tion with the portal veins and can be summarized as follows.
The function of the hepatic vascular system is discussed in Chapter 15 in connec-
Hepatic Vascular and Lymph Systems
large portions of the plasma proteins diffuse freely into these spaces.
endothelium, substances in the plasma move freely into the spaces of Disse. Even
these spaces is removed through the lymphatics. Because of the large pores in the
connect with lymphatic vessels in the interlobular septa. Therefore, excess fluid in
The millions of spaces of Disse
perisinusoidal spaces.
, also known as the
endothelial cells and the hepatic cells, are narrow tissue spaces called the
are almost 1 micrometer in diameter. Beneath this lining, lying between the
The endothelial lining of the sinusoids has extremely large pores, some of which
capable of phagocytizing bacteria and other foreign matter in the hepatic sinus
loendothelial cells), which are resident macrophages that line the sinusoids and are
Kupffer cells
of cell: (1) typical
In addition to the hepatic cells, the venous sinusoids are lined by two other types
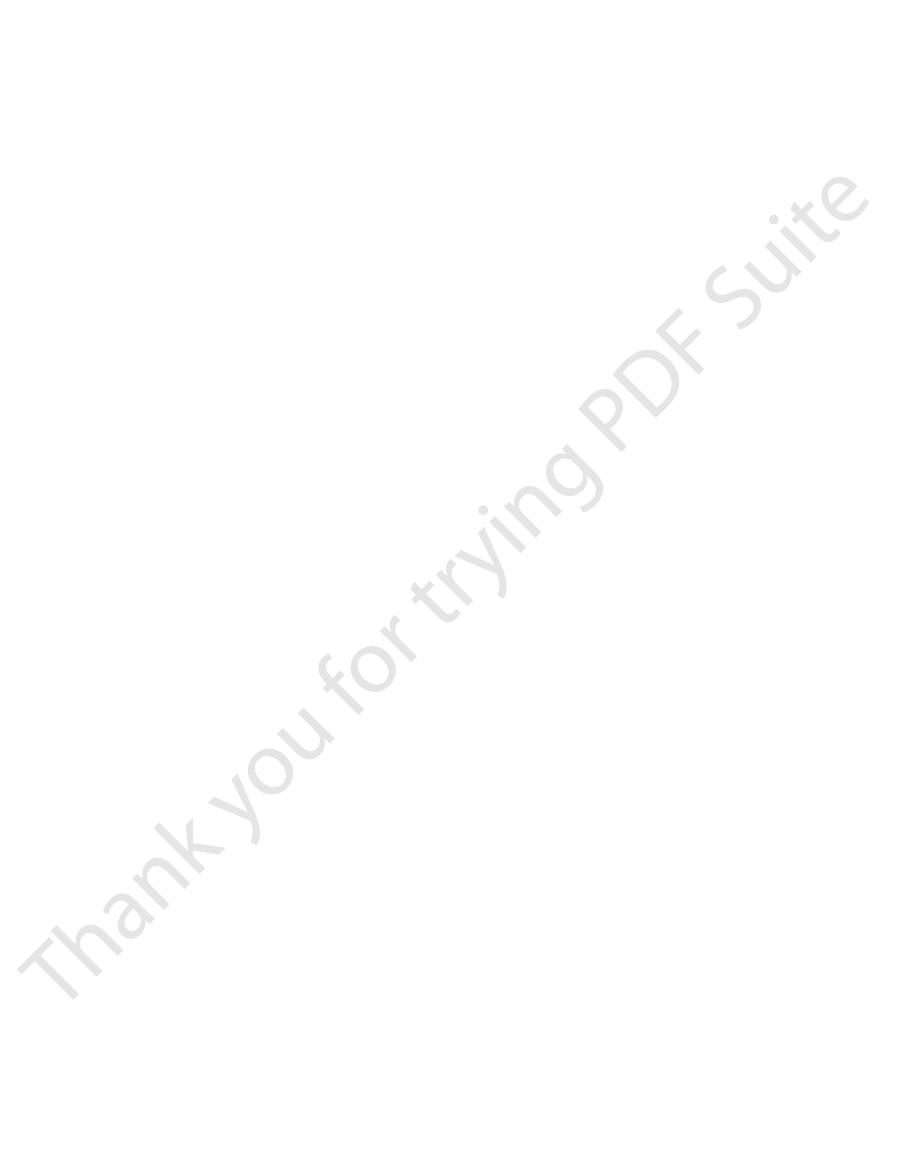
septa, as shown in Figure 70–1.
