
way: Each sympathetic pathway from the cord to the stimulated tissue is composed
The sympathetic nerves are different from skeletal motor nerves in the following
then to the tissues and organs that are stimulated by the sympathetic nerves.
sympathetic chain
between cord segments T-1 and L-2 and pass first into the
The sympathetic nerve fibers originate in the spinal cord along with spinal nerves
nal organs.
), and (3) nerves extending from the ganglia to the different inter-
nerves on the side of the vertebral column, (2) two
paravertebral sympathetic chains of ganglia
pathetic nervous system. Shown specifically in the figure are (1) one of the two
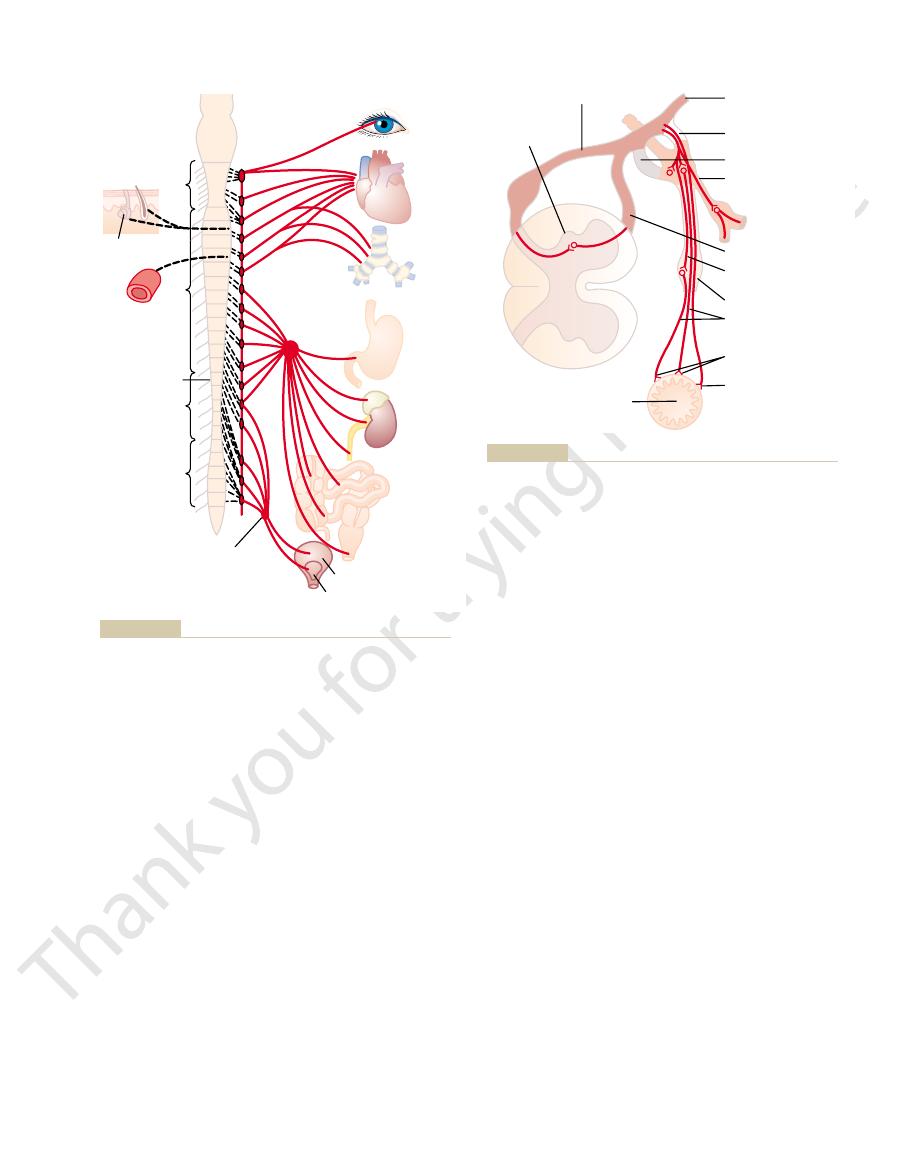
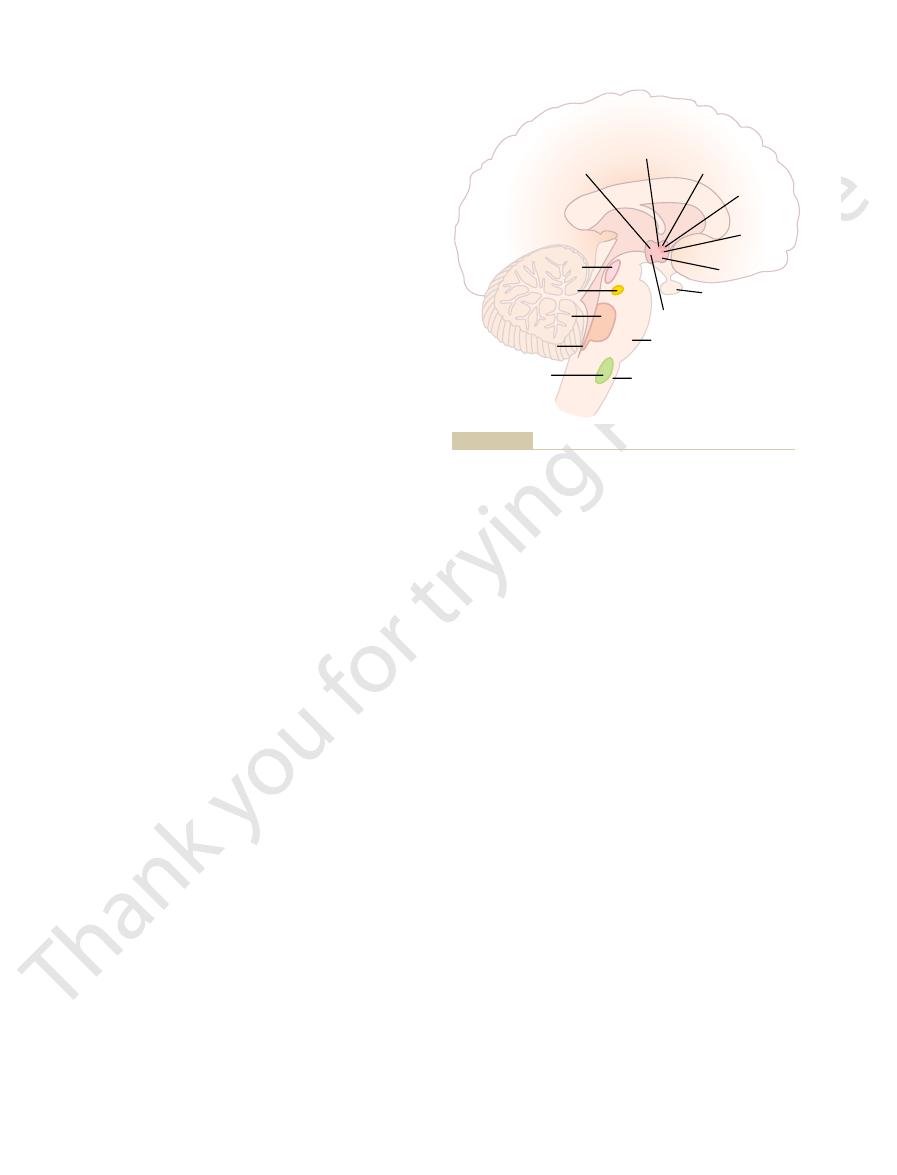
Figure 60–1 shows the general organization of the peripheral portions of the sym-
Physiologic Anatomy of the Sympathetic Nervous System
follow.
, the characteristics and functions of which
The efferent autonomic signals are transmitted to the various organs of the
activities.
the autonomic ganglia, the brain stem, or the hypothalamus and then return
. That is, subconscious sensory signals from a visceral organ can enter
reflexes
The autonomic nervous system also often operates by means of
especially of the limbic cortex, can transmit signals to the lower centers and in
. Also, portions of the cerebral cortex,
, and
spinal cord
The autonomic nervous system is activated mainly by centers located in the
Nervous System
General Organization of the Autonomic
bladder may empty involuntarily, also within seconds.
seconds to cause fainting. Sweating can begin within seconds, and the urinary
extreme, the arterial pressure can be decreased low enough within 10 to 15
and within 10 to 15 seconds the arterial pressure can be doubled; or, at the other
instance, within 3 to 5 seconds it can increase the heart rate to twice normal,
the rapidity and intensity with which it can change visceral functions. For
activities, some of which are controlled almost
ing, sweating, body temperature, and many other
gastrointestinal secretion, urinary bladder empty-
control arterial pressure, gastrointestinal motility,
This system helps to
The portion of the nervous system that controls
and the Adrenal Medulla
The Autonomic Nervous System
C
H
A
P
T
E
R
6
0
748
most visceral functions of the body is called the
autonomic nervous system.
entirely and some only partially by the autonomic
nervous system.
One of the most striking characteristics of the autonomic nervous system is
, brain stem
hypothalamus
this way influence autonomic control.
visceral
subconscious reflex responses directly back to the visceral organ to control its
body through two major subdivisions called the sympathetic nervous system and
the parasympathetic nervous system
that are interconnected with the spinal
prevertebral ganglia (the celiac
and hypogastric
and
Preganglionic and Postganglionic Sympathetic Neurons
lateral horn cells of the spinal cord, through the
, all the way from the intermedio-
Preganglionic sympathetic nerve fibers pass,
Special Nature of the Sympathetic Nerve Endings in the Adrenal
into the thorax. Likewise, the abdominal organs receive
which the organ originated. For instance, the heart
The distribution of sympathetic nerves to each organ
greatly.
