
intercostals.
press the abdominal contents upward against the diaphragm, and (2)
The muscles that pull the rib cage downward during expiration are mainly
which lift the first two ribs.
ribs; and (3)
which lift upward on the sternum; (2)
muscles,
nal intercostals,
of expiration. The most important muscles that raise the rib cage are the
ration, and those muscles that depress the chest cage are classified as muscles
fore, all the muscles that elevate the chest cage are classified as muscles of inspi-
20 per cent greater during maximum inspiration than during expiration. There-
away from the spine, making the anteroposterior thickness of the chest about
ribs project almost directly forward, so that the sternum also moves forward,
backward toward the vertebral column. But when the rib cage is elevated, the
ward, as shown on the left side of Figure 37–1, thus allowing the sternum to fall
expands the lungs because, in the natural resting position, the ribs slant down-
The second method for expanding the lungs is to raise the rib cage. This
upward against the bottom of the diaphragm, thereby compressing the lungs.
abdominal muscles,
the necessary rapid expiration, so that extra force is achieved mainly by con-
heavy breathing, however, the elastic forces are not powerful enough to cause
wall, and abdominal structures compresses the lungs and expels the air. During
of the lungs, chest
ration, the diaphragm simply relaxes, and the
diaphragm pulls the lower surfaces of the lungs downward. Then, during expi-
that is, by movement of the diaphragm. During inspiration, contraction of the
methods.
anteroposterior diameter of the chest cavity. Figure 37–1 shows these two
upward movement of the diaphragm to lengthen or shorten the chest cavity,
The lungs can be expanded and contracted in two ways: (1) by downward and
Muscles That Cause Lung Expansion and Contraction
Mechanics of Pulmonary Ventilation
abnormalities.
discussion of pulmonary ventilation, and the subsequent five chapters
and other facets of respiration. This chapter is a
to and from the body’s tissue cells; and
dioxide in the blood and body fluids
transport of oxygen and carbon
of oxygen and carbon dioxide between the alveoli
the atmosphere and the lung alveoli; (2)
four major functions: (1)
achieve these goals, respiration can be divided into
the tissues and to remove carbon dioxide. To
The goals of respiration are to provide oxygen to
Pulmonary Ventilation
C
H
A
P
T
E
R
3
7
471
pulmonary ventilation,
which means the inflow and outflow of air between
diffusion
and the blood; (3)
(4) regulation of ventilation
cover other respiratory functions plus the physiology of special respiratory
and (2) by elevation and depression of the ribs to increase and decrease the
Normal quiet breathing is accomplished almost entirely by the first method,
elastic recoil
traction of the
which pushes the abdominal contents
exter-
but others that help are the (1) sternocleidomastoid
anterior serrati, which lift many of the
scaleni,
the (1) abdominal recti, which have the powerful effect of pulling downward on
the lower ribs at the same time that they and other abdominal muscles also com-
internal
to about –1 centimeter of water. This slight negative
during normal inspiration, alveolar pressure decreases
“alveolar pressure”) of Figure 37–2 demonstrates that
pheric pressure (below 0). The second curve (labeled
air into the alveoli during inspiration, the pressure in
0 centimeters water pressure. To cause inward flow of
to be zero reference pressure in the airways—that is,
are equal to atmospheric pressure, which is considered
parts of the respiratory tree, all the way to the alveoli,
flowing into or out of the lungs, the pressures in all
lung alveoli. When the glottis is open and no air is
Alveolar Pressure
volume of 0.5 liter. Then, during expiration, the events
37–2, showing in the lower panel the increasing nega-
changing lung volume are demonstrated in Figure
These relationships between pleural pressure and
average of about –7.5 centimeters of water.
greater force and creates more negative pressure, to an
resting level. Then, during normal inspiration, expan-
is about –5 centimeters of water, which is the amount
pressure. The
suction, which means a slightly
pleura. As noted earlier, this is normally a slight
Pleural Pressure and Its Changes
freely as the chest expands and contracts.
lungs are held to the thoracic wall as if glued there,
pleural surface of the thoracic cavity. Therefore, the
cavity. Further, continual suction of excess fluid into
thoracic cavity, surrounded by a thin layer of
from the mediastinum. Instead, the lung “floats” in the
the chest cage, except where it is suspended at its hilum
ever there is no force to keep it inflated. Also, there
The lung is an elastic structure that collapses like a
That Cause the Movement
Movement of Air In and Out of the
and cause opposite leverage.
site manner, functioning as expiratory muscles because
The internal intercostals function exactly in the oppo-
ribs to raise them upward, thereby causing inspiration.
tion to the lower ribs, and this causes leverage on the
they contract, they pull the upper ribs forward in rela-
intercostals are elongated forward and downward. As
expiration are angled downward, and the external
tion and expiration. To the left, the ribs during
Figure 37–1 also shows the mechanism by which the
472
Unit VII
Respiration
external and internal intercostals act to cause inspira-
they angle between the ribs in the opposite direction
Lungs and the Pressures
balloon and expels all its air through the trachea when-
are no attachments between the lung and the walls of
pleural
fluid that lubricates movement of the lungs within the
lymphatic channels maintains a slight suction between
the visceral surface of the lung pleura and the parietal
except that they are well lubricated and can slide
During Respiration
Pleural pressure is the pressure of the fluid in the thin
space between the lung pleura and the chest wall
negative
normal pleural pressure at the beginning of inspiration
of suction required to hold the lungs open to their
sion of the chest cage pulls outward on the lungs with
tivity of the pleural pressure from –5 to –7.5 during
inspiration and in the upper panel an increase in lung
are essentially reversed.
Alveolar pressure is the pressure of the air inside the
the alveoli must fall to a value slightly below atmos-
A–P diameter
EXPIRATION
INSPIRATION
Abdominals
contracted
Elevated
rib cage
Diaphragmatic
contraction
Increased
vertical diameter
Increased
External
intercostals
contracted
Internal
intercostals
relaxed
tion of the intercostal muscles, and elevation and depression of
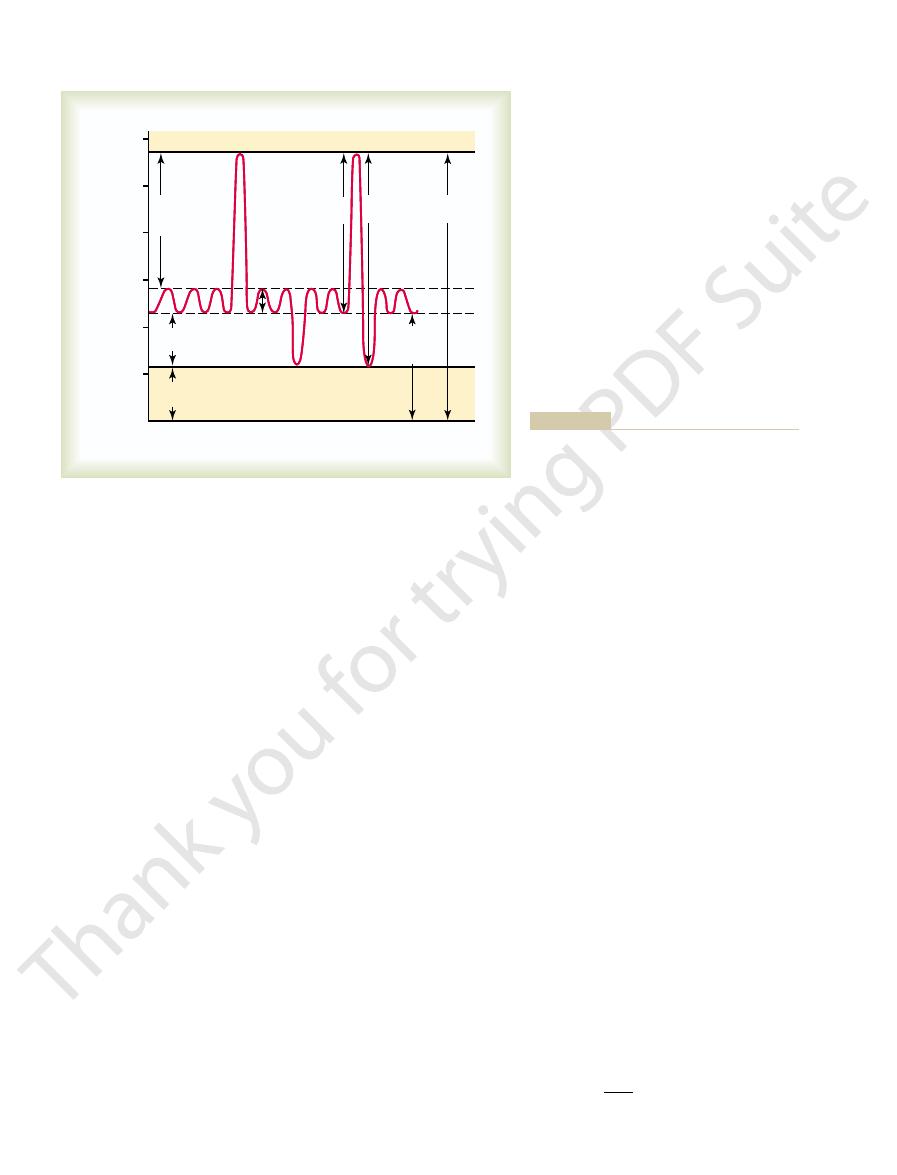
Figure 37–1
Contraction and expansion of the thoracic cage during expiration
and inspiration, demonstrating diaphragmatic contraction, func-
the rib cage.
