147
Epithelial ,Connective ,Muscular &
:
four basic types of tissue
only
Human body composed of
Nervous Tissues. These tissues, which are formed by cells and molecules of the extracellular
matrix, exist not as isolated units but rather in association with one another and in variable
proportions, forming different organs and systems of the body.
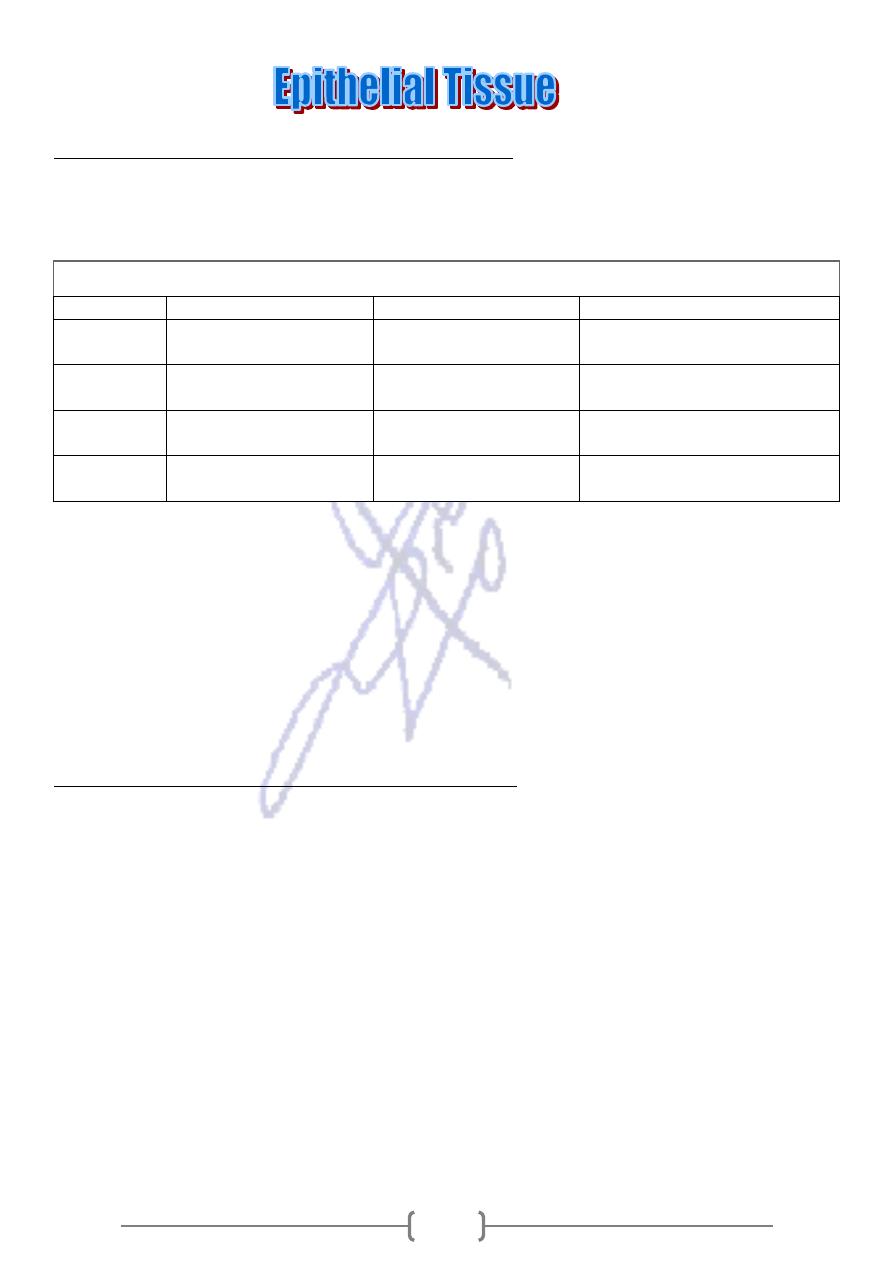
Table 4–1. Main Characteristics of the Four Basic Types of Tissues.
Tissue
Cells
Extracellular Matrix
Main Functions
Nervous
Intertwining elongated
processes
None
Transmission of nervous
impulses
Epithelial
Aggregated polyhedral
cells
Very small amount
Lining of surface or body
cavities, glandular secretion
Muscle
Elongated contractile
cells
Moderate amount
Movement
Connective
Several types of fixed
and wandering cells
Abundant amount
Support and protection
Most organs can be divided into two components: parenchyma, which is composed of the cells
responsible for the main functions typical of the organ, and stroma, which is the supporting tissue.
Except in the brain and spinal cord, the stroma is made of C.T.
The principal functions of epithelial tissues are the covering and lining of surfaces (eg, skin,
intestines), absorption (e.g., intestines), secretion (e.g., glands), sensation (e.g gustative and
olfactory neuroepithelium), & contractility (e.g., myoepithelial cells), everything that enters or
leaves the body must cross an epithelial sheet.
The Forms & Characteristics of Epithelial Cells
The forms and dimensions of epithelial cells range from high columnar to cuboidal to low
squamous cells. Epithelial cell nuclei have distinctive shapes, varying from spherical to elongated
or elliptic. The form of the nuclei of epithelial cells corresponds roughly to the cell shape; thus,
cuboidal cells have spherical nuclei and squamous cells have flattened nuclei. The long axis of the
nucleus is always parallel to the main axis of the cell.
Almost all epithelial cells, whether lining a surface or forming gland units, rest on a connective
tissue. In the case of epithelia that line the cavity of internal organs (especially the digestive,
respiratory, and urinary systems) this layer of connective tissue is often called lamina propria. The
lamina propria not only serves to support the epithelium but also provides nutrition and binds it to
neighboring structures. The area of contact between epithelium and lamina propria is increased by
irregularities in the connective tissue surface in the form of small evaginations
called papillae.
Papillae occur most frequently in epithelial tissues subject to stress, such as the skin and the tongue
.
148
Basal Lamina & Basement Membrane
extracellular material by which Most epithelial cells are separated from
a sheet of
:
basal lamina
the connective tissue.This structure is visible only with the E.M. , where it appears as a dense
layer, 20–100 nm thick, consisting of a delicate network of very fine fibrils (lamina densa)
(Figure 4–2A). In addition, basal laminae may have an electron-lucent layer on one or both sides
of the lamina densa, called lamina rara or lamina lucida. Between cell layers without
intervening connective tissue, such as in lung alveoli and in the renal glomerulus (Figure 4–1),
the basal lamina is thicker as a result of fusion of the basal laminae of each epithelial cell layer.
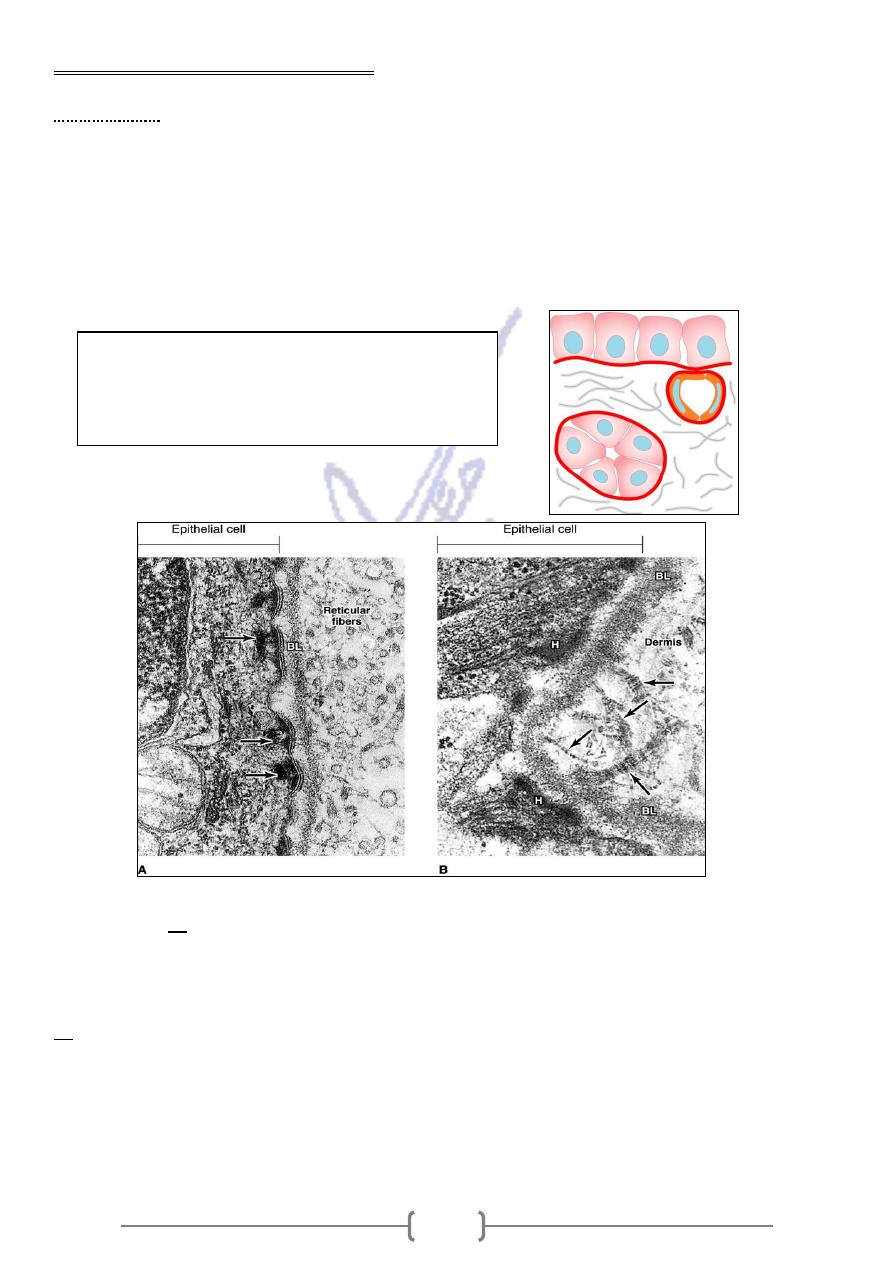
connective tissue junction showing the basal
–
Section of skin at the epithelial
A:
2.
