The
Effect of Contact of Food with the Epithelium—Function of Enteric Nervous Stimuli.
Tract Glands
Basic Mechanisms of Stimulation of the Alimentary
finally empty into the alimentary tract itself.
lined with secreting glandular cells; these acini feed into a system of ducts that
tract and, in this, differ from all other alimentary glands. They contain millions of
the type shown in Figure 64–2. These glands lie outside the walls of the alimentary
Chapter 70. The salivary glands and the pancreas are compound acinous glands of
sification of food. The liver has a highly specialized structure that is discussed in
salivary glands, pancreas,
Fourth, also associated with the alimentary tract are several complex glands—the
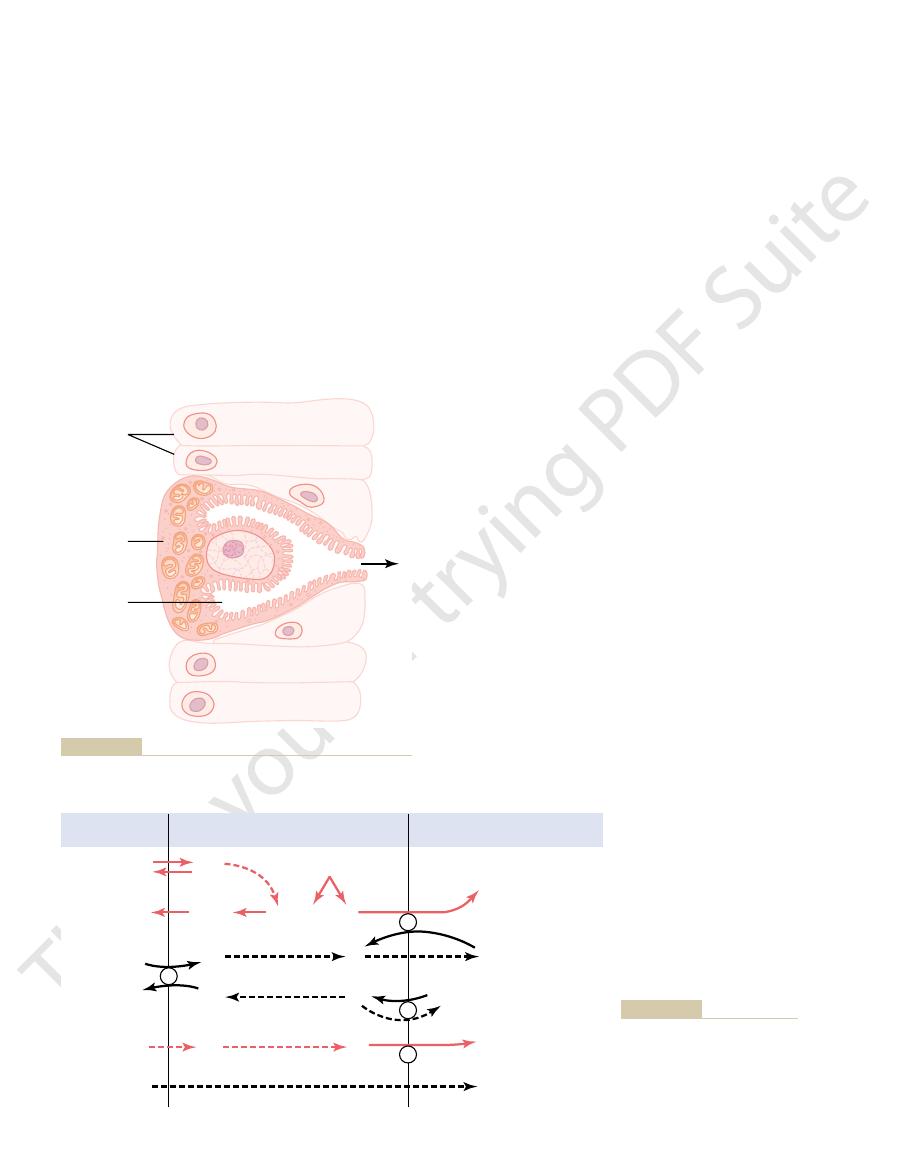
A typical tubular gland can be seen in Figure 64–4, which shows an acid- and
glands.
Third, in the stomach and upper duodenum are large numbers of deep
cells. One of these cells is shown in Figure 64–1.
, are deep and contain specialized secretory
these pits, called
resent invaginations of the epithelium into the submucosa. In the small intestine,
Second, many surface areas of the gastrointestinal tract are lined by
tation of the epithelium: they extrude
because they look like goblets. They function mainly in response to local irri-
First, on the surface of the epithelium in most parts of the gastrointestinal tract are
Several types of glands provide the different types of alimentary tract secretions.
Anatomical Types of Glands
Tract Secretion
General Principles of Alimentary
fore, is to describe the different alimentary secretions, their functions, and reg-
accordance with the types of food present. The purpose of this chapter, there-
proper digestion. Furthermore, in some portions of the gastrointestinal tract,
response to the presence of food in the alimentary tract, and the quantity
to the anus, provide
the ileum. Second, mucous glands, from the mouth
mentary tract, from the mouth to the distal end of
glands subserve two primary functions: First,
Throughout the gastrointestinal tract, secretory
Alimentary Tract
C
H
A
P
T
E
R
6
4
791
Secretory Functions of the
diges-
tive enzymes are secreted in most areas of the ali-
mucus for lubrication and pro-
tection of all parts of the alimentary tract.
Most digestive secretions are formed only in
secreted in each segment of the tract is almost exactly the amount needed for
even the types of enzymes and other constituents of the secretions are varied in
ulation of their production.
billions of single-cell mucous glands called simply mucous cells or sometimes goblet
cells
mucus directly onto the epithelial surface to
act as a lubricant that also protects the surfaces from excoriation and digestion.
pits that rep-
crypts of Lieberkühn
tubular
pepsinogen-secreting gland of the stomach (oxyntic gland).
and liver—that provide secretions for digestion or emul-
acini
mechanical presence of food in a particular segment of the gastrointestinal tract
usually causes the glands of that region and often of adjacent regions to secrete
substrates provided by the nutrients, is then used
3. Energy from the ATP, along with appropriate
adenosine triphosphate (ATP).
mitochondria
2. Many
1. The nutrient material needed for formation of
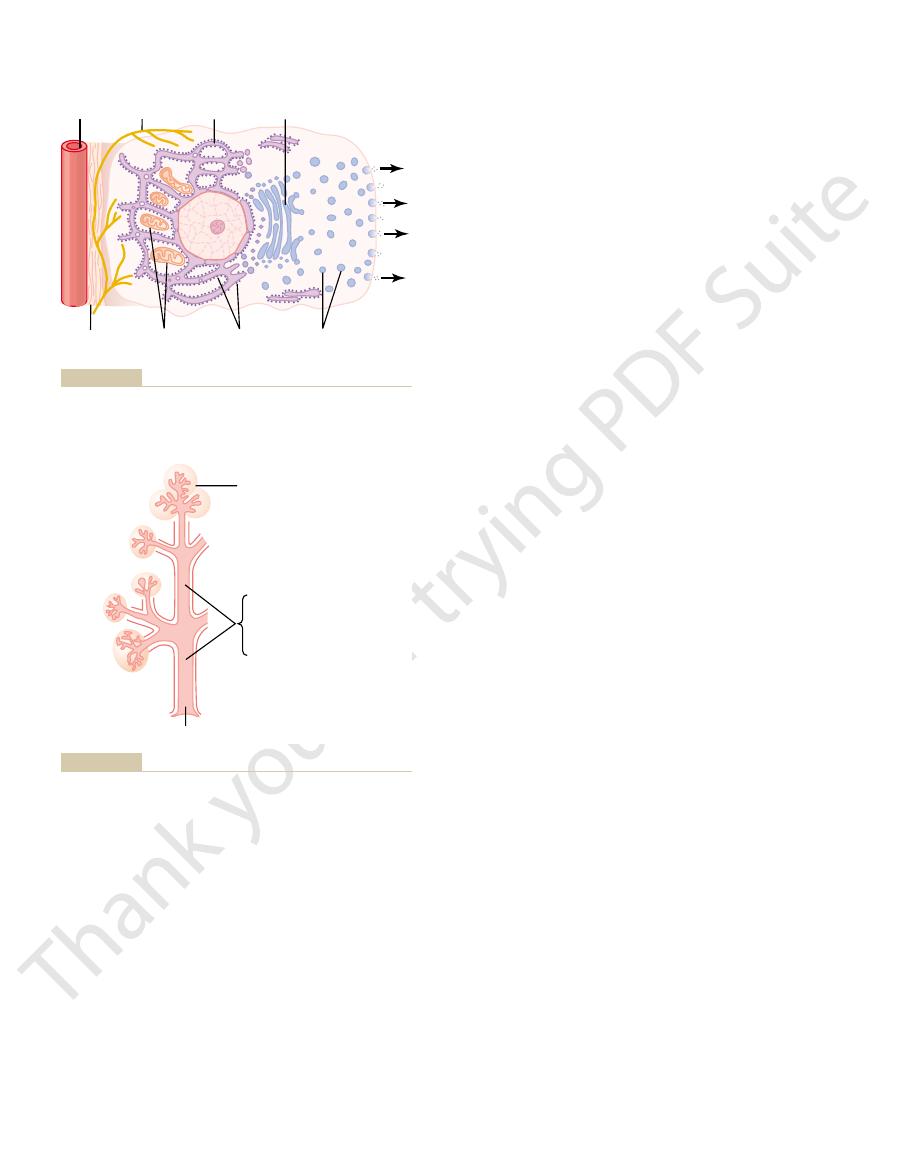
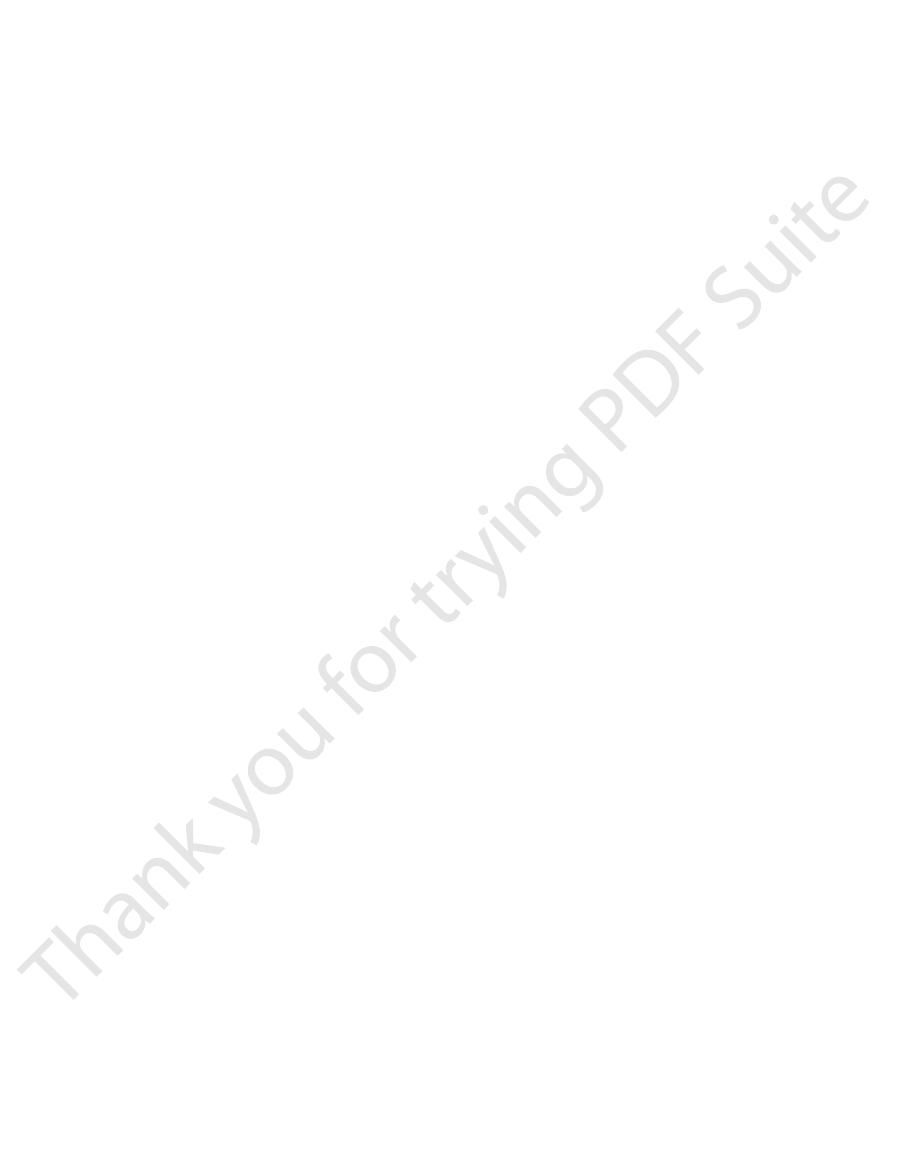
following principles of secretion, as shown in Figure
are not known, experimental evidence points to the
Basic Mechanism of Secretion
polypeptides or polypeptide derivatives.
