; therefore
be digested. Also, chewing aids the digestion of food for still another simple
Chewing is important for digestion of all foods, but especially important for
another time; this is repeated again and again.
which inhibits the jaw muscles once again, allowing the jaw to drop and rebound
teeth, but it also compresses the bolus again against the linings of the mouth,
contraction. This automatically raises the jaw to cause closure of the
to drop. The drop in turn initiates a stretch reflex of the jaw muscles that leads
tiates reflex inhibition of the muscles of mastication, which allows the lower jaw
explained as follows: The presence of a bolus of food in the mouth at first ini-
, which may be
chewing reflex
taste and smell can often cause chewing.
thalamus, amygdala, and even the cerebral cortex near the sensory areas for
cause rhythmical chewing movements. Also, stimulation of areas in the hypo-
stem. Stimulation of specific reticular areas in the brain stem taste centers will
fifth cranial nerve, and the chewing process is controlled by nuclei in the brain
as 55 pounds on the incisors and 200 pounds on the molars.
viding a strong cutting action and the posterior teeth (molars), a grinding action.
The teeth are admirably designed for chewing, the anterior teeth (incisors) pro-
swallowing
mechanics of ingestion, especially
tion of the body. The current discussion of food ingestion is confined to the
tional supply for the body; they are discussed in Chapter 71 in relation to nutri-
. These mechanisms in themselves are extremely
. The type of food that a person preferentially seeks
The amount of food that a person ingests is determined principally by intrinsic
The purpose of this chapter is to discuss these movements, especially the auto-
too rapidly, not too slowly.
each of these so that they will occur optimally, not
processing, multiple automatic nervous and hor-
provided. Yet because the requirements for mixing
tract is critical. Also, appropriate mixing must be
tary tract, the time that it remains in each part of the
For food to be processed optimally in the alimen-
Food in the Alimentary Tract
C
H
A
P
T
E
R
6
3
781
Propulsion and Mixing of
and propulsion are quite different at each stage of
monal feedback mechanisms control the timing of
matic mechanisms of this control.
Ingestion of Food
desire for food called hunger
is determined by appetite
important automatic regulatory systems for maintaining an adequate nutri-
mastication and
.
Mastication (Chewing)
All the jaw muscles working together can close the teeth with a force as great
Most of the muscles of chewing are innervated by the motor branch of the
Much of the chewing process is caused by a
to rebound
most fruits and raw vegetables because these have indigestible cellulose mem-
branes around their nutrient portions that must be broken before the food can
reason: Digestive enzymes act only on the surfaces of food particles
,
occurring in less than 2 seconds.
food into the upper esophagus, the entire process
agus is opened, and a fast peristaltic wave initiated by
stage of swallowing: The trachea is closed, the esoph-
To summarize the mechanics of the pharyngeal
by peristalsis into the esophagus.
inferior pharyngeal areas, which propels the food
the entire muscular wall of the pharynx contracts,
5. Once the larynx is raised and the
epiglottis rather than over its surface; this adds
glottis out of the main stream of food flow, so
into the esophagus during respiration. The
contracted, thereby preventing air from going
Between swallows, this sphincter remains strongly
posterior pharynx into the upper esophagus.
) relaxes, thus
of the esophageal muscular wall, called the
At the same time, the upper 3 to 4 centimeters
up and enlarges the opening to the esophagus.
4. The upward movement of the larynx also pulls
cords. Destruction of the vocal cords or of the
of the vocal cords, but the epiglottis helps to
trachea. Most essential is the tight approximation
of the larynx. All these effects acting together
prevent upward movement of the epiglottis, cause
and anteriorly by the neck muscles. These actions,
approximated, and the larynx is pulled upward
3. The vocal cords of the larynx are strongly
the esophagus.
swallowing lasts less than 1 second, any large
sufficiently to pass with ease. Because this stage of
action, allowing food that has been masticated
posterior pharynx. This slit performs a selective
other. In this way, these folds form a sagittal
2. The palatopharyngeal folds on each side of the
nasal cavities.
posterior nares, to prevent reflux of food into the
1. The soft palate is pulled upward to close the