—
Figure 4
lamina (BL) and hemidesmosomes (arrows). The basal lamina together with part of the reticular
lamina (to the right of the basal lamina in this micrograph) forms a typical basement membrane
that can be seen with the light microscope.
Section of human skin showing hemidesmosomes (H), a basal lamina (BL), and anchoring
B:
fibrils (arrows) that apparently insert into the basal lamina. The characteristic spacing of these
fibrils distinguishes them from the more common type I collagen fibrils.)
Basal laminae are found not only in epithelial tissues but also where other cell types come into
contact with connective tissue such as around muscle, adipose, and Schwann cells of nervous tissue.
Fig 4-1 :
A basal lamina always lies at the interface
between epithelial cells and connective tissue.
Two basal laminas can fuse in places where no
intervening connective tissue is present.
149
The main components of basal laminae are type IV collagen, the glycoproteins laminin and
entactin, and proteoglycans (eg, the heparan sulfate proteoglycan called perlecan). The precise
molecular composition of these components varies between and within tissues. Basal laminae are
attached to the underlying connective tissues by anchoring fibrils formed by type VII collagen
(Figure 4–2B). These components are secreted by epithelial, muscle, adipose, and Schwann cells. In
some instances, reticular fibers are closely associated with the basal lamina, forming the reticular
lamina (Figure 4–2A). Connective tissue cells produce the reticular fibers.
Basal laminae have many functions. In addition to simple structural functions supporting the cells,
they provide a barrier that limits or regulates the exchange of macromolecules between connective
tissue and cells of other tissues. The basal lamina is also able to influence cell polarity, regulate cell
proliferation and differentiation by binding with growth factors, influence cell metabolism, and
serve as pathways for cell migration. The basal lamina seems to contain the information necessary
for certain cell-to-cell interactions, such as the reinnervation of denervated muscle cells. The
presence of the basal lamina around a muscle cell is necessary for the establishment of new
neuromuscular junctions.
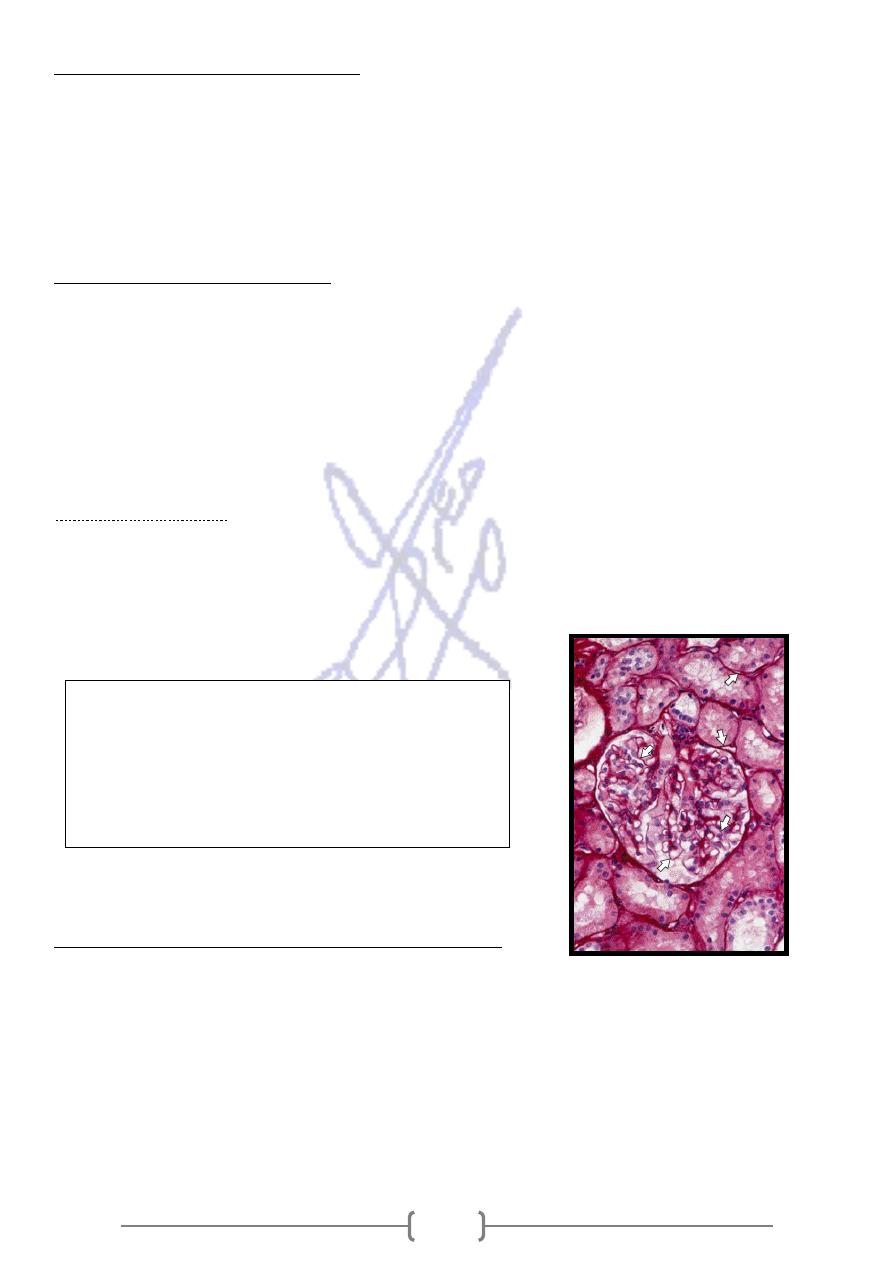
basement membrane : This term is used to specify a periodic acid–Schiff (PAS)-positive layer,
visible with the light microscope, present beneath some epithelia. Figure 4–3 shows basement
membranes in a renal glomerulus and in renal tubules. The basement membrane is usually formed
by the association of either two basal laminae (Figure 4–1) or a basal lamina and a reticular lamina
(Figure 4–2A) and is therefore thicker.
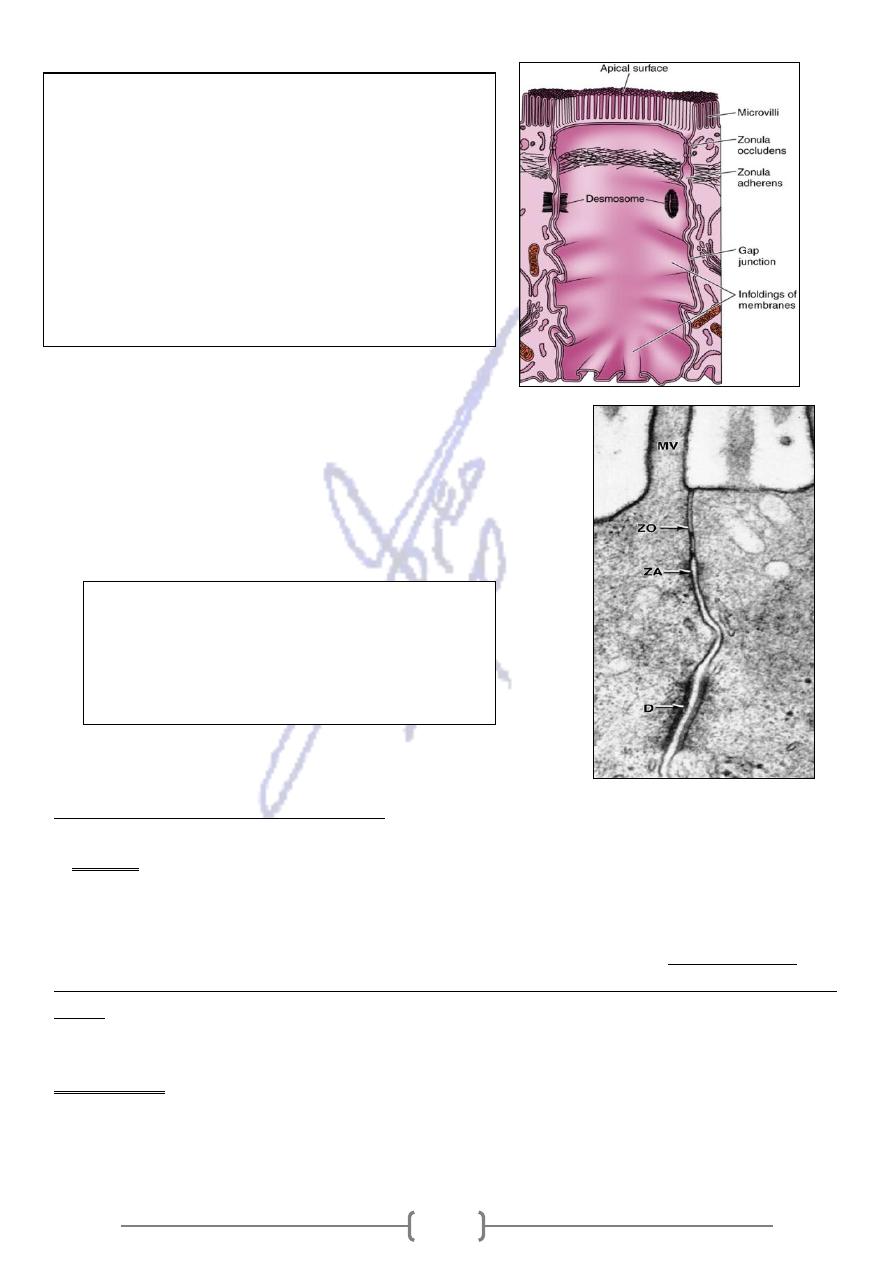
Adhesion & Intecellular junction
Intercellular
Several membrane-associated structures contribute to cohesion and communication between cells.
