Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
Burns
Definition
A burn injury is a coagulative type of necrosis of varying
depth of skin and deeper tissues.
Pathophysiology
Causes of burn shock or burn reaction
1. Dilatation of small vessels which leads to release of
various inflammatory mediators.
2. Increased permeability of the injured capillaries.
causing edema. This exudative fluid collects in blisters.
3. The extensive loss of fluid is an important factor in
producing the burns shock. The volume loss is greatest
in the first 8 hours.
4. Neurogenic factor, caused by severe pain.
5. Psychogenic resulting from the horror of burning.
6. Release of toxic metabolic products from the burnt
area.
7. Tissue anoxia and metabolic acidosis secondary to the
fall of blood pressure.
8. Sepsis — Eschar of burn wound acts as a good culture
media for bacterial growth.
Both gram positive and gram negative bacteria are found.
Common organisms are:
Staphylococcus aureus, Psuedomonas aeruginosa, Proteus, E.
coli.
In the postburn period uncontrolled infection leads to the
condition known as septic or endotoxic shock.
Inhalational injury
Inhalational injury is caused by the minute particles within
thick smoke and often gives rise to a bacterial pneumonia.
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
Carbon Monoxide Poisoning CO injury is the most
commonly recognized form of inhalation injury and the
most common cause of death in inhalation injury.
The affinity of CO for hemoglobin is approximately 200–250
times more than that of oxygen, which decreases the levels of
normal oxygenated hemoglobin and can quickly lead to
anoxia and death.
Clinical signs and symptoms of CO toxicity correlate with
arterial carboxyhemoglobin levels, which can be used to
quickly and precisely determine the degree of CO
intoxication.
treated with 100% inhaled oxygen, which rapidly accelerates
the dissociation of CO from hemoglobin.
Carboxyhemoglobin level correlations with patient
symptoms
Carboxyhemoglobin level (%) Symptoms
<10
None
15 – 25
Nausea, headache
30 – 40
Confusion, stupor, weakness
40 - 60
Coma
>60
Death
Classification of burns
According to Agent
i.
Thermal burn (90%) —
Burns caused by dry heat like flames, fire, bomb
injuries.
Scalds are due to hot liquids.
ii. Others (10%)
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
a. Chemical burn — Due to any strong acid or alkali.
b. Electrical burn— May be caused by high voltage or low
voltage current.
c. Radiation burn— Due to X-rays or radium.
According to Depth
Burn wounds are commonly classified as
1.
Superficial (first degree),
• It involves only the epidermis.
• Erythematous and painful such as a sunburn.
• heal within 3 to 4 days, without scarring.
• treatment is a soothing moisturizing lotion.
2.
Partial thickness (second degree),
Partial-thickness burns are then subclassified as either;
a. Superficial partial thickness
-
Epidermis and superficial dermis up to the
reticular layer.
-
Blistering is their hallmark
-
pink, moist, and painful
-
Pinprick sensation is normal
-
capillary return is clearly visible when blanched
-
heal within 2 to 3 weeks, without scarring or
functional impairment.
b. Deep partial thickness burns
-
extend through the epidermis and into the
papillary dermis.
-
mottled pink-and-white, dry
-
does not blanch with pressure
-
variably painful
-
heal in 3 to 8 weeks with severe scarring
contraction, and loss of function.
3.
Full thickness (third degree)

Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
-
extend through the entire dermis and into the
subcutaneous tissue.
-
white or black, dry,
-
painless
-
do not blanch with pressure.
-
heal only by contraction.
So all full-thickness burns, unless they are quite
small be treated with excision and grafting.
4.
fourth-degree burns,
-
It extends beyond the skin into deeper tissues like
the muscles, bone, etc.
Burn Zones
Jackson described three zones of tissue injury following
burn injury.
1.
zone of coagulation
-
center of the wound.
-
coagulated or necrotic tissue.
2.
zone of stasis
-
vasoconstriction and resultant ischemia.
3.
zone of hyperemia
-
vasodilatation.
Estimation of the extent of burn or burn size
I.
Rule of nines also called the Rule of Wallace
Patients own hand represents 1 percent of his total body
surface area (TBSA).
The calculations are:
i.