This distribution is only approximate and overlaps
the abdomen; and from T-12, L-1, and L-2 into the legs.
into the thorax; from T-7, T-8, T-9, T-10, and T-11 into
to terminate in the neck; from T-3, T-4, T-5, and T-6
the sympathetic chain to terminate in the head; from T-2
pathetic fibers from cord segment T-1 generally pass up
nerve fibers from the same segments. Instead, the
The
Segmental Distribution of the Sympathetic Nerve Fibers.
fibers, a fact that indicates their great importance.
piloerector muscles of the hairs. About 8 per cent of the
nerves. They control the blood vessels, sweat glands, and
pathetic fibers are all very small type C fibers, and they
levels of the cord, as shown in Figure 60–2. These sym-
gray rami
Sympathetic Nerve Fibers in the Skeletal Nerves.
organs.
From either of these two sources, the postganglionic
The postganglionic sympathetic neuron thus origi-
chain, finally synapsing in a
other ganglia of the chain; or (3) it can pass for variable
in the ganglion that it enters; (2) it can pass upward
of the fibers can be one of the following three: (1) It
Then the course
sympathetic chain.
canal, the preganglionic sympathetic fibers leave the
spinal nerve.
spinal cord; its fiber passes, as shown in Figure 60–2,
skeletal motor pathway. The cell body of each pregan-
, in contrast to only a single neuron in the
of two neurons, a
The Autonomic Nervous System and the Adrenal Medulla
Chapter 60
749
preganglionic neuron and a postgan-
glionic neuron
glionic neuron lies in the intermediolateral horn of the
through an anterior root of the cord into the corre-
sponding
Immediately after the spinal nerve leaves the spinal
spinal nerve and pass through a white ramus into one of
the ganglia of the
can synapse with postganglionic sympathetic neurons
or downward in the chain and synapse in one of the
distances through the chain and then through one
of the sympathetic nerves radiating outward from the
peripheral sympathetic
ganglion.
nates either in one of the sympathetic chain ganglia
or in one of the peripheral sympathetic ganglia.
fibers then travel to their destinations in the various
Some of the
postganglionic fibers pass back from the sympathetic
chain into the spinal nerves through
at all
extend to all parts of the body by way of the skeletal
fibers in the average skeletal nerve are sympathetic
sympathetic pathways that originate in the different
segments of the spinal cord are not necessarily distrib-
uted to the same part of the body as the somatic spinal
sym-
is determined partly by the locus in the embryo from
receives many sympathetic nerve fibers from the neck
portion of the sympathetic chain because the heart orig-
inated in the neck of the embryo before translocating
most of their sympathetic innervation from the lower
thoracic spinal cord segments because most of the prim-
itive gut originated in this area.
Medullae.
without synapsing
Bronchi
Heart
Eye
Celiac
ganglion
Blood
vessel
Sweat
gland
Piloerector
muscle
12
T-1
5
5
L-1
8
Hypogastric plexus
Pylorus
Adrenal
medulla
Kidney
Ureter
Intestine
Ileocecal valve
Anal sphincter
Detrusor
Trigone
sweat glands, and piloerector muscles.
postganglionic fibers in the gray rami leading from the sympa-
Sympathetic nervous system. The black dashed lines represent
Figure 60–1
thetic chains into spinal nerves for distribution to blood vessels,
Peripheral ganglion
Postganglionic nerve
fibers
Preganglionic nerve
fiber
Effector endings
Sensory endings
Anterior root
Sympathetic chain
Gray ramus
White ramus
Spinal nerve
Posterior root
Gut
Intermedio-
lateral horn
Nerve connections between the spinal cord, spinal nerves, sym-
Figure 60–2
pathetic chain, and peripheral sympathetic nerves.

a very few blood vessels are cholinergic.
glands, to the piloerector muscles of the hairs, and to
.
However,
the
. Conversely,
neurons of the parasympathetic system are also cholin-
neurons. Either
stances, when applied to the ganglia, will excite both
systems. Acetylcholine or acetylcholine-like sub-
cholinergic
is an alternate name for epinephrine.
, a term derived from
. Those that secrete norepinephrine are said
cholinergic
Those fibers that secrete acetylcholine are said to be
acetylcholine
mitter substances,
The sympathetic and parasympathetic nerve fibers
Secretion of Acetylcholine or
Cholinergic and Adrenergic Fibers—
abdomen, rather than in the excited organ itself.
arrangement of the sympathetic ganglia, because the
neurons to innervate the tissues of the organ. This loca-
a millimeter to several centimeters in length, leave the
and very, very short postganglionic fibers, a fraction of
The preganglionic fibers synapse with these,
neurons.
pathetic nerves, the
However, except in the case of a few cranial parasym-
both preganglionic and postganglionic neurons.
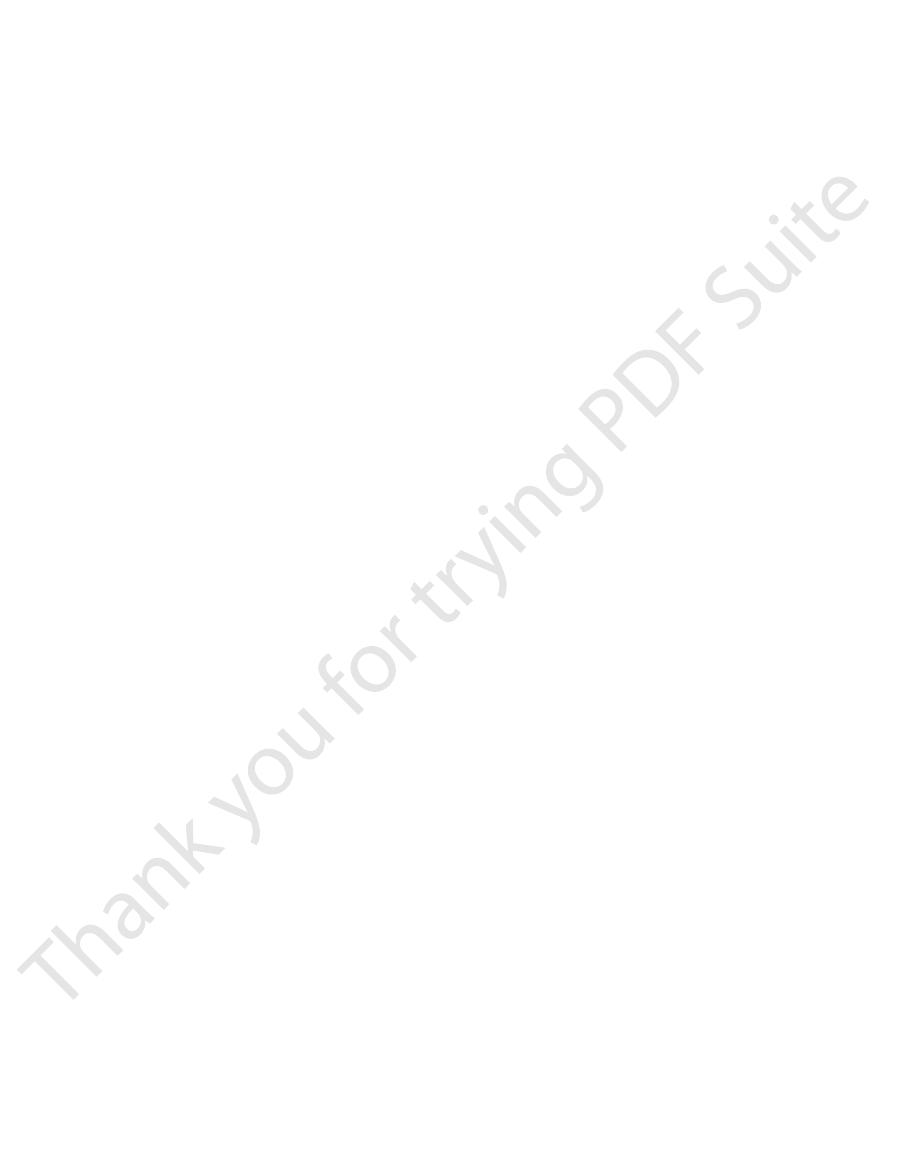
The parasympathetic system, like the sympathetic, has
ureters. Also, this sacral group of parasympathetics sup-
rectum, urinary bladder, and lower portions of the
These fibers then distribute to the descending colon,
plexus on each side of the cord at the S-2 and S-3 levels.
, which pass through the spinal nerve sacral
The sacral parasympathetic fibers are in the
lacrimal, nasal, and submandibular glands. And fibers
Fibers from the
the pupillary sphincter and ciliary muscle of the eye.
third cranial nerve
upper portions of the ureters.
of the colon, liver, gallbladder, pancreas, kidneys, and
esophagus, stomach, entire small intestine, proximal half
supply parasympathetic nerves to the heart, lungs,
thinks mainly of the two vagus nerves. The vagus nerves
abdominal regions of the body. Therefore, a physiologist
(cranial nerve X), passing to the entire thoracic and
the first and fourth sacral nerves. About 75 per cent of
VII, IX, and X; additional parasympathetic fibers leave
60–3, demonstrating that parasympathetic fibers leave
is shown in Figure
The
Physiologic Anatomy of the
norepinephrine.
nerve fibers, and it is the endings of these fibers that
glionic neurons; indeed, they even have rudimentary
These secretory cells embryologically are derived from
and finally into the two adrenal medullae. There they
sympathetic chains, then through the splanchnic nerves,
The Nervous System: C. Motor and Integrative Neurophysiology
750
Unit XI
end directly on modified neuronal cells that secrete epi-
nephrine and norepinephrine into the blood stream.
nervous tissue and are actually themselves postgan-
secrete the adrenal hormones epinephrine
and
Parasympathetic Nervous System
parasympathetic nervous system
the central nervous system through cranial nerves III,
the lowermost part of the spinal cord through the
second and third sacral spinal nerves and occasionally
all parasympathetic nerve fibers are in the vagus nerves
speaking of the parasympathetic nervous system often
Parasympathetic fibers in the
go to
seventh cranial nerve pass to the
from the ninth cranial nerve go to the parotid gland.
pelvic
nerves
plies nerve signals to the external genitalia to cause
erection.