They are present in most tissues but are prominent in epithelia, which is why they are described in
this chapter. Epithelial cells are extremely cohesive, and relatively strong mechanical forces are
necessary to separate them. Intercellular adhesion is especially marked in epithelial tissues that are
subjected to traction and pressure (eg, the skin). Adhesion is due in part to the binding action of a
family of transmembrane glycoproteins called cadherins. Cadherins lose their adhesive properties in
the absence of Ca
2+
. Interdigitations between folds of membranes of neighbor cells also help to
increase intercellular adhesion (Figure 4-4)
Figure 4-3. Kidney section showing type IV collagen
of the glomerular and tubular basement membranes
(arrows). In the glomeruli the basement membrane,
besides having a supporting function, has an
important role as a filter. Picrosirius– hematoxylin
(PSH) stain. Medium magnification.
151
1-Tight junction or Zonnula occludens
2- Zonula adherens
3- Gap or communicating junction
4- Desmosome or macula adherens
5- Hemidesmosomes (half desmosome)
the cell surface
Specialization of
Microvili
1.
cytoplasm projections in absorptive cells lining epithelium of small intestine & cell of the
proximal renal tubule.
The complex of
In these absorptive cells the glycocalyx is thicker than it is in most other cells.
en with the light microscope and is called the brush, or striated,
microvilli and glycocalyx may be se
linked to each other and to
-
. Within the microvilli are clusters of actin filaments that are cross
border
the surrounding plasma membrane by several other proteins.
2. Stereocilia
Stereocilia are long, nonmotile extensions of cells of the epididymis and ductus
deferens that are actually long and branched microvilli and should not be confused with true cilia.
Stereocilia increase the cell surface area, facilitating the movement of molecules into and out of the
cell.
Figur4-4. The main structures that participate in
cohesion among epithelial cells. The drawing shows 3
cells from the intestinal epithelium. The cell in the
middle was emptied of its contents to show the inner
surface of its membrane. The zonula occludens and
zonula adherens form a continuous ribbon around the
cell apex, whereas the desmosomes and gap junctions
make spotlike plaques. Multiple ridges form the
zonula occludens, where the outer laminae of apposed
membranes fuse.
Figure 4—5. Electron micrograph of a section of
epithelial cells in the large intestine showing a
junctional complex with its zonula occludens
(ZO), zonula adherens (ZA), and desmosome
(D). Also shown is a microvillus (MV). x80,000.
151
Cilia and Flagella
3.
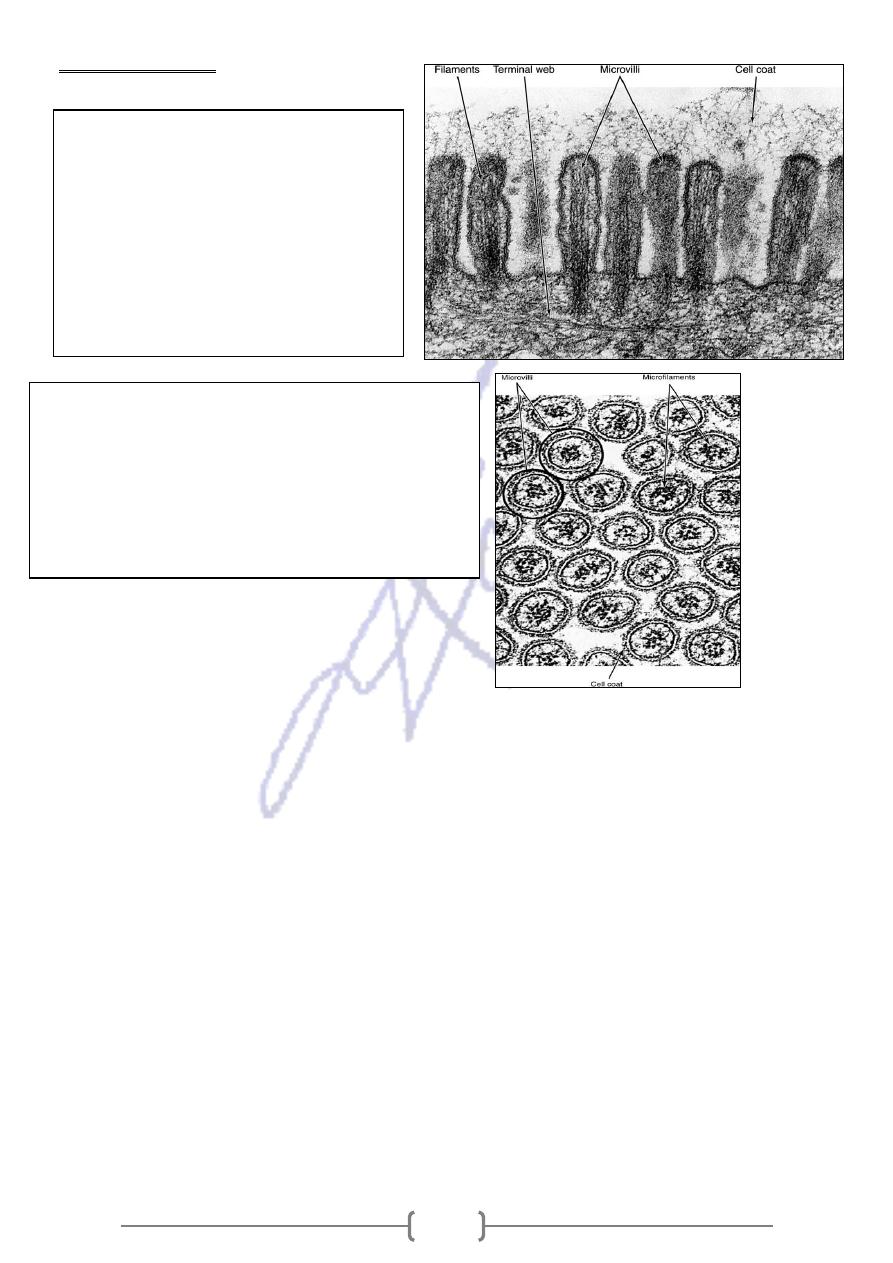
Figure 4—8. Apical region of an
intestinal epithelial cell seen with
transmission electron microscopy. The
terminal web is a network that contains
mainly actin filaments. Filaments that
constitute the core of the microvilli are
clearly seen. An extracellular cell coat
(glycocalyx) is bound to the
plasmalemma of the microvilli. x45,000.
