fallopian tubes soon after both the sperm and the ovum enter the ampulla. But
Fertilization of the ovum normally takes place in the ampulla of one of the
billion sperm deposited in the vagina, a few thousand succeed in reaching each
posterior pituitary gland of the female during her orgasm. Of the almost half a
fallopian tubes near the ovarian ends of the tubes. This transport of the sperm
intercourse, a few sperm are transported within 5 to 10 minutes upward from
the opposite fallopian tube.
with relative ease of conception, thus demonstrating that ova can even enter
succeed in this task. Indeed, in some recorded cases, women with one ovary
on the basis of conception studies, it is probable that as many as 98 per cent
It seems likely that many ova might fail to enter the fallopian tubes. However,
one of the fallopian tubes.
slow fluid current flowing toward the ostium. By this means, the ovum enters
of the involved fallopian tube. One can actually see a
the opening, or
are activated by estrogen from the ovaries, which causes the cilia to beat toward
faces of the fimbriated tentacles are lined with ciliated epithelium, and the
ated ends of each fallopian tube fall naturally around the ovaries. The inner sur-
enter one of the fallopian tubes to reach the cavity of the uterus. The fimbri-
When ovulation occurs, the ovum,
Entry of the Ovum into the Fallopian Tube (Oviduct).
end of one of the fallopian tubes.
into the abdominal cavity. Then, almost immediately, it enters the fimbriated
It is at this time that the ovum, still in the secondary oocyte stage, is ovulated
chromosomes in the secondary oocyte.
that is expelled. This leaves 23
somes loses one of its partners, which becomes incorporated in a
In this process, each of the 23 pairs of chromo-
secondary oocyte.
is expelled from the nucleus of the oocyte. The primary oocyte then
it is released from the ovarian follicle, its nucleus divides by meiosis and a
stage. Shortly before
While still in the ovary, the ovum is in the
Maturation and Fertilization of the Ovum
discuss the physiology of pregnancy. In Chapter 83, some special aspects of fetal
eventually develops into a full-term fetus. The
takes place, and the fertilized ovum
pregnancy,
fertilized, a new sequence of events called
fertilization of the ovum. If the ovum becomes
In Chapters 80 and 81, the sexual functions of the
Pregnancy and Lactation
C
H
A
P
T
E
R
8
2
1027
male and female are described to the point of
gestation,
or
purpose of this chapter is to discuss the early stages
of ovum development after fertilization and then to
and early childhood physiology are discussed.
primary oocyte
first
polar body
becomes the
polar body
unpaired
along with a hundred or more attached granulosa cells that constitute the
corona radiata, is expelled directly into the peritoneal cavity and must then
cilia
ostium,
removed and the opposite fallopian tube removed have had several children
Fertilization of the Ovum.
After the male ejaculates semen into the vagina during
the vagina and through the uterus and fallopian tubes to the ampullae of the
is aided by contractions of the uterus and fallopian tubes stimulated by
prostaglandins in the male seminal fluid and also by oxytocin released from the
ampulla.
This delayed transport of the fertilized ovum
into the uterus.
then the progesterone activates the receptors, exerting
first 3 days after ovulation. After this time, the rapidly
fluid current. Also, the
The fallopian tubes are lined with a rugged, cryptoid
fallopian tube may also aid the ovum passage.
beat toward the uterus. Weak contractions of the
ciliated epithelium that lines the tube; the cilia always
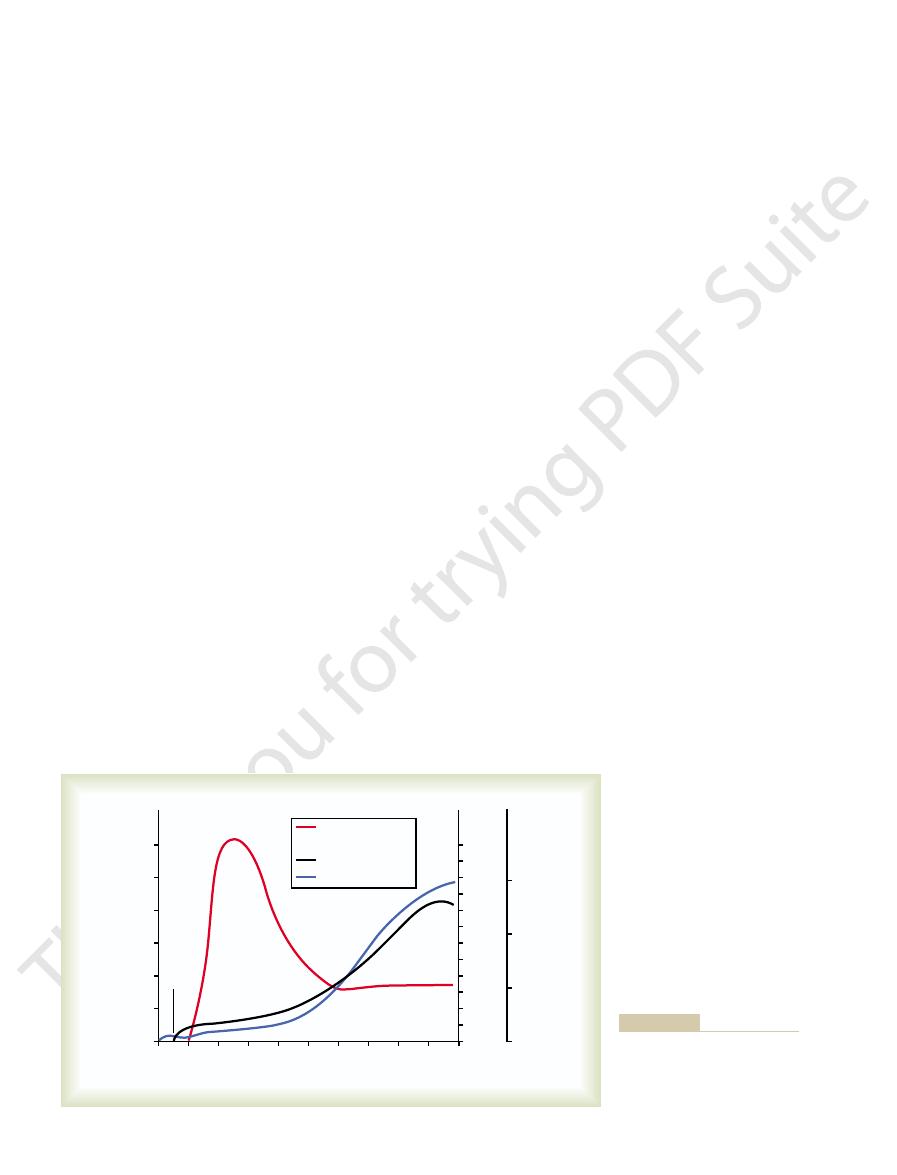
the cavity of the uterus (Figure 82–2). This transport is
After fertilization has occurred, an additional 3 to 5
in the Fallopian Tube
Transport of the Fertilized Ovum
some from an ovum, giving an XY combination, a male
be born, as explained in Chapter 80. But if a Y chro-
ovum, giving an XX combination, a female child will
chromosome). Therefore, if an X chromosome from
some) and half carry a Y chromosome (the male
formation of the mature sperm, half of these carry in
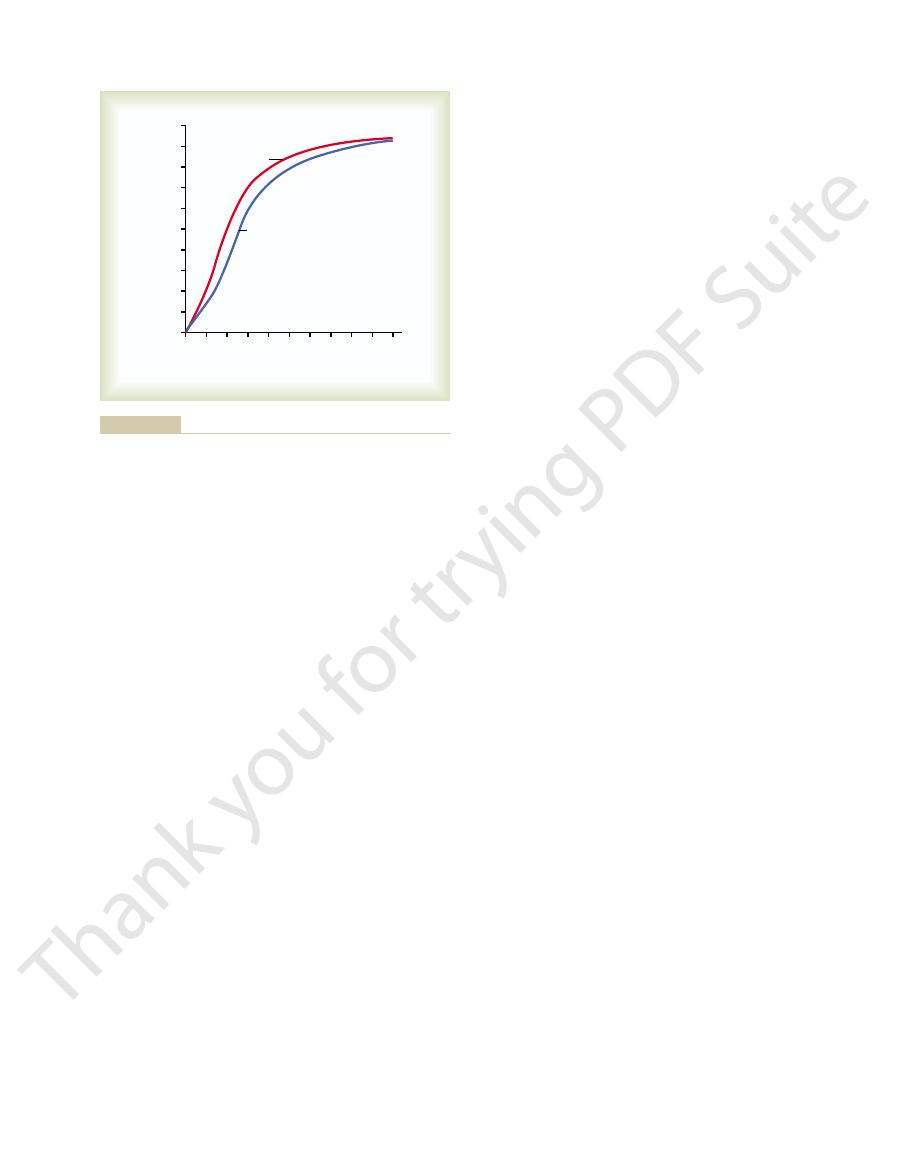
(see Figure 82–1
ovum
fertilized
. Later, the
shown in Figure 82–1
male pronucleus,
changed. On entering the ovum, its head swells to form
In the meantime, the fertilizing sperm has also
chromosome.
somes is the female chromosome, known as the
) 23 chromosomes. One of these chromo-
that is expelled. The mature
mature ovum
oocyte divides again to form the
in the secondary oocyte stage of development), the
the ovum itself. The mechanisms used by the sperm for
zona pellucida
before a sperm can enter the ovum, it must first pene-
1028
Unit XIV
Endocrinology and Reproduction
trate the multiple layers of granulosa cells attached to
the outside of the ovum (the corona radiata) and then
bind to and penetrate the
surrounding
these purposes are presented in Chapter 80.
Once a sperm has entered the ovum (which is still
plus
a second polar body
ovum still carries in its nucleus (now called the female
pronucleus
X
a
D
23 unpaired chromosomes of the male pronucleus and
the 23 unpaired chromosomes of the female pronu-
cleus align themselves to re-form a complete comple-
ment of 46 chromosomes (23 pairs) in the
E).
What Determines the Sex of the Fetus That Is Created?
After
their genome an X chromosome (the female chromo-
a sperm combines with an X chromosome from an
mosome from a sperm is paired with an X chromo-
child will be born.
days is normally required for transport of the fertilized
ovum through the remainder of the fallopian tube into
effected mainly by a feeble fluid current in the tube
resulting from epithelial secretion plus action of the
surface that impedes passage of the ovum despite the
isthmus of the fallopian tube
(the last 2 centimeters before the tube enters the
uterus) remains spastically contracted for about the
increasing progesterone secreted by the ovarian
corpus luteum first promotes increasing progesterone
receptors on the fallopian tube smooth muscle cells;
a tubular relaxing effect that allows entry of the ovum
through the fallopian tube allows several stages of cell
division to occur before the dividing ovum—now
called a blastocyst, with about 100 cells—enters the
C
D
E
Corona
radiata
Sperm
A
B
Female
pronucleus
Centrosome
Sperm
Male
pronucleus
Dispersed corona radiata
Anatomy: A Textbook and Laboratory Manual of Embryology, 7th
division of the ovum. (Modified from Arey LB: Developmental
ganization of a full complement of chromosomes and beginning
Formation of the male and female pronuclei.
sperm.
Entry of the
Dispersal of the corona radiata.
corona radiata.
