Approach to
Jaundice
DR.Bilal Natiq Nuaman
C.A.B.M. ,F.I.B.M.S. ,D.I.M. ,M.B.Ch.B.
2015-2016
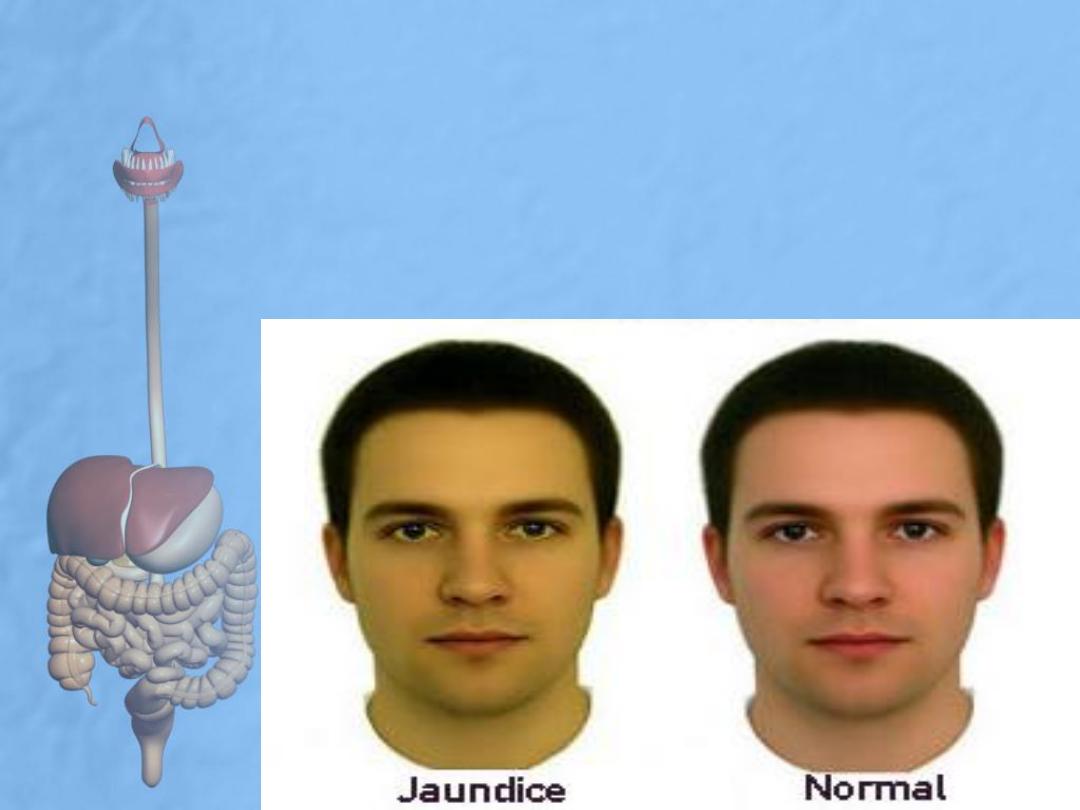
• Jaundice, or icterus, is a yellowish discoloration of the skin,
sclerae and mucous membranes due to hyperbilirubinaemia,
serum bilirubin >2mg/dl).
• The term jaundice comes from the French word jaune, meaning
yellow.
• It is a sign of either liver disease or, less often, a hemolytic
blood disorder.
