediate and as severe as a transfusion reac-
Erythroblastosis fetalis is a disease of the fetus and
newborn child characterized by agglutination and
the mother develops anti-Rh agglutinins from expo-
agglutinins diffuse through the placenta into the fetus
and cause red blood cell agglutination.
Incidence of the Disease.
An Rh-negative mother having
her first Rh-positive child usually does not develop
sufficient anti-Rh agglutinins to cause any harm.
babies exhibit some signs of erythroblastosis fetalis;
about 10 per cent of third babies exhibit the disease;
and the incidence rises progressively with subsequent
After anti-
slowly through the placental membrane into the
throblastotic newborn baby is usually anemic at birth,
and the anti-Rh agglutinins from the mother usually
spleen become greatly enlarged and produce red
blood cells in the same manner that they normally do
nucleated blastic forms
nucleated blastic red blood cells that the disease is
called erythroblastosis fetalis.
Although the severe anemia of erythroblastosis
barely survive the anemia exhibit permanent mental
impairment or damage to motor areas of the brain
because of precipitation of bilirubin in the neuronal
kernicterus.
One treatment
Rh-negative blood is infused over a period of 1.5 or
to keep the bilirubin level low and thereby prevent
Rh agglutinins that had come from the mother will
have been destroyed.
the Rh blood group system is the primary culprit in
causing immunization of an Rh-negative mother to
tion in the incidence of erythroblastosis fetalis was
achieved with the development of Rh immunoglobu-
that is administered to
the expectant mother starting at 28 to 30 weeks of
Rh-negative women who deliver Rh-positive babies to
prevent sensitization of the mothers to the D antigen.
globin prevents sensitization of the D antigen is not
administered anti-D antibody also attaches to D-
antigen sites on Rh-positive fetal red blood cells that
may cross the placenta and enter the circulation of
immune response to the D antigen.
If donor blood of one blood type is transfused into a
reaction is likely to occur in which the red blood cells
of the donor blood
transfused blood causes agglutination
cells
the donor blood immediately becomes diluted by all
well as on the tissue cells. Therefore, tissue typing for
The HLA antigens occur on the white blood cells as
the same six HLA antigens. Development of signifi-
persons, except in the case of identical twins, to have
Consequently, it is virtually impossible for two
represents more than a trillion possible combinations.
ferent HLA antigens to choose from. Therefore, this
branes of each person, but there are about 150 dif-
. Six of
The most important antigens for causing graft rejec-
Tissue Typing—The HLA Complex of Antigens
experimental success.
associated with transplantation. The following specific
planting certain tissues and organs, serious attempts
Reactions in Transplanted Tissue
graft liver and heart transplants for 1 to 15 years.
have been successful for at least 5 to 15 years, and allo-
of tissues between persons, many kidney allografts
tissue, bone marrow, and lung. With proper “matching”
to another are skin, kidney, heart, liver, glandular
mentally or for therapeutic purposes, from one person
have been transplanted as allografts, either experi-
prevent the immune reactions.
immune reactions almost always occur, causing death
xenografts
At the other extreme, in the case of
, cells in the transplant contain vir-
Transplantation of Cellular Tissues.
xenograft
animal of one species to one of another species, a
another animal of the same species, an
from one identical twin to another, an
foreign bacteria or red cells.
other words, most recipients are just as able to resist
body of a recipient can produce immune reactions. In
quently, foreign cells transplanted anywhere into the
its own additional complement of antigens. Conse-
in other cells of the body, and each bodily tissue has
and Organs
Transplantation of Tissues
with an artificial kidney.
to 12 days, as explained in Chapter 31, unless treated
plete and fails to resolve, the patient dies within a week
cause acute renal shutdown. If the shutdown is com-
latory shock, and renal tubular blockage together
the kidney tubules. Thus, renal vasoconstriction, circu-
sorbed. Yet water continues to be reabsorbed, causing
harm; if it is great, then only a small percentage is reab-
amount is still slight, it can be reabsorbed through the
glomerular membranes into the kidney tubules. If this
hemoglobin), much of the excess leaks through the
globin” (a plasma protein that binds small amounts of
greater than the quantity that can bind with “hapto-
output decrease. Third, if the total amount of free
pressure falls very low, and renal blood flow and urine
tion, often causes circulatory shock. The arterial blood
recipient, along with production of toxic substances
striction. Second, loss of circulating red cells in the
causes: First, the antigen-antibody reaction of the
The kidney shutdown seems to result from three
renal failure.