O)
V
olume change (liters)
Pressure (cm H
2
0.25
0
+2
0
–2
–4
–6
–8
0.50
Expiration
Inspiration
Transpulmonary pressure
Lung volume
Alveolar pressure
Pleural pressure
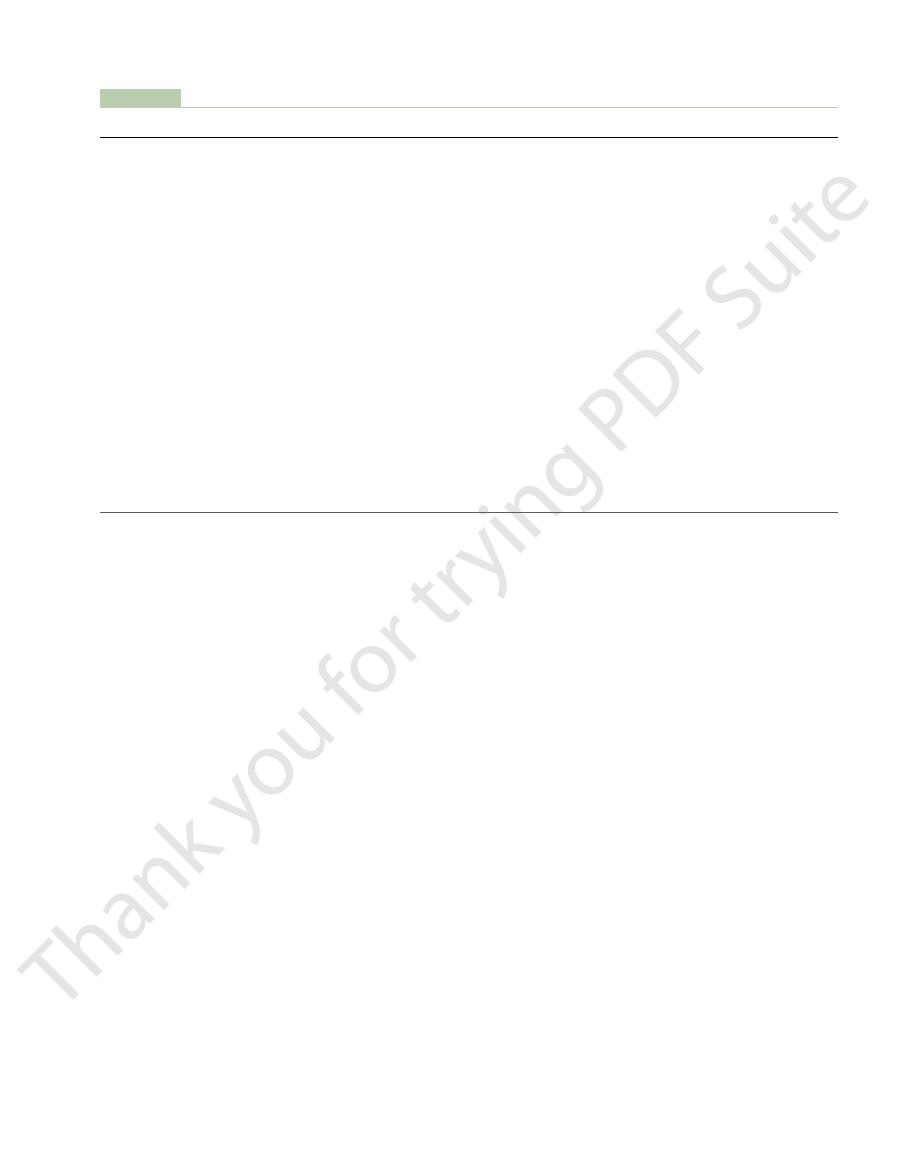
transpulmonary pressure during normal breathing.
Changes in lung volume, alveolar pressure, pleural pressure, and
Figure 37–2
about one third of the total lung elasticity, whereas the
to cause collapse of the air-filled lung represent only
required to expand saline solution–filled lungs. Thus,
air-filled lungs are about three times as great as those
saline solution–filled lung.
interface; therefore, the surface tension effect is not
the saline solution–filled lungs, there is no air-fluid
alveolar fluid and the air in the alveoli. In the case of
are filled with air, there is an interface between the
saline solution and when filled with air. When the lungs
tension is shown in Figure 37–4, which compares the
much more complex. The significance of surface
The elastic forces caused by surface tension are
ing even more elastic force.
stretched and unkinked, thereby elongating and exert-
then, when the lungs expand, the fibers become
among the lung parenchyma. In deflated lungs, these
The elastic forces of the lung tissue are determined
and other lung air spaces.
elastic forces caused by surface
be divided into two parts: (1)
determined by the elastic forces of the lungs. These can
The characteristics of the compliance diagram are
compliance diagram of the lungs.
expiratory compliance curve,
respectively, the
between successive steps. The two curves are called,
inspiration and expiration. Each curve is recorded by
monary pressure. Note that the relation is different for
Figure 37–3 is a diagram
after 10 to 20 seconds, will expand 200 milliliters.
sure increases 1 centimeter of water, the lung volume,
pressure. That is, every time the transpulmonary pres-
The total compliance of both lungs together in
pliance.
The extent to which the lungs will expand for each unit
recoil pressure.
piration, called the
the alveoli and that on the outer surfaces of the lungs,
pressure.
pleural pressure. This is called the
Finally, note in Figure 37–2 the
Transpulmonary Pressure.
1 centimeter of water,
During expiration, opposite pressures occur: The
Pulmonary Ventilation
Chapter 37
473
pressure is enough to pull 0.5 liter of air into the lungs
in the 2 seconds required for normal quiet inspiration.
alveolar pressure rises to about
+
and this forces the 0.5 liter of inspired air out of the
lungs during the 2 to 3 seconds of expiration.
difference between the alveolar pressure and the
transpulmonary
It is the pressure difference between that in
and it is a measure of the elastic forces in the lungs
that tend to collapse the lungs at each instant of res-
Compliance of the Lungs
increase in transpulmonary pressure (if enough time is
allowed to reach equilibrium) is called the lung com-
the normal adult human being averages about 200 mil-
liliters of air per centimeter of water transpulmonary
Compliance Diagram of the Lungs.