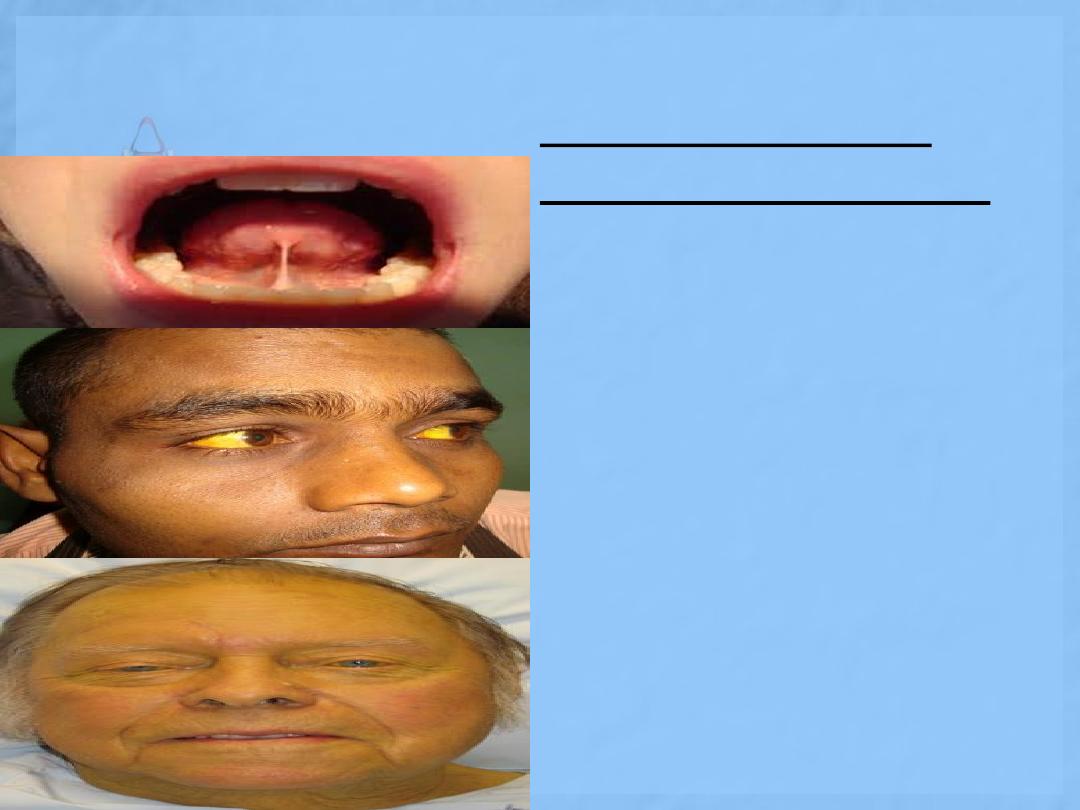
Sequential sites of
jaundice examination
1
st
stage:
frenulum of tongue
2
nd
stage:
sclera of eye
most important to
exclude carotinemia
3
rd
stage:
skin
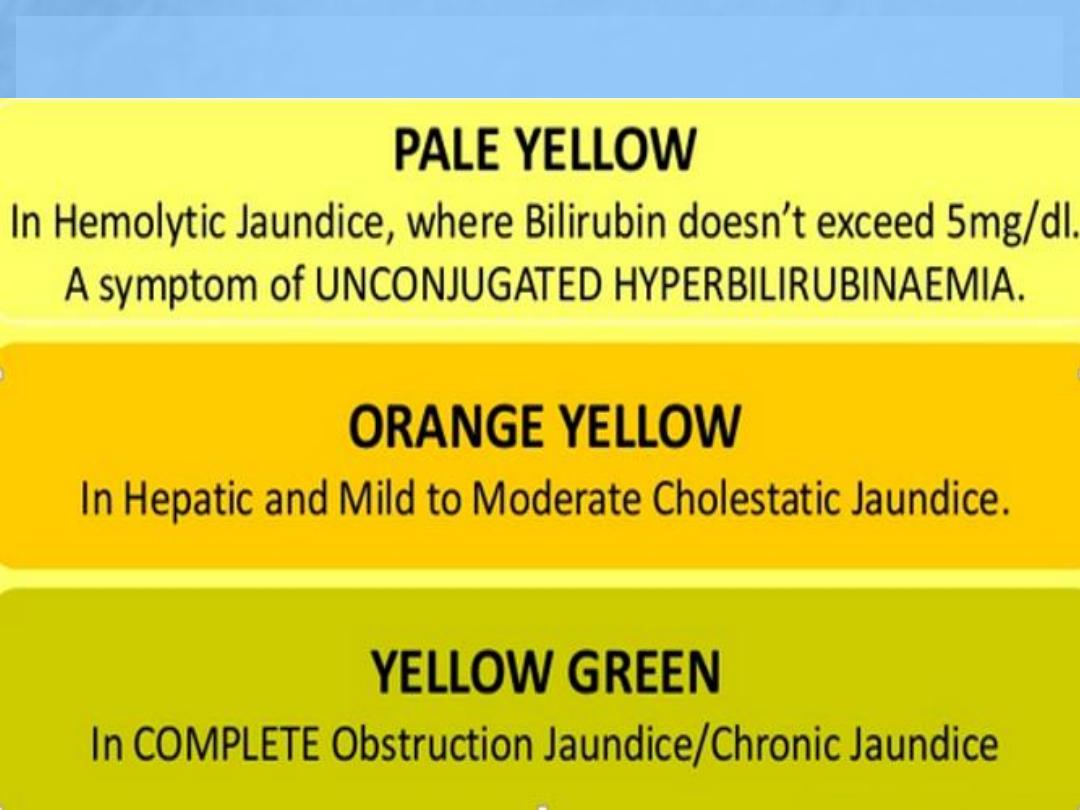
Sequential color change
• Normal serum bilirubin level is less than 1
mg/dl.