Preganglionic and Postganglionic Parasympathetic Neurons.
preganglionic fibers pass uninter-
rupted all the way to the organ that is to be controlled.
In the wall of the organ are located the postganglionic
tion of the parasympathetic postganglionic neurons in
the visceral organ itself is quite different from the
cell bodies of the sympathetic postganglionic neurons
are almost always located in the ganglia of the sympa-
thetic chain or in various other discrete ganglia in the
Basic Characteristics
of Sympathetic and
Parasympathetic Function
Norepinephrine
secrete mainly one or the other of two synaptic trans-
or norepinephrine.
to be adrenergic
adrenalin, which
All preganglionic neurons are
in both
the sympathetic and the parasympathetic nervous
sympathetic and parasympathetic postganglionic
all or almost all of the postganglionic
ergic
most of the postganglionic sym-
pathetic neurons are adrenergic
postganglionic sympathetic nerve fibers to the sweat
Heart
Parotid gland
Otic ganglion
Submandibular gland
Submandibular ganglion
Nasal glands
Lacrimal glands
Sphenopalatine ganglion
Pupillary sphincter
Ciliary muscles of eye
Ciliary ganglion
Pylorus
Colon
Small intestine
Ileocecal valve
Anal sphincter
Bladder
Detrusor
Trigone
Sacral
Stomach
1
X
IX
VII
V
III
2
3
4
Figure 60–3
Parasympathetic nervous system.
Therefore, when secreted into the blood, both norepi-
methyl transferase; this occurs mainly in the liver.
tissue, where they can be destroyed by catechol-
tissue are rapid. However, the norepinephrine and
a tissue remains active for only a few seconds, demon-
Ordinarily, the norepinephrine secreted directly into
, which is present diffusely in all tissues).
catechol-O-methyl trans-
nerve endings, and another is
, which is found in the
monoamine oxidase
of the remaining norepinephrine; and (3) destruction
secreted norepinephrine; (2) diffusion away from the
three ways: (1) reuptake into the adrenergic nerve
nerve endings, it is removed from the secretory site in
epinephrine into epinephrine, as follows:
In the adrenal medulla, this reaction goes still one
3. Transport of dopamine into the vesicles
cles. The basic steps are the following:
for synthesis of new acetylcholine.
minal nerve ending, where it is used again and again
muscular junctions of skeletal nerve fibers. The choline
the local connective tissue. This is the same mechanism
acetylcholinesterase
, catalyzed by the enzyme
choline
mitter function. Then it is split into an
cholinergic nerve ending, it persists in the tissue for a
centrated form until it is released. The basic chemical
The molecular structures of acetylcholine and nor-
Therefore, acetylcholine is called a
respective parasympathetic or sympathetic effects.
, but a few secrete acetylcholine. These
acetylcholine
Thus, the terminal nerve endings of the parasympa-
The Autonomic Nervous System and the Adrenal Medulla
Chapter 60
751
thetic system all or virtually all secrete
.
Almost all of the sympathetic nerve endings secrete
norepinephrine
hormones in turn act on the different organs to cause
parasympathetic
transmitter and norepinephrine is called a sympathetic
transmitter.
epinephrine are the following:
Synthesis of Acetylcholine, Its Destruction After Secretion, and
Its Duration of Action.
Acetylcholine is synthesized in the
terminal endings and varicosities of the cholinergic
nerve fibers where it is stored in vesicles in highly con-
reaction of this synthesis is the following:
Once acetylcholine is secreted into a tissue by a
few seconds while it performs its nerve signal trans-
acetate ion and
that is bound with collagen and glycosaminoglycans in
for acetylcholine signal transmission and subsequent
acetylcholine destruction that occurs at the neuro-
that is formed is then transported back into the ter-
Synthesis of Norepinephrine, Its Removal, and Its Duration of
Action.
Synthesis of norepinephrine begins in the axo-
plasm of the terminal nerve endings of adrenergic
nerve fibers but is completed inside the secretory vesi-
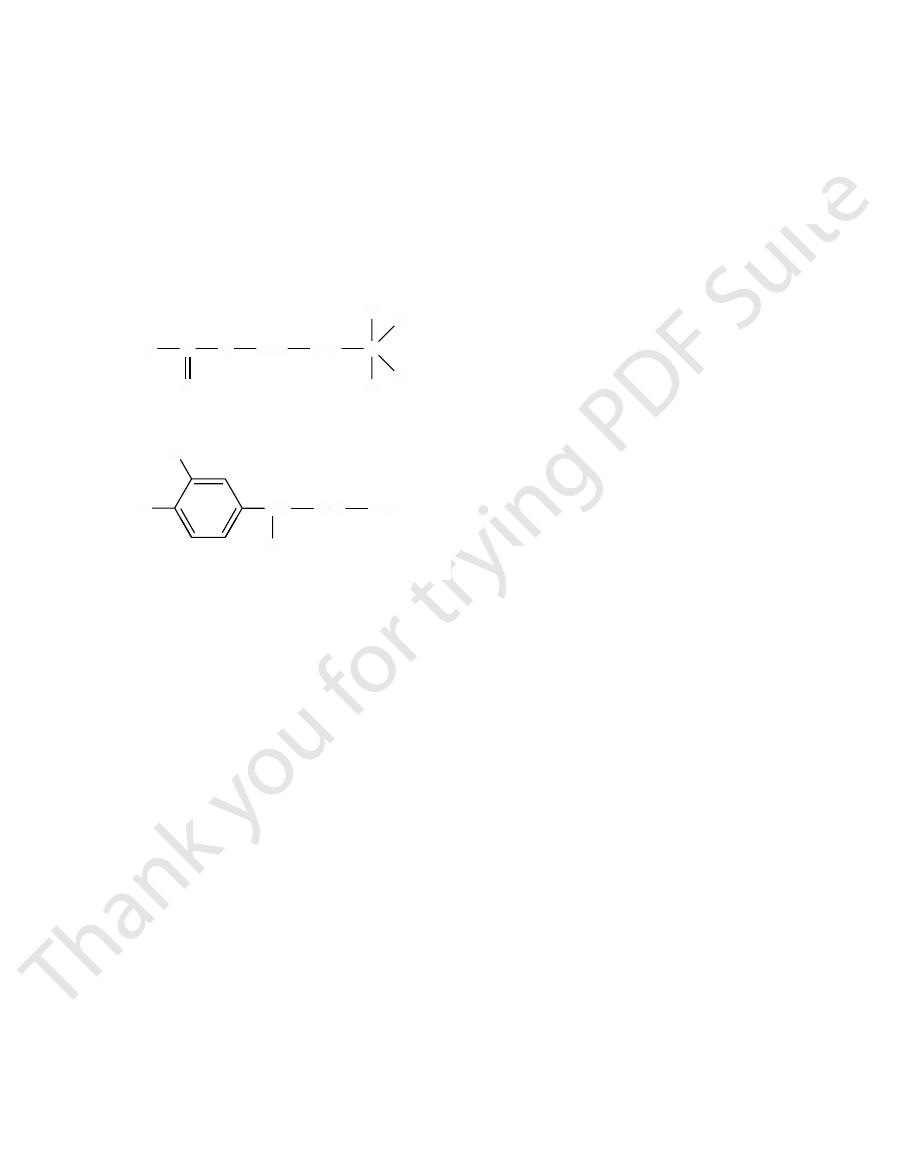
1.
2.
4.
step further to transform about 80 per cent of the nor-
5.
After secretion of norepinephrine by the terminal
endings themselves by an active transport process—
accounting for removal of 50 to 80 per cent of the
nerve endings into the surrounding body fluids and
then into the blood—accounting for removal of most
of small amounts by tissue enzymes (one of these
enzymes is
ferase
strating that its reuptake and diffusion away from the
epinephrine secreted into the blood by the adrenal
medullae remain active until they diffuse into some
O-
nephrine and epinephrine remain very active for 10 to
Norepinephrine
Epinephrine
methylation
æ
Æ
æææ
Dopamine
Norepinephrine
hydroxylation
æ
Æ
ææææ
Dopa
Dopamine
decarboxylation
æ
Æ
ææææ
æ
Tyrosine
Dopa
hydroxylation
æ
Æ
ææææ
A
+
æ
Æ
choline acetyl-
cetyl-CoA
Choline
Acetylcholine
transferase
ææææ
O
CH
Acetylcholine
Norepinephrine
2
CH
2
C
N
O
CH
3
NH
2
CH
2
CH
HO
OH
CH
3
CH
3
CH
3
+
HO
rior. Thus, the transmitter substance is secreted.
varicosities. The calcium ions in turn cause the termi-
ber membrane to calcium ions, allowing
bers, the depolarization process increases the perme-
When an action potential spreads over the terminal
nephrine synthesis.
mitochondria that supply adenosine triphosphate,
stored. Also in the varicosities are large numbers of
or pass over or near the cells to be stimulated, they
that are to be stimulated. Where these
vate as they pass by; or in some instances, they termi-
tion. However, many of the parasympathetic nerve
parasympathetic nerves, are similar to but much
autonomic nerve endings, especially those of the
glionic Nerve Endings.