relating lung volume changes to changes in transpul-
changing the transpulmonary pressure in small steps
and allowing the lung volume to come to a steady level
inspiratory compliance curve and the
and the entire diagram is
called the
elastic forces of the lung
tissue itself and (2)
tension of the fluid that lines the inside walls of the
alveoli
mainly by elastin and collagen fibers interwoven
fibers are in an elastically contracted and kinked state;
compliance diagram of the lungs when filled with
present—only tissue elastic forces are operative in the
Note that transpleural pressures required to expand
one can conclude that the tissue elastic forces tending
Lung volume change (liters)
0.50
Expiration
Inspiration
0.25
0
– 4
–5
–6
Pleural pressure (cm H
2
O)
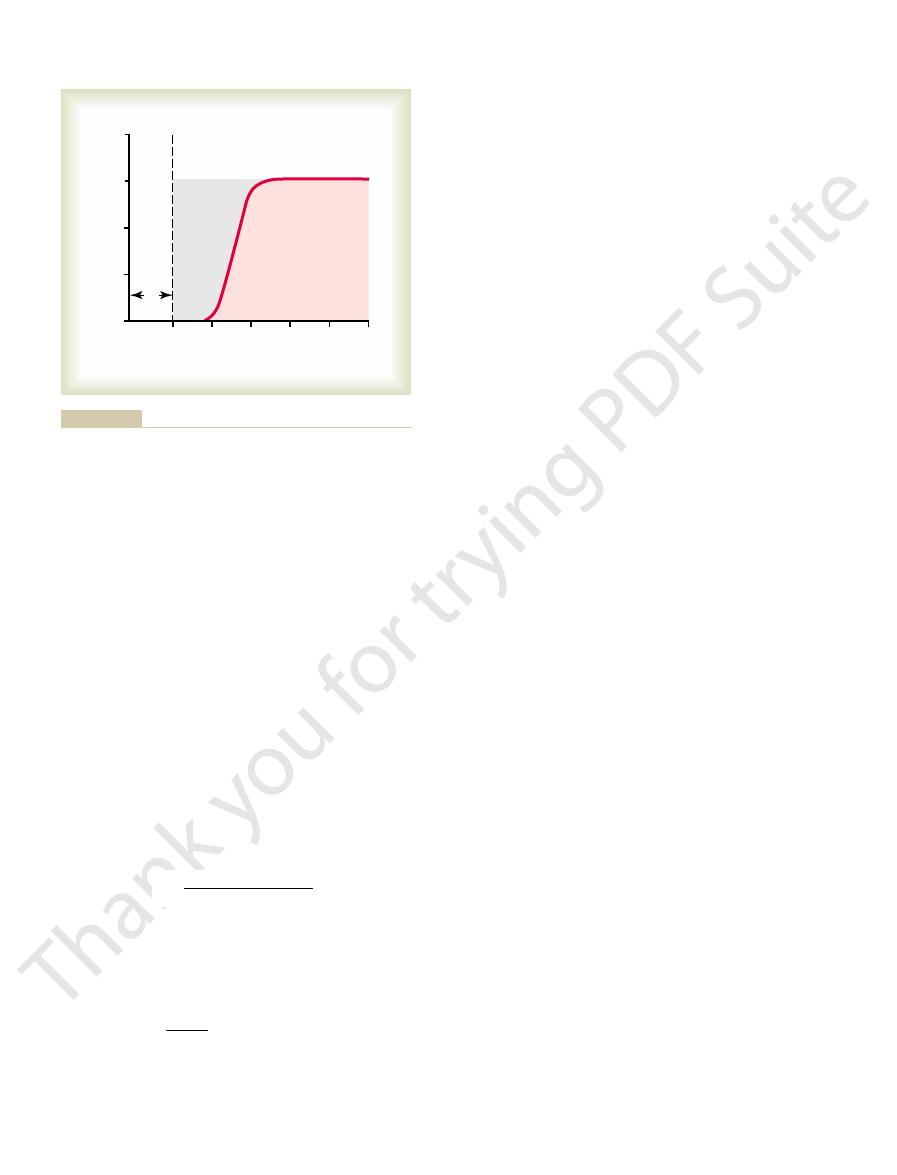
Figure 37–3
Compliance diagram in a healthy person. This diagram shows
compliance of the lungs alone.
Saline-filled
Air-filled
Lung volume change (liters)
0.50
0.25
0
0
–2
– 4
–6
–8
Pleural pressure (cm H
2
O)
Inspiration
Expiration
O) and pleural pressure is changed.
pheric pressure (0 cm H
filled lungs when the alveolar pressure is maintained at atmos-
Comparison of the compliance diagrams of saline-filled and air-
Figure 37–4
2
volumes, the limitations of the chest become extreme;
the lungs alone. Furthermore, when the lungs are
the combined system, compared with 200 ml/cm for
after removal from the chest cage. Therefore, the com-
inflate this total pulmonary system, almost twice as
a time while recording lung pressures and volumes. To
person. To do this, air is forced into the lungs a little at
The compliance of the entire pulmonary system (the
Lungs Together
still be required to expand the thoracic cage.
were not present in the thorax, muscular effort would
teristics, similar to those of the lungs; even if the lungs
lungs alone, without considering the thoracic cage. The
Thus far, we have discussed the expansibility of the
Effect of the Thoracic Cage
applied continuous positive pressure breathing.
not treated with strong measures, especially properly
adult person. This causes the condition called
and their lungs have an extreme tendency to collapse,
later than that. Therefore, many premature babies have
seventh months of gestation, and in some cases, even
Further, surfactant does not normally begin to be
in small premature babies, many of whom have alveoli
noted earlier are doubled. This is especially significant
radius (50 instead of 100 micrometers), the pressures
tension. Thus, when the alveoli have half the normal
lus, which means that the smaller the alveolus, the
Tension.
to expand the lungs.
great. Thus, one sees how important surfactant is in
be about 18 centimeters of water pressure, 4.5 times as
without any surfactant, the pressure would calculate to
(3 mm Hg). If the alveoli were lined with pure water
For the average-sized alveolus with a radius of about
alveoli, attempting to push the air out. The amount of
lapse the alveoli. This creates positive pressure in the
blocked, the surface tension in the alveoli tends to col-
Pressure in Occluded Alveoli Caused by Surface Tension.
included, between 5 and 30 dynes/cm.
without surfactant, 50 dynes/cm; normal fluids lining
water, 72 dynes/cm; normal fluids lining the alveoli but
ent water fluids is approximately the following: pure
In quantitative terms, the surface tension of differ-
surface.
water in the alveoli. This surface has from one
surface. Instead, part of the molecule dissolves,
for reducing the surface tension. It does this by not
several less important phospholipids, is responsible
The dipalmitoylphosphatidylcholine, along with
ions.
phatidylcholine, surfactant apoproteins,
dipalmitoylphos-
phospholipids, proteins, and ions. The most important
These cells are granular, containing lipid inclusions
type II alveolar epithelial cells,
greatly reduces the surface tension of water. It is
surface active agent in water,
Surfactant and Its Effect on Surface Tension.
surface tension elastic force.
elastic contractile force of the entire lungs, which is
alveoli to try to collapse. The net effect is to cause an
alveoli through the bronchi and, in doing so, causes the
This results in an attempt to force the air out of the
Here, the water surface is also attempting to contract.
raindrop. Now let us reverse these principles and see
together: that is, there is a tight contractile membrane
attempting to contract. This is what holds raindrops
another. As a result, the water surface is always
with air, the water molecules on the surface of the
When water forms a surface
Principle of Surface Tension.
Surfactant, Surface Tension, and Collapse
tension forces.
present in the alveolar fluid. Let
The fluid-air surface tension elastic forces of the
about two thirds.
474
Unit VII
Respiration
fluid-air surface tension forces in the alveoli represent
lungs also increase tremendously when the substance
called surfactant is not
us now discuss surfactant and its relation to the surface
of the Alveoli
water have an especially strong attraction for one
of water molecules around the entire surface of the
what happens on the inner surfaces of the alveoli.
called the
Surfactant is a
which means that it
secreted by special surfactant-secreting epithelial cells
called
which constitute
about 10 per cent of the surface area of the alveoli.
that are secreted in the surfactant into the alveoli.