pillars, and impulses from these pass to the brain stem
opening of the pharynx, especially on the tonsillar
epithelial swallowing receptor areas
enters the posterior mouth and pharynx, it stimulates
Pharyngeal Stage of Swallowing.
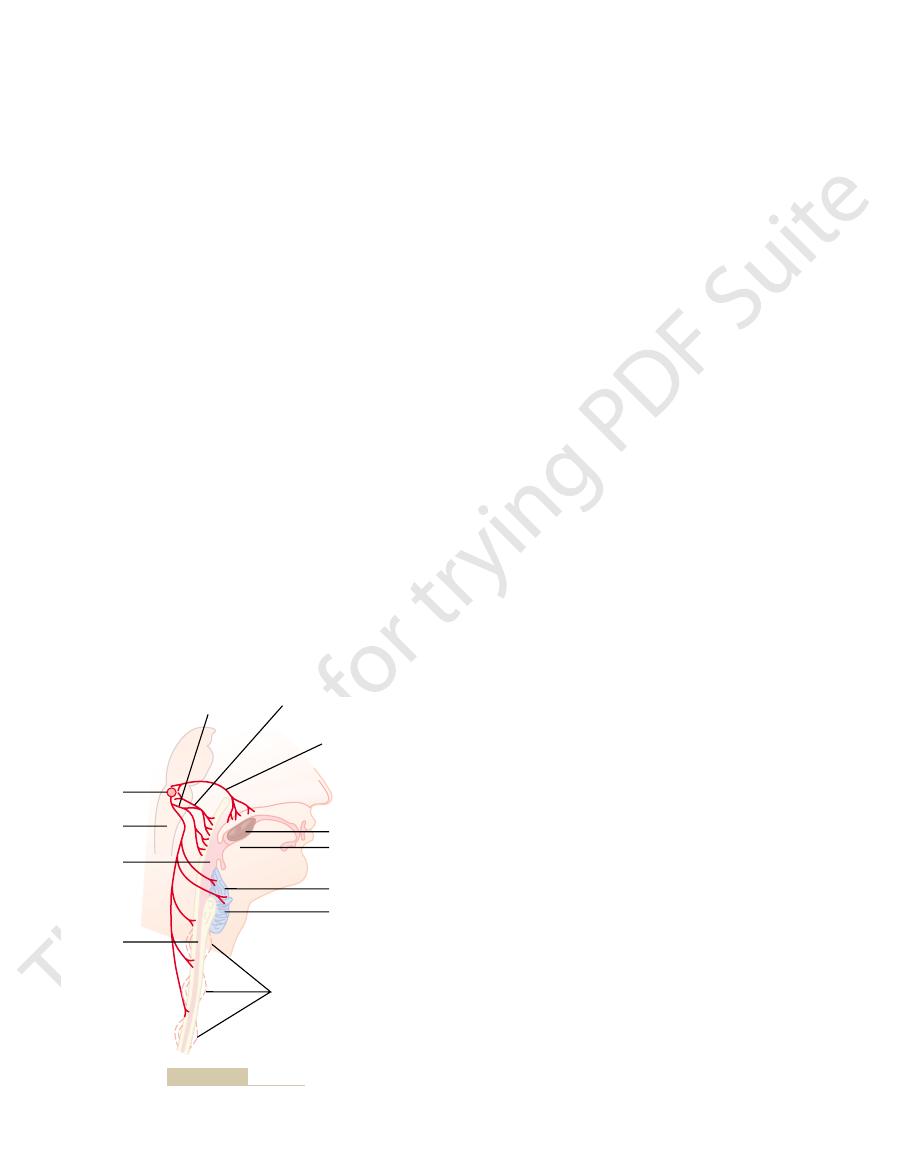
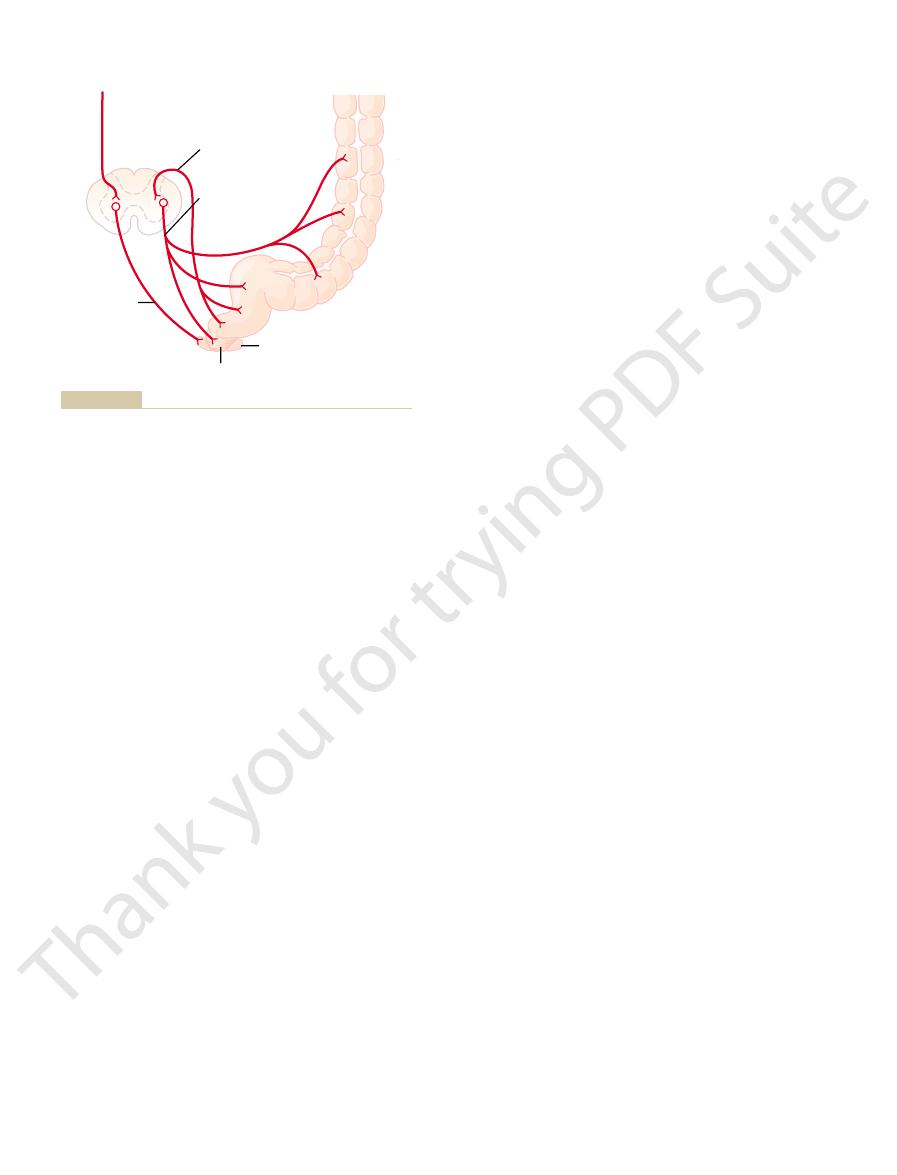
Figure 63–1. From here on, swallowing becomes
upward and backward against the palate, as shown in
swallowing, it is “voluntarily” squeezed or rolled pos-
When the food is ready for
Voluntary Stage of Swallowing.
, another invol-
esophagus; and (3) an
, which is involuntary and consti-
, which initiates the swallowing process; (2)
In general, swallowing can be divided into (1) a
promised because of swallowing.
swallowing. The pharynx is converted for only a few
Swallowing is a complicated mechanism, principally
emptied from the stomach into the small intestine,
consistency prevents excoriation of the gastrointesti-
In addition, grinding the food to a very fine particulate
total surface area exposed to the digestive secretions.
782
Unit XII
Gastrointestinal Physiology
the rate of digestion is absolutely dependent on the
nal tract and increases the ease with which food is
then into all succeeding segments of the gut.
Swallowing (Deglutition)
because the pharynx subserves respiration as well as
seconds at a time into a tract for propulsion of food.
It is especially important that respiration not be com-
vol-
untary stage
a pharyngeal stage
tutes passage of food through the pharynx into the
esophageal stage
untary phase that transports food from the pharynx to
the stomach.
teriorly into the pharynx by pressure of the tongue
entirely—or almost entirely—automatic and ordinar-
ily cannot be stopped.
As the bolus of food
all around the
to initiate a series of automatic pharyngeal muscle
contractions as follows:
pharynx are pulled medially to approximate each
slit through which the food must pass into the
object is usually impeded too much to pass into
combined with the presence of ligaments that
the epiglottis to swing backward over the opening
prevent passage of food into the nose and
prevent food from ever getting as far as the vocal
muscles that approximate them can cause
strangulation.
upper esophageal sphincter (also called the
pharyngoesophageal sphincter
allowing food to move easily and freely from the
upward movement of the larynx also lifts the
that the food mainly passes on each side of the
still another protection against entry of food into
the trachea.
pharyngoesophageal sphincter becomes relaxed,
beginning in the superior part of the pharynx,
then spreading downward over the middle and
the nervous system of the pharynx forces the bolus of
Esophagus
Vagus
Glossopharyngeal
nerve
Trigeminal nerve
Bolus of food
Uvula
Epiglottis
Vocal cords
Peristalsis
Pharynx
Medulla
Swallowing
center
Figure 63–1
Swallowing mechanism.

esophagus except under very abnormal conditions.
action of gastric secretions. Fortunately, the tonic con-
agus, is not capable of resisting for long the digestive
mucosa, except in the lower one eighth of the esoph-
contain many proteolytic enzymes. The esophageal
The stomach secretions are highly acidic and
achalasia
satisfactorily, resulting in a condition called
into the stomach. Rarely, the sphincter does not relax
esophageal sphincter ahead of the peristaltic wave,
agus, there is “receptive relaxation” of the lower
the esophagus, which normally remains relaxed. When
of about 30 mm Hg, in contrast to the midportion of
. This
, also called the
lower esophageal sphinc-
juncture with the stomach, the esophageal circular
agus, extending upward about 3 centimeters above its
Function of the Lower Esophageal Sphincter (Gastro-
extent, even the duodenum become relaxed as this
Furthermore, the entire stomach and, to a lesser
myenteric inhibitory neurons, precedes the peristalsis.
stomach, a wave of relaxation, transmitted through
When the
reflex, food fed by tube or in some other way into the
without support from the vagal reflexes. Therefore,
the esophagus are cut, the myenteric nerve plexus of
myenteric nervous system. When the vagus nerves to
, but this portion of
vagus nerves. In the lower two thirds of the esophagus,
. Therefore, the
The musculature of the pharyngeal wall and upper
stomach. The secondary peristaltic waves are initiated
the esophagus itself by the retained food; these waves
stomach all the food that has entered the esophagus,
itself, in about 5 to 8 seconds, because of the additional
Food swallowed by a person who is in the upright posi-
the pharynx to the stomach in about 8 to 10 seconds.
