
tory muscles, mainly the diaphragm, is not an instantaneous burst of action
The nervous signal that is transmitted to the inspira-
Inspiratory “Ramp” Signal.
the medulla as well, and is responsible for the basic rhythm of respiration.
neurons is present in the human being, located entirely within the medulla; it
fore, most respiratory physiologists believe that some similar network of
mechanism repeats itself, continuing throughout the life of the animal. There-
a second set, which in turn inhibits the first. Then, after a period of time, the
basic cause of these repetitive discharges is unknown. In primitive animals,
The
inspiratory neuronal action potentials.
and the brain stem transected both above and below the medulla, this group of
of respiration is generated mainly in the dorsal respiratory group of neurons.
The basic rhythm
Rhythmical Inspiratory Discharges from the Dorsal Respiratory Group.
receptors in the lungs.
from (1) peripheral chemoreceptors, (2) baroreceptors, and (3) several types of
sopharyngeal nerves, which transmit sensory signals into the respiratory center
medulla also play important roles in respiratory control. The nucleus of the
tarius,
medulla. Most of its neurons are located within the
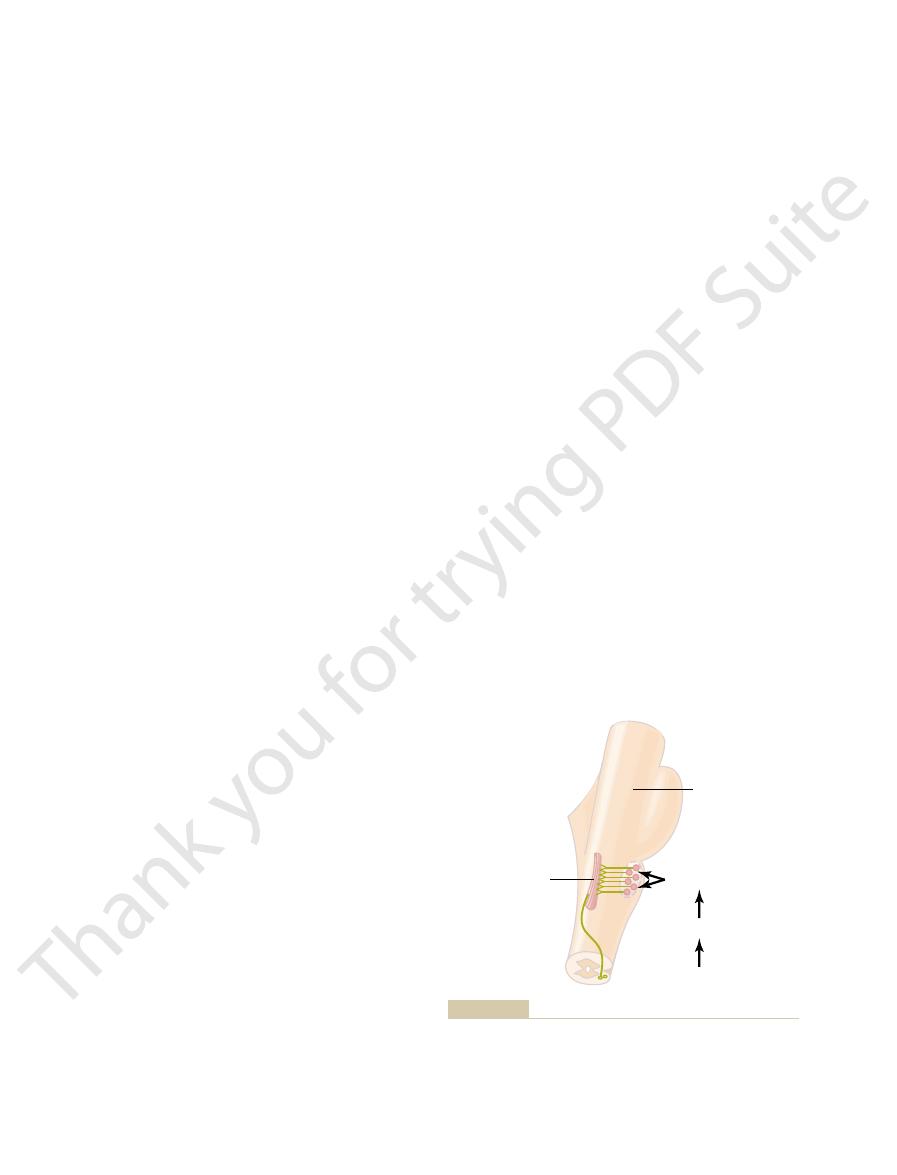
The dorsal respiratory group of neurons extends most of the length of the
of Inspiration and of Respiratory Rhythm
fundamental role in the control of respiration. Therefore, let us discuss its func-
and depth of breathing. The dorsal respiratory group of neurons plays the most
located dorsally in the superior portion of the pons, which mainly controls rate
pneumotaxic center,
the medulla, which mainly causes expiration; and (3) the
ventral respiratory group,
inspiration; (2) a
located in the dorsal portion of the medulla, which mainly causes
tory group,
41–1. It is divided into three major collections of neurons: (1) a
and pons of the brain stem, as shown in Figure
The
Respiratory Center
most other types of respiratory stress. This chapter
are hardly altered even during heavy exercise and
The nervous system normally adjusts the rate of
C
H
A
P
T
E
R
4
1
514
Regulation of Respiration
alveolar ventilation almost exactly to the demands
of the body so that the oxygen pressure (Po
2
) and
carbon dioxide pressure (Pco
2
) in the arterial blood
describes the function of this neurogenic system for
regulation of respiration.
respiratory center is composed of several groups of neurons located bilat-
erally in the medulla oblongata
dorsal respira-
located in the ventrolateral part of
tion first.
Dorsal Respiratory Group of Neurons—Its Control
nucleus of the tractus soli-
although additional neurons in the adjacent reticular substance of the
tractus solitarius is the sensory termination of both the vagal and the glos-
Even when all the peripheral nerves entering the medulla have been sectioned
neurons still emits repetitive bursts of
neural networks have been found in which activity of one set of neurons excites
probably involves not only the dorsal respiratory group but adjacent areas of

brain stem, sensory nerve signals from the lungs also
during heavy exercise.
pulmonary ventilation are required, especially
Thus, this area operates more or less as an
expiration. They are especially important in
stimulation of others causes expiration. Therefore,
the ventral group causes inspiration, whereas
4. Electrical stimulation of a few of the neurons in
area. As a consequence, the ventral respiratory
normal, respiratory signals spill over into the
3. When the respiratory drive for increased
2. There is no evidence that the ventral respiratory
recoil of the lungs and thoracic cage.
the diaphragm, and expiration results from elastic
respiration. Therefore, normal quiet breathing is
1. The neurons of the ventral respiratory group
caudally. The function of this
ventral respiratory group of neurons,
of neurons, is the
Located in each side of the medulla, about 5 millime-
Functions in Both
Ventral Respiratory Group of
minute.
breaths per minute, whereas a weak pneumotaxic
period of each respiration. A strong pneumotaxic
increasing the rate of breathing, because limitation
to limit inspiration. This has a secondary effect of
The function of the pneumotaxic center is primarily
excess of air.
or more seconds, thus filling the lungs with a great
taxic signal is weak, inspiration might continue for 5
thus filling the lungs only slightly; when the pneumo-
strong, inspiration might last for as little as 0.5 second,
of the lung cycle. When the pneumotaxic signal is
ramp, thus controlling the duration of the filling phase
is to control the “switch-off” point of the inspiratory
the inspiratory area. The primary effect of this center
of the upper pons, transmits signals to
parabrachialis
pneumotaxic center,
Duration of Inspiration and Increases
A Pneumotaxic Center Limits the
expiration. Thus, the frequency of respiration is
of inspiration. This also shortens the duration of
earlier the ramp ceases, the shorter the duration
controlling the rate of respiration; that is, the
This is the usual method for
suddenly ceases.
limiting point at which the ramp
2. Control of the
rapidly.
so that during heavy respiration, the ramp
1. Control of the
are controlled, as follows:
There are two qualities of the inspiratory ramp that
during inspiration, rather than inspiratory gasps.