In adults—
Burns of head and neck 9 percent,
each superior extremity 9 percent,
each inferior extremity 9 percent× 2,
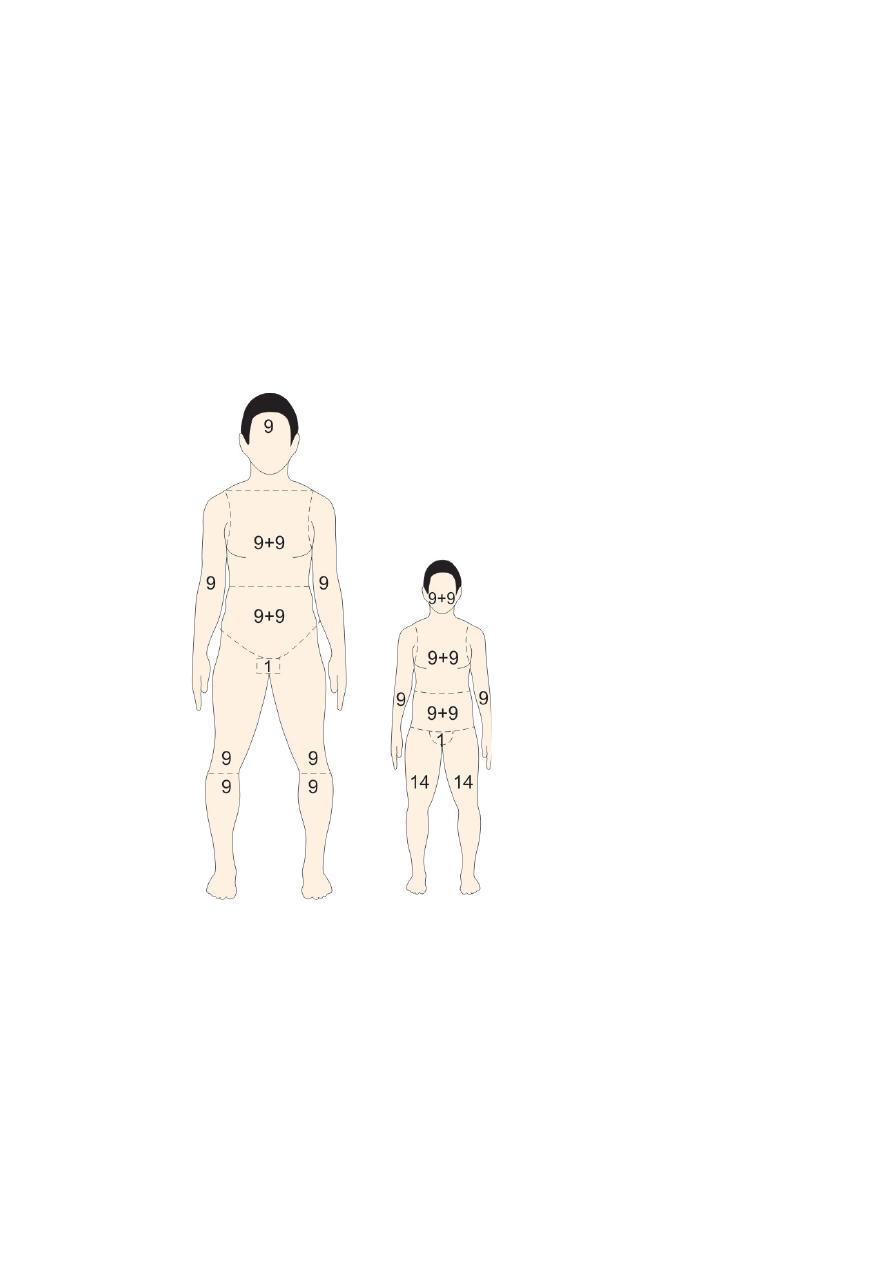
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
Front of trunk 9 percent × 2,
Back of trunk 9 percent × 2,
and genitalia 1 percent.
ii.
In children —
Each inferior extremity 14 percent,
each superior extremity 9 percent,
front and back trunk each 18 percent,
Head and neck 9 percent ×2.
v
Superficial or first-degree burns should not be included
when calculating the percent of TBSA.