stage of swallowing. This wave passes all the way from
. Primary peristalsis is simply continuation of
The esophagus normally exhibits two types of peri-
the stomach, and its movements are organized specif-
The esophagus functions
Esophageal Stage of Swallowing.
short time that it is hardly noticeable.
is talking, swallowing interrupts respiration for such a
allow swallowing to proceed. Yet, even while a person
this time, halting respiration at any point in its cycle to
piratory cycle. The swallowing center specifically
usually occurs in less than 6 seconds, thereby inter-
The entire pharyngeal stage of swallowing
Effect of the Pharyngeal Stage of Swallowing on Res-
mouth, which in turn excites involuntary pharyngeal
principally a reflex act. It is almost always initiated by
In summary, the pharyngeal stage of swallowing is
cervical nerves.
ing are transmitted successively by the 5th, 9th, 10th,
The motor impulses from the swallowing center to
swallowing center
remains constant from one swallow to the next. The
to the next, and the timing of the entire cycle also
medulla and lower portion of the pons. The sequence
The successive stages of the swallowing process
, which receives essentially all sensory impulses
pillars. Impulses are transmitted from these areas
opening, with greatest sensitivity on the tonsillar
The most sensitive tactile areas of the posterior
Nervous Initiation of the Pharyngeal Stage of Swallow-
Propulsion and Mixing of Food in the Alimentary Tract
Chapter 63
783
ing.
mouth and pharynx for initiating the pharyngeal stage
of swallowing lie in a ring around the pharyngeal
through the sensory portions of the trigeminal and
glossopharyngeal nerves into the medulla oblongata,
either into or closely associated with the tractus soli-
tarius
from the mouth.
are then automatically initiated in orderly sequence
by neuronal areas of the reticular substance of the
of the swallowing reflex is the same from one swallow
areas in the medulla and lower pons that control
swallowing are collectively called the deglutition or
.
the pharynx and upper esophagus that cause swallow-
and 12th cranial nerves and even a few of the superior
voluntary movement of food into the back of the
sensory receptors to elicit the swallowing reflex.
piration.
rupting respiration for only a fraction of a usual res-
inhibits the respiratory center of the medulla during
primarily to conduct food rapidly from the pharynx to
ically for this function.
staltic movements: primary peristalsis and secondary
peristalsis
the peristaltic wave that begins in the pharynx and
spreads into the esophagus during the pharyngeal
tion is usually transmitted to the lower end of the
esophagus even more rapidly than the peristaltic wave
effect of gravity pulling the food downward.
If the primary peristaltic wave fails to move into the
secondary peristaltic waves result from distention of
continue until all the food has emptied into the
partly by intrinsic neural circuits in the myenteric
nervous system and partly by reflexes that begin in the
pharynx and are then transmitted upward through
vagal afferent fibers to the medulla and back again to
the esophagus through glossopharyngeal and vagal
efferent nerve fibers.
third of the esophagus is striated muscle
peristaltic waves in these regions are controlled by
skeletal nerve impulses from the glossopharyngeal and
the musculature is smooth muscle
the esophagus is also strongly controlled by the vagus
nerves acting through connections with the esophageal
the esophagus becomes excitable enough after several
days to cause strong secondary peristaltic waves even
even after paralysis of the brain stem swallowing
esophagus still passes readily into the stomach.
Receptive Relaxation of the Stomach.
esophageal peristaltic wave approaches toward the
wave reaches the lower end of the esophagus and
thus are prepared ahead of time to receive the food
propelled into the esophagus during the swallowing
act.
esophageal Sphincter).
At the lower end of the esoph-
muscle functions as a broad
ter
gastroesophageal sphincter
sphincter normally remains tonically constricted with
an intraluminal pressure at this point in the esophagus
a peristaltic swallowing wave passes down the esoph-
which allows easy propulsion of the swallowed food
,
which is discussed in Chapter 66.
striction of the lower esophageal sphincter helps to
prevent significant reflux of stomach contents into the

is that of a murky semifluid or paste.
digestion that has occurred. The appearance of chyme
water, and stomach secretions and on the degree of
The degree of fluidity of the chyme leaving the
chyme
oughly mixed with the stomach secretions, the result-
“retropulsion,” is an exceedingly important mixing
combined with this upstream squeezing action, called
pylorus. Thus, the moving peristaltic constrictive ring,
ring toward the body of the stomach, not through the
through the pylorus. Therefore, most of the antral con-
often contracts, which further impedes emptying
wave approaches the pylorus, the pyloric muscle itself
with each peristaltic wave. Also, as each peristaltic
contents in the antrum. Yet the opening of the pylorus
wall toward the pylorus, it digs deeply into the food
These constrictor rings also play an important role
higher pressure toward the pylorus.
stomach into the antrum, they become more intense,
waves” that occur spontaneously in the stomach wall.
cussed in Chapter 62, consisting of electrical “slow
, which was dis-
once every 15 to 20 seconds. These waves are initiated
, begin in the mid- to upper portions of
, called
stomach, weak peristaltic
surface of the stomach. As long as food is in the
strip on the lesser curvature of the stomach. These
, which are present in almost the entire
The digestive juices of the stomach are secreted by
Rhythm of the Stomach Wall
Mixing and Propulsion of Food in the
the completely relaxed stomach of 0.8 to 1.5 liters. The
the wall bulges progressively outward, accommodating
a “vagovagal reflex” from the stomach to the brain
stomach. Normally, when food stretches the stomach,
of the food in the orad portion of the stomach, the