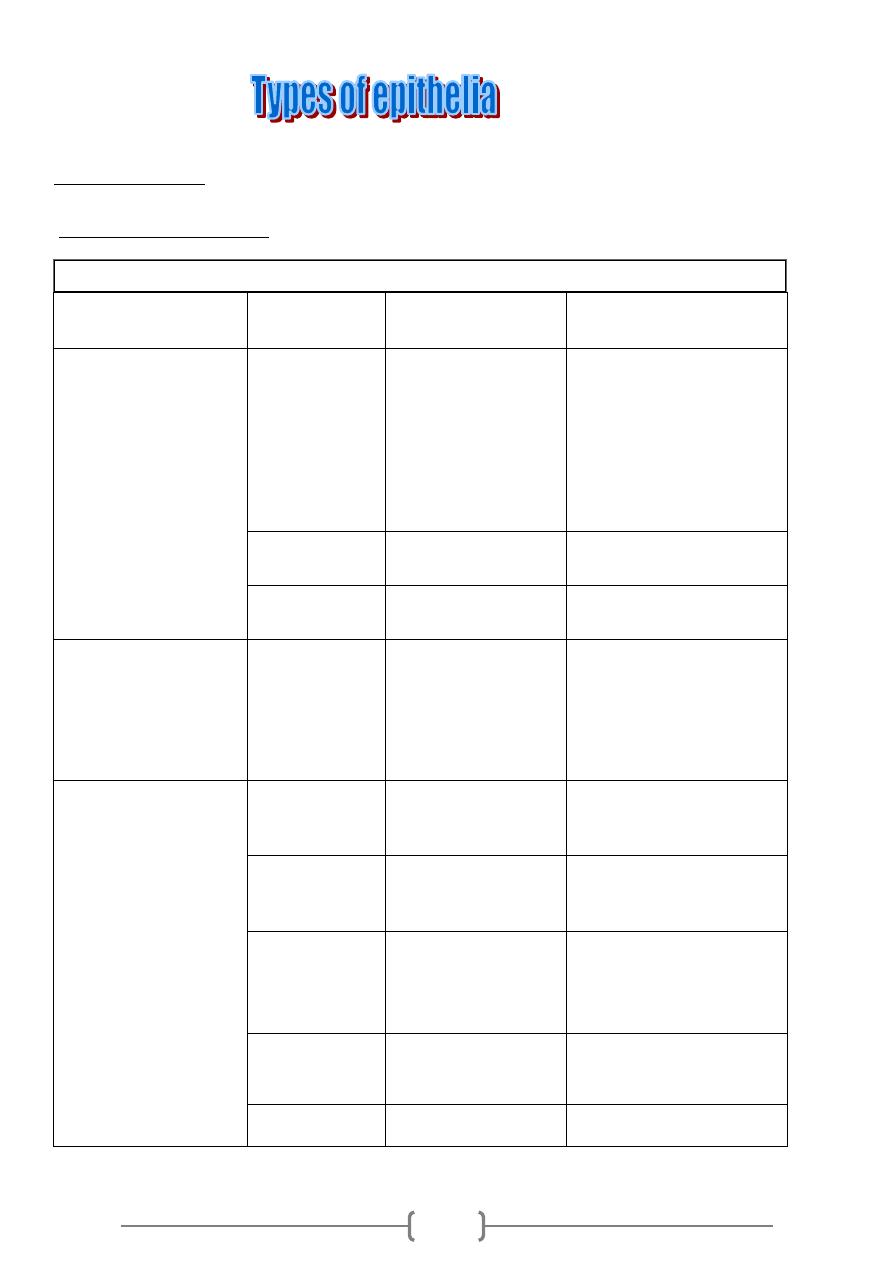
Figure 4—9. Electron micrograph of a section from
the apical region of a cell from the intestinal lining
showing cross-sectioned microvilli. In their interiors,
note the microfilaments in a cross section. The
surrounding unit membrane can be clearly discerned
and is covered by a layer of glycocalyx, or cell coat.
x100,000.
152
Glandular ep.
-
2
Covering ep.
-
1
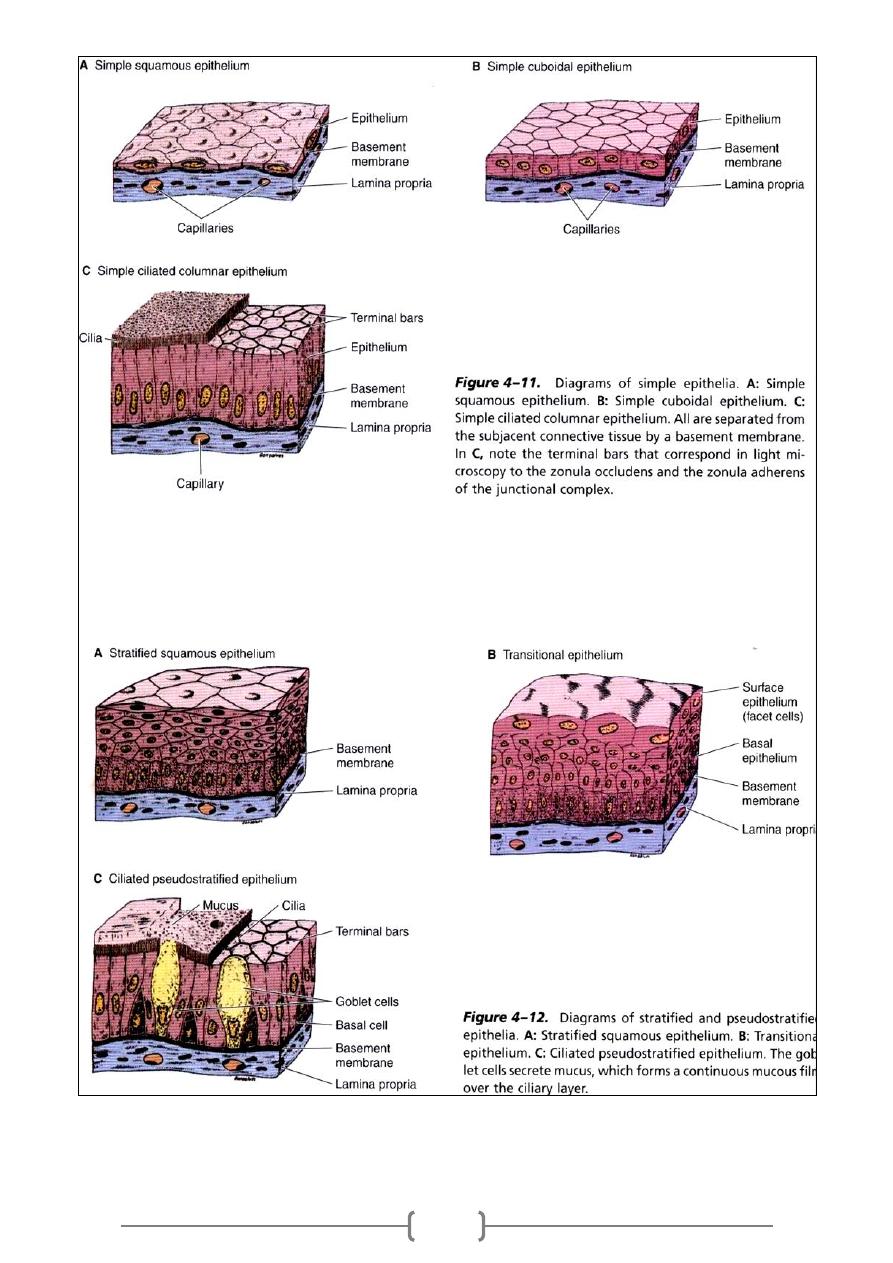
Types of epithelia
Covering epithelia
-
1
Table 4–2. Common types of covering epithelia in the human body.
Number of Cell
Layers
Cell Form
Examples of
Distribution
Main Function
Simple (one layer)
Squamous
Lining of vessels
(endothelium).
Serous lining of
cavities; pericardium,
pleura, peritoneum
(mesothelium).
Facilitates the movement
of the viscera
(mesothelium), active
transport by pinocytosis
(mesothelium and
endothelium), secretion of
biologically active
molecules (mesothelium).
Cuboidal
Covering the ovary,
thyroid.
Covering, secretion.
Columnar
Lining of intestine,
gallbladder.
Protection, lubrication,
absorption, secretion.
Pseudostratified (layers
of cells with nuclei at
different levels; not all
cells reach surface but
all adhere to basal
lamina)
Lining of trachea,
bronchi, nasal cavity.
Protection, secretion; cilia-
mediated transport of
particles trapped in mucus
out of the air passages.
Stratified (two or more
layers)
Squamous
keratinized
(dry)
Epidermis.
Protection; prevents water
loss.
Squamous
nonkeratinized
(moist)
Mouth, esophagus,
larynx, vagina, anal
canal.
Protection, secretion;
prevents water loss.
Cuboidal
Sweat glands,
developing ovarian
follicles.
Protection, secretion.
Transitional
Bladder, ureters,
renal calyces.
Protection, distensibility.
Columnar
Conjunctiva.
Protection.