Surfactant is a complex mixture of several
components are the phospholipid
and calcium
dissolving uniformly in the fluid lining the alveolar
while the remainder spreads over the surface of the
twelfth to one half the surface tension of a pure water
the alveoli and with normal amounts of surfactant
If the
air passages leading from the alveoli of the lungs are
pressure generated in this way in an alveolus can be cal-
culated from the following formula:
100 micrometers and lined with normal surfactant, this
calculates to be about 4 centimeters of water pressure
reducing alveolar surface tension and therefore also
reducing the effort required by the respiratory muscles
Effect of Alveolar Radius on the Pressure Caused by Surface
Note from the preceding formula that the pres-
sure generated as a result of surface tension in the
alveoli is inversely affected by the radius of the alveo-
greater the alveolar pressure caused by the surface
with radii less than one quarter that of an adult person.
secreted into the alveoli until between the sixth and
little or no surfactant in the alveoli when they are born,
sometimes as great as six to eight times that in a normal
respira-
tory distress syndrome of the newborn. It is fatal if
on Lung Expansibility
thoracic cage has its own elastic and viscous charac-
Compliance of the Thorax and the
lungs and thoracic cage together) is measured while
expanding the lungs of a totally relaxed or paralyzed
much pressure is needed as to inflate the same lungs
pliance of the combined lung-thorax system is almost
exactly one half that of the lungs alone—110 milliliters
of volume per centimeter of water pressure for
expanded to high volumes or compressed to low
Pressure
Surface tension
Radius of alveolus
=
¥
2
This is the maximum amount of
reserve volume.
3. The
This is the amount of air that remains in
volume.
2. The
breathe in, beginning at the normal expiratory
This is the
inspiratory reserve volume.
1. The
the important pulmonary capacities, which can be
To the right in Figure 37
monary capacities.
volumes together. Such combinations are called
In describing events in the pulmonary cycle, it is
Pulmonary Capacities
1200 milliliters.
expiration; this volume averages about
4. The
1100 milliliters.
tidal expiration; this normally amounts to about
3. The
3000 milliliters.
with full force; it is usually equal to about
2. The
about 500 milliliters in the adult male.
expired with each normal breath; it amounts to
1. The
The signi
lung volumes that, when added together, equal the
To the left in Figure 37
Pulmonary Volumes
capacities,
lation, the air in the lungs has been subdivided in this
For ease in describing the events of pulmonary venti-
lung volume under different conditions of breathing.
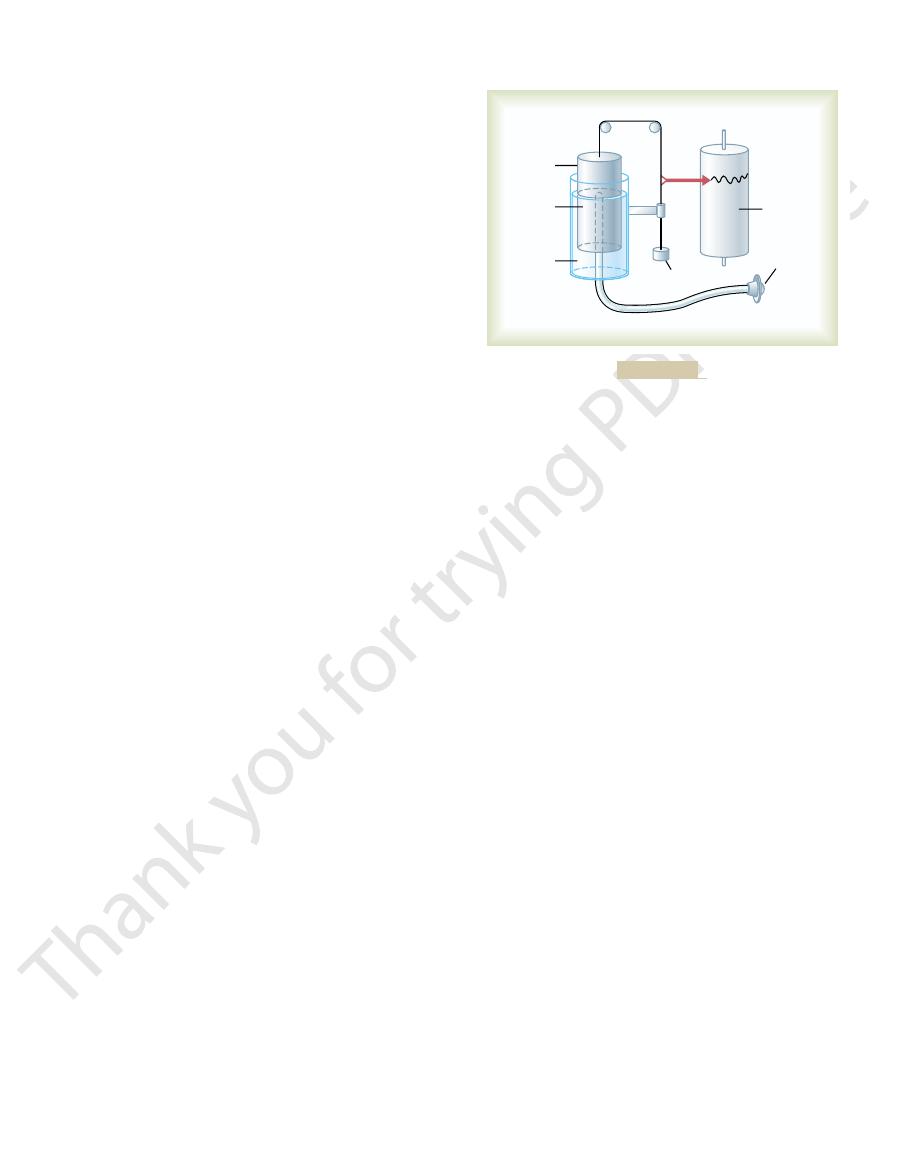
Figure 37
sheet of paper.
into and out of the chamber, the drum rises and falls,
the mouth with the gas chamber. When one breathes
breathing gas, usually air or oxygen; a tube connects
drum counterbalanced by a weight. In the drum is a
a drum inverted over a chamber of water, with the
5. It consists of
basic spirometer is shown in Figure 37
spirometry.
of the lungs, a process called
Volume—Spirometry
Pulmonary Volumes
muscle energy for the respiratory process alone.
creased pulmonary compliance. Therefore, one of the
can increase as much as 50-fold, especially if the person
during heavy exercise, the amount of energy required
by the body is required for pulmonary ventilation. But
ration, only 3 to 5 per cent of the total energy expended
airway resistance work.
airway resistance to movement of air into the lungs,
cosity of the lung and chest wall structures, called
the lung and chest elastic forces, called
fractions: (1) that required to expand the lungs against
The work of inspiration can be divided into three
chest cage. Thus, under resting conditions, the respira-
during inspiration; expiration is almost entirely a
breathing, all respiratory muscle contraction occurs
We have already pointed out that during normal quiet
“Work” of Breathing
that of the lungs alone.
when near these limits, the compliance of the com-
Pulmonary Ventilation
Chapter 37
475
bined lung-thorax system can be less than one fifth
passive process caused by elastic recoil of the lungs and
tory muscles normally perform “work” to cause inspi-
ration but not to cause expiration.
compliance work
or elastic work; (2) that required to overcome the vis-
tissue
resistance work; and (3) that required to overcome
called
Energy Required for Respiration.
During normal quiet respi-
has any degree of increased airway resistance or de-
major limitations on the intensity of exercise that can
be performed is the person’s ability to provide enough
and Capacities
Recording Changes in Pulmonary
A simple method for studying pulmonary ventilation
is to record the volume movement of air into and out
A typical
–
and an appropriate recording is made on a moving
–6 shows a spirogram indicating changes in
diagram into four volumes and four
which
are the average for a young adult man.
–6 are listed four pulmonary
maximum volume to which the lungs can be expanded.
ficance of each of these volumes is the
following:
tidal volume is the volume of air inspired or
inspiratory reserve volume is the extra volume
of air that can be inspired over and above the
normal tidal volume when the person inspires
expiratory reserve volume is the maximum
extra volume of air that can be expired by
forceful expiration after the end of a normal
residual volume is the volume of air
remaining in the lungs after the most forceful
sometimes desirable to consider two or more of the
pul-
–6 are listed
described as follows:
inspiratory capacity equals the tidal volume
plus the
amount of air (about 3500 milliliters) a person can
level and distending the lungs to the maximum
amount.
functional residual capacity equals the
expiratory reserve volume plus the residual
the lungs at the end of normal expiration (about
2300 milliliters).
vital capacity equals the inspiratory reserve
volume plus the tidal volume plus the expiratory
air a person can expel from the lungs after first
filling the lungs to their maximum extent and then
Water
Recording
drum
Mouthpiece
Counterbalancing
weight
Floating
drum
Oxygen
chamber
Spirometer.