As food enters the stomach, it forms concentric circles
Storage Function of the Stomach
thirds of the body, and (2) the “caudad” portion, com-
(1) the “orad” portion, comprising about the first two
Physiologically, it is more appropriately divided into
into two major parts: (1) the
stomach. Anatomically, the stomach is usually divided
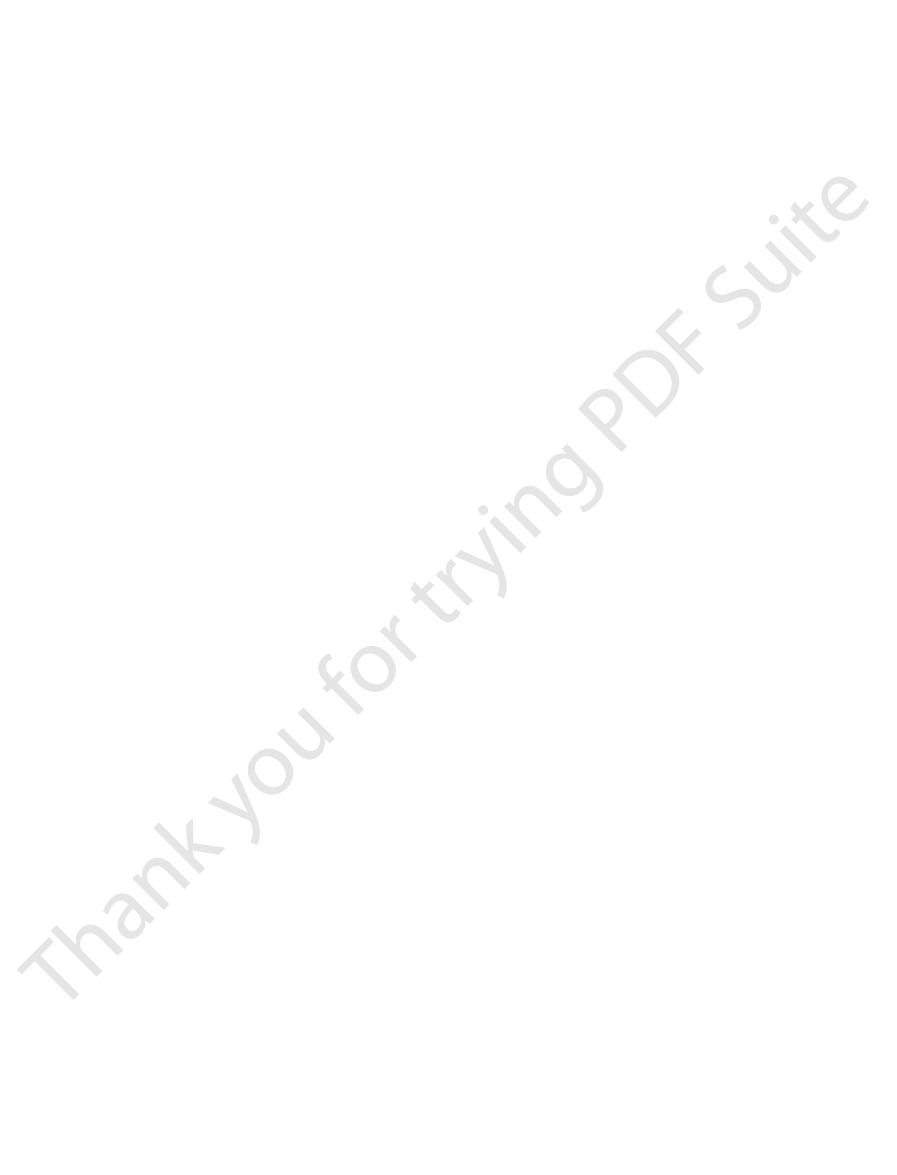
Figure 63–2 shows the basic anatomy of the
proper digestion and absorption by the small intestine.
; and (3) slow emptying of the chyme from the
chyme
intestinal tract; (2) mixing of this food with gastric
be processed in the stomach, duodenum, and lower
The motor functions of the stomach are threefold: (1)
esophagus.
or breathed hard, we might expel stomach acid into the
esophagus. Otherwise, every time we walked, coughed,
point. Thus, this valvelike closure of the lower esoph-
that extends slightly into the stomach. Increased intra-
like Closure of the Distal End of the Esophagus.
Additional Prevention of Esophageal Reflux by Valve-
784
Unit XII
Gastrointestinal Physiology
Another factor that helps to prevent reflux is a valve-
like mechanism of a short portion of the esophagus
abdominal pressure caves the esophagus inward at this
agus helps to prevent high intra-abdominal pressure
from forcing stomach contents backward into the
Motor Functions of the
Stomach
storage of large quantities of food until the food can
secretions until it forms a semifluid mixture called
stomach into the small intestine at a rate suitable for
body and (2) the antrum.
prising the remainder of the body plus the antrum.
newest food lying closest to the esophageal opening
and the oldest food lying nearest the outer wall of the
stem and then back to the stomach reduces the tone
in the muscular wall of the body of the stomach so that
greater and greater quantities of food up to a limit in
pressure in the stomach remains low until this limit is
approached.
Stomach—The Basic Electrical
gastric glands
wall of the body of the stomach except along a narrow
secretions come immediately into contact with that
portion of the stored food lying against the mucosal
constrictor waves
mixing waves
the stomach wall and move toward the antrum about
by the gut wall basic electrical rhythm
As the constrictor waves progress from the body of the
some becoming extremely intense and providing pow-
erful peristaltic action potential–driven constrictor
rings that force the antral contents under higher and
in mixing the stomach contents in the following way:
Each time a peristaltic wave passes down the antral
is still small enough that only a few milliliters or less
of antral contents are expelled into the duodenum
tents are squeezed upstream through the peristaltic
mechanism in the stomach.
Chyme.
After food in the stomach has become thor-
ing mixture that passes down the gut is called
.
stomach depends on the relative amounts of food,
Duodenum
Antrum
Fundus
Esophagus
Cardia
Angular
notch
Pyloric
sphincter
Rugae
Body
Pylorus
Figure 63–2
Physiologic anatomy of the stomach.

the vagus nerves all the way to the brain stem, where
stomach, and (3) probably to a slight extent through
in the gut wall, (2) through extrinsic nerves that go to
ated by three routes: (1) directly from the duodenum
denum becomes too much. These reflexes are medi-
When food enters the duodenum, multiple
Inhibitory Effect of Enterogastric Nervous Reflexes from the
Powerful Duodenal Factors That Inhibit
Thus, it, too, probably promotes stomach emptying.
it seems to enhance the activity of the pyloric pump.
functions in the body of the stomach. Most important,
acidic gastric juice by the stomach glands. Gastrin also
This has potent effects to cause secretion of highly
Chapter 64, we shall see that stomach wall stretch and
inhibit the pylorus.
However, stretching of the stomach wall does elicit
in the usual normal range of volume, the increase
stomach that causes the increased emptying because,
tying from the stomach. But this increased emptying
Effect of Gastric Food Volume on Rate of Emptying.
Gastric Factors That Promote Emptying
in the small intestine.
potent of the signals, controlling the emptying of
However, the duodenum provides by far the more
The rate at which the stomach empties is regulated by
Regulation of Stomach Emptying
the duodenum, as discussed shortly.
sistency. The degree of constriction of the pylorus is
duodenum with ease. Conversely, the constriction
sphincter, the pylorus usually is open enough for water
pyloric sphincter
tracted almost all the time. Therefore, the pyloric cir-
stomach antrum, and it remains slightly tonically con-
. Here the
pylorus
The
action called the “pyloric pump.”
causing mixing in the stomach, also provide a pumping
duodenum. Thus, the peristaltic waves, in addition to
When pyloric tone is normal, each strong peristaltic
mixing type of peristaltic waves.
often create 50 to 70 centimeters of water pressure,
the antrum. These intense peristaltic contractions
stomach, gradually pinching off the food in the body
progressively more and more empty, these constric-
can cause stomach emptying. As the stomach becomes
strong peristaltic, very tight ringlike constrictions that
stomach, the contractions become intense, beginning
cause mixing of food and gastric secretions. However,
Most of the time, the rhythmical
to passage of chyme at the pylorus.
contractions in the stomach antrum. At the same time,
succeeding days.
ingestion of food; in starvation, they reach their great-
. Hunger pangs
of the stomach, called
sugar. When hunger contractions occur in the stomach,
person’s having lower than normal levels of blood
testinal tonus; they are also greatly increased by the
Hunger contractions are most intense in young,
contraction that sometimes lasts for 2 to 3 minutes.
strong, they often fuse to cause a continuing tetanic
When the successive contractions become extremely
for several hours or more. They are rhythmical
when the stomach has been
, often occurs
another type of intense contractions, called
Propulsion and Mixing of Food in the Alimentary Tract
Chapter 63
785
Hunger Contractions.