Subsequent Removal of the Transmitter
Mechanisms of Transmitter Secretion and
at the Postganglionic Endings
Secretion of Acetylcholine and Norepinephrine by Postgan-
A few of the postganglionic
smaller than those of the skeletal neuromuscular junc-
fibers and almost all the sympathetic fibers merely
touch the effector cells of the organs that they inner-
nate in connective tissue located adjacent to the cells
filaments touch
usually have bulbous enlargements called varicosities;
it is in these varicosities that the transmitter vesicles of
acetylcholine or norepinephrine are synthesized and
which is required to energize acetylcholine or norepi-
fi
ability of the fi
these ions to diffuse into the nerve terminals or nerve
nals or varicosities to empty their contents to the exte-
but essentially no action on alpha receptors.
rine,
isopropyl norepineph-
nephrine and norepinephrine,
inhibitory. Therefore, alpha and beta receptors are not
are excitatory, whereas others are inhibitory. Likewise,
by the sympathetics. Note that certain alpha functions
Table 60
beta receptors, epinephrine will be the more effective
types of receptors in the organs. If they are all
types of receptors approximately equally. Therefore,
extent as well. Conversely, epinephrine excites both
beta receptors. Norepinephrine excites mainly alpha
Norepinephrine and epinephrine, both of which are
receptors.)
receptors. Also, there is a division of alpha receptors
. (The beta
tors,
There are also two major types of adrenergic recep-
Adrenergic Receptors—Alpha and
the other of the two types of receptors.
instance, at the neuromuscular junctions in skeletal
parasympathetic systems. (Nicotinic receptors are also
tine activates only nicotinic receptors; acetylcholine
and will not activate nicotinic receptors, whereas nico-
from toadstools, activates only muscarinic receptors
reason for these names is that muscarine, a poison
receptors. The
They are called
Two Principal Types of Acetylcholine
organs.
formational state. In each organ, the resulting effects
or excitation in others. This is usually determined by
of many different intracellular actions, the exact effect
. The cAMP in turn can initiate any one
on the inside of the cell, and
protrudes into the interior of the cell. For instance,
lar chemical) inside the cell. The enzyme often is
ment will cause an internal cell action, such as a direct
In some cells, the changed intracellular ion environ-
sium ions to diffuse out of the cell, and this usually
times, potassium channels are opened, allowing potas-
the cell. At other
the respective ions into the cell, usually depolarizing
For instance, sodium and/or calcium ion channels
permeability of the cell membrane to various ions.
interstices of the protein molecule, thus altering the
opens or closes an ion channel
is an integral part of the cell membrane, a conforma-
Membrane Permeability.
or inhibits the cell, most often by (1) causing a change
molecule. In turn, the altered protein molecule excites
stance binds with the receptor, this causes a confor-
through the cell membrane. When the transmitter sub-
outside of the cell membrane, bound as a prosthetic
on the effector cells. The receptor is on the
ulate an effector organ, it must
Before an acetylcholine, norepinephrine, or epineph-
over 1 to several minutes.
30 seconds; but their activity declines to extinction
The Nervous System: C. Motor and Integrative Neurophysiology
752
Unit XI
Receptors on the Effector Organs
rine secreted at an autonomic nerve ending can stim-
first bind with specific
receptors
group to a protein molecule that penetrates all the way
mational change in the structure of the protein
in cell membrane permeability to one or more ions or
(2) activating or inactivating an enzyme attached to
the other end of the receptor protein where it pro-
trudes into the interior of the cell.
Excitation or Inhibition of the Effector Cell by Changing Its
Because the receptor protein
tional change in structure of the receptor protein
often
through the
frequently become opened and allow rapid influx of
the cell membrane and exciting
inhibits the cell because loss of electropositive
potassium ions creates hypernegativity inside the cell.
effect of calcium ions to promote smooth muscle
contraction.
Receptor Action by Altering Intracellular “Second Messenger”
Enzymes.
Another way a receptor often functions is to
activate or inactivate an enzyme (or other intracellu-
attached to the receptor protein where the receptor
binding of norepinephrine with its receptor on the
outside of many cells increases the activity of the
enzyme adenylyl cyclase
this causes formation of cyclic adenosine monophos-
phate (cAMP)
depending on the chemical machinery of the effector
cell.
It is easy to understand how an autonomic trans-
mitter substance can cause inhibition in some organs
the nature of the receptor protein in the cell mem-
brane and the effect of receptor binding on its con-
are likely to be entirely different from those in other
Receptors—Muscarinic and Nicotinic
Receptors
Acetylcholine activates mainly two types of receptors.
muscarinic and nicotinic
activates both of them.
Muscarinic receptors are found on all effector cells
that are stimulated by the postganglionic cholinergic
neurons of either the parasympathetic nervous system
or the sympathetic system.
Nicotinic receptors are found in the autonomic
ganglia at the synapses between the preganglionic and
postganglionic neurons of both the sympathetic and
present at many nonautonomic nerve endings—for
muscle [discussed in Chapter 7].)
An understanding of the two types of receptors is
especially important because specific drugs are fre-
quently used as medicine to stimulate or block one or
Beta Receptors
alpha receptors and beta receptors
receptors in turn are divided into beta
1
and beta
2
recep-
tors because certain chemicals affect only certain beta
into alpha
1
and alpha
2
secreted into the blood by the adrenal medulla,
have slightly different effects in exciting the alpha and
receptors but excites the beta receptors to a lesser
the relative effects of norepinephrine and epinephrine
on different effector organs are determined by the
excitant.
–1 gives the distribution of alpha and beta
receptors in some of the organs and systems controlled
certain beta functions are excitatory and others are
necessarily associated with excitation or inhibition but
simply with the affinity of the hormone for the recep-
tors in the given effector organ.
A synthetic hormone chemically similar to epi-
has an extremely strong action on beta receptors
sion of contents along the tract. This propulsive effect
and relaxing the sphincters, thus allowing rapid propul-
stimulation, in general, increases overall degree of activ-
the gastrointestinal intramural plexus. Parasympathetic
, located in the walls of the gut.Also, both
The
Intramural Nerve Plexus of the Gastrointestinal System.
parasympathetic centers.
close embryological relation to sweat glands, are acti-
the shoulder joint. The apocrine glands, despite their
ulation. This secretion actually functions as a lubricant
lation, but they do not respond to parasympathetic stim-
The
could be called a parasympathetic function, even though
to be parasympathetic centers. Therefore, sweating
more, the sweat glands are stimulated primarily by
bers, which are adrenergic. Further-
bers to the palms and soles), in contrast to almost all
cholinergic
glands are
nerves. However, the sympathetic
when the sympathetic nerves are stimulated, but no
sweat glands
The
enzymes and mucus. But it also causes vasoconstriction
less by the autonomic nerves.
those of the mouth and stomach. On the other hand, the
parasympathetics are those of the upper tract, especially
copious quantities of watery secretion. The glands of
parasympathetic nervous system, usually resulting in
, and many
The
Glands of the Body.
tion of the eyes.
objects near at hand. The detailed focusing mechanism
become more convex, causing the eye to focus on
of the lens radial ligaments. This contraction releases
, which is a ringlike body of
of its radial ligaments. Parasympathetic excitation con-
the parasympathetic nervous system. The lens is nor-
Focusing of the lens is controlled almost entirely by
increase pupillary opening at these times.
that strikes the retina. Conversely, the sympathetics
which is explained in Chapter 51; this re
exly stimulated when excess light enters the eyes,
The parasympathetics that control the pupil are
the pupil, whereas parasym-
contracts the meridional
opening and (2) the focus of the lens.
autonomic nervous system. They are (1) the pupillary
Two functions of the eyes are controlled by the
Effects of Sympathetic and
ed in still greater detail, as follows.
2. Some of these functions need to
listed in Table 60
tions of these two nervous systems on each organ, as
thetic function, one must learn all the separate func-
Therefore, to understand sympathetic and parasympa-
There is no generalization one can use to explain
of the two systems.
occasionally act reciprocally to each other. But most
times inhibits it, demonstrating that the two systems
particular organ, parasympathetic stimulation some-
Also, when sympathetic stimulation excites a
others.
inhibitory effects in others. Likewise, parasympathetic
From this table, it can be seen again that
parasympathetic nerves or the sympathetic nerves.
Table 60
Actions of Sympathetic and
Excitatory and Inhibitory
The Autonomic Nervous System and the Adrenal Medulla
Chapter 60
753
Parasympathetic Stimulation
–2 lists the effects on different visceral func-
tions of the body caused by stimulating either the
sympathetic
stimulation causes excitatory effects in some organs but
stimulation causes excitation in some but inhibition in
organs are dominantly controlled by one or the other
whether sympathetic or parasympathetic stimulation
will cause excitation or inhibition of a particular organ.
–
be clarifi
Parasympathetic Stimulation
on Specific Organs
Eyes.