The mature ovum surrounded by the
Fertilization of the ovum.
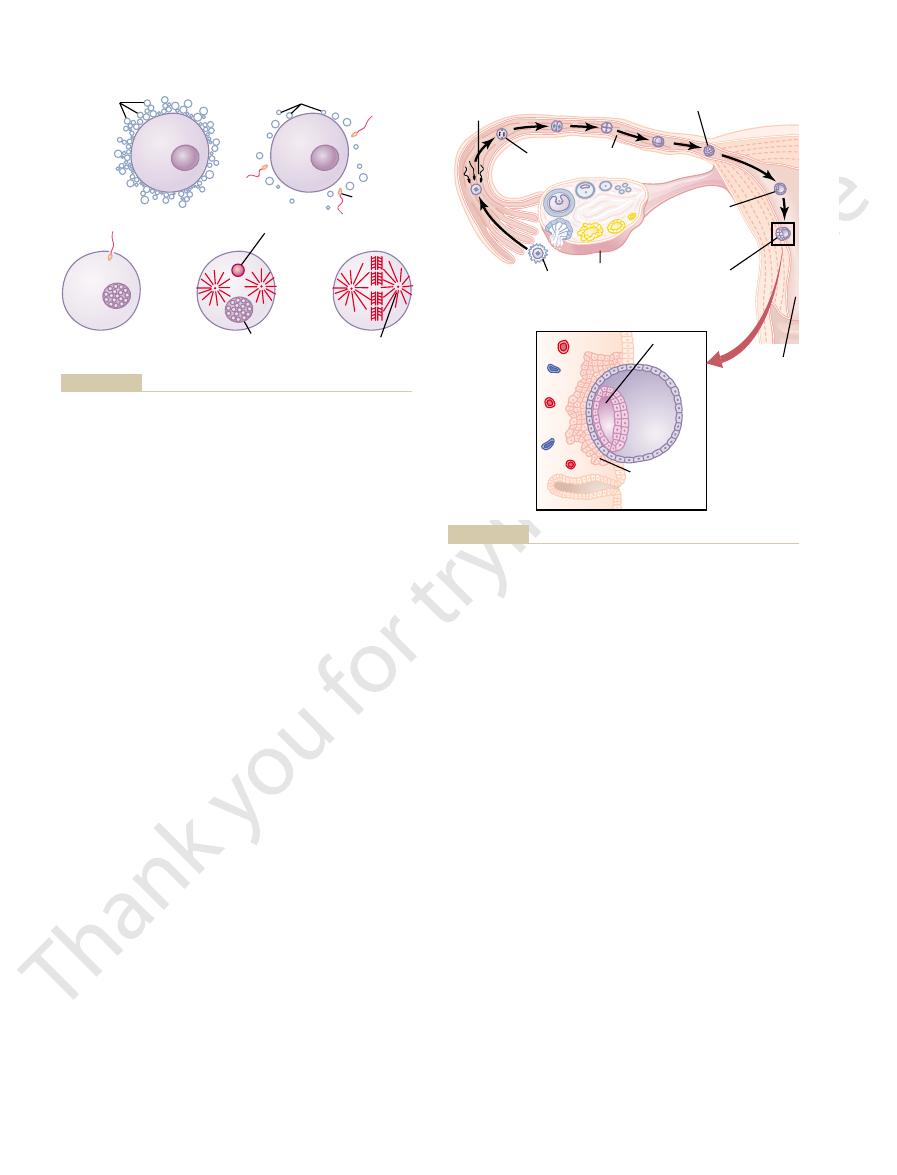
Figure 82–1
A,
B,
C,
D,
E, Reor-
ed. Philadelphia: WB Saunders, 1974.)
Fertilization
(day 1)
Cell division
Fallopian
tube
Ovary
Ovum
Ovulation
Zygote
Blastocyst
Blastocyst
reaches
uterus
(days 4-5)
Blastocyst
implants
(days 5-7)
Uterus
A
B
Amniotic
cavity
Trophoblastic
cells invading
endometrium
Action of tro-
Ovulation, fertilization of the ovum in the fallopian tube, and
Figure 82–2
A,
implantation of the blastocyst in the uterus. B,
phoblast cells in implantation of the blastocyst in the uterine
endometrium.
and more projections, which become
phoblastic cords. The trophoblast cells send out more
Simultaneously,
begins to be pumped by the heart of the embryo itself.
embryo. By the 16th day after fertilization, blood also
attaching to the uterus, blood capillaries grow into the
While the trophoblastic cords from the blastocyst are
Anatomy of the Placenta
phoblastic period of nutrition, which gradually gives
week after implantation). Figure 82–4 shows this tro-
nutrition in this way for up to 8 weeks, although the
During the first week after implantation, this is the
ing and imbibing it, the stored nutrients in the decidua
As the trophoblast cells invade the decidua, digest-
decidual cells,
and to store even more nutrients. These cells are now
the endometrium, the continued secretion of proges-
the conceptus. Then, when the conceptus implants in
taining extra quantities of glycogen, proteins, lipids,
effect on the uterine endometrium, converting the
latter half of each monthly sexual cycle has an
In Chapter 81, we pointed out that the progesterone
Early Nutrition of the Embryo
branes of pregnancy.
rapidly, forming the placenta and the various mem-
blastocyst and the uterine endometrium) proliferate
a small embryo. Once implantation has taken place,
82–3 shows an early implanted human blastocyst, with
tocyst, adding more sustenance for growth. Figure
These cells secrete proteolytic enzymes that digest and
that develop over the surface of the blastocyst.
endometrial secretions, called “uterine milk.”
the blastocyst obtains its nutrition from the uterine
seventh day after ovulation. Before implantation,
3 days before it implants in the endometrium; thus,
After reaching the uterus, the developing blastocyst
in the Uterus
Implantation of the Blastocyst
nutrition of the developing blastocyst.
uterus. During this time, the fallopian tube secretory
Chapter 82
Pregnancy and Lactation
1029
cells produce large quantities of secretions used for the
usually remains in the uterine cavity an additional 1 to
implantation ordinarily occurs on about the fifth to
Implantation results from the action of trophoblast
cells
liquefy the adjacent cells of the uterine endometrium.
Some of the fluid and nutrients released are actively
transported by the same trophoblast cells into the blas-
the trophoblast cells and other adjacent cells (from the
secreted by the ovarian corpus luteum during the
endometrial stromal cells into large swollen cells con-
and even some minerals necessary for development of
terone causes the endometrial cells to swell further
called
and the total mass of cells is called
the decidua.
are used by the embryo for growth and development.
only means by which the embryo can obtain nutrients;
the embryo continues to obtain at least some of its
placenta also begins to provide nutrition after about
the 16th day beyond fertilization (a little more than 1
way to placental nutrition.
Function of the Placenta
Developmental and Physiologic
cords from the vascular system of the newly forming
blood sinuses supplied with blood from
the mother develop around the outsides of the tro-
placental villi into
Trophoblasts
Ovum
Endometrium
Hertig.)
digestion and invasion of the endometrium. (Courtesy Dr. Arthur
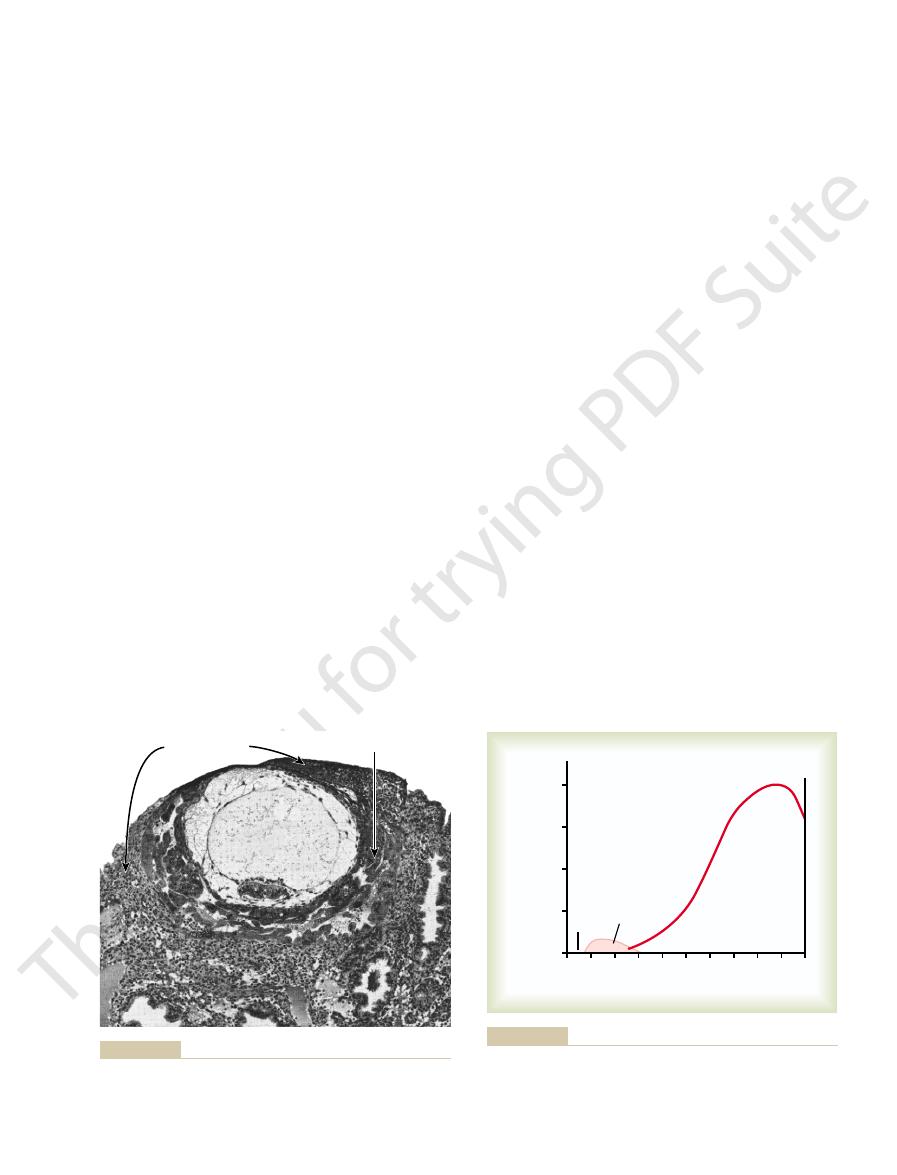
Implantation of the early human embryo, showing trophoblastic
Figure 82–3
diffusion
Trophoblastic
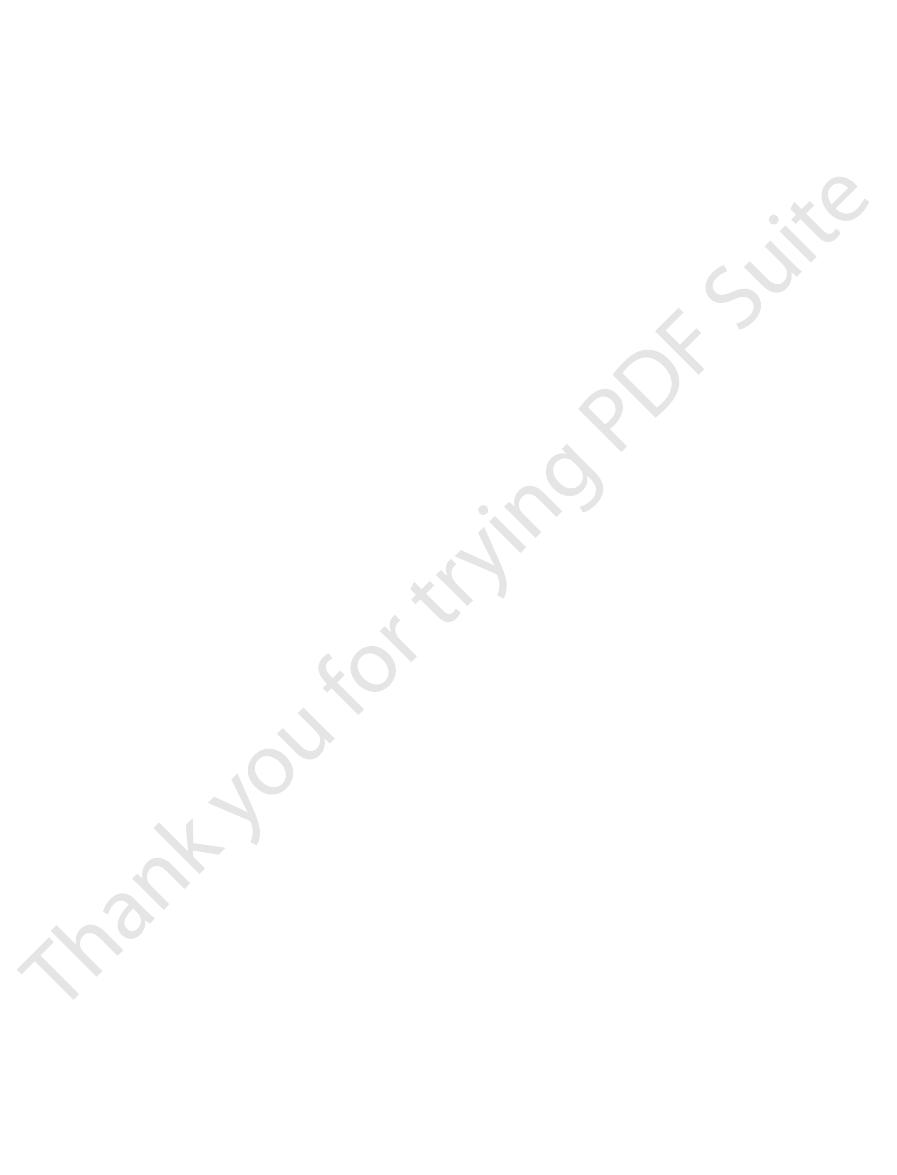
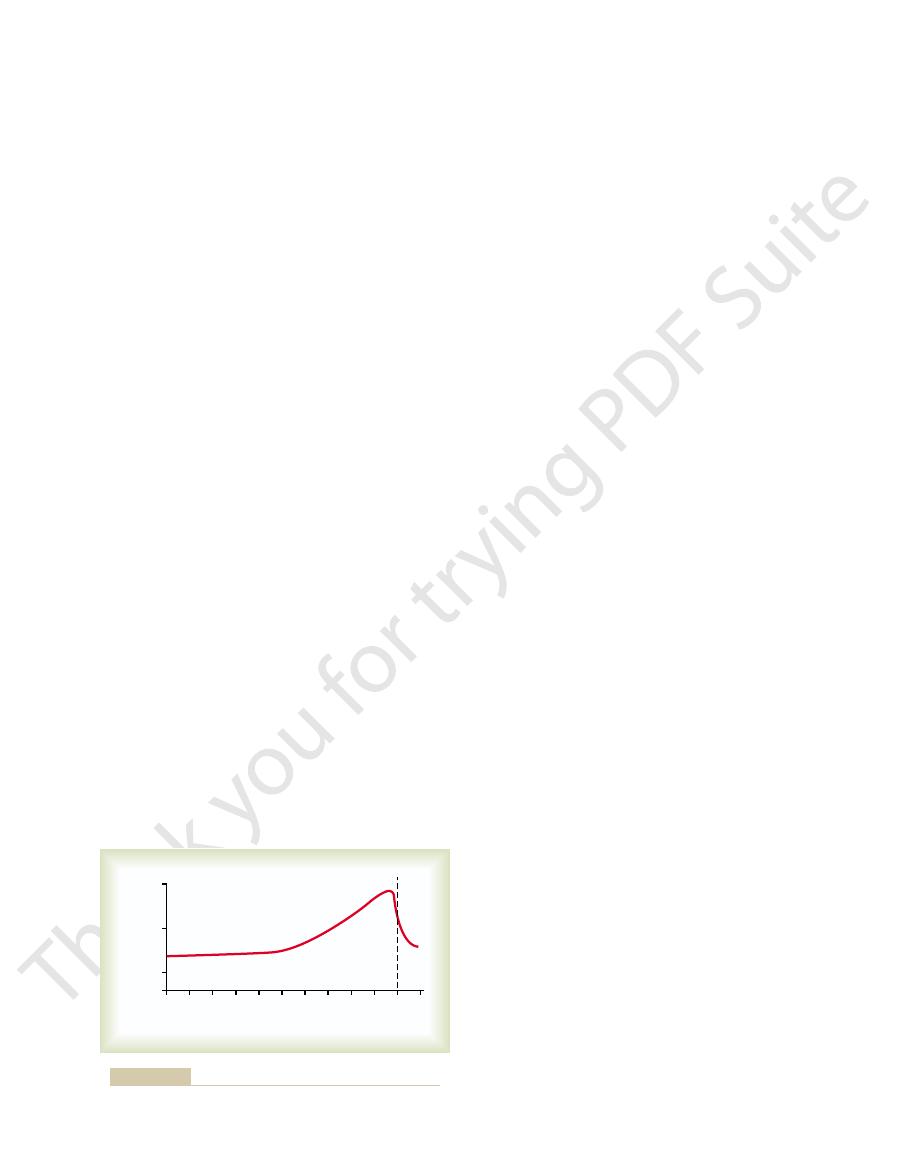
0
4
8
12 16 20 24 28 32 36
Parturition
Ovulation
nutrition
Placental
40
0
25
50
75
100
Duration of pregnancy (weeks)
Placental membrane conductivity
(per cent of maximum)
diffusion through the placental membrane.
trial decidua, and essentially all the later nutrition results from
phoblastic digestion and absorption of nutrients from the endome-
Nutrition of the fetus. Most of the early nutrition is due to tro-
Figure 82–4
lung in Chapter 40, provides another mechanism to
Third, the
amount of oxygen transported to the fetal tissues.
Second, the
in fetal blood, the fetal hemoglobin can carry 20 to 50
nal hemoglobin. This means that at the low P