of the small arterioles also empty directly into the hepatic sinusoids, most frequently
supply arterial blood to the septal tissues between the adjacent lobules, and many
are also present in the interlobular septa. These arterioles
hepatic plates and then into the central vein. Thus, the hepatic cells are exposed con-
venules blood flows into flat, branching
venous outflow of the gastrointestinal tract by way of the portal vein. From these
lobules.
hepatic plate is usually two cells thick, and between the adjacent cells lie small
shown in Figure 70–1) that radiate from the central vein like spokes in a wheel. Each
that empties into the hepatic veins and then into the vena cava. The
The liver lobule, shown in cut-away format in Figure 70–1, is constructed around
100,000 individual lobules.
length and 0.8 to 2 millimeters in diameter. The human liver contains 50,000 to
which is a cylindrical structure several millimeters in
liver lobule,
body weight, or about 1.5 kg in the average adult human. The basic functional unit
The liver is the largest organ in the body, contributing about 2 per cent of the total
of vitamins and iron; and (5) formation of coagulation factors.
and foreign chemicals; (3) formation of bile; (4) storage
metabolism of carbohydrates, proteins, fats, hormones,
including (1) filtration and storage of blood; (2)
chapter is to summarize the liver’s different functions,
are disturbed simultaneously. The purpose of this
abnormalities of the liver, because many of its functions
with one another. This becomes especially evident in
a discrete organ, and many of its functions interrelate
The liver performs many different functions yet is also
The Liver as an Organ
C
H
A
P
T
E
R
7
0
859
Physiologic Anatomy of the Liver
of the liver is the
a central vein
lobule itself is composed principally of many liver cellular plates (two of which are
bile
canaliculi that empty into bile ducts in the fibrous septa separating the adjacent liver
In the septa are small portal venules that receive their blood mainly from the
hepatic sinusoids that lie between the
tinuously to portal venous blood.
Hepatic arterioles
emptying into those located about one third the distance from the interlobular
endothelial cells and (2) large
(also called reticu-
blood.
spaces of
Disse

mated to replicate once or twice, and after the original
in rats. During liver regeneration, hepatocytes are esti-
and restore the liver to its original size. This regenera-
liver is removed, causes the remaining lobes to enlarge
Partial hepatectomy, in which up to 70 per cent of the
hepatectomy or acute liver injury, as long as the injury
The liver possesses a remarkable ability to restore itself
Regulation of Liver Mass
ascites.
of the gut into the abdominal cavity. This, too, can cause
of the gastrointestinal tract, resulting in edema of
ascites.
in the abdominal cavity, which is called
normal, and the “sweating” from the surface of the liver
plasma. At vena caval pressures of 10 to 15 mm Hg,
abdominal cavity. This fluid is almost pure plasma, con-
only 3 to 7 mm Hg above normal, excessive amounts of
When the pressure in the hepatic veins rises
High Hepatic Vascular Pressures Can Cause Fluid Transudation
arises in the liver.
ties of lymph to form. Therefore, about half of all the
concentration of plasma. Also, the extreme permeabil-
about 6 g/dl, which is only slightly less than the protein
proteins into the spaces of Disse, the lymph draining
Lymph Flow
The Liver Has Very High
volume.
able, venous organ capable of acting as a valuable blood
Chapter 22. Thus, in effect, the liver is a large, expand-
failure with peripheral congestion, which is discussed in
veins and sinuses. This occurs especially in cardiac
backpressure in the liver, the liver expands, and 0.5 to 1
volume. When high pressure in the right atrium causes
liters, or almost 10 per cent of the body’s total blood
veins and that in the hepatic sinuses, is about 450 milli-
normal blood volume, including both that in the hepatic
ties of blood can be stored in its blood vessels. Its
Because the liver is an expandable organ, large quanti-
into the lumens and walls of the intestines.
normal. The patient often dies within a few hours
sure in the intestinal wall to 15 to 20 mm Hg above
temic circulation is tremendously impeded, resulting in
branches. When the portal system is suddenly blocked,
The portal system is also occasionally blocked by a
ducts, and infectious processes in the bile ducts.
eases such as infectious hepatitis, obstruction of the bile
tion of poisons such as carbon tetrachloride, viral dis-
commonly from alcoholism, but it can also follow inges-
cirrhosis of the liver.
flow of portal blood through the liver. This disease
around the blood vessels, thereby greatly impeding the
When liver parenchymal cells are destroyed, they are
Cirrhosis of the Liver Greatly Increases Resistance to Blood Flow.