Figure 37–5
culated from the degree of dilution of the helium, using
diluted by the functional residual capacity gases, and the
the gases of the lungs. As a result, the helium becomes
the spirometer, and the gases of the spirometer mix with
point, the subject immediately begins to breathe from
lungs is equal to the functional residual capacity. At this
the end of this expiration, the remaining volume in the
ing from the spirometer, the person expires normally. At
with helium at a known concentration. Before breath-
helium dilution method, as follows.
used in an indirect manner, usually by means of a
functional residual capacity, the spirometer must be
one half of the functional residual capacity. To measure
into the spirometer, and this volume constitutes about
to measure the functional residual capacity, because the
capacity. The spirometer cannot be used in a direct way
pulmonary disease, it is often desirable to measure this
each normal expiration, is important to lung function.
The functional residual capacity (FRC), which is the
Volume, and Total Lung Capacity—
Residual Capacity, Residual
Determination of Functional
ERV
ERV
ERV
IRV
these interrelations.
capacities; the student should think through and verify
1. Using these symbols, we present
given in Table 37
become standardized. The more important of these are
data, a number of abbreviations and symbols have
mathematical computations. To simplify these calcula-
dures that the pulmonary physician uses daily. Many of
asthenic people.
residual volume.
possible effort (about 5800 milliliters); it is equal
4. The
476
Unit VII
Respiration
expiring to the maximum extent (about
4600 milliliters).
total lung capacity is the maximum volume to
which the lungs can be expanded with the greatest
to the vital capacity plus the
All pulmonary volumes and capacities are about 20
to 25 per cent less in women than in men, and they are
greater in large and athletic people than in small and
Abbreviations and Symbols Used
in Pulmonary Function Studies
Spirometry is only one of many measurement proce-
these measurement procedures depend heavily on
tions as well as the presentation of pulmonary function
–
here a few simple algebraic exercises showing some of
the interrelations among the pulmonary volumes and
VC
=
+ V
T
+
VC
= IC +
TLC
= VC + RV
TLC
= IC + FRC
FRC
=
+ RV
Helium Dilution Method
volume of air that remains in the lungs at the end of
Because its value changes markedly in some types of
air in the residual volume of the lungs cannot be expired
A spirometer of known volume is filled with air mixed
volume of the functional residual capacity can be cal-
the following formula:
FRC
Ci
Cf
Vi
He
He
Spir
=
-
Ê
Ë
ˆ
¯
1
Lung volume (ml)
5000
6000
1000
2000
3000
4000
Time
Inspiration
Inspiratory
capacity
Inspiratory
reserve
volume
Expiratory
reserve volume
Vital
capacity
Expiration
Total lung
capacity
Tidal
volume
Functional
residual
capacity
Residual
volume
normal breathing and during maximal inspiration
Diagram showing respiratory excursions during
Figure 37–6
and maximal expiration.
the subject suddenly takes a deep breath of oxygen. This
7. In making this measurement,
the graph in Figure 37
Measurement of the Dead Space Volume.
lungs.
atmosphere. Therefore, the dead space is very disad-
rst, before any of the air from the alveoli reaches the
On expiration, the air in the dead space is expired
because it is not useful for gas exchange.
nose, pharynx, and trachea. This air is called
sages where gas exchange does not occur, such as the
on Alveolar Ventilation
and Its Effect
alveolar ducts, and respiratory bronchioles. The rate at
blood. These areas include the alveoli, alveolar sacs,
of the lungs, where air is in proximity to the pulmonary
The ultimate importance of pulmonary ventilation is
Alveolar Ventilation
thirds these values for longer than 1 minute.
greater than 200 L/min, or more than 30 times normal.
adult man. This can give a minute respiratory volume
as the vital capacity, about 4600 milliliters in a young
per minute, and the tidal volume can become as great
The respiratory rate occasionally rises to 40 to 50
only 2 to 4 breaths per minute.
volume as low as 1.5 L/min and a respiratory rate of
respiratory volume averages about 6 L/min.
is about 12 breaths per minute. Therefore, the
about 500 milliliters, and the normal respiratory rate
The normal tidal volume is
piratory rate per minute.
minute; this is equal to the
The
Times Tidal Volume
Equals Respiratory Rate
Minute Respiratory Volume
ERV
RV
capacity (IC) to the FRC. That is,
spirometry, from the FRC. Also, the total lung capacity
tory reserve volume (ERV), as measured by normal
volume (RV) can be determined by subtracting expira-
Once the FRC has been determined, the residual
initial volume of the spirometer.
concentration of helium in the spirometer, and Vi
concentration of helium in the spirometer, Cf
where FRC is functional residual capacity, Ci
Pulmonary Ventilation
Chapter 37
477
He
is initial
He
is final
Spir
is
(TLC) can be determined by adding the inspiratory
= FRC –
and
TLC
= FRC + IC
minute respiratory volume is the total amount of
new air moved into the respiratory passages each
tidal volume times the res-
minute
A person
can live for a short period with a minute respiratory
Most people cannot sustain more than one half to two
to continually renew the air in the gas exchange areas
which new air reaches these areas is called alveolar
ventilation.
“Dead Space”
Some of the air a person breathes never reaches the
gas exchange areas but simply fills respiratory pas-
dead space
air
fi
vantageous for removing the expiratory gases from the
A simple method
for measuring dead space volume is demonstrated by
–
Table 37–1
rate of carbon monoxide uptake per minute
Sa
amount of carbon dioxide eliminated per
S
rate of oxygen uptake per minute
Cv
alveolar ventilation per minute
Ca
inspired volume of ventilation per minute
cardiac output
volume of alveolar gas
R
respiratory exchange ratio
volume of dead space gas
P
ACO
C
compliance
P
ow of air into
P
Raw
resistance of the airways to
VC
vital capacity
Pa
TLC
total lung capacity
Pa
IRV
inspiratory reserve volume
P
IC
inspiratory capacity
P
RV
residual volume
P
ERV
expiratory reserve volume
Ppl
pleural pressure
FRC
functional residual capacity
Palv
alveolar pressure
tidal volume
P
Abbreviations and Symbols for Pulmonary Function
V
T
B
atmospheric pressure
O2
partial pressure of oxygen
CO2
partial pressure of carbon dioxide
N2
partial pressure of nitrogen
O2
partial pressure of oxygen in arterial blood
CO2
partial pressure of carbon dioxide in arterial blood
fl
AO2
partial pressure of oxygen in alveolar gas
the lung
2
partial pressure of carbon dioxide in alveolar gas
V
D
AH2O
partial pressure of water in alveolar gas
V
A
V
.
I
V
.
E
expired volume of ventilation per minute
V
.
s
shunt flow
V
.