and fetal hemoglobin, demonstrating that the curve for
fetus before birth. Figure 82–6 shows the comparative
First, the hemoglobin of the fetus is mainly
mother’s blood to her tissues.
of only 30 mm Hg. There are
membrane is about 20 mm Hg.
is about 30 mm Hg. Therefore, the mean pressure gra-
sinuses is about 50 mm Hg, and the mean P
of the mother’s blood in the placental
blood to the fetus’s blood. Near the end of pregnancy,
by an oxygen pressure gradient from the mother’s
gen through the placental membrane. The dissolved
tured placental membrane.
severely into the mother’s circulation because of a rup-
the fetus. Fortunately, it is rare for the fetus to bleed
or, even less commonly, the mother’s cells to pass into
Rarely, “breaks” occur in the placental membrane,
Figure 82–4.
surface area expands many times over, thus giving the
nancy, the permeability increases because of thinning
ductance is minuscule at first. Conversely, in later preg-
grown significantly. Therefore, the total diffusion con-
oped. Therefore, its permeability is low. Further, the
In the early months of pregnancy, the placental
from the fetus back into the mother.
blood into the fetus’s blood and
from the mother’s
diffusion of foodstuffs and oxygen
The major function of the placenta is to provide for
Diffusion Conductance
Placental Permeability and Membrane
membranes elsewhere in the body.
ertheless, nutrients and other substances pass through
the area of the pulmonary membrane in the lungs. Nev-
The total surface area of all the villi of the mature pla-
the mother. The lower part of Figure 82–5 shows the
fetus. At the same time, the mother’s blood flows from
umbilical arteries,
82–5. Note that the fetus’s blood flows through two
The final structure of the placenta is shown in Figure
blood, are surrounded by sinuses that contain maternal
which fetal capillaries grow. Thus, the villi, carrying fetal
1030
Unit XIV
Endocrinology and Reproduction
blood.
then into the capillaries of the villi,
and finally back through a single umbilical vein into the
her uterine arteries into large maternal sinuses that sur-
round the villi and then back into the uterine veins of
relation between the fetal blood of each fetal placental
villus and the blood of the mother surrounding the out-
sides of the villus in the fully developed placenta.
centa is only a few square meters—many times less than
this placental membrane mainly by diffusion in much
the same manner that diffusion occurs through the
alveolar membranes of the lungs and the capillary
diffusion of excretory
products
membrane is still thick because it is not fully devel-
surface area is small because the placenta has not
of the membrane diffusion layers and because the
tremendous increase in placental diffusion shown in
which allows fetal blood cells to pass into the mother
Diffusion of Oxygen Through the Placental Membrane.
Almost the same principles for diffusion of oxygen
through the pulmonary membrane (discussed in detail
in Chapter 39) are applicable for diffusion of oxy-
oxygen in the blood of the large maternal sinuses
passes into the fetal blood by simple diffusion, driven
the mean P
O
2
O
2
in the
fetal blood after it becomes oxygenated in the placenta
dient for diffusion of oxygen through the placental
One might wonder how it is possible for a fetus to
obtain sufficient oxygen when the fetal blood leaving
the placenta has a P
O
2
three reasons why even this low P
O
2
is capable of
allowing the fetal blood to transport almost as much
oxygen to the fetal tissues as is transported by the
fetal
hemoglobin, a type of hemoglobin synthesized in the
oxygen dissociation curves for maternal hemoglobin
fetal hemoglobin is shifted to the left of that for mater-
O
2
levels
per cent more oxygen than maternal hemoglobin can.
hemoglobin concentration of fetal blood
is about 50 per cent greater than that of the mother; this
is an even more important factor in enhancing the
Bohr effect, which is explained in relation
to the exchange of carbon dioxide and oxygen in the
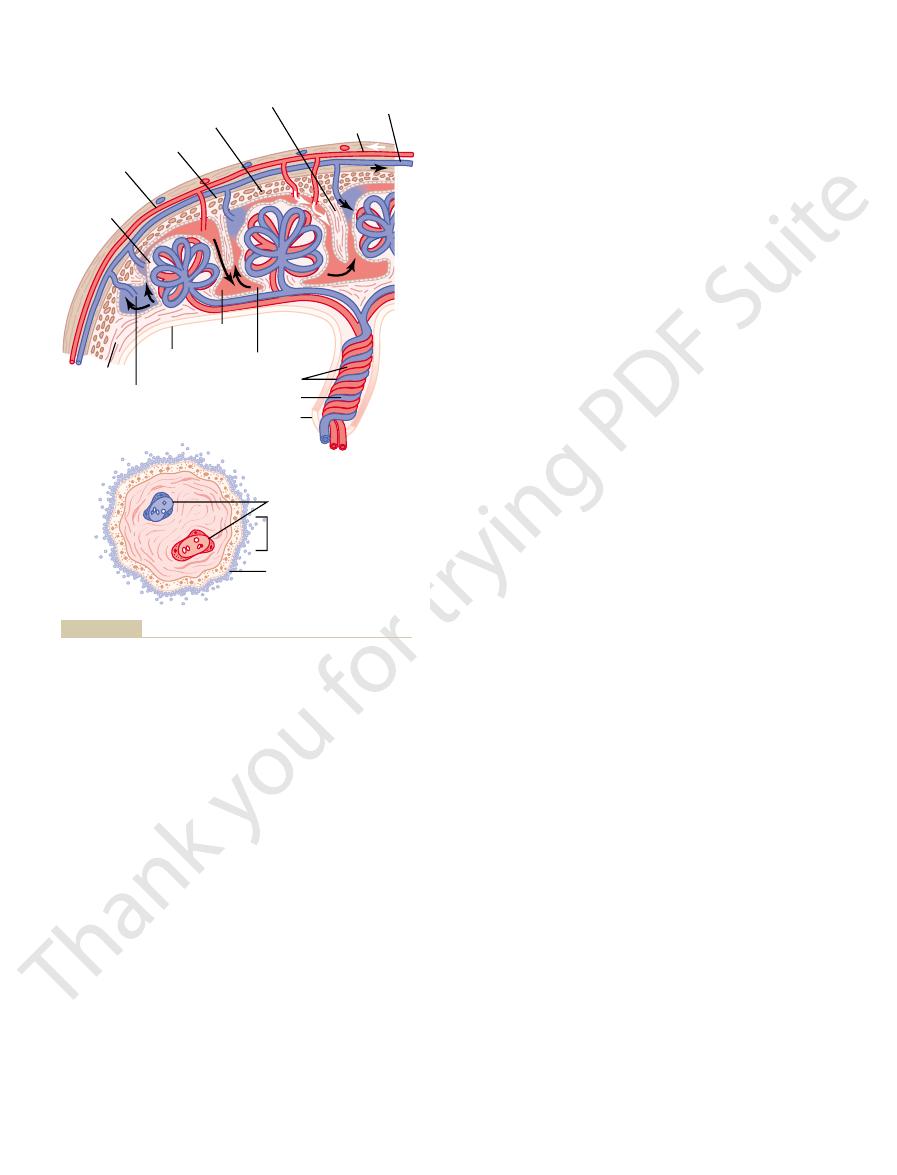
Villus
Maternal
vessels
Marginal
sinus
VILLUS
PLACENTA
Chorion
Amnion
Trophoblast
Umbilical arteries
Umbilical vein
Umbilical cord
Fetal capillaries
Intervillous space
Chorionic epithelium
Intravillus
space
Limiting layer
Stratum spongiosum
Placental septum
To the mother
From the mother
tory Manual of Embryology, 7th ed. Philadelphia: WB Saunders,
from Arey LB: Developmental Anatomy: A Textbook and Labora-
Human Body, 25th ed. Philadelphia: Lea & Febiger, 1948; and
villous spaces. (Modified from Gray H, Goss CM: Anatomy of the
fetal blood in the villus capillaries to the mother’s blood in the inter-
Below,
Organization of the mature placenta.