1350 milliliters of blood flows by this route each minute.
mally very low, especially when one considers that about
pressure difference, only 9 mm Hg, shows that the resist-
normally averages almost exactly 0 mm Hg. This small
averages about 9 mm Hg, and the pressure in the
The pressure in the portal vein leading into the liver
This amounts to 27 per cent of the resting cardiac
hepatic artery, the total averaging about 1350 ml/min.
vein into the liver sinusoids each minute, and an addi-
The Liver Has High Blood Flow and Low Vascular Resistance.
the Portal Vein and Hepatic Artery
Blood Flows Through the Liver from
Metabolism and Temperature Regulation
860
Unit XIII
About 1050 milliliters of blood flows from the portal
tional 300 milliliters flows into the sinusoids from the
output.
hepatic vein leading from the liver into the vena cava
ance to blood flow through the hepatic sinusoids is nor-
replaced with fibrous tissue that eventually contracts
process is known as
It results most
large clot that develops in the portal vein or its major
the return of blood from the intestines and spleen
through the liver portal blood flow system to the sys-
portal hypertension and increasing the capillary pres-
because of excessive loss of fluid from the capillaries
The Liver Functions as
a Blood Reservoir
liter of extra blood is occasionally stored in the hepatic
reservoir in times of excess blood volume and capable
of supplying extra blood in times of diminished blood
Because the pores in the hepatic sinusoids are very
permeable and allow ready passage of both fluid and
from the liver usually has a protein concentration of
ity of the liver sinusoid epithelium allows large quanti-
lymph formed in the body under resting conditions
into the Abdominal Cavity from the Liver and Portal Capillaries—
Ascites.
fluid begin to transude into the lymph and leak through
the outer surface of the liver capsule directly into the
taining 80 to 90 per cent as much protein as normal
hepatic lymph flow increases to as much as 20 times
can be so great that it causes large amounts of free fluid
Block-
age of portal flow through the liver also causes high
capillary pressures in the entire portal vascular system
the gut wall and transudation of fluid through the serosa
—
Regeneration
after significant hepatic tissue loss from either partial
is uncomplicated by viral infection or inflammation.
tion is remarkably rapid and requires only 5 to 7 days
Lymphatic
Kupffer cell
Terminal
Liver cell plate
Sinusoids
Space of Disse
lymphatics
Portal
vein
Hepatic
artery
Bile duct
Central
vein
Bile canaliculi
duct
Circulatory Physiology. Vol 2: Dynamics and Control of the Body
lymphatics. (Modified from Guyton AC, Taylor AE, Granger HJ:
Basic structure of a liver lobule, showing the liver cellular plates,
Figure 70–1
the blood vessels, the bile-collecting system, and the lymph flow
system composed of the spaces of Disse and the interlobular
Fluids. Philadelphia: WB Saunders, 1975.)
hydrates and proteins also occurs in the liver. After fat
structures, and multiple chemical substances that are
used by the cells to form membranes, intracellular
lipoproteins. Both cholesterol and phospholipids are
everywhere in the body. Phospholipids are likewise syn-
into the bile; the remainder is transported in the
the liver is converted into bile salts, which are secreted
of the metabolism of fats.
manner. Thus, the liver is responsible for a major part
other tissues. These tissues reconvert the acetoacetic
acetyl-CoA that is formed; instead, it is converted by the
in the hepatic cells. The liver itself cannot use all the
in all cells of the body, but it occurs especially rapidly
dous amounts of energy. Beta-oxidation can take place
the citric acid cycle and be oxidized to liberate tremen-
(acetyl-CoA). This can enter
acetyl coenzyme A
beta-oxidation
into glycerol and fatty acids; then the fatty acids are split
To derive energy from neutral fats, the fat is first split
3. Synthesis of fat from proteins and carbohydrates
phospholipids, and most lipoproteins
2. Synthesis of large quantities of cholesterol,
1. Oxidation of fatty acids to supply energy for other
summarized from Chapter 68, are the following:
Specific functions of the liver in fat metabolism, as
aspects of fat metabolism occur mainly in the liver.