, which can begin within a few minutes
kidney failure
Acute Kidney Shutdown After Transfusion Reactions.
than a day.
into the intestines by way of the liver bile, so that jaun-
function is normal, the bile pigment will be excreted
. But if liver
colored with yellow bile pigment
that is, the person’s internal tissues and skin
as discussed in Chapter 70. The concentration of biliru-
into bilirubin and later excreted in the bile by the liver,
from the red cells is then converted by the phagocytes
tosis of agglutinated cells. The hemoglobin released
hemolysins or later hemolysis resulting from phagocy-
As explained earlier, all transfusion reactions even-
matched donor cells.
recipient’s agglutinins can still agglutinate the mis-
the agglutinins in the recipient’s plasma. Therefore, the
low to cause agglutination. Conversely, the small
Blood Types; Transfusion; Tissue and Organ Transplantation
Chapter 35
455
titer of the infused agglutinins to a level usually too
amount of infused blood does not significantly dilute
tually cause either immediate hemolysis resulting from
bin in the body fluids often rises high enough to cause
jaundice—
become
dice usually does not appear in an adult person unless
more than 400 milliliters of blood is hemolyzed in less
One of
the most lethal effects of transfusion reactions is
to few hours and continue until the person dies of
transfusion reaction releases toxic substances from the
hemolyzing blood that cause powerful renal vasocon-
from the hemolyzed cells and from the immune reac-
hemoglobin released into the circulating blood is
tubular epithelium into the blood and will cause no
the tubular hemoglobin concentration to rise so high
that the hemoglobin precipitates and blocks many of
Most of the different antigens of red blood cells that
cause transfusion reactions are also widely present
invasion by foreign tissue cells as to resist invasion by
Autografts, Isografts, Allografts, and Xenografts.
A trans-
plant of a tissue or whole organ from one part of the
same animal to another part is called an autograft;
isograft; from
one human being to another or from any animal to
allograft; and
from a lower animal to a human being or from an
.
In the case of auto-
grafts and isografts
tually the same types of antigens as in the tissues of
the recipient and will almost always continue to live
normally and indefinitely if an adequate blood supply
is provided.
,
of the cells in the graft within 1 day to 5 weeks after
transplantation unless some specific therapy is used to
Some of the different cellular tissues and organs that
Attempts to Overcome Immune
Because of the extreme potential importance of trans-
have been made to prevent antigen-antibody reactions
procedures have met with some degrees of clinical or
tion are a complex called the HLA antigens
these antigens are present on the tissue cell mem-
cant immunity against any one of these antigens can
cause graft rejection.
transplantation. Curr Opin Hematol 9:527, 2002.
Triulzi DJ: Specialized transfusion support for solid organ
Suppl):1051, 2004.
Trigg ME: Hematopoietic stem cells. Pediatrics 113(4
Semin Hematol 37:130, 2000.
possible roles in normal human physiology and disease.
Telen MJ: Red blood cell surface adhesion molecules: their
Physiol Lung Cell Mol Physiol 286:L1129, 2004.
in the pathogenesis of lung transplant rejection. Am J
graft rejection: a focus on immunity to type V collagen
Sumpter TL, Wilkes DS: Role of autoimmunity in organ allo-
plantation tolerance in humans. Transplantation 77:932,
Strober S, Lowsky RJ, Shizuru JA, et al: Approaches to trans-
stitutes. News Physiol Sci 16:38, 2001.
Spahn DR, Pasch T: Physiological properties of blood sub-
plantation: a passing era. J Surg Res 117:154, 2004.