A
O2
concentration of oxygen in arterial blood
V
.
o
2
¯o
2
concentration of oxygen in mixed venous blood
V
.
co
2
O2
percentage saturation of hemoglobin with oxygen
minute
V
.
co
O2
percentage saturation of hemoglobin with oxygen
in arterial blood
Dlo
2
diffusing capacity of the lungs for oxygen
Dl
CO
diffusing capacity of the lungs for carbon
monoxide
˙
Q
slightly with age.
a young adult man is about 150 milliliters. This increases
The normal dead space air in
Normal Dead Space Volume.
milliliters. The dead space would be
square centimeters, and the total volume expired is 500
graph is 30 square centimeters, the pink area is 70
Let us assume, for instance, that the gray area on the
of expired air.
is dead space air and V
cation, the following equation is used:
For exact quanti
this area is a measure of the volume of dead space air.
gure. With a little thought, the student can see that the
concentration in the alveoli, as shown to the right in the
only alveolar air remains. Therefore, the recorded nitro-
dead space air has been washed from the passages, and
space air. After still more air has been expired, all the
centration rises rapidly, because alveolar air containing
begins to reach the nitrogen meter, the nitrogen con-
gen concentration is zero. Then, when alveolar air
part of the record, only oxygen appears, and the nitro-
completely replaced by oxygen. Therefore, in the early
the respiratory passageways, where the air has been
gure. The
through a rapidly recording nitrogen meter, which
completely replace this air. Then the person expires
lls the entire dead space with pure oxygen. Some
478
Unit VII
Respiration
fi
oxygen also mixes with the alveolar air but does not
makes the record shown in the fi
first portion
of the expired air comes from the dead space regions of
large amounts of nitrogen begins to mix with the dead
gen concentration reaches a plateau level equal to its
fi
gray area represents the air that has no nitrogen in it;
fi
where V
D
E
is the total volume
, or
ml
500
150
30 70
30
+
¥
Pink area Gray area
Gray area V
V
D
E
=
¥
+
walls of the bronchi, less extensive curved cartilage
ve sixths of the way around the trachea. In the
trachea from collapsing, multiple cartilage rings extend
passage of air to and from the alveoli. To keep the
bronchioles.
tributed to the lungs by way of the trachea, bronchi, and
ing especially the respiratory passageways. The air is dis-
8 shows the respiratory system, demonstrat-
Figure 37
Trachea, Bronchi, and Bronchioles
Functions of the Respiratory
dioxide in the alveoli. Therefore, almost all discussions
150), or 4200 ml/min.
rate of 12 breaths per minute, alveolar ventilation
normal dead space of 150 milliliters, and a respiratory
Thus, with a normal tidal volume of 500 milliliters, a
logic dead space volume.
is the tidal volume, and V
minute, V
minute, Freq is the frequency of respiration per
Freq
areas each minute. It is equal to the respiratory rate
Rate of Alveolar Ventilation
monary diseases.
space, or 1 to 2 liters. These problems are discussed
parts of the lungs, the physiologic dead space may be as
are functional in the normal lung, but in a person with
dead space. In a normal person, the anatomic and phys-
logic dead space,
measurement of dead space, this is called the
When the alveolar dead space is included in the total
view, these alveoli must also be considered dead space.
monary capillaries. Therefore, from a functional point of
On occasion, some of the alveoli themselves are
space.
exchange areas; this space is called the
The method just
Anatomic Versus Physiologic Dead Space.
described for measuring the dead space measures the
volume of all the space of the respiratory system other
than the alveoli and their other closely related gas
anatomic dead
nonfunctional or only partially functional because of
absent or poor blood flow through the adjacent pul-
physio-
in contradistinction to the anatomic
iologic dead spaces are nearly equal because all alveoli
partially functional or nonfunctional alveoli in some
much as 10 times the volume of the anatomic dead
further in Chapter 39 in relation to pulmonary gaseous
exchange and in Chapter 42 in relation to certain pul-
Alveolar ventilation per minute is the total volume of
new air entering the alveoli and adjacent gas exchange
times the amount of new air that enters these areas
with each breath.
A
=
•
(V
T
– V
D
)
where
A
is the volume of alveolar ventilation per
T
D
is the physio-
equals 12
¥ (500 –
Alveolar ventilation is one of the major factors
determining the concentrations of oxygen and carbon
of gaseous exchange in the following chapters on the
respiratory system emphasize alveolar ventilation.
Passageways
–
One of the most important problems in all the respi-
ratory passageways is to keep them open and allow easy
about fi
plates also maintain a reasonable amount of rigidity yet
allow sufficient motion for the lungs to expand and
V
.
V
.
200
300
400
500
0
100
Per cent nitrogen
0
20
40
Inspiration of pure oxygen
60
80
Air expired (ml)
R
e
c
o
rd
e
d
n
itr
og
en concen
t
ration
after a single previous inspiration of pure oxygen. This record can
Record of the changes in nitrogen concentration in the expired air
Figure 37–7
be used to calculate dead space, as discussed in the text.
Local Secretory Factors Often Cause Bronchiolar Constriction.
when microemboli occlude small pulmonary arteries.
tion. Also, a bronchiolar constrictor re
noxious gases, dust, cigarette smoke, or bronchial infec-
of the respiratory passageways themselves, initiated by
exes that originate in the lungs. Most of
atropine,
effects of acetylcholine, such as
When this occurs, administration of drugs that block the
bronchiolar constriction, superimposed parasympa-
to moderate constriction of the bronchioles. When a
and, when activated, cause mild
acetylcholine
nerves penetrate the lung parenchyma. These nerves
bronchial tree.
especially epinephrine, because of its greater stimula-
of the adrenal gland medullae. Both these hormones
central portions of the lung. However, the bronchial tree
Nervous and Local Control of the Bronchiolar Musculature—
lecting in the lumens of the bronchioles.
walls, (2) edema occurring in the walls, or (3) mucus col-
Yet in disease conditions, the smaller bronchioles
only a minute amount of air must pass.
parallel terminal bronchioles, through each of which
bronchi near the trachea. The reason for this high resist-
breathing. The greatest amount of resistance to air
respiratory conditions,
Resistance to Airflow in the Bronchial Tree.
itself.
of the smaller bronchi and larger bronchioles, often
bers. Many
respiratory bronchiole,
terminal bronchiole, called the
entirely smooth muscle, with the exception of the most
bronchioles
muscle. Also, the walls of the
tilage plates, the walls are composed mainly of smooth
bronchi
trachea
Muscular Wall of the Bronchi and Bronchioles and Its Control.
enlarge, the bronchioles also enlarge, but not as much.
pressures that expand the alveoli. That is, as the alveoli
collapsing by the rigidity of their walls. Instead, they are
1.5 millimeters. The bronchioles are not prevented from
the bronchioles, which usually have diameters less than
contract. These plates become progressively less exten-
Pulmonary Ventilation
Chapter 37
479
sive in the later generations of bronchi and are gone in
kept expanded mainly by the same transpulmonary
In
all areas of the
and
not occupied by car-
are almost
which is mainly pulmonary epithelium and underlying
fibrous tissue plus a few smooth muscle fi
obstructive diseases of the lung result from narrowing
because of excessive contraction of the smooth muscle
Under normal
air flows through the respiratory
passageways so easily that less than 1 centimeter of
water pressure gradient from the alveoli to the atmos-
phere is sufficient to cause enough airflow for quiet
flow
occurs not in the minute air passages of the terminal
bronchioles but in some of the larger bronchioles and
ance is that there are relatively few of these larger
bronchi in comparison with the approximately 65,000
often play a far greater role in determining airflow
resistance because of their small size and because they
are easily occluded by (1) muscle contraction in their
“Sympathetic” Dilation of the Bronchioles.
Direct control of
the bronchioles by sympathetic nerve fibers is relatively
weak because few of these fibers penetrate to the
is very much exposed to norepinephrine and epineph-
rine released into the blood by sympathetic stimulation
—
tion of beta-adrenergic receptors—cause dilation of the
Parasympathetic Constriction of the Bronchioles.
A few
parasympathetic nerve fibers derived from the vagus
secrete
disease process such as asthma has already caused some
thetic nervous stimulation often worsens the condition.
can sometimes
relax the respiratory passages enough to relieve the
obstruction.