Although most cells of the body metabolize fat, certain
erol from triglycerides are converted into glucose,
In such a case, large amounts of amino acids and glyc-
person with poor liver function, blood glucose concen-
of the liver. In a
blood glucose concentration begins to fall too low. This
blood, store it, and then return it to the blood when the
normal blood glucose concentration. Storage of glyco-
The liver is especially important for maintaining a
4. Formation of many chemical compounds from
3. Gluconeogenesis
2. Conversion of galactose and fructose to glucose
1. Storage of large amounts of glycogen
lowing functions, as summarized from Chapter 67:
In carbohydrate metabolism, the liver performs the fol-
physiology of the body.
devoted to the metabolic reactions in the liver. But here,
myriad other metabolic functions. For these reasons, a
ported to other areas of the body, and performing
energy from one metabolic system to another, process-
have a high rate of metabolism, sharing substrates and
The liver is a large, chemically reactant pool of cells that
digested. Probably less than 1 per cent of the bacteria
bacterium passes inward through the wall of the Kupffer
contact with a Kupffer cell, in less than 0.01 second the
the sinuses; when a bacterium comes into momentary
line the hepatic venous sinuses, have demonstrated that
Kupffer cells, the large phagocytic macrophages that
temic circulation is extremely rare.
many bacteria from the intestines. Indeed, a sample of
is severely impaired, and liver function deteriorates.
infections, however, the regenerative process of the liver
diseases associated with fibrosis, inflammation, or viral
is maintained for optimal metabolic function. In liver
body size, so that an optimal liver-to-body weight ratio
hepatic cells, is a potent inhibitor of liver cell prolifera-
a cytokine secreted by
transforming growth factor-
the factors involved are not well understood, although
process of hepatic cell division is terminated. Again,
After the liver has returned to its original size, the
stimulating regeneration of liver cells.
mal growth factor, and cytokines such as tumor necro-
affected organ. Other growth factors, especially epider-
usually found only in the liver after these operations,
after partial hepatectomy, but mitogenic responses are
tocytes. Blood levels of HGF rise more than 20-fold
cells in the liver and in other tissues, but not by hepa-
sion and growth. HGF is produced by mesenchymal
hepatocyte growth factor (HGF)
poorly understood, but
cytes revert to their usual quiescent state.
size and volume of the liver are achieved, the hepato-
Chapter 70
The Liver as an Organ
861
Control of this rapid regeneration of the liver is still
appears to be an important factor causing liver cell divi-
suggesting that HGF may be activated only in the
sis factor and interleukin-6 may also be involved in
b,
tion and has been suggested as the main terminator of
liver regeneration.
Physiologic experiments indicate that liver growth is
closely regulated by some unknown signal related to
Hepatic Macrophage System Serves
a Blood-Cleansing Function
Blood flowing through the intestinal capillaries picks up
blood taken from the portal veins before it enters the
liver almost always grows colon bacilli when cultured,
whereas growth of colon bacilli from blood in the sys-
Special high-speed motion pictures of the action of
these cells efficiently cleanse blood as it passes through
cell to become permanently lodged therein until it is
entering the portal blood from the intestines succeeds
in passing through the liver into the systemic
circulation.
Metabolic Functions
of the Liver
ing and synthesizing multiple substances that are trans-
major share of the entire discipline of biochemistry is
let us summarize those metabolic functions that are
especially important in understanding the integrated
Carbohydrate Metabolism
intermediate products of carbohydrate metabolism
gen allows the liver to remove excess glucose from the
is called the glucose buffer function
tration after a meal rich in carbohydrates may rise two
to three times as much as in a person with normal liver
function.
Gluconeogenesis in the liver is also important in
maintaining a normal blood glucose concentration,
because gluconeogenesis occurs to a significant extent
only when the glucose concentration falls below normal.
thereby helping to maintain a relatively normal blood
glucose concentration.
Fat Metabolism
body functions
by
into two-carbon acetyl radicals that
form
condensation of two molecules of acetyl-CoA into
acetoacetic acid, a highly soluble acid that passes from
the hepatic cells into the extracellular fluid and is then
transported throughout the body to be absorbed by
acid into acetyl-CoA and then oxidize it in the usual
About 80 per cent of the cholesterol synthesized in
lipoproteins and carried by the blood to the tissue cells
thesized in the liver and transported principally in the
important to cellular function.
Almost all the fat synthesis in the body from carbo-
Chapter 32. However, it also provides
product of hemoglobin degradation, as pointed out in
This is a major end
and then eliminated in the feces. One of these is the
65. In addition, many substances are excreted in the bile
The formation of bile by the liver and the function of
Diagnostic Tool
in the Bile as a Clinical
Measurement of Bilirubin
which then passes into the gut and is lost in the feces.
from the body is secretion by the liver into the bile,
Finally, one of the major routes for excreting calcium
systems.
aldosterone. Liver damage can lead to excess accumu-
all the steroid hormones, such as estrogen, cortisol, and
excreted by the liver, including thyroxine and essentially
In a similar manner, several of the hormones secreted
cillin, and erythromycin.