Figure 82–5
Above,
Relation of the
1974.)
pregnancy.
the fourth as well, are all essential to a normal
the first three of which, and probably
human chorionic somatomam-
progesterone,
human chorionic gonadotropin, estrogens,
In pregnancy, the placenta forms especially large
in Pregnancy
Hormonal Factors
of diffusion gradients across the placental membrane,
from the fetus occurs mainly, if not entirely, as a result
than that in the mother’s blood. Therefore, excretion
However, creatinine, which does not diffuse as easily,
fuses through the placental membrane with great ease.
greater than that in maternal blood, because urea dif-
The level of urea in fetal blood is only slightly
tinine.
urea, uric acid,
products of the mother. These include especially the
from the fetal blood into the maternal blood, other
Excretion of Waste Products Through the Placental Membrane.
and potassium, sodium, and chloride ions diffuse with
for nutrition. Also, such substances as ketone bodies
glucose, so that glucose is used more easily by the fetus
blood into the fetal blood, but more slowly than
membranes, these also diffuse from the maternal
cells of the membrane. Even so, the glucose level in
through the placental membrane. That is, the glucose
much glucose, the trophoblast cells lining the placen-
the entire body of the mother uses. To provide this
pregnancy, the fetus often uses as much glucose as
oxygen does. For instance, in the late stages of
Diffusion of Foodstuffs Through the Placental Membrane.
diffusion of carbon dioxide, because the extreme sol-
mm Hg higher than that of the maternal blood. This
mother’s blood. The P
tissues, and the only means for excreting the carbon
with that of the lungs of the newborn baby.
ference across the membrane.This compares favorably
The total
of only 30 mm Hg.
membrane, despite the fact that the fetal blood leaving
By these three means, the fetus is capable of receiv-
exchange in the lungs; therefore, it is called the
tion in the fetal blood. These two effects make the
the fetal blood. Thus, the Bohr shift operates in one
the maternal blood, while enhancing oxygen uptake by
blood to decrease. This forces still more oxygen from
These changes cause the capacity of fetal blood to
makes it more acidic.
dioxide makes the fetal blood more alkaline, whereas
blood into the maternal blood. Loss of the carbon
placenta carries large amounts of carbon dioxide, but
. The fetal blood entering the
is, hemoglobin can carry more oxygen at a low P
enhance the transport of oxygen by fetal blood. That
Chapter 82
Pregnancy and Lactation
1031
CO
2
than it can at a high P
CO
2
much of this carbon dioxide diffuses from the fetal
the increased carbon dioxide in the maternal blood
combine with oxygen to increase and that of maternal
direction in the maternal blood and in the other direc-
Bohr shift twice as important here as it is for oxygen
double
Bohr effect.
ing more than adequate oxygen through the placental
the placenta has a P
O
2
diffusing capacity of the entire placenta for
oxygen at term is about 1.2 milliliters of oxygen per
minute per millimeter of mercury oxygen pressure dif-
Diffusion of Carbon Dioxide Through the Placental Membrane.
Carbon dioxide is continually formed in the tissues of
the fetus in the same way that it is formed in maternal
dioxide from the fetus is through the placenta into the
CO
2
of the fetal blood is 2 to 3
small pressure gradient for carbon dioxide across the
membrane is more than sufficient to allow adequate
ubility of carbon dioxide in the placental membrane
allows carbon dioxide to diffuse about 20 times as
rapidly as oxygen.
Other metabolic substrates needed by the fetus
diffuse into the fetal blood in the same manner as
tal villi provide for facilitated diffusion of glucose
is transported by carrier molecules in the trophoblast
fetal blood is 20 to 30 per cent lower than that in
maternal blood.
Because of the high solubility of fatty acids in cell
relative ease from the maternal blood into the fetal
blood.
In the same manner that carbon dioxide diffuses
excretory products formed in the fetus also diffuse
through the placental membrane into the maternal
blood and are then excreted along with the excretory
nonprotein nitrogens such as
and crea-
has a fetal blood concentration considerably higher
because there are higher concentrations of the excre-
tory products in the fetal blood than in the maternal
blood.
quantities of
and
motropin,
60
80
100
0
20
40
Fetal
Maternal
Human
0
100
80
60
40
20
P
O2
(mm Hg)
Oxyhemoglobin (per cent)
Fed Proc 23:775, 1964.)
Metcalfe J, Moll W, Bartels H: Gas exchange across the placenta.
. (Data from
oxygen than can maternal blood for a given blood P
blood, showing that fetal blood can carry a greater quantity of
Oxygen-hemoglobin dissociation curves for maternal and fetal
Figure 82–6
O
2
estrogens and progesterone. Histochemical and
The placenta, like the corpus luteum, secretes both
organs. Near the end of pregnancy, the testosterone
in male fetuses until the time of birth. This small secre-
male fetus, resulting in the production of testosterone
Testes.
Effect of Human Chorionic Gonadotropin on the Fetal
period. The corpus luteum involutes slowly after the
maintain pregnancy for the remainder of the gestation
the 12th week. After that time, the placenta secretes
abortion almost always occurs, sometimes even up to
mately the 7th week of pregnancy, spontaneous
for the early development of the fetus.
nature of the uterine endometrium, which is necessary
after pregnancy begins, and its continued secretion of
gonadotropin, the corpus luteum in the mother’s ovary
blastocyst implants.
sexual cycle become actual
menstruum. As a result, the
terone and estrogens—for the next few months. These
cycle. Instead, it causes the corpus luteum to secrete
hormone secreted by the pituitary gland. By far, its
der of pregnancy.
16 to 20 weeks. It continues at this level for the remain-
of pregnancy and decreases back to a lower value by
the endometrium. Then the rate of secretion rises
after ovulation, shortly after the blastocyst implants in
mother, as shown in Figure 82–7. The secretion of this
the syncytial trophoblast cells into the fluids of the
human chorionic gonadotropin
phoblast cells from the early fertilized ovum, the
tissues in the following manner.
the pregnancy would terminate. However, this is
from the uterine wall and is expelled to the exterior.
woman about 14 days after ovulation, at which time
to Prevent Menstruation
of the Corpus Luteum and
1032
Unit XIV
Endocrinology and Reproduction
Human Chorionic Gonadotropin
and Its Effect to Cause Persistence
Menstruation normally occurs in a nonpregnant
most of the endometrium of the uterus sloughs away
If this should happen after an ovum has implanted,
prevented by the secretion of human chorionic
gonadotropin by the newly developing embryonic
Coincidental with the development of the tro-
hormone
is secreted by
hormone can first be measured in the blood 8 to 9 days
rapidly to reach a maximum at about 10 to 12 weeks
Function of Human Chorionic Gonadotropin.
Human
chorionic gonadotropin is a glycoprotein having a
molecular weight of about 39,000 and much the
same molecular structure and function as luteinizing
most important function is to prevent involution of the
corpus luteum at the end of the monthly female sexual
even larger quantities of its sex hormones—proges-
sex hormones prevent menstruation and cause the
endometrium to continue to grow and store large
amounts of nutrients rather than being shed in the
decidua-like cells that
develop in the endometrium during the normal female
decidual cells—greatly
swollen and nutritious—at about the time that the
Under the influence of human chorionic
grows to about twice its initial size by a month or so
estrogens and progesterone maintains the decidual
If the corpus luteum is removed before approxi-
sufficient quantities of progesterone and estrogens to
13th to 17th week of gestation.
Human chorionic gonadotropin also exerts an
interstitial cell–stimulating effect on the testes of the
tion of testosterone during gestation is what causes the
fetus to grow male sex organs instead of female
secreted by the fetal testes also causes the testes to
descend into the scrotum.
Secretion of Estrogens
by the Placenta
24
28
32
36
40
0
4
8
12
16
20
Human chorionic
gonadotropin
Progesterone
Estrogens
Ovulation
0
0
24
22
20
18
16
14
12
10
8
6
4
2
0
300
200
100
120
100
80
60
40
20
Duration of pregnancy (weeks)
Human chorionic gonadotropin (IU/mL)
Estrogens (mg/24 hr estradiol equivalent)
Progesterone (mg/24 hr)
Parturition
of pregnancy.
gonadotropin at different stages
and progesterone, and con-
Rates of secretion of estrogens
Figure 82–7
centration of human chorionic
both the mother and the fetus.
during pregnancy. Therefore, it appears that human
native source of energy for the mother’s metabolism
the fat stores of the mother, thus providing this alter-
of such a hormonal effect is obvious. Further, the
fetus to energize its growth, the possible importance
larger quantities of glucose available to the fetus.
lization of glucose in the mother, thereby making
Third,
human chorionic somatomammotropin
growth hormone, but 100 times as much human
does. It also has a chemical structure similar to that of
those of growth hormone, causing the formation of
Second, this hormone has weak actions similar to
prolactin. However, attempts to promote lactation in
covered, it was first named
causes at least partial development of the animal’s
animals,
human chorionic somatomammotropin
First, when administered to several types of lower
important effects.
nancy hormones combined. It has several possible
somatomammotropin are uncertain, it is secreted in
the placenta. Although the functions of chorionic
of pregnancy in direct proportion to the weight of
fifth week of pregnancy. Secretion of this hormone
protein with a molecular weight of about 38,000, and
human chorionic somatomammotropin.
lactation, which is discussed later in this chapter.
the estrogen prepare the mother’s breasts for
4. The progesterone secreted during pregnancy helps
the early developing embryo.
There is also reason to
mother’s fallopian tubes and uterus to provide
the conceptus even before implantation, because
3. Progesterone contributes to the development of
of the pregnant uterus, thus preventing uterine
2. Progesterone decreases the contractility
embryo.
in the uterine endometrium, and these cells play
1. Progesterone causes decidual cells to develop
tial for the normal progression of pregnancy are as
The special effects of progesterone that are essen-
course of pregnancy, as shown in Figure 82–7.
placenta, averaging about a 10-fold increase during the
by the corpus luteum at the beginning of pregnancy, it
pregnancy—in fact, it is just as important as estrogen.
by the Placenta
embryo.
of fetal development during pregnancy, for example,
through the birth canal. There is much reason to
elastic. These changes allow easier passage of the fetus
of the mother, so that the sacroiliac joints become
The estrogens also relax the pelvic ligaments
mother’s female external genitalia.
breast ductal structure, and (3) enlargement of the
enlargement of the mother’s breasts and growth of the
cause (1) enlargement of the mother’s uterus, (2)
During pregnancy, the extreme quantities of estrogens
reproductive and associated organs of the mother.
estrogens in Chapter 81, we pointed out that these hor-
Function of Estrogen in Pregnancy.
pregnancy.)
fetal zone,
large, and about 80 per cent consists of a so-called
(The cortices of the fetal adrenal glands are extremely
the trophoblast cells into estradiol, estrone, and estriol.
glands of the fetus. These weak androgens are trans-
both in the mother’s adrenal glands and in the adrenal
hydroxydehydroepiandrosterone,
compounds,
basic substrates in the placenta. Instead, they are
the ovaries. Most important, the estrogens secreted
of production. However, the secretion of estrogens
creases to about 30 times the mother’s normal level
Figure 82–7 shows that toward the end of pregnancy,
like most other placental hormones, are secreted by
physiological studies show that these two hormones,
Chapter 82
Pregnancy and Lactation
1033
the syncytial trophoblast cells of the placenta.
the daily production of placental estrogens in-
by the placenta is quite different from secretion by
by the placenta are not synthesized de novo from
formed almost entirely from androgenic steroid
dehydroepiandrosterone and 16-
which are formed
ported by the blood to the placenta and converted by
the primary function of which seems to
be to secrete dehydroepiandrosterone during
In the discussions of
mones exert mainly a proliferative function on most
relatively limber and the symphysis pubis becomes
believe that estrogens also affect many general aspects
by affecting the rate of cell reproduction in the early
Secretion of Progesterone
Progesterone is also essential for a successful
In addition to being secreted in moderate quantities
is secreted later in tremendous quantities by the
follows:
an important role in the nutrition of the early
contractions from causing spontaneous
abortion.
it specifically increases the secretions of the
appropriate nutritive matter for the developing
morula and blastocyst.
believe that progesterone affects cell cleavage in
Human Chorionic
Somatomammotropin
A more recently discovered placental hormone is
called
It is a
it begins to be secreted by the placenta at about the
increases progressively throughout the remainder
quantities several times greater than all the other preg-
breasts and in some instances causes lactation.