The obvious advantage of the ramp is that it
ring in between. Thus, the inspiratory signal is a
cycle repeats again and again, with expiration occur-
inspiratory signal begins again for another cycle; this
lungs and the chest wall to cause expiration. Next, the
mately the next 3 seconds, which turns off the excita-
about 2 seconds. Then it ceases abruptly for approxi-
potentials. Instead, in normal respiration, it begins
Chapter 41
Regulation of Respiration
515
weakly and increases steadily in a ramp manner for
tion of the diaphragm and allows elastic recoil of the
ramp
signal.
causes a steady increase in the volume of the lungs
rate of increase of the ramp signal,
increases rapidly and therefore fills the lungs
increased.
the Respiratory Rate
A
located dorsally in the nucleus
of inspiration also shortens expiration and the entire
signal can increase the rate of breathing to 30 to 40
signal may reduce the rate to only 3 to 5 breaths per
Neurons
—
Inspiration and Expiration
ters anterior and lateral to the dorsal respiratory group
found in the nucleus ambiguus rostrally and the
nucleus retroambiguus
neuronal group differs from that of the dorsal respi-
ratory group in several important ways:
remain almost totally inactive during normal quiet
caused only by repetitive inspiratory signals from
the dorsal respiratory group transmitted mainly to
neurons participate in the basic rhythmical
oscillation that controls respiration.
pulmonary ventilation becomes greater than
ventral respiratory neurons from the basic
oscillating mechanism of the dorsal respiratory
area contributes extra respiratory drive as well.
these neurons contribute to both inspiration and
providing the powerful expiratory signals to the
abdominal muscles during very heavy expiration.
overdrive mechanism when high levels of
Lung Inflation Signals Limit
Inspiration—The Hering-Breuer
Inflation Reflex
In addition to the central nervous system respiratory
control mechanisms operating entirely within the
Pneumotaxic center
Fourth ventricle
Dorsal respiratory
group (inspiration)
Vagus and
glossopharyngeal
? Apneustic center
Inhibits
Ventral respiratory
group (expiration
and inspiration)
Respiratory motor
pathways
Organization of the respiratory center.
Figure 41–1
stimulating the neurons in the chemosensitive area, it
Chemosensitive Area
arily by changing the hydrogen ion concentration, as
changes in blood carbon dioxide, even though carbon
barrier. For this reason, changes in hydrogen ion con-
tant direct stimulus for these neurons. However,
especially excited by hydrogen ions; in fact, it is
The sensor neurons in the chemosensitive area are
Hydrogen Ions Is Likely the Primary Stimulus
Excitation of the Chemosensitive Neurons by
other portions of the respiratory center.
hydrogen ion concentration, and it in turn excites the
beneath the ventral surface of the medulla. This area
41–2, is located bilaterally, lying only 0.2 millimeter
shown in Figure
chemosensitive area,
neuronal area, a
hydrogen ion concentration. Instead, an additional
respiratory group, and the pneumotaxic center. It
the dorsal respiratory group of neurons, the ventral
We have dis-
Chemosensitive Area of the Respiratory Center.
Respiratory Center Activity by Carbon
center itself by carbon dioxide and hydrogen ions.
aortic bodies,
chemoreceptors
controlling respiration. Instead, it acts almost entirely
Oxygen, in contrast, does not have a significant
respiratory muscles.
itself, causing greatly increased strength of both the
each of these.
gen ions in the tissues. It is fortunate, therefore, that
concentrations of oxygen, carbon dioxide, and hydro-
The ultimate goal of respiration is to maintain proper
Chemical Control
needs of the body.
increases in pulmonary ventilation. The major purpose
much as 20 times normal, requiring commensurate
during heavy exercise, the rates of oxygen usage and
match the ventilatory needs of the body. For example,
nisms for causing inspiration and expiration, but it is
Up to this point, we have discussed the basic mecha-
Center Activity
Control of Overall Respiratory
liters per breath). Therefore, this reflex appears to be
In human beings, the Hering-Breuer reflex probably
motaxic center.
rate of respiration, as is true for signals from the pneu-
This reflex also increases the
thus stops further inspiration. This is called the
response that “switches off” the inspiratory ramp and
that is, when the lungs become overly inflated, the
overstretched. These signals affect inspiration in much
stretch receptors
help control respiration. Most important, located in
516
Unit VII
Respiration
the muscular portions of the walls of the bronchi and
bronchioles throughout the lungs are
that transmit signals through the vagi into the dorsal
respiratory group of neurons when the lungs become
the same way as signals from the pneumotaxic center;
stretch receptors activate an appropriate feedback
Hering-
Breuer inflation reflex.
is not activated until the tidal volume increases to
more than three times normal (greater than about 1.5
mainly a protective mechanism for preventing excess
lung inflation rather than an important ingredient in
normal control of ventilation.
also important to know how the intensity of the respi-
ratory control signals is increased or decreased to
carbon dioxide formation are often increased to as
of the remainder of this chapter is to discuss this
control of ventilation in accord with the respiratory
of Respiration
respiratory activity is highly responsive to changes in
Excess carbon dioxide or excess hydrogen ions in
the blood mainly act directly on the respiratory center
inspiratory and the expiratory motor signals to the
direct effect on the respiratory center of the brain in
on peripheral
located in the carotid
and
and these in turn transmit appropri-
ate nervous signals to the respiratory center for
control of respiration.
Let us discuss first the stimulation of the respiratory
Direct Chemical Control of
Dioxide and Hydrogen Ions
cussed mainly three areas of the respiratory center:
is believed that none of these is affected directly by
changes in blood carbon dioxide concentration or
is highly sensitive to changes in either blood Pco
2
or
believed that hydrogen ions may be the only impor-
hydrogen ions do not easily cross the blood-brain
centration in the blood have considerably less effect
in stimulating the chemosensitive neurons than do
dioxide is believed to stimulate these neurons second-
explained in the following section.
Carbon Dioxide Stimulates the
Although carbon dioxide has little direct effect in
Chemosensitive
area
Inspiratory area
H
+
+
HCO
3
-
H
2
CO
3
CO
2
+
H
2
O
but carbon dioxide in the fluid gives rise to most of the hydrogen
Note also that hydrogen ions stimulate the chemosensitive area,
a fraction of a millimeter beneath the ventral medullary surface.
chemosensitive area
area by signals from the
brain stem inspiratory
Figure 41–2
Stimulation of the
located bilaterally in the medulla, lying only
ions.
70 mm Hg, as explained in the next section.
blood oxygen falls too low, mainly below a P
piratory center; this mechanism responds when the
the peripheral chemoreceptors, outside the brain res-
get into trouble for lack of oxygen, the body has a
Yet, for those special conditions in which the tissues
dioxide the major controller of respiration, not
inversely with the rate of pulmonary ventilation; thus,
more times normal. This is not true for carbon dioxide,
under special conditions, adequate delivery of oxygen
up to a value as high as 1000 mm Hg. Therefore, except
We learned in Chapter 40 that the hemoglobin-
chemoreceptors, as explained in the next section).