Chemically, the gastrointestinal hormones are
where they stimulate secretion. This type of stimula-
absorbed into the blood and carried to the glands,
food in the lumen of the gut. The hormones then are
the secretions. These hormones are liberated from the
stomach and intestine, several different
constrictive reduction of the blood supply.
sometimes significantly so, mainly because of vaso-
causing copious secretion by the glands, superimposed
usually slightly increases secretion. But, second, if
have a dual effect: First, sympathetic stimulation alone
the glands. Therefore, sympathetic stimulation can
of the local glands. But sympathetic stimulation also
pathetic nerves. Secretion in the remainder of the
of the large intestine, innervated by pelvic parasym-
num. It is also true of some glands in the distal portion
glands, pancreas, and Brunner’s glands in the duode-
such as the salivary glands, esophageal glands, gastric
sopharyngeal and vagus parasympathetic nerves)
secretion. This is especially true of the glands in the
wall. The resulting nervous reflexes stimulate both the
(2) chemical irritation, and (3) distention of the gut
of the gut wall. The
In addition, local epithelial stimulation also acti-
cells, results from direct contact stimulation of the
effect, especially the secretion of mucus by mucous
moderate to large quantities of juices. Part of this local
792
Unit XII
Gastrointestinal Physiology
surface glandular cells by the food.
vates the enteric nervous system
types of stimuli that do this are (1) tactile stimulation,
mucous cells on the gut epithelial surface and the deep
glands in the gut wall to increase their secretion.
Autonomic Stimulation of Secretion
Parasympathetic Stimulation.
Stimulation of the
parasympathetic nerves to the alimentary tract almost
invariably increases the rates of alimentary glandular
upper portion of the tract (innervated by the glos-
small intestine and in the first two thirds of the large
intestine occurs mainly in response to local neural and
hormonal stimuli in each segment of the gut.
Sympathetic Stimulation.
Stimulation of the sympa-
thetic nerves going to the gastrointestinal tract causes
a slight to moderate increase in secretion by some
results in constriction of the blood vessels that supply
parasympathetic or hormonal stimulation is already
sympathetic stimulation usually reduces the secretion,
Regulation of Glandular Secretion by Hormones.
In the
gastrointestinal
hormones help regulate the volume and character of
gastrointestinal mucosa in response to the presence of
tion is particularly valuable to increase the output of
gastric juice and pancreatic juice when food enters the
stomach or duodenum.
by Glandular Cells
Secretion of Organic Substances.
Although all the
basic mechanisms by which glandular cells function
64–1.
the secretion must first diffuse or be actively
transported by the blood in the capillaries into the
base of the glandular cell.
located inside the glandular
cell near its base use oxidative energy to form
to synthesize the organic secretory substances;
this synthesis occurs almost entirely in the
endoplasmic reticulum and Golgi complex of the
glandular cell. Ribosomes adherent to the
Zymogen
granules
Ribosomes
Mitochondria
Nerve
fiber
Basement
membrane
Endoplasmic
reticulum
Golgi
apparatus
Secretion
Capillary
enzymes and other secretory substances.
Typical function of a glandular cell for formation and secretion of
Figure 64–1
Primary secretion:
1. Ptyalin
2. Mucus
3. Extracellular fluid
Saliva
Na
+
active absorption
Cl
-
passive absorption
K
+
active secretion
HCO
3
-
secretion
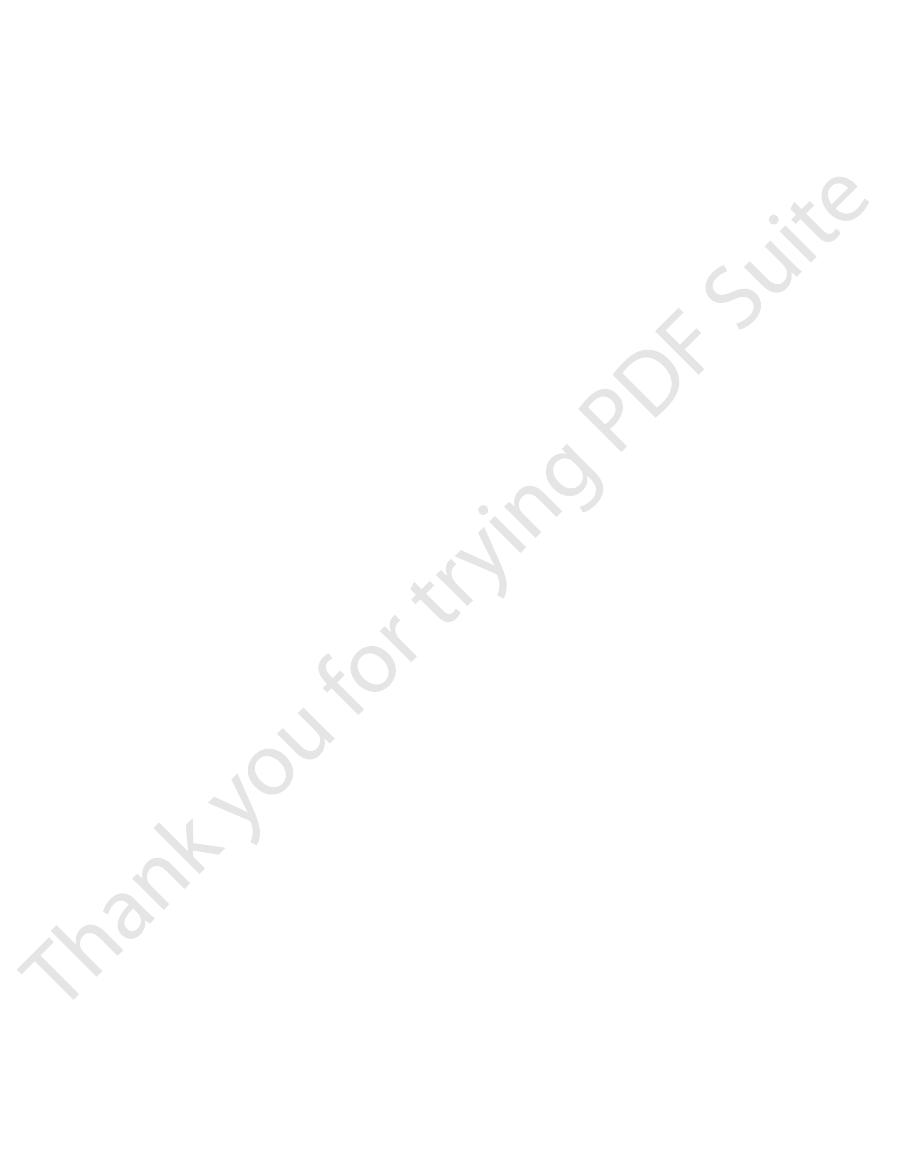
Formation and secretion of saliva by a submandibular salivary
Figure 64–2
gland.
serous type of secretion, while the submandibular and
The parotid glands secrete almost entirely the
cating and for surface protective purposes.
-amylase), which is an enzyme for digesting starches,
the average value of 1000 milliliters in Table 64–1.
ranges between 800 and 1500 milliliters, as shown by
glands. Daily secretion of saliva normally
; in addition, there are many very
The principal
Salivary Glands; Characteristics of Saliva.
Secretion of Saliva
water.
secrete saliva, because then it is difficult to swallow solid
lium. A person becomes acutely aware of the lubricat-
In summary, mucus has the ability to allow easy slip-
cally neutralize acids.
of either acids or alkalies; also, mucus often contains
teins of mucus have amphoteric properties, which
, the glycopro-
the gastrointestinal enzymes. And
, mucus is strongly resistant to digestion by
Fourth
can slide along the epithelium with great ease.
has a low resistance for slippage, so that the particles
, mucus
Third
, it has sufficient
over the surfaces.
trointestinal tract, but everywhere it has several im-
electrolytes, and a mixture of several glycoproteins,
Mucus is a thick secretion composed mainly of water,
Gastrointestinal Tract
Importance of Mucus in the
Properties of Mucus, and
Lubricating and Protective
for nerve impulses to regulate secretion. Hormones
theoretical, it does explain how it would be possible
through the membrane to the interior of the cell, thus
signal has arrived, indicating that it is caused by move-
negative than normal. This increase in polarization
ity on the interior and positivity on the exterior.
the cell is between 30 and 40 millivolts, with negativ-
Second, microelectrode studies show that the normal
dular cells are principally on the bases of the cells.
the following findings: First, the nerve endings on glan-
causing flushing of water, electrolytes, and organic
4. The pressure in the cell then initiates minute
pressure inside the cell, causing the cell itself to
force that causes osmosis of water to the interior,
3. Now, the new excess of both negative and
2. The resulting increase in electronegativity induced
transport of chloride ions to the cell interior.
1. Nerve stimulation has a specific effect on the
through the glandular cells in great profusion, washing
The following is a postulated method by which
electrolytes to go along with the organic substances.
Water and Electrolyte Secretion.
open, thus emptying the vesicles to the exterior;
membrane. Then the apical cell membrane breaks
calcium enters the cell. The
, and
membrane permeability to calcium ions
way: The control signal first
surface. This probably occurs in the following
6. These vesicles remain stored until nervous or
are stored in the apical ends of the secretory cells.
, which
cytoplasm in the form of
added to, concentrated, and discharged into the
5. In the Golgi complex, the materials are modified,
the tubules of the endoplasmic reticulum, passing
4. The secretory materials are transported through
Secretory Functions of the Alimentary Tract
Chapter 64
793
reticulum are specifically responsible for
formation of the proteins that are secreted.
in about 20 minutes all the way to the vesicles of
the Golgi complex.
secretory vesicles
hormonal control signals cause the cells to
extrude the vesicular contents through the cells’
increases the cell
calcium in turn causes
many of the vesicles to fuse with the apical cell
this process is called exocytosis.
A second necessity for
glandular secretion is secretion of sufficient water and
nervous stimulation causes water and salts to pass
the organic substances through the secretory border of
the cells at the same time:
basal portion of the cell membrane to cause active
inside the cell by excess negatively charged
chloride ions then causes positive ions such as
sodium ions also to move through the cell
membrane to the interior of the cell.
positive ions inside the cell creates an osmotic
thereby increasing cell volume and hydrostatic
swell.
openings of the secretory border of the cell,
materials out of the secretory end of the glandular
cell.
In support of these secretory processes have been
electrical potential across the membrane at the base of
Parasympathetic stimulation increases this polariza-
tion voltage to values some 10 and 20 millivolts more
voltage lasts for 1 second or longer after the nerve
ment of negative ions (presumably chloride ions)
leading to secretion.
Although this mechanism for secretion is still partly
acting on the cell membrane are believed also to cause
similar secretory results to those caused by nervous
stimulation.
which themselves are composed of large polysaccha-
rides bound with much smaller quantities of protein.
Mucus is slightly different in different parts of the gas-
portant characteristics that make it both an excellent
lubricant and a protectant for the wall of the gut. First,
mucus has adherent qualities that make it adhere tightly
to the food or other particles and to spread as a thin film
Second
body that
it coats the wall of the gut and prevents actual contact
of most food particles with the mucosa.