• In good light, most clinicians will recognize
jaundice when bilirubin levels exceeds 35-
45
µmol/L (2-2.5 mg/dL). (convertor factor
17)
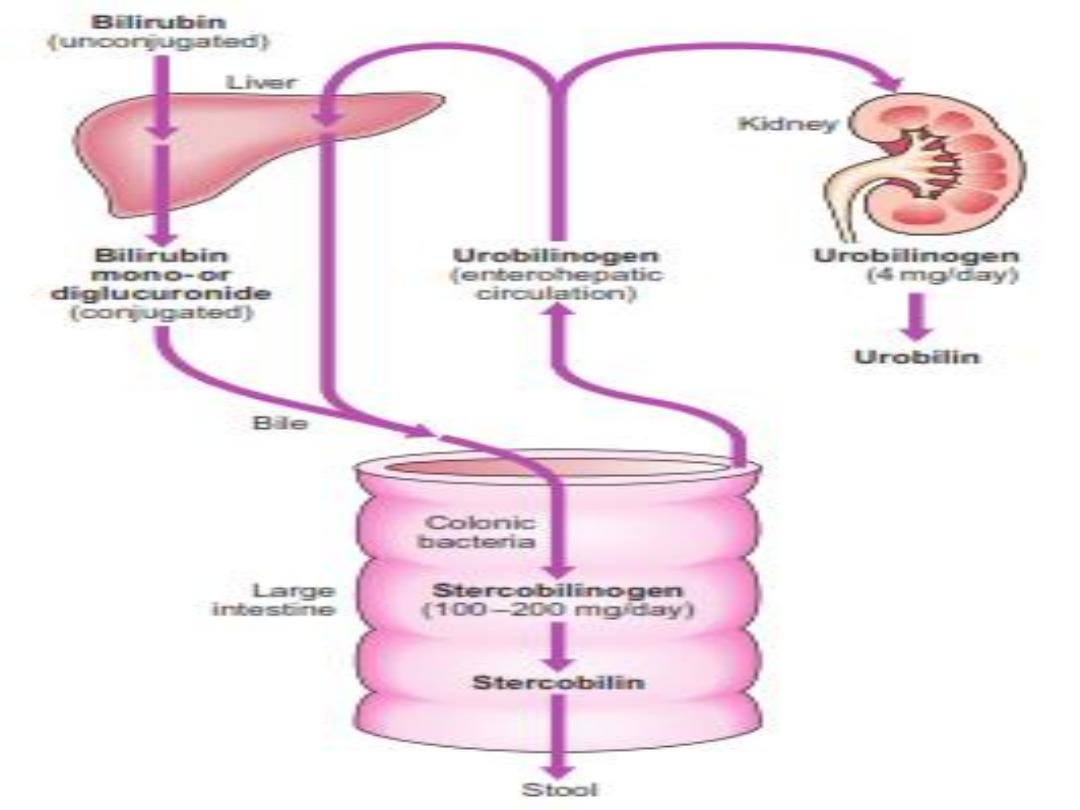
• Another sensitive indicator of increased
serum bilirubin is darkening of the urine,
which is due to the renal excretion of
conjugated bilirubin.