153
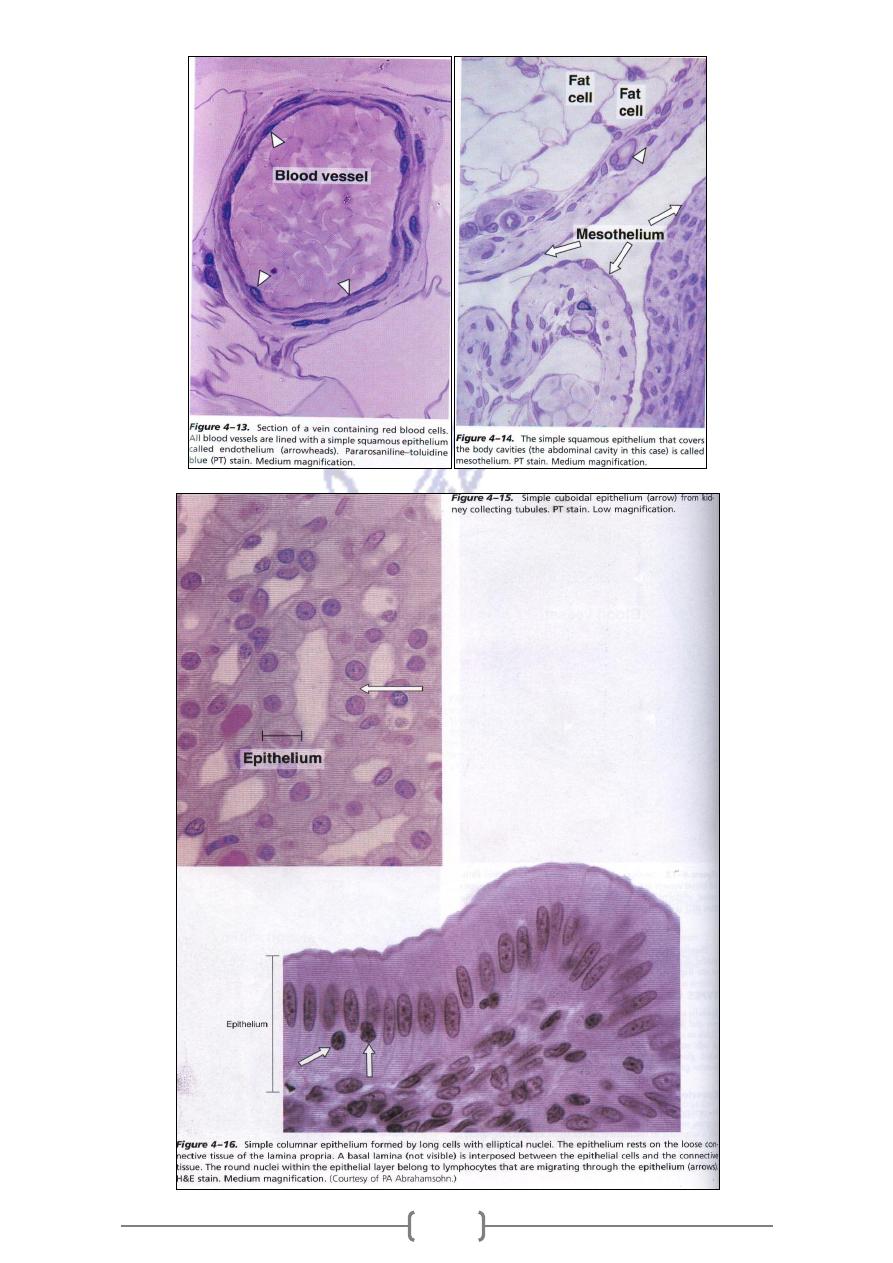
154
155
The two other types of epithelium
Epithelial origin with specialized sensory function ( e.g. Cell of taste buds
cell:
Neuroepithelial
-
1
& cell of olfactory mucosa)
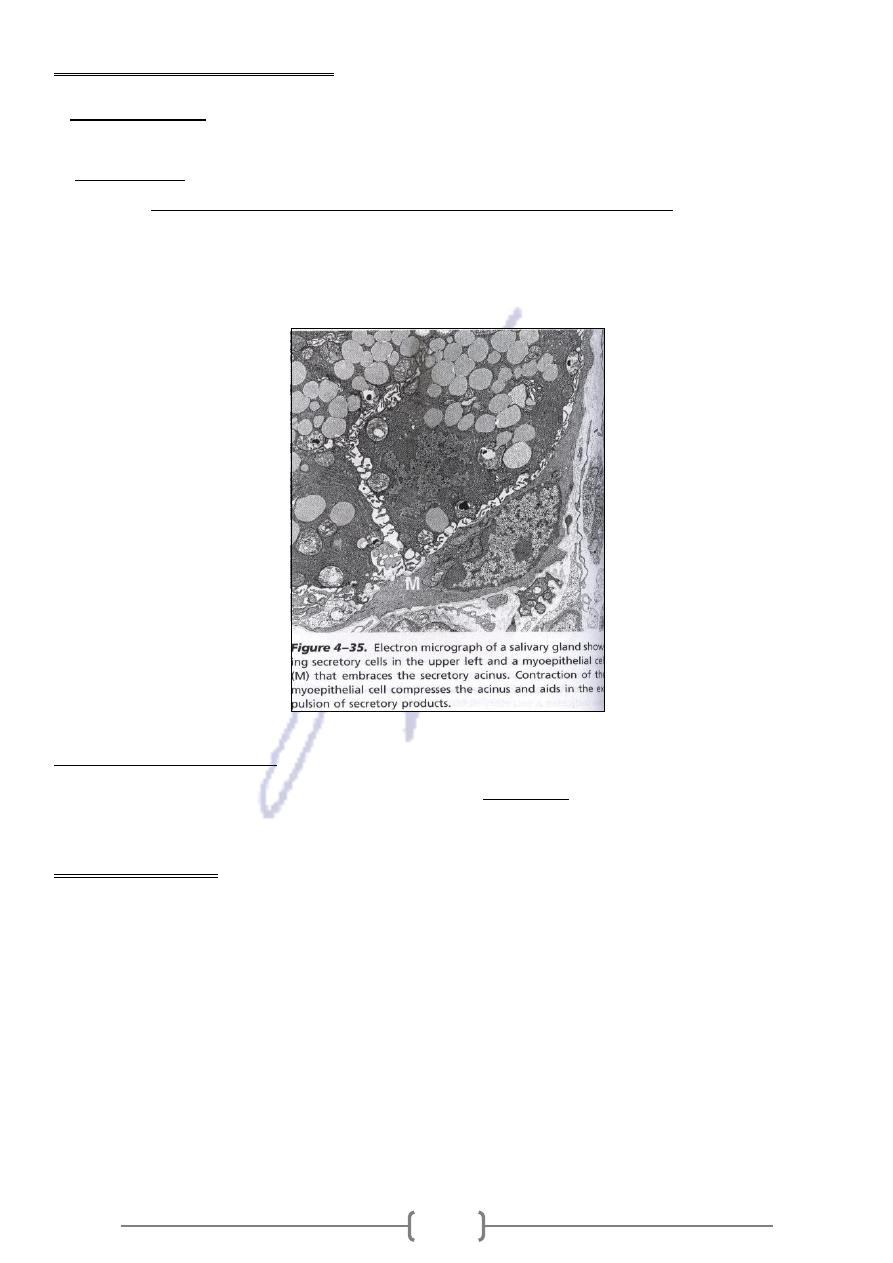
sin & actins filament specialized for
Are branched that contain myo
cells:
Myoepithelial
-
2
They are
.
mainly of secretory units of the mammary , sweat & salivary gland
contraction,
located between the basal lamina &the basal surface of secretory or ductal cells .They have
intermediate filaments .They embrace gland acini to help propel secretory products toward the
exterior.
2. Glandular epithelia
which is molecules stored in
secretion ,
Formed by cell specialized to produce
Glandular ep.:
small membrane – bound vesicles (secretory granules)
Glandular ep. Cell
1- Synthesize proteins
2- Store
3- Secret a- protein (pancreas) b- Lipid ( adrenal , sebaceous gland )
c- Carbohydrates & proteins (salivary glands )
The mammary glands secret all a , b , & c
Sweat glands ; have low synthesizing activity
156
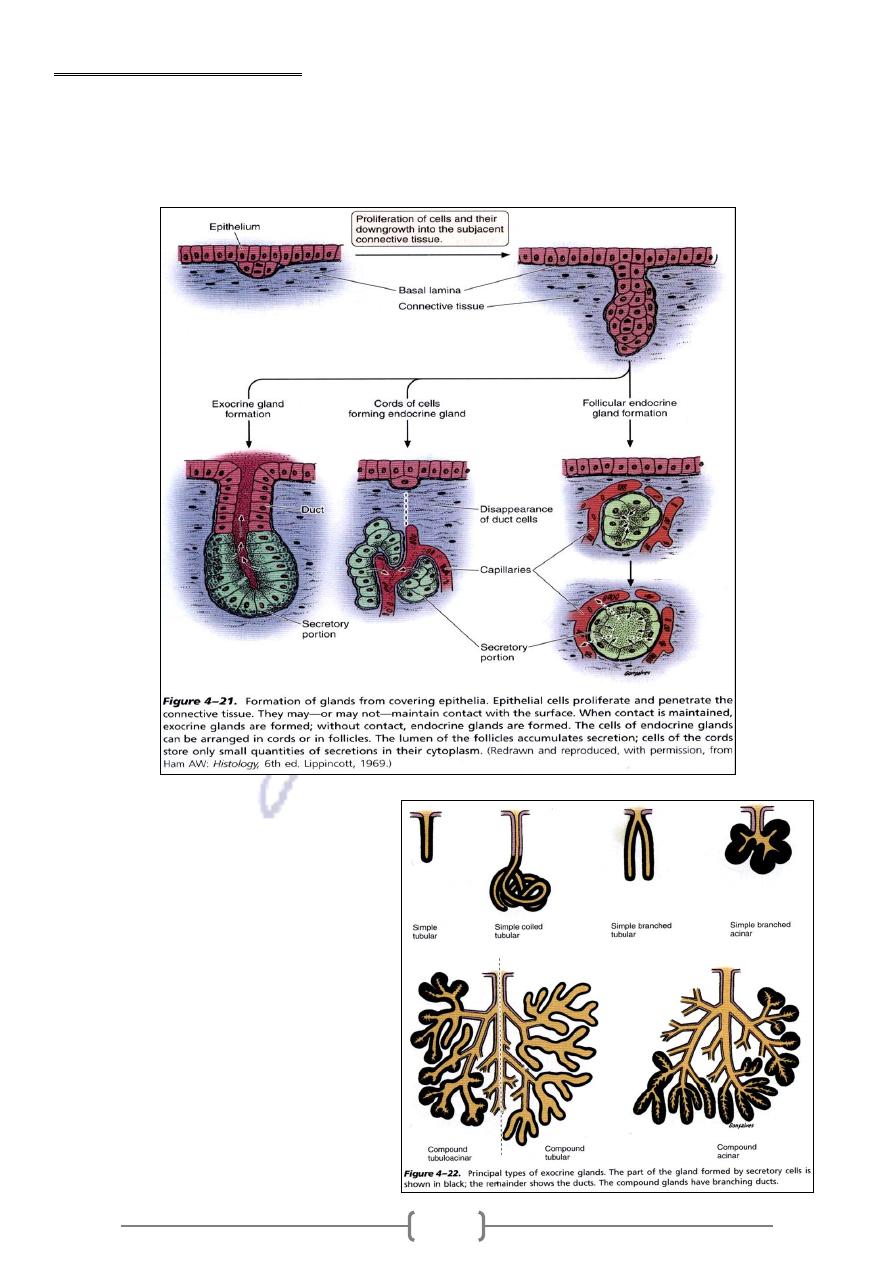
Types of Glandular Epithelia
According to number of cell
1- Unicellular glands : Goblet cell of lining of small intestin
2- Multicellular glands a- Exocrine b- Endocrine
Exocrine glands have a secretory
portion & Duct
157
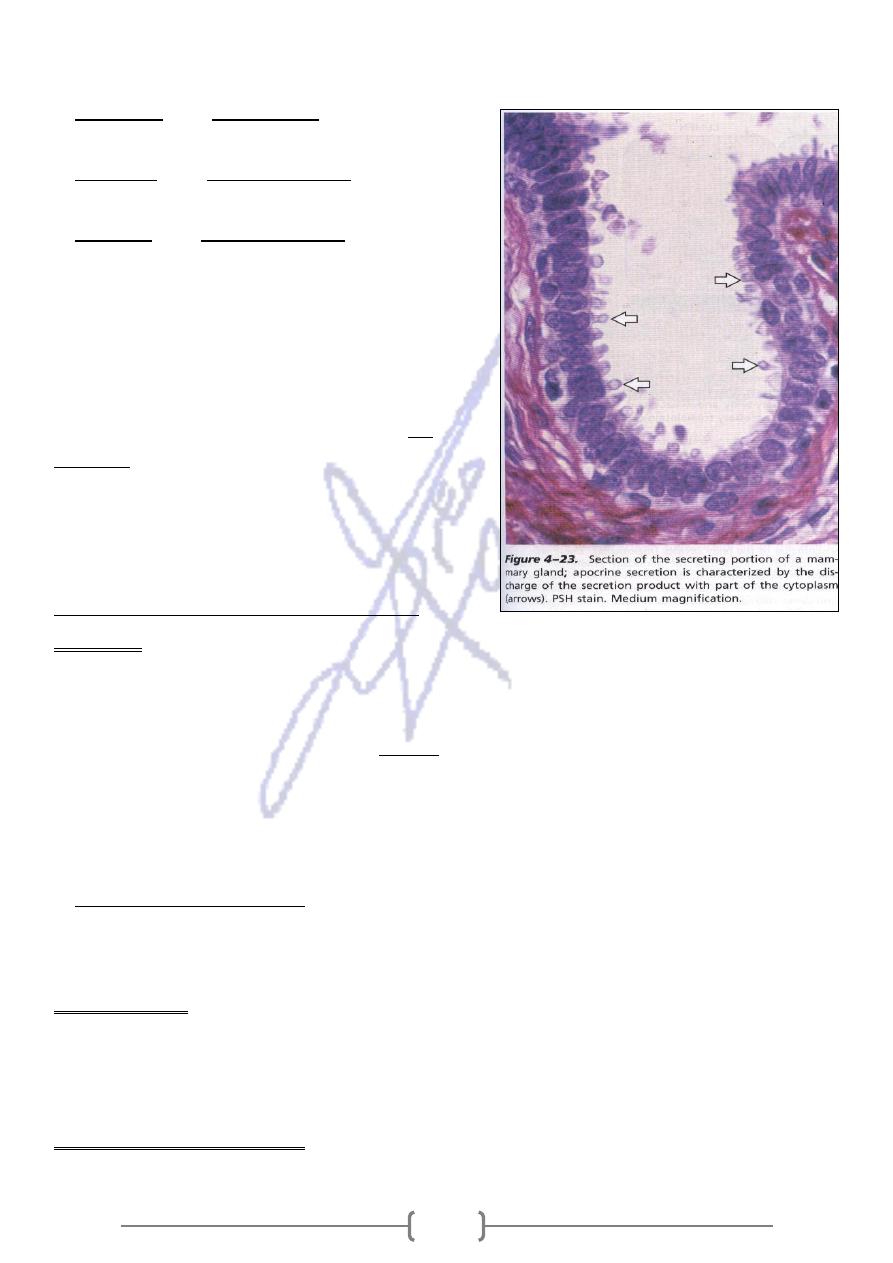
According to how the secretory products leave the cell
,
) by Exocytosis
the pancreas
( e.g.
Merocrine
-
1
no loss of cellular material
) the
sebaceous glands
( e.g.
Holocrine
-
2
product of secretion is shed with the whole cell
) the
mammary glands
(e.g.
Apocrine
-
3
secretory product is discharged to gather with
parts of apical cytoplasm's.
Some organs have both endocrine and exocrine
functions _e.g. , in the liver.
In other organs, some cells are specialized in
in
exocrine secretion and others are endocrine ;
, the acinar cells secret digestive
pancreas
enzymes into the intestinal lumen , whereas
the islet cells secrete insulin and glucagon into