Sympathetic stimulation
fibers of the iris that dilate
pathetic stimulation contracts the circular muscle of the
iris to constrict the pupil.
refl
flex reduces the
pupillary opening and decreases the amount of light
become stimulated during periods of excitement and
mally held in a flattened state by intrinsic elastic tension
tracts the ciliary muscle
smooth muscle fibers that encircles the outside ends
the tension on the ligaments and allows the lens to
is discussed in Chapters 49 and 51 in relation to func-
nasal, lacrimal, salivary
gastrointestinal glands are strongly stimulated by the
the alimentary tract most strongly stimulated by the
glands of the small and large intestines are controlled
principally by local factors in the intestinal tract itself
and by the intestinal enteric nervous system and much
Sympathetic stimulation has a direct effect on most
alimentary gland cells to cause formation of a concen-
trated secretion that contains high percentages of
of the blood vessels that supply the glands and in this
way sometimes reduces their rates of secretion.
secrete large quantities of sweat
effect is caused by stimulating the parasympathetic
fibers to most sweat
(except for a few adrenergic
fi
other sympathetic fi
centers in the hypothalamus that are usually considered
it is controlled by nerve fibers that anatomically are dis-
tributed through the sympathetic nervous system.
apocrine glands in the axillae secrete a thick,
odoriferous secretion as a result of sympathetic stimu-
to allow easy sliding motion of the inside surfaces under
vated by adrenergic fibers rather than by cholinergic
fibers and are also controlled by the sympathetic centers
of the central nervous system rather than by the
gastrointestinal system has its own intrinsic set of nerves
known as the intramural plexus or the intestinal enteric
nervous system
parasympathetic and sympathetic stimulation originat-
ing in the brain can affect gastrointestinal activity
mainly by increasing or decreasing specific actions in
ity of the gastrointestinal tract by promoting peristalsis
is associated with simultaneous increases in rates of
Table 60–1
Bladder sphincter contraction
Calorigenesis (
Pilomotor contraction
Bronchodilation (
Intestinal sphincter contraction
Intestinal relaxation (
Intestinal relaxation
Increased myocardial
Iris dilation
Cardioacceleration (
Vasoconstriction
Vasodilation (
Alpha Receptor
Beta Receptor
Adrenergic Receptors and Function
b
2
)
b
1
)
strength (
b
1
)
b
2
)
Uterus relaxation (
b
2
)
b
2
)
b
2
)
Glycogenolysis (
b
2
)
Lipolysis (
b
1
)
Bladder wall relaxation (
b
2
)
sympathetic vascular constriction, but this occurs rarely
Under some conditions, the beta function of the sym-
restricted areas, such as in the blush area of the face.
limbs, are constricted by sympathetic stimulation.
Most systemic blood vessels, espe-
Systemic Blood Vessels.
strenuous activity.
pumping, allowing the heart to rest between bouts of
heart as a pump, as required during heavy exercise,
tion. To express these effects in another way, sympa-
overall activity of the heart. This is accomplished by
In general, sympathetic stimulation increases the
increases the tone of the sphincters. The net result is
very dependent on sympathetic stimulation. However,
described earlier.
secretion by many of the gastrointestinal glands,
The Nervous System: C. Motor and Integrative Neurophysiology
754
Unit XI
Normal function of the gastrointestinal tract is not
strong sympathetic stimulation inhibits peristalsis and
greatly slowed propulsion of food through the tract and
sometimes decreased secretion as well—even to the
extent of sometimes causing constipation.
Heart.
increasing both the rate and force of heart contraction.
Parasympathetic stimulation causes mainly opposite
effects—decreased heart rate and strength of contrac-
thetic stimulation increases the effectiveness of the
whereas parasympathetic stimulation decreases heart
cially those of the abdominal viscera and skin of the
Parasympathetic stimulation has almost no effects on
most blood vessels except to dilate vessels in certain
pathetics causes vascular dilation instead of the usual
except after drugs have paralyzed the sympathetic alpha
Table 60–2
Skeletal muscle
Increased glycogenolysis
None
Piloerector muscles
Contracted
None
Mental activity
Increased
None
Adrenal medullary secretion
Increased
None
Basal metabolism
Increased up to 100%
None
Lipids
Increased
None
Glucose
Increased
None
Coagulation
Increased
None
Skin
Constricted
None
)
None
Muscle
Constricted (adrenergic
Abdominal viscera
Constricted
None
Penis
Ejaculation
Erection
Trigone
Contracted
Relaxed
Detrusor
Relaxed (slight)
Contracted
Kidney
Decreased output and renin secretion
None
Gallbladder and bile ducts
Relaxed
Contracted
Liver
Glucose released
Slight glycogen synthesis
Sphincter
Increased tone (most times)
Relaxed (most times)
Lumen
Decreased peristalsis and tone
Increased peristalsis and tone
Blood vessels
Mildly constricted
? Dilated
Bronchi
Dilated
Constricted
)
Dilated
); constricted (
Coronaries
Dilated (
Increased force of contraction
Decreased force of contraction (especially of atria)
Muscle
Increased rate
Slowed rate
Blood vessels
Most often constricted
Most often little or no effect
Apocrine glands
Thick, odoriferous secretion
None
Sweat glands
Copious sweating (cholinergic)
Sweating on palms of hands
Nasal
enzyme-secreting glands)
Glands
Vasoconstriction and slight secretion
Stimulation of copious secretion (containing many enzymes for
Ciliary muscle
Slight relaxation (far vision)
Constricted (near vision)
Pupil
Dilated
Constricted
Organ
Effect of Sympathetic Stimulation
Effect of Parasympathetic Stimulation
Autonomic Effects on Various Organs of the Body
Eye
Lacrimal
Parotid
Submandibular
Gastric
Pancreatic
Heart
b
2
a
Lungs
Gut
Bladder
Systemic arterioles
a
Dilated (adrenergic
b
2
)
Dilated (cholinergic)
Blood
Increased strength
Fat cells
Lipolysis
None
bers.
by these hormones, especially by epinephrine,
bers. For instance,
missing.
factor, one mechanism substituting for the other if it is
almost all the necessary duties. Thus, the dual mecha-
blood and indirectly cause stimulation. Likewise,
most instances, substitute for the other. For instance,
of stimulation support each other, and either can, in
the adrenal medullary hormones. The two means
fore, the organs are actually stimulated in two ways:
directly by generalized sympathetic activation. There-
thetic Nervous System.
Value of the Adrenal Medullae to the Function of the Sympa-
over.
longed, lasting 2 to 4 minutes after the stimulation is
stimulation, except that the effects are greatly pro-
epinephrine, which together have almost the same
In summary, stimulation of the adrenal medullae
such as glycogenolysis in the liver and muscle, and
also increases the rates of other metabolic activities,
increasing the activity and excitability of the body. It
as much as 100 per cent above normal, in this way
great a metabolic effect as norepinephrine. Indeed, the
tissue metabolism. Epinephrine has 5 to 10 times as
cardiac output more.
elevates arterial pressure, whereas epinephrine raises
a major segment of the vessels of the body, this differ-
norepinephrine. Because the muscle vessels represent
constriction of the blood vessels in the muscles, in com-
epinephrine. Second, epinephrine causes only weak
greater effect in stimulating the beta receptors, has a
following respects: First, epinephrine, because of its
caused by norepinephrine, but the effects differ in the
gastrointestinal tract, dilation of the pupils of the eyes,
causes increased activity of the heart, inhibition of the
of essentially all the blood vessels of the body; it also
The circulating norepinephrine causes constriction
slowly over a period of 2 to 4 minutes.
The circulating epinephrine and norepinephrine
physiologic conditions.
20 per cent is norepinephrine, although the relative
the blood to all tissues of the body. On the average,
blood, and these two hormones in turn are carried in
Function of the Adrenal Medullae
acts, as explained in Chapters 80 and 81.
Finally, the sympathetics and parasympathetics are
basal metabolic rate, and increase in mental activity.
muscle, increase in skeletal muscle strength, increase in
centration, increase in glycogenolysis in both liver and
glucose from the liver, increase in blood glucose con-
parasympathetic stimulation. Sympathetic stimulation
gallbladder, ureter, urinary bladder, and bronchi, are
entodermal structures, such as the ducts of the liver,
to multiple body functions. In general, most of the
the sympathetic and parasympathetic control systems,
Functions of the Body.
rary loss of all or most arterial pressure.
rial pressure. But
Therefore, the usual effect is a slight decrease in arte-
has virtually no effect on vascular peripheral resistance.
Conversely, moderate parasympathetic stimulation
the same time.
ow, which usually causes a
ow of blood through the peripheral blood vessels.
factors: propulsion of blood by the heart and resistance
The arterial pressure is determined by two
usually far dominant over the beta effects.
vasoconstrictor effects, which, in blood vessels, are
The Autonomic Nervous System and the Adrenal Medulla
Chapter 60
755
Effect of Sympathetic and Parasympathetic Stimulation on Arter-
ial Pressure.
to fl
Sympathetic stimulation increases both propulsion by
the heart and resistance to fl
marked acute increase in arterial pressure but often very
little change in long-term pressure unless the sympa-
thetics stimulate the kidneys to retain salt and water at
via the vagal nerves decreases pumping by the heart but
very strong vagal parasympathetic
stimulation can almost stop or occasionally actually stop
the heart entirely for a few seconds and cause tempo-
Effects of Sympathetic and Parasympathetic Stimulation on Other
Because of the great importance of
they are discussed many times in this text in relation
inhibited by sympathetic stimulation but excited by
also has multiple metabolic effects such as release of
involved in execution of the male and female sexual
Stimulation of the sympathetic nerves to the adrenal
medullae causes large quantities of epinephrine and
norepinephrine to be released into the circulating
about 80 per cent of the secretion is epinephrine and
proportions can change considerably under different
have almost the same effects on the different organs
as the effects caused by direct sympathetic stimulation,
except that the effects last 5 to 10 times as long because
both of these hormones are removed from the blood
and so forth.