,
mucus causes fecal particles to adhere to one another
to form the feces that are expelled during a bowel move-
ment. Fifth
sixth
means that they are capable of buffering small amounts
moderate quantities of bicarbonate ions which specifi-
page of food along the gastrointestinal tract and to
prevent excoriative or chemical damage to the epithe-
ing qualities of mucus when the salivary glands fail to
food even when it is eaten along with large amounts of
glands of salivation are the parotid, submandibular,
and sublingual glands
small buccal
Saliva contains two major types of protein secretion:
(1) a serous secretion that contains ptyalin (an
a
and (2) mucus secretion that contains mucin for lubri-
sublingual glands secrete both serous secretion and
(e.g., a pebble), cause marked salivation, whereas
the basal rate of secretion. Also, certain tactile stimuli,
stimuli, especially the sour taste (caused by acids),
other areas of the mouth and pharynx. Many taste
The salivatory nuclei are located approximately at
ways for regulating salivation, demonstrating that the
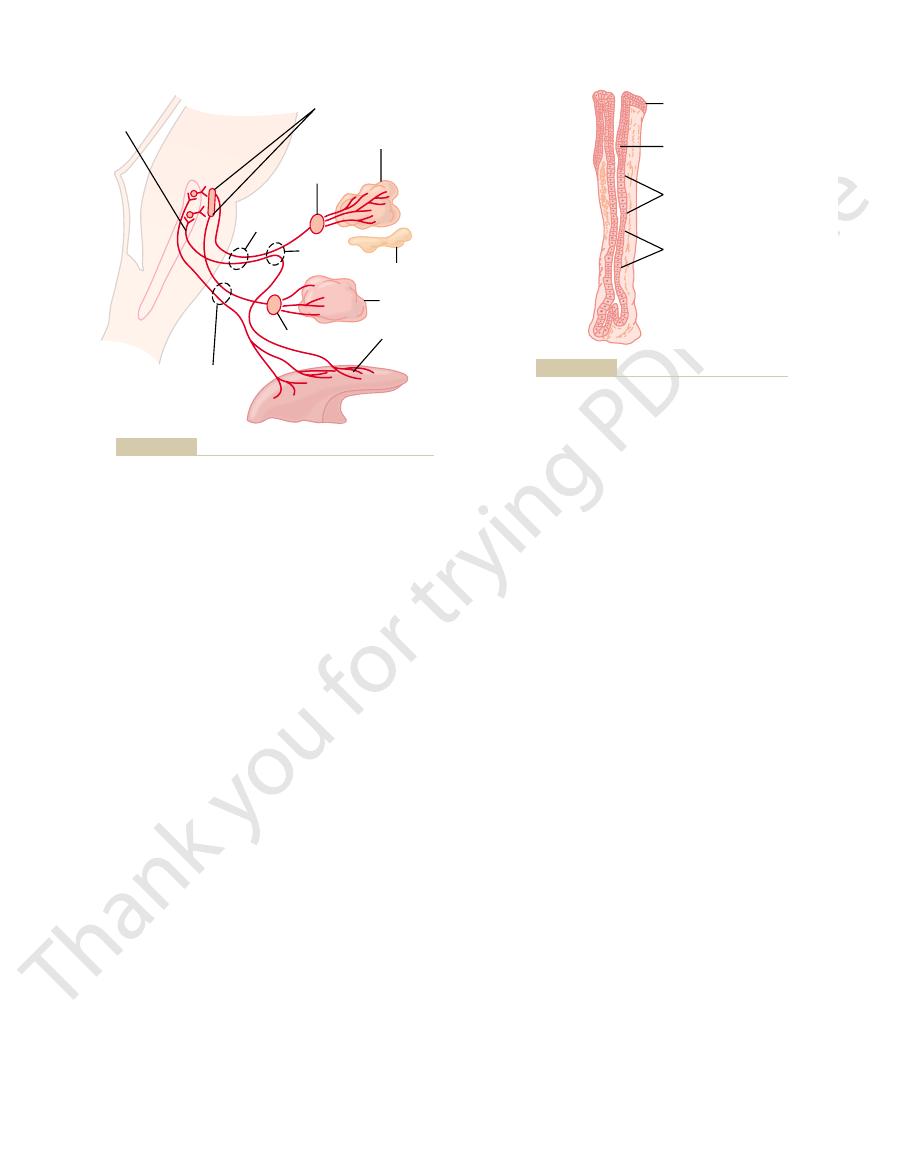
Figure 64–3 shows the parasympathetic nervous path-
erwise infected, and caries of the teeth can become
salivation, oral tissues often become ulcerated and oth-
ing some that cause dental caries. In the absence of
protein antibodies that can destroy oral bacteria, includ-
, saliva often contains significant amounts of
Third
cles, thus helping further to remove the bacterial meta-
in turn become bactericidal, and (c) digest food parti-
cyanate ions in entering the bacteria where these ions
that (a) attack the bacteria, (b) aid the thio-
bacteria. One of these is
, saliva contains several factors that destroy
, the flow of saliva itself helps wash away patho-
in several ways.
caries. Saliva helps prevent the deteriorative processes
oral tissues. The mouth is loaded with pathogenic bac-
sleep, secretion becomes very little. This secretion plays
the mucous type, is secreted each minute; but during
ditions, about 0.5 milliliter of saliva, almost entirely of
rises only to one half or two thirds that of plasma, and
are being secreted, the sodium chloride concentration
reduced. Therefore, when copious quantities of saliva
increase as much as 20-fold. This acinar secretion
, the salivary ionic con-
ions is 50 to 70 mEq/L, about two to three times that
as in plasma; and the concentration of bicarbonate
potassium ions is about 30 mEq/L, seven times as great
trations in plasma. Conversely, the concentration of
L each, about one seventh to one tenth their concen-
, the concentrations of sodium
The net result of these transport processes is that
active secretory process.
chloride ions, but it may also result partly from an
epithelium into the lumen of the duct. This is at least
level, matching the ductal decrease in sodium ion
to be reabsorbed passively. Therefore, the chloride ion
in the salivary ducts; this in turn causes chloride ions
sodium reabsorption over potassium secretion, and
tration becomes increased. However, there is excess
greatly reduced, whereas the potassium ion concen-
secreted in exchange for the sodium. Therefore, the
First,
primary secretion flows through the ducts, two major
from those of typical extracellular fluid. As the
second, the salivary ducts. The acini secrete a
operation: the first stage involves the acini, and the
. Salivary secretion is a two-stage
gland, a typical compound gland that contains
Figure 64–2 shows secretion by the submandibular
plasma. One can understand these special concentra-
Conversely, the concentrations of both sodium and
large quantities of potassium and bicarbonate ions.
has a pH between 6.0 and 7.0, a favorable range for
mucus. The buccal glands secrete only mucus. Saliva
794
Unit XII
Gastrointestinal Physiology
the digestive action of ptyalin.
Secretion of Ions in Saliva.
Saliva contains especially
chloride ions are several times less in saliva than in
tions of ions in the saliva from the following descrip-
tion of the mechanism for secretion of saliva.
acini
and salivary ducts
primary
secretion that contains ptyalin and/or mucin in a solu-
tion of ions in concentrations not greatly different
active transport processes take place that markedly
modify the ionic composition of the fluid in the saliva.
sodium ions are actively reabsorbed from all
the salivary ducts and potassium ions are actively
sodium ion concentration of the saliva becomes
this creates electrical negativity of about
-70 millivolts
concentration in the salivary fluid falls to a very low
concentration.
Second, bicarbonate ions are secreted by the ductal
partly caused by passive exchange of bicarbonate for
under resting conditions
and chloride ions in the saliva are only about 15 mEq/
of plasma.
During maximal salivation
centrations change considerably because the rate of
formation of primary secretion by the acini can
then flows through the ducts so rapidly that the ductal
reconditioning of the secretion is considerably
the potassium concentration rises to only four times
that of plasma.
Function of Saliva for Oral Hygiene.
Under basal awake con-
an exceedingly important role for maintaining healthy
teria that can easily destroy tissues and cause dental
First
genic bacteria as well as food particles that provide their
metabolic support.
Second
thiocyanate ions and another
is several proteolytic enzymes—most important,
lysozyme—
bolic support.
rampant.
Nervous Regulation of Salivary
Secretion
salivary glands are controlled mainly by parasympa-
thetic nervous signals all the way from the superior and
inferior salivatory nuclei in the brain stem.
the juncture of the medulla and pons and are excited
by both taste and tactile stimuli from the tongue and
elicit copious secretion of saliva—often 8 to 20 times
such as the presence of smooth objects in the mouth
rough objects cause less salivation and occasionally
even inhibit salivation.
Salivation can also be stimulated or inhibited by
nervous signals arriving in the salivatory nuclei from
Table 64–1
Brunner’s gland secretion
200
8.0–8.9
Small intestine secretion
1800
7.5–8.0
Bile
1000
7.8
Pancreatic secretion
1000
8.0–8.3
Gastric secretion
1500
1.0–3.5
Saliva
1000
6.0–7.0
Daily Volume (ml)
pH
Daily Secretion of Intestinal Juices
Large intestinal secretion
200
7.5–8.0
Total
6700
) cells, which secrete large quantities of
chief
, which secrete mainly
neck cells
64–4. It is composed of three types of cells: (1)
A typical stomach oxyntic gland is shown in Figure
Secretions from the Oxyntic (Gastric) Glands
proximal 80 per cent of the stomach. The pyloric
of the body and fundus of the stomach, constituting the
The oxyntic glands are located on the inside surfaces
pyloric mucosa from the stomach acid. They also
. The pyloric
, and
hydrochloric acid
. The oxyntic
pyloric glands
oxyntic glands
surface of the stomach, the stomach mucosa has two
Characteristics of the Gastric
Gastric Secretion
occur at the gastric end of the esophagus.
Despite this protection, a peptic ulcer at times can still
from the stomach back into the lower esophagus.
food, whereas the compound glands located near the
The mucus
compound mucous glands.
extent in the initial portion of the esophagus, there
. At the gastric end and to a lesser
The main body of the esophagus is lined with many
acter and principally provide lubrication for swallowing.
The esophageal secretions are entirely mucous in char-
Esophageal Secretion
vasodilator.
an alpha2-globulin, to form
acts as an enzyme to split one of the blood proteins,
secreted by the activated salivary cells, which in turn
nutrition as needed by the secreting cells. Part of this
vessels, thus providing increased salivatory gland
addition, salivation itself directly dilates the blood
salivation also moderately dilate the blood vessels. In
The parasympathetic nerve signals that induce copious
glands.
thetic stimulation. The sympathetic nerves originate
a slight amount, much less so than does parasympa-
by diluting or neutralizing the irritant substances.
abnormality. The saliva, when swallowed, helps to
parasympathetic centers of the anterior hypothalamus,
regulates these effects, is located in proximity to the
of the brain, which partially
or eaten. The
instance, when a person smells or eats favorite foods,
higher centers of the central nervous system. For
Secretory Functions of the Alimentary Tract
Chapter 64
795
salivation is greater than when disliked food is smelled
appetite area
and it functions to a great extent in response to signals
from the taste and smell areas of the cerebral cortex
or amygdala.
Salivation also occurs in response to reflexes origi-
nating in the stomach and upper small intestines—par-
ticularly when irritating foods are swallowed or when
a person is nauseated because of some gastrointestinal
remove the irritating factor in the gastrointestinal tract
Sympathetic stimulation can also increase salivation
from the superior cervical ganglia and travel along the
surfaces of the blood vessel walls to the salivary
A secondary factor that also affects salivary secre-
tion is the blood supply to the glands because secretion
always requires adequate nutrients from the blood.
additional vasodilator effect is caused by kallikrein
bradykinin, a strong
simple mucous glands
are also many
secreted by the compound glands in the upper esopha-
gus prevents mucosal excoriation by newly entering
esophagogastric junction protect the esophageal wall
from digestion by acidic gastric juices that often reflux
Secretions
In addition to mucus-secreting cells that line the entire
important types of tubular glands:
(also
called gastric glands) and
(acid-forming) glands secrete
,
pepsinogen, intrinsic factor
mucus
glands secrete mainly mucus for protection of the
secrete the hormone gastrin.
glands are located in the antral portion of the stomach,
the distal 20 per cent of the stomach.
mucous
mucus; (2) peptic
(or
Superior and inferior
salivatory nuclei
Submandibular gland
Submandibular
ganglion
Sublingual gland
Chorda
tympani
Otic ganglion
Taste and
tactile stimuli
Tongue
Glossopharyngeal
nerve
Parotid
gland
Tractus
solitarius
Facial
nerve
Parasympathetic nervous regulation of salivary secretion.
Figure 64–3
Surface
epithelium
Mucous neck
cells
Oxyntic
(or parietal)
cells
Peptic
(or chief)
cells
Oxyntic gland from the body of the stomach.
Figure 64–4
concentration of about 150 to 160 mEq/L,
contains water, hydrochloric acid at a
Thus, the final secretion from the canaliculus
because of extra ions secreted into the canaliculus.
3. Water passes into the canaliculus by osmosis
of hydrochloric acid in the canaliculus. The
place in the canaliculus, giving a strong solution
the cell cytoplasm, and hydrogen ions take their
reabsorbed by a separate sodium pump. Thus,
ATPase. In addition, the sodium ions are actively
canaliculus in exchange for potassium ions: this
in the cell cytoplasm. The
hydroxyl ions
2. Water becomes dissociated into
canaliculus.
effect, mainly potassium chloride and much
cell cytoplasm into the canaliculus. Thus, in
millivolts in the canaliculus, which in turn causes
cytoplasm of the parietal cell. These two effects
the canaliculus, and sodium ions are actively
cytoplasm of the parietal cell into the lumen of
1. Chloride ion is actively transported from the
One of these, shown in Figure 64–6, consists of the
The hydrochloric acid is formed at
Figure 64–5 shows schematically the functional
energy per liter of gastric juice.
blood. To concentrate the hydrogen ions this tre-
its extreme acidity. At this pH, the hydrogen ion con-
fluids. The pH of this acid is about 0.8, demonstrating
per liter, which is almost exactly isotonic with the body
stimulated, the parietal cells secrete an acid solution
When
special mechanisms, as follows.
. Secretion
hydrochloric acid
, which
oxyntic
; and (3)
796
Unit XII
Gastrointestinal Physiology
pepsinogen
parietal (or
) cells
secrete
and intrinsic factor
of hydrochloric acid by the parietal cells involves
Basic Mechanism of Hydrochloric Acid Secretion.
that contains about 160 millimoles of hydrochloric acid
centration is about 3 million times that of the arterial
mendous amount requires more than 1500 calories of
structure of a parietal cell (also called oxyntic cell),
demonstrating that it contains large branching intra-
cellular canaliculi.
the villus-like projections inside these canaliculi and is
then conducted through the canaliculi to the secretory
end of the cell.