bloodstream.
General Biology of Epithelial Tissues
Polarity
-
1
In many types of epithelial cells the distribution of organelles and membrane proteins is
different when comparing the basal and apical poles of the cell. This differential and stable
.
polarity
organization of cell components is called
Because blood vessels do not normally penetrate an epithelium, all nutrients must pass out of the
capillaries in the underlying lamina propria. These nutrients diffuse across the basal lamina and are
taken up through the basal and lateral surfaces (basolateral surface) of the cell, usually by an
energy-dependent process.
membrane
the apical cell membrane may contain, as integral
In absorptive epithelial cells,
proteins, enzymes such as disaccharidases and peptidases, which complete the digestion of
molecules to be absorbed.
They are the sites where epithelial tissues receive a rich supply of sensory
Innervations:
-
2
nerve ending from nerve plexuses in the lamina propria ( e.g.. Sensitivity of cornea , the epi.
Covering the anterior surface of eye , is due to the great of sensory nerve fibers that ramify
between corneal epithelial cells
They are renewed continuously by mitotic activity . the renewal
:
Renewal of Epithelial Cells
-
3
rate can be fast in tissues (eg,.the intestinal ep.) or slow as in liver & pancreas . In stratified &
158
pseudo stratified ep. , mitosis occurs within the germinal layer ,closest to the basal lamina ,
stem cells
which contains the
It is a reversible process which lead one type of ep. Tissue undergo
Meta plasia :
-
4
transformation into another type under abnormal conditions such as:
A. In heavy cigarette smoker ,the ciliated pseudo stratified ep. Lining the bronchi can be
transformed into stratified squamous epi.
B- In individuals with chronic vitamin A deficiency , epi. T. of bronchi & urinary bladder
,replaced by stratified squamous epithelium
Control of glandular activity
Both of Neural & Endocrine control the activity of the glands Ex.
1.