Epinephrine causes almost the same effects as those
greater effect on cardiac stimulation than does nor-
parison with much stronger constriction caused by
ence is of special importance because norepinephrine
greatly increases the total peripheral resistance and
the arterial pressure to a lesser extent but increases the
A third difference between the actions of epineph-
rine and norepinephrine relates to their effects on
epinephrine secreted by the adrenal medullae can
increase the metabolic rate of the whole body often to
glucose release into the blood.
causes release of the hormones epinephrine and nor-
effects throughout the body as direct sympathetic
Epinephrine and norepinephrine
are almost always released by the adrenal medullae at
the same time that the different organs are stimulated
directly by the sympathetic nerves and indirectly by
destruction of the direct sympathetic pathways to
the different body organs does not abrogate sympa-
thetic excitation of the organs because norepinephrine
and epinephrine are still released into the circulating
loss of the two adrenal medullae usually has little
effect on the operation of the sympathetic nervous
system because the direct pathways can still perform
nism of sympathetic stimulation provides a safety
Another important value of the adrenal medullae
is the capability of epinephrine and norepinephrine
to stimulate structures of the body that are not
innervated by direct sympathetic fi
the metabolic rate of every cell of the body is increased
even though only a small proportion of all the cells
in the body are innervated directly by sympathetic
fi
because of the lost vascular tone, but over a period of
rst, the blood
tone is lost. At
stellate ganglion is removed, and normal sympathetic
ow lasting a minute or so. Then the
200 ml/min; a test dose of norepinephrine causes only a
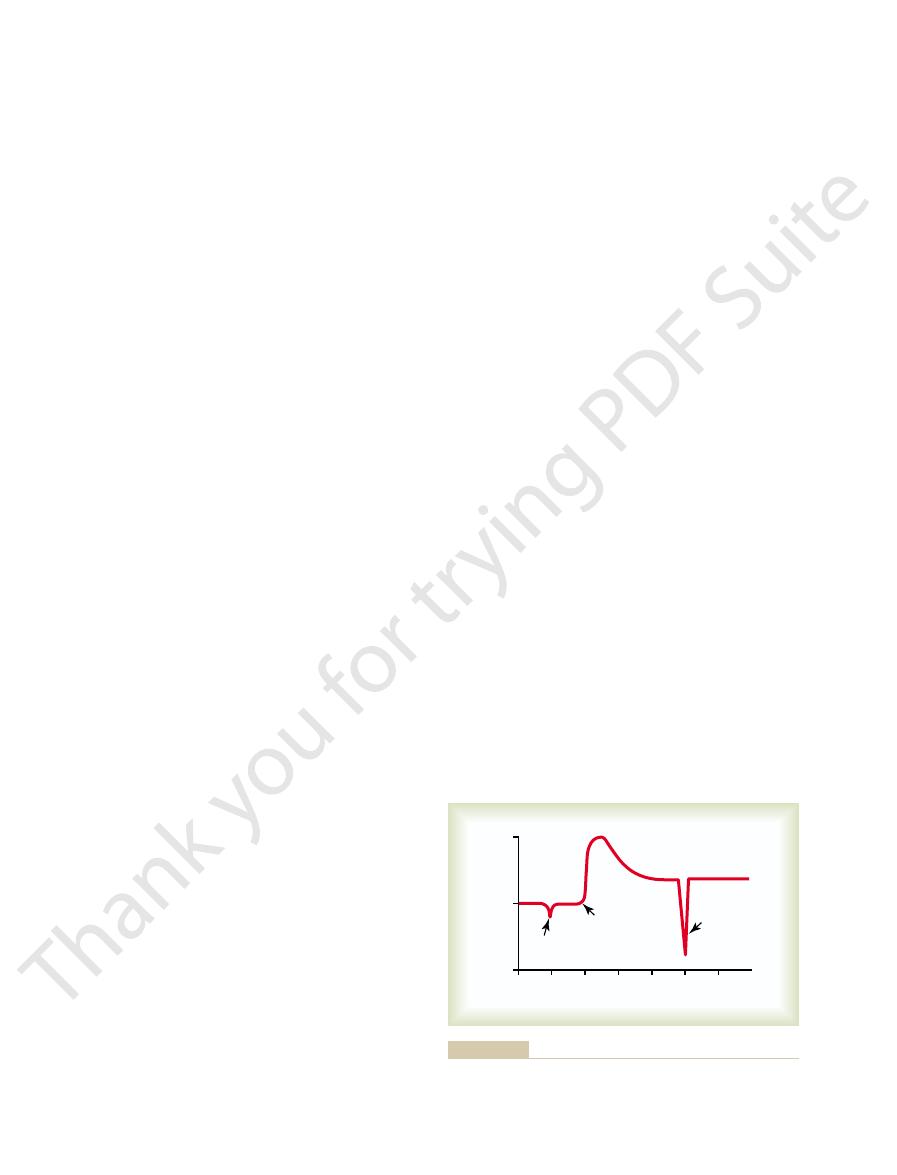
4, showing blood
strated in Figure 60
rine or acetylcholine, respectively. This effect is demon-
parasympathetic nerve is destroyed, the innervated
Organs After Denervation
will still be partially elevated 6 months later.
heart rate to 160 beats per minute in a dog, and this
many months. For instance, loss of parasympathetic
thetic system, the compensation sometimes requires
its normal basal level. However, in the parasympa-
thetic tone is lost. That is, intrinsic compensation soon
This intrinsic tone eventually restores almost normal
bers themselves.
that is, increased tone caused by
days, or weeks,
maximal vasodilation. However, over minutes, hours,
case of the blood vessels, for instance, cutting the sym-
loses its sympathetic or parasympathetic tone. In the
parasympathetic nerve is cut, the innervated organ
Denervation.
Effect of Loss of Sympathetic or Parasympathetic Tone After
the cardiovascular system are removed. Therefore, it is
indeed, enough to maintain the blood pressure almost
of norepinephrine. These quantities are considerable
The normal resting
Tone Caused by Basal Secretion of Epinephrine and Norepi-
nal activity.
increased, thereby promoting increased gastrointesti-
thereby inhibiting gastrointestinal motility, or it can be
required. This tone can be decreased by the brain,
serious constipation,
thus demonstrating that
gastrointestinal tract. Surgical removal of the parasym-
the continual background sympathetic tone, the sym-
normal, the arterioles can be dilated. If it were not for
more; conversely, by decreasing the stimulation below
above normal, these vessels can be constricted even
stricted to about one half their maximum diameter.
. For instance, sympathetic tone nor-
it allows a single nervous
The value of tone is that
activity are known, respectively, as
systems are continually active, and the basal rates of
Normally, the sympathetic and parasympathetic
Parasympathetic “Tone”
20 times per second. This compares with full activation
normal sympathetic or parasympathetic effect, and full
vation of autonomic effectors. In general, only one
low frequency of stimulation is required for full acti-
to Degree of Sympathetic and
Relation of Stimulus Rate
The Nervous System: C. Motor and Integrative Neurophysiology
756
Unit XI
Parasympathetic Effect
A special difference between the autonomic nervous
system and the skeletal nervous system is that only a
nerve impulse every few seconds suffices to maintain
activation occurs when the nerve fibers discharge 10 to
in the skeletal nervous system at 50 to 500 or more
impulses per second.
Sympathetic and
sympathetic tone
and parasympathetic tone.
system both to increase and to decrease the activity of
a stimulated organ
mally keeps almost all the systemic arterioles con-
By increasing the degree of sympathetic stimulation
pathetic system could cause only vasoconstriction,
never vasodilation.
Another interesting example of tone is the back-
ground “tone” of the parasympathetics in the
pathetic supply to most of the gut by cutting the vagus
nerves can cause serious and prolonged gastric and
intestinal “atony” with resulting blockage of much of
the normal gastrointestinal propulsion and consequent
parasympathetic tone to the gut is normally very much
nephrine by the Adrenal Medullae.
rate of secretion by the adrenal medullae is about
0.2
mg/kg/min of epinephrine and about 0.05 mg/kg/min
—
up to normal even if all direct sympathetic pathways to
obvious that much of the overall tone of the sympa-
thetic nervous system results from basal secretion of
epinephrine and norepinephrine in addition to the tone
resulting from direct sympathetic stimulation.
Immediately after a sympathetic or
pathetic nerves results within 5 to 30 seconds in almost
intrinsic tone in the smooth muscle of
the vessels increases—
increased smooth muscle contractile force that is not
the result of sympathetic stimulation but of chemical
adaptations in the smooth muscle fi
vasoconstriction.