Sometimes the parasympathetic nerves are also acti-
vated by refl
these begin with irritation of the epithelial membrane
flex often occurs
Several substances formed in the lungs themselves are
Trachea
Epiglottis
Pharynx
Esophagus
Pulmonary arteries
Pulmonary
capillary
Alveolus
O
2
O
2
O
2
CO
2
CO
2
CO
2
Pulmonary veins
Conchae
Alveoli
Glottis
Larynx, vocal
cords
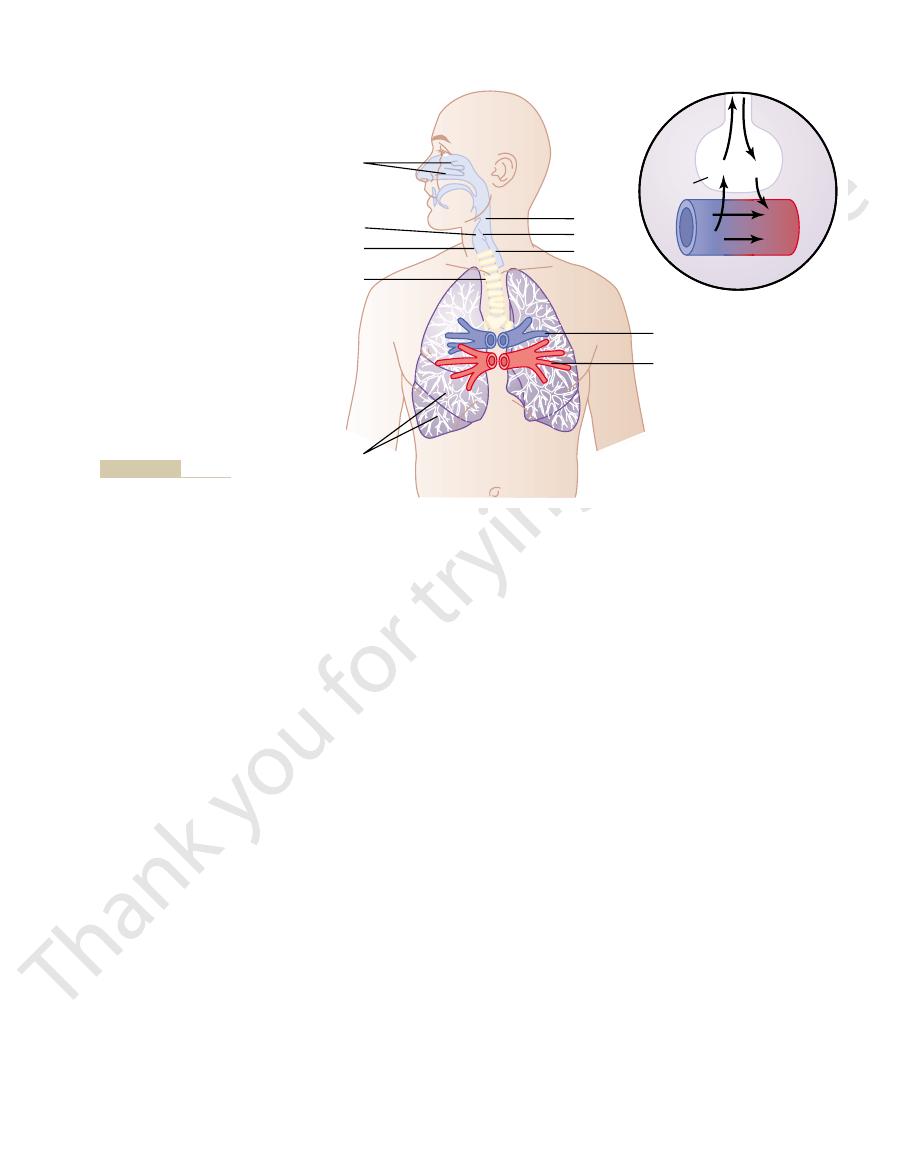
Respiratory passages.
Figure 37–8
uid. But many particles smaller than 0.5
because of settled dust particles. Some of the still
For instance, termi-
Of the remaining particles, many that are between 1
cells.
the nose. This size is smaller than the size of red blood
The nasal turbulence mechanism for removing particles
tinue forward, striking the surfaces of the obstructions,
of travel as rapidly as the air can. Therefore, they con-
and momentum than air, cannot change their direction
The particles suspended in the air, having far more mass
obstructions, it must change its direction of movement.
and the pharyngeal wall. Each time air hits one of these
because they cause turbulence of the air), the septum,
turbinates,
conchae
obstructing vanes: the
That is, the air
ticles. Much more important, though, is the removal
The hairs at the entrance to
trachea. When a person breathes air through a tube
narily, the temperature of the inspired air rises to within
of the upper respiratory passageways. Ordi-
These functions together are called the
beyond the nose; and (3) the air is
8); (2) the air is
square centimeters (see Figure 37
the conchae and septum, a total area of about 160
ties: (1) the air is
As air passes through the nose, three distinct normal
helping to clear the nasal passages of foreign matter.
large amounts of air pass rapidly through the nose, thus
takes place; however, the uvula is depressed, so that
ex is triggered. A
nerve to the medulla, where the re
sageways; the afferent impulses pass in the
of the lower respiratory passages. The initiating stimu-
The sneeze re
The rapidly
tracheal slits.
bronchial
invaginate inward, so that the exploding air actually
ranging from 75 to 100 miles per hour. Importantly, the
Indeed, sometimes this air is expelled at velocities
and the epiglottis suddenly open widely, so that air
much as 100 mm Hg or more. Fourth, the vocal cords
quently, the pressure in the lungs rises rapidly to as
the internal intercostals, also contract forcefully. Conse-
the diaphragm while other expiratory muscles, such as
abdominal muscles contract forcefully, pushing against
tightly to entrap the air within the lungs. Third, the
Second, the epiglottis closes, and the vocal cords shut
First, up to 2.5 liters of air are rapidly inspired.
medulla, causing the following effect.
medulla of the brain. There, an automatic sequence of
gas. Afferent nerve impulses pass from the respiratory
bronchi) are especially sensitive, and the terminal bron-
ex. The larynx
The bronchi and trachea are so sensitive to light touch
either swallowed or coughed to the exterior.
pharynx. Then the mucus and its entrapped particles are
velocity of a few millimeters per minute, toward the
ow slowly, at a
whereas those in the nose beat downward. This contin-
pharynx. That is, the cilia in the lungs beat upward,
by the mechanism explained in Chapter 2, and the direc-
with about 200 cilia on each epithelial cell. These cilia
terminal bronchioles, is lined with ciliated epithelium,
The entire surface of the respiratory passages, both in
following manner.
The mucus itself is removed from the passages in the
cosal glands. In addition to keeping the surfaces moist,
that coats the entire surface. The mucus is secreted
minal bronchioles, are kept moist by a layer of mucus
All the respiratory passages, from the nose to the ter-
Mucus Lining the Respiratory Passageways, and Action of Cilia
the airways.
act directly on the lung tissues to initiate local, non-
dioxide, and some of the acidic elements in smog
smoke, dust, sulfur
The same irritants that cause parasympathetic con-
cially true of the slow reactive substance of anaphylaxis.
obstruction that occurs in allergic asthma; this is espe-
Therefore, they play key roles in causing the airway
reactions, especially those caused by pollen in the air.
slow reactive substance of anaphylaxis.
Two of the most important of these are
480
Unit VII
Respiration
often quite active in causing bronchiolar constriction.
histamine and
Both of these are
released in the lung tissues by mast cells during allergic
strictor reflexes of the airways—
—often
nervous reactions that cause obstructive constriction of
to Clear the Passageways
partly by individual mucous goblet cells in the epithe-
lial lining of the passages and partly by small submu-
the mucus traps small particles out of the inspired air
and keeps most of these from ever reaching the alveoli.
the nose and in the lower passages down as far as the
beat continually at a rate of 10 to 20 times per second
tion of their “power stroke” is always toward the
ual beating causes the coat of mucus to fl
Cough Reflex
that very slight amounts of foreign matter or other
causes of irritation initiate the cough refl
and carina (the point where the trachea divides into the
chioles and even the alveoli are sensitive to corrosive
chemical stimuli such as sulfur dioxide gas or chlorine
passages mainly through the vagus nerves to the
events is triggered by the neuronal circuits of the
under this high pressure in the lungs explodes outward.
strong compression of the lungs collapses the bronchi
and trachea by causing their noncartilaginous parts to
passes through
and
moving air usually carries with it any foreign matter that
is present in the bronchi or trachea.
Sneeze Reflex
flex is very much like the cough reflex,
except that it applies to the nasal passageways instead
lus of the sneeze reflex is irritation in the nasal pas-
fifth cranial
fl
series of reactions similar to those for the cough reflex
Normal Respiratory Functions
of the Nose
respiratory functions are performed by the nasal cavi-
warmed by the extensive surfaces of
–
almost completely humidified even before it passes
partially filtered.
air conditioning
function
1°F of body temperature and to within 2 to 3 per cent
of full saturation with water vapor before it reaches the
directly into the trachea (as through a tracheostomy),
the cooling and especially the drying effect in the lower
lung can lead to serious lung crusting and infection.