an indirect effect, acting through the peripheral
Respiratory Center
Unimportance of Oxygen for Control of the
ration. By contrast, the change in respiration in the
75 mm Hg. This demonstrates the tremendous effect
tration) on alveolar ventilation. Note especially the
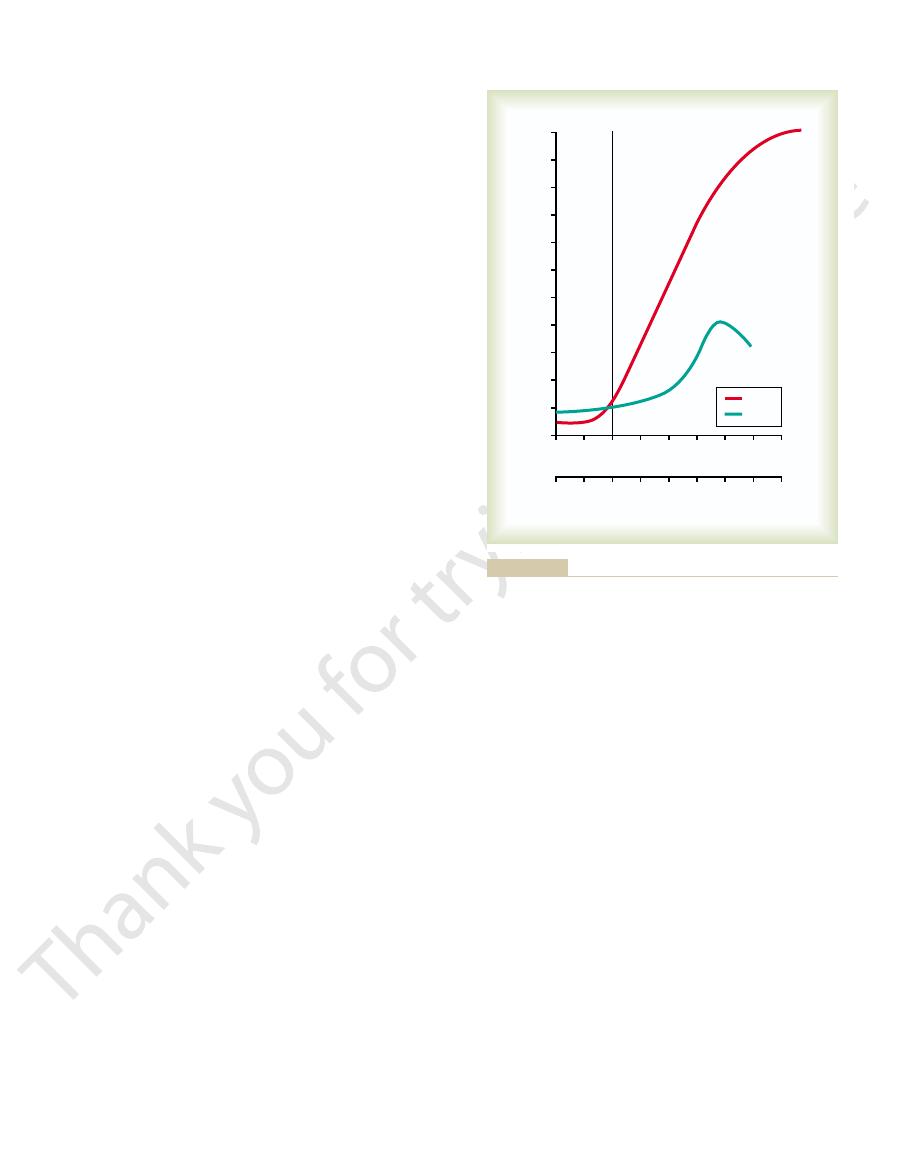
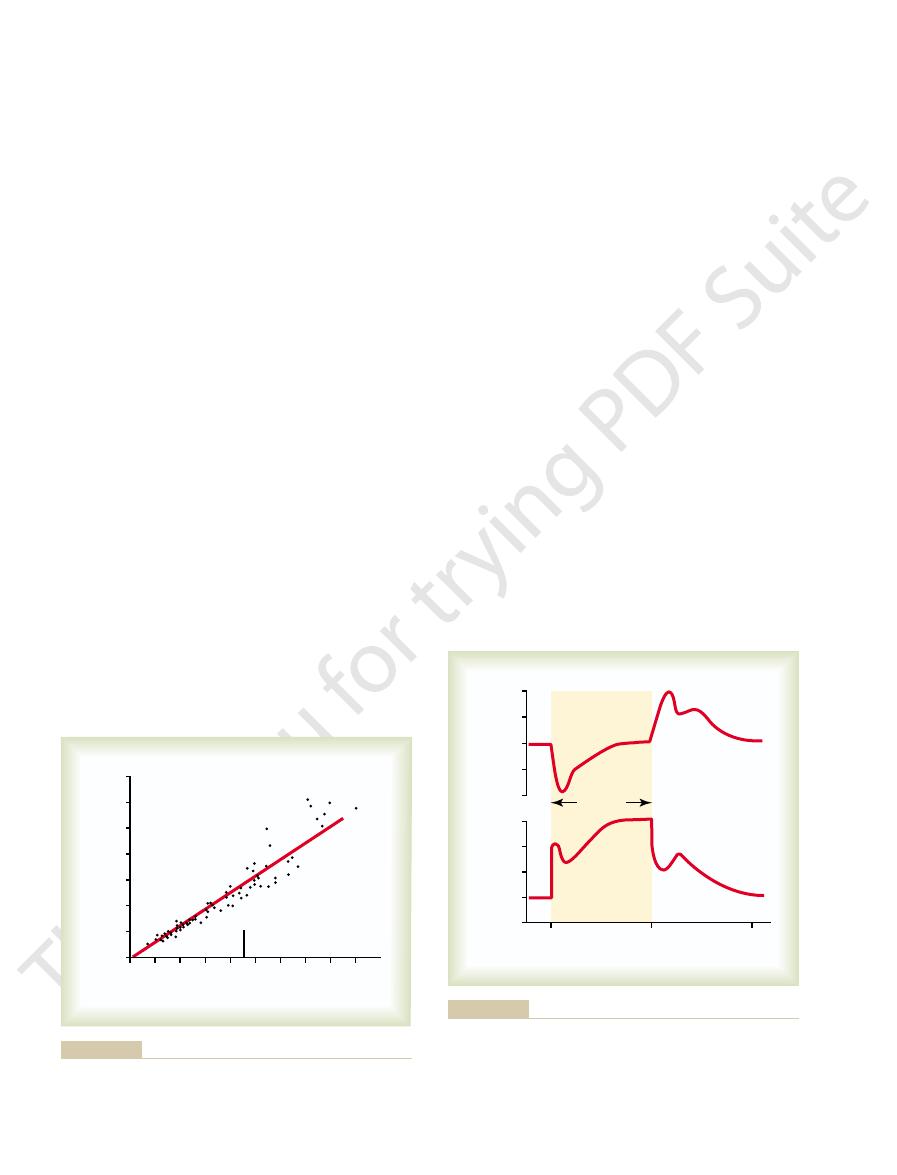
Figure 41–3 shows quantitatively the approximate
Alveolar Ventilation
and Hydrogen Ion Concentration on
Quantitative Effects of Blood P
chronic
normal. A change in blood carbon dioxide concentra-
as well, thus reducing the hydrogen ions back to near
over a period of hours, the bicarbonate ions also
reduce their concentrations. But even more important,
increasing the blood bicarbonate, which binds with the
hydrogen concentration. The kidneys achieve this by
about one fifth the initial effect. Part of this decline
ually declines over the next 1 to 2 days, decreasing to
blood carbon dioxide first increases, but then it grad-
Decreased Stimulatory Effect of Carbon Dioxide After the First
quantitatively.
carbon dioxide, a fact that we subsequently discuss
tration increases. For this reason, respiratory center
Thus, paradoxically, more hydrogen ions are released
ately reacts with the water to form new hydrogen ions.
fluid. In both these fluids, the carbon dioxide immedi-
increases, so does the P
as if the barrier did not exist. Consequently, whenever
brain barrier is not very permeable to hydrogen ions,
do blood hydrogen ions? The answer is that the blood-
Why does blood carbon dioxide have a more potent
in Figure 41–2.
tory effect on respiration. These reactions are shown
does have a potent indirect effect. It does this by react-
Chapter 41
Regulation of Respiration
517
ing with the water of the tissues to form carbonic acid,
which dissociates into hydrogen and bicarbonate ions;
the hydrogen ions then have a potent direct stimula-
effect in stimulating the chemosensitive neurons than
but carbon dioxide passes through this barrier almost
the blood Pco
2
co
2
of both the
interstitial fluid of the medulla and the cerebrospinal
into the respiratory chemosensitive sensory area of the
medulla when the blood carbon dioxide concentration
increases than when the blood hydrogen ion concen-
activity is increased very strongly by changes in blood
1 to 2 Days.
Excitation of the respiratory center by
carbon dioxide is great the first few hours after the
results from renal readjustment of the hydrogen ion
concentration in the circulating blood back toward
normal after the carbon dioxide first increases the
hydrogen ions in the blood and cerebrospinal fluid to
slowly diffuse through the blood-brain and blood–
cerebrospinal fluid barriers and combine directly with
the hydrogen ions adjacent to the respiratory neurons
tion therefore has a potent acute effect on controlling
respiratory drive but only a weak
effect after
a few days’ adaptation.
CO
2
effects of blood Pco
2
and blood pH (which is an
inverse logarithmic measure of hydrogen ion concen-
very marked increase in ventilation caused by an
increase in Pco
2
in the normal range between 35 and
that carbon dioxide changes have in controlling respi-
normal blood pH range between 7.3 and 7.5 is less than
one tenth as great.