• Patients often describe their urine as tea- or
cola-colored.
• Bilirubinuria indicates an elevation of the
direct serum bilirubin fraction and,
therefore, the presence of liver disease
Gilbert’s
syndrome
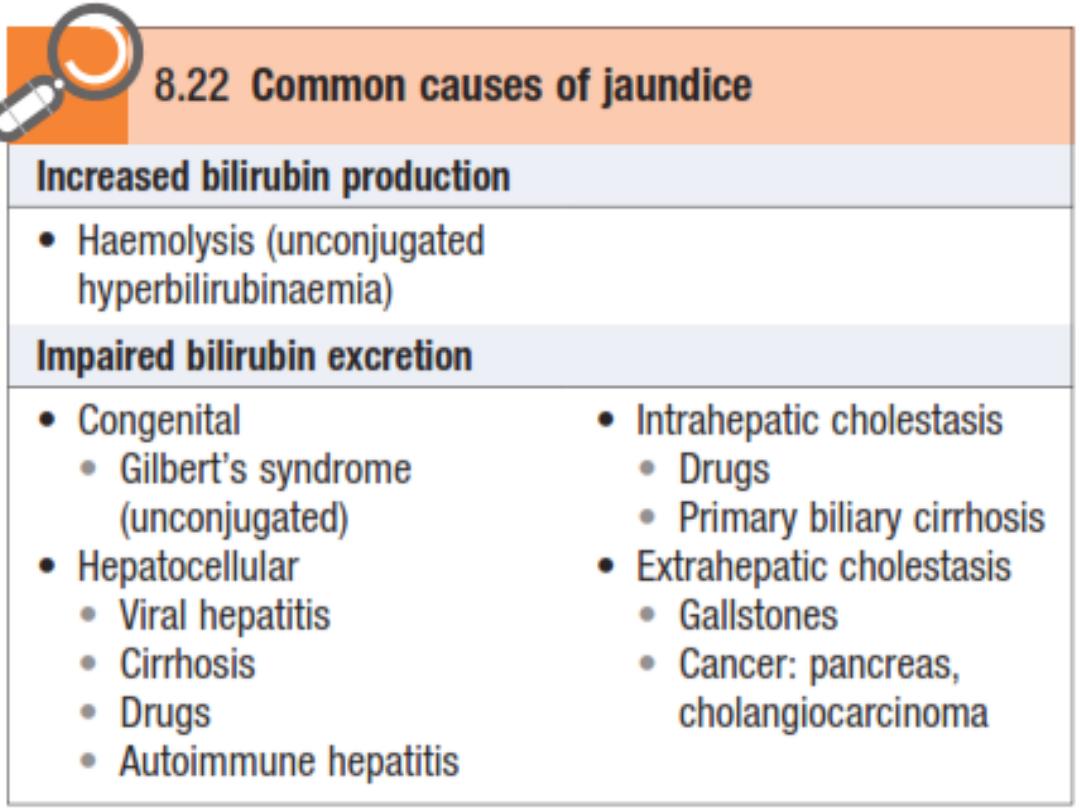