Because this was the first function of the hormone dis-
human placental lactogen
and was believed to have functions similar to those of
humans with its use have not been successful.
protein tissues in the same way that growth hormone
chorionic somatomammotropin as growth hormone
is required to promote growth.
causes decreased insulin sensitivity and decreased uti-
Because glucose is the major substrate used by the
hormone promotes the release of free fatty acids from
chorionic somatomammotropin is a general metabolic
hormone that has specific nutritional implications for
iron, and the vitamins. For example, about 375 mil-
ciencies can occur, especially in calcium, phosphates,
a pregnant woman’s diet, a number of maternal defi-
normal storage depots of the mother.
these substances—some in the placenta, but most in the
extra needs, the mother’s body has already been storing
extra needs of the fetus. However, anticipating these
diet during the last months of pregnancy to supply these
ficient protein, calcium, phosphates, and iron from her
pregnancy. Ordinarily, the mother does not absorb suf-
the fetus occurs during the last trimester of pregnancy;
Nutrition During Pregnancy.
expended for muscle activity.
ing, greater amounts of energy than normal must be
heated. Also, owing to the extra load that she is carry-
a result, she frequently has sensations of becoming over-
about 15 per cent during the latter half of pregnancy. As
adrenocortical hormones, and the sex hormones, the
hormones during pregnancy, including thyroxine,
pounds.
priate prenatal control of diet, the mother’s weight gain
and partly because of hormonal factors. Without appro-
of food substrates from the mother’s blood by the fetus
increased desire for food, partly as a result of removal
During pregnancy, a woman often has a greatly
days after birth, that is, after loss of the fluid-retaining
remaining 3 pounds is generally fat accumulation. The
fluid in the blood and extracellular fluid, and the
increase of 9 pounds. About 6 pounds of this is extra
another 2 pounds, still leaving an average weight
The uterus increases about 2 pounds and the breasts
pounds is amniotic fluid, placenta, and fetal membranes.
two trimesters. Of this, about 7 pounds is fetus and 4
pounds, with most of this gain occurring during the last
The average weight gain during pregnancy is about 24
Weight Gain in the Pregnant Woman
edema, acne, and masculine or acromegalic features.
appearance, sometimes resulting in the development of
can cause marked changes in a pregnant woman’s
introitus opens more widely. Also, the various hormones
size. At the same time, the vagina enlarges and the
1100 grams, and the breasts approximately double in
instance, the uterus increases from about 50 grams to
is the increased size of the various sexual organs. For
to the fetus and to the excessive hormones of pregnancy
Body to Pregnancy
Response of the Mother’s
woman at the time of delivery.
cause relaxation of the pelvic ligaments. It has also been
probably played mainly by the estrogens, which also
bly even absent in pregnant women. Instead, this role is
estrous rat and guinea pig. This effect is weak or possi-
about 9000. This hormone, when injected, causes relax-
and progesterone.
of the ovary and by placental tissues. Its secretion is
hormone called relaxin, is secreted by the corpus luteum
substance besides the estrogens and progesterone, a
many times more calcium than the fetus does.
the baby’s birth, because the growing baby requires
to ossify its own bones. This secretion of parathyroid
ing normal calcium ion concentration in the mother’s
absorption from the mother’s bones, thereby maintain-
diet. Enlargement of these glands causes calcium
roid glands usually enlarge during pregnancy; this is
The mother’s parathy-
human chorionic thyrotropin,
hormone,
chorionic gonadotropin
ding amount. The increased thyroxine production is
ordinarily enlarges up to 50 per cent during pregnancy
The mother’s thyroid gland
tubules and, therefore, to retain fluid, occasionally
estrogens, causes a tendency for even a normal pregnant
at the end of gestation. This, along with the actions of
aldosterone,
in the fetus.
corticoids help mobilize amino acids from the mother’s
throughout pregnancy. It is possible that these gluco-
The rate of adrenocortical secre-
Conversely, pituitary secretion
corticotropin, thy-
mother enlarges at least 50 per cent during pregnancy
The anterior pituitary gland of the
Pituitary Secretion.
most notable effects are the following.
hormones on the pituitary and other glands. Some of the
but also, to some extent, from the effects of placental
mother also react markedly to pregnancy. This results
1034
Unit XIV
Endocrinology and Reproduction
Other Hormonal Factors
in Pregnancy
Almost all the nonsexual endocrine glands of the
mainly from the increased metabolic load on the mother
and increases its production of
rotropin, and prolactin.
of follicle-stimulating hormone and luteinizing
hormone is almost totally suppressed as a result of the
inhibitory effects of estrogens and progesterone from
the placenta.
Corticosteroid Secretion.
tion of the glucocorticoids is moderately increased
tissues so that these can be used for synthesis of tissues
Pregnant women usually have about a twofold
increase in the secretion of
reaching a peak
woman to reabsorb excess sodium from her renal
leading to pregnancy-induced hypertension.
Secretion by the Thyroid Gland.
and increases its production of thyroxine a correspon-
caused at least partly by a thyrotropic effect of human
secreted by the placenta and
by small quantities of a specific thyroid-stimulating
also secreted by
the placenta.
Secretion by the Parathyroid Glands.
especially true if the mother is on a calcium-deficient
extracellular fluid even while the fetus removes calcium
hormone is even more intensified during lactation after
Secretion of “Relaxin” by the Ovaries and Placenta.
Another
increased by a stimulating effect of human chorionic
gonadotropin at the same time that the corpus luteum
and the placenta secrete large quantities of estrogens
Relaxin is a polypeptide having a molecular weight of
ation of the ligaments of the symphysis pubis in the
claimed that relaxin softens the cervix of the pregnant
Most apparent among the many reactions of the mother
extra fluid is excreted in the urine during the first few
hormones from the placenta.
can be as great as 75 pounds instead of the usual 24
Metabolism During Pregnancy
As a consequence of the increased secretion of many
basal metabolic rate of the pregnant woman increases
By far the greatest growth of
its weight almost doubles during the last 2 months of
If appropriate nutritional elements are not present in
ligrams of iron is needed by the fetus to form its blood,
and an additional 600 milligrams is needed by the
occur in the normal pregnant woman. The renal effects
decreased, which is exactly opposite to the changes that
nificantly in the kidneys, brain, and liver. Both the renal
occurs in many parts of the mother’s body, most sig-
tion of the vascular endothelium, and arterial spasm
sion in the mother. In addition, there is impaired func-
salt and water retention by the mother’s kidneys and by
toxemia of pregnancy.
into the urine. This condition is called
levels during the last few months of pregnancy. This is
directly through the amniotic membranes.
turnover of the amniotic fluid is still present, which indi-
However, even after in utero death of a fetus, some
of the gastrointestinal tract and lungs of the fetus.
Likewise, a certain amount of absorption occurs by way
the fluid is derived from renal excretion by the fetus.
an average of once every 15 hours. A large portion of
water in amniotic fluid is replaced once every 3 hours,
formation of amniotic fluid show that, on average, the
as much as several liters. Isotope studies of the rate of
liliters and 1 liter, but it can be only a few milliliters or
Normally, the volume of
the urine. When all these effects are considered, the
much as 50 per cent during pregnancy, which tends to
Second, the glomerular filtration rate increases as
sodium, chloride, and water is increased as much as
First, the renal tubules’ reabsorptive capacity for
occur.
addition, several special alterations of urinary function
intake and increased load or excretory products. But in
The rate of urine formation by a pregnant woman is
Function of the Maternal Urinary System During Pregnancy
sion of the diaphragm is decreased. Consequently, the
upward against the diaphragm, so that the total excur-
upward against the abdominal contents, and these press
woman. Simultaneously, the growing uterus presses
respiratory center’s sensitivity to carbon dioxide. The
tion even more, because progesterone increases the
esterone during pregnancy increase the minute ventila-
increase. It is also believed that the high levels of prog-
These effects cause the mother’s minute ventilation to
birth of the baby is about 20 per cent above normal, and
nant woman and because of her greater size, the total
erable safety factor for the mother.
during delivery of the baby, thereby allowing a consid-
extra blood in her circulatory system. Only about one
birth of the baby, the mother has about 1 to 2 liters of
with the excess fluid volume. Therefore, at the time of
by the kidneys. Also, the bone marrow becomes increas-
increased in pregnancy, and to increased fluid retention
in part, to aldosterone and estrogens, which are greatly
The cause of the increased volume is likely due, at least
half of pregnancy, as shown by the curve of Figure 82–8.
normal. This increase occurs mainly during the latter
The maternal blood
Blood Volume During Pregnancy.
despite the high uterine blood flow.
above normal during the last 8 weeks of pregnancy,
unexplained, the cardiac output falls to only a little
normal by the 27th week of pregnancy; then, for reasons
the mother’s cardiac output to 30 to 40 per cent above
general increase in the mother’s metabolism, increases
during the last month of pregnancy. This, plus the
Pregnancy.
Blood Flow Through the Placenta, and Cardiac Output During
Changes in the Maternal Circulatory
hemorrhage, caused by the birth process.
thrombin to prevent hemorrhage, particularly brain
mother’s diet so that the baby will have sufficient pro-
birth of the baby, vitamin K is often added to the
testinal tract without vitamin D. Finally, shortly before
is normally poorly absorbed by the mother’s gastroin-
quantity of calcium used by the fetus is small, calcium
that she receive vitamin D, because although the total
. Also, it is especially important
hypochromic anemia
iron in her food, a pregnant woman usually develops
more than 700 milligrams. Therefore, without sufficient
pregnancy is often only 100 milligrams and almost never
mother to form her own extra blood. The normal store
Chapter 82
Pregnancy and Lactation
1035
of nonhemoglobin iron in the mother at the outset of
System During Pregnancy
About 625 milliliters of blood flows through
the maternal circulation of the placenta each minute
volume shortly before term is about 30 per cent above
ingly active and produces extra red blood cells to go
fourth of this amount is normally lost through bleeding
Maternal Respiration During Pregnancy
Because of the increased basal metabolic rate of a preg-
amount of oxygen used by the mother shortly before
a commensurate amount of carbon dioxide is formed.
net result is an increase in minute ventilation of about
50 per cent and a decrease in arterial P
CO
2
to several
millimeters of mercury below that in a nonpregnant
respiratory rate is increased to maintain the extra
ventilation.
usually slightly increased because of increased fluid
50 per cent as a consequence of increased production
of steroid hormones by the placenta and adrenal
cortex.
increase the rate of water and electrolyte excretion in
normal pregnant woman ordinarily accumulates only
about 6 pounds of extra water and salt.
Amniotic Fluid and Its Formation
amniotic fluid (the fluid inside
the uterus in which the fetus floats) is between 500 mil-
and the electrolytes sodium and potassium are replaced
cates that some of the fluid is formed and absorbed
Preeclampsia and Eclampsia
About 5 per cent of all pregnant women experience a
rapid rise in arterial blood pressure to hypertensive
also associated with leakage of large amounts of protein
preeclampsia or
It is often characterized by excess
weight gain and development of edema and hyperten-
blood flow and the glomerular filtration rate are
0
4
8
12 16 20 24 28 32 36 40 44
Parturition
0
6
5
4
Duration of pregnancy (weeks)
Blood volume
(liters)
Effect of pregnancy to increase the mother’s blood volume.
Figure 82–8
tions. For instance, the obstetrician frequently induces
There is reason to
Stretch or Irritation of the Cervix.
stretch in eliciting uterine contractions.
child, which emphasizes the importance of mechanical
19 days
twins are born, on average,
elicit smooth muscle contraction. Note especially that
edly in the uterus because of fetal movements, can also
tility. Further, intermittent stretch, as occurs repeat-
Mechanical Factors That Increase
the intensity of uterine contractions.
centration at the time of labor. These, too, can increase
sol, another possible uterine stimulant. In addition, the
fetus’s adrenal glands secrete large quantities of corti-
which might play a role in exciting the uterus. Also, the
The fetus’s pitu-
occurs during labor, can cause a neurogenic reflex
that irritation or stretching of the uterine cervix, as
prolonged. (4) Experiments in animals indicate
animals can still deliver their young at term, labor is
at the time of labor. (3) Although hypophysectomized
months of pregnancy. (2) The rate of oxytocin secre-
receptors and, therefore, increases its responsiveness
term: (1) The uterine muscle increases its oxytocin
causes uterine contraction (see Chapter 75). There are
uterus.
toward the end of pregnancy to be at least partly
slightly. Therefore, it has been postulated that the
nancy, but from the seventh month onward, estrogen
also because of other poorly understood effects. Both
between the adjacent uterine smooth muscle cells, but
degree of uterine contractility,
partly because
estrogens have a definite tendency to increase the
helping to prevent expulsion of the fetus. Conversely,
inhibits uterine contractility during pregnancy, thereby
Hormonal Factors That Increase
(2) progressive mechanical changes.
increased excitability of the uterine musculature, and
tion: (1) progressive hormonal changes that cause
known, but at least two major categories of effects lead
cal contractions that the baby is expelled. The exact
excitable, until finally it develops such strong rhythmi-
pregnancy, the uterus becomes progressively more
means birth of the baby. Toward the end of
Parturition
Near Term
Parturition
mothers has been reduced to 1 per cent or less.
immediate termination of pregnancy—by cesarean
to reduce the arterial pressure to normal, followed by
centage of eclamptic mothers die. However, with optimal
before birth of the baby. Without treatment, a high per-
toxic condition of the body. It usually occurs shortly
the liver; often extreme hypertension; and a generalized
coma; greatly decreased kidney output; malfunction of
clonic seizures in the mother, sometimes followed by
tumor necrosis factor-
lial dysfunction are still uncertain, some experimental
increased blood pressure. Although the factors that link
flow to the kidneys, excess salt and water retention, and
impaired vascular endothelial function, decreased blood
stances that enter the mother’s circulation and cause
This, in turn, causes the placenta to release various sub-
these adaptive changes, for reasons that are still unclear,
preeclampsia, the maternal arterioles fail to undergo
with low resistance to blood flow. In patients with
placental development, the trophoblasts invade the
of the maternal vascular endothelium. During normal
resulting in the placenta’s
within a few days after birth of the baby. There is also
support of this, the acute symptoms usually disappear
in the mother caused by the presence of the fetus. In
basis is still lacking. Another theory is that preeclamp-
cental or adrenal hormones, but proof of a hormonal
Various attempts have been made to prove that
protein deposit in the basement membranes.