Different suggestions for the chemical mechanism
of hydrochloric acid formation have been offered.
following steps:
transported out of the canaliculus into the
together create a negative potential of
-40 to -70
diffusion of positively charged potassium ions
and a small number of sodium ions from the
smaller amounts of sodium chloride enter the
hydrogen ions
and
hydrogen ions are then actively secreted into the
active exchange process is catalyzed by H
+
,K
+
-
most of the potassium and sodium ions that had
diffused into the canaliculus are reabsorbed into
hydrochloric acid is then secreted outward
through the open end of the canaliculus into the
lumen of the gland.
Mucous
neck cells
Oxyntic
(parietal)
cell
Canaliculi
Secretion
Figure 64–5
Schematic anatomy of the canaliculi in a parietal (oxyntic) cell.
Parietal cell
Lumen of canaliculus
Extracellular fluid
CO
2
CO
2
H
2
O
H
2
O
H
2
O
(Osmosis)
HCO
3
-
HCO
3
-
CO
2
+
OH
-
+
H
+
K
+
K
+
K
+
Na
+
Na
+
Na
+
Na
+
Cl–
Cl–
(3 mEq/L)
Cl–
H
+
(155 mEq/L)
K
+
(15 mEq/L)
Cl
-
(173 mEq/L)
P
P
P
P
represent free diffusion and
tion of hydrochloric acid. (The
Postulated mechanism for secre-
Figure 64–6
points labeled “P” indicate active
pumps, and the dashed lines
osmosis.)
these are important, the smaller is more abundant.
G-17, which contains 17 amino acids. Although both of
which contains 34 amino acids, and a smaller form,
tide secreted in two forms: a large form called G-34,
distal end of the stomach. Gastrin is a large polypep-
pyloric glands
These cells are located in the
, also called
wall. Let us discuss first the gastrin mechanism for
(2) In addition, the ECL cells can be stimulated by
, which is formed almost
different ways: (1) Probably the most potent mecha-
tamine secreted by the ECL cells. In turn, the ECL
contact with the parietal cells of the glands. The rate
The ECL cells lie in the deep recesses of the oxyntic
enterochromaf-
Furthermore, the parietal cells operate in close associ-
tinuous control by both endocrine and nervous signals.
low as 0.8. However, secretion of this acid is under con-
secreted by these cells can be very great, with pH as
noted earlier in the chapter, the acidity of the fluid
are the only cells that secrete hydrochloric acid. As
, located deep
The
Stimulation of Gastric Acid Secretion
ties of this thick, alkaline, viscid mucus.
stomach secretion. Even the slightest contact with
not directly exposed to the highly acidic, proteolytic
. Therefore, the
mucus often more than 1 millimeter thick, thus
They secrete large quantities of a very
mucous cells called simply “surface mucous cells.”
The entire surface of the stomach mucosa between
shortly.
key role in controlling gastric secretion, as we discuss
from digestion by the gastric enzymes. The pyloric
food movement, as well as to protect the stomach wall
of pepsinogen, as discussed earlier, and an especially
the oxyntic glands. These cells secrete a small amount
no parietal cells. Instead, they contain mostly mucous
The pyloric glands are structurally similar to the
ulation of the bone marrow. This is discussed in detail
achlorhydria
occurs in chronic gastritis, the person develops not only
cells of the stomach are destroyed, which frequently
hydrochloric acid. When the acid-producing parietal
in the ileum, is
The substance
Secretion of Intrinsic Factor.
protein digestion in the stomach; this is discussed
time. Hydrochloric acid is as necessary as pepsin for
a highly acid medium (optimum pH 1.8 to 3.5), but
form a pepsin molecule, having a molecular weight of
having a molecular weight of about 42,500, is split to
In this process, the pepsinogen molecule,
with hydrochloric acid, it is activated to form active
tive activity. However, as soon as it comes in contact
When pepsinogen is first secreted, it has no diges-
functions.
Even so, all the pepsinogens perform the same
the peptic and mucous cells of the gastric glands.
are later secreted into the canaliculus.
diffuse out of the cell cytoplasm into the
step 2) to form bicarbonate ions. These then
the blood, combines under the influence of
4. Finally, carbon dioxide, either formed during
L, and a small amount of sodium chloride.
potassium chloride at a concentration of 15 mEq/
Secretory Functions of the Alimentary Tract
Chapter 64
797
metabolism in the cell or entering the cell from
carbonic anhydrase with the hydroxyl ions (from
extracellular fluid in exchange for chloride ions
that enter the cell from the extracellular fluid and
Secretion and Activation of Pepsinogen.
Several slightly
different types of pepsinogen are secreted by
pepsin.
about 35,000.
Pepsin functions as an active proteolytic enzyme in
above a pH of about 5 it has almost no proteolytic
activity and becomes completely inactivated in a short
further in Chapter 65.
intrinsic factor,
essential for absorption of vitamin B
12
secreted by the parietal cells along with the secretion of
(lack of stomach acid secretion) but often
also pernicious anemia because of failure of maturation
of the red blood cells in the absence of vitamin B
12
stim-
in Chapter 32.
Pyloric Glands—Secretion of Mucus
and Gastrin
oxyntic glands but contain few peptic cells and almost
cells that are identical with the mucous neck cells of
large amount of thin mucus that helps to lubricate
glands also secrete the hormone gastrin, which plays a
Surface Mucous Cells
glands has a continuous layer of a special type of
viscid mucus
that coats the stomach mucosa with a gel layer of
providing a major shell of protection for the stomach
wall as well as contributing to lubrication of food
transport.
Another characteristic of this mucus is that it is alka-
line
normal underlying stomach wall is
food or any irritation of the mucosa directly stimulates
the surface mucous cells to secrete additional quanti-
Parietal Cells of the Oxyntic Glands Are the Only Cells That
Secrete Hydrochloric Acid.
parietal cells
in the oxyntic glands of the main body of the stomach,
ation with another type of cell called
fin-like cells (ECL cells), the primary function of which
is to secrete histamine.
glands and therefore release histamine in direct
of formation and secretion of hydrochloric acid by the
parietal cells is directly related to the amount of his-
cells can be stimulated to secrete histamine in several
nism for stimulating histamine secretion is by the hor-
monal substance gastrin
entirely in the antral portion of the stomach mucosa
in response to proteins in the foods being digested.
(a) acetylcholine released from stomach vagal nerve
endings and (b) probably also by hormonal substances
secreted by the enteric nervous system of the stomach
control of the ECL cells and their subsequent control
of parietal cell secretion of hydrochloric acid.
Stimulation of Acid Secretion by Gastrin.
Gastrin is itself a
hormone secreted by gastrin cells
G cells.
in the
influences.
other times. This inhibition results from at least two
secretion, it paradoxically inhibits gastric secretion at
Intestinal Factors
Inhibition of Gastric Secretion
small amounts of gastric juice, probably partly because
denum, will continue to cause stomach secretion of
portion of the small intestine, particularly in the duo-
The presence of food in the upper
about 1500 milliliters.
remains in the stomach. The gastric phase of secretion
and (3) the gastrin mechanism, all of which in turn cause
brain and back to the stomach, (2) local enteric reflexes,
Once food enters the stomach, it excites
thence through the vagus nerves to the stomach. This
of the amygdala and hypothalamus. They are trans-
the more intense is the stimulation. Neurogenic signals
thought, or taste of food, and the greater the appetite,
while it is being eaten. It results from the sight, smell,
occurs even before food enters the stomach, especially
The cephalic phase of gastric secretion
intestinal phase.
, a
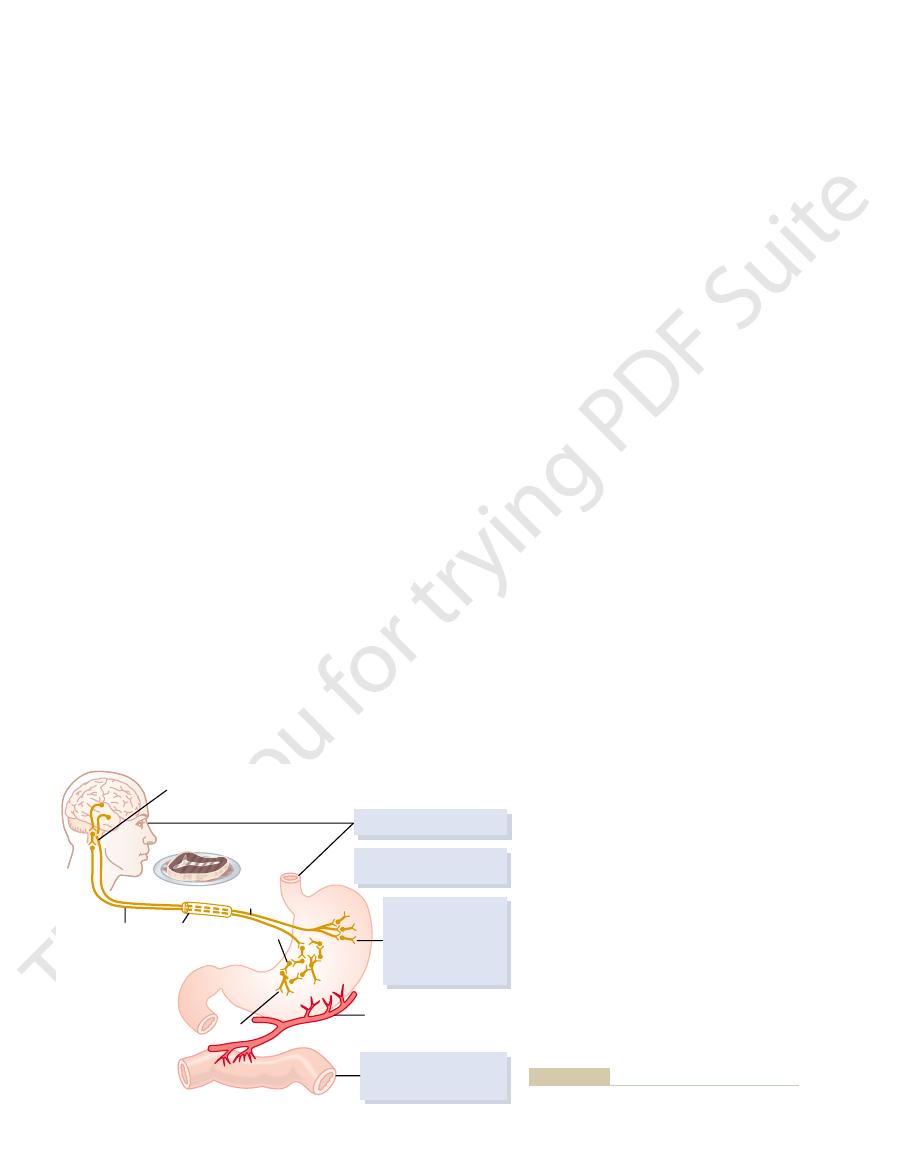
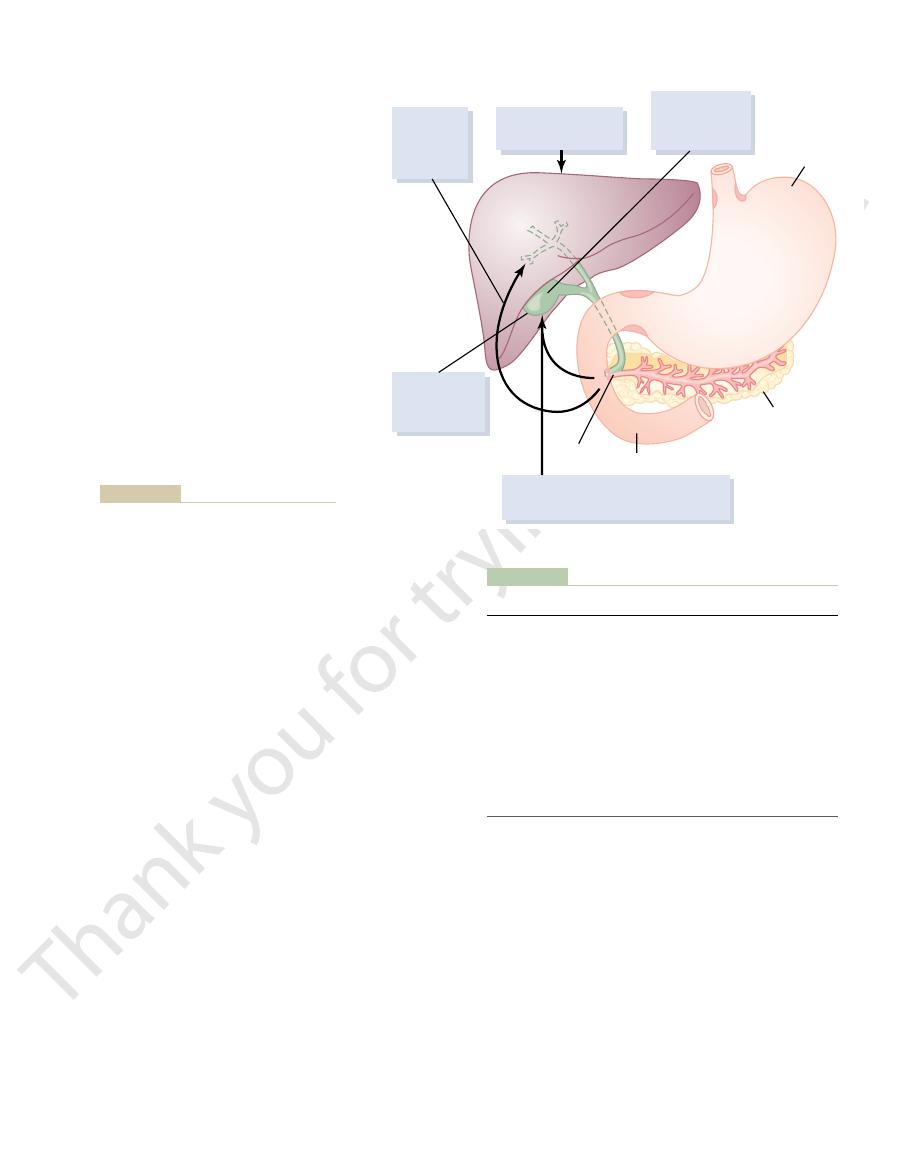
shown in Figure 64–7): a
Gastric secretion is said to occur in three “phases” (as
also decreased, even though the peptic cells may
normal amounts of acid, secretion of pepsinogen is
stomach. In people who have lost the ability to secrete
that causes protein digestion, is
nervous signals to the peptic cells. Therefore, the rate
stomach. The acid probably does not stimulate the
, and (2) stimulation
acetylcholine
types of signals: (1) stimulation of the
lation of acid secretion; it occurs in response to two
Regulation of Pepsinogen Secretion
The histamine
directly into the deep oxyntic glands.