many drugs, including sulfonamides, penicillin, ampi-
The active chemical medium of the liver is well
The Liver Removes or Excretes Drugs, Hormones, and Other Sub-
concentrations of all these decrease markedly, and this
Factors VII, IX, and X. In the absence of vitamin K, the
several of these substances, especially prothrombin and
other important factors. Vitamin K is required by the
and several
thrombin, accelerator globulin, Factor VII,
fibrinogen, pro-
well as an iron storage medium. Other functions of the
blood iron buffer,
level, the ferritin releases the iron. Thus, the apoferritin-
form in the hepatic cells until needed elsewhere. When
able in the body fluids in extra quantities, it combines
ing reversibly with iron. Therefore, when iron is avail-
The hepatic cells contain large amounts of a
hemoglobin of the blood, by far the greatest proportion
to last for at least 1 year and maybe several years.
for 3 to 4 months, and enough vitamin B
Sufficient vitamin D can be stored to prevent deficiency
prevent vitamin A deficiency for as long as 10 months.
Sufficient quantities of vitamin A can be stored to
quantity in the liver is vitamin A, but large quantities of
treatment of patients. The vitamin stored in greatest
The liver has a par-
Other Metabolic Functions
be formed is synthesized.Then an amino radical is trans-
this, a keto acid having the same chemical composition
amino acids can all be synthesized in the liver. To do
amino acids. For instance, the so-called nonessential
edema and ascites, as explained in Chapter 29.
albumin, may fall to very low levels, causing generalized
liver disease (e.g., cirrhosis), plasma proteins, such as
plasma concentration returns to normal. With chronic
growth of the liver to a larger size; these effects are
the body, they can be replenished in 1 or 2 weeks.
teins at a maximum rate of 15 to 50 g/day. Therefore,
lymph tissue of the body. The liver can form plasma pro-
the plasma proteins. The remaining gamma globulins
hepatic cells. This accounts for about 90 per cent of all
of part of the gamma globulins, are formed by the
Essentially all the plasma proteins, with the exception
excessive ammonia in the blood, an extremely toxic
Indeed, even greatly decreased blood flow through the
does not form urea, the plasma ammonia concentration
and then absorbed into the blood. Therefore, if the liver
formed by the deamination process, and additional
from the body fluids. Large amounts of ammonia are
Formation of urea by the liver removes ammonia
amino acids by the liver.
other tissues of the body, especially in the kidneys, but
or fats. A small amount of deamination can occur in the
4. Interconversions of the various amino acids and
3. Formation of plasma proteins
2. Formation of urea for removal of ammonia from
1. Deamination of amino acids
in protein metabolism, as summarized from Chapter 69,
death ensuing. The most important functions of the liver
The body cannot dispense with the liver’s contribution
is synthesized in the liver, it is transported in the
Metabolism and Temperature Regulation
862
Unit XIII
lipoproteins to the adipose tissue to be stored.
Protein Metabolism
to protein metabolism for more than a few days without
are the following:
the body fluids
synthesis of other compounds from amino acids
Deamination of amino acids is required before they
can be used for energy or converted into carbohydrates
this is much less important than the deamination of
amounts are continually formed in the gut by bacteria
rises rapidly and results in hepatic coma and death.
liver—as occurs occasionally when a shunt develops
between the portal vein and the vena cava—can cause
condition.
are the antibodies formed mainly by plasma cells in the
even if as much as half the plasma proteins are lost from
It is particularly interesting that plasma protein
depletion causes rapid mitosis of the hepatic cells and
coupled with rapid output of plasma proteins until the
Among the most important functions of the liver is
its ability to synthesize certain amino acids and to
synthesize other important chemical compounds from
(except at the keto oxygen) as that of the amino acid to
ferred through several stages of transamination from an
available amino acid to the keto acid to take the place
of the keto oxygen.
of the Liver
The Liver Is a Storage Site for Vitamins.
ticular propensity for storing vitamins and has long been
known as an excellent source of certain vitamins in the
vitamin D and vitamin B
12
are normally stored as well.
12
can be stored
The Liver Stores Iron as Ferritin.
Except for the iron in the
of iron in the body is stored in the liver in the form of
ferritin.
protein called apoferritin, which is capable of combin-
with apoferritin to form ferritin and is stored in this
the iron in the circulating body fluids reaches a low
ferritin system of the liver acts as a
as
liver in relation to iron metabolism and red blood cell
formation are considered in Chapter 32.
The Liver Forms a Large Proportion of the Blood Substances Used
in Coagulation.