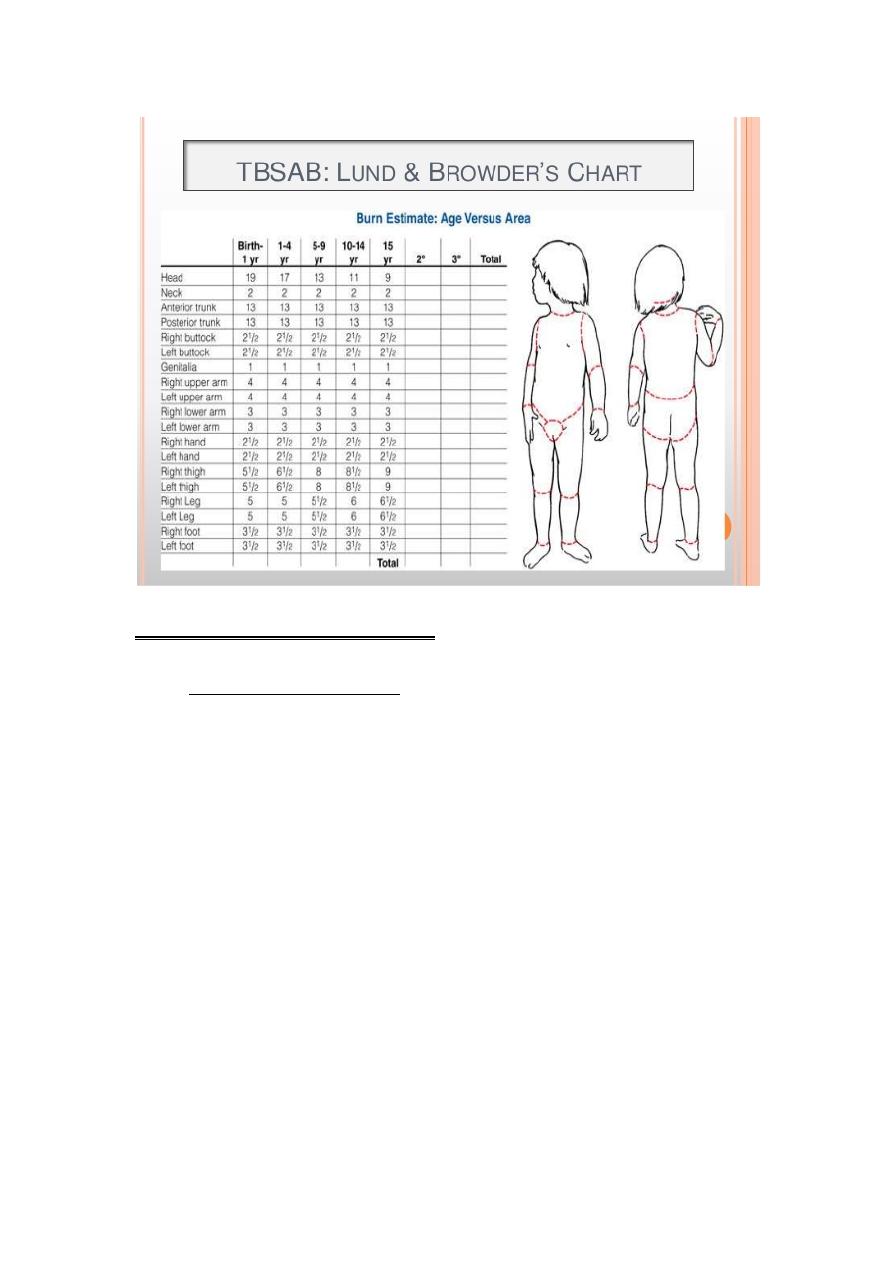
II. The Lund and Browder chart is useful in larger
burns
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
Complications of burn injury
1. Early Complications
A. General
o Systemic inflammatory response syndrome
(SIRS) along with presence of infection increases
morbidity and mortality. It may also lead to
multiorgan dysfunction syndrome (MODS).
o On a cellular level, complement causes release of
large quantities of free radicals and proteases.
These can in turn cause further damage to the
tissues.
o Organ changes:
a. Gastrointestinal tract —
1. Curling’s ulcer of the stomach and duodenum.
Such ulcers are prone to cause gastrointestinal bleeding.
2. ischaemia to the gut mucosa.
3. Reduction in gut motility

Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
4. Diminished absorption of food.
5. Translocation of gut bacteria.
6. Gut mucosal swelling, gastric stasis and peritoneal
oedema can also cause abdominal compartment
syndrome, which splints the diaphragm and increases
the airway pressures needed for respiration.
7. Acute pancreatitis in about 30 percent cases of
extensive burns.
b. Respiratory tract—Pneumonia, Pulmonary edema, ARDS
(Adult Respiratory Distress Syndrome).
c. Kidney — low blood perfusion leads to renal tubular
damage and acute renal failure, hematuria.
d. Anemia, bone marrow depression.
e. Toxemia, septicemia, pyemia.
f. Psychosis, loss of morale.
g. Liver — liver necrosis.
h. Adrenals — slightly enlarged and deeply congested.