Besides the peristaltic contractions
that occur when food is present in the stomach,
hunger
contractions
empty
peristaltic contractions in the body of the stomach.
healthy people who have high degrees of gastroin-
the person sometimes experiences mild pain in the pit
hunger pangs
usually do not begin until 12 to 24 hours after the last
est intensity in 3 to 4 days and gradually weaken in
Stomach Emptying
Stomach emptying is promoted by intense peristaltic
emptying is opposed by varying degrees of resistance
Intense Antral Peristaltic Contractions During Stomach Empty-
ing—“Pyloric Pump.”
stomach contractions are weak and function mainly to
for about 20 per cent of the time while food is in the
in midstomach and spreading through the caudad
stomach no longer as weak mixing contractions but as
tions begin farther and farther up the body of the
of the stomach and adding this food to the chyme in
which is about six times as powerful as the usual
wave forces up to several milliliters of chyme into the
Role of the Pylorus in Controlling Stomach Emptying.
distal opening of the stomach is the
thickness of the circular wall muscle becomes 50 to 100
per cent greater than in the earlier portions of the
cular muscle is called the
.
Despite normal tonic contraction of the pyloric
and other fluids to empty from the stomach into the
usually prevents passage of food particles until they
have become mixed in the chyme to almost fluid con-
increased or decreased under the influence of nervous
and humoral reflex signals from both the stomach and
signals from both the stomach and the duodenum.
chyme into the duodenum at a rate no greater than the
rate at which the chyme can be digested and absorbed
Increased
food volume in the stomach promotes increased emp-
does not occur for the reasons that one would expect.
It is not increased storage pressure of the food in the
in volume does not increase the pressure much.
local myenteric reflexes in the wall that greatly accen-
tuate activity of the pyloric pump and at the same time
Effect of the Hormone Gastrin on Stomach Emptying.
In
the presence of certain types of foods in the stomach—
particularly digestive products of meat—elicit release
of a hormone called gastrin from the antral mucosa.
has mild to moderate stimulatory effects on motor
Stomach Emptying
Duodenum.
nervous reflexes are initiated from the duodenal wall
that pass back to the stomach to slow or even stop
stomach emptying if the volume of chyme in the duo-
to the stomach through the enteric nervous system
the prevertebral sympathetic ganglia and then back
through inhibitory sympathetic nerve fibers to the
they inhibit the normal excitatory signals transmitted
minute. The contractions cause “segmentation” of the
tended with chyme, stretching of the intestinal wall
When a portion of the small intestine becomes dis-
usual classification of these processes is the following.
least some degree of both mixing and propulsion. The
great extent, this separation is artificial because essen-
. To a
where in the gastrointestinal tract, can be divided into
The movements of the small intestine, like those else-
process.
ing. In this way, the rate of stomach emptying is limited
protein or fat, is hypotonic or hypertonic, or is irritat-
excessively acidic, contains too much unprocessed
back reflexes and hormonal feedback by CCK. These
gastrin on stomach peristalsis. Probably the more
Summary of the Control of Stomach Emptying
especially acidic or fatty chyme, enter the duodenum
gastric emptying when excess quantities of chyme,
In summary, hormones, especially CCK, can inhibit
elsewhere in this text, especially in Chapter 64 in rela-
These hormones are discussed at greater length
stimulate secretion of insulin by the pancreas.
inhibit gastric motility under some conditions, its effect
extent to carbohydrates as well. Although GIP does
response mainly to fat in the chyme, but to a lesser
weak effect of decreasing gastrointestinal motility.
stomach through the pylorus. GIP has a general but
. Secretin is released mainly from the duodenal
response to fatty substances in the chyme. This
cholecystokinin (CCK)
The most potent appears to be
feedback inhibition of the stomach is not fully clear.
other foods.
the pyloric sphincter. These effects are important
stomach, where they inhibit the pyloric pump and at
the epithelial cells or in some other way. In turn, the
epithelium, either by binding with “receptors” on
On entering the duodenum, the fats extract several
degree.
mainly fats entering the duodenum, although other
released from the upper intestine do so as well. The
stomach inhibit stomach emptying, but hormones
tinal contents.
intestine is prevented, thereby also preventing rapid
cially hypertonic) elicit the inhibitory reflexes. Thus,
Finally, either hypotonic or hypertonic fluids (espe-
intestine.
stomach emptying, sufficient time is ensured for ade-
inhibitory enterogastric reflexes; by slowing the rate of
creatic and other secretions.
about 3.5 to 4, the reflexes frequently block further
vated within as little as 30 seconds. For instance, when-
duodenal chyme, and they often become strongly acti-
The enterogastric inhibitory reflexes are especially
the chyme, especially breakdown products of
5. The presence of certain breakdown products in
4. The degree of osmolality of the chyme
3. The degree of acidity of the duodenal chyme
2. The presence of any degree of irritation of the
1. The degree of distention of the duodenum
The types of factors that are continually monitored
pyloric sphincter.
contractions, and second, they increase the tone of the
they strongly inhibit the “pyloric pump” propulsive
reflexes have two effects on stomach emptying: first,
to the stomach through the vagi. All these parallel
786
Unit XII
Gastrointestinal Physiology
in the duodenum and that can initiate enterogastric
inhibitory reflexes include the following:
duodenal mucosa
proteins and perhaps to a lesser extent of fats
sensitive to the presence of irritants and acids in the
ever the pH of the chyme in the duodenum falls below
release of acidic stomach contents into the duodenum
until the duodenal chyme can be neutralized by pan-
Breakdown products of protein digestion also elicit
quate protein digestion in the duodenum and small
too rapid flow of nonisotonic fluids into the small
changes in electrolyte concentrations in the whole-
body extracellular fluid during absorption of the intes-
Hormonal Feedback from the Duodenum Inhibits Gastric Emp-
tying—Role of Fats and the Hormone Cholecystokinin.
Not
only do nervous reflexes from the duodenum to the
stimulus for releasing these inhibitory hormones is
types of foods can increase the hormones to a lesser
different hormones from the duodenal and jejunal
hormones are carried by way of the blood to the
the same time increase the strength of contraction of
because fats are much slower to be digested than most
Precisely which hormones cause the hormonal
,
which is released from the mucosa of the jejunum in
hormone acts as an inhibitor to block increased
stomach motility caused by gastrin.
Other possible inhibitors of stomach emptying are
the hormones secretin and gastric inhibitory peptide
(GIP)
mucosa in response to gastric acid passed from the
GIP is released from the upper small intestine in
at physiologic concentrations is probably mainly to
tion to control of gallbladder emptying and control of
rate of pancreatic secretion.
from the stomach.