body of the stomach, causing release of
transports the gastrin rapidly to the ECL cells in the
stomach. The vigorous mixing of the gastric juices
gastrin cells in the pyloric glands
reach the antral end of the stomach, some of the pro-
When meats or other protein-containing foods
798
Unit XII
Gastrointestinal Physiology
teins from these foods have a special stimulatory effect
on the
to cause
release of gastrin into the digestive juices of the
histamine
then acts quickly to stimulate gastric hydrochloric acid
secretion.
Regulation of pepsinogen secretion by the peptic cells
in the oxyntic glands is much less complex than regu-
peptic cells by
released from the vagus nerves or from
the gastric enteric nervous plexus
of peptic cell secretion in response to acid in the
peptic cells directly but instead elicits additional
enteric nervous reflexes that support the original
of secretion of pepsinogen, the precursor of the
enzyme pepsin
strongly influenced by the amount of acid in the
otherwise appear to be normal.
Phases of Gastric Secretion
cephalic phase
gastric phase,
and an
Cephalic Phase.
that cause the cephalic phase of gastric secretion origi-
nate in the cerebral cortex and in the appetite centers
mitted through the dorsal motor nuclei of the vagi and
phase of secretion normally accounts for about 20 per
cent of the gastric secretion associated with eating a
meal.
Gastric Phase.
(1) long vagovagal reflexes from the stomach to the
secretion of gastric juice during several hours while food
accounts for about 70 per cent of the total gastric secre-
tion associated with eating a meal and therefore
accounts for most of the total daily gastric secretion of
Intestinal Phase.
of small amounts of gastrin released by the duodenal
mucosa.
by Other Post-Stomach
Although intestinal chyme slightly stimulates gastric
secretion during the early intestinal phase of stomach
Vagal center
of medulla
Cephalic phase via vagus
Parasympathetics excite
pepsin and acid production
Intestinal phase:
1. Nervous mechanisms
2. Hormonal mechanisms
Circulatory system
Afferent
fibers
Vagus
trunk
Secretory
fiber
Small bowel
Gastrin
Food
Local nerve
plexus
Gastric phase:
1. Local nervous
secretory reflexes
2. Vagal reflexes
3. Gastrin-histamine
stimulation
Phases of gastric secretion and their regulation.
Figure 64–7
secreted into the intestinal tract. Trypsinogen is
cally. They become activated only after they are
, which are all inactive enzymati-
boxypolypeptidase
, and
chymotrypsinogen
When first synthesized in the pancreatic cells, the
phospholipids.
phospholipase,
, which causes hydrolysis of cholesterol esters;
cholesterol
into fatty acids and monoglycerides; (2)
, which is capable of hydrolyzing neutral fat
The main enzymes for fat digestion are (1)
to form mostly disaccharides and a few trisaccharides.
gen, and most other carbohydrates (except cellulose)
, which hydrolyzes starches, glyco-
The pancreatic enzyme for digesting carbohydrates
some proteins all the way to the amino acid state.
individual amino acids, thus completing digestion of
not cause release of individual amino acids. However,
Trypsin and chymotrypsin split whole and partially
. By far the most abundant of these
boxypolypeptidase
, and
chymotrypsin
The most important of the pancreatic enzymes for
ties of bicarbonate ions, which play an important role
carbohydrates, and fats. It also contains large quanti-
digesting all of the three major types of food: proteins,
creas. These are discussed in detail in Chapter 78.)
juice. Instead, insulin is secreted directly into the
, but this is not secreted by the same
the types of food in the chyme. (The pancreas also
tions of the small intestine, and the characteristics of
, surrounded by the
papilla of Vater
ducts leading from the acini. The combined product of
, and large volumes of sodium bicarbonate
to that of the salivary glands shown in Figure 64–2. The
stomach (illustrated in Figure 64–10), is a large com-
The pancreas, which lies parallel to and beneath the
Pancreatic Secretion
the natural gastrin. This synthetic product is called
alanine, has all the same physiologic properties as
A synthetic gastrin, composed of the terminal four
eight amino acids. All the amino acids in the secretin
the activity for cholecystokinin resides in the terminal
gastrin resides in the terminal four amino acids, and
ular chains are the same. The functional activity of
amino acids in the gastrin and cholecystokinin molec-
respectively, of 2000, 4200, and 3400. The terminal five
polypeptides with approximate molecular weights,
, and
cholecystokinin
Chemical Composition of Gastrin and
ment of peptic ulcers, as discussed in Chapter 66.
tion excites secretion at the onset of a meal. This
acidic) to 50 milliliters or more per hour, in very much
Unfortunately, emotional stimuli frequently increase
nonoxyntic type, composed mainly of
no digestion is occurring anywhere in the gut. The secre-
hour during the “interdigestive period,” when little or
The
that they reduce gastric secretion, as was discussed in
already filled or already overactive. In fact, the entero-
The functional purpose of inhibitory gastric secretion
, and
secretin opposes stomach secretion. Three other
for control of pancreatic secretion. However,
, which is especially important
causes release of several intestinal hormones. One
products, hyperosmotic or hypo-osmotic fluids, or
2. The presence of acid, fat, protein breakdown
This is part of the complex mechanism discussed in
breakdown products, or by irritation of the mucosa.
in the upper intestine, by the presence of protein
distending the small bowel, by the presence of acid
stomach secretion. This reflex can be initiated by
extrinsic sympathetic and vagus nerves, that inhibits
, transmitted through
1. The presence of food in the small intestine initiates
Secretory Functions of the Alimentary Tract
Chapter 64
799
a reverse enterogastric reflex
the myenteric nervous system as well as through
Chapter 63 for slowing stomach emptying when the
intestines are already filled.
any irritating factor in the upper small intestine
of these is secretin
hormones—gastric inhibitory peptide, vasoactive
intestinal polypeptide
somatostatin—also have
slight to moderate effects in inhibiting gastric
secretion.
by intestinal factors is presumably to slow passage of
chyme from the stomach when the small intestine is
gastric inhibitory reflexes plus inhibitory hormones
usually also reduce stomach motility at the same time
Chapter 63.
Gastric Secretion During the Interdigestive Period.
stomach secretes a few milliliters of gastric juice each
tion that does occur usually is almost entirely of the
mucus but little
pepsin and almost no acid.
interdigestive gastric secretion (highly peptic and
the same way that the cephalic phase of gastric secre-
increase of secretion in response to emotional stimuli is
believed to be one of the causative factors in develop-
Other Gastrointestinal Hormones
Gastrin,
secretin are all large
molecule are essential.
amino acids of natural gastrin plus the amino acid
pentagastrin.
pound gland with most of its internal structure similar
pancreatic digestive enzymes are secreted by pancre-
atic acini
solution are secreted by the small ductules and larger
enzymes and sodium bicarbonate then flows through
a long pancreatic duct that normally joins the hepatic
duct immediately before it empties into the duodenum
through the
sphinc-
ter of Oddi.
Pancreatic juice is secreted most abundantly in
response to the presence of chyme in the upper por-
the pancreatic juice are determined to some extent by
secretes insulin
pancreatic tissue that secretes intestinal pancreatic
blood—not into the intestine—by the islets of Langer-
hans that occur in islet patches throughout the pan-
Pancreatic Digestive Enzymes
Pancreatic secretion contains multiple enzymes for
in neutralizing the acidity of the chyme emptied from
the stomach into the duodenum.
digesting proteins are trypsin,
car-
is trypsin.
digested proteins into peptides of various sizes but do
carboxypolypeptidase does split some peptides into
is pancreatic amylase
pancre-
atic lipase
esterase
and (3)
which splits fatty acids from
proteolytic digestive enzymes are in the inactive
forms trypsinogen,
procar-
cholecystokinin, stimulate the acinar cells of the
The first two of these stimuli, acetylcholine and
, which is also secreted by the duodenal
, which is secreted by the
, which is released from the
Acetylcholine
Three basic stimuli are important in causing pancre-
Basic Stimuli That Cause Pancreatic Secretion
of water also into the pancreatic duct, thus
3. The overall movement of sodium and bicarbonate
neutrality for the secreted bicarbonate ions.
luminal border
This supplies the sodium ions (Na
cell by a secondary active transport process.
sodium ions through the blood border
exchanged for
2. The hydrogen ions formed by dissociation of
luminal border
). Then the bicarbonate ions
). The carbonic acid in turn
carbonic anhydrase, combines with water to form
cell from the blood and, under the influence of
1. Carbon dioxide diffuses to the interior of the
ductules and ducts are shown in Figure 64–8. They are
The basic steps in the cellular mechanism for secret-
ate ions in the plasma. This provides a large quantity
145 mEq/L, a value about five times that of bicarbon-
to secrete copious quantities of pancreatic juice, the
lead from the acini. When the pancreas is stimulated
juice, bicarbonate ions and water, are secreted mainly
secreted entirely by the acini of the pancreatic glands,
Secretion of Bicarbonate Ions
time of pancreatic insufficiency.
even if not lethal, it usually leads to a subsequent life-
. This sometimes is
entire pancreas within a few hours, giving rise to the
whelmed, in which case the pancreatic secretions
tions, the effect of trypsin inhibitor is often over-
damaged areas of the pancreas. Under these condi-
when a duct becomes blocked, large quantities of pan-
When the pancreas becomes severely damaged or
enzymes, trypsin inhibitor prevents activation of the
the acini and ducts of the pancreas. And, because it is
cytoplasm of the glandular cells, and it prevents acti-
. This substance is formed in the
digest the pancreas itself. Fortunately, the same cells
Secretion of Trypsin Inhibitor Prevents Digestion of the
in a similar manner.
motrypsin, and procarboxypolypeptidase is activated
in contact with the mucosa. Also, trypsinogen can be
, which is
800
Unit XII
Gastrointestinal Physiology
activated by an enzyme called enterokinase
secreted by the intestinal mucosa when chyme comes
autocatalytically activated by trypsin that has already
been formed from previously secreted trypsinogen.
Chymotrypsinogen is activated by trypsin to form chy-
Pancreas Itself.
It is important that the proteolytic
enzymes of the pancreatic juice not become activated
until after they have been secreted into the intestine
because the trypsin and the other enzymes would
that secrete proteolytic enzymes into the acini of the
pancreas secrete simultaneously another substance
called trypsin inhibitor
vation of trypsin both inside the secretory cells and in
trypsin that activates the other pancreatic proteolytic
others as well.
creatic secretion sometimes become pooled in the
rapidly become activated and can literally digest the
condition called acute pancreatitis
lethal because of accompanying circulatory shock;
Although the enzymes of the pancreatic juice are
the other two important components of pancreatic
by the epithelial cells of the ductules and ducts that
bicarbonate ion concentration can rise to as high as
of alkali in the pancreatic juice that serves to neutral-
ize the hydrochloric acid emptied into the duodenum
from the stomach.
ing sodium bicarbonate solution into the pancreatic
the following:
carbonic acid (H
2
CO
3
dissociates into bicarbonate ions and hydrogen
ions (HCO
3
_
and H
+
are actively transported in association with
sodium ions (Na
+
) through the
of
the cell into the lumen of the duct.
carbonic acid inside the cell are
of the
+
) that are
transported through the
into the
pancreatic duct lumen to provide electrical
ions from the blood into the duct lumen creates
an osmotic pressure gradient that causes osmosis
forming an almost completely isosmotic
bicarbonate solution.