In severe cases, there may be bilateral necrosis of adrenal
cortex.
i. Multiple endocrine aberrations –
elevated glucagon, cortisol and catecholamines.
Insulin and T3 hormone levels are depressed.
j. Neurogenic changes -- delirium and disorientation are seen
due to less blood flow to the brain and electrolyte imbalance.
k. Immunologic impairment — Cell mediated immunity is
significantly reduced in large burns, leaving the victims
more susceptible to bacterial and fungal
infections.
l. peripheral circulation -- A circumferential full-thickness
burn to a limb acts as a tourniquet as the limb swells. If
untreated, this will progress to limb-threatening ischemia.
B. Local complications — Eschar formation, gangrene.
Late Complications
a. Keloids and hypertrophic scar.
b. Contractures and deformities.
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
c. Marjolin’s ulcer, a slowly growing squamous cell
carcinoma arising from scars.
Treatment
Pre-hospital care
• Ensure rescuer safety.
• Stop the burning process.
• Check for other injuries.
• Cool the burn wound. and hypothermia must be avoided.
• Give oxygen.
• Elevate. - Elevation of burned limbs will reduce swelling
and discomfort.
Guidelines for Referral to a Burn Center (Indications of
admission)
1.
Partial-thickness burns greater than 10% TBSA.
2.
Burns involving the face, hands, feet, genitalia,
perineum, or major joints.
3.
Third-degree burns in any age group.
4.
Electrical burns, including lightning injury.
5.
Chemical burns.
6.
Inhalation injury.
7.
Burn injury in patients with complicated pre-
existing medical disorders
8.
Patients with burns and concomitant trauma.
9.
Burned children in hospitals without qualified
personnel for the care of children.
10. Burn injury in patients who will require special
social, emotional, or rehabilitative intervention.
11. Any suspicion of non-accidental injury (abuse or self
induced)
Hospital care
The principles of managing an acute burn injury are the
same as in any acute trauma case according to advanced
trauma life support (ATLS) guidelines:
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
A: Airway control and cervical spine stabilization.
B: Breathing and ventilation.
C: Circulation.
D: Disability – neurological status.
E: Exposure with environmental control.
F: Fluid resuscitation.
Airway
secure the airway with an oral guard or endotracheal tube
if needed or even cricothyroidotomy.
Warning signs of burns to the respiratory system
ý
Burns around the face and neck
ý
A history of being trapped in a burning room
ý
Change in voice (hoarseness)
ý
wheezing, or stridor;
ý
subjective dyspnea is a particularly concerning
symptom, and should trigger prompt elective
endotracheal intubation.
ý
blisters on the hard palate,
ý
burned nasal mucosa
ý
loss of all the hair in the nose
ý
deep burns around the mouth and in the neck
Breathing
A. Inhalational injury
The clinical features are
-
progressive increase in respiratory effort and rate
-
rising pulse
-
anxiety and confusion
-
decreasing oxygen saturation.
Treatment: Physiotherapy, nebulisers and warm humidified
oxygen.
B. Mechanical block to breathing
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
Circulation
Fluid resuscitation:
• Venous access is best obtained with IV catheters or
venflons (canulas) using veins in unburned skin.
• Lactated Ringer’s solution without dextrose is the fluid of
choice except in children younger than 2 years; who should
receive 5 percent dextrose and Ringer lactate.
• The amount of fluid necessary to maintain adequate
perfusion is easily monitored in burned patients with normal
renal functions by following the volume of urine output,
which should be at least 0.5 ml/kg/hour in adults and
1ml/Kg/hour in children.
Burn Resuscitation Formulas
§
Isotonic crystalloid formulas
Parkland formula:
Lactated Ringer's
[ 4 x body weight (kg) x burned TBSA ]
1 /2 volume during first 8 h postinjury;
1 /2 during next 16 h postinjury
Modified Brooke formula
§
Hypertonic formulas
§
Colloid formulas
Complications of fluid administration
1. compartment syndrome involving the abdomen or
extremities
2. pulmonary edema, and pleural effusion.
Additional aspects of treating the burned patient
1.Tetanus prophylaxis.
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
2. Never administer prophylactic antibiotics, it may cause
gram negative or fungal infection.