Substances formed in the liver that are
used in the coagulation process include
metabolic processes of the liver for the formation of
almost prevents blood coagulation.
stances.
known for its ability to detoxify or excrete into the bile
by the endocrine glands are either chemically altered or
lation of one or more of these hormones in the body
fluids and therefore cause overactivity of the hormonal
the bile salts in the digestive and absorptive processes
of the intestinal tract are discussed in Chapters 64 and
greenish yellow pigment bilirubin.
an exceedingly
valuable tool for diagnosing both hemolytic blood
ditions, this can rise to as high as 40 mg/dl, and much of
averages 0.5 mg/dl of plasma. In certain abnormal con-
tion of bilirubin, which is almost entirely the free form,
or conjugated bilirubin. The normal plasma concentra-
bilirubin in the extracellular fluids, either free bilirubin
tissues. The usual cause of jaundice is large quantities of
refers to a yellowish tint to the body tissues,
Jaundice
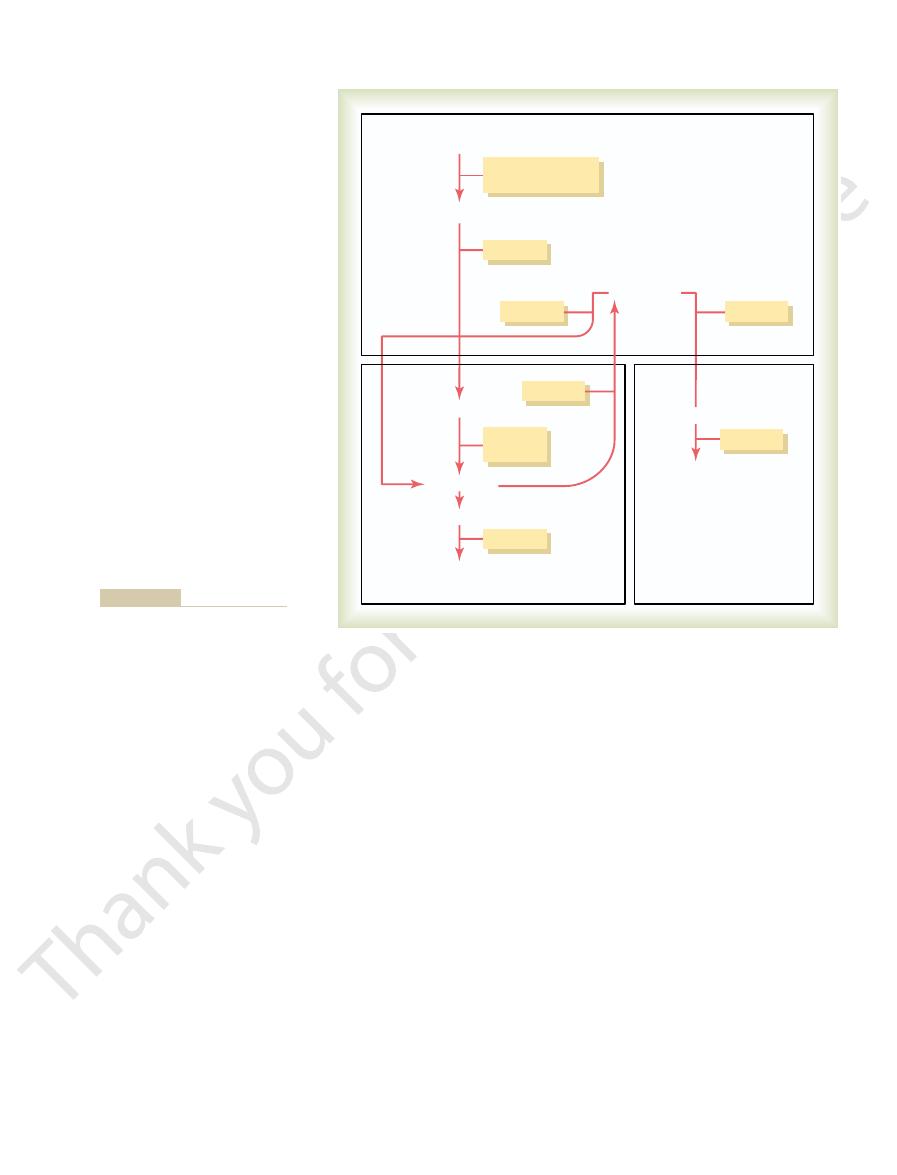
bilirubin products are shown in Figure 70–2.