Emptying of the stomach is controlled only to a mod-
erate degree by stomach factors such as the degree
of filling in the stomach and the excitatory effect of
important control of stomach emptying resides in
inhibitory feedback signals from the duodenum,
including both enterogastric inhibitory nervous feed-
feedback inhibitory mechanisms work together to
slow the rate of emptying when (1) too much chyme
is already in the small intestine or (2) the chyme is
to that amount of chyme that the small intestine can
Movements of the
Small Intestine
mixing contractions and propulsive contractions
tially all movements of the small intestine cause at
Mixing Contractions (Segmentation
Contractions)
elicits localized concentric contractions spaced at
intervals along the intestine and lasting a fraction of a

folds to appear in the intestinal mucosa. In addition,
The
minutes, sweeping the contents of the intestine into the
the gut wall itself. The powerful peristaltic contractions
. This is initiated
peristalsis, called the
infectious diarrhea, can cause both powerful and rapid
intestinal mucosa, as occurs in some severe cases of
intestine is normally weak, intense irritation of the
these two classifications.
the food down the intestine. The difference between
seconds at a time, often also travel 1 centimeter or so
mentation movements, although lasting for only a few
The seg-
valve into the cecum of the large intestine.
hours until the person eats another meal; at that time,
cal valve, the chyme is sometimes blocked for several
chyme enters the duodenum. On reaching the ileoce-
intestine; and this process intensifies as additional
stalsis, this immediately spreads the chyme along the
chyme along the intestinal mucosa. As the chyme
The function of the peristaltic waves in the small
controlling motility is still questionable.
inhibit small intestinal motility. The physio-
phases of food processing. Conversely,
, all of which enhance
, and
also affect peristalsis. They include
small intestinal peristalsis, several hormonal factors
intestine.
the duodenal wall, but also by a so-called
after a meal. This is caused partly by the beginning
Control of Peristalsis by Nervous and Hormonal Signals.
the ileocecal valve.
averages only 1 cm/min. This means that 3 to 5 hours
movement of the chyme is very slow, so slow in fact
very rarely farther than 10 centimeters, so that forward
usually die out after traveling only 3 to 5 centimeters,
minal intestine. They normally are very weak and
move toward the anus at a velocity of 0.5 to 2.0 cm/sec,
can occur in any part of the small intestine, and they
. These
plexus.
muscle itself that cause the segmentation contractions,
fore, even though it is the slow waves in the smooth
nervous system is blocked by the drug atropine. There-
The segmentation contractions become exceedingly
is usually 8 to 9 contractions per minute.
ulation. In the terminal ileum, the maximum frequency
contractions in these areas is also about 12 per minute,
frequency of the segmentation
jejunum, the
Chapter 62. Because this frequency normally is not
electrical slow waves
frequency of
The maximum frequency of the segmentation con-
intestine.
to three times per minute, in this way promoting pro-
the segmentation contractions “chop” the chyme two
points between the previous contractions. Therefore,
mentation contractions relaxes, a new set often begins,
appearance of a chain of sausages. As one set of seg-
small intestine, as shown in Figure 63–3. That is, they
Propulsion and Mixing of Food in the Alimentary Tract
Chapter 63
787
divide the intestine into spaced segments that have the
but the contractions this time occur mainly at new
gressive mixing of the food with secretions of the small
tractions in the small intestine is determined by the
in the intestinal wall,
which is the basic electrical rhythm described in
over 12 per minute in the duodenum and proximal
maximum
but this occurs only under extreme conditions of stim-
weak when the excitatory activity of the enteric
these contractions are not effective without back-
ground excitation mainly from the myenteric nerve
Propulsive Movements
Peristalsis in the Small Intestine.
Chyme is propelled
through the small intestine by peristaltic waves
faster in the proximal intestine and slower in the ter-
that net movement along the small intestine normally
are required for passage of chyme from the pylorus to
Peri-
staltic activity of the small intestine is greatly increased
entry of chyme into the duodenum causing stretch of
gastroenteric
reflex that is initiated by distention of the stomach and
conducted principally through the myenteric plexus
from the stomach down along the wall of the small
In addition to the nervous signals that may affect
gastrin, CCK,
insulin, motilin
serotonin
intestinal motility and are secreted during various
secretin and
glucagon
logic importance of each of these hormonal factors for
intestine is not only to cause progression of chyme
toward the ileocecal valve but also to spread out the
enters the intestines from the stomach and elicits peri-
a gastroileal reflex intensifies peristalsis in the ileum
and forces the remaining chyme through the ileocecal
Propulsive Effect of the Segmentation Movements.
in the anal direction and during that time help propel
the segmentation and the peristaltic movements is not
as great as might be implied by their separation into
Peristaltic Rush.
Although peristalsis in the small
peristaltic rush
partly by nervous reflexes that involve the autonomic
nervous system and brain stem and partly by intrinsic
enhancement of the myenteric plexus reflexes within
travel long distances in the small intestine within
colon and thereby relieving the small intestine of irri-
tative chyme and excessive distention.
Movements Caused by the Muscularis Mucosae and Muscle Fibers
of the Villi.
muscularis mucosae can cause short
Regularly spaced
Isolated
Irregularly spaced
Weak regularly spaced
Figure 63–3
Segmentation movements of the small intestine.
intestine, large circular constrictions occur in the large
ments and propulsive movements.
gish. Yet in a sluggish manner, the movements still
wall movements are not required for these functions,
and the distal half with storage. Because intense colon
Figure 63–5, is concerned principally with absorption,
expelled. The proximal half of the colon, shown in
The principal functions of the colon are (1) absorption
nerves, especially by way of the prevertebral sympa-
emptying of the ileum into the cecum. The reflexes
a person has an inflamed appendix, the irritation of
tant in the cecum delays emptying. For instance, when
chyme into the cecum from the ileum. Also, any irri-
is distended, contraction of the ileocecal sphincter
nificantly by reflexes from the cecum. When the cecum
The degree of
Feedback Control of the Ileocecal Sphincter.
liliters of chyme empty into the cecum each day.
facilitates absorption. Normally, only 1500 to 2000 mil-
cecum proceeds.
in the ileum, and emptying of ileal contents into the
the cecum. However, immediately after a meal, a gas-
. This sphincter normally remains mildly
In addition, the wall of the ileum for several cen-
of water.
backward against the valve lips. The valve usually can
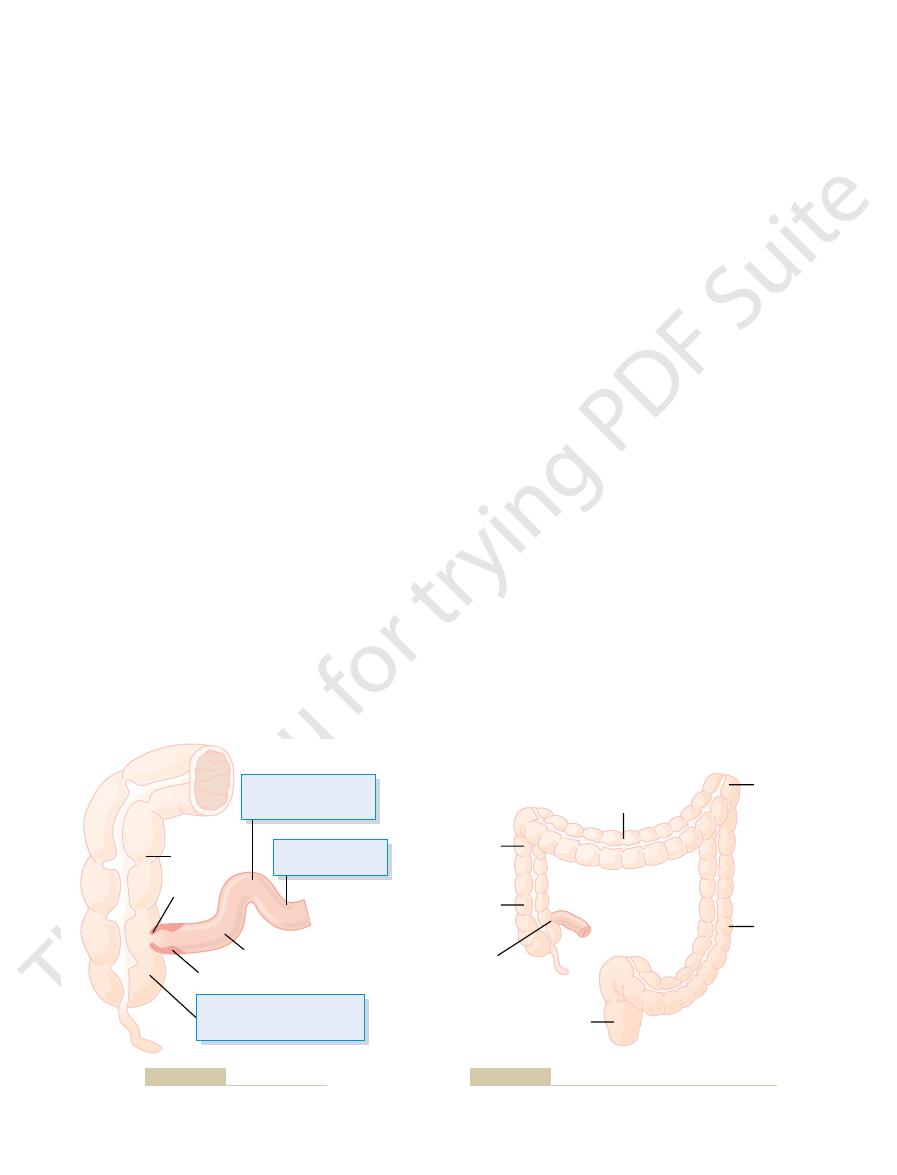
small intestine. As shown in Figure 63–4, the ileocecal
Function of the Ileocecal Valve
the small intestine.