3. Intravenous H2 blocker is given as a prophylactic
measure against stress ulcerations.
4. Dressings must allow full range of motion.
5. Physical therapy is an essential component of burn
management.
Sedation and analgesia:
Intravenous opiates.
Powerful short acting analgesia should be administered
before dressing changes.
Deep Vein Thrombosis Prophylaxis
subcutaneous unfractionated heparin, 5,000 U twice a day.
Transfusion
any burn > 40 % should have blood transfusion.
Local Treatment of Burn Wound
a. Escharotomy and fasciotomy: When full thickness burn
wounds encompass the circumference of an extremity,
peripheral circulation to the limb can be compromised.
Clinical signs are cyanosis, impaired capillary refill and
deep muscle pain.
Arterial flow can be assessed by determination of doppler
signals.
• Compromised extremities require escharotomies which are
release incisions made with a scalpel or electrocautery unit
at the bedside over the lateral and medial aspects of the
extremity.
Increased muscle compartment pressures may necessitate
fasciotomies.
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
b. Burn wound excision: Burn wounds of full thickness and
deep partial thickness should be excised as soon as possible
with a scalpel.
The excision should be restricted to less than 20 percent of
total body surface area.
The advantages are
-
reduced infection rate,
-
less hospital stay, and
-
reduced stress response to the burn in burns over
40 percent.
c. Wound closure:
By closure wound desiccation and evaporative losses are
minimized.
The pain and protein loss get reduced and exposed vessels,
tendons and nerves are protected.
This can be done by various methods:
i. Autografts are preferred.
ii. In the absence of autografts, other alternatives are
cadaveric cutaneous allograft, cutaneous xenograft,
synthetic membranes like Biobrane and culture derived
epidermal sheets.
Options for topical treatment of deep burns
■ 1% silver sulphadiazine cream
■ 0.5% silver nitrate solution
■ Mafenide acetate cream
Nutrition
patients with major thermal injury experience
hypermetabolism; hence, these patients have exaggerated
caloric requirements.
Any adult with a burn greater than 15% (10% in children)
of TBSA has an increased nutritional requirement.
All patients with burns of 20% of TBSA or greater should
receive a nasogastric tube. (Feeding should start within 6
hours of the injury to reduce gut mucosal damage.)
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
Enteral nutrition is preferred.
Infection Control
The mainstay of both prevention and treatment is
1. daily washing with soap and water
2. application of a topical broad-spectrum antimicrobial
agent.
3. excision and grafting.
Physiotherapy and rehabilitation
Elevation,
splintage and exercise reduce swelling and improve the final
outcome.
Psychological support
OTHER TYPES OF BURN INJURY
Electrical Burn
• always a deep burn and needs hospitalization.
• wound of entry and wound of exit.
• Release of myoglobin due to damage of the muscles can
cause renal tubular damage and renal failure.
• Mannitol is used to prevent myoglobin induced renal
damage.
• Electrical injuries are divided into low and high voltage
injuries, the threshold being 1000 V.
• Low voltage injuries cause small localized deep burns.
They can cause cardiac arrest through normal pacing
interruption without significant direct myocardial damage.
• High voltage injuries cause damage by flash (external
burn) and conduction (internal burn).
Myocardium may be directly damaged without pacing
interruption.
A baseline ECG is recommended in all patients with
electrical injury.
Iraqia University College of Medicine Surgery
3
rd
stage Wed. 23
rd
– Mar – 2016 Dr. Firas Fadhil
Chemical Injury
• occur by strong acid or alkalies which produce burns as
long as the contact continues.
The severity depends on the amount and concentration of
the agent and the period of contact.
There may be superficial or deep burns.
Alkalies are usually the more destructive and especially
dangerous if they come in contact with the eyes.
• The initial management of any chemical injury is copious
lavage with water for a minimum of 30 minutes.
• In case of extensive tissue damage in chemical burns early
excision and skin grafting should be done.
Ionizing Radiation Injury
+These injuries can be divided into two groups
— localized injury which is much more common and
— whole body radiation injury.
Management of these injuries is mainly supportive.
Cold Injuries
Cold injuries are mainly of two types:
a. Injuries from industrial accidents e.g. liquid nitrogen.
b. Frost bite.
Prognosis
The Baux score (mortality = age + percent TBSA)
However, age and burn size, as well as inhalation injury,
continue to be the most robust markers for burn mortality.