Exocrine secretion of pancreas depend on stimulation by the hormones
C
holecystokinin
2. Salivary glands are principally under neural control .Both controls occur through the
action of ( Chemical messenger )
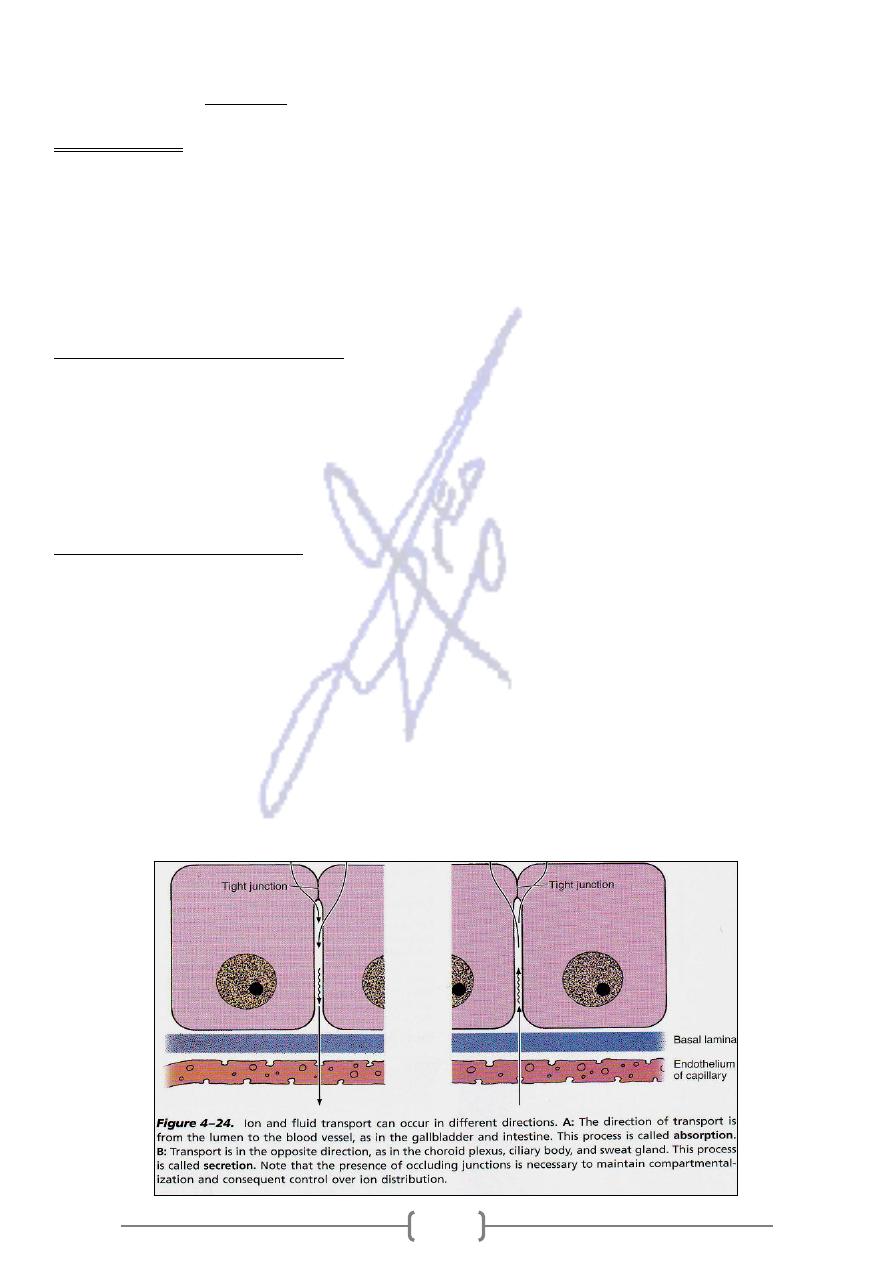
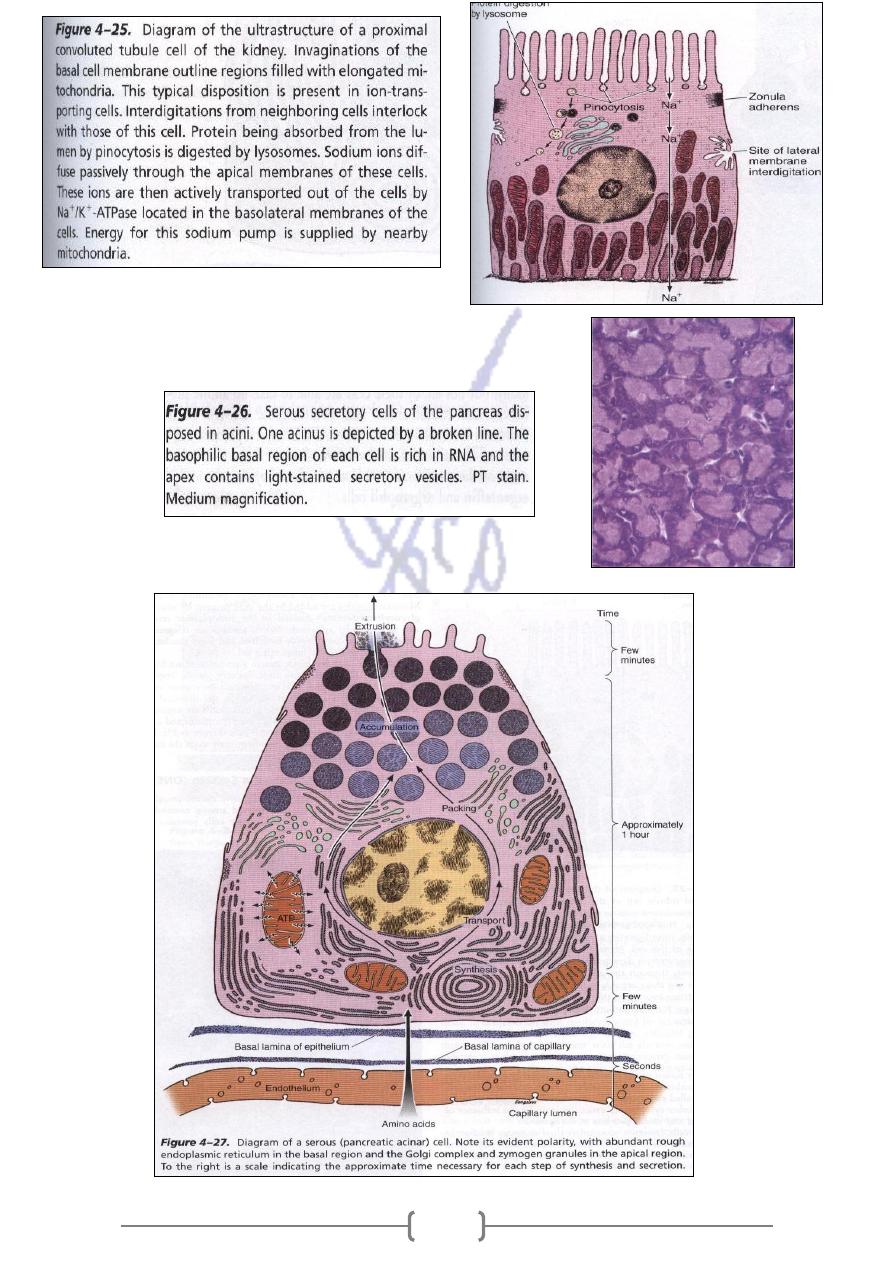
Cell that transport ions
All cells have the ability to transport ions against a concentration & electrical –potential
gradient through ACTIVE TRANSPORT
In mammals , sodium concentration in extracellular fluid is 140 mm/ L. whereas the
intracellular concentration is 5-15 m mol / L The cell uses the energy stored in ATP to actively
extrude Na by mean of Mg activated Na / K –ATP ( SODIUM PUMP), thereby maintaining the
required low intracellular sodium concentration .
Some cells transfer ions & fluid across epithelium ,from apex to its base or from its base to
its apex in (Tran cellular transport) .which involved absorption & secretion.
159
Serous cells Ex. Acinar cells of Pancreas & Parotid salivary
glands
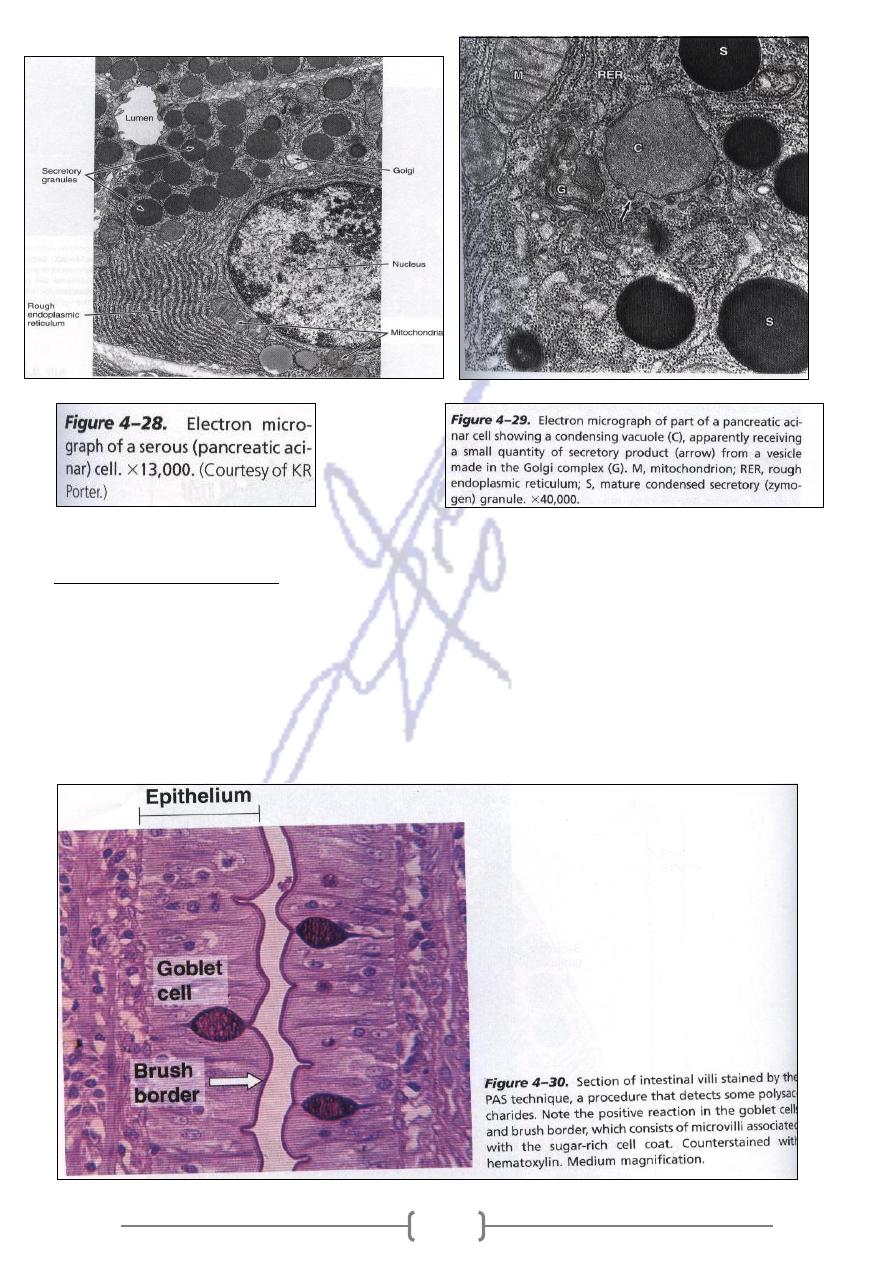
161
secreting cells
-
Mucus
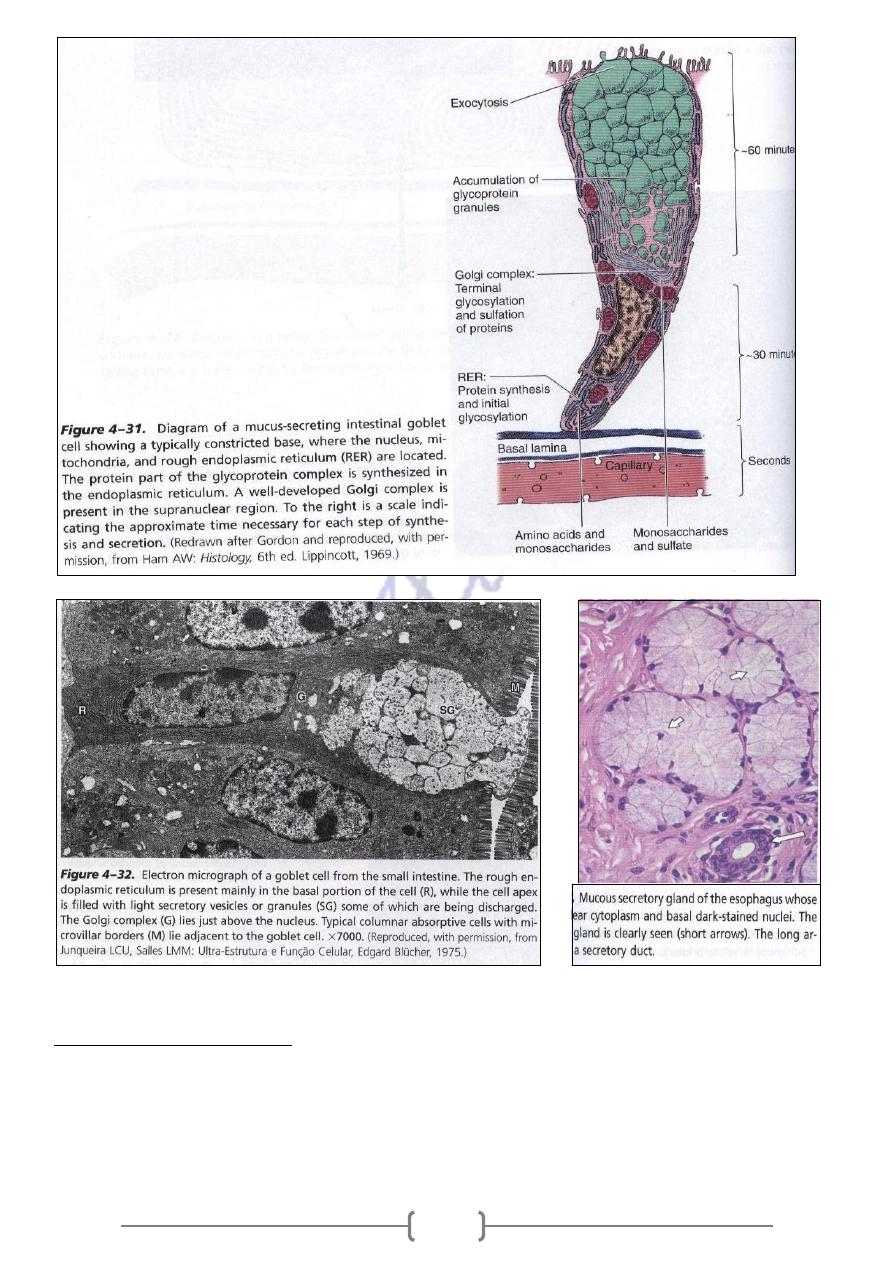
The most thoroughly studied mucus- secreting cell is goblet cell of intestines .the cell has