1036
Unit XIV
Endocrinology and Reproduction
also include thickened glomerular tufts that contain a
preeclampsia is caused by excessive secretion of pla-
sia results from some type of autoimmunity or allergy
evidence that preeclampsia is initiated by insufficient
blood supply to the placenta,
release of substances that cause widespread dysfunction
arterioles of the uterine endometrium and completely
remodel the maternal arterioles into large blood vessels
and there is insufficient blood supply to the placenta.
reduced placental blood supply with maternal endothe-
studies suggest a role for increased levels of inflamma-
tory cytokines such as
a and
interleukin-6.
Eclampsia is an extreme degree of preeclampsia,
characterized by vascular spasm throughout the body;
and immediate use of rapidly acting vasodilating drugs
section if necessary—the mortality even in eclamptic
Increased Uterine Excitability
cause of the increased activity of the uterus is not
up to the intense contractions responsible for parturi-
Uterine Contractility
Increased Ratio of Estrogens to Progesterone.
Progesterone
estrogens increase the number of gap junctions
progesterone and estrogen are secreted in progres-
sively greater quantities throughout most of preg-
secretion continues to increase while progesterone
secretion remains constant or perhaps even decreases
estrogen-to-progesterone ratio increases sufficiently
responsible for the increased contractility of the
Effect of Oxytocin on the Uterus.
Oxytocin is a hormone
secreted by the neurohypophysis that specifically
four reasons to believe that oxytocin might be impor-
tant in increasing the contractility of the uterus near
to a given dose of oxytocin during the latter few
tion by the neurohypophysis is considerably increased
through the paraventricular and supraoptic nuclei of
the hypothalamus that causes the posterior pituitary
gland (the neurohypophysis) to increase its secretion
of oxytocin.
Effect of Fetal Hormones on the Uterus.
itary gland secretes increasing quantities of oxytocin,
fetal membranes release prostaglandins in high con-
Uterine Contractility
Stretch of the Uterine Musculature.
Simply stretching
smooth muscle organs usually increases their contrac-
earlier than a single
believe that stretching or irritating the uterine cervix
is particularly important in eliciting uterine contrac-
labor by rupturing the membranes so that the head of
The uterine contractions during labor begin mainly at
Mechanics of Parturition
the baby.
contractions of these muscles. The abdominal contrac-
spinal cord to the abdominal muscles, causing intense
causing suffering, elicit neurogenic reflexes in the
and from the birth canal. These signals, in addition to
labor, pain signals originate both from the uterus itself
contractions would fade away.
back could go into a retrograde decline, and the labor
to re-excite the uterus sufficiently, the positive feed-
tive feedback must be stronger than the previous one.
new cycle of the posi-
each
vicious circle to continue,
stronger and then fade away. Remember that for a
labor, in which the contractions become stronger and
initiates a vicious circle when the gain of the feedback
because positive feedback
traction greater than the preceding one, the process
cause this type of feedback, with each succeeding con-
the first, a third stronger than the second, and so forth.
cially at the cervix, and this increases uterine
becomes strong enough to irritate the uterus, espe-
end of pregnancy. Eventually a uterine contraction
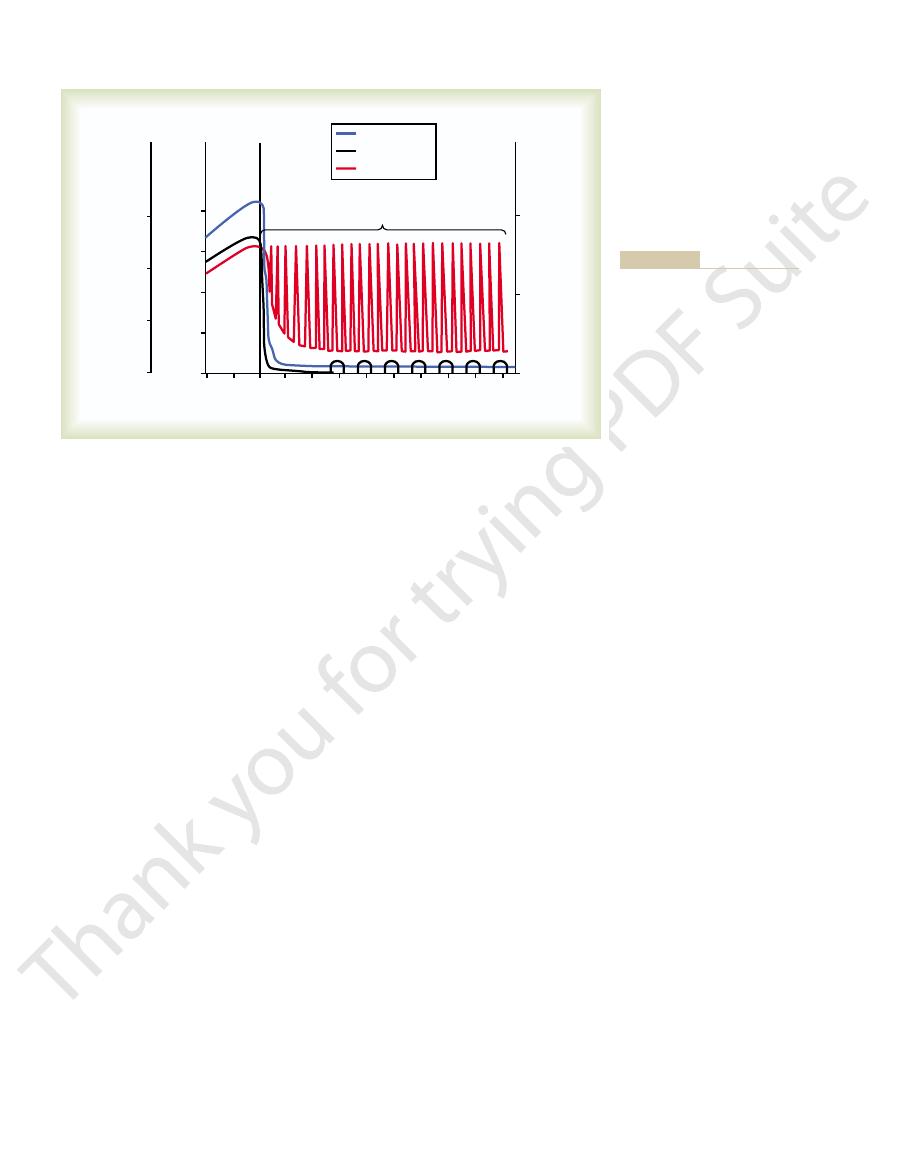
To summarize, we can assume that multiple factors
means for increasing uterine contractility.
pituitary gland to secrete oxytocin, which is another
baby’s head. (2) Cervical stretching also causes the
to contract, and this contraction stretches the cervix
increase uterine contractions during labor: (1) Stretch-
Second, two known types of positive feedback
a critical value.
positive feedback in control systems, one can see that
achieved. Referring to the discussion in Chapter 1 of
contraction becomes greater than a critical value, each
positive feedback. That is, once the strength of uterine
First, labor contractions obey all the principles of
porting it are the following.
is shown in Figure 82–9, and the observations sup-
process repeats until the baby is expelled. This theory
positive feedback to the uterine body. Thus, the
ity of the uterine body. This pushes the baby forward,
the cervix by the fetus’s head finally becomes great
positive feedback
been proposed for explaining the onset of labor. The
types of physiological control systems, a theory has
tractions. However, based on experience with other
We do not know what suddenly changes the slow,
labor contractions.
labor,
parturition. This process is called
force the baby through the birth canal, thereby causing
denly, within hours, to become exceptionally strong
toward the end of pregnancy; then they change sud-
These contractions become progressively stronger
Braxton Hicks contractions.
During most of the months of pregnancy, the uterus
Onset of Labor—A Positive Feedback
the uterus.
cervix initiates reflexes to the body of the uterus, but
the body of the uterus is not known. It has been
The mechanism by which cervical irritation excites
usual or irritates it in other ways.
Chapter 82
Pregnancy and Lactation
1037
the baby stretches the cervix more forcefully than
suggested that stretching or irritation of nerves in the
the effect could also result simply from myogenic
transmission of signals from the cervix to the body of
Mechanism for Its Initiation
undergoes periodic episodes of weak and slow rhyth-
mical contractions called
contractions that start stretching the cervix and later
and the strong
contractions that result in final parturition are called
weak rhythmicity of the uterus into strong labor con-
theory suggests that stretching of
enough to elicit a strong reflex increase in contractil-
which stretches the cervix more and initiates more
contraction leads to subsequent contractions that
become stronger and stronger until maximum effect is
this is the precise nature of all positive feedback mech-
anisms when the feedback gain becomes greater than
ing of the cervix causes the entire body of the uterus
even more because of the downward thrust of the
increase the contractility of the uterus toward the
contractility still more because of positive feedback,
resulting in a second uterine contraction stronger than
Once these contractions become strong enough to
proceeds to completion—all
is greater than a critical level.
One might ask about the many instances of false
If at any time after labor starts some contractions fail
Abdominal Muscle Contractions
During Labor
Once uterine contractions become strong during
tions add greatly to the force that causes expulsion of
the top of the uterine fundus and spread downward over
1. Baby's head stretches cervix
2. Cervical stretch excites fundic contraction
3. Fundic contraction pushes baby down and stretches
cervix some more
4. Cycle repeats over and over again
Theory for the onset of intensely strong contractions during labor.
Figure 82–9

in the development of the breasts.
metabolism, which presumably explains their function
adrenal glucocorticoids,
growth hormone, pro-
stroma of the breasts increases in quantity, and large
breasts to grow and branch. Simultaneously, the
through pregnancy, the large quantities of estrogens
estrogen state of pregnancy, and only then does the
addition, far greater growth occurs during the high-
plus the deposition of fat to give the breasts mass. In
estrogens of the monthly female sexual cycle; estro-
at puberty. This development is stimulated by the
The breasts, shown in Figure 82–10, begin to develop
ready for normal, nongravid sex life again.
continuing for a total of about 10 days. After this time,
“lochia,” which is first bloody and then serous in nature,
surface autolyzes, causing a vaginal discharge known as
of the uterus, the placental site on the endometrial
of lactation, as discussed later. During early involution
it was before pregnancy. This effect of lactation results
the mother lactates, the uterus may become as small as
ate postpartum weight within 1 week, and in 4 weeks, if
involutes. Its weight becomes less than half its immedi-
During the first 4 to 5 weeks after parturition, the uterus
instead of by the visceral sensory nerves.
mother’s spinal cord and brain by somatic nerves
in the vaginal canal itself. This pain is conducted to the
ineal stretching, and stretching or tearing of structures
more severe pain is caused by cervical stretching, per-
fetus is being expelled through the birth canal, much
However, during the second stage of labor, when the
sensory fibers leading from the uterus, have been
hypogastric nerves,
in the uterus. This pain is not felt when the visceral
considerable pain. The cramping pain in early labor
With each uterine contraction, the mother experiences
centa. In addition, it is believed that vasoconstrictor
through the uterine wall. Therefore, contraction of
liliters by the following mechanism: The smooth muscle
opens the placental sinuses and causes bleeding. The
from its implantation site. Separation of the placenta
the uterus and the placenta, thus separating the placenta
size, which causes a
For 10 to 45 minutes after birth of the baby, the
of the Placenta
pregnancy.
of labor,
until delivery is effected. This is called the
above, it continues to wedge its way through the canal
into the birth canal, and with additional force from
through the vagina. Then the fetus’s head moves rapidly
Once the cervix has dilated fully, the fetal membranes
many pregnancies.
the first pregnancy but often only a few minutes after
of the fetus. This stage usually lasts for 8 to 24 hours in
labor contractions begin in the uterus. The so-called
cervix becomes soft, which allows it to stretch when
is the uterine cervix. Toward the end of pregnancy, the
The first major obstruction to expulsion of the fetus
ing instances, the buttocks are presented first. The head
of the baby to be expelled, and in most of the remain-
In about 95 per cent of births, the head is the first part
death of the fetus.
stimulants, such as oxytocin, can cause uterine spasm
were continuous. Indeed, overuse of various uterine
intermittently, because strong contractions impede or
contractions. The combined contractions of the uterine
greatly, with only a short period of relaxation between
to 3 minutes, and the intensity of contraction increases
the contractions finally appear as often as once every 1
occur only once every 30 minutes. As labor progresses,
In the early part of labor, the contractions might
Therefore, each uterine contraction tends to force the
the body of the uterus. Also, the intensity of contraction
1038
Unit XIV
Endocrinology and Reproduction
is great in the top and body of the uterus but weak in
the lower segment of the uterus adjacent to the cervix.
baby downward toward the cervix.
and abdominal musculature during delivery of the baby
cause a downward force on the fetus of about 25 pounds
during each strong contraction.