Regulation of Pancreatic Secretion
atic secretion:
1.
parasympathetic vagus nerve endings and from
other cholinergic nerves in the enteric nervous
system
2. Cholecystokinin
duodenal and upper jejunal mucosa when food
enters the small intestine
3. Secretin
and jejunal mucosa when highly acid food enters
the small intestine
Blood
Lumen
Ductule cells
(Active
transport)
(Active
transport)
(Carbonic anhydrase)
Na
+
Na
+
H
+
Na
+
H
+
HCO
3
-
HCO
3
H
2
CO
3
H
2
O
+
CO
2
CO
2
H
2
O H
2
O
creatic ductules and ducts.
Secretion of isosmotic sodium bicarbonate solution by the pan-
Figure 64–8
num) stimulated by cholecystokinin.
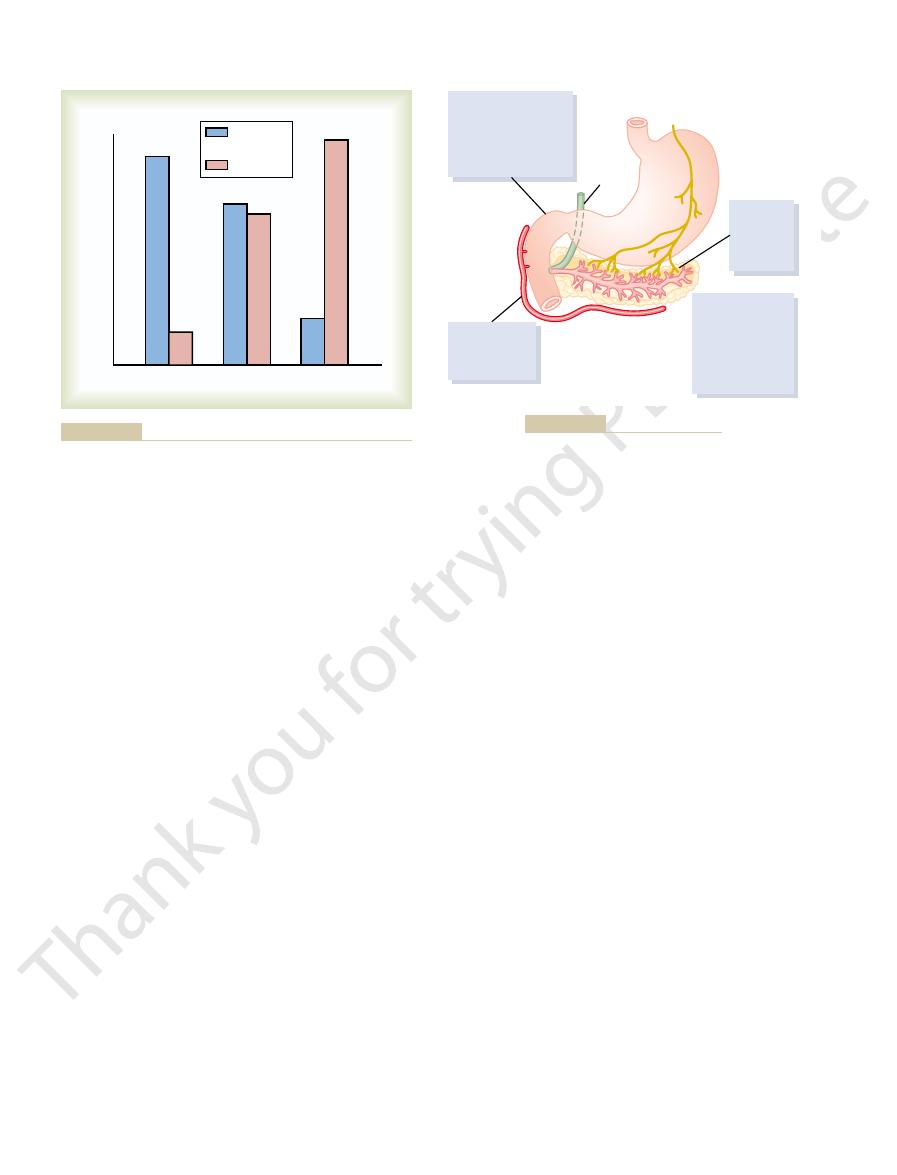
response to soap (a fat), and (3) intense digestive
denum, stimulated by secretin, (2) a dual effect in
Figure 64–9, which demonstrates (1) intense sodium
effects of secretin and cholecystokinin are shown in
The differences between the pancreatic stimulatory
ulation but even more pronounced, accounting for 70
cells. This effect is similar to that caused by vagal stim-
Cholecystokinin, like secretin, passes by way of the
long-chain fatty acids
num and upper jejunum. This release of cholecys-
, in the mucosa of the duode-
group of cells, the
taining 33 amino acids, to be released from yet another
, a polypeptide con-
cholecystokinin
second hormone,
The presence
Its Contribution to Control of Diges-
tion averages 8.0.
Fortunately, the pH of the sodium bicarbonate secre-
alkaline or neutral medium, at a pH of 7.0 to 8.0.
tive enzymes, which function optimally in a slightly
prevent development of duodenal ulcers, as is dis-
juice, this is an essential protective mechanism to
blocked. Because the mucosa of the small intestine
neutralized, so that further peptic digestive activity by
ride in the duodenum. In this way, the acid contents
lungs, thus leaving a neutral solution of sodium chlo-
into carbon dioxide and water. The carbon dioxide
Then the carbonic acid immediately dissociates
of sodium bicarbonate. The net result is then the fol-
pH falls to 3.0. This immediately causes copious secre-
below 4.5 to 5.0, and its release increases greatly as the
especially important for two reasons: First, secretin
tration of chloride ion. The secretin mechanism is
bicarbonate ion (up to 145 mEq/L) but a low concen-
absorbed into the blood. The one truly potent con-
release and activation of secretin, which is then
num from the stomach, it causes duodenal mucosal
mucosa of the duodenum and jejunum. When acid
inactive form, prosecretin, in so-called S cells in the
acids (molecular weight about 3400), present in an
Secretin is a polypeptide, containing 27 amino
Neutralization of Acidic Stomach
becomes copious, mainly in response to the hormone
enters the small intestine, pancreatic secretion
meal. But, again, only small amounts reach the duo-
enzyme secretion continues, accounting for another 5
During the gastric phase, the nervous stimulation of
enzymes.
of pancreatic enzymes after a meal. But little of the
in the pancreas. This causes moderate amounts of
of pancreatic secretion, the same nervous signals from
as follows.
. Their characteristics are
, and the
, the
as for gastric secretion: the
Pancreatic secretion occurs in three phases, the same
Phases of Pancreatic Secretion
stimuli, not from one alone.
one another. Thus, pancreatic secretion normally
various stimuli are said to “multiply,” or “potentiate,”
tions caused by each one separately. Therefore, the
ferent stimuli of pancreatic secretion occur at once, the
When all the dif-
basic stimuli, stimulates secretion of large quantities of
the duodenum. Secretin, in contrast to the first two
enzymes. Without the water, most of the enzymes
pancreas, causing production of large quantities of
Secretory Functions of the Alimentary Tract
Chapter 64
801
pancreatic digestive enzymes but relatively small
quantities of water and electrolytes to go with the
remain temporarily stored in the acini and ducts until
more fluid secretion comes along to wash them into
water solution of sodium bicarbonate by the pancre-
atic ductal epithelium.
Multiplicative Effects of Different Stimuli.
total secretion is far greater than the sum of the secre-
results from the combined effects of the multiple basic
cephalic phase
gastric
phase
intestinal phase
Cephalic and Gastric Phases.
During the cephalic phase
the brain that cause secretion in the stomach also
cause acetylcholine release by the vagal nerve endings
enzymes to be secreted into the pancreatic acini,
accounting for about 20 per cent of the total secretion
secretion flows immediately through the pancreatic
ducts into the intestine because only small amounts of
water and electrolytes are secreted along with the
to 10 per cent of pancreatic enzymes secreted after a
denum because of continued lack of significant fluid
secretion.
Intestinal Phase.
After chyme leaves the stomach and
secretin.
Secretin Stimulates Secretion of Copious Quantities of
Bicarbonate Ions—
Chyme.
chyme with pH less than 4.5 to 5.0 enters the duode-
stituent of chyme that causes this secretin release is the
hydrochloric acid from the stomach.
Secretin in turn causes the pancreas to secrete large
quantities of fluid containing a high concentration of
begins to be released from the mucosa of the small
intestine when the pH of the duodenal contents falls
tion of pancreatic juice containing abundant amounts
lowing reaction in the duodenum:
is absorbed into the blood and expired through the
emptied into the duodenum from the stomach become
the gastric juices in the duodenum is immediately
cannot withstand the digestive action of acid gastric
cussed in further detail in Chapter 66.
Bicarbonate ion secretion by the pancreas provides
an appropriate pH for action of the pancreatic diges-
Cholecystokinin—
tive Enzyme Secretion by the Pancreas.
of food in the upper small intestine also causes a
I cells
tokinin results especially from the presence of
proteoses and peptones (products of partial protein
digestion) and
in the chyme
coming from the stomach.
blood to the pancreas but instead of causing sodium
bicarbonate secretion causes mainly secretion of still
much more pancreatic digestive enzymes by the acinar
to 80 per cent of the total secretion of the pancreatic
digestive enzymes after a meal.
bicarbonate secretion in response to acid in the duo-
enzyme secretion (when peptones enter the duode-
+
Æ
+
3
2
3
HCl NaHCO
NaCl H CO
tion of chloride ions, water, and most other diffusible
epithelium, and this is followed by secondary absorp-
lecithin, and bilirubin.
constituents that contain the bile salts, cholesterol,
bladder mucosa, concentrating the remaining bile
water, sodium, chloride, and most other small elec-
can hold is only 30 to 60 milliliters. Nevertheless, as
duodenum. The maximum volume that the gallbladder
secreted continually by the liver cells, but most of it is
Storing and Concentrating Bile in the Gallbladder.
, which causes
much as an additional 100 per cent. The second secre-
that line the ductules and ducts. This second secretion
of liver secretion is added to the initial bile. This addi-
In its course through the bile ducts, a second portion
, shown in Figure 64
From these the bile either empties directly
ducts,
interlobular septa, where the canaliculi empty into
(2) Next, the bile
that originate between the hepatic cells.
organic constituents. It is secreted into minute
large amounts of bile acids, cholesterol, and other
; this initial secretion contains
the liver, the
Bile is secreted in two stages by the liver: (1) The initial
Physiologic Anatomy of
cholesterol
hemoglobin destruction, and excesses of
, an end product of
These include especially
Second, bile serves as a means for excretion of
the intestinal mucosal membrane.
enzymes secreted in pancreatic juice, and (2) they aid
fat particles of the food into many minute particles,
bile do two things: (1) they help to emulsify the large
that cause fat digestion, but because
and absorption, not because of any enzymes in the bile
First, bile plays an important role in fat digestion
normally between 600 and 1000 ml/day. Bile serves two
Functions of the Biliary Tree
Secretion of Bile by the Liver;
total amount secreted each day is about 1 liter.
factors in the regulation of pancreatic secretion. The
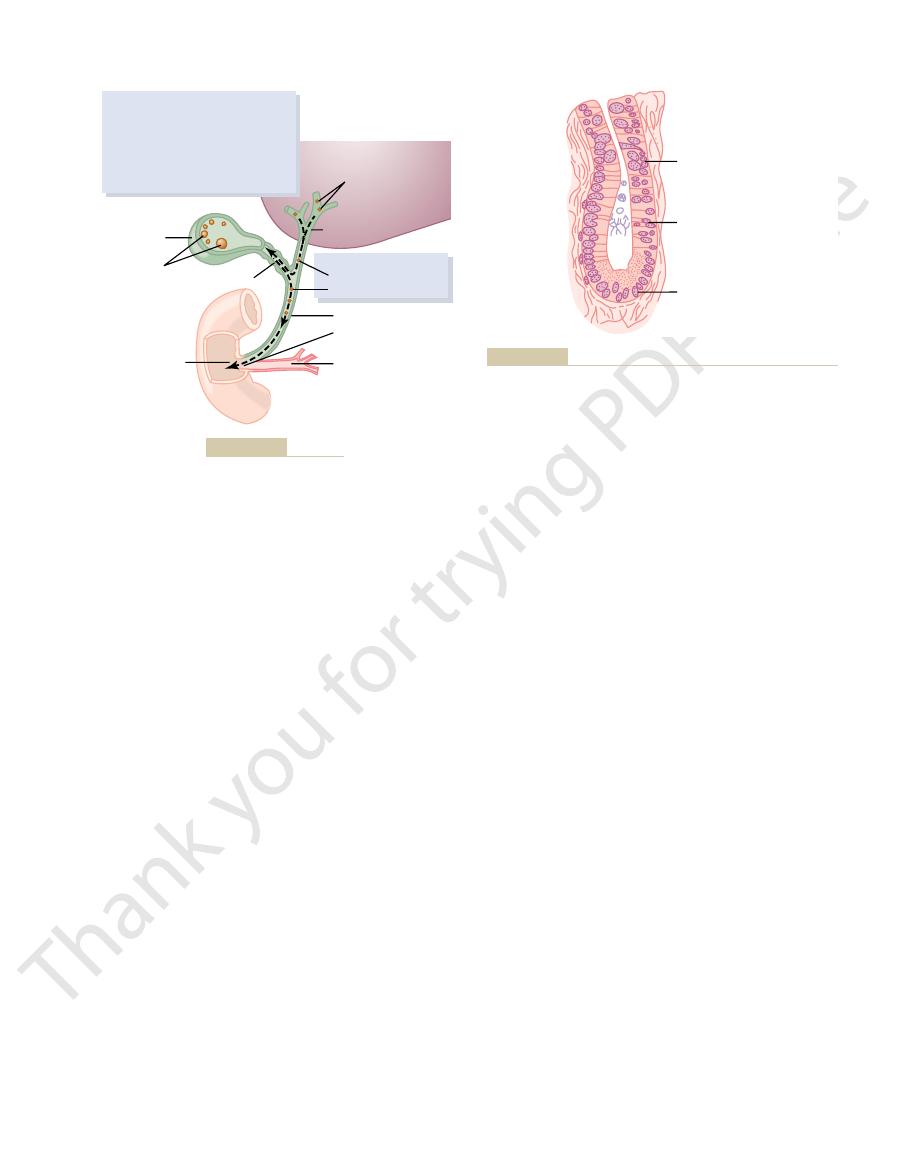
Figure 64
802
Unit XII
Gastrointestinal Physiology
–10 summarizes the more important
One of the many functions of the liver is to secrete bile,
important functions:
bile acids in the
the surface of which can then be attacked by lipase
in absorption of the digested fat end products through
several important waste products from the blood.
bilirubin
.