Changes in oxygen concentration have virtually no
direct effect on the respiratory center itself to alter
respiratory drive (although oxygen changes do have
oxygen buffer system delivers almost exactly normal
amounts of oxygen to the tissues even when the pul-
monary Po
2
changes from a value as low as 60 mm Hg
can occur despite changes in lung ventilation ranging
from slightly below one half normal to as high as 20 or
because both the blood and tissue Pco
2
changes
the processes of animal evolution have made carbon
oxygen.
special mechanism for respiratory control located in
o
2
of
7.6
7.5
7.4
7.3
7.2
7.1
7.0
6.9
80
90
100
20
30
40
50
60
70
P
CO
2
pH
Alveolar ventilation (basal rate = 1)
Normal
11
10
9
8
7
6
5
4
3
2
1
0
pH
P
CO
2
(mm Hg)
(increased hydrogen ion concentration) on the rate of alveolar
and decreased arterial pH
Effects of increased arterial blood P
Figure 41–3
CO
2
ventilation.
bodies is still unknown. However, these bodies have
The exact means by which low P
Oxygen Deficiency.
response to carbon dioxide at the onset of exercise.
ulation, so that the peripheral chemoreceptors might
peripheral and central effects of carbon dioxide: the
considered. Yet there is one difference between the
seven times as powerful) that, for practical purposes,
indirectly increases respiratory activity. However, the
also excites the chemoreceptors and, in this way,
Chemoreceptor Activity.
Effect of Carbon Dioxide and Hydrogen Ion Concentration on
saturation with oxygen decreases rapidly.
60 down to 30 mm Hg, a range in which hemoglobin
a carotid body. Note that the impulse rate is particu-
41–5, which shows the effect of different levels of
strongly stimulated. This is demonstrated in Figure
blood falls below normal, the chemoreceptors become
When the oxygen concentration in the arterial
blood, and their P
the chemoreceptors
is virtually zero. This means that
of the bodies themselves each minute. Therefore, the
through these bodies is extreme, 20 times the weight
from the adjacent arterial trunk. Further, blood flow
located along the arch of the aorta; their afferent
respiratory area of the medulla. The
afferent nerve fibers pass through Hering’s nerves to
bifurcations of the common carotid arteries. Their
The
ies of the thoracic and abdominal regions.
shown in the lower part of Figure 41–4, and a very few
aortic bodies,
However, a few are also in the
bodies.
regulate respiratory activity.
concentrations. The chemoreceptors transmit nervous
in the blood, although they also respond to a lesser
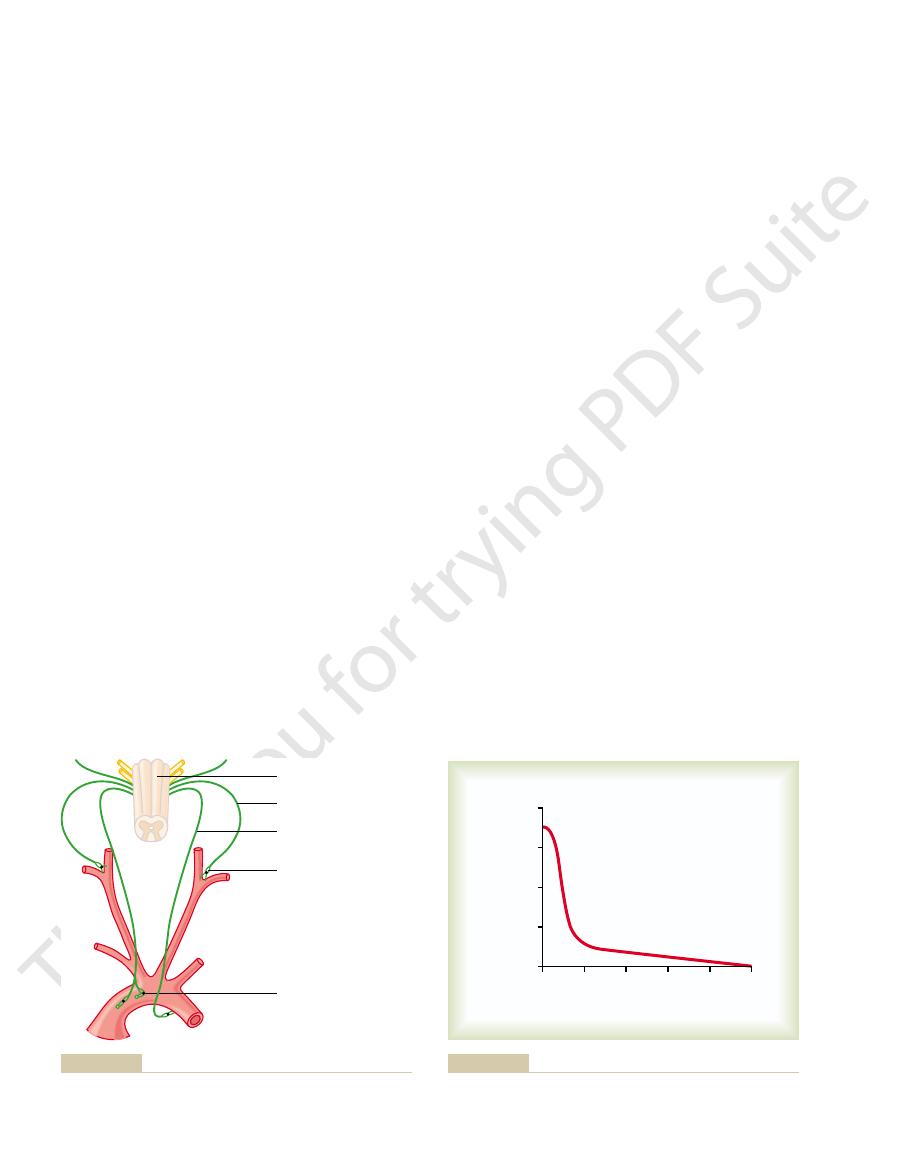
located in several areas outside the brain. They are
chemoreceptors,
nervous chemical receptors, called
shown in Figure 41–4. Special
chemoreceptor system,
able for controlling respiration. This is the
piratory center itself, still another mechanism is avail-
Oxygen in Respiratory Control
Respiratory Activity—Role of
System for Control of
Peripheral Chemoreceptor
518
Unit VII
Respiration
In addition to control of respiratory activity by the res-
peripheral
are
especially important for detecting changes in oxygen
extent to changes in carbon dioxide and hydrogen ion
signals to the respiratory center in the brain to help
Most of the chemoreceptors are in the carotid
are located elsewhere in association with other arter-
carotid bodies are located bilaterally in the
the glossopharyngeal nerves and then to the dorsal
aortic bodies are
nerve fibers pass through the vagi, also to the dorsal
medullary respiratory area.
Each of the chemoreceptor bodies receives its own
special blood supply through a minute artery directly
percentage of oxygen removed from the flowing blood
are exposed at all times to arterial blood, not venous
o
2
s are arterial Po
2
s.
Stimulation of the Chemoreceptors by Decreased Arterial
Oxygen.
arte-
rial Po
2
on the rate of nerve impulse transmission from
larly sensitive to changes in arterial Po
2
in the range of
An increase in either carbon
dioxide concentration or hydrogen ion concentration
direct effects of both these factors in the respiratory
center itself are so much more powerful than their
effects mediated through the chemoreceptors (about
the indirect effects of carbon dioxide and hydrogen
ions through the chemoreceptors do not need to be
stimulation by way of the peripheral chemoreceptors
occurs as much as five times as rapidly as central stim-
be especially important in increasing the rapidity of
Basic Mechanism of Stimulation of the Chemoreceptors by
o
2
excites the nerve endings in the carotid and aortic
Aortic bodies
Medulla
Glossopharyngeal nerve
Vagus nerve
Carotid body
and aortic bodies.