These interrelations of bilirubin and the other
the feces, it becomes altered and oxidized to form
alternatively, in
into the urine.After exposure to air in the urine, the uro-
the gut, but about 5 per cent is excreted by the kidneys
blood. Most of this is re-excreted by the liver back into
is highly soluble. Some of the urobilinogen is reab-
about half of the “conjugated” bilirubin is converted by
Once in the intestine,
then into the intestines.
forms, the bilirubin is excreted from the hepatocytes by
per cent with a multitude of other substances. In these
bilirubin sulfate,
bilirubin glucuronide,
the liver cells, it is released from the plasma albumin and
the hepatic cell membrane. In passing to the inside of
Within hours, the free bilirubin is absorbed through
bin,” which is discussed later.
“free bilirubin” to distinguish it from “conjugated biliru-
bound with plasma protein, this bilirubin is still called
throughout the blood and interstitial fluids. Even when
released from the macrophages into the plasma. The
biliverdin,
The first substance formed is
straight chain of four pyrrole nuclei, which is the sub-
transported in the blood by transferrin, and (2) a
the heme ring is opened to give (1) free iron, which is
heme,
reticuloendothelial system) throughout the body. The
phagocytized by tissue macrophages (also called the
membranes rupture, and the released hemoglobin is
fragile to exist in the circulatory system, their cell
life span (on average, 120 days) and have become too
Briefly, when the red blood cells have lived out their
while referring to Figure 70–2, let us explain this.
Therefore,
diseases and various types of liver diseases.
Chapter 70
The Liver as an Organ
863
hemoglobin is first split into globin and
and
strate from which bilirubin will eventually be formed.
but this is
rapidly reduced to free bilirubin, which is gradually
free bilirubin immediately combines strongly with
plasma albumin and is transported in this combination
soon thereafter conjugated about 80 per cent with glu-
curonic acid to form
about 10 per
cent with sulfate to form
and about 10
an active transport process into the bile canaliculi and
Formation and Fate of Urobilinogen.
bacterial action into the substance urobilinogen, which
sorbed through the intestinal mucosa back into the
bilinogen becomes oxidized to urobilin;
ster-
cobilin.
Jaundice—Excess Bilirubin in the
Extracellular Fluid
including a yellowness of the skin as well as the deep
Intestinal Contents
Urine
Fragile red blood cells
Reticuloendothelial
system
Liver
Liver
Absorbed
Conjugated bilirubin
Urobilinogen
Urobilinogen
Urobilin
Stercobilinogen
Stercobilin
Oxidation
Oxidation
Bacterial
action
Kidneys
Urobilinogen
Free bilirubin (protein-bound)
Plasma
Bilirubin formation and excretion.
Figure 70–2
Physiol Gastrointest Liver Physiol 284:G175, 2003.
physiology. I. Hepatocyte transport of bile acids. Am J
Wolkoff AW, Cohen DE: Bile acid regulation of hepatic
acterization, function, and regulation. Physiol Rev 83:633,
Trauner M, Boyer JL: Bile salt transporters: molecular char-
test Liver Physiol 283:G256, 2002.
anisms of Kupffer cell activation. Am J Physiol Gastroin-
Su GL: Lipopolysaccharides in liver injury: molecular mech-
in cardiac failure and cirrhosis. Semin Nephrol 21:157,
Schrier RW, Gurevich AK, Cadnapaphornchai MA: Patho-
cyte’s survival kit. Clin Sci (Lond) 107:13, 2004.
Schoemaker MH, Moshage H: Defying death: the hepato-
65:543, 2003.
Sands JM: Mammalian urea transporters. Annu Rev Physiol
function. News Physiol Sci 14:117, 1999.
Reichen J: The role of the sinusoidal endothelium in liver
cell type or two? Liver 22:283, 2002.
Ramadori G, Saile B: Mesenchymal cells in the liver—one
research trends. J Hepatol 39:864, 2003.
and aquaporins in bile formation: recent advances and
Portincasa P, Moschetta A, Mazzone A, et al: Water handling
Liver Dis 24:21, 2004.
Li MK, Crawford JM: The pathology of cholestasis. Semin
regeneration. J Am Coll Surg 197:634, 2003.
Koniaris LG, McKillop IH, Schwartz SI, Zimmers TA: Liver
rational and targeted treatments. BMJ 327:143, 2003.
Iredale JP: Cirrhosis: new research provides a basis for
drome. Lancet 362:1819, 2003.
Gines P, Guevara M, Arroyo V, Rodes J: Hepatorenal syn-
cirrhosis and ascites. N Engl J Med 350:1646, 2004.
Gines P, Cardenas A, Arroyo V, Rodes J: Management of
trointest Liver Physiol 282:G1, 2002.
macrophage function and cytokines. Am J Physiol Gas-
Diehl AM: Nonalcoholic steatosis and steatohepatitis. IV.