Biliary Secretion
portion is secreted by the principal functional cells of
hepatocytes
bile
canaliculi
flows in the canaliculi toward the
ter-
minal bile ducts and then into progressively larger
finally reaching the hepatic duct and common
bile duct.
into the duodenum or is diverted for minutes up to
several hours through the cystic duct into the gall-
bladder
–11.
tional secretion is a watery solution of sodium and
bicarbonate ions secreted by secretory epithelial cells
sometimes increases the total quantity of bile by as
tion is stimulated especially by secretin
release of additional quantities of bicarbonate ions to
supplement the bicarbonate ions in pancreatic secre-
tion (for neutralizing acid that empties into the duo-
denum from the stomach).
Bile is
normally stored in the gallbladder until needed in the
much as 12 hours of bile secretion (usually about 450
milliliters) can be stored in the gallbladder because
trolytes are continually absorbed through the gall-
Most of this gallbladder absorption is caused by
active transport of sodium through the gallbladder
HCI
Soap
Peptone
Water and
NaHCO
3
Enzymes
Rate of pancreatic secretion
the pancreas, caused by the presence of acid (HCl), fat (soap),
), water, and enzyme secretion by
Figure 64–9
Sodium bicarbonate (NaHCO
3
or peptone solutions in the duodenum.
Vagal
stimulation
releases
enzymes
into acini
Secretin causes
copious secretion
of pancreatic fluid
and bicarbonate;
cholecystokinin
causes secretion
of enzymes
Acid from stomach
releases secretin from
wall of duodenum;
fats and amino acids
cause release of
cholecystokinin
Common
bile duct
Secretin and
cholecystokinin
absorbed into
blood stream
Regulation of pancreatic secretion.
Figure 64–10
to the cholecystokinin stimulus that itself is initiated
In summary, the gallbladder empties its store of con-
enteric nervous system. They are the same nerves that
In addition to cholecystokinin, the gallbladder is
acinar cells of the pancreas. The stimulus for cholecys-
This is the same cholecystokinin discussed earlier that
cholecystokinin
the gallbladder, but effective emptying also requires
30 minutes after a meal. The mechanism of gallblad-
gastrointestinal tract, the gallbladder begins to empty,
When food begins to be digested in the upper
Emptying of the Gallbladder—Stimulatory Role of Cholecys-
highly concentrated in the gallbladder bile.
lecithin, are not reabsorbed and, therefore, become
mucosa; essentially all other constituents, especially
In the concentrating process in the gallbladder,
, and the usual
cholesterol
about one half of the total solutes also in the bile. Also
, which account for
it has been concentrated in the gallbladder. This table
Table 64
about 5-fold, but it can be concentrated up to a
constituents. Bile is normally concentrated in this way
Secretory Functions of the Alimentary Tract
Chapter 64
803
maximum of 20-fold.
Composition of Bile.
–2 gives the composition of
bile when it is first secreted by the liver and then after
shows that by far the most abundant substances
secreted in the bile are bile salts
secreted or excreted in large concentrations are biliru-
bin,
, lecithin
electrolytes of
plasma.
water and large portions of the electrolytes (except
calcium ions) are reabsorbed by the gallbladder
the bile salts and the lipid substances cholesterol and
tokinin.
especially when fatty foods reach the duodenum about
der emptying is rhythmical contractions of the wall of
simultaneous relaxation of the sphincter of Oddi,
which guards the exit of the common bile duct into the
duodenum.
By far the most potent stimulus for causing the gall-
bladder contractions is the hormone
.
causes increased secretion of digestive enzymes by the
tokinin entry into the blood from the duodenal
mucosa is mainly the presence of fatty foods in the
duodenum.
stimulated less strongly by acetylcholine-secreting
nerve fibers from both the vagi and the intestinal
promote motility and secretion in other parts of the
upper gastrointestinal tract.
centrated bile into the duodenum mainly in response
Stomach
Acid
Liver
Bile acids via blood
stimulate parenchymal
secretion
Secretin via
blood stream
stimulates
liver ductal
secretion
Bile stored and
concentrated up
to 15 times in
gallbladder
Cholecystokinin via blood stream causes:
1. Gallbladder contraction
2. Relaxation of sphincter of Oddi
Vagal stimulation
causes weak
contraction of
gallbladder
Pancreas
Sphincter of
Oddi
Duodenum
Liver secretion and gallbladder emptying.
Figure 64–11
Table 64–2
100 mEq/L
25 mEq/L
5 mEq/L
23 mEq/L
5 mEq/L
12 mEq/L
145.04 mEq/L
130 mEq/L
Lecithin
0.04 g/dl
0.3 g/dl
Fatty acids
0.12 g/dl
0.3 to 1.2 g/dl
Cholesterol
0.1 g/dl
0.3 to 0.9 g/dl
Bilirubin
0.04 g/dl
0.3 g/dl
Bile salts
1.1 g/dl
6 g/dl
Water
97.5 g/dl
92 g/dl
Liver Bile
Gallbladder Bile
Composition of Bile
Na
+
K
+
Ca
++
Cl
-
28 mEq/L
10 mEq/L
HCO
3
-
mucosa, sometimes allowing excessive absorption of
resulting from low-grade chronic infection, may also
ammation of the gallbladder epithelium, often
development of gallstones.
metabolism in the body. For this reason, people on a
by the quantity of fat that the person eats, because liver
12. The
, as shown in Figure 64
cholesterol gallstones
cipitate in the gallbladder, resulting in the formation of
Under abnormal conditions, the cholesterol may pre-
terol, which keeps the cholesterol in solution.
concentrated in the gallbladder, the bile salts and
in more detail in Chapter 65. When the bile becomes
in the form of a colloidal solution, as explained
water, but the bile salts and lecithin in bile combine
day.
bile salts, about 1 to 2 grams of cholesterol are removed
terol in the blood plasma. In the process of secreting the
Liver Secretion of Cholesterol and
ducts.
stomach. Thus, the secretin feedback mechanism for
themselves. The bicarbonate in turn passes into the
by the epithelial cells of the bile ductules and ducts, and
a meal. This increase in secretion is almost entirely
pancreatic secretion increases bile secretion, sometimes
bile secretion, the hormone
This demonstrates that the daily rate of liver bile salt
duction of bile salts 6- to 10-fold, which increases the
reabsorbed from the ileum, the liver increases its pro-
several hundred milliliters per day.
greater the rate of bile secretion. Indeed, ingestion of
culation (usually a total of only about 2.5 grams), the
The quantity of bile secreted by the liver each day is
salts.
continually by the liver cells. This recirculation of the
carried out in the feces. The small quantities of bile salts
recirculated into the bile, so that on the average these
In this way, about 94 per cent of all the bile salts are
resecreted into the bile.
to the liver. On reaching the liver, on
ileum. They then enter the portal blood and pass back
small intestine, about one half of this by
nutrient loss.
the ingested fats are lost into the feces, and the person
of bile salts in the intestinal tract, up to 40 per cent of
described in detail in Chapter 65.Without the presence
they are then absorbed into the blood, as will be
in this form to the intestinal mucosa, where
charges of the bile salts. The intestinal lipids are
, and they are
lipids; the complexes are called
(4) other lipids from the intestinal tract. They do this
(1) fatty acids, (2) monoglycerides, (3) cholesterol, and
fying function, bile salts help in the absorption of
Second, and even more important than the emulsi-
salts.
to break the fat globules into minute sizes. This is
cles in the food. This decreases the surface tension of
First, they have a detergent action on the fat parti-
The bile salts have two important actions in the
sodium salts, are then secreted in the bile.
. The salts of these acids, mainly
in about equal quantities. These
nodeoxycholic acid
che-
cholic acid
liver cells during the course of fat metabolism. The
cholesterol
daily. The precursor of the bile salts is
The liver cells synthesize about 6 grams of
Function of Bile Salts in Fat Digestion
bladder, and its ultimate release from the bladder to
marizes the secretion of bile, its storage in the gall-
empties completely in about 1 hour. Figure 64
quantities of fat are present, the gallbladder normally
the gallbladder empties poorly, but when signi
mainly by fatty foods. When fat is not in the food,
804
Unit XII
Gastrointestinal Physiology
ficant
–11 sum-
the duodenum.
and Absorption
bile salts
,
which is either present in the diet or synthesized in the
cholesterol is first converted to
or
acids in turn combine principally with glycine and to a
lesser extent with taurine to form glyco- and tauro-
conjugated bile acids
intestinal tract:
the particles and allows agitation in the intestinal tract
called the emulsifying or detergent function of bile
by forming very small physical complexes with these
micelles
semi-soluble in the chyme because of the electrical
“ferried”
often develops a metabolic deficit because of this
Enterohepatic Circulation of Bile Salts.
About 94 per cent of
the bile salts are reabsorbed into the blood from the
diffusion
through the mucosa in the early portions of the small
intestine and the remainder by an active transport
process through the intestinal mucosa in the distal
first passage
through the venous sinusoids these salts are absorbed
almost entirely back into the hepatic cells and then are
salts make the entire circuit some 17 times before being
lost into the feces are replaced by new amounts formed
bile salts is called the enterohepatic circulation of bile
highly dependent on the availability of bile salts—the
greater the quantity of bile salts in the enterohepatic cir-
supplemental bile salts can increase bile secretion by
If a bile fistula empties the bile salts to the exterior
for several days to several weeks so that they cannot be
rate of bile secretion most of the way back to normal.
secretion is actively controlled by the availability (or
lack of availability) of bile salts in the enterohepatic
circulation.
Role of Secretin in Helping to Control Bile Secretion.
In addi-
tion to the strong stimulating effect of bile acids to cause
secretin that also stimulates
more than doubling its secretion for several hours after
secretion of a sodium bicarbonate-rich watery solution
not increased secretion by the liver parenchymal cells
small intestine and joins the bicarbonate from the pan-
creas in neutralizing the hydrochloric acid from the
neutralizing duodenal acid operates not only through its
effects on pancreatic secretion but also to a lesser extent
through its effect on secretion by the liver ductules and
Gallstone Formation
Bile salts are formed in the hepatic cells from choles-
from the blood plasma and secreted into the bile each
Cholesterol is almost completely insoluble in pure
physically with the cholesterol to form ultramicroscopic
micelles
lecithin become concentrated along with the choles-
–
amount of cholesterol in the bile is determined partly
cells synthesize cholesterol as one of the products of fat
high-fat diet over a period of years are prone to the
Infl
change the absorptive characteristics of the gallbladder
water and bile salts but leaving behind the cholesterol
ions together cause osmotic movement of water.
uid. Finally, all these
crypts and (2) active secretion of bicarbonate ions. The
processes: (1) active secretion of chloride ions into the
The exact
Mechanism of Secretion of the Watery Fluid.
chyme when it comes in contact with the villi. Thus, the
secretions also are rapidly reabsorbed by the villi. This
a slightly alkaline pH in the range of 7.5 to 8.0. The
cytes of the crypts at a rate of about 1800 ml/day. These
The intestinal secretions are formed by the entero-
cent villi, reabsorb the water and electrolytes along
water and electrolytes and, over the surfaces of adja-
, which, in the crypts, secrete large quantities of
intestinal surfaces, and (2) a large number of
types of cells: (1) a moderate number of
the intestinal villi. The surfaces of both the crypts and
13. These crypts lie between
is illustrated in Figure 64
, one of which
Juices by the Crypts of Lieberk
Secretion of Intestinal Digestive
ulcers in about 50 per cent of ulcer patients.
ulation; therefore, such stimulation in very excitable
of bicarbonate ions, which add to the bicarbonate ions
stomach. In addition, the mucus contains a large excess
The function of the mucus secreted by Brunner
(3) gastrointestinal hormones, especially
concurrently with increase in stomach secretion; and
stimuli on the duodenal mucosa; (2) vagal stimulation,
the duodenum. These glands secrete large amounts of
Vater where pancreatic secretion and bile empty into
rst few centimeters of the duodenum, mainly
, is located in the wall of the
An extensive array of compound mucous glands,
Glands in the Duodenum
Secretions of the
gallstones.
amed mucosa, but then progressing to large
Then the cholesterol begins to precipitate,
in the bladder in progressively greater concentrations.