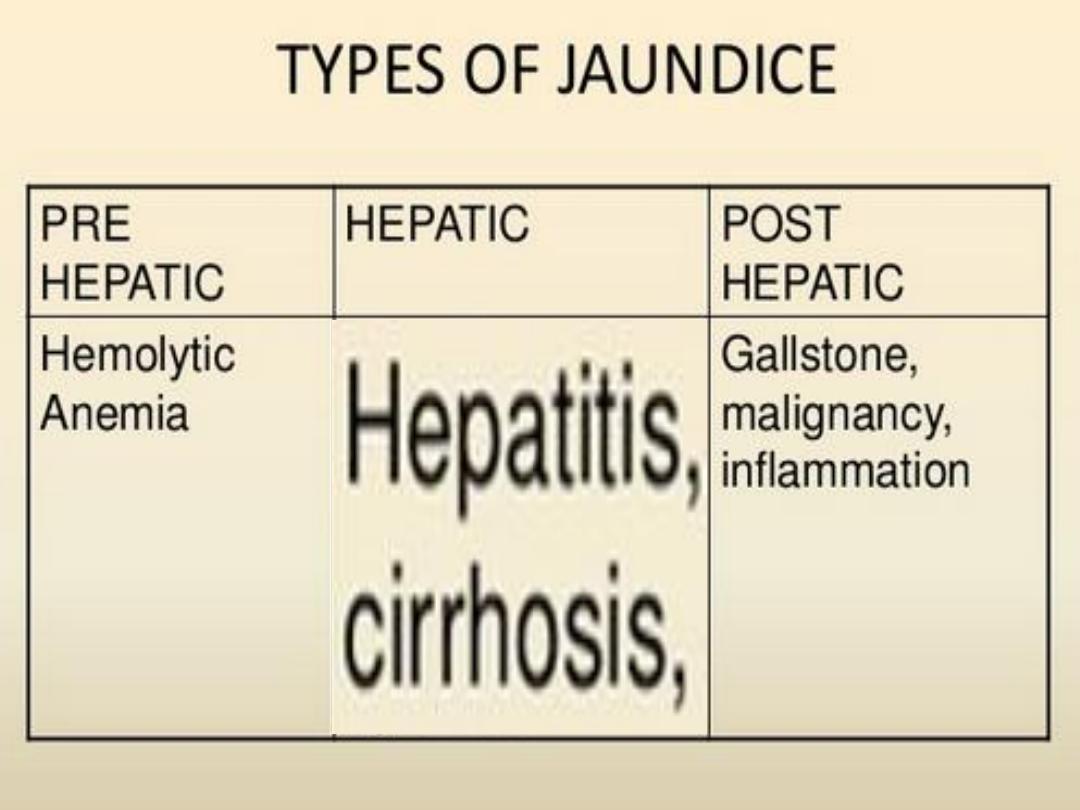
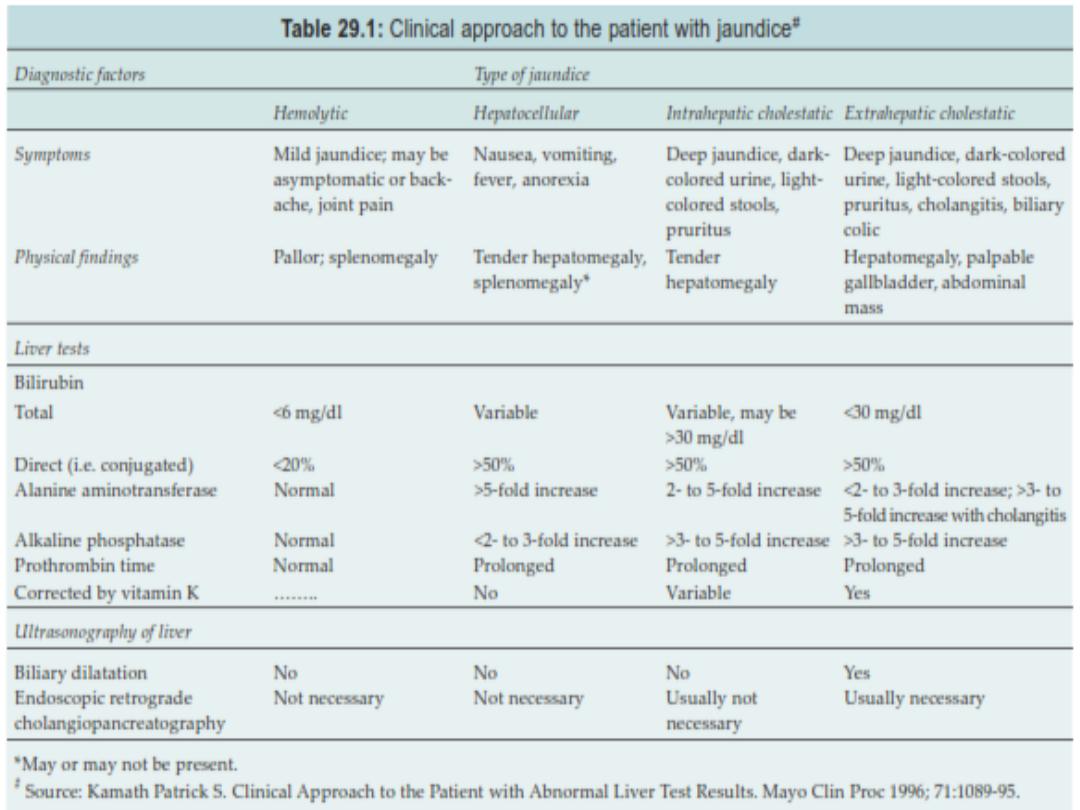
Prehepatic jaundice
In haemolytic disorders the accompanying anemic pallor
combined with jaundice may produce a pale lemon
complexion. The stools and urine are normal in color.