Respiratory control by peripheral chemoreceptors in the carotid
Figure 41–4
0
100
200
300
400
500
Carotid body nerve
impulses per second
0
200
400
600
800
Arterial P
O
2
(mm Hg)
on impulse rate from the carotid body of a
Effect of arterial P
Figure 41–5
O
2
cat.
changed from lower to higher levels. Thus, this
100 mm Hg. For each of these curves, the P
—40 mm Hg, 50 mm Hg, 60 mm Hg, and
These curves were recorded at different levels of
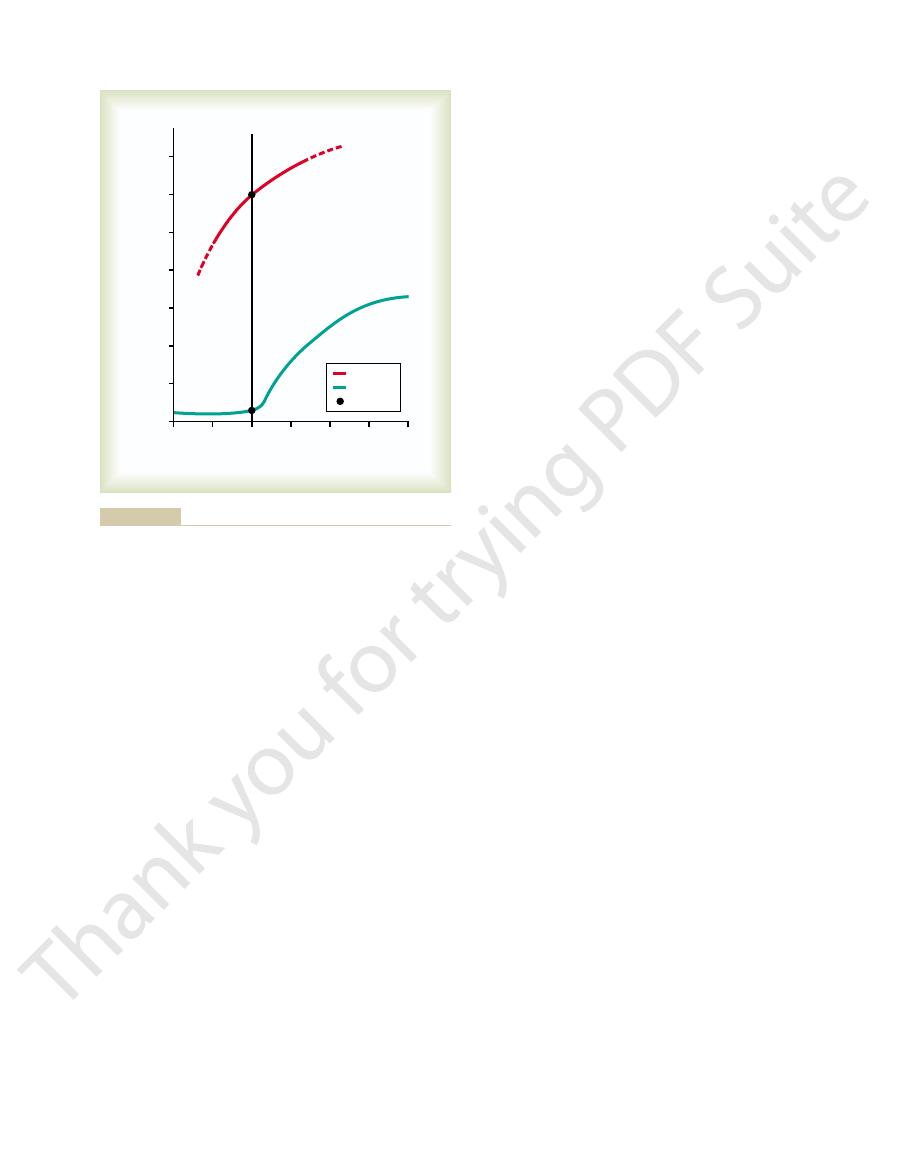
this diagram, first observe the four red curves.
together—affect alveolar ventilation. To understand
, and pH—
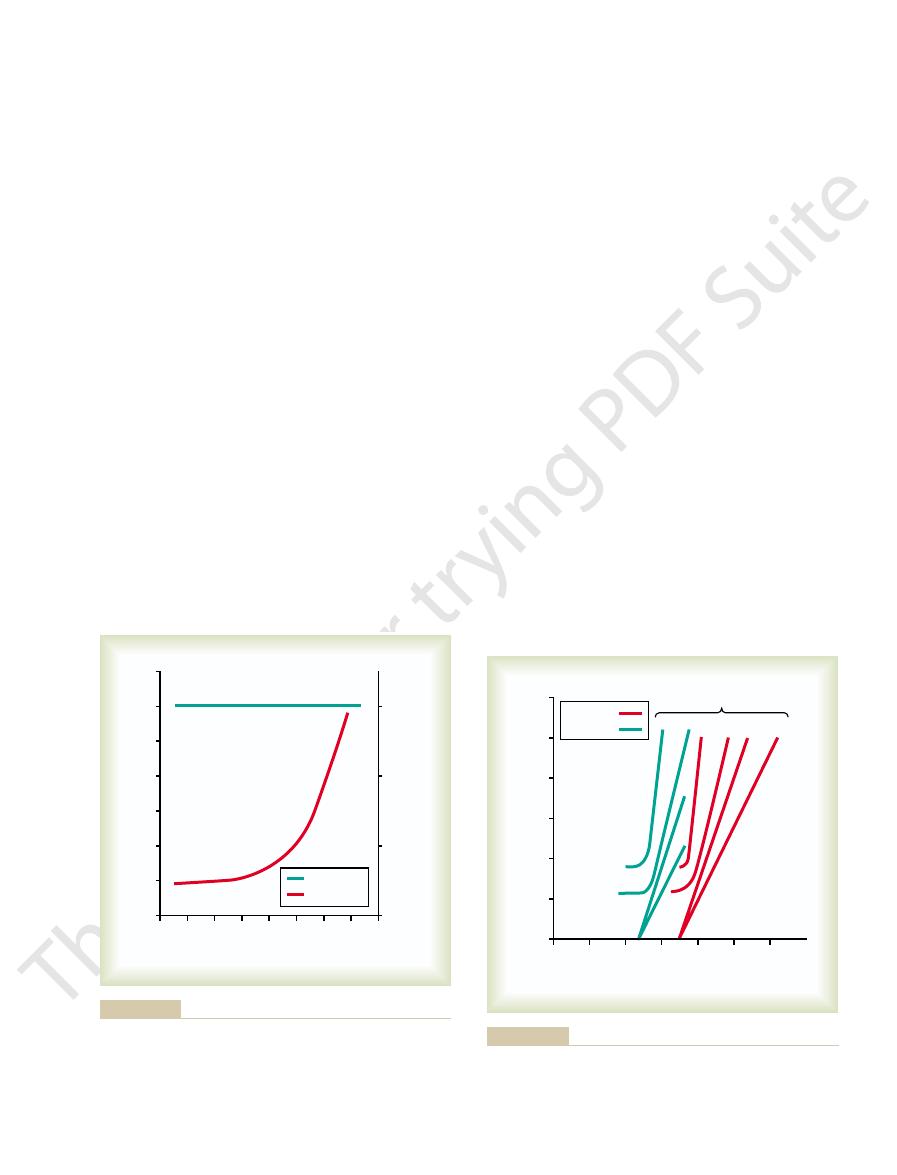
Figure 41–7 gives a quick overview of the manner in
on Alveolar Ventilation
, pH, and
Composite Effects of P
mountain climber.
to 500 per cent after 2 to 3 days of low oxygen; this
oxygen, the alveolar ventilation often increases 400
conditions. Instead of the 70 per cent increase in ven-
an increase in respiration fails to occur, and low
and hydrogen ions. Therefore, the excess ventilatory
days, the respiratory center in the brain stem loses
The reason for acclimatization is that, within 2 to 3
concentrations than when they ascend rapidly. This is
period of hours, they breathe much more deeply and
a mountain slowly, over a period of days rather than a
Respiration Even More—The Phenomenon
Chronic Breathing of Low Oxygen Stimulates
process quite strongly.
tions, low arterial P
s. Under these condi-
falls to 60 mm Hg and can increase as
100 mm Hg, ventilation approximately doubles when
greater than 100 mm Hg. But at pressures lower than
chemoreceptors is active. The figure shows almost no
levels. In other words, in this figure, only the ventila-
Figure 41–6 shows the effect of low arterial P
Remain Normal
Dioxide and Hydrogen Ion Concentrations
Alveolar Ventilation When Arterial Carbon
Effect of Low Arterial P
chemoreceptors and then stimulate the nerve endings.
with the nerve endings. Some investigators have sug-
glomus cells,
multiple highly characteristic glandular-like cells,
Chapter 41
Regulation of Respiration
519
called
that synapse directly or indirectly
gested that these glomus cells might function as the
But other studies suggest that the nerve endings them-
selves are directly sensitive to the low Po
2
.