Schulak JA: Steroid immunosuppression in kidney trans-
the “Holy Grail” of transplantation. J Surg Res 111:109,
Schroeder RA, Marroquin CE, Kuo PC: Tolerance and
and immunological challenges. Nat Rev Immunol 4:259,
Ricordi C, Strom TB: Clinical islet transplantation: advances
questions. Transplantation 77:940, 2004.
human organ transplants: a few additional corollaries and
Miller J, Mathew JM, Esquenazi V: Toward tolerance to
13:36, 1999.
of polyagglutination in transfusion medicine. Blood Rev
Horn KD: The classification, recognition and significance
summary and update. Am J Transplant 3:525, 2003.
Heeger PS: T-cell allorecognition and transplant rejection: a
Arch Dis Child Fetal Neonatal Ed 88:F6, 2003.
Gottstein R, Cooke RW: Systematic review of intravenous
blood transfusion. Hematol J 4:87, 2003.
Goodnough LT, Shander A: Evolution in alternatives to
43:1661, 2003.
Bowman J: Thirty-five years of Rh prophylaxis. Transfusion
Blood 95:375, 2000.
Avent ND, Reid ME: The Rh blood group system: a review.
new biotherapeutic approach? Oncogene 22:6564, 2003.
therapy of solid malignancies via HLA class II antigens: a
Altomonte M, Fonsatti E, Visintin A, Maio M: Targeted
bin? Nat Rev Drug Discov 3:152, 2004.
Alayash AI: Oxygen therapeutics: can we tame haemoglo-
nity for disease, the story will change overnight.
the same time destroying the recipient’s specific immu-
success. When someone does finally succeed in block-
To summarize, transplantation of living tissues in
early cancer cells before they can begin to proliferate.
in an immunosuppressed person, presumably because
tion, the incidence of cancer is several times as great
bacterial and viral infections become rampant. In addi-
tected from infectious disease; therefore, sometimes
rejection reaction. This has proved to be one of
is especially efficacious in blocking the T-cell
on the formation of helper T cells and, therefore,
, which has a specific inhibitory effect
of antibodies and T cells, especially the drug
and, therefore, block formation
Various drugs that have a toxic effect on the
formation of antibodies and T cells.
lymphoid tissue and, therefore, decrease
, which suppress the growth of all
plasma antibodies. Some of the therapeutic agents that
system important for killing grafted cells, their sup-
the T cells are mainly the portion of the immune
suppress the immune system. Furthermore, because
typing, allografts seldom resist rejection for more than
the normal person, even with the best possible tissue
use of significant therapy to prevent rejection. But in
immune system, grafts can be successful without the
graft rejection would not occur. In fact, in an occa-
Prevention of Graft Rejection by Suppressing
rejected because of immune reactions.
child. The match in identical twins is exact, so that
hazardous. The best success has been with tissue-type
recipient, the grafting procedure has become far less
essential to allow allograft acceptance. Therefore, by
genic, for which reason a precise match of some
cells of a special dye.
the rate of trans-membrane uptake by the lymphocytic
are tested for membrane damage, usually by testing
antisera and complement; after incubation, the cells
blood. The lymphocytes are mixed with appropriate
cytes that have been separated from the person’s
Blood Cells, Immunity, and Blood Clotting
456
Unit VI
these antigens is done on the membranes of lympho-
Some of the HLA antigens are not severely anti-
antigens between donor and recipient is not always
obtaining the best possible match between donor and
matches between siblings and between parent and
transplants between identical twins are almost never
the Immune System
If the immune system were completely suppressed,
sional person who has serious depression of the
a few days or weeks without use of specific therapy to
pression is much more important than suppression of
have been used for this purpose include the following:
1. Glucocorticoid hormones isolated from adrenal
cortex glands (or drugs with glucocorticoid-like
activity)
2.
lymphoid system
azathioprine.
3. Cyclosporine
the most valuable of all the drugs because it does
not depress some other portions of the immune
system.
Use of these agents often leaves the person unpro-
the immune system is important in destroying many
human beings has had very limited but important
ing the immune response of the recipient without at
References
immunoglobulin in haemolytic disease of the newborn.
2004.
2003.
2004.