Gilbert’s syndrome is common and causes unconjugated
hyperbilirubinaemia. Serum liver enzyme concentrations
are normal and jaundice is mild (plasma bilirubin <100
µmol/l) but increases during prolonged fasting or
intercurrent febrile illness.
Hepatic jaundice
Hepatocellular disease causes hyperbilirubinaemia that is
both unconjugated and conjugated. Conjugated bilirubin is
soluble and filtered by the kidney, so
the urine is dark
brown.
The stools are normal in color.
Post-hepatic/ cholestatic (obstructive)
jaundice
In biliary obstruction, conjugated bilirubin in the bile does
not reach the intestine, so
the stools are pale.
Obstructive jaundice may be accompanied by pruritus
(generalized itch) due to skin deposition of bile salts.
Plasmodium falciparum
malaria causes pre-hepatic
, hepatic, and obstructive
jaundice
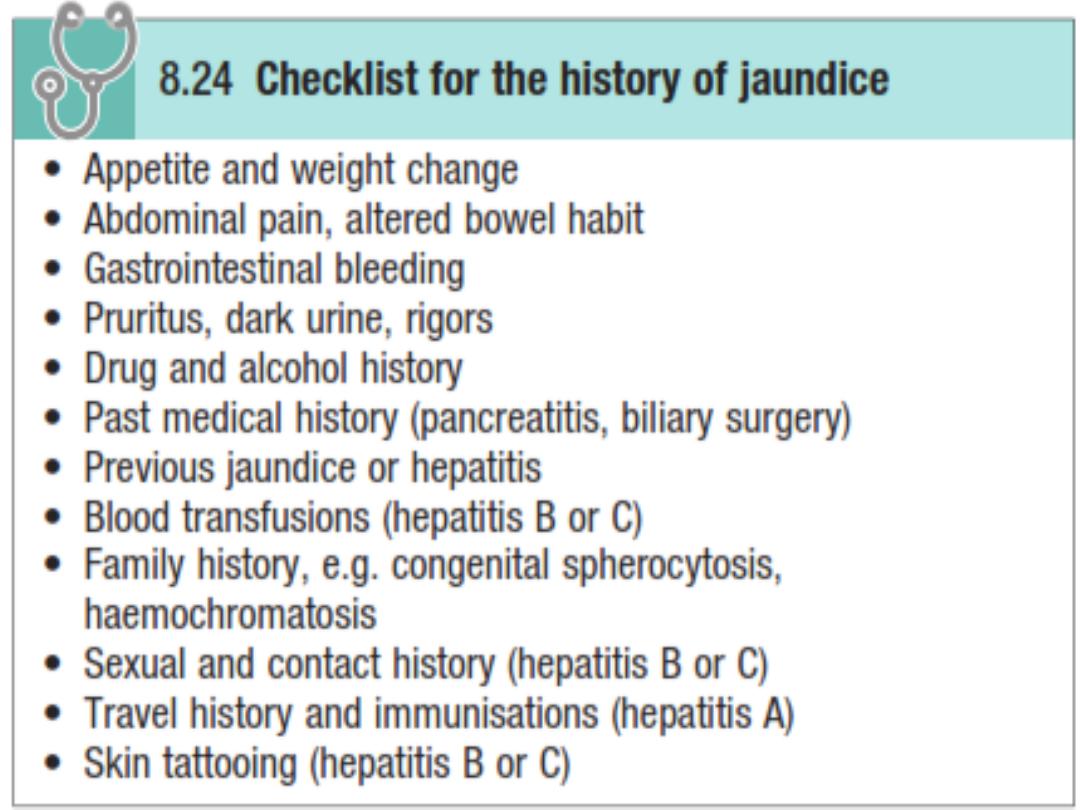
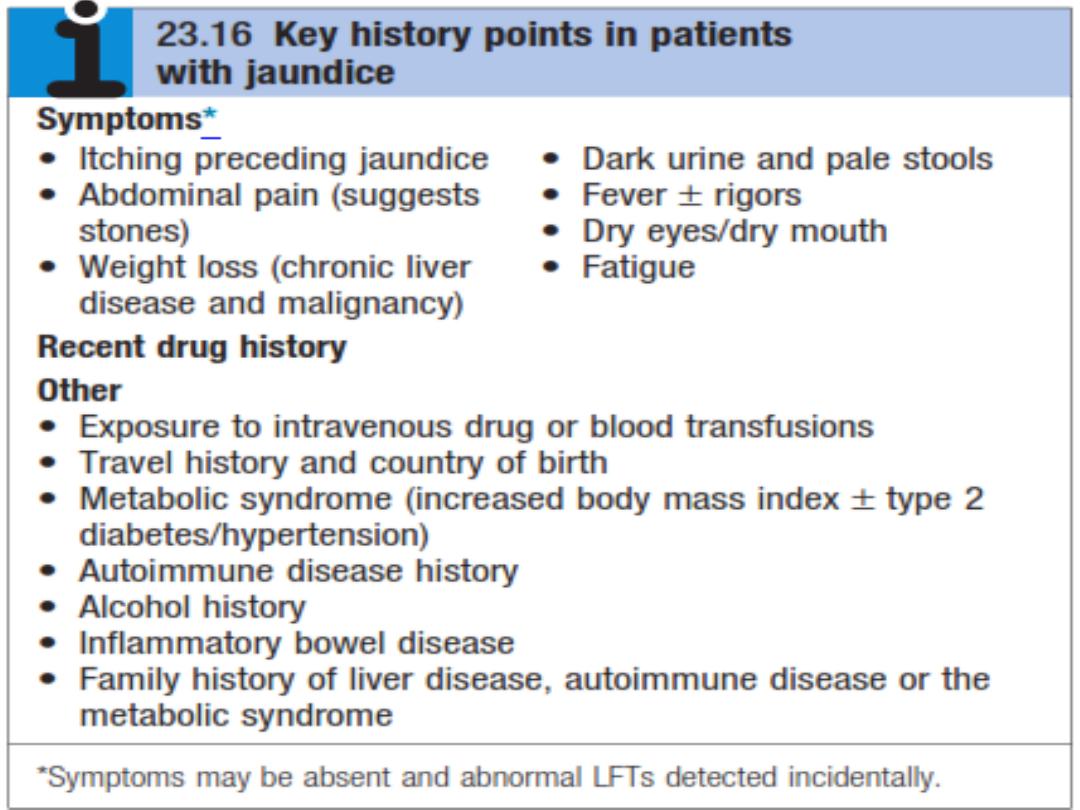
His or her age (hepatitis is more common in the young and
carcinoma in the elderly).
Sore throat and rash (infectious mononucleosis).
Occupation (Well's disease in sewerage and farm workers).
Contact with jaundice (hepatitis A).
Drug history (oral contraceptives, phenothiazines ,and
antiT.B. drugs).
Blood transfusions, injections (hepatitis B).
Alcohol consumption.
Pruritus (cholestasis due to hepatitis A, primary biliary
cirrhosis).
Colour of the uriue
Colour of the stools (pale stools in obstructive jaundice).
Abdominal pain (cholecystitis, gallstones, cholangitis,
carcinoma of the pancreas).
Fever, rigors and abdominal pain (suggests cholangitis).
• Is the jaundice acute or chronic?
• Acute onset of jaundice suggests
H
A
V
infection,
cholangitis, acute biliary tract obstruction, or acute liver
failure
.
• Gradual onset of jaundice points to
alcoholic liver disease
,
chronic liver disease (e.g.
H
B
V/H
C
V
infection).
• A lifelong history of jaundice suggests an
inherited
metabolic or hemolytic cause