O
2
to Stimulate
o
2
on
alveolar ventilation when the Pco
2
and the hydrogen
ion concentration are kept constant at their normal
tory drive due to the effect of low oxygen on the
effect on ventilation as long as the arterial Po
2
remains
the arterial Po
2
much as fivefold at very low Po
2
o
2
obviously drives the ventilatory
of “Acclimatization”
Mountain climbers have found that when they ascend
therefore can withstand far lower atmospheric oxygen
called acclimatization.
about four fifths of its sensitivity to changes in Pco
2
blow-off of carbon dioxide that normally would inhibit
oxygen can drive the respiratory system to a much
higher level of alveolar ventilation than under acute
tilation that might occur after acute exposure to low
helps immensely in supplying additional oxygen to the
CO
2
P
O
2
which the chemical factors Po
2
, Pco
2
arterial Po
2
co
2
was
Ventilation
140 120 100
80
60
40
20
0
160
Alveolar ventilation (normal = 1)
0
1
2
3
4
5
6
7
0
20
30
40
Arterial P
O
2
(mm Hg)
Arterial P
CO
2
(mm Hg)
P
CO
2
at a constant level during the measurements of this study; pH also
to 20 mm Hg. The upper line shows that the arterial P
decreases from the normal level of 100 mm Hg
on alveolar ventilation, showing a sixfold increase in ven-
The lower curve demonstrates the effect of different levels of arte-
Figure 41–6
rial P
O
2
tilation as the P
O
2
CO
2
was kept
was kept constant.
20
30
40
50
60
40
50 60
100
0
10
40
pH = 7.4
pH = 7.3
50
60
100
P
O
2
(mm Hg)
Alveolar ventilation (L/min)
0
10
20
30
40
50
60
Alveolar P
CO
2
(mm Hg)
DJC, Lloyd BB: The Regulation of Human Respiration. Oxford:
and pH on alveolar ventilation. (Drawn from data in Cunningham
Composite diagram showing the interrelated effects of P
Figure 41–7
CO
2
, P
O
2
,
Blackwell Scientific Publications, 1963.)
. In fact, this
cise, the alveolar ventilation increases instantaneously,
. Note that at the onset of exer-
This is demonstrated in Figure 41–9, which shows in
tions of the body fluids as nearly normal as possible.
oxygen, carbon dioxide, and hydrogen ion concentra-
are either too strong or too weak. Then chemical
ally, however, the nervous respiratory control signals
cise and to blow off extra carbon dioxide. Occasion-
person exercises, direct nervous signals presumably
When a
Interrelation Between Chemical Factors and Nervous: Factors
chemicals have had time to change. It is likely that
diately on initiation of the exercise, before any blood
Actually, when a person begins to exercise, a large
taneous increase in arterial pressure.
the brain stem to excite the respiratory center. This is
motor impulses to the exercising muscles, is believed
seems to be predominant. The brain, on transmitting
intense ventilation during exercise? At least one effect
Therefore, the question must be asked: What causes
significantly during exercise, so that none of them
pH, and P
questionable, because measurements of arterial P
ions, plus a decrease in blood oxygen. However, this is
tilation during exercise, one is tempted to ascribe this
, and pH remain
The arterial P
as illustrated in Figure 41–8, in the healthy athlete,
dioxide formation can increase as much as 20-fold.Yet,
In strenuous exercise, oxygen consumption and carbon
During Exercise
, and arterial pH.
, alveolar P
Thus, using this diagram, one can predict the level of
at higher pHs and displaced to the left at lower pHs.
on ventilation at two different pH values. Still
measured at a pH of 7.3. We now have two families of
measured at a blood pH of 7.4; the green curves were
Now observe the green curves. The red curves were
“family” of red curves represents the combined effects
520
Unit VII
Respiration
of alveolar Pco
2
and Po
2
on ventilation.
curves representing the combined effects of Pco
2
and
Po
2
other families of curves would be displaced to the right
alveolar ventilation for most combinations of alveolar
Pco
2
o
2
Regulation of Respiration
alveolar ventilation ordinarily increases almost exactly
in step with the increased level of oxygen metabolism.
o
2
, Pco
2
almost exactly
normal.
In trying to analyze what causes the increased ven-
to increases in blood carbon dioxide and hydrogen
co
2
,
o
2
show that none of these values changes
becomes abnormal enough to stimulate respiration.
to transmit at the same time collateral impulses into
analogous to the stimulation of the vasomotor center
of the brain stem during exercise that causes a simul-
share of the total increase in ventilation begins imme-
most of the increase in respiration results from neuro-
genic signals transmitted directly into the brain stem
respiratory center at the same time that signals go to
the body muscles to cause muscle contraction.
in the Control of Respiration During Exercise.
stimulate the respiratory center almost the proper
amount to supply the extra oxygen required for exer-
factors play a significant role in bringing about the
final adjustment of respiration required to keep the
the lower curve changes in alveolar ventilation during
a 1-minute period of exercise and in the upper curve
changes in arterial Pco
2
without an initial increase in arterial Pco
2
110
2.0
3.0
4.0
0
1.0
Moderate
exercise
Severe
exercise
Total ventilation (L/min)
0
20
40
60
80
100
120
O
2
consumption (L/min)
(From Gray JS: Pulmonary Ventilation and Its Physiological Regu-
Effect of exercise on oxygen consumption and ventilatory rate.
Figure 41–8
lation. Springfield, Ill: Charles C Thomas, 1950.)
0
1
2
Arterial P
CO
2
(mm Hg)
36
Exercise
38
40
42
44
Minutes
Alveolar ventilation
(L/min)
2
6
10
14
18
ventilation in dogs during active exercise. J Appl Physiol 33:778,
in dogs in Bainton CR: Effect of speed vs grade and shivering on
mination of exercise. (Extrapolated to the human being from data
during a 1-minute period of exercise and also after ter-
and arterial P
Figure 41–9
Changes in alveolar ventilation (bottom curve)
CO
2
(top curve)
1972.)
piration within a few minutes.
remove some of the fluids of the brain, thus relieving
trated mannitol solution. These solutions osmotically
Occasionally, respiratory depression resulting from
vault and thus partially blocking cerebral blood supply.
object, after which the damaged brain tissues swell,
instance, the head might be struck against some solid
brain edema resulting from brain concussion. For
The activity of the respiratory
the J receptors is not clear, their excitation may give the
congestive heart failure. Although the functional role of
name “J receptors.” They are stimulated especially when
coughing and sneezing, as discussed in Chapter 39. They
that are stimulated by many incidents. These cause
the trachea, bronchi, and bronchioles is supplied with
The epithelium of
Effect of Irritant Receptors in the Airways.
, pH, and P
time, respiration can be controlled voluntarily and that
ration. However, we all know that for short periods of
Thus far, we have dis-
Voluntary Control of Respiration.
Affect Respiration
learned response.
the cerebral cortex is involved in this learning, because
normal level. Also, there is reason to believe that even
at its
That is, with repeated periods of exercise, the brain
response.
in Figure 41–10, is at least partly a
ventilatory response curve during exercise, as shown
ments suggest that the brain’s ability to shift the
Possibility That the Neurogenic Factor for Control of Ventila-
less than 40 mm Hg.
greater than 40 mm Hg and a depres-
40 mm Hg, it has an extra stimulatory effect on venti-
Figure 41–10 also shows that if, during exercise, the
near its normal value. The upper curve of
the rate of carbon dioxide release, thus keeping arte-
upward direction, so that ventilation almost matches
is at the normal level of 40 mm Hg. In other words, the
exercising state. Note in both instances that the P
cise. The points indicated on the two curves show the
cising. The upper curve shows the approximate shift of
ventilation when the body is at rest—that is, not exer-
quantitatively. The lower curve of this figure shows the
during exercise in still another way, this time more
Figure 41–10 summarizes the control of respiration
of exercise in the figure.
tinues, as shown toward the end of the 1-minute period
increased rate of ventilation, and the arterial P
is needed. However, after about 30 to 40 seconds,
cise, causing extra alveolar ventilation even before it
tory” stimulation of respiration at the onset of exer-
carbon dioxide is that the brain provides an “anticipa-
as shown in the figure. The presumed reason that the
Chapter 41
Regulation of Respiration
521
increase in ventilation is usually great enough so that
at first it actually decreases arterial Pco
2
below normal,
ventilation forges ahead of the buildup of blood
the amount of carbon dioxide released into the blood
from the active muscles approximately matches the
co
2
returns essentially to normal even as the exercise con-
effect of different levels of arterial Pco
2
on alveolar
this ventilatory curve caused by neurogenic drive from
the respiratory center that occurs during heavy exer-
arterial Pco
2
first in the resting state and then in the
co
2
neurogenic factor shifts the curve about 20-fold in the
rial Pco
2
arterial Pco
2
does change from its normal value of
lation at a Pco
2
sant effect at a Pco
2
tion During Exercise Is a Learned Response.