It is fortunate that the contractions of labor occur
sometimes even stop blood flow through the placenta
and would cause death of the fetus if the contractions
rather than rhythmical contractions and can lead to
acts as a wedge to open the structures of the birth canal
as the fetus is forced downward.
first
stage of labor is a period of progressive cervical dilation,
lasting until the cervical opening is as large as the head
usually rupture and the amniotic fluid is lost suddenly
second stage
and it may last from as little as 1 minute after
many pregnancies to 30 minutes or more in the first
Separation and Delivery
uterus continues to contract to a smaller and smaller
shearing effect between the walls of
amount of bleeding is limited to an average of 350 mil-
fibers of the uterine musculature are arranged in figures
of eight around the blood vessels as the vessels pass
the uterus after delivery of the baby constricts the
vessels that had previously supplied blood to the pla-
prostaglandins formed at the placental separation site
cause additional blood vessel spasm.
Labor Pains
is probably caused mainly by hypoxia of the uterine
muscle resulting from compression of the blood vessels
sensory
which carry the visceral
sectioned.
Involution of the Uterus
After Parturition
from the suppression of pituitary gonadotropin and
ovarian hormone secretion during the first few months
the endometrial surface becomes re-epithelialized and
Lactation
Development of the Breasts
gens stimulate growth of the breasts’ mammary glands
glandular tissue become completely developed for the
production of milk.
Growth of the Ductal System—Role of the Estrogens.
All
secreted by the placenta cause the ductal system of the
quantities of fat are laid down in the stroma.
Also important for growth of the ductal system are
at least four other hormones:
lactin, the
and insulin. Each of
these is known to play at least some role in protein
The hypothal-
erably after 7 to 9 months.
several years if the child continues to suckle, although
or so. However, milk production can continue for
itary damage or if nursing does not continue, the
subsequent nursing periods. If this prolactin surge is
prolactin acts on the mother’s breasts to keep the
1 hour, which is also shown in Figure 82–11. This
each time the mother nurses her baby, nervous signals
next few weeks, as shown in Figure 82–11. However,
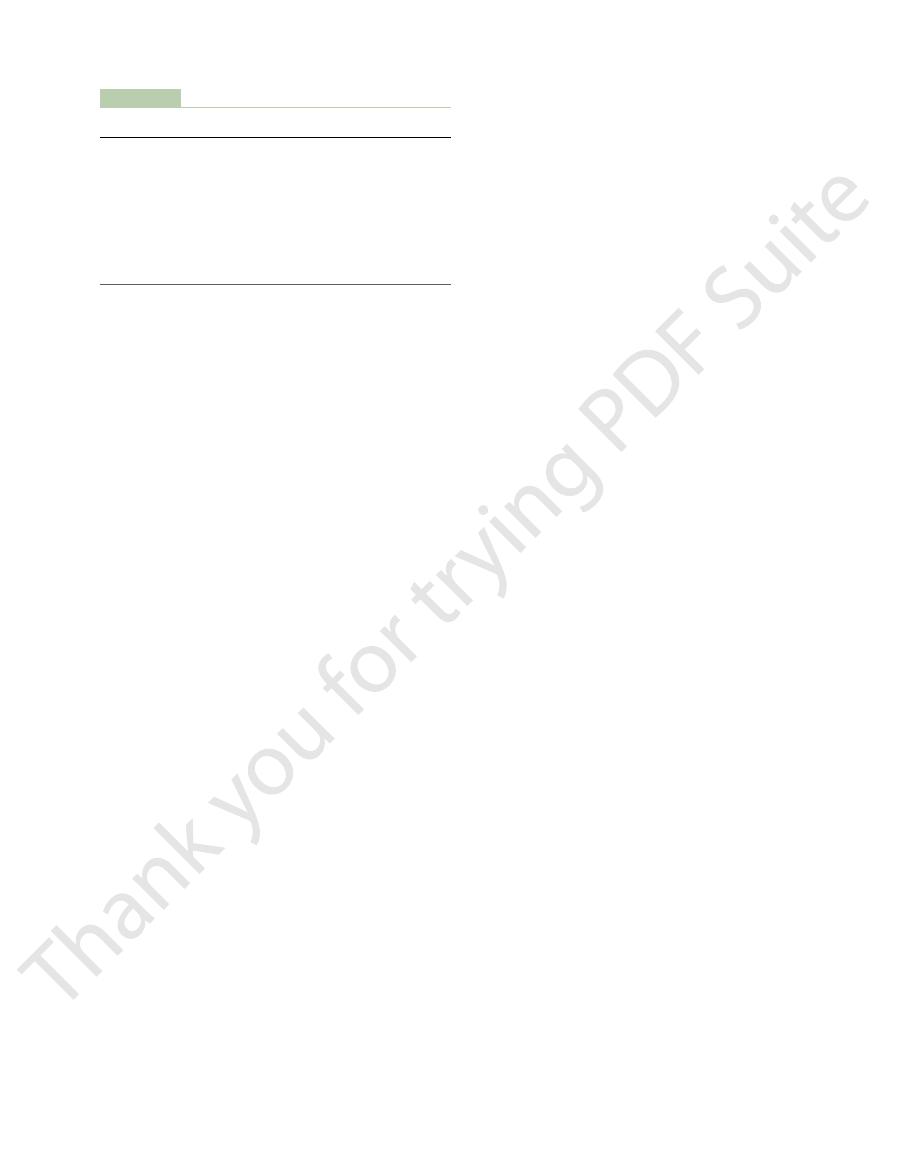
After birth of the baby, the
the amino acids, fatty acids, glucose, and calcium
These hormones are necessary to provide
growth hormone, cortisol, parathyroid hormone,
mother’s other hormones as well, but most important
instead of colostrum. This secretion of milk requires
promoting role, and over the next 1 to 7 days, the
the mother’s pituitary gland to assume its natural milk-
Immediately after the baby is born, the sudden loss
teins and lactose as milk, but it has almost no fat, and
The fluid secreted during the last few days before and
and progesterone, no more than a few milliliters of
Even so, because of the suppressive effects of estrogen
lactin from the mother’s pituitary during pregnancy.
bly has lactogenic properties, thus supporting the pro-
human chorionic somatomammotropin,
In addition, the placenta secretes large quantities of
end of pregnancy is shown in Figure 82–11.
nonpregnant level. This high level of prolactin at the
fifth week of pregnancy until birth of the baby, at
secreted by the mother’s anterior pituitary gland, and
on milk secretion—promoting it. This hormone is
Conversely, the
nancy, a specific effect of both these hormones is to
of Prolactin
menstrual cycle.
the alveoli. These changes are analogous to the
of the breast lobules, with budding of alveoli and
synergistically with estrogen, as well as with the other
ductal system has developed, progesterone—acting
progesterone.
Final development of the breasts into milk-
Chapter 82
Pregnancy and Lactation
1039
Development of the Lobule-Alveolar System—Role of Proges-
terone.
secreting organs also requires
Once the
hormones just mentioned—causes additional growth
development of secretory characteristics in the cells of
secretory effects of progesterone on the endometrium
of the uterus during the latter half of the female
Initiation of Lactation—Function
Although estrogen and progesterone are essential for
the physical development of the breasts during preg-
inhibit the actual secretion of milk.
hormone prolactin has exactly the opposite effect
its concentration in her blood rises steadily from the
which time it has risen to 10 to 20 times the normal
which proba-
fluid are secreted each day until after the baby is born.
the first few days after parturition is called colostrum;
it contains essentially the same concentrations of pro-
its maximum rate of production is about 1/100 the
subsequent rate of milk production.
of both estrogen and progesterone secretion from the
placenta allows the lactogenic effect of prolactin from
breasts begin to secrete copious quantities of milk
an adequate background secretion of most of the
are
and insulin.
required for milk formation.
basal level of prolactin
secretion returns to the nonpregnant level over the
from the nipples to the hypothalamus cause a 10- to
20-fold surge in prolactin secretion that lasts for about
mammary glands secreting milk into the alveoli for the
absent or blocked as a result of hypothalamic or pitu-
breasts lose their ability to produce milk within 1 week
the rate of milk formation normally decreases consid-
Hypothalamic Control of Prolactin Secretion.
amus plays an essential role in controlling prolactin
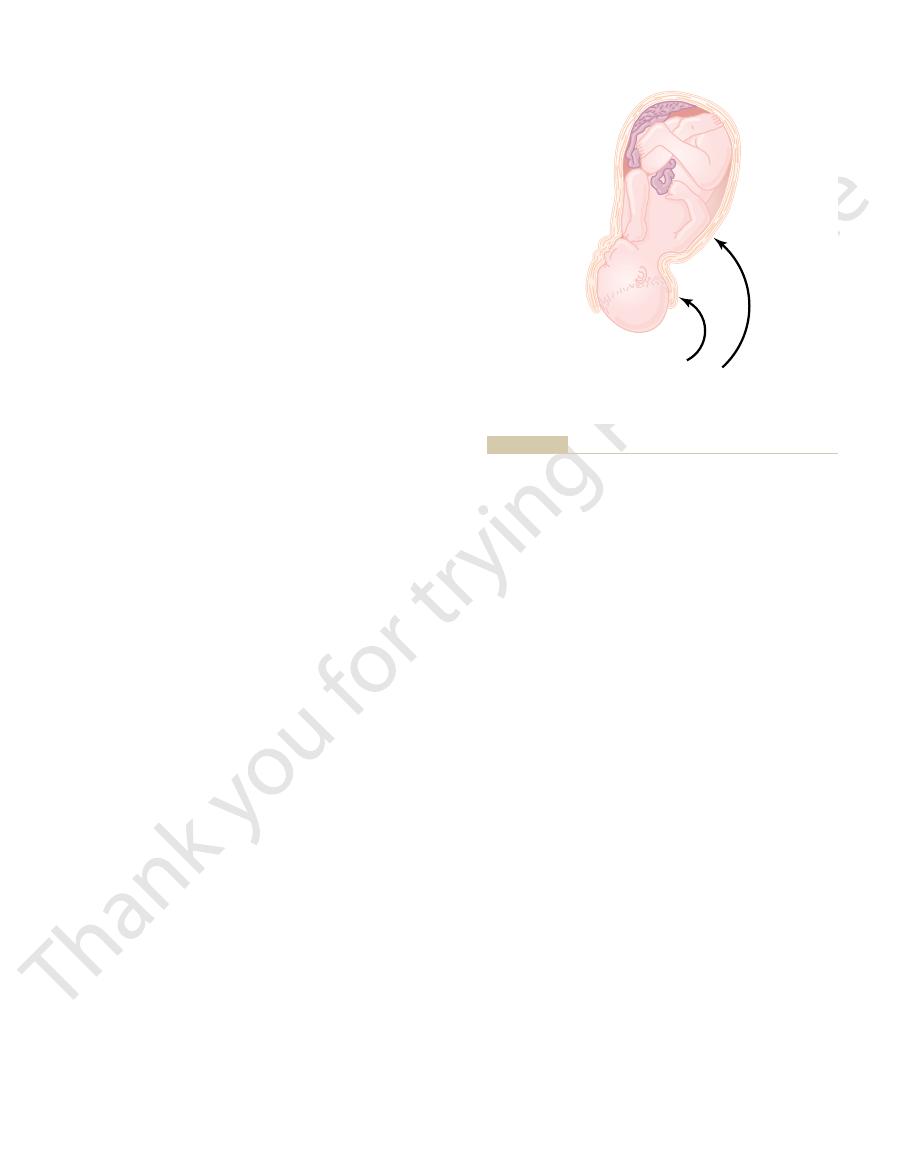
Pectoralis major
Adipose tissue
Lobules and
alveoli
Lactiferous
sinus (ampulla)
Lactiferous duct
Nipple
Areola
Ductule
Alveoli
A
B
C
Milk
Milk
secreting
epithelial
cells
Lobule
Myoepithelial cells
and milk-secreting cells of an alveolus
(milk ducts) that constitute its mammary gland
The breast and its secretory lobules, alveoli, and lactiferous ducts
Figure 82–10
(A). The enlarge-
ments show a lobule (B)
(C).
nervous system stimulation throughout the mother’s
that breast but also in the opposite breast. It is espe-
milk let-down.