system. These mucosal and villous contractions are ini-
ing again—“milk” the villi, so that lymph flows freely
tions of the villi—shortening, elongating, and shorten-
chyme, thereby increasing absorption. Also, contrac-
tinal villi and cause them to contract intermittently. The
788
Unit XII
Gastrointestinal Physiology
individual fibers from this muscle extend into the intes-
mucosal folds increase the surface area exposed to the
from the central lacteals of the villi into the lymphatic
tiated mainly by local nervous reflexes in the submu-
cosal nerve plexus that occur in response to chyme in
A principal function of the ileocecal valve is to prevent
backflow of fecal contents from the colon into the
valve itself protrudes into the lumen of the cecum and
therefore is forcefully closed when excess pressure
builds up in the cecum and tries to push cecal contents
resist reverse pressure of at least 50 to 60 centimeters
timeters immediately upstream from the ileocecal
valve has a thickened circular muscle called the ileo-
cecal sphincter
constricted and slows emptying of ileal contents into
troileal reflex (described earlier) intensifies peristalsis
Resistance to emptying at the ileocecal valve pro-
longs the stay of chyme in the ileum and thereby
contraction of the ileocecal sphincter and the intensity
of peristalsis in the terminal ileum are controlled sig-
becomes intensified and ileal peristalsis is inhibited,
both of which greatly delay emptying of additional
this vestigial remnant of the cecum can cause such
intense spasm of the ileocecal sphincter and partial
paralysis of the ileum that these effects together block
from the cecum to the ileocecal sphincter and ileum
are mediated both by way of the myenteric plexus in
the gut wall itself and of the extrinsic autonomic
thetic ganglia.
Movements of the Colon
of water and electrolytes from the chyme to form solid
feces and (2) storage of fecal matter until it can be
the movements of the colon are normally very slug-
have characteristics similar to those of the small intes-
tine and can be divided once again into mixing move-
Mixing Movements—“Haustrations.”
In the same manner
that segmentation movements occur in the small
Pressure or chemical irritation
in cecum inhibits peristalsis
of ileum and excites sphincter
Ileocecal sphincter
Ileum
Valve
Colon
Pressure and chemical
irritation relax sphincter
and excite peristalsis
Fluidity of contents
promotes emptying
Figure 63–4
Emptying at the ileocecal valve.
Mush
Semifluid
Fluid
Ileocecal
valve
Solid
Poor motility causes
greater absorption, and
hard feces in transverse
colon causes
constipation
Semi-
mush
Semi-
solid
Excess motility causes
less absorption and
diarrhea or loose feces
Figure 63–5
Absorptive and storage functions of the large intestine.
. These parasympathetic signals greatly intensify
to the descending colon, sigmoid, rectum, and anus by
mitted first into the spinal cord and then reflexly back
endings in the rectum are stimulated, signals are trans-
the spinal cord, shown in Figure 63–6. When the nerve
by another type of defecation reflex, a
tive in causing defecation, it usually must be fortified
ing by itself normally is relatively weak. To be effec-
The intrinsic myenteric defecation reflex function-
relaxed at the same time, defecation occurs.
anal sphincter is also consciously, voluntarily
inhibitory signals from the myenteric plexus; if the
the anus, the
toward the anus. As the peristaltic wave approaches
descending colon, sigmoid, and rectum, forcing feces
When feces enter the rectum, distention of the rectal
in the rectal wall. This can be described as follows:
. One of these reflexes is an
defecation reflexes
Ordinarily, defecation is initiated
; subconsciously,
, which is part of the somatic nervous
the internal sphincter and extends distal to it. The
, com-
inside the anus, and (2) an
, a several-centimeters-long thickening
ation of the anal sphincters.
rectum, the desire for defecation occurs immediately,
When a mass movement forces feces into the
rectum. There is also a sharp angulation here that con-
Most of the time, the rectum is empty of feces. This
the time.
movements. For instance, a person who has an ulcer-
to the colon have been removed; therefore, the reflexes
the stomach and duodenum. They occur either not at
. These reflexes result from distention of
colic reflexes
Initiation of Mass Movements by Gastrocolic and Duo-
into the rectum, the desire for defecation is felt.
half day later. When they have forced a mass of feces
to 30 minutes. Then they cease but return perhaps a
mass movement occurs, this time perhaps farther along
occurs during the next 2 to 3 minutes. Then, another
sively more force for about 30 seconds, and relaxation
down the colon. The contraction develops progres-
haustrations and instead contract as a unit, propelling
distal to the constrictive ring
transverse colon. Then, rapidly, the 20 or more cen-
tended or irritated point in the colon, usually in the
First, a
three times each day, in many people especially for
sive role. These movements usually occur only one to
can, for many minutes at a time, take over the propul-
mass movements
From the cecum to the sigmoid,
chyme itself becomes fecal in quality, a semisolid slush
from the ileocecal valve through the colon, while the
from the slow but persistent haustral contractions,
only 80 to 200 milliliters of feces are expelled each day.
the mucosal surface of the large intestine, and fluid and
this way, all the fecal material is gradually exposed to
much the same manner that one spades the earth. In
dug into and rolled over
in other areas nearby. Therefore, the fecal material in
another few minutes, new haustral contractions occur
of forward propulsion of the colonic contents. After
ascending colon, and thereby provide a minor amount
anus during contraction, especially in the cecum and
60 seconds. They also at times move slowly toward the
, contracts. These combined
colon, which is aggregated into three longitudinal
sion. At the same time, the longitudinal muscle of the
timeters of the circular muscle contracts, sometimes
intestine. At each of these constrictions, about 2.5 cen-
Propulsion and Mixing of Food in the Alimentary Tract
Chapter 63
789
constricting the lumen of the colon almost to occlu-
strips called the teniae coli
contractions of the circular and longitudinal strips of
muscle cause the unstimulated portion of the large
intestine to bulge outward into baglike sacs called
haustrations.