Secretory Functions of the Alimentary Tract
Chapter 64
805
first forming
many small crystals of cholesterol on the surface of
the infl
Small Intestine
Secretion of Mucus by Brunner’s
called Brunner’s glands
fi
between the pylorus of the stomach and the papilla of
alkaline mucus in response to (1) tactile or irritating
which causes increased Brunner’s glands secretion
secretin.
’s
glands is to protect the duodenal wall from digestion
by the highly acid gastric juice emptying from the
from pancreatic secretion and liver bile in neutralizing
the hydrochloric acid entering the duodenum from the
stomach.
Brunner’s glands are inhibited by sympathetic stim-
persons is likely to leave the duodenal bulb unpro-
tected and is perhaps one of the factors that cause this
area of the gastrointestinal tract to be the site of peptic
ühn
Located over the entire surface of the small intestine
are small pits called crypts of Lieberkühn
–
the villi are covered by an epithelium composed of two
goblet cells,
which secrete mucus that lubricates and protects the
entero-
cytes
with end products of digestion.
secretions are almost pure extracellular fluid and have
flow of fluid from the crypts into the villi supplies a
watery vehicle for absorption of substances from
primary function of the small intestine is to absorb
nutrients and their digestive products into the blood.
mechanism that controls the marked secretion of
watery fluid by the crypts of Lieberkühn is not known.
It is believed to involve at least two active secretory
secretion of both of these ions causes electrical drag
as well of positively charged sodium ions through the
membrane and into the secreted fl
Course followed by bile:
1. During rest
2. During digestion
Liver
Stones
Hepatic duct
Common bile duct
Sphincter of Oddi
Pancreatic duct
Duodenum
Papilla of Vater
Cystic duct
Stones
Gallbladder
Causes of gallstones:
1. Too much absorption of water
from bile
2. Too much absorption of bile
acids from bile
3. Too much cholesterol in bile
4. Inflammation of epithelium
Formation of gallstones.
Figure 64–12
Paneth cell
Epithelial cell
Mucous goblet
cell
between the villi, which secretes almost pure extracellular fluid.
, found in all parts of the small intestine
crypt of Lieberkühn
Figure 64–13
A
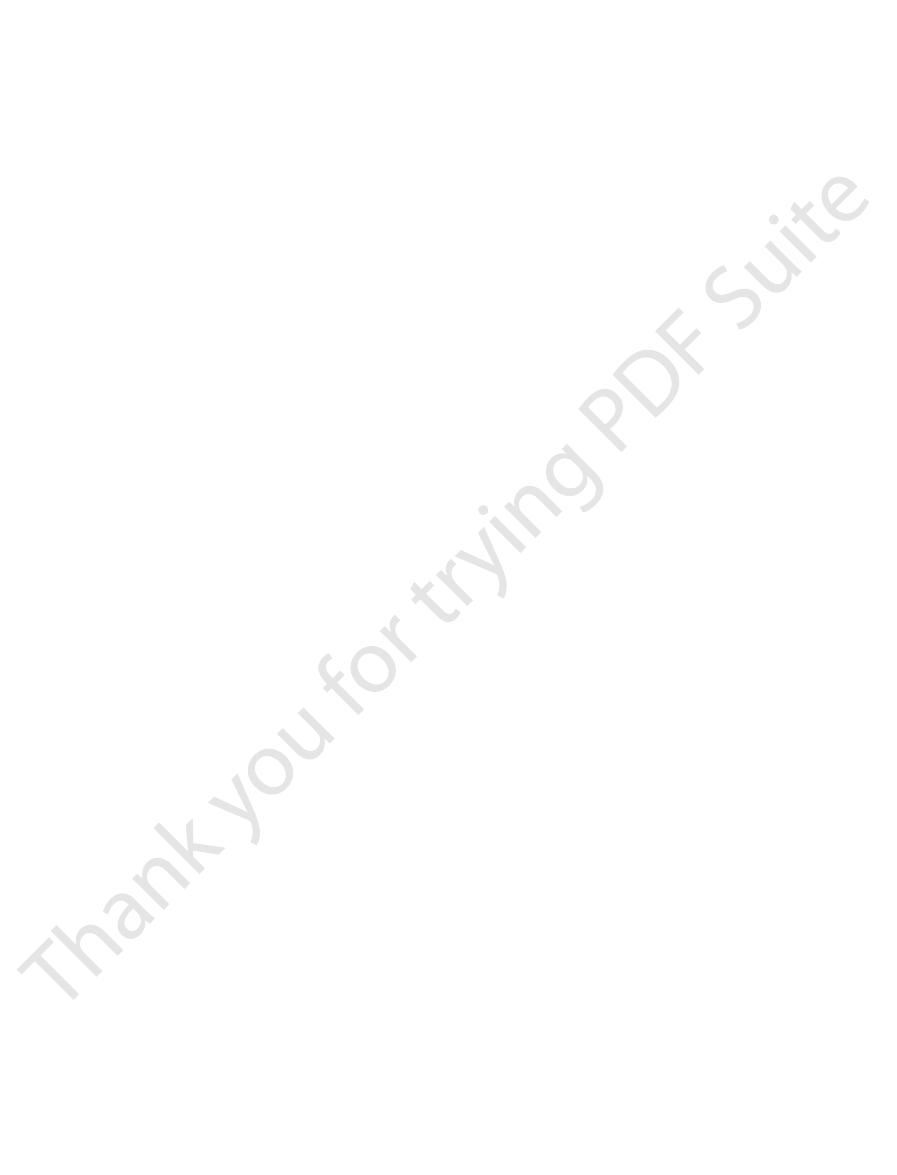
acid synthesis. Annu Rev Biochem 72:137, 2003.
Russell DW: The enzymes, regulation, and genetics of bile
disease. Curr Gastroenterol Rep 6:151, 2004.
Portincasa P, Di Ciaula A, vanBerge-Henegouwen GP:
bladder function. News Physiol Sci 13:64, 1998.
Marve GM: Nerves and hormones interact to control gall-
between membrane transporters. JOP 2(4 Suppl):203,
Lee MG, Ahn W, Lee JA, Kim JY, et al: Coordination of pan-
tion in secretory cells. Annu Rev Physiol 62:493, 2000.
Kidd JF, Thorn P: Intracellular Ca
Mosby, 2001.
Johnson LR: Gastrointestinal Physiology, 6th ed. St. Louis:
trointestinal tract: a review. J Cell Mol Med 5:327, 2001.
Jass JR, Walsh MD: Altered mucin expression in the gas-
gene regulation. Ann N Y Acad Sci 1014:97, 2004.
Hocker M: Molecular mechanisms of gastrin-dependent
284:G551, 2003.
challenges. Am J Physiol Gastrointest Liver Physiol
ulation of bile acid synthesis: past progress and future
Fuchs M: Bile acid regulation of hepatic physiology: III. Reg-
secretion and mucosal protection. News Physiol Sci 16:23,
Flemstrom G, Isenberg JI: Gastroduodenal mucosal alkaline
ucts. Physiol Rev 76:767,1996.
gene expression, processing, and targeting of active prod-
Dockray GJ, Varro A, Dimaline R: Gastric endocrine cells:
63:119, 2001.
production and biological activities. Annu Rev Physiol
Dockray GJ,Varro A, Dimaline R,Wang T:The gastrins: their
test Liver Physiol 284:G349, 2003.
Bile acids and nuclear receptors. Am J Physiol Gastroin-
Chiang JY: Bile acid regulation of hepatic physiology: III.
Rev Physiol 62:535, 2000.
epithelium: molecular basis and regulatory aspects. Annu
Barrett KE, Keely SJ: Chloride secretion by the intestinal
recovery from the disease than might otherwise occur.
washes away irritant factors, which promotes earlier
ties of water and electrolytes. But the diarrhea also
anus. The result is
alkaline mucus. This acts to dilute the irritating factors
, the mucosa secretes extra large quantities of
large intestine becomes intensely irritated, as occurs
Whenever a segment of the
Diarrhea Caused by Excess Secretion of Water and Electrolytes
nally, the mucus plus the alka-
inside the feces, and,
Furthermore, it protects the intestinal wall from the
adherent medium for holding fecal matter together.
wall against excoriation, but in addition, it provides an
often as every 30 minutes; this mucus often contains
caused by emotional disturbances, so much mucus can
During extreme parasympathetic stimulation, often
colon, which was discussed in Chapter 63.
can cause marked increase in mucus secretion. This
distal one half to two thirds of the large intestine, also
cord, which carry
by direct, tactile stimulation of the epithelial cells
The rate of secretion of mucus is regulated principally
mucus-secreting epithelial cells.
This mucus
mucus.
that secrete only mucus. The great preponderance of
enzymes. Instead, they consist mainly of mucous cells
are no villi. The epithelial cells contain almost no
hn; however, unlike the small intestine, there
that of the small intestine, has many crypts of
The mucosa of the large intestine, like
Large Intestine
Secretions of the
stimuli from the chyme in the intestines.
exes,
Regulation of Small Intestine
of an intestinal epithelial cell is about 5 days. This rapid
nally shed into the intestinal secretions. The life cycle
digestive enzymes. As the villus cells age, they are
crypts toward the tips of the villi, thus continually
continually undergo mitosis, and new cells migrate
The epithelial cells deep in the crypts of Lieberk
acids.
monosaccharides, and (3) small amounts of
, and
amino acids, (2) four enzymes
the epithelium. These enzymes are the following:
villi, do contain digestive enzymes that digest speci
terocytes of the mucosa, especially those that cover the
cellular debris, they have almost no enzymes. The en-
When
806
Unit XII
Gastrointestinal Physiology
Digestive Enzymes in the Small Intestinal Secretion.
secretions of the small intestine are collected without
fic
food substances while they are being absorbed through
(1) several peptidases for splitting small peptides into
—sucrase, maltase, iso-
maltase
lactase—for splitting disaccharides into
intestinal
lipase for splitting neutral fats into glycerol and fatty
ühn
along the basement membrane upward out of the
replacing the villus epithelium and also forming new
fi
growth of new cells also allows rapid repair of excori-
ations that occur in the mucosa.
Secretion—Local Stimuli
By far the most important means for regulating small
intestine secretion are local enteric nervous refl
especially reflexes initiated by tactile or irritative
Mucus Secretion.
Lieberkü
secretion in the large intestine is
contains moderate amounts of bicarbonate ions
secreted by a few non–
lining the large intestine and by local nervous reflexes
to the mucous cells in the crypts of Lieberkühn.
Stimulation of the pelvic nerves from the spinal
parasympathetic innervation to the
occurs along with increase in peristaltic motility of the
occasionally be secreted into the large intestine that
the person has a bowel movement of ropy mucus as
little or no fecal material.
Mucus in the large intestine protects the intestinal
great amount of bacterial activity that takes place
fi
linity of the secretion (pH of 8.0 caused by large
amounts of sodium bicarbonate) provides a barrier to
keep acids formed in the feces from attacking the
intestinal wall.
in Response to Irritation.
when bacterial infection becomes rampant during
enteritis
water and electrolytes in addition to the normal viscid
and to cause rapid movement of the feces toward the
diarrhea, with loss of large quanti-
References
2001.
2+
and Cl
-
channel activa-
creatic HCO
3
_
secretion by protein-protein interaction
2001.
Smooth muscle function and dysfunction in gallbladder

Sci 971:389, 2002.
n-like cells. Ann N Y Acad
Zanner R, Gratzl M, Prinz C: Circle of life of secretory vesi-
Physiol 63:77, 2001.
digestive enzymes in pancreatic acinar cells. Annu Rev
by cholecystokinin-regulating synthesis and secretion of
Williams JA: Intracellular signaling mechanisms activated
acterization, function, and regulation. Physiol Rev 83:633,
Trauner M, Boyer JL: Bile salt transporters: molecular char-
spective. Anat Rec 264:121, 2001.
from an ultrastructural, functional, and evolutionary per-
striated ducts of mammalian major salivary glands: review
Tandler B, Gresik EW, Nagato T, Phillips CJ: Secretion by
Secretory Functions of the Alimentary Tract
Chapter 64
807
2003.
cles in gastric enterochromaffi