glycoprotein called mucins .The proteins are synthesized in the cell base where most R.E.R. is
located . When mucins are released from the cells , they become highly hydrated and form mucus
,viscous, elastic, protective lubricating gel. Other cells that synthesize mucins are found in salivary
glands, respiratory tract .Many of these mucous cells are organized as tubules .
161
secreting cells
–
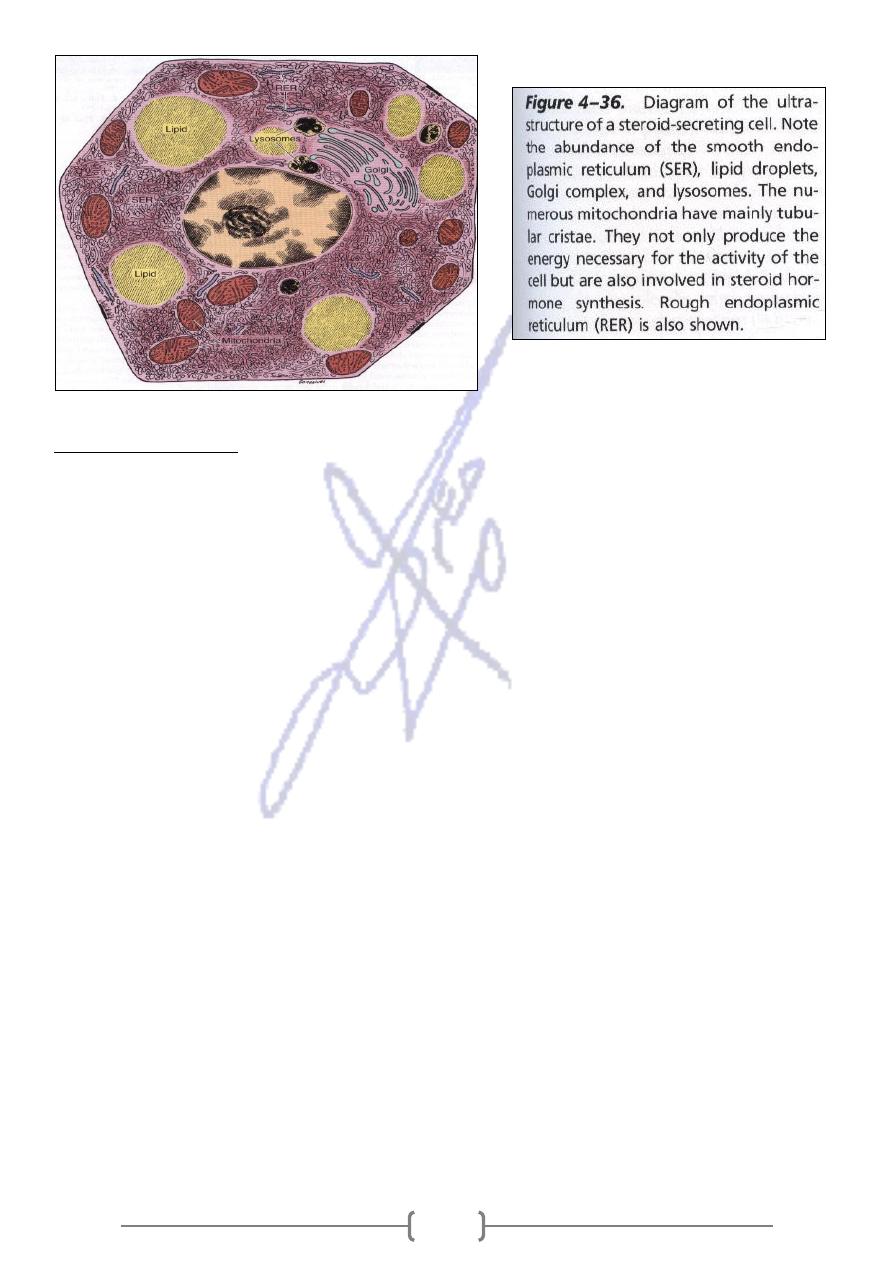
Steroid
The cells that secrete steroid are found in( testes, ovaries, adrenals They are endocrine cells
specialized for synthesizing and secreting steroids with hormonal activity ,and have following
characteristics
162
Medical application
Both benign and malignant tumors can arise from most types of epithelial cells. A carcinoma (Gr.
karkinos, cancer, + oma, tumor) is a malignant tumor of epithelial cell origin. Malignant tumors
derived from glandular epithelial tissue are usually called adenocarcinomas (Gr. adenos, gland, +
karkinos); these are by far the most common tumors in adults. In children up to age 10 years, most
tumors develop (in decreasing order) from hematopoietic organs, nerve tissues, connective tissues,
and epithelial tissues. This proportion gradually changes, and after age 45 years,