Each haustration usually reaches peak intensity in
about 30 seconds and then disappears during the next
the large intestine is slowly
in
dissolved substances are progressively absorbed until
Propulsive Movements—“Mass Movements.”
Much of the
propulsion in the cecum and ascending colon results
requiring as many as 8 to 15 hours to move the chyme
instead of semifluid.
about 15 minutes during the first hour after eating
breakfast.
A mass movement is a modified type of peristalsis
characterized by the following sequence of events:
constrictive ring occurs in response to a dis-
timeters of colon
lose their
the fecal material in this segment en masse further
the colon.
A series of mass movements usually persists for 10
denocolic Reflexes.
Appearance of mass movements
after meals is facilitated by gastrocolic and duodeno-
all or hardly at all when the extrinsic autonomic nerves
almost certainly are transmitted by way of the auto-
nomic nervous system.
Irritation in the colon can also initiate intense mass
ated condition of the colon mucosa (ulcerative colitis)
frequently has mass movements that persist almost all
Defecation
results partly from the fact that a weak functional
sphincter exists about 20 centimeters from the anus
at the juncture between the sigmoid colon and the
tributes additional resistance to filling of the rectum.
including reflex contraction of the rectum and relax-
Continual dribble of fecal matter through the anus
is prevented by tonic constriction of (1) an internal
anal sphincter
of the circular smooth muscle that lies immediately
external anal sphincter
posed of striated voluntary muscle that both surrounds
external sphincter is controlled by nerve fibers in the
pudendal nerve
system and therefore is under voluntary, conscious
or at least subconscious control
the external sphincter is usually kept continuously
constricted unless conscious signals inhibit the
constriction.
Defecation Reflexes.
by
intrin-
sic reflex mediated by the local enteric nervous system
wall initiates afferent signals that spread through the
myenteric plexus to initiate peristaltic waves in the
internal anal sphincter is relaxed by
external
parasympathetic
defecation reflex that involves the sacral segments of
way of parasympathetic nerve fibers in the pelvic
nerves
the peristaltic waves as well as relax the internal anal
options. Am J Gastroenterol 99:739, 2004.
motor abnormalities, sensory dysfunction, and therapeutic
Timmons S, Liston R, Moriarty KJ: Functional dyspepsia:
troenterol 38:421, 2003.
nitric oxide synthase in the gastrointestinal tract. J Gas-
Takahashi T: Pathophysiological significance of neuronal
News Physiol Sci 15:291, 2000.
maker Mechanism Drives Gastrointestinal Rhythmicity.
Sanders KM, Ordog T, Koh SD, Ward SM:A Novel Pace-
troenterology 126(1 Suppl 1):S14, 2004.
Rao SS: Pathophysiology of adult fecal incontinence. Gas-
Physiol 283:G1226, 2002.
motility and aging. Am J Physiol Gastrointest Liver
IV. Clinical and physiological aspects of gastrointestinal
Orr WC, Chen CL: Aging and neural control of the GI tract:
inflammatory bowel disease. News Physiol Sci 16:272,
tion of intestinal mucosal immunity: implications in
Laroux FS, Pavlick KP, Wolf RE, Grisham MB: Dysregula-
test Liver Physiol 280:G787, 2001.
I. Receptors on visceral afferents. Am J Physiol Gastroin-
mission in the brain-gut axis: potential for novel therapies.
Kirkup AJ, Brunsden AM, Grundy D: Receptors and trans-
Mosby, 2001.
Johnson LR: Gastrointestinal Physiology, 6th ed. St. Louis:
orders. Pharmacol Toxicol 91:333, 2002.
Jensen RT: Involvement of cholecystokinin/gastrin-related
Am J Physiol Heart Circ Physiol 285:H1791, 2003.
tion in the pathogenesis of inflammatory bowel disease.
Hatoum OA, Miura H, Binion DG: The vascular contribu-
motility. Physiol Res 52:1, 2003.
Hansen MB: Neurohumoral control of gastrointestinal
Am J Physiol Gastrointest Liver Physiol 283:G827, 2002.
control of the aging gut: can an old dog learn new tricks?
Hall KE: Aging and neural control of the GI tract. II. Neural
ters. Physiol Rev 67:902, 1987.
Gonella J, Bouvier M, Blanquet F: Extrinsic nervous control
terology 126:1872, 2004.
neuropathies of the enteric nervous system. Gastroen-
De Giorgio R, Guerrini S, Barbara G, et al: Inflammatory
Physiol Sci 18:43, 2003.
you”: ATP in gut mechanosensory transduction. News
Cooke HJ, Wunderlich J, Christofi FL: “The force be with
Neurol 23:453, 2003.
autonomic disorders of the gastrointestinal tract. Semin
Chelimsky G, Chelimsky TC: Evaluation and treatment of
Physiol Sci 19:27, 2004.
sonomicrometry and gastrointestinal motility. News
Adelson DW, Million M: Tracking the moveable feast:
vesicointestinal reflexes
ysis, especially in patients with peritonitis. The
of the peritoneum; it strongly inhibits the excitatory
The
renointestinal reflex, and vesicointestinal reflex.
bowel activity. They are the peritoneointestinal reflex,
discussed in this chapter, several other important
enterogastric, and defecation reflexes that have been
Aside from the duodenocolic, gastrocolic, gastroileal,
That Affect Bowel Activity
relaxation of the external anal sphincter.
sected spinal cords, the defecation reflexes cause auto-
tive as those that arise naturally, for which reason
fecal contents into the rectum to cause new reflexes.
increase the pressure in the abdomen, thus forcing
cate, the defecation reflexes can purposely be activated
When it becomes convenient for the person to defe-
evaginate the feces.
the glottis, and contraction of the abdominal wall
other effects, such as taking a deep breath, closure of
flexure of the colon to the anus.
sphincter, thus converting the intrinsic myenteric defe-
790
Unit XII
Gastrointestinal Physiology
cation reflex from a weak effort into a powerful
process of defecation that is sometimes effective in
emptying the large bowel all the way from the splenic
Defecation signals entering the spinal cord initiate
muscles to force the fecal contents of the colon down-
ward and at the same time cause the pelvic floor to
relax downward and pull outward on the anal ring to
by taking a deep breath to move the diaphragm down-
ward and then contracting the abdominal muscles to
Reflexes initiated in this way are almost never as effec-
people who too often inhibit their natural reflexes are
likely to become severely constipated.
In newborn babies and in some people with tran-
matic emptying of the lower bowel at inconvenient
times during the day because of lack of conscious
control exercised through voluntary contraction or
Other Autonomic Reflexes
nervous reflexes also can affect the overall degree of
peritoneointestinal reflex results from irritation
enteric nerves and thereby can cause intestinal paral-
reno-
intestinal and
inhibit intestinal
activity as a result of kidney or bladder irritation.
References
of motility of small and large intestines and related sphinc-
peptides and their receptors in clinical gastrointestinal dis-
2001.
From
conscious
cortex
Afferent
nerve
fibers
Parasympathetic
nerve fibers
(pelvic nerves)
Sigmoid
colon
Rectum
External anal sphincter
Internal anal sphincter
Descending
colon
Skeletal
motor nerve
nism for enhancing the defecation reflex.
Afferent and efferent pathways of the parasympathetic mecha-
Figure 63–6