milk ejection
begins to suckle, milk begins to flow. This process is
milk. Thus, within 30 seconds to 1 minute after a baby
baby’s suckling becomes effective in removing the
10 to 20 mm Hg. Then the
tract, thereby expressing the milk from the alveoli into
blood to the breasts, where it causes
cause prolactin secretion. The oxytocin is carried in the
oxytocin
hypothalamus, where they cause nerve signals that
nipples to the mother’s spinal cord and then to her
for the first half minute or so. Sensory impulses must
When the baby suckles, it receives virtually no milk
as follows.
oxytocin,
the baby can obtain it. This is caused by a combined
ually leak from the breast nipples. Instead, the milk
into the ductal system and, therefore, does not contin-
breasts, but milk does not flow easily from the alveoli
Milk Secretion—Function of Oxytocin
though nursing continues.
hormones to reinstate the monthly sexual cycle, even
those who nurse their babies only some of the time,
months of lactation, in some mothers, especially in
follicle-stimulating hormone. However, after several
mus. This, in turn, suppresses formation of the pituitary
until a few weeks after cessation of nursing. The reason
the ovarian cycle (and ovulation) does not resume
In most nursing mothers,
for Many Months After Delivery.
dopamine,
hormone.
gland. This factor is called
Therefore, it is believed that anterior pituitary secre-
anterior pituitary hormones.
prolactin production. Consequently, damage
production of all the other hormones, but it mainly
in one aspect: The hypothalamus mainly
pituitary hormones. However, this control is different
secretion, as it does for almost all the other anterior
1040
Unit XIV
Endocrinology and Reproduction
stimulates
inhibits
to the hypothalamus or blockage of the hypothalamic-
hypophysial portal system often increases prolactin
secretion while it depresses secretion of the other
tion of prolactin is controlled either entirely or almost
entirely by an inhibitory factor formed in the hypo-
thalamus and transported through the hypothalamic-
hypophysial portal system to the anterior pituitary
prolactin inhibitory
It is almost certainly the same as the cate-
cholamine
which is known to be secreted
by the arcuate nuclei of the hypothalamus and can
decrease prolactin secretion as much as 10-fold.
Suppression of the Female Ovarian Cycles in Nursing Mothers
seems to be that the same nervous signals from
the breasts to the hypothalamus that cause prolactin
secretion during suckling—either because of the
nervous signals themselves or because of a subsequent
effect of increased prolactin—inhibit secretion of
gonadotropin-releasing hormone by the hypothala-
gonadotropic hormones—luteinizing hormone and
the pituitary begins to secrete sufficient gonadotropic
Ejection (or “Let-Down”) Process in
Milk is secreted continuously into the alveoli of the
must be ejected from the alveoli into the ducts before
neurogenic and hormonal reflex that involves the
posterior pituitary hormone
first be transmitted through somatic nerves from the
promote
secretion at the same time that they
myoepithelial cells
(which surround the outer walls of the alveoli) to con-
the ducts at a pressure of
+
called
or
Suckling on one breast causes milk flow not only in
cially interesting that fondling of the baby by the
mother or hearing the baby crying often gives enough
of an emotional signal to the hypothalamus to cause
milk ejection.
Inhibition of Milk Ejection.
A particular problem in
nursing a baby comes from the fact that many psy-
chogenic factors or even generalized sympathetic
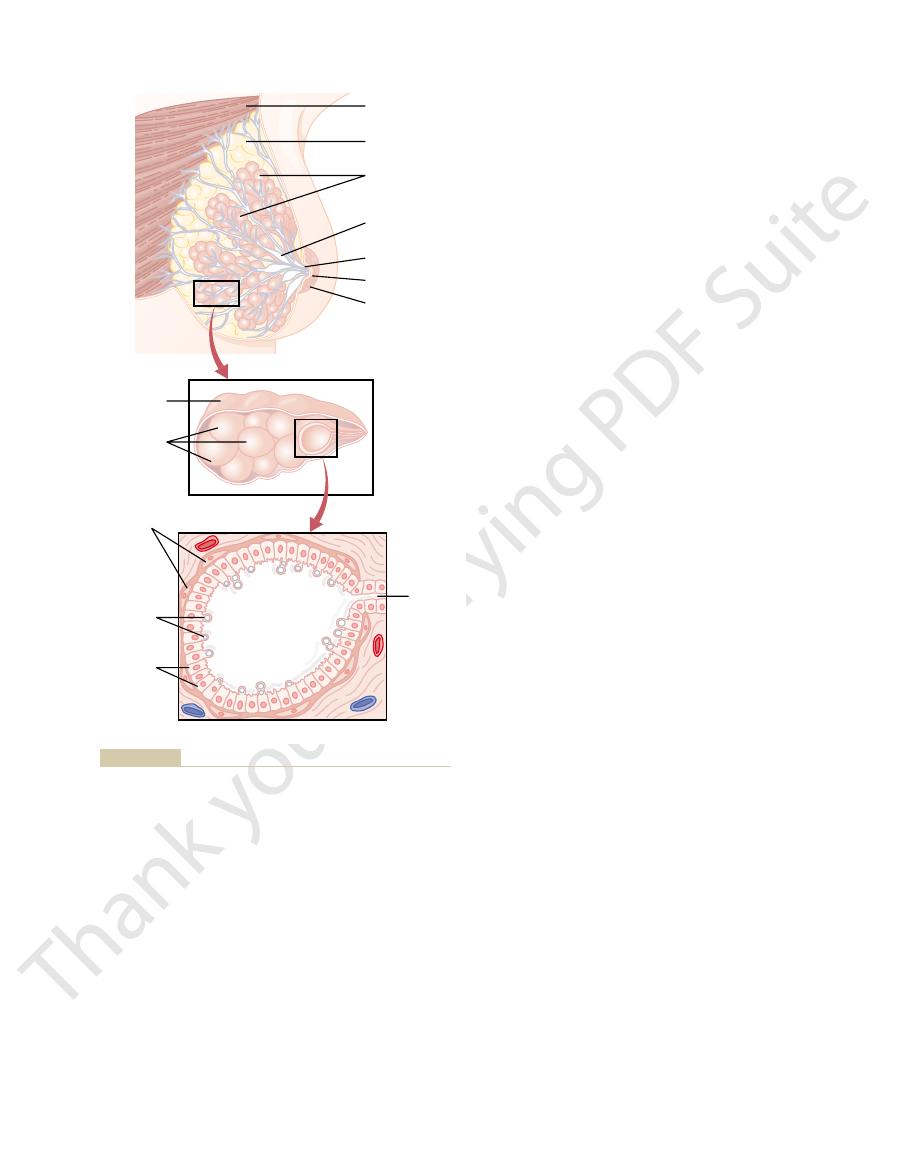
Weeks after parturition
24
28
32
36
4
0
4
8
12
16
20
-
8
-
Intermittent secretion
of prolactin during
nursing
Progesterone
Prolactin
Estrogens
Parturition
0
300
2.0
200
100
0
1.5
1.0
0.5
0
200
100
Progesterone (mg/24 hr)
Estrogens (mg/24 hr estradiol equivalent)
Prolactin (ng/mL)
time) during and after periods of
secretion (for about 1 hour at a
tent periods of marked prolactin
parturition, but also the intermit-
prolactin secretion back to basal
Note especially the decrease of
turition and 36 weeks thereafter.
prolactin for 8 weeks before par-
of estrogens, progesterone, and
Changes in rates of secretion
Figure 82–11
levels within a few weeks after
nursing.
fetal development. J Nutr 134:2169, 2004.
Wu G, Bazer FW, Cudd TA, et al: Maternal nutrition and
tension During Pregnancy. Hypertension 41:437, 2003.
of the NHLBI Working Group on Research on Hyper-
Roberts JM, Pearson G, Cutler J, Lindheimer M: Summary
pre-eclampsia. Lancet 357:53, 2001.
Roberts JM, Cooper DW: Pathogenesis and genetics of
Immunol 2:656, 2002.
Moffett-King A: Natural killer cells and pregnancy. Nat Rev
Ann N Y Acad Sci 997:136, 2003.
pituitary-adrenal axes during pregnancy and postpartum.
Mastorakos G, Ilias I: Maternal and fetal hypothalamic-
differentiation. N Engl J Med 350:367, 2004.
MacLaughlin DT, Donahoe PK: Sex determination and
Immunol 4:565, 2004.
taining an irreplaceable immunological resource. Nat Rev
Labbok MH, Clark D, Goldman AS: Breastfeeding: main-
models.Am J Physiol Regul Integr Comp Physiol 283:R29,
arterial pressure in preeclampsia: lessons from animal
Khalil RA, Granger JP: Vascular mechanisms of increased
327:610, 2003.
Khalaf Y: ABC of subfertility: tubal subfertility. BMJ
ine growth retardation. Ann N Y Acad Sci 997:150, 2003.
Kanaka-Gantenbein C, Mastorakos G, Chrousos GP:
Hall JG: Twinning. Lancet 362:735, 2003.
biology of an old hormone. Annu Rev Physiol 64:47, 2002.
Goffin V, Binart N, Touraine P, Kelly PA: Prolactin: the new
ture, function, and regulation. Physiol Rev 81:629, 2001.
Gimpl G, Fahrenholz F: The oxytocin receptor system: struc-
Rev 80:1523, 2000.
structure, function, and regulation of secretion. Physiol
Freeman ME, Kanyicska B, Lerant A, Nagy G: Prolactin:
tion of pre-eclampsia. Lancet 357:209, 2001.
Dekker G, Sibai B: Primary, secondary, and tertiary preven-
15:2440, 2004.
the pathophysiology of preeclampsia. J Am Soc Nephrol
Davison JM, Homuth V, Jeyabalan A, et al: New aspects in
Ann N Y Acad Sci 995:84, 2003.
phogenesis and formation of the placental villous tree.
Cross JC, Simmons DG, Watson ED: Chorioallantoic mor-
labor. Ann N Y Acad Sci 943:225, 2001.
Challis JR, Lye SJ, Gibb W, et al: Understanding preterm
parturition. Ann N Y Acad Sci 828:273, 1997.
Casey ML, MacDonald PC: The endocrinology of human
inhibitor. Endocr Rev 22:724, 2001.
Ben-Jonathan N, Hnasko R: Dopamine as a prolactin (PRL)
cular-renal dysfunction. News Physiol Sci 16:282, 2001.
Preeclampsia: linking placental ischemia with cardiovas-
Alexander BT, Bennett WA, Khalil RA, Granger JP:
environment of the human being.
baby in place of mother’s milk, the protective agents
When cow’s milk is used to supply nutrition for the
rhea in newborns.
bacteria, which often cause lethal diar-
Escherichia coli
infections in newborn babies. Particularly important
macrophages,
types of white blood cells are secreted, including both
milk along with the nutrients. Also, several different
against infection. For instance, multiple types of
nutrients, but it also provides important protection
big problem during pregnancy, but it can become more
fied. The mother’s bone decalcification is usually not a
greatly, and the bones become progressively decalci-
calcium and phosphate, the parathyroid glands enlarge
the intake of these substances. To supply the needed
of vitamin D, the output of calcium and phosphate by
phate may be lost each day; unless the mother is drink-
mother’s glucose. Also, 2 to 3 grams of calcium phos-
lactose, which must be derived by conversion from the
enter the milk each day, and about 100 grams of
from the mother. For instance, about 50 grams of fat
if the mother has twins). With this degree of lactation,
At the height of lactation in the human mother, 1.5
cow’s milk.
other minerals, is found in human milk compared with
one third as much ash, which contains calcium and
or more times greater than in human milk. Finally, only
concentration of protein in cow’s milk is ordinarily two
about 50 per cent greater than in cow’s milk, but the
milk. The concentration of lactose in human milk is
Table 82–1 lists the contents of human milk and cow’s
Caused by Lactation
Metabolic Drain on the Mother
Milk Composition and the
successful in nursing their babies.
depress milk ejection. For this reason, many mothers
Chapter 82
Pregnancy and Lactation
1041
body can inhibit oxytocin secretion and consequently
must have an undisturbed puerperium if they are to be
liters of milk may be formed each day (and even more
great quantities of metabolic substrates are drained
ing large quantities of milk and has an adequate intake
the lactating mammae will often be much greater than
important during lactation.
Antibodies and Other Anti-infectious Agents in Milk.
Not only
does milk provide the newborn baby with needed
anti-
bodies and other anti-infectious agents are secreted in
neutrophils and
some of which are
especially lethal to bacteria that could cause deadly
are antibodies and macrophages that destroy
in it are usually of little value because they are
normally destroyed within minutes in the internal
References
Endocrine-related causes and consequences of intrauter-
2002.
Table 82–1
Lactalbumin and other
0.4
0.7
Casein
0.9
2.7
Lactose
6.8
4.8
Fat
3.3
3.5
Water
88.5
87.0
Constituent
Human Milk (%)
Cow’s Milk (%)
Composition of Milk
proteins
Ash
0.2
0.7