Essentially the same effects occur in most other
effector organs whenever sympathetic or parasympa-
develops to return the function of the organ almost to
tone to the heart after cardiac vagotomy increases the
Denervation Supersensitivity of
Sympathetic and Parasympathetic
During the first week or so after a sympathetic or
organ becomes more sensitive to injected norepineph-
–
flow in the
forearm before removal of the sympathetics to be about
slight depression in fl
fi
flow rises markedly
days to weeks the blood flow returns much of the way
back toward normal because of progressive increase in
0
1
2
3
4
5
6
Effect of same
Effect of test dose
400
Normal
of norepinephrine
Stellate
ganglionectomy
test dose of
norepinephrine
Blood flow in arm (ml/min)
200
0
Weeks
Weeks
of the vasculature to norepinephrine.
test dose of norepinephrine before and after sympathectomy,
Effect of sympathectomy on blood flow in the arm, and effect of a
Figure 60–4
showing supersensitization
mainly by the stomach glands. Finally, the rectal emp-
the mouth glands, or in other instances secretion is
increase or decrease its rate of beating. Likewise, other
c. For instance, parasympathetic
response of the sympathetic system, control functions
motor or secretory activity.
gut mainly to the paravertebral ganglia, and then back
not even enter the spinal cord, merely passing from the
whereas cooling causes opposite effects. (3) Many of
causes local vasodilation and enhanced local sweating,
ex responses. For instance, heating a local skin area
organs innervated by the sympathetics. (2) Many
of heat regulation, the sympathetics control sweating
tant of these are the following: (1) During the process
of the sympathetic nervous system. The most impor-
At other times, activation occurs in isolated portions
, which we shall discuss shortly.
by fright or fear or severe pain. The result is a wide-
. This
mass discharge
plete unit, a phenomenon called
many instances, almost all portions of the sympathetic
Organs in Some Instances and
Stimulation of Discrete
ceral functions, all of which are discussed in detail at
ing, blood glucose concentration, and many other vis-
gallbladder emptying, kidney excretion of urine, sweat-
, and then
mainly a parasympathetic func-
sources converge on the sacral cord and, in the male,
stimuli from the sexual organs. Impulses from these
exes, which are ini-
bladder and relaxation of the urinary sphincters,
cord, and this in turn causes re
of the colon; these result in strong peristaltic contrac-
the spinal cord, and a re
of the alimentary canal, sensory impulses initiated by
When fecal matter
the mouth and stomach, causing secretion of digestive
of the brain stem. These in turn transmit signals through
to the vagal, glossopharyngeal, and salivatory nuclei
exes. For instance, the
The uppermost part of
excite the parasympathetics; this allows the arterial
transmitted to the brain stem, where they inhibit the
these become stretched by high pressure, signals are
internal carotid arteries and the arch of the aorta. When
walls of several major arteries, including especially the
exes. Brie
, which is described in Chapter
arterial blood pressure and the heart rate. One of these
Several re
organ systems; to illustrate their importance, a few are
Throughout this text, the functions
autonomic reflexes.
injected into the circulating blood, the effector reaction
tors. Therefore, when a dose of the hormone is now
synapses, a process called
The cause of
Mechanism of Denervation Supersensitivity.
extent in some organs than in others, occasionally
denervation supersensitivity.
epinephrine as previously. This phenomenon is called
before, demonstrating that the blood vessels have
tered, and the blood
Then, another test dose of norepinephrine is adminis-
partially compensating for the loss of sympathetic tone.
intrinsic tone of the vascular musculature itself, thus
The Autonomic Nervous System and the Adrenal Medulla
Chapter 60
757
flow decreases much more than
become about two to four times as responsive to nor-
It occurs in both sympa-
thetic and parasympathetic organs but to far greater
increasing the response more than 10-fold.
denervation supersensitivity is only partially known.
Part of the answer is that the number of receptors in
the postsynaptic membranes of the effector cells
increases—sometimes manyfold—when norepineph-
rine or acetylcholine is no longer released at the
“up-regulation” of the recep-
is vastly enhanced.
Autonomic Reflexes
Many visceral functions of the body are regulated by
of these reflexes are discussed in relation to individual
presented here briefly.
Cardiovascular Autonomic Reflexes.
flexes in the
cardiovascular system help to control especially the
is the baroreceptor reflex
18 along with other cardiovascular refl
fly,
stretch receptors called baroreceptors are located in the
sympathetic impulses to the heart and blood vessels and
pressure to fall back toward normal.
Gastrointestinal Autonomic Reflexes.
the gastrointestinal tract and the rectum are controlled
principally by autonomic refl
smell of appetizing food or the presence of food in
the mouth initiates signals from the nose and mouth
the parasympathetic nerves to the secretory glands of
juices sometimes even before food enters the mouth.
fills the rectum at the other end
stretching the rectum are sent to the sacral portion of
flex signal is transmitted back
through the sacral parasympathetics to the distal parts
tions that cause defecation.
Other Autonomic Reflexes.
Emptying of the urinary bladder
is controlled in the same way as emptying the rectum;
stretching of the bladder sends impulses to the sacral
flex contraction of the
thereby promoting micturition.
Also important are the sexual refl
tiated both by psychic stimuli from the brain and by
result first in erection,
tion
ejaculation, partially a sympathetic
function.
Other autonomic control functions include reflex
contributions to the regulation of pancreatic secretion,
other points in this text.
Mass Stimulation in Other
Instances by the Sympathetic
and Parasympathetic Systems
Sympathetic System Often Responds by Mass Discharge.
In
nervous system discharge simultaneously as a com-
frequently occurs when the hypothalamus is activated
spread reaction throughout the body called the alarm
or stress response
and blood flow in the skin without affecting other
“local reflexes” involving sensory afferent fibers travel
centrally in the peripheral nerves to the sympathetic
ganglia and spinal cord and cause highly localized
refl
the sympathetic reflexes that control gastrointestinal
functions operate by way of nerve pathways that do
to the gut through sympathetic nerves to control
Parasympathetic System Usually Causes Specific Localized
Responses.
In contrast to the common mass discharge
by the parasympathetic system are much more likely
to be highly specifi
cardiovascular reflexes usually act only on the heart to
parasympathetic reflexes cause secretion mainly by
tying reflex does not affect other parts of the bowel to
a major extent.
extent, therefore, the autonomic centers in the brain
tinal activity, and cause bladder emptying. To some
other hypothalamic centers control body temperature,
arterial pressure to more than twice normal. Likewise,
brain stem autonomic control centers. For instance,
functions of the body.
ered to be an autonomic function, it is one of the
discussed in Chapter 41. Although this is not consid-
pontine centers for regulation of respiration, which are
hypothalamus. Conversely, transection immediately
. Indeed, transection of the brain
trolled in the brain stem are arterial pressure, heart rate,
cussed at appropriate points in this text. Suf
of the urinary bladder. Control of each of these is dis-
gastrointestinal peristalsis, and degree of contraction
rate, glandular secretion in the gastrointestinal tract,
autonomic functions such as arterial pressure, heart
5), control different
many special nuclei (Figure 60
the medulla, pons, and mesencephalon, as well as in
Mesencephalic Control of the
Medullary, Pontine, and
s subsequent activities vigorous.
event, the sympathetic alarm reaction makes the
ght or to run. In either
. It is also called the
events ensue immediately. This is called the sympa-
pathetic discharge; most aforementioned sympathetic
ulating the hypothalamus, signals are transmitted
, which is elicited to a great extent by stim-
vated in many emotional states. For instance, in the
The sympathetic system is especially strongly acti-
states of stress: this is called the sympathetic
can excite the sympathetic system, it is
would otherwise be possible. Because either
The sum of these effects permits a person to
8. Increased rate of blood coagulation
7. Increased mental activity
6. Increased muscle strength
5. Increased glycolysis in the liver and in muscle
4. Increased blood glucose concentration
3. Increased rates of cellular metabolism throughout
2. Increased blood
1. Increased arterial pressure
body to perform vigorous muscle activity. Let us sum-
charge
that is, a
When large portions of the sympathetic nervous
Response of the
or
tiate rectal emptying.
Conversely, the bladder emptying re
ex, resulting in simulta-
time. Also, the rectal emptying re
secretion, these two also often occur together, and
parasympathetic functions. For instance, although sali-
Yet there is often association between closely allied
The Nervous System: C. Motor and Integrative Neurophysiology
758
Unit XI
vary secretion can occur independently of gastric
pancreatic secretion frequently occurs at the same
flex often initiates a
urinary bladder emptying refl
neous emptying of both the bladder and the rectum.
flex can help ini-
“Alarm”
“Stress”
Sympathetic Nervous System
system discharge at the same time—
mass dis-
—this increases in many ways the ability of the
marize these ways:
flow to active muscles concurrent
with decreased blood flow to organs such as the
gastrointestinal tract and the kidneys that are not
needed for rapid motor activity
the body
perform far more strenuous physical activity than
mental or
physical stress
frequently said that the purpose of the sympathetic
system is to provide extra activation of the body in
stress
response.
state of rage
downward through the reticular formation of the brain
stem and into the spinal cord to cause massive sym-
thetic alarm reaction
fight or flight
reaction because an animal in this state decides almost
instantly whether to stand and fi
animal’
Autonomic Nervous System
Many neuronal areas in the brain stem reticular sub-
stance and along the course of the tractus solitarius of
–
fice it to
point out here that the most important factors con-
and respiratory rate
stem above the midpontine level allows basal control
of arterial pressure to continue as before but prevents
its modulation by higher nervous centers such as the
below the medulla causes the arterial pressure to fall
to less than one-half normal.
Closely associated with the cardiovascular regula-
tory centers in the brain stem are the medullary and
invol-
untary
Control of Brain Stem Autonomic Centers by Higher Areas.
Signals from the hypothalamus and even from the
cerebrum can affect the activities of almost all the
stimulation in appropriate areas mainly of the poste-
rior hypothalamus can activate the medullary cardio-
vascular control centers strongly enough to increase
increase or decrease salivation and gastrointes-
stem act as relay stations for control activities
Heat control
Parasympathetic
Water
balance
Feeding
control
Hypothalamus
Adenohypophysis
Mamillary body
Respiratory center
Cardiac slowing
Cardiac acceleration
and vasoconstriction
Pneumotaxic center
Urinary bladder control
Pons
Medulla
Sympathetic
Autonomic control areas in the brain stem and hypothalamus.