Many experi-
learned
becomes progressively more able to provide the
proper signals required to keep the blood Pco
2
experiments that block only the cortex also block the
Other Factors That
cussed the involuntary system for the control of respi-
one can hyperventilate or hypoventilate to such an
extent that serious derangements in Pco
2
o
2
can occur in the blood.
sensory nerve endings called pulmonary irritant recep-
tors
may also cause bronchial constriction in such diseases
as asthma and emphysema.
Function of Lung “J Receptors.”
A few sensory nerve
endings have been described in the alveolar walls in
juxtaposition to the pulmonary capillaries—hence the
the pulmonary capillaries become engorged with blood
or when pulmonary edema occurs in such conditions as
person a feeling of dyspnea.
Effect of Brain Edema.
center may be depressed or even inactivated by acute
compressing the cerebral arteries against the cranial
brain edema can be relieved temporarily by intravenous
injection of hypertonic solutions such as highly concen-
intracranial pressure and sometimes re-establishing res-
60
80
100
20
30
40
50
Exercise
Alveolar ventilation (L/min)
Arterial P
CO
2
(mm Hg)
0
140
120
100
80
60
40
20
Resting
Normal
during heavy exercise.
at the normal level of 40 mm Hg both in the resting state and
factors, is almost exactly the right amount to maintain arterial P
than normal. The shift, believed to be caused by neurogenic
-ventilation response curve to a level much higher
Approximate effect of maximum exercise in an athlete to shift the
Figure 41–10
alveolar P
CO
2
CO
2
adequate airflow. Some individuals have an especially
inspiration. During sleep, these muscles usually relax,
The muscles of the pharynx normally keep this
Airway.
Obstructive Sleep Apnea Is Caused by Blockage of the Upper
impaired central nervous system respiratory drive.
of the upper airways, especially the pharynx, or by
each night. Sleep apneas can be caused by obstruction
are greatly increased, with episodes of apnea lasting for
the frequency and duration
sleep apnea,
ing. Occasional apneas occur during normal sleep, but
The term
occurring.
in the brain, not with the
the respiratory neurons. But the depth of respiration
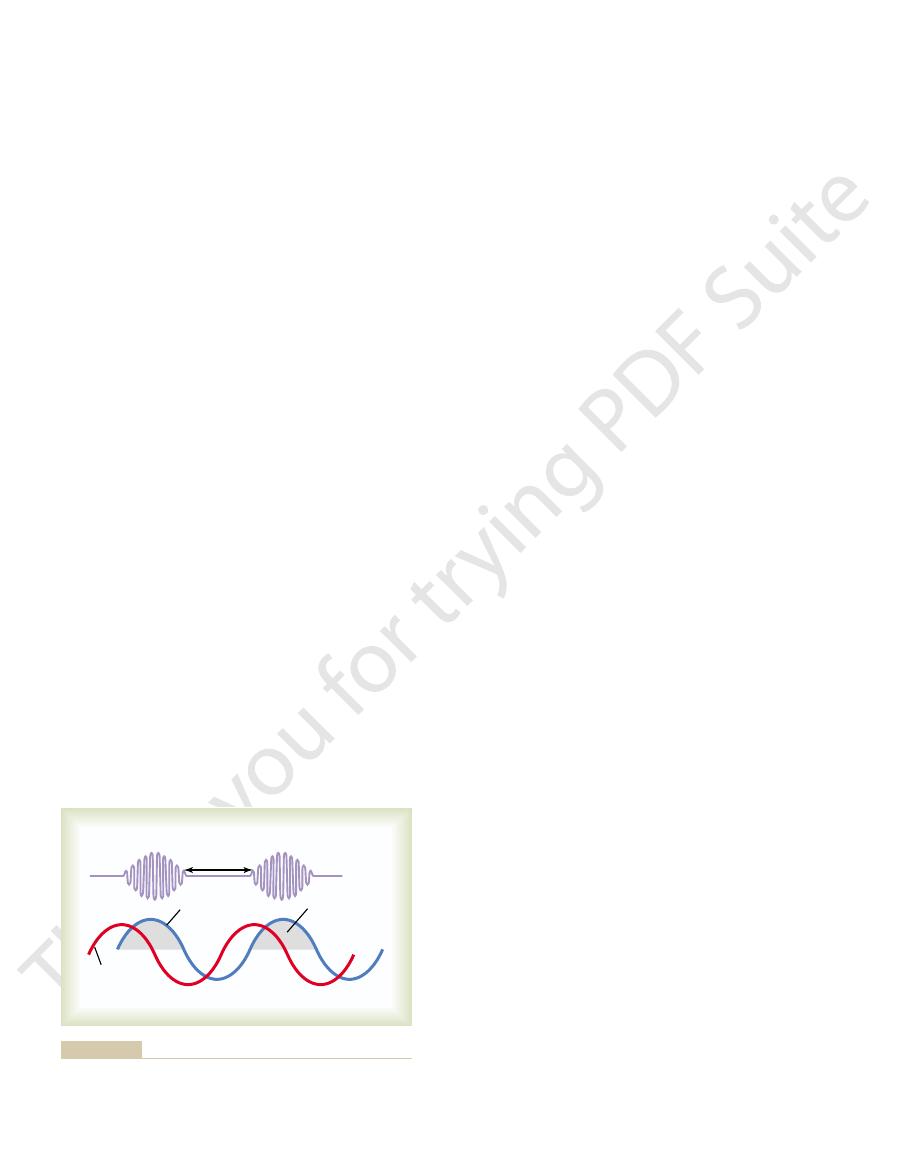
shown in Figure 41–11. Note that the P
Typical records of changes in pulmonary and respira-
with great force. Cheyne-Stokes breathing of this
entirely for a few seconds; then an extra intense
. The brain
brain. This type of Cheyne-Stokes breathing occurs
tendency for periodic breathing is now strong
ventilation 10- to 20-fold. The brain feedback
3 mm Hg, the same 3 mm Hg rise might increase
change in ventilation than normally. For instance,
control areas. This means that a change in blood
increased negative feedback gain
2. A second cause of Cheyne-Stokes breathing is
sometimes occur on and off for months.
heart failure, Cheyne-Stokes breathing can
lungs to the brain. In fact, in patients with chronic
because blood flow is slow,
severe cardiac failure
Stokes breathing begins. This type of Cheyne-
respiratory drive becomes extreme, and Cheyne-
then, after a few more seconds, the periodic
conditions, the storage capacities of the alveoli and
for many more seconds than usual. Under these
long delay occurs for transport of blood
1. When a
ridden, and Cheyne-Stokes breathing does occur:
separate conditions, the damping factors can be over-
the next cycle of the periodic breathing. But under two
carbon dioxide and oxygen. Therefore, normally, the
mechanism is highly “damped.” That is, the fluids of the
in everyone. However, under normal conditions, this
The basic cause of Cheyne-Stokes breathing occurs
cycle repeats.
respond, the person breathes hard once again, and the
respond to these new changes. When the brain does
Again, it takes a few seconds before the brain can
amount. Then the opposite cycle begins. That is, carbon
center, the center becomes depressed an excessive
for an extra few seconds. Therefore, when the overven-
tion. By this time, the person has already overventilated
same time increasing blood oxygen, it takes several
When a person overbreathes, thus blowing off too much
The basic
ring about every 40 to 60 seconds, as illustrated in Figure
ized by slowly waxing and waning respiration occur-
Cheyne-Stokes breathing,
odic breathing,
cycle repeating itself over and over. One type of peri-
slightly or not at all for an additional interval, with the
occurs in a number of disease conditions. The person
one time, morphine was used as an anesthetic, but this
more than many other anesthetics, such as halothane. At
with anesthetics or narcotics. For instance, sodium pen-
522
Unit VII
Respiration
Anesthesia.