Immunol 3:51, 2003.
Crispe IN: Hepatic T cells and liver tolerance. Nat Rev
Physiol Gastrointest Liver Physiol 284:G729, 2003.
ment to splanchnic organs to reduce inflammation. Am J
editorial perspectives. II. Modulating leukocyte recruit-
Bonder CS, Kubes P: The future of GI and liver research:
117:306, 2004.
cellular features of hepatic regeneration. J Surg Res
Black D, Lyman S, Heider TR, Behrns KE: Molecular and
Hepatology 38:286, 2003.
Bauer M: Heme oxygenase in liver transplantation: heme
Metab 285:E685, 2003.
of hepatic gluconeogenesis. Am J Physiol Endocrinol
Barthel A, Schmoll D: Novel concepts in insulin regulation
of Prometheus. News Physiol Sci 14:149, 1999.
Ankoma-Sey V: Hepatic regeneration—revisiting the myth
346:1221, 2002.
Angulo P: Nonalcoholic fatty liver disease. N Engl J Med
inside and outside the liver? Cell Prolif 37:1, 2004.
Alison MR, Vig P, Russo F, et al: Hepatic stem cells: from
mine the severity of the disease.
hemolytic diseases and liver diseases, as well as to deter-
by the liver and by the use of a few simple tests, it is
ing the foam, which turns an intense yellow. Thus,
conjugated bilirubin appear in the urine. This can be
in severe obstructive jaundice, significant quantities of
but not the albumin-bound free bilirubin. Therefore,
pigments.
are completely negative. Also, the stools become clay
obstructive jaundice, tests for urobilinogen in the urine
the kidneys into the urine. Consequently, in
reabsorbed into the blood, and none can be excreted by
bilinogen by bacteria. Therefore, no urobilinogen is
When there is total obstruction of bile flow, no biliru-
two.
in the “conjugated” form. A test called the
in the “free” form; in obstructive jaundice, it is mainly
plasma. In hemolytic jaundice, almost all the bilirubin is
rather than the free type.
Thus,
emptying of the bile into the lymph leaving the liver.
gated bilirubin is then returned to the blood, probably
and becomes conjugated in the usual way. This conju-
intestines. The free bilirubin still enters the liver cells
), the rate of bilirubin formation is normal, but
In obstructive jaundice, caused either by
the urine.
in the intestine is greatly increased, and much
normal levels. Likewise, the rate of formation of
bilirubin as quickly as it is formed. Therefore, the
is not impaired, but red blood cells are hemolyzed so
In hemolytic jaundice, the excretory function of the liver
ways.
They differ from each other in the following
jaundice.
called, respectively,
trointestinal tract. These two types of jaundice are
bilirubin into the blood, and (2) obstruction of the bile
destruction of red blood cells, with rapid release of
The common causes of jaundice are (1) increased
to about three times normal—that is, above 1.5 mg/dl.
it can become the conjugated type. The skin usually
Metabolism and Temperature Regulation
864
Unit XIII
begins to appear jaundiced when the concentration rises
ducts or damage to the liver cells so that even the usual
amounts of bilirubin cannot be excreted into the gas-
hemolytic jaundice and obstructive
Hemolytic Jaundice Is Caused by Hemolysis of Red Blood Cells.
rapidly that the hepatic cells simply cannot excrete the
plasma concentration of free bilirubin rises to above-
uro-
bilinogen
of this is absorbed into the blood and later excreted in
Obstructive Jaundice Is Caused by Obstruction of Bile Ducts or
Liver Disease.
obstruction of the bile ducts (which most often occurs
when a gallstone or cancer blocks the common bile
duct) or by damage to the hepatic cells (which occurs in
hepatitis
the bilirubin formed cannot pass from the blood into the
by rupture of the congested bile canaliculi and direct
most of the bilirubin in the plasma becomes the
conjugated type
Diagnostic Differences Between Hemolytic and Obstructive
Jaundice.
Chemical laboratory tests can be used to dif-
ferentiate between free and conjugated bilirubin in the
van den
Bergh reaction can be used to differentiate between the
bin can reach the intestines to be converted into uro-
total
colored owing to a lack of stercobilin and other bile
Another major difference between free and conju-
gated bilirubin is that the kidneys can excrete small
quantities of the highly soluble conjugated bilirubin
demonstrated simply by shaking the urine and observ-
by understanding the physiology of bilirubin excretion
often possible to differentiate among multiple types of
References
catabolism and metabolites in the search of function.
Nonalcoholic fatty liver disease abnormalities in
genesis and management of sodium and water retention
2001.
2003.