Figure 60–5
carinic actions.
muscarinic actions, whereas
, have both nicotinic and
methacholine
drugs, such as
nicotinic drugs.
Therefore, drugs
nicotinic type of acetylcholine receptor.
throughout the body.
neurons of both systems, thereby causing at the same
the postganglionic neurons. Furthermore, injected
at their endings, and this acetylcholine in turn stimulates
The
skeletal muscle.
. These drugs
acetylcholine on the muscarinic type of cholinergic effec-
block the action of
and similar drugs, such as
stimuli, and the degree of action also increases.
parasympathetic nerve endings. As a consequence, the
ing rapid destruction of the acetylcholine
These drugs inhibit acetylcholinesterase, thus
, and
pyridostigmine
of acetylcholine at the neuromuscular junction. They
at the parasympathetic endings.They are the same drugs
muscarinic type of cholinergic receptors.
They act directly on the
methacholine.
Two commonly used parasympathomimetic drugs are
drugs.
thetic effects, and they are called
Yet a number of other drugs that are not so rapidly
uids before it can reach all the effector organs.
Drugs That Act on Cholinergic
section, but an important drug for blockade of both
autonomic ganglia. They are discussed in a later
5. Sympathetic activity can be blocked by drugs that
4. The sympathetic
phentolamine.
phenoxybenzamine
Two drugs that cause this effect are
3. The sympathetic
guanethidine.
endings can be blocked. This is caused by
2. Release of norepinephrine from the sympathetic
reserpine.
sympathetic nerve endings can be prevented. The
1. The synthesis and storage of norepinephrine in the
process, as follows:
Drugs That Block Adrenergic Activity.
sympathetic effects.
endings. The released norepinephrine in turn causes the
Their effect is to cause release of norepinephrine
mine.
ephedrine, tyramine,
These drugs include
instead of directly exciting adrenergic effector organs.
Drugs That Cause Release of Norepinephrine from Nerve Endings.
(beta receptors), and
minutes to 2 hours.
as 1 to 2 minutes, whereas the actions of some other
there are many others. They differ from one another in
are also sympathomimetic drugs, and
methoxamine
adrenergic drug. Epinephrine
stimulation. Therefore, norepinephrine is called a
From the foregoing discussion, it is obvious that intra-
Drugs That Act on Adrenergic
Autonomic Nervous System
Pharmacology of the
stomach or duodenum, constipation, heart palpitation,
system. Indeed, some higher areas of the brain can
of the brain stem, and (3) the autonomic nervous
through (1) the hypothalamus, (2) the reticular areas
In Chapters 58 and 59, it is pointed out also that
hypothalamus.
initiated at higher levels of the brain, especially in the
The Autonomic Nervous System and the Adrenal Medulla
Chapter 60
759
many of our behavioral responses are mediated
alter function of the whole autonomic nervous system
or of portions of it strongly enough to cause severe
autonomic-induced disease such as peptic ulcer of the
or even heart attack.
Effector Organs—
Sympathomimetic Drugs
venous injection of norepinephrine causes essentially
the same effects throughout the body as sympathetic
sympathomimetic or
and
the degree to which they stimulate different sympa-
thetic effector organs and in their duration of action.
Norepinephrine and epinephrine have actions as short
commonly used sympathomimetic drugs last for 30
Important drugs that stimulate specific adrenergic
receptors but not others are phenylephrine (alpha
receptors), isoproterenol
albuterol
(only beta
2
receptors).
Certain drugs have an indirect sympathomimetic action
and ampheta-
from its storage vesicles in the sympathetic nerve
Adrenergic activity
can be blocked at several points in the stimulatory
best known drug that causes this effect is
alpha receptors can be blocked.
and
beta receptors can be blocked.
A drug that blocks beta
1
and beta
2
receptors is
propranolol. One that blocks mainly beta
1
receptors is metoprolol.
block transmission of nerve impulses through the
sympathetic and parasympathetic transmission
through the ganglia is hexamethonium.
Effector Organs
Parasympathomimetic Drugs (Cholinergic Drugs).
Acetyl-
choline injected intravenously usually does not cause
exactly the same effects throughout the body as
parasympathetic stimulation because most of the acetyl-
choline is destroyed by cholinesterase in the blood and
body fl
destroyed can produce typical widespread parasympa-
parasympathomimetic
pilocarpine and
Drugs That Have a Parasympathetic Potentiating Effect—Anti-
cholinesterase Drugs.
Some drugs do not have a direct
effect on parasympathetic effector organs but do poten-
tiate the effects of the naturally secreted acetylcholine
as those discussed in Chapter 7 that potentiate the effect
include neostigmine,
ambenonium.
prevent-
liberated at
quantity of acetylcholine increases with successive
Drugs That Block Cholinergic Activity at Effector Organs—
Antimuscarinic Drugs.
Atropine
homatropine and scopolamine,
tor organs
do not affect the nicotinic action
of acetylcholine on the postganglionic neurons or on
Drugs That Stimulate or Block
Sympathetic and Parasympathetic
Postganglionic Neurons
Drugs That Stimulate Autonomic Postganglionic Neurons.
preganglionic neurons of both the parasympathetic and
the sympathetic nervous systems secrete acetylcholine
acetylcholine can also stimulate the postganglionic
time both sympathetic and parasympathetic effects
Nicotine is another drug that can stimulate postgan-
glionic neurons in the same manner as acetylcholine
because the membranes of these neurons all contain the
that cause autonomic effects by stimulating postgan-
glionic neurons are called
Some other
pilocarpine has only mus-
macol Sci 24:414, 2003.
tor function using gene targeting technology. Trends Phar-
Wess J: Novel insights into muscarinic acetylcholine recep-
Sci 998:66, 2003.
nicotinic acetylcholine receptor assembly. Ann N Y Acad
Wanamaker CP, Christianson JC, Green WN: Regulation of
in vertebrates. Physiol Rev 79:855, 1999.
Taylor EW, Jordan D, Coote JH: Central control of the car-
Annu Rev Neurosci 25:433, 2002.
Saper CB: The central autonomic nervous system: conscious
term blood pressure regulation. Am J Hypertens 14:147S,
Lohmeier TE: The sympathetic nervous system and long-
Circulation 101:1634, 2000.
cardiac beta-adrenergic receptors, and heart failure.
Lefkowitz RJ, Rockman HA, Koch WJ: Catecholamines,
naling. Annu Rev Physiol 62:237, 2000.
Koch WJ, Lefkowitz RJ, Rockman HA: Functional conse-
550:337, 2003.
micity and neural control of gut smooth muscle. J Physiol
Hirst GD, Ward SM: Interstitial cells: involvement in rhyth-
tens 14:103S, 2001.
of leptin and sympathetic nervous system. Am J Hyper-
Hall JE, Hildebrandt DA, Kuo J: Obesity hypertension: role
Intern Med 137:753, 2002.
clinical disorders of the autonomic nervous system. Ann
Goldstein DS, Robertson D, Esler M, et al: Dysautonomias:
37:69, 2003.
Goldstein DS: Catecholamines and stress. Endocr Regul
177:237, 2003.
of peripheral vasomotor pathways. Acta Physiol Scand
Gibbins IL, Jobling P, Morris JL: Functional organization
Physiol Rev 77:75, 1997.
DiBona GF, Kopp UC: Neural control of renal function.
motor tone. Acta Physiol Scand 177:209, 2003.
Dampney RA, Horiuchi J, Tagawa T, et al: Medullary and
Pharmacol Sci 25:317, 2004.
receptors and the regulation of neuronal signalling. Trends
Dajas-Bailador F, Wonnacott S: Nicotinic acetylcholine
284:G357, 2003.
to the gut. Am J Physiol Gastrointest Liver Physiol
ex? IV. Current concepts of vagal efferent projections
derer: what
Chang HY, Mashimo H, Goyal RK: Musings on the wan-
tractus solitarius. Ann N Y Acad Sci 940:132, 2001
Andresen MC, Doyle MW, Jin YH, Bailey TW: Cellular
sure in many patients with hypertension, but these drugs
the effects of parasympathetic blockade. The ganglionic
the parasympathetic systems simultaneously. They are
These drugs block acetylcholine stimulation of
, and
neurons to the postganglionic neurons, including
trointestinal activity and, sometimes, slowing of the
pathetic postganglionic neurons at the same time,
The Nervous System: C. Motor and Integrative Neurophysiology
760
Unit XI
Nicotine excites both the sympathetic and parasym-
resulting in strong sympathetic vasoconstriction in the
abdominal organs and limbs but at the same time result-
ing in parasympathetic effects such as increased gas-
heart.
Ganglionic Blocking Drugs.
Many important drugs block
impulse transmission from the autonomic preganglionic
tetraethyl ammonium ion, hexamethonium ion
pen-
tolinium.
the postganglionic neurons in both the sympathetic and
often used for blocking sympathetic activity but seldom
for blocking parasympathetic activity because their
effects of sympathetic blockade usually far overshadow
blocking drugs especially can reduce the arterial pres-
are not very useful clinically because their effects are
difficult to control.
References
mechanisms of baroreceptor integration at the nucleus
’s new in our understanding of vago-vagal
refl
supramedullary mechanisms regulating sympathetic vaso-
quences of altering myocardial adrenergic receptor sig-
2001.
visceral perception and autonomic pattern generation.
diovascular and respiratory systems and their interactions