Perhaps the most prevalent cause of respi-
ratory depression and respiratory arrest is overdosage
tobarbital depresses the respiratory center considerably
drug is now used only as an adjunct to anesthetics
because it greatly depresses the respiratory center while
having less ability to anesthetize the cerebral cortex.
Periodic Breathing
An abnormality of respiration called periodic breathing
breathes deeply for a short interval and then breathes
is character-
41–11.
Basic Mechanism of Cheyne-Stokes Breathing.
cause of Cheyne-Stokes breathing is the following:
carbon dioxide from the pulmonary blood while at the
seconds before the changed pulmonary blood can be
transported to the brain and inhibit the excess ventila-
tilated blood finally reaches the brain respiratory
dioxide increases and oxygen decreases in the alveoli.
blood and the respiratory center control areas have
large amounts of dissolved and chemically bound
lungs cannot build up enough extra carbon dioxide or
depress the oxygen sufficiently in a few seconds to cause
from the lungs to the brain, changes in carbon
dioxide and oxygen in the alveoli can continue
pulmonary blood for these gases are exceeded;
Stokes breathing often occurs in patients with
thus delaying the transport of blood gases from the
in the respiratory
carbon dioxide or oxygen causes a far greater
instead of the normal 2- to 3-fold increase in
ventilation that occurs when the Pco
2
rises
enough to cause Cheyne-Stokes breathing without
extra blood flow delay between the lungs and
mainly in patients with brain damage
damage often turns off the respiratory drive
increase in blood carbon dioxide turns it back on
type is frequently a prelude to death from brain
malfunction.
tory center Pco
2
during Cheyne-Stokes breathing are
co
2
of the
pulmonary blood changes in advance of the Pco
2
of
corresponds with the Pco
2
Pco
2
in the pulmonary blood where the ventilation is
Sleep Apnea
apnea means absence of spontaneous breath-
in persons with
10 seconds or longer and occurring 300 to 500 times
passage open to allow air to flow into the lungs during
but the airway passage remains open enough to permit
Depth of
respiration
P
CO
2
of
respiratory
neurons
P
CO
2
of
lung blood
Respiratory
center excited
fluids of the respiratory center
(red line)
monary blood
Cheyne-Stokes breathing, showing changing P
Figure 41–11
CO
2
in the pul-
and delayed changes in the P
CO
2
of the
(blue line).

tory neurons. Respir Physiol Neurobiol 131:121, 2002.
Zuperku EJ, McCrimmon DR: Gain modulation of respira-
sleep apnea in adults. JAMA 291:2013, 2004.
Young T, Skatrud J, Peppard PE: Risk factors for obstructive
apnea, and hypertension. Hypertension 42:1067, 2003.
Wolk R, Shamsuzzaman AS, Somers VK: Obesity, sleep
Lippincott Williams & Wilkins, 2003.
West JB: Pulmonary Physiology—The Essentials. Baltimore:
in vertebrates. Physiol Rev 79:855, 1999.
Taylor EW, Jordan D, Coote JH: Central control of the car-
brain. Nat Rev Neurosci 5:437, 2004.
Sharp FR, Bernaudin M: HIF1 and oxygen sensing in the
Physiol 96:1173, 2004.
control of cardiorespiratory physiology by HIF-1. J Appl
-regulated gene expression: transcriptional
Semenza GL: O
5:449, 2004.
sensors that maintain pH homeostasis. Nat Rev Neurosci
Richerson GB: Serotonergic neurons as carbon dioxide
Physiol 62:847, 2000.
temperature in mammals and other vertebrates.Annu Rev
Mortola JP, Frappell PB: Ventilatory responses to changes in
plasticity in respiratory control. J Appl Physiol 94:1242,
Morris KF, Baekey DM, Nuding SC, et al: Neural network
377, 2003.
ology and clinical implications. Acta Physiol Scand 177:
Kara T, Narkiewicz K, Somers VK: Chemoreflexes—physi-
airways. Respir Physiol 125:67, 2001.
Jordan D: Central nervous pathways and control of the
grad Med J 77:700, 2001.
ological and clinical aspects of breathing after stroke. Post-
Howard RS, Rudd AG, Wolfe CD, Williams AJ: Pathophysi-
rhythm in adult mammals. News Physiol Sci 18:23, 2003.
Hilaire G, Pasaro R: Genesis and control of the respiratory
sensory denervation. J Appl Physiol 94:784, 2003.
Forster HV: Plasticity in the control of breathing following
plasticity, chemosensitivity. Annu Rev Neurosci 26:239,
Feldman JL, Mitchell GS, Nattie EE: Breathing: rhythmicity,
biol 131:57, 2002.
regulating upper airway patency. Respir Physiol Neuro-
Dutschmann M, Paton JF: Inhibitory synaptic mechanisms
J Physiol Lung Cell Mol Physiol 283:L665, 2002.
chemoreception and respiratory control. Am
Dean JB, Ballantyne D, Cardone DL, et al: Role of gap junc-
necessary.
helpful, but ventilation with CPAP at night is usually
the stimulatory effects of carbon dioxide. Medications
even small doses of sedatives or narcotics, which further
stimulatory effects of carbon dioxide and hydrogen ions.
unknown, although instability of the respiratory drive
In most patients, the cause of central sleep apnea is
reached that eventually stimulates respiration. These
During sleep, their breathing disorders usually worsen,
they are fully capable of normal voluntary breathing.
decreased ventilation when they are awake, although
. Patients affected by central sleep apnea may have
the ventilatory muscles transiently ceases. Disorders
with sleep apnea, the central nervous system drive to
tory Muscles Is Transiently Abolished.
airway pressure (CPAP)
sleep, and (2) nasal ventilation with
adenoids, or to create an opening in the trachea (tra-
), to remove enlarged tonsils or
tion. The most common treatments of obstructive sleep
nasal obstruction, a very large tongue, enlarged tonsils,
In a few individuals, sleep apnea may be associated with
older, obese persons in whom there is increased fat dep-
cardiovascular disease.
systemic hypertension, and a greatly elevated risk for
pathetic activity, high heart rates, pulmonary and
as well as other disorders, including increased sym-
drowsi-
ing in fragmented, restless sleep. Therefore, patients
repeated several hundred times during the night, result-
apnea. The periods of apnea and labored breathing are
sudden attempts to breathe, which result in loud snorts
which greatly stimulate respiration. This, in turn, causes
ing (apnea) occurs. These periods of apnea result
proceeds, often becoming louder, and is then inter-
occur soon after falling asleep. The snoring
In persons with sleep apnea, loud
cannot flow into the lungs.
narrow passage, and relaxation of these muscles during
Chapter 41
Regulation of Respiration
523
sleep causes the pharynx to completely close so that air
snoring and labored
breathing
rupted by a long silent period during which no breath-
in significant decreases in Po
2
and increases in Pco
2
,
and gasps followed by snoring and repeated episodes of
with sleep apnea usually have excessive daytime
ness
Obstructive sleep apnea most commonly occurs in
osition in the soft tissues of the pharynx or compression
of the pharynx due to excessive fat masses in the neck.
or certain shapes of the palate that greatly increase
resistance to the flow of air to the lungs during inspira-
apnea include (1) surgery to remove excess fat tissue
at the back of the throat (a procedure called uvu-
lopalatopharyngoplasty
cheostomy) to bypass the obstructed airway during
continuous positive
.
“Central” Sleep Apnea Occurs When the Neural Drive to Respira-
In a few persons
that can cause cessation of the ventilatory drive during
sleep include damage to the central respiratory centers
or abnormalities of the respiratory neuromuscular appa-
ratus
resulting in more frequent episodes of apnea that
decrease Po
2
and increase Pco
2
until a critical level is
transient instabilities of respiration cause restless sleep
and clinical features similar to those observed in
obstructive sleep apnea.
can result from strokes or other disorders that make the
respiratory centers of the brain less responsive to the
Patients with this disease are extremely sensitive to
reduce the responsiveness of the respiratory centers to
that stimulate the respiratory centers can sometimes be
References
tions in CO
2
2003.
2003.
2
diovascular and respiratory systems and their interactions