Filtration Function of the Nose.
the nostrils are important for filtering out large par-
of particles by turbulent precipitation.
passing through the nasal passageways hits many
(also called
and are entrapped in the mucous coating and trans-
ported by the cilia to the pharynx to be swallowed.
Size of Particles Entrapped in the Respiratory Passages.
from air is so effective that almost no particles larger
than 6 micrometers in diameter enter the lungs through
and 5 micrometers settle in the smaller bronchioles as a
result of gravitational precipitation.
nal bronchiolar disease is common in coal miners
smaller particles (smaller than 1 micrometer in diame-
ter) diffuse against the walls of the alveoli and adhere
to the alveolar fl

tory system. Physiol Rev 79:325, 1999.
Hilaire G, Duron B: Maturation of the mammalian respira-
Curr Opin Crit Care 10:18, 2004.
for acute lung injury/acute respiratory distress syndrome.
Haitsma JJ, Papadakos PJ, Lachmann B: Surfactant therapy
Pulm Pharmacol Ther 15:277, 2002.
Foster WM: Mucociliary transport and cough in humans.
evolution of air breathing. News Physiol Sci 18:151, 2003.
Daniels CB, Orgeig S: Pulmonary surfactant: the key to the
and airway diseases. Pharmacol Ther 98:59, 2003.
Coulson FR, Fryer AD: Muscarinic acetylcholine receptors
Respirology 8:291, 2003.
Carr MJ, Undem BJ: Bronchopulmonary afferent nerves.
blocks the air passages to these resonators.
qualities of these structures. For instance, the function
Again, we are all familiar with the resonating
cavity.
chest
ciated nasal sinuses,
The resonators include the
vocalizations.
They
soft palate.
lips, tongue,
The three major organs of
gurations of the vocal cords shown in Figure 37
Finally, several other sets of small laryngeal muscles
ing them for the more bass sounds.
shapes and masses of the vocal cord edges,
Also, slips of these muscles
thyroid cartilage and, therefore, loosen the vocal cords.
muscles, can pull the arytenoid cartilages toward the
cords lateral to the vocal ligaments, the thyroarytenoid
the cricoid cartilage. Muscles located within the vocal
the arytenoid cartilages, activated by muscles stretching
The vocal cords can be stretched by either forward
cricoid cartilage.
9, the
not shown in Figure 37
The thyroid cartilage and the arytenoid
tenoid cartilages.
Posteriorly, the vocal
s apple.
thyroid cartilage,
This is attached anteriorly to
folds after removal of the mucous epithelial lining.
Figure 37
and by the mass of their edges.
mainly by the degree of stretch of the cords, but also by
cause vibration. The pitch of the vibration is determined
allow easy passage of air. During phonation, the cords
During normal breathing, the cords are wide open to
when looking into the glottis with a laryngoscope.
Figure 37
itself.
toward the center of the glottis; they are stretched and
The
vocal cords.
vocal folds,
cially adapted to act as a vibrator. The vibrating element
, is espe-
The larynx, shown in Figure 37
larynx, and (2)
functions: (1)
nasal cavities. Speech is composed of two mechanical
respiratory control centers of the brain; and (3) the
cerebral cortex, which are discussed in Chapter 57; (2)
Vocalization
permanent debility.
brous tissue in the alveolar septa, leading to
the lung lymphatics. An excess of particles can cause
explained in Chapter 33, and others are carried away by
alveolar macrophages,
remaining suspended and expelled in the expired air.
the alveoli by the diffusion process, with the balance
Unfortunately, up to one third of them do precipitate in
particles of cigarette smoke are about 0.3 micrometer.
olar air and are expelled by expiration. For instance, the
Pulmonary Ventilation
Chapter 37
481
micrometer in diameter remain suspended in the alve-
Almost none of these particles are precipitated in the
respiratory passageways before they reach the alveoli.
Many of the particles that become entrapped in
the alveoli are removed by
as
growth of fi
Speech involves not only the respiratory system but
also (1) specific speech nervous control centers in the
articulation and resonance structures of the mouth and
phonation, which is achieved by the
articulation, which is achieved by the
structures of the mouth.
Phonation.
–9A
is the
commonly called the
vocal cords protrude from the lateral walls of the larynx
positioned by several specific muscles of the larynx
–9B shows the vocal cords as they are seen
move together so that passage of air between them will
how tightly the cords are approximated to one another
–9A shows a dissected view of the vocal
Immediately inside each cord is a strong elastic ligament
called the vocal ligament.
the large
which is the cartilage that
projects forward from the anterior surface of the neck
and is called the “Adam’
”
ligament is attached to the vocal processes of two ary-
cartilages articulate from below with another cartilage
–
rotation of the thyroid cartilage or posterior rotation of
from the thyroid cartilage and arytenoid cartilages to
within the vocal cords can
change the
sharpening them to emit high-pitched sounds and blunt-
lie between the arytenoid cartilages and the cricoid car-
tilage and can rotate these cartilages inward or outward
or pull their bases together or apart to give the various
confi
–9B.
Articulation and Resonance.
articulation are the
and
need not be discussed in detail because we are all famil-
iar with their movements during speech and other
mouth, the nose and asso-
the pharynx, and even the
of the nasal resonators is demonstrated by the change
in voice quality when a person has a severe cold that
References
Vocal
Transverse
Thyroarytenoid
muscle
Full
abduction
Gentle
abduction
Stage
whisper
Phonation
Intermediate position–
loud whisper
Lateral
cricoarytenoid
muscle
Posterior
cricoarytenoid
muscle
arytenoid
muscle
Thyroid
cartilage
Arytenoid
cartilage
ligament
A
B
Its Disorders, 4th ed. Philadel-
from Greene MC: The Voice and
vocal cords during different
Laryngeal function in phona-
Anatomy of the larynx.
Figure 37–9
A,
B,
tion, showing the positions of the
types of phonation. (Modified
phia: JB Lippincott, 1980.)
N Engl J Med 349:882, 2003.
Zeitels SM, Healy GB: Laryngology and phonosurgery.
defense. J Clin Invest 111:1453, 2003.
Wright JR: Pulmonary surfactant: a front line of lung host
drug therapy. Curr Opin Pharmacol 2:256, 2002.
Widdicombe J: Neuroregulation of cough: implications for
News Physiol Sci 17:47, 2002.
West JB: Why doesn
versity Press, 1996.
West JB: Respiratory Physiology. New York: Oxford Uni-
Birkhauser Verlag, 1998.
Uhlig S, Taylor AE: Methods in Pulmonary Research. Basel:
rapidly adapting receptors. Respir Physiol 125:33, 2001.
Ambrogio G, Widdicombe J: Re
Sci 19:55, 2004.
complexity: implications for gas exchange. News Physiol
Powell FL, Hopkins SR: Comparative physiology of lung
J Anat 201:319, 2002.
ow in mammals.
Paton JF, Dutschmann M: Central control of upper airway
muscle function and training. Sports Med 34:117, 2004.
obstructive pulmonary disease: the role of respiratory
McConnell AK, Romer LM: Dyspnoea in health and
techniques for lung volume reduction. Chest 125:777,
eld RA: New and emerging minimally invasive
Cell Mol Physiol 282:L345, 2002.
and other regulators. Am J Physiol Lung
Massaro D, Massaro GD: Pulmonary alveoli: formation, the
Lung Cell Mol Physiol 275:L1, 1998.
surfactant protein D in health and disease. Am J Physiol
Mason RJ, Greene K, Voelker DR: Surfactant protein A and
Rev 84:385, 2004.
uid exchange. Physiol
Lai-Fook SJ: Pleural mechanics and
482
Unit VII
Respiration
fl
“call for oxygen,”
Maxfi
2004.
resistance regulating respiratory airfl
Sant’
flexes from airway
’t the elephant have a pleural space?